Abstract
Lens dislocation is a significant complication after cataract surgery. Scleral fixation of 3-piece intraocular lens provides favorable visual outcome and can spare patients the need for lens exchange. Two patients presented with dislocated 3-piece lenses implanted over 10 years earlier. Both patients underwent pars plana vitrectomy and dropped lens rescue with scleral fixation. Postoperatively, the lens optic was found flipped nearly 90° at the optic-haptic junctions secondary to fluid-air exchange performed during vitrectomy. Both patients underwent intraocular lens exchange with a four point sclera fixated lens. Our study found that air tamponade is better avoided during rescue of old dislocated 3-piece lens implants. Intraocular lens exchange is preferred, when possible, to avoid complications associated with old dislocated lenses. Larger studies are needed to determine the effect of time on dislocated lens implants materials.
Keywords: intraocular lens, tilt, decentration, scleral fixation, fluid-air exchange
Introduction
Cataract surgery is an exceedingly common procedure in the United States. Typically, the surgery achieves successful outcomes with low rates of visually significant complications [1, 2]. However, among possible adverse events, rupture of the posterior capsule has been reported as the “most common serious complication” [2, 3]. Post-operative zonular instability or trauma can result in lens decentration or dislocation [2]. Obtaining a successful visual outcome following these events requires secure fixation of the intraocular lens (IOL).
Achieving secure IOL placement may occur via scleral or iris fixation, in addition to placing the lens in the anterior chamber. For scleral fixation, a sutured or a sutureless approach can be used to secure the lens haptics [4, 5]. Pertinent complications include suture erosion/breakage, lens decentration, and increase in the intraocular pressure (IOP) [6–8].
The IOL may tilt following placement in patients with poor lens or zonular support. Lens tilt is defined as the angle formed between the IOL optical axis and baseline axis [9]. The resulting positional change has the potential to alter visual acuity and lead to further complications such as astigmatism or Uveitis-Glaucoma-Hyphema syndrome [9, 10]. Here, we present two cases of significant lens tilt of scleral-fixated IOLs following fluid-air exchange (FAX) during concurrent vitrectomy. In each case, the lens was found to be nearly 90° flipped, having tilted at the both optic-haptic junctions. These cases represent a distinctive type of IOL damage in the setting of combined vitrectomy using FAX.
Cases presentation
Case 1
A 69-year-old female presented to clinic with a 3-day history of a floater in her right eye. Her ocular history was significant for cataract extraction with intraocular lenses placement in both eyes (OU) over 10 years earlier, retinal detachment repaired with vitrectomy in the right eye (OD), and retinal tears treated with laser in the left eye (OS). On clinical exam, visual acuity was 20/800 OD with pinhole correction to 20/200, and 20/25 OS. Slit-lamp examination demonstrated a posteriorly displaced posterior-chamber intraocular lens (PCIOL) OD with the lens capsule into the vitreous cavity, with the intraocular lens laying on the fundus. This was thought to be related to underlying zonulopathy as an examination roughly 1 year prior demonstrated pseudophakodonesis within the right IOL. Patient reported good vision before lens subluxation and requested to use the same lens if possible.
The patient underwent a vitrectomy, lens capsule removal from the dislocated lens, then scleral fixation of the dislocated IOL via modified Yamane technique. 7–0 Vicryl sutures were placed at the scleral tunnels to secure lens haptics. This procedure also involved endolaser photocoagulation of peripheral retinal scars, and partial FAX. On post-operative day one, the superior lens haptic was not visible at the sclera and thought to be displaced. IOP at this time was 16 mmHg. The patient returned to the operating room for repositioning of the intraocular lens wherein the superior haptic was retrieved through the superior scleral tunnel, cauterized the terminal bulb, and secured with 7–0 vicryl suture. Partial FAX was done to lower the risk of endophthalmitis and promote scleral wound closure; air was used rather than isovolumetric gas because of the lack of need for prolonged retinal tamponade [11–13]. At post-operative day one, the lens appeared tilted. Intraocular pressure at this time was 14 mmHg.
Three days later, the IOL optic remained tilted at the optic-haptic junction, so the patient underwent surgery for lens exchange. Intraoperatively, ophthalmic endoscopy revealed the lens haptics in the correct scleral orientation, but the optic was twisted 90°. This lens was then removed and replaced with an AKREOS lens, which was scleral fixated using non-absorbable 8–0 monofilament sutures. A year later, best corrected visual acuity was 20/60 OD with a centered lens implant.
Case 2
A 47-year-old female presented to clinic for evaluation of blurred vision OD. Past ocular history consisted of bilateral cataract extraction with IOL placement in addition to two vitrectomies on the left eye for IOL subluxation and epiretinal membrane. On examination, vision OD was 20/800 with posteriorly dislocated 3-piece IOL into the vitreous cavity atop the fundus.
The patient underwent pars plana vitrectomy (PPV). The lens capsule was removed from the dislocated lens followed by same lens scleral fixation and 7–0 Vicryl sutures to the scleral tunnels (Fig. 1). Ophthalmic endoscopy confirmed final position of the lens haptic in the sulcus, and partial FAX was performed.
Figure 1.
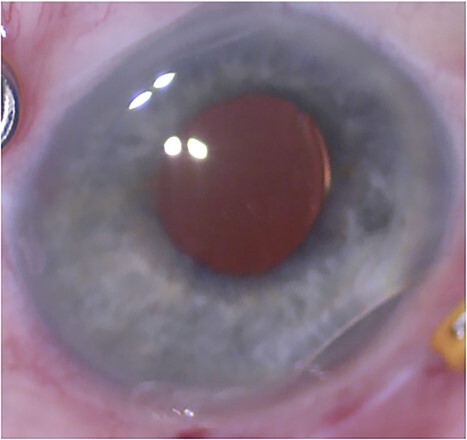
External photograph at the conclusion of initial scleral fixation. The IOL is well-positioned.
On post-operative day one, the lens optic was seen tilted (Fig. 2A) while the lens haptic were visible at the sclera superiorly and inferiorly. Intraocular pressure at this time was 6 mmHg. The patient was taken to surgery on the following week. Intraoperatively, the lens optic was found tilted nearly 90° with noticeable damage to the bilateral optic-haptic junctions (Fig. 2B) with intact haptic at orientation into the sclera on endoscopic view (Fig. 2C). The damaged lens was exchanged with an AKREOS lens fixated using 8–0 monofilament sutures as the previous case. FAX was performed once more. On post-operative day one, the AKREOS lens implant was well-positioned, intraocular pressure was 4 mmHg, and air bubble was visible in the vitreous. The AKREOS lens has been well-positioned more than a year later, with intraocular pressure within normal range (13 mmHg) and stable visual acuity of 20/25 + 2 measured at the most recent post-operative visits.
Figure 2.
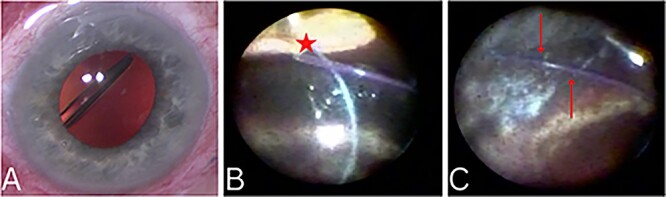
External photograph showing significant lens tilt (A). Ophthalmic endoscopy demonstrating lens tilt with twisting and subsequent damage to the optic-haptic junction (Star in 2B). Endoscopy revealed haptic remained secured in the scleral tunnel (Arrows in 2C).
Discussion
Our report of two cases detail significant lens optic tilt of scleral fixated 3-piece IOLs shortly after the use of FAX. Both patients had their lenses implanted over 10 year earlier and the same dislocated lenses were scleral fixated. However, the concern for this complication is to be balanced with the established benefits of air tamponade. For each of our reported patients, air tamponade was performed to promote scleral wound closure, and reduce the risk of post-operative infection and hypotony. Literature reviews on vitrectomy techniques supported the use of FAX with minimal to no cases of endophthalmitis following FAX [11, 12, 14]. Likewise, the use of air in vitrectomy can improve healing of vitrectomy incisions through the pressure applied to the internal wound-edges [11, 13].
One retrospective study found the most common complication of scleral-fixation with concurrent vitrectomy was elevated IOP [15], but this did not occur in our two patients. Low post-operative intraocular pressure early after surgery can result from wound leak. Surgical wounds leak needs immediate attention to avoid hypotony and other serious complications (e.g. endophthalmitis, choroidal hemorrhage). In Case 2, the IOP was 6mmhg on the first post-operative day. On anterior segment exam, the anterior chamber was formed with no corneal wound leak (Seidel negative). On dilated fundus exam, there was no choroidal effusion or choroidal hemorrhage displacing the lens, and the lens haptic were in the intended orientation. In this case, a possible etiology for the lower IOP on the first post-operative day is scleral tunnels leak during the first 24 h after surgery, but with air tamponade and pressure patch placed immediately after surgery the eye was able to maintain an IOP of 6 mmHg on the first post-operative day.
Other studies have examined the role of vitrectomy on lens tilt when combined with primary phacoemulsification with no lens scleral fixation [16–19]. Tan et al. found PPV was associated with a greater degree of IOL tilt and silicone oil tamponade to be positively correlated with IOL tilt, and Iwama et al. reported PPV with air tamponade to increase rate of tilt while Leiser et al. showed no significant effect from air tamponade. Shiraki et al. showed that tamponade with expansile gas leads to a sustained, statistically significant anterior shift of the lens position but no sustained change in IOL tilt after phaco-vitrectomy [17]. These studies show overall mixed results on the effect of different gas agents on IOL tilt and suggest the need for further studies. Beyond just lens positioning, our cases represent a new complication as they demonstrate structural damage to the optic-haptic junctions of scleral fixated lenses.
Kang and Joo reported cutting through the haptics of a one-piece lenses with a needle during scleral fixation. The proposed mechanism can be related to the increased flexibility and fragility of the hydrophobic IOL [20, 21]. Our cases were different because the haptics ends were fixated in scleral tunnels while the lens damage occurred at the optic-haptic junction. We believe the combination of air tamponade and use of older than 10 years dislocated lenses resulted in the mechanical optic rotation. In the context of our two presented cases, it may be beneficial to replace the dislocated IOLs, rather than attempting rescue of an aged lens.
IOL-capsule complex maybe fixated by passing the fixation sutures through the lens capsule, lens fenestrations (i.e. eyelets) and scleral [22]. The dislocated lenses in our patients did not have fenestrations to pass scleral fixations sutures through. The lens capsule can also be kept during in 3-piece IOL-capsule iris fixation, the lens haptic in contact with the iris and may cause iris transillumination defects, cystoid macular edema, or lens subluxation [23]. For lens haptics externalization approach, lens capsule removal from dislocated 3-piece lenses implants helped examining the haptics for existing damage, assure correct haptic orientation, and facilitated externalizing the haptics through the sclera. After discussing surgical procedure options with patients, scleral fixation through haptics externalization (modified Yamane) was selected by patients and surgeon.
The primary weakness of this study is our limited number of cases and retrospective nature of review. Future studies could employ prospective data collection on the use of air tamponade in combination with secondary IOL placement.
Conclusion
To conclude, scleral fixation of IOLs is a useful procedure performed when there is a lack of lens capsular support. Air tamponade is better avoided during rescue of old dislocated 3-piece IOLs. IOL exchange is preferred, when possible, to avoid complications associated with old lenses decay. Larger studies are needed to determine the effect of time on dislocated lens implants materials.
Contributor Information
Nathaniel W Cameron, Department of Ophthalmology, University of Kansas Medical Center, Kansas City, KS, United States.
Amin Karadaghy, Department of Ophthalmology, University of Kansas Medical Center, Kansas City, KS, United States.
Mary K Mitchell, Department of Ophthalmology, University of Kansas Medical Center, Kansas City, KS, United States.
Radwan S Ajlan, Department of Ophthalmology, University of Kansas Medical Center, Kansas City, KS, United States.
Author contributions
NC data collection and drafted the manuscript. AK manuscript editing and literature review. MM drafted and edited sections of the manuscript. RA data collection and manuscript editing. All authors read and approved the final manuscript.
Conflict of interest statement
All authors declare that they have no competing interests or conflicts of interest to disclose.
Funding
No funding was received for this study.
Data availability
All data available relevant to the cases described is included in the manuscript.
References
- 1. Powe NR, Schein OD, Gieser SC. et al. . Synthesis of the literature on visual acuity and complications following cataract extraction with intraocular lens implantation. Arch Ophthalmol 1994;112:239–52. [DOI] [PubMed] [Google Scholar]
- 2. Kohnen T, Wang L, Friedman N, Koch D. Complications of Cataract Surgery. In: Ophthalmology [Elsevier]. 5th ed. Elsevier Inc. The Netherlands; [cited 2022 Oct 3]. p. 401–9. Available from: https://www.clinicalkey.com/#!/content/book/3-s2.0-B9780323528191001985?scrollTo=%23hl0000510. [Google Scholar]
- 3. Ng DT, Rowe NA, Francis IC. et al. . Intraoperative complications of 1000 phacoemulsification procedures: a prospective study. J Cataract Refract Surg 1998;24:1390–5. [DOI] [PubMed] [Google Scholar]
- 4. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged Intrascleral intraocular lens fixation with double-needle technique. Ophthalmology 2017;124:1136–42. [DOI] [PubMed] [Google Scholar]
- 5. Yamane S, Ito A. Flanged fixation: Yamane technique and its application. Curr Opin Ophthalmol 2021;32:19–24. [DOI] [PubMed] [Google Scholar]
- 6. Solomon K, Gussler JR, Gussler C, Van Meter WS. Incidence and management of complications of transsclerally sutured posterior chamber lenses. J Cataract Refract Surg 1993;19:488–93. [DOI] [PubMed] [Google Scholar]
- 7. Davies EC, Pineda R. Complications of scleral-fixated intraocular lenses. Semin Ophthalmol 2018;33:23–8. [DOI] [PubMed] [Google Scholar]
- 8. Shahid SM, Flores-Sánchez BC, Chan EW. et al. . Scleral-fixated intraocular lens implants—evolution of surgical techniques and future developments. Eye 2021;35:2930–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Intraocular Lens (IOL) Tilt and Astigmatism – EyeWiki [The United States of America]. [cited 2022 Sep 28]. Available from:https://eyewiki.aao.org/Intraocular_Lens_(IOL)_Tilt_and_Astigmatism#cite_note-2.
- 10. Guyton DL, Uozato H, Wisnicki HJ. Rapid determination of intraocular lens tilt and Decentration through the Undilated pupil. Ophthalmology 1990;97:1259–64. [DOI] [PubMed] [Google Scholar]
- 11. Warrier SK, Jain R, Gilhotra JS, Newland HS. Sutureless vitrectomy. Indian J Ophthalmol 2008;56:453–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Scott IU, Flynn HWJ, Dev S. et al. . Endophthalmitis after 25-gauge and 20-gauge pars plana vitrectomy: incidence and outcomes. Retina 2008;28:138–42. [DOI] [PubMed] [Google Scholar]
- 13. Rizzo S, Genovesi-Ebert F, Vento A. et al. . Modified incision in 25-gauge vitrectomy in the creation of a tunneled airtight sclerotomy: an ultrabiomicroscopic study. Graefes Arch Clin Exp Ophthalmol 2007;245:1281–8. [DOI] [PubMed] [Google Scholar]
- 14. Bahrani HM, Fazelat AA, Thomas M. et al. . Endophthalmitis in the era of small gauge Transconjunctival Sutureless vitrectomy—meta analysis and review of literature. Semin Ophthalmol 2010;25:275–82. [DOI] [PubMed] [Google Scholar]
- 15. Melamud A, Topilow JS, Cai L, He X. Pars Plana vitrectomy combined with either secondary scleral-fixated or anterior chamber intraocular lens implantation. Am J Ophthalmol 2016;168:177–82. [DOI] [PubMed] [Google Scholar]
- 16. Shiraki N, Wakabayashi T, Sakaguchi H, Nishida K. Effect of gas tamponade on the intraocular lens position and refractive error after Phacovitrectomy: a swept-source anterior segment OCT analysis. Ophthalmology 2020;127:511–5. [DOI] [PubMed] [Google Scholar]
- 17. Leisser C, Hirnschall N, Findl O. Effect of air tamponade on tilt of the intraocular lens after Phacovitrectomy. Ophthalmologica 2019;242:118–22. [DOI] [PubMed] [Google Scholar]
- 18. Tan X, Liu Z, Chen X. et al. . Characteristics and risk factors of intraocular lens tilt and Decentration of phacoemulsification after pars Plana vitrectomy. Transl Vis Sci Technol 2021 Mar 24;10:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Iwama Y, Maeda N, Ikeda T. et al. . Impact of vitrectomy and air tamponade on aspheric intraocular lens tilt and decentration and ocular higher-order aberrations: phacovitrectomy versus cataract surgery. Jpn J Ophthalmol 2020;64:359–66. [DOI] [PubMed] [Google Scholar]
- 20. Kang MJ, Joo CK. Three cases of a torn haptic after scleral fixation using a hydrophobic acrylic intraocular lens: case reports. Medicine (Baltimore) 2018;97:e9853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gregori NZ, Spencer TS, Mamalis N, Olson RJ. In vitro comparison of glistening formation among hydrophobic acrylic intraocular lenses. J Cataract Refract Surg 2002;28:1262–8. [DOI] [PubMed] [Google Scholar]
- 22. Scleral Fixated Intraocular Lens – EyeWiki [The United States of America]. [cited 2022 Oct 4]. Available from:https://eyewiki.aao.org/Scleral_Fixated_Intraocular_Lens.
- 23. Dzhaber D, Mustafa OM, Tian J. et al. . Outcomes and complications of iris-fixated intraocular lenses in cases with inadequate capsular support and complex ophthalmic history. Eye Lond Engl 2020;34:1875–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data available relevant to the cases described is included in the manuscript.


