Abstract
Tension pneumothorax (TPX) is a severe chest complication of blunt or penetrating trauma. Immediate decompression is the lifesaving action in patients with TPX. Needle decompression (ND) is frequently used for this purpose, particularly in limited resources setting such as the prehospital arena. Despite the safe profile, the blind nature of the procedure can result in a serious range of complications, including injury to the vital intrathoracic structures such as the lungs, great vessels, and heart. Here, we reported 2 cases of blunt chest trauma resulting in TPX demanding immediate ND; however, nonintentional pericardial and pulmonary artery injuries occurred. The first case was a 42-year-old man with a needle-related pulmonary artery injury that required surgery. The second case was a 19-year-old man in whom a needle-related pneumopericardium occurred and was treated conservatively. In both cases, trained personnel performed the ND. Although ND in the field is a lifesaving intervention, it may further complicate the patient condition. Therefore, it should be performed in adherence to the universal guidelines.
Keywords: trauma, pneumopericardium, needle decompression, tension pneumothorax
Introduction
Tension pneumothorax (TPX) is a cause of preventable death in trauma. 1 Penetrating trauma with TPX can occur in up to 50% of patients. 1 In military practice, it is responsible for up to 33% of preventable battlefield deaths. 2 Immediate decompression can be lifesaving. 3 Decompression can be done by needle (ND), finger, or tube thoracocentesis (TT). Tube thoracocentesis is the definitive procedure. However, the needle is a lifesaver when TT is unavailable, such as prehospital settings. 4
We report 2 cases of needle-related intrathoracic injuries after ND placement in the field (prehospital). The needle injured the pulmonary artery with subsequent cardiac tamponade in one case and with pneumopericardium in the second one. In both cases, an anterior approach was performed (needle was in a left anterior position and inserted by the critical care paramedics [CCP] of the emergency medical services [EMS] staff).
Case Presentation I
A 42-year-old man fell from 3.5 m height. He had an initial Glasgow Coma Scale (GCS) score of 11 and a right-sided chest injury with subcutaneous emphysema in addition to head injury. He was desaturating (initial SaO2 of 82%) with a GCS of 8 requiring rapid sequence intubation. Post-intubation desaturation was dramatic (SaO2 63%). The CCP of the EMS team performed a quick DOPES (D: displacement, O: obstruction, P: pneumothorax, E: equipment failure, and S: secretions) approach 5 to identify the cause of the patient desaturation. Bilateral pneumothorax was suspected and managed with bilateral needle decompression (ND), using an angiocath (3.25 inch and 14 Gauge) in the midclavicular line (MCL) at the second intercostal space (ICS) on both sides. A gush of air was observed but soon stopped.
Due to persistent desaturation, a second needle was inserted lateral to the first one at the same space, but the low oximetry reading continued en route to the hospital; therefore, a third needle was inserted laterally in the fifth ICS anterior to the mid-axillary line with minimal effect. Upon arrival to the trauma resuscitation bay, the patient’s saturation worsened, with a drop in blood pressure.
Extended focused assessment sonography for trauma (eFAST) revealed bilateral pneumothoraces. Bilateral chest tubes were inserted immediately without removing the previous catheters, releasing a significant amount of air. Following this, the saturation and pressure improved. The second left-sided anterior catheter started to drain dark blood (Figure 1); the patient became hypotensive; a repeated eFAST examination revealed pericardial tamponade (Figure 2). The patient was immediately taken to the operating room (OR) and the tamponade was released through a subxiphoid pericardial window followed by an anterolateral thoracotomy. Exploration revealed a through-and-through lung injury (Figure 3), with an anterior puncture to the pulmonary artery just distal to its emergence from the right ventricle. The arterial repair was done with one stitch using Proline 4:0 sutures (Figure 4). Postoperatively, computed tomography (CT) of the head showed a severe head injury and a decompressive craniectomy was performed. Although he continued to be hemodynamically stable, he was diagnosed as brain dead after a few days.
Figure 1.

Bilateral needle decompression at second intercostal space; notice blood emerging from laterally placed left catheter directed downward and medially, it is not perpendicular to the chest wall.
Figure 2.
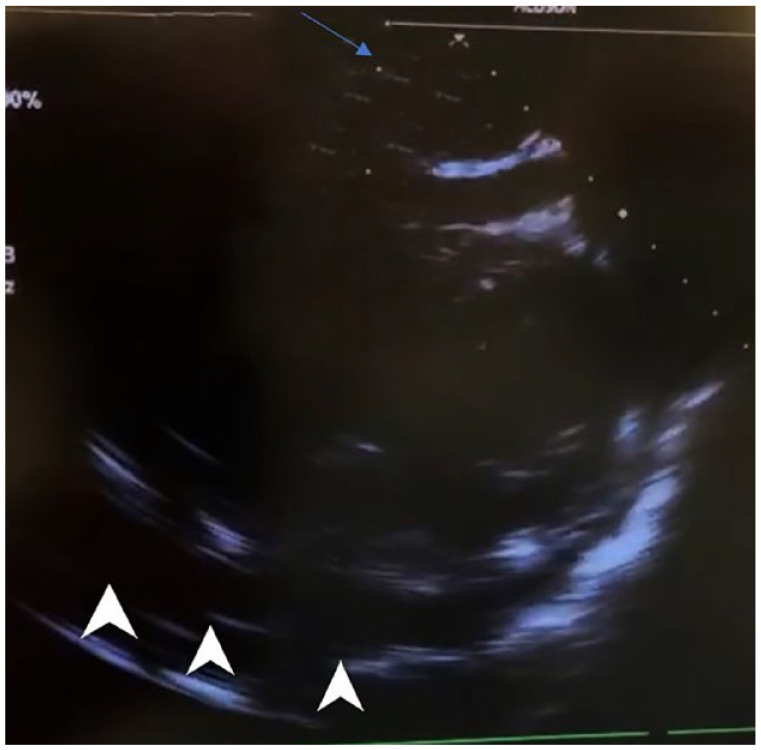
eFAST with evidence of pericardial fluid (Tamponade) on subxiphoid view (3 arrows).
Figure 3.
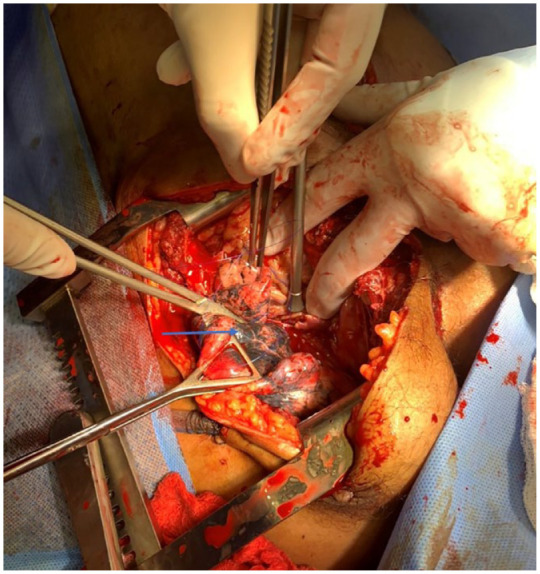
Intraoperative view of the lung injury (through and through).
Figure 4.
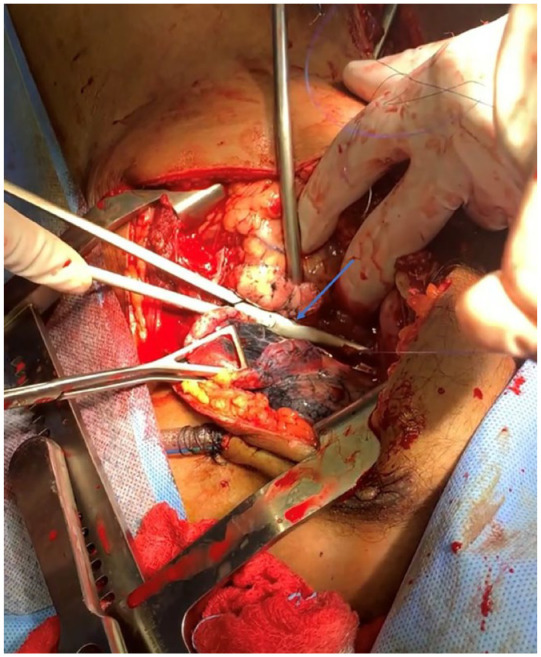
Repair of cardiac injury with Proline 4/0 “Figure of 8” technique.
Case Presentation II
A 19-year-old man with head and chest trauma secondary to a motor vehicle collision was intubated at the scene for a low GCS, and a ND was attempted many times for a low O2 saturation (68%). Upon arrival, the patient was vitally stable with a saturation of 90% on FiO2 of 100%. The trauma team noticed that the decompressing needle was medially directed and pulsating, and therefore, a chest x-ray was obtained (Figures 5 and 6). The needle was pushed out (halfway) during log rolling the patient. The needle was safely taken out after chest tube insertion. A CT scan showed extensive pneumopericardium, pneumomediastinum, and subcutaneous emphysema extending to the neck (Figures 7 and 8). The saturation was corrected after chest tube insertion, and the patient was admitted to the intensive care unit (ICU) for head injury management.
Figure 5.

Case II: the needle decompression(ND) directed medially toward the heart. It shows misplacement of the needle decompression (it should be midclavicular), and markers of repeated attempts are also misplaced.
Figure 6.
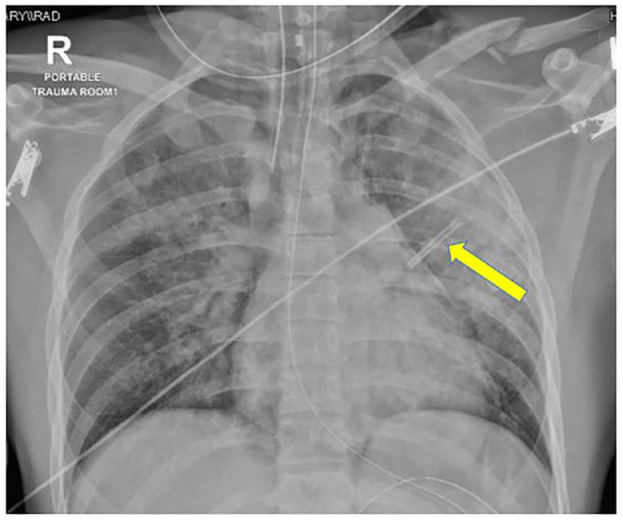
Case II: chest x-ray shows the decompression catheter touching the heart.
Figure 7.
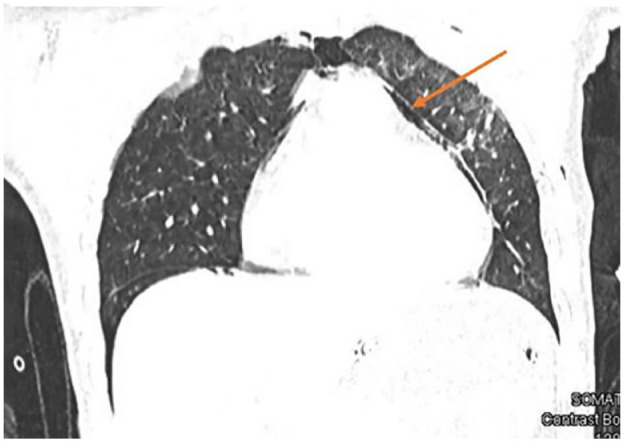
Case II: computed tomography scan of the chest showing a pneumopericardium.
Figure 8.
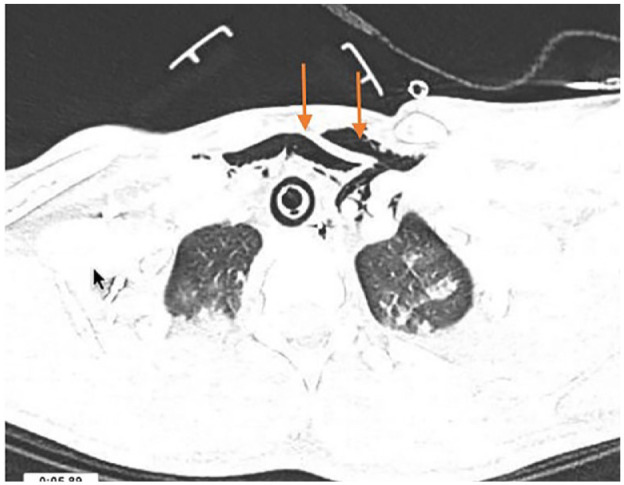
Case II: subcutaneous emphysema that extended to the root of the neck.
Discussion
We presented 2 cases with TPX treated with ND at the scene and complicated with injuries of the pulmonary artery and the pericardium. Tension pneumothorax is a life-threatening injury and requires immediate recognition and decompression. 4 The incidence of TPX varies between 1% and 30%, and up to 50% in penetrating trauma. 1 Bilateral TPXs are rare. Here, the 2 reported cases showed multiple attempts at ND with misplacements related to the direction of the needle or the location of the needle by a trained staff member.
Trauma patients with TPX can present with chest pain, respiratory distress, tracheal deviation, congested neck veins, and in extreme cases, hypotension. 5 The diagnosis should be made clinically, especially in the prehospital setting, which requires a high index of suspicion. Bedside ultrasound can support this diagnosis (absence of pleural sliding) in the emergency department (ED). Chest decompression can be integral in resuscitating traumatic cardiac arrest patients. 5 For differential diagnosis, DOPES checklist can be applied to determine the possible cause of post-intubation hypoxia, as well as the possibility of a right main stem bronchus intubation, lung collapse, as well as auscultation errors.5,6
Immediate chest decompression is lifesaving and can be achieved in different ways. Although chest tubes are the definitive intervention, in settings where access to that is limited, such as in the prehospital settings, ND is the available immediate intervention.4,5 Traditionally, it can be done through the anterior approach at midclavicular in the second ICS. Recently, a move to a lateral approach at either Anterior Axillary Line (AAL) or Mid Axillary Line (MAL) (fourth or fifth ICS) showed a better success rate. The Advanced Trauma Life Support (ATLS) recommends lateral and anterior location in adults and children, respectively. 4
Chang et al 7 report on the CT-based assessment of chest wall thickness at the anterior and lateral positions and demonstrated that a needle length of 8.0 cm is longer than 96% of chest wall thicknesses. They concluded that a longer needle has a higher success rate than the shorter one for pneumothorax decompression. Although longer needles have a higher success rate, they are more likely to produce intrathoracic iatrogenic injuries, especially if misplaced or misdirected.
Overall, the “catheter-over-needle” device is considered safe; nevertheless, complications can be severe and devastating. Complications include pneumothorax, particularly in chronic obstructive pulmonary disease, hemothorax, cardiovascular injuries, nerve injuries, and infections have occurred. 8
The most commonly reported complication of anteriorly placed needles is failure to relieve the pneumothorax. Possible explanations include disparity between the length of needles and chest wall thickness. 8 Evidence supports the ability of longer needles reaching the pleural space and effectively releasing the tension and draining the air. The angiocath (catheter-over-needle 14-gauge, 3.25 inch in length) is preferred over the traditional Venflons (5 cm), which are shorter and have high chances of kinking or dislodgement. Tamponade after ND of a suspected TPX is a recognized, critical complication.9,10
Conclusion
Needle decompression is an emergency lifesaving intervention in the suboptimal trauma setting. However, the risks of injury are heightened by the emergent blind nature of the procedure. Its high failure rate in the prehospital phase and its possible fatal complications raise the question of optimization. The clinical need for the procedure, diligence in the needle selection, attention to landmarks and needle insertion technique, and consideration of alternative means of decompression such as finger or TT must always be considered, as well as an awareness of potential complications. Technological point-of-care support such as ultrasound may improve diagnosis and decrease the complication rate.
Acknowledgments
We thank the cardiothoracic surgery team, ambulance service staff of Hamad Medical Corporation (HMC), and the Trauma Research Office at Hamad General Hospital.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: The Medical Research Centre of HMC, Doha, Qatar, has granted permission (MRC-04-23-571) for this case report to be published on condition that no patient identifiable data (including patient name and photograph) are included.
Informed Consent: As data were collected anomalously and retrospectively with no direct contact with the patients and no patient identifier or photos, the medical research center granted the approval for this publication (MRC-04-23-571) without an informed consent.
ORCID iDs: James Laughton  https://orcid.org/0000-0002-9486-5157
https://orcid.org/0000-0002-9486-5157
Ayman El-Menyar  https://orcid.org/0000-0003-2584-953X
https://orcid.org/0000-0003-2584-953X
References
- 1. Sharrock MK, Shannon B, Garcia Gonzalez C, et al. Prehospital paramedic pleural decompression: a systematic review. Injury. 2021;52(10):2778-2786. [DOI] [PubMed] [Google Scholar]
- 2. Kotwal RS, Montgomery HR, Kotwal BM, et al. Eliminating preventable death on the battlefield. Arch Surg. 2011;146:1350-1358. [DOI] [PubMed] [Google Scholar]
- 3. Jalota R, Sayad E. Tension Pneumothorax. Updated August 11, 2020. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK559090/ [Google Scholar]
- 4. American College of Surgeons Committee on Trauma: Advanced Trauma Life Support for Doctors . ATLS Student Course Manual. American College of Surgeons; 2018. [Google Scholar]
- 5. Cusmà Piccione R. “DOPES”: acronym to help critical care nurses in the intensive care unit during the COVID Age. Dimens Crit Care Nurs. 2021;40:129-130. [DOI] [PubMed] [Google Scholar]
- 6. Mistry N, Bleetman A, Roberts KJ. Chest decompression during the resuscitation of patients in prehospital traumatic cardiac arrest. Emerg Med J. 2009;26(10):738-740. [DOI] [PubMed] [Google Scholar]
- 7. Chang SJ, Ross SW, Kiefer DJ, et al. Evaluation of 8.0-cm needle at the fourth anterior axillary line for needle chest decompression of tension pneumothorax. J Trauma Acute Care Surg. 2014;76(4):1029-1034. [DOI] [PubMed] [Google Scholar]
- 8. Wernick B, Hon HH, Mubang RN, et al. Complications of needle thoracostomy: a comprehensive clinical review. Int J Crit Illn Inj Sci. 2015;5(3):160-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Butler KL, Best IM, Weaver WL, et al. Pulmonary artery injury and cardiac tamponade after needle decompression of a suspected tension pneumothorax. J Trauma. 2003;54(3):610-611. [DOI] [PubMed] [Google Scholar]
- 10. Thomas A, Wilkinson KH, Young K, et al. Complications from needle thoracostomy: penetration of the myocardium. Prehosp Emerg Care. 2021;25(3):438-440. [DOI] [PubMed] [Google Scholar]


