Abstract
Objectives:
Stigmatization was reported throughout the COVID pandemic for COVID-19 patients and close contacts. The aim of this systematic review was to comprehensively examine the prevalence and impact of stigmatization during COVID-19 pandemic.
Methods:
English articles were searched using online databases that included PubMed, Scopus, Embase, and Web of Science up to 24 August 2022. A two-step screening and selection process was followed utilizing an inclusion and exclusion criteria and then data was extracted from eligible articles. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist was followed, and the risk of bias was assessed using the Newcastle-Ottawa Scale.
Results:
Seventy-six studies were eligible for inclusion. Twenty-two studies reported the prevalence of social stigma due to COVID-19 infection with social isolation being the most commonly reported stigma. There were 20 studies that reported the majority of participants experienced stigma due to COVID-19 infection, which was as high as 100% of participants in two studies. Participants in 16 studies reported blaming from others as the second most common type of stigma, with various other types reported such as psychological pressure, verbal violence, avoidance, and labeling. The most common effect of the stigma was anxiety followed by depression, and then reduction of socialization.
Conclusion:
Findings from the present review have identified that COVID-19-related stigma studies have generally focused on its prevalence, type, and outcome. Greater awareness of this topic may assist with improving public education during pandemics such as COVID-19 as well as access to support services for individuals impacted by stigmatization.
Keywords: COVID-19, SARS-CoV-2, stigma, social stigma, public stigma
Introduction
People who are considered to be a possible source of disease and may constitute a threat to social life in society may be subjected to stigmatization. 1 Consequently, this activity is associated with unfavorable discriminating attitudes, sentiments, and behaviors against persons with specific physical, behavioral, or ethnic characteristics who are considered a risk to society. 2
Historically, stigma has been related to several infectious diseases, resulting in prejudice against particular patient groups, with harmful repercussions for both people and society.3,4 During epidemics or pandemics, social anxiety emerges from concern about a disease with an unknown source and potentially lethal consequence, particularly when patient safety procedures such as isolation and quarantine are used to ensure community safety. 5
It seems to be a cultural tendency to accuse someone of the outbreak. This issue has deteriorated because of unproven claims about the virus. As a result, even individuals who have recovered and have passed their quarantine time may face social stigma. Groups susceptible to social stigma face discrimination in the manner of rejection by those who boycott and disregard them, as well as denial of good medical care and access to social facilities. They are also subjected to physical and verbal assault. 6
After COVID-19 was announced as a pandemic,7–9 individuals all over the world readily adopted stigmatizing attitudes and beliefs against COVID-19 patients and their close connections, as well as places, people, and ethnic communities suspected to be the source of the pandemic.10,11 COVID-19-related stigma results in a wide range of undesirable outcomes, including hesitation to access health care services after testing positive for the COVID-19 infection and severe exacerbations of pre-existing mental health issues. 12
COVID-19 patients may be charged with not obeying to stay in a safe place or neglecting to take precautions when moving outside. 13 Even if people have not been infected with the virus, they may be stigmatized. Someone with allergies, for instance, who has coughing and sneezing, may be embarrassed in society. 14
Exploration of the impact of stigma during the COVID pandemic is of great importance in identifying its effects and developing strategies to minimize any harmful effects. The aim of this systematic review was to comprehensively examine the prevalence and impact of stigmatization during COVID-19 pandemic.
Methods
This systematic review comprehensively explored the social stigma during the COVID-19 pandemic with regard to prevailing literature. To ensure that the outcomes reported were reliable and authentic, this review conforms to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist.
Data sources
Four online databases were searched including PubMed, Scopus, Embase, and Web of Science for relevant articles published in English until 24 August 2022. Keywords and their combinations were used when searching the databases and are shown below:
“Coronavirus disease 2019” OR “COVID-19” OR “Novel coronavirus” OR “2019-nCoV” OR “SARS-CoV2” OR “Severe acute respiratory syndrome coronavirus 2” OR “SARS-CoV-2” [Title/Abstract]
“Stigma” OR “Social stigma” OR “Public stigma” [Title/Abstract]
[A] and [B]
Study selection
A two-step screening and selection process was used to identify eligible articles. Initially, seven researchers assessed titles and abstracts and cultivated appropriate articles for the second and more diligent step. This second step involved full-text screening which was carried out by another five researchers. Studies were eligible for inclusion in our investigation if they were original and descriptive articles that were written in English language and published in a peer-reviewed journal related to stigma/social stigma during COVID-19. Exclusion of studies occurred for any systematic review publications, non-human research studies, investigations lacking published data, studies including abstracts without available full text, duplicated articles, case series, case reports, conference abstracts, letters to editors, preprints, and opinions.
Data extraction
Data extraction was performed for the studies that met the eligibility criteria. Five researchers were responsible for the extraction of data from the full texts. Another researcher was responsible for checking the eligibility of the included papers (i.e., possible duplications of papers) and the accuracy of extracted data. Data/information extracted included ID, reference number, and country of origin of the publications, articles type of social stigma, prevalence of social stigma, outcome of social stigma, and other important findings relevant to the research topic.
Quality assessment and bias risk evaluation
We utilized Newcastle-Ottawa Scale (NOS) 15 to evaluate the bias risk of the included studies. The criterion of this numerical tool is divided into three sections that include selection, comparability, and exposure/outcome. Maximum values of 4, 2, and 3 are allocated to these sections respectively. Studies are graded one point each for all items except for comparability which has the potential to score up to two points, with the minimum and maximum possible scores of 0 and 9. Studies which are rated 0–2 are considered poor quality, 3–5 are fair quality, and 6–9 are considered good/high quality. Table 1 shows ratings for individual studies by this tool.
Table 1.
Risk of bias for the included studies.
| Reference | Selection (out of 4) | Comparability (out of 2) | Exposure/outcome (out of 3) | Total (out of 9) |
|---|---|---|---|---|
| 16 | *** | ** | *** | 8 |
| 17 | **** | ** | *** | 9 |
| 18 | ** | ** | *** | 7 |
| 19 | ** | ** | ** | 6 |
| 20 | **** | ** | ** | 8 |
| 21 | *** | * | * | 5 |
| 22 | **** | * | ** | 7 |
| 23 | **** | ** | *** | 9 |
| 24 | **** | ** | *** | 9 |
| 25 | *** | ** | *** | 8 |
| 26 | *** | * | * | 5 |
| 27 | ** | ** | *** | 7 |
| 28 | * | ** | *** | 6 |
| 29 | *** | ** | *** | 8 |
| 30 | **** | ** | *** | 9 |
| 31 | *** | * | * | 5 |
| 32 | **** | ** | ** | 8 |
| 33 | ** | ** | ** | 6 |
| 34 | **** | ** | *** | 9 |
| 35 | *** | * | * | 5 |
| 36 | **** | ** | ** | 8 |
| 37 | ** | ** | *** | 7 |
| 38 | **** | ** | *** | 9 |
| 39 | **** | ** | *** | 9 |
| 40 | ** | ** | ** | 6 |
| 41 | *** | ** | *** | 8 |
| 42 | ** | ** | *** | 7 |
| 43 | **** | ** | *** | 9 |
| 44 | **** | * | ** | 7 |
| 45 | *** | ** | *** | 8 |
| 46 | *** | * | * | 5 |
| 47 | ** | ** | *** | 7 |
| 48 | *** | ** | *** | 8 |
| 49 | * | ** | *** | 6 |
| 50 | **** | ** | *** | 9 |
| 51 | *** | * | * | 5 |
| 52 | *** | ** | *** | 8 |
| 53 | ** | ** | *** | 7 |
| 54 | **** | ** | *** | 9 |
| 55 | *** | ** | *** | 8 |
| 56 | **** | * | ** | 7 |
| 57 | *** | ** | *** | 8 |
| 58 | ** | ** | *** | 7 |
| 59 | **** | ** | *** | 9 |
| 60 | *** | * | * | 5 |
| 61 | *** | ** | *** | 8 |
| 62 | **** | * | ** | 7 |
| 63 | **** | ** | *** | 9 |
| 64 | * | ** | *** | 6 |
| 65 | ** | ** | *** | 7 |
| 66 | *** | * | ** | 6 |
| 67 | **** | ** | *** | 9 |
| 68 | *** | ** | *** | 8 |
| 69 | * | ** | *** | 6 |
| 70 | **** | ** | ** | 8 |
| 71 | *** | * | * | 5 |
| 72 | **** | ** | *** | 9 |
| 73 | *** | ** | *** | 8 |
| 74 | ** | ** | ** | 6 |
| 75 | **** | ** | ** | 8 |
| 76 | **** | ** | *** | 9 |
| 77 | **** | ** | *** | 9 |
| 78 | *** | ** | *** | 8 |
| 79 | ** | ** | *** | 7 |
| 80 | **** | ** | *** | 9 |
| 81 | **** | ** | ** | 8 |
| 82 | ** | ** | *** | 7 |
| 83 | **** | ** | ** | 8 |
| 84 | ** | ** | *** | 7 |
| 85 | ** | ** | ** | 6 |
| 86 | **** | ** | ** | 8 |
| 87 | ** | ** | *** | 7 |
| 88 | ** | ** | ** | 6 |
| 89 | ** | ** | ** | 6 |
| 90 | **** | ** | *** | 9 |
| 91 | ** | ** | ** | 6 |
Note. Good quality: 3 or 4 stars in selection domain AND 1 or 2 stars in comparability domain AND 2 or 3 stars in exposure/outcome domain; Fair quality: 2 stars in selection domain AND 1 or 2 stars in comparability domain AND 2 or 3 stars in exposure/outcome domain; Poor quality: 0 or 1 star in selection domain OR 0 stars in comparability domain OR 0 or 1 stars in exposure/outcome domain.
Results
Description of reviewed studies
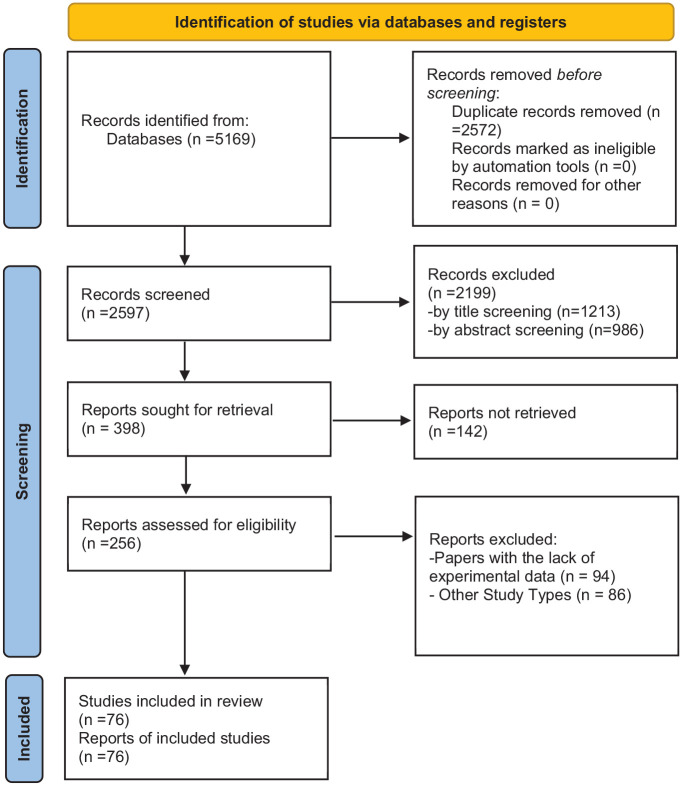
The reviewed studies were published between 2020 and June 2023, and included a total of 76 studies (Figure 1). Of these studies, 73 included both male and female subjects, while two studies exclusively included male subjects, and one study did not report. The sample size for all studies combined was 1,988,008 individuals, with data collected from both male and female participants. The findings of the studies are presented in Table 2.
Figure 1.
PRISMA flow diagram of study retrieval process.
Table 2.
Description of the findings reported in eligible studies.
| Reference | Country | Population (n=)Female (%)Male (%) | Mean age ± SD | Social stigma assessment methods | Time of the COVID-19 pandemic | Prevalence of social stigma | Type of social stigma | The outcome of social stigma associated with COVID-19 | Other findings |
|---|---|---|---|---|---|---|---|---|---|
| 16 | Jordan | 777 Female (58.5) Male (41.5) |
34.5 ± 8.8 | Self-administered questionnaire | May to July, 2021 | 50% | Social isolation | NA | Hearing news all time, smoking, and having children served as predictors of stigma toward healthcare providers (HCPs). |
| 17 | Jordan | 1655 Female (63.8) Male (33.2) |
29.5 ± 7.7 | Self-administered questionnaire | June to August, 2020 | 64% | Labeling, social isolation | NA | Income, living area, and downloaded applications to trace COVID-19 cases acted as potential predictors of stigma. |
| 18 | Nepal | 213 Female (50.2) Male (49.8) |
29.90 ± 6.43 | Structured Google form | January 10 to February 6, 2021 | 57% | Disgrace | Anxiety and depression | healthcare workers (HCWs) working as frontline workers had significant odds of stigma compared to those not working in frontline |
| 19 | Ghana | 28 Female (25) Male (75) |
20–59 | Personal interviews and focus group | March 30 to April 30, 2020 | 100% | Social isolation, labeling | Psychological distress and mental health disorders (anxious, confusion, restless, anger, apathy) | The infection can contribute to mild to severe mental health |
| 20 | Jordan | 397 Female (70) Male (30) |
30.1 ± 9.82 | Questionnaire | May to June, 2020 | 64.3% | Bullying, verbal violence | NA | Most people assumed that patients with COVID-19 are getting bullied. |
| 21 | Saudi Arabia | 15 Female (47) Male (53) |
Aged between 25–55 | Interview | 2020 | NA | Social isolation, labeling | NA | A positive association between social stigma and COVID-19. No significant difference between male and female in terms of stigma incident |
| 22 | Saudi Arabia | 226 Female (62.6) Male (37.4) |
NA | Questionnaire | N/A | NA | Blaming, avoidance | Social avoidance | Discontinued workgroups are more affected by communication impairments, social avoidance, and stigma, less emotional and personal deprivation |
| 23 | Saudi Arabia | 174 Male (35.4) Male (35.4) |
31.58 ± 10.2 | Interview | July to December, 2020 | NA | Blaming, avoidance | Depression, anxiety | Participants’ stigma scores were significantly associated with higher scores on depression and anxiety |
| 24 | Saudi Arabia | 847 Female (79) Male (21) |
Over 18 years | Questionnaire | May 2020 | 100% | Social isolation, labeling, avoidance | NA | Significant association existed between stigma, and older age groups, being married and lower levels of education. |
| 25 | Indonesia | 322 Female (69.9) Male (30.4) |
27.2 ± 8.9 | NA | NA | NA | NA | NA | Stigma since the COVID- 19 pandemic outbreak was influenced by demographic, knowledge and behavior factors, while the attitude variable in this study did not affect the occurrence of stigma, knowledge aspect had a positive relationship with stigma, behavior aspect indicated a negative relationship. |
| 26 | Burkina Faso, Ethiopia, and Nigeria | 900 Female (58.67) Male (41.33) |
39.77 ± 10.79 | Questionnaire | — | 73.7% | Social avoidance or rejection: 46%, denial of services:7.22%, physical violence: 4.78, no acknowledgment: 43.33% | NA | Perceived stigma had not significant association with correct perceptions toward COVID-19 among healthcare providers |
| 27 | Ghana | 45 Female (35.6) Male (64.4) |
37.7 ± 16.9 | Interview | March 2020 to Feb 2021 | NA | Labeling | Weakened individuals’ health, happiness, morale self-confidence, frustration, anxiety disorders and insomnia | — |
| 28 | Iran | 312 Female (74) Male (26) |
23.53 ± 6.46 | Questionnaire | April to June, 2020 | NA | NA | NA | Positive association was detected between stress and stigma. Mental health can act as a predictor of stigma |
| 29 | India | 311 Female (20) Male (80) |
NA | Questionnaire | May 15 to June 30, year | 84.5% | Self-stigma, labeling, rejection, discrimination | Changed interpersonal relations, losing business | Significant association between stigma and age. Those aged 46–60 years, self-employed individuals, those with income of 10–20 thousand per month, those living in slums had the highest incidence of stigma |
| 30 | Italy | 174 Female (84.5) Male (15.5) |
NA | Questionnaire | NA | NA | NA | Burnout, secondary traumatic stress | Perceived stigma had negative association with compassion satisfaction and positive association with burnout and secondary traumatic stress. Stigma and identification interact with each other |
| 31 | Colombia | 1687 Female (59) Male (41) |
36.3 ± 12.5 | Questionnaire | NA | NA | NA | Fear | Stigmatization was significantly higher in the general population relative to health workers. Significant associations were found between most of questions from the stigma questionnaire and high fear of the virus |
| 32 | Congo | 1267 Female (40.9) Male (59.1) |
32 ± 10.1 | Questionnaire | March to May, 2020 | N/A | N/A | Depression | Stigmatization related to COVID-19 served as a strong predictor of depression |
| 33 | India | 303 Female (42.2) Male (57.8) |
36.5 ± 14 | Questionnaire | December 1, 2020 to June 21, 2021 | 34% | Rejection, social isolation | NA | Individuals with low economy and education level were more worried regarding rejoining the society after the isolation. Individuals with low economy level and lower education level were more worried about discrimination toward their family |
| 34 | China | 186 Female (64) Male (36) |
36 (26–47) | questionnaire | August 2021 | NA | Attitudinal | NA | Patients, their family, and healthy individuals viewed COVID-19 patients with stigma |
| 35 | Malaysia | 12 Female (50) Male (50) |
36·5 ± 29 | telephone interview | April and June 2020 | NA | Social isolation, labeling | Non-disclosure of medical history | Public misconception and fear hindered disclosure |
| 36 | Kenya | 311 teachers Female (56) Male (44) |
15 | telephone survey | June and November 2020 | 18% (teachers) | Labeling, social isolation | Loss of social or financial support | No HIV-positive adolescents reported losing social or financial support owing to COVID-19 |
| 19 ALWH Female (57.89) Male (42.11) | |||||||||
| 37 | India | 91 Female (31.9) Male (68.1) |
30–49 | Questionnaire | April 15 to June 1, 2020 | 98% | Self-stigma, rejection, social isolation | Reduction of socialization | Enacted stigma was more prevalent among men and individuals with advanced education |
| 38 | USA | 845 Female (41.4) Male (58.6) |
40.15 ± 11.67 | Online survey | April2020 | NA | NA | Reluctance to seek testing for COVID-19 | Resistance to COVID testing among individuals with COVID-19 stigma and stereotypes anticipation |
| 39 | USA | 30 Female (70) Male (30) |
21–29 | Online video interview | June to August, 2020 | 26.7% | Social isolation, blaming | Limited access to services and social isolation | Older people were more stigmatized |
| 40 | India | 12 Female (50) Male (50) |
NA | Telephone interviews | May and July 2020 | NA | Blaming, avoidance | Anger, anxiety, humiliation, helplessness, loneliness | Other stigma manifestations were physical violence, unemployment, and social exclusion |
| 41 | USA | 498 Female (35.94) Male (63.65) |
25–34 | Online survey | August 2020 | 65.46% | Social isolation, avoidance | NA | Men, social media users, Hispanics, Blacks, college or higher-degree holders endorsed stigma more |
| 42 | India | 206 Female (46.1) Male (53.9) |
36.08 ± 13.12 | Online survey | May to June, 2021 | 20 % from family, 31.1% self-stigma, 50 % from societ | Self-stigma, avoidance, social isolation | NA | PTSD sufferers reported greater anxiety, depression, stigma, fatigue, and cognitive difficulties |
| 43 | USA | 1366 Female (41.2) Male (58.7) |
N/A | Online survey | April 2020 | 3.1% | Social isolation, structural | Anxiety, depression | Most individuals linked COVID-19 stigma with Asian race and ethnicity |
| 44 | Lebanon | 405 Female (79.8) Male (20.2) |
28.38 ± 12.02 | Online survey | December 2020 to January, 2021 | 65.9% | Self-stigma, Social isolation, rejection | NA | Anxiety, fear, having COVID-19 or a family member with the condition mediated the knowledge-disease association |
| 45 | Bangladesh | 1056 Female (49.9) Male (50.1) |
35.75 ± 12.18 | Online survey | May 2020 | 90.8% | Attitudinal | Fear and denial of interaction with patients | Education, marital status, risk perception, location of living, and views on COVID-19 influenced stigmatized attitudes |
| 46 | India | 120 Female (47.5) Male (52.5) |
29.2 ± 6.65 | Questionnaires | October 2020 | 56.6% | Self-stigma, rejection, blaming | Loss of accommodation, social harassment and isolation | Male gender, age, marital status, education, and occupation increased stigmatization |
| 47 | Sri Lanka | 80 Female (42.4) Male (57.6) |
43 ± 11.2 | Telephone interviews | March to June, 2020 | 38.8% | Social isolation, rejection, avoidance | Reluctance to seek care, social isolation, severe mental issues | Media was a key driver of stigma. |
| 48 | China | 5039 Female (58.5) Male (41.5) |
33.0 ± 12.5 | Questionnaires | March 2020 | 5.1% in patients over 50, 1.2% in patients under 20 | Social isolation, blaming | NA | Stigmatized behaviors were associated with living in high case areas, health illiteracy, and ethnic minority status |
| 49 | Korea | 107 Female (47.7) Male (52.3) |
NA | Retrospective observational study | 5 March to 8 April, 2020 | NA | Social isolation, avoidance, rejection | Depression, anxiety, somatic symptoms and possible PTSD | The prevalence of more-than-moderate depression was 24.3%, more-than-moderate anxiety was 14.9%, more-than-moderate somatic symptoms was 36.5% and possible PTSD was 5.6% of total population |
| 50 | Korea | 600 Female (50) Male (50) |
NA | Online survey w | 19 February to 29 February 2021 | N/A | Verbal violence, rejection | Anger | In 20–29 years old participants anticipated stigma increased their compliance with COVID-19 prevention guidelines |
| 51 | Pakistan | 134 Male (40.3) Female (59.7) |
18–60 | An interview based, pre-tested, semi-constructed questionnaire | November 2020 to January 2021 | 51.5% | Verbal violence, blaming | NA | 69.4% of healthcare workers knew of other people who faced similar stigmatization due to their exposure to COVID-19 |
| 52 | Japan | 429 Female (53.2) Male (46.8) |
mean age 55, 40–67 | Questionnaire | 14 June 2020 to 5 July 2020. 15 October 2020 and 25 October 2020 | NA | Verbal violence, blame | NA | People with higher community social capital reported lower stigmatization |
| 53 | Indonesia | 1385 Male (25.5) Female (74.5) |
NA | Online survey questionnaire | NA | NA | Self-stigma, social isolation, blame | depressive, anxiety, and stress symptoms | Controlling demographics factors, clear self-stigma increased the risk for depression |
| 54 | China | 13,994 Male (55.4) Female (44.6) |
Age 30.4 ± 9.6 | Questionnaires | NA | NA | Self-stigma, avoidance, blame, and secondary discrimination | NA | Obtaining COVID-19-related information from social media (91.3%) and newspaper or television (77.1%). 61.0% of them found information from newspapers or television most reliable |
| 55 | China | 122 Male (59.8) Female (40.2) |
⩽ 50 years old or > 50 years old | Wilcoxon signed-ranks test (nonparametric test) | From February 27th to March 12th, 2020 | NA | Verbal violation, blame | NA | Age is an independent factor that affects the perceived stigma level of COVID-19 patients. Patients who were unmarried and severely ill have a higher level of perceived stigma |
| 56 | Finland | 64 Male (50) Female (50) |
Over the age of 12, youth ages 13 to 17 and adults over the age of 18. | Interviews | between April and May 2020 | NA | Verbal violation, rejection, social isolation, self-stigma | Reluctant to disclose COVID-19 | NA |
| 57 | Egyptian | 509 Females (69.4) Male (30.6) |
mean age: 41.5 ± 10.2 | Anonymous online questionnaire | 7 to 21 June 2020 | 40.6% | Self-stigma, social isolation | Negative self-image | Overall COVID-19-related stigma score was higher in participants with lower qualifications, and in those working in a quarantine hospital |
| 58 | Indonesian | 2,156 Male 700(32.5) Female 1456 (67.5) |
age 20–54 years | Questionnaire electronic form | December 2020 –August 2021 | NA | Social isolation | Anxiety, fear, depression, mental health crisis | Results of the inferential analysis showed that all P < 0.05 which indicated that psychological status and social stigma had a significant relationship with anxiety, fear, depression, and mental health crisis in nurses |
| 59 | Iraq, Jordan, Egypt, Saudi Arabia, Indonesia, Philippines, and Kuwait | 1726 Male (44.3) Female (55.2) |
20 and above | Self-administered online survey | from June–July 2020 | NA | Verbal violation | NA | Statistical significance between COVID-19 stigma and demographic variables were found in all aspect of the S19-HCPs |
| 60 | Netherlands | 908 Male (39) Female (61) |
13.2 ± 1.27 | Questionnaire | March 17 to April 20, 2020 | NA | Social isolation, blame, rejection | Anger | Sympathy and helping determinants were rated significantly higher than the anger and cognitive attributions determinants. |
| 61 | Italy | 260 Female (52.7) Male (47.3) |
46.67 | Questionnaire | 17 March to 2 April, year | NA | Verbal violence | NA | Stigma may influence worker compliance and can guide management communication strategies relating to pandemic risk for HCWs |
| 62 | India | 150 Male (64) Female (36) |
NA | Questionnaire | N/A | NA | Psychological pressure, blaming | stress, anxiety, depression | N/A |
| 63 | UK | 2006 Female (73.4) Male (68.6) |
16 and above | Questionnaire | 10–13 February, 2020 | 26.1% | Attitudinal | stress | Relationship between stigmatizing attitude, having a dependent child, lower education, chronic illness and younger age |
| 64 | Iran | 176 Female (50), Male (50) |
Majority were above 60 years of age (62.5%) | Questionnaire | March and April 2020 | NA | Discrimination from medical settings | NA | NA |
| 65 | Russia | 1800 Female (81.05) Male (18.95) |
42 ± 12 years | Questionnaire | March 30 to April 5 and May 4 to May 10, 2020 | NA | Attitudinal | NA | The increase in stigmatizing attitudes of medical staff was mostly related to their fear of their own lives |
| 66 | Brazil | 92 Male (100) |
between 29 and 39 years old | Interview | May to August 2020 | NA | Psycho-emotional, social interactions, labeling | Fear, isolation | NA |
| 67 | Turkey | 634 Female (68) Male (32) |
35.89 ± 8.63 years | Questionnaire | April 16 to May 16, 2020 | 28% | Psychological | NA | Prevalence of moderate and severe depression in health care workers: 36%, prevalence of anxiety: 35%, prevalence of stress: 22% |
| 68 | USA and Canada | 3551 Female (42) Male (58) |
54 ± 15 years | Questionnaire | May 6–19, 2020 | 33% | Psychological | NA | NA |
| 69 | Turkey | 452 Female (66.2) Male (33.8) |
35.8 ± 8.9 | Questionnaire | 20 May 2020 and 10 June 2020 | NA | Psychological | Depression, anxiety | Positive and significant correlation between stigma score, hospital depression and anxiety scale. Negative correlation between perceived stigma score and psychological well-being score, problem-oriented coping, emotion-focused coping and quality of life |
| 70 | Indonesia | 547 Female (49.73) Male (50.27) |
20 years or older | Questionnaire | October to December 2020 | 70.2% | Psychological | NA | Moderate stigma is more related to quality of life and mental health than low stigma. Women experience less stigma associated with mental health than men. Quality of life and mental health are affected by stigma, gender and occupation. |
| 71 | USA | 632 Female (71) Male (29) |
51 | Questionnaire | April 17, 2020, and April 18, 2021 | NA | Psychological | NA | Being female, working at home or not working due to covid-19, previous mental health diagnosis, history of chronic illness, current or former smoking were associated with higher stigma scores. Older age was associated with lower stigma scores. |
| 72 | India | 122 Male (100) |
33.5 ± 8.9 years | Questionnaire | 22 October 20 to 21 November 20 | 19% | Psychological | NA | NA |
| 73 | China | 154 COVID-19 survivors Male (43.5) Female (56.5) |
COVID-19 survivors: 42.2 ± 13.7 | Questionnaire | May 27 and September 4, 2020 | NA | Social rejection, internalized shame, lack of financial security, social isolation | Shame | Having infected family members, being married, economic loss during the epidemic, depressive symptoms were positively related to higher stigma |
| 194 healthy Male (20.6) Female (79.4) |
Healthy: 35.7 ± 9 | ||||||||
| 74 | Indonesia | 288 Female (65.3) Male (34.7) |
⩽ 30 years old or > 30 yearsold | Questionnaire | March 6 to March 25, 2020 | 21.9% | Attitudinal | NA | Physicians perceived less stigma associated with COVID-19 compared to other healthcare workers |
| 75 | Iran | 894 Female (71.4) Male (28.6) |
30 years and older | Questionnaire | March 20 to April 3, 2020 | NA | Psychological | stress | Prevalence of post-traumatic stress was higher in women than in men. |
| 76 | China | 1212 Female (73.27) Male (26.73) |
18 years or older | Questionnaire | 7 May to 25 May in 2020 | 31.8% | Social isolation, blaming, rejection | Fear, anger | Older age, married, lower education, having mental problems are associated with higher general stigma scores. |
| 77 | China | 1920 Female (56.93) Male (43.07) |
20.51 ± 4.51 | Questionnaire | October to December, 2020 | 44.58% | Shame, verbal violence | NA | Knowledge about COVID-19 was associated with COVID-19-related stigma |
| 78 | Japanese | N/A | NA | Data from the Google COVID-19 Community Mobility Reports | January 3rd to February 6th, 2020. | NA | Fear | Affects mobility behavior | The study modifies the stigma model for mobility behavior during COVID-19 by incorporating the impact of the Go to travel campaign |
| 79 | India | 376 Female 163 (43) Male 213 (57) |
20–60 years | Questionnaire-based survey, semi-structured interviews | April and November 2020 | 34 % | Psychological | NA | Three distinct forms of negative social experiences during the pandemic: 3.1. Neighborhood tensions around restrictions of mobility, experiences of social distancing, harassment |
| 80 | Germany | 61 Male (58) Female (42) |
51 ± 14.6 | Questionnaires | NA | NA | Shame and rejection | Social rejection, internalized shame, social isolation, financial insecurity | There was no significant difference in experienced stigma regarding gender, education, occupational status or residual symptoms |
| 81 | UK | 966 Female (84·6) Male (15) |
48·3 ± 10·7 | Questionnaire | NA | 95·4% (n = 847), enacted stigma was 62·7% (n = 557), internalized stigma was 86·4% (n = 767), and anticipated stigma 90·8% (n = 806) | Psychological | NA | Prevalence of stigma was higher in respondents with a formal diagnosis of long COVID (97·5%; n=429) than in those without (93·2%; n = 413). |
| 82 | Egyptian | 565 Male 166 (29.4 %) Female 399(70.6%) |
30-40> | Questionnaire | NA | 94.7% | Shame | NA | Significantly high impact stigma scores were detected among those aged < 30 years, females, workers primarily in sites susceptible for contracting COVID-19 infection, those had severe worry from contracting infection at work, and high internalized shame scale. |
| 83 | India | COVID-19 stigma:303, Community COVID-19 stigma: 1976 | 18–60> | Questionnaire | September 2020 to January 2021 | 51.3% | social exclusion, stereotyping, insults, blame or threat, verbal abuse or gossip, physical abuse, denial of housing, medicine, dismissal from (job, and refusal from stores and restaurants) | N/A | Risk factors of stigmatizing attitude toward COVID-19 among individuals from the community: residents of high prevalent COVID-19 zone, staying in rural areas, age: 18–30 years, male, illiterate, living in Maharashtra risk factors of stigmatizing attitude toward COVID-19 among individuals recovered from the infection: age: 6–15 years, those who had poor knowledge about the infection transmission, and belonged to Delhi |
| 84 | Qatar | 576 Female (29.5) Male (70.5) |
median age 38 ± 31–46 | Questionnaire | June to August 2021 | 26% | Shame, disapproval, or disgrace that results in the rejection of an individual, discrimination against them, and the exclusion from participating in the different areas | N/A | Occupation, ethnicity, and low educational level predicted COVID-19 perceived stigma. The CPSS-22 showed excellent reliability |
| 85 | Nigeria | 332 Female (38.9) Male (61.1) |
33.35 ± 7.10 | Questionnaire | — | N/A | N/A | N/A | Respondents with a higher perception of vulnerability to diseases reported higher COVID-19 risk and perception of COVID-19-related stigma. Gender, age, and education impacted COVID-19 risk and perception of COVID-19-related stigma |
| 86 | Iran | 1064 Female (49.9) Male (51.1) |
38 [30.75, 52] | questionnaire | 27 to 30 September 2020 | 86.8% | embarrassment and shame to the patient and his/her family, fear of being fired, identification and penalized | N/A | None of patients showed higher level of stigma. Stigma was found less among those with high education level. |
| 87 | Egypt | 150 Female (54) Male (46) |
36.9 ± 10.6 | questionnaire | February 2021 to April 2021 | 70% | Depression, anxiety, and symptoms of post-traumatic stress disorder | N/A | Being a woman and nurse were significantly associated with the total perceived COVID-19-related stigma score. COVID-19-related stigma perception had significant association with depression, anxiety, and post-traumatic stress |
| 88 | India | 420 Female (29.2) Male (70.7) |
38.77 ± 11.85 | Questionnaire | June 2020 to February 2021 | NA | Personalized stigma, social isolation | Fear, anger, anxiety, shame | Urban populations and males faced more stigma and discrimination |
| 89 | Germany | 4,059 Female (49.5) Male (50.5%) |
45.68 | Questionnaire | December 16–29, 2020 | NA | blame, negative affect, discriminatory inclinations | Blame, deservingness, lack of sympathy, anger, avoidance, insult, healthcare access restriction | Higher COVID-19 stigma than flu, lower stigma for females, more discrimination and negative emotions among affected respondents |
| 90 | Japan | 1573 Female (49.8) Male (50.2) |
54.5 ± 14.4 | Questionnaire | December 2020 to March 2021 | 16.3% | COVID-19 stigma | negative effect on quality of life, psychological distress | Older age, severity, anxiety, funding hesitancy, and lack of knowledge contributed to COVID-19 stigma |
| 91 | Germany, Austria, Switzerland | 253 Female (88.5) Male (11.5) |
45.49 ± 12.03 | Questionnaire | June 2021 and October 2021 | NA | enacted stigma, perceived external stigma, disclosure concerns, internalized stigma | stress, depression, anxiety, lower mental health-related quality of life | Social stigma had a stronger impact on mental health than physical health in long COVID |
Prevalence
Out of the 37 studies that reported on the prevalence of social stigma related to COVID-19 infection, 20 studies found that the majority of participants experienced stigmatization16–20,24,26,27,29,37,41,42,44–46,51,70,83,84,86–88,91; In two studies conducted in China (28 participants) and Saudi Arabia (847 participants), the prevalence of social isolation and labeling reached 100%.19,24 In another study conducted in India with 91 participants, 98% of participants reported experiencing self-stigma, rejection, and social isolation. 37 The remaining 17 studies reported a prevalence ranging from 3.1% to 44.56%,33,36,39,43,47,48,57,63,67,68,72,74,76,77,79,84,89 the lowest prevalence of 3.1% was associated with social isolation and structural stigma and was found in a study conducted in the USA with 1366 participants.
The stigmas experienced by patients of COVID-19 in the present study were classified into three categories: personal, interpersonal, and organizational stigmas.
Personal stigmas
The personal stigmas identified through the literature review included attitudinal stigma, self-stigma, psychological pressure (Depression, anxiety, and symptoms of post-traumatic stress disorder), psycho-emotional stigma, internalized shame, lack of financial security, and shame.
Interpersonal or social stigmas
In the interpersonal domain, the following stigmas were identified: labeling, social isolation, disgrace, bullying, verbal violence, blaming, avoidance, physical violence, social rejection or avoidance, discrimination, and secondary discrimination (as presented in Table 2).
Organizational stigmas
Finally, at the organizational level, the study identified denial of services and discrimination in medical settings as forms of stigma.
The most important stigmas were the interpersonal or social stigmas. The most common was social isolation.16,17,19–21,33–35,37,39,41,42,44,47,48,53,56,57,60,73,76,88 In 16 studies blaming from others was the second most common social stigma reported due to being infected with COVID-19.22,23,39,40,46,48,51–55,60,62,72,83,89 In 13 studies, participants experienced rejection from the social environment.29,33,37,44,46,47,50,56,60,73,76,80,83 Other stigmas experienced by COVID-19 patients included psychological pressure,62,66–72,75,79,81 verbal violence,20,50–52,55,56,59,61,77,83 avoidance,22–24,26,40–42,47,54 labeling,17,19,21,23,27,29,34,35 attitudinal stigma,34,45,63,64,74 disgrace,18,26 discrimination,54,64 shame,73,77,80,82–84,86 structural stigma, 43 bullying, 20 denial of service and physical violence.26,83,84 In eight studies self-stigma due to being infected by SARS-CoV-2 was reportedly experienced by participants.29,37,42,44,46,53,54,57
Negative consequences were reportedly experienced by COVID-19 patients with anxiety being the most common,18,19,23,27,40,43,49,53,58,62,69,86,91 followed by depression,18,23,32,43,49,53,58,62,69,91 reduction of socialization,22,37,39,45–47,66,80 fear,31,45,58,66,76,87,89 distress,19,52,63,75 anger,40,50,58,76 mental health disorders,19,47,58,90 secondary traumatic stress,30,49 non-disclosure of COVID-19,35,56 reluctance to test/seek care,38,47 loss of financial support, 36 loss of accommodation, 46 helplessness, 40 loneliness, 40 burnout, 30 less happiness, 27 insomnia, 27 losing business, 29 changed interpersonal relation, 29 shame, 73 negative self-image, 57 somatic symptoms, 49 and affects mobility behavior. 78
In the present study, the majority of information was obtained through questionnaires, and studies reporting a prevalence of social stigma higher than 50% were mostly collected through questionnaires. This suggests that self-report questionnaires may have advantages over interviews and focus groups, as participants are more likely to report their experiences truthfully. Self-report questionnaires allow participants to answer anonymously, which may help reduce social desirability bias and encourage more honest responses.
Discussion
The purpose of this systematic review was to explore the social stigma surrounding the COVID-19 infection. There were 76 studies included which represented 37 countries worldwide. Most of the studies were conducted in eastern countries (Middle East and East Asia). The most common method used to collect data was via questionnaires. A relatively even split of sexes was represented (52.16% females and 47.84% males) with a mean age of 36.74 years. Prevalence of social stigma, the types of social stigma, the outcomes of social stigma, and other important findings were examined.
Prevalence
Among the top 10 countries with the highest prevalence of stigma, the majority were underdeveloped, with over 50% of the population experiencing stigma. However, the reported prevalence of stigma varied significantly between studies, even within the same country or among different nations. Possible reasons for this variability include a lack of standardized COVID-19 stigma questionnaires, limited access to medical services, and a shortage of accurate information about the disease in underdeveloped countries.
The degree to which disease-related stigma is prevalent varies among communities, and socioeconomic factors at both the individual and community levels impact different types of stigmas in distinct ways. 92 For example, communities with a better understanding of the disease and higher levels of mobilization efforts are less likely to exhibit stigma, while communities with concerns regarding providing aid and care during epidemics are more likely to endorse stigma.93,94 Additionally, individuals with higher socioeconomic status or education levels experience less stigma, likely due to their greater access to accurate information about the disease. These results are consistent with earlier research demonstrating that individuals from lower social classes experience more stigma compared to those from higher social classes.
For the studies included in the present review there was a higher prevalence of stigma in Asian countries,16,18,21,29,44,45,51,70,82,83,86 which could be attributed to the Asian origin of the virus, for example, Asians being accused of spreading the disease. The prevalence of stigma is exacerbated by an excess of news and conflicting messages, particularly during large-scale disasters such as COVID-19.95–97 In similar studies, the prevalence of infectious diseases such as H1N1, bubonic plague, Asian flu, cholera, Ebola, Zika virus, tuberculosis, SARS, and middle east respiratory syndrom (MERS) has been associated with stigma and discrimination against patients. 98 A recent comparative study reported a higher prevalence of stigma for COVID-19 infection than AIDS/HIV, which has been one of the most stigmatized health conditions worldwide for decades. 54 COVID-19 infected patients and their family members were stigmatized and isolated as being infectious or dangerous to the health of those coming into contact with them. The widespread concern and media coverage of COVID-19 contributed to its high prevalence of stigma, which was fueled by individuals perceiving the disease as a mortal infection, and the lack of treatments for the virus. Misleading news likely caused people to be frightened, but accurate knowledge about the disease may have reduced the stigma. Education and good communication have the potential to significantly improve the knowledge, attitudes, and behaviors related to infectious diseases, such as Ebola and COVID-19, and reduce infectious disease-related stigma.99,100
Types of stigma
In previous studies, various types of stigma have been defined for AIDS/HIV disease. For instance, a study that investigated a conceptual model of HIV/AIDS stigma from five African countries identified three types of stigma: received, internal, and associated. 101 Received stigma is a type of stigma directed toward a person living with HIV/AIDS by others. It includes various stigmatizing behaviors such as neglecting, fearing contagion, avoiding, rejecting, labeling, pestering, negating, abusing, and gossiping. Internal stigma is the negative thoughts and behaviors that a person living with HIV has about themselves based on their HIV status. This type of stigma is based on the person’s own perceived view of stigma, and can include self-perception, social withdrawal, self-exclusion, and fear of disclosure. 102
Associated stigma refers to the stigma that arises from a person’s association with individuals who have HIV/AIDS, such as having an HIV-positive family member or working with HIV-positive individuals. In the present review, the most reported stigma was social isolation.16,17,19,21,24,33,35–37,39,41–44,47–49,53,56–58,60,73,76,80,88 Furthermore, in 16 studies22,23,39,40,46,48,51–55,60,62,76,83,89 participants experienced blaming from others. Additionally, participants in 14 studies reported rejection from social environment.26,33,37,44,46,47,49,50,56,60,73,76,80,84 Labeling was reported in nine studies,17,19,21,24,27,29,35,36,66 and avoidance was also reported in 10 studies.22–24,26,40–42,47,49,54 Denial of service, and violence were reported in two studies,26,83 disgrace was also claimed in only two studies.18,84 In another study, discrimination and self-stigma were reported,29,84,89,91 and verbal violence and bullying in 10 studies.20,50–52,55,56,59,61,77,83 Attitudinal stigma was reported in eight studies.34,45,63,65,74,83,84,91 Other related studies also reported psychological distress and decreased resilience during the outbreak of viruses H1N1, H7N9, MERS, and Ebola. 103
The stigmatization of various diseases has both similarities and differences. While isolation is a common stigma in infectious diseases, different diseases have varying prevalence and types of stigma. For example, tropical infectious diseases with visible symptoms such as scars and deformities have the highest rates of stigmatization and social isolation, while HIV is stigmatized due to its origin and being a sexually transmitted disease. COVID-19 patients also face stigma due to a perceived lack of precautionary measures or social distancing, making them a potential threat to others’ health.
The COVID-19 pandemic has resulted in a variety of isolation and social avoidance behaviors toward patients infected with the virus. These behaviors are possibly due to community fears of getting infected since the disease is highly contagious. Social isolation and other forms of rejection from others were frequently reported and are consistent with previous studies on attitudes toward patients during epidemics and pandemics. 104
Outcomes of stigma
The review findings indicated there were various outcomes experienced by participants, such as anxiety which was the most experienced one,18,23,27,40,43,49,53,58,62,69,88,91 followed by depression,18,23,32,43,49,53,58,62,69,91 fear,31,45,58,66,76,88 anger,19,40,50,60,76,87,89 mental health disorders,19,47,49,58,90,91 secondary traumatic stress,30,53,62,63,76 non-disclosure of COVID-19,25,35,47,56,80,89 loss of financial support,36,73,80 burnout, 30 less happiness, 27 insomnia, 27 losing business, 29 changed interpersonal relation,29,66 psychological pressure,62,67,68,70–72,75,90 discrimination from medical settings,54,64,89 psycho-emotional, 66 internalized shame.73,77,80
Stigma can cause unpleasant feelings such as anxiety and depression, which can threaten mental health. In turn, mental health can also act as a predictor of stigma. The consequences of stigma can be serious, as evidenced by patients who were reluctant to disclose their symptoms and seek medical attention during the early stages of COVID-19 due to social stigma. This non-disclosure can lead to a more rapid spread of the disease. 105 Evidence in other studies suggests that stigma has caused psychological distress and post-traumatic stress disorder (PTSD) in infected patients and healthcare workers during outbreaks of SARS, H1N1, MERS, Ebola, and COVID-19.106–109 Similar findings have been reported in studies on other diseases, such as AIDS and previous SARS epidemics.
In various infectious diseases, including human immunodeficiency virus (HIV), hepatitis C virus (HCV), tuberculosis, and Zika, stigma persists at all levels and impedes effective treatment. This stigma may lead to reduced treatment uptake and under- or non-participation in available treatments. 110 HIV/AIDS has always been stigmatized with negative connotations such as drug abuse, sex work, poverty, or incarceration associated with deviant behavior disapproved by society. 111 In contrast, epidemic-related diseases like SARS and COVID-19 are caused mainly by external factors, which are not considered morally reprehensible. Hence, stigmatization of these infectious diseases is primarily driven by fear of the disease itself, and the perceived threat level will decrease as public awareness of the disease increases.112,113 It is crucial to improve public awareness of the nature of the disease to reduce fear and anxiety and, subsequently, reduce stigma. 114 Furthermore, people with higher education levels and socioeconomic status may be less likely to stigmatize others, especially in high-income countries. 115
Strengths and limitations
This review provided a broad and representative overview of the COVID-19-related stigma issue. The methods used to find, screen, and select the included studies were rigorous. Additionally, data was extracted via three researchers and the discrepancies were addressed by a third researcher to ensure the quality of included studies and reduce the risk of bias. However, the results of this review may be subject to limitations related to the selection process of eligible studies. Specifically, studies published in outlets other than the first-tier journals were included in the review. Due to the heterogeneity of the included studies, performing a meta-analysis was not suitable; therefore, we only performed a qualitative synthesis of selected literature.
Conclusion
This systematic review identified the three most researched targets of COVID-19-related stigma. First, prevalence of social stigma: limited access to medical services, shortage of accurate information about the disease in underdeveloped countries, socioeconomic, and geographical location. Second, types of stigma: social isolation, labeling, rejection from the social environment, blaming from others, denial of service, violence, discrimination, self-stigma, verbal violence, and attitudinal stigma. Third, the outcome of the stigma: anxiety, depression, fear, anger, mental health disorders, secondary traumatic stress, non-disclosure of COVID-19, loss of financial support, burnout, less happiness, insomnia, losing business, changed interpersonal relations, psychological pressure, discrimination from medical settings, psycho-emotional, internalized shame. The stigma associated with COVID-19 is closely related to the quality of life and mental health of individuals, and our findings can inform policymakers to ensure the availability of a safe environment with respectful care and urgent action is needed to tackle COVID-19 at every level, from the personal to the political. It seems that according to the issues raised in this review, it is necessary to deal with the psychosocial discomforts that society is facing during the outbreak of COVID-19. To deal with these feelings, psychological evaluations, and support, including ensuring a cultural approach, and taking into account different needs in society, are necessary. In addition, social support is necessary to reduce the adverse effects of stigma that may lead to further spread of disease and social unrest. It is better to correct health education, social behaviors, and psychological interventions by targeting people as the most effective method to prevent social stigma caused by COVID-19, which is recommended to form specialized teams of medical, social, and behavioral science experts. To update the review, more studies are recommended in the future. Greater awareness of this topic may assist with improving public education during pandemics such as COVID-19 as well as access to support services for individuals impacted by stigmatization.
Supplemental Material
Supplemental material, sj-doc-1-smo-10.1177_20503121231208273 for Social stigma during COVID-19: A systematic review by SeyedAhmad SeyedAlinaghi, Amir Masoud Afsahi, Ramin Shahidi, Arian Afzalian, Pegah Mirzapour, Mohammad Eslami, Sepide Ahmadi, Parisa Matini, Soudabeh Yarmohammadi, Seyed Saeed Tamehri Zadeh, Pooria Asili, Parinaz Paranjkhoo, Maryam Ramezani, Sahar Nooralioghli Parikhani, Foziye Sanaati, Iman Amiri Fard, Elham Emamgholizade Baboli, Somaye Mansouri, Ava Pashaei, Esmaeil Mehraeen and Daniel Hackett in SAGE Open Medicine
Acknowledgments
The present study was conducted in collaboration with Khalkhal University of Medical Sciences, Iranian Institute for Reduction of High Risk Behaviors, Tehran University of Medical Sciences, and the University of Sydney.
Footnotes
Authors’ contributions: The conception and design of the study: Esmaeil Mehraeen, Seyed Ahmad Seyed Alinaghi. Acquisition of data: Ramin Shahidi, Arian Afzalian. Analysis and interpretation of data: Amir Masoud Afsahi. Drafting the article: Esmaeil Mehraeen, Pegah Mirzapour, Sepehr Eslami, Sepide Ahmadi, Parisa Matini, Soudabeh Yarmohammadi, Seyed Saeed Tamehri Zadeh, Pooria Asili, Parinaz Paranjkhoo, Maryam Ramezani, Sahar Nooralioghli Parikhani, Foziye Sanaati, Iman Amiri Fard, Elham Emamgholizade, Somaye Mansouri, Ava Pashaei. Revising it critically for important intellectual content: Seyed Ahmad Seyed Alinaghi, Daniel Hackett. Final approval of the version to be submitted: Seyed Ahmad Seyed Alinaghi, Esmaeil Mehraeen, Daniel Hackett.
Availability of data and material: The authors stated that all information provided in this article could be shared.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval and consent to participate: Not applicable.
Consent to publication: Not applicable.
ORCID iDs: Amir Masoud Afsahi  https://orcid.org/0000-0002-8906-7767
https://orcid.org/0000-0002-8906-7767
Esmaeil Mehraeen  https://orcid.org/0000-0003-4108-2973
https://orcid.org/0000-0003-4108-2973
Supplemental material: Supplemental material for this article is available online.
References
- 1. Bhanot D, Singh T, Verma SK, et al. Stigma and discrimination during COVID-19 pandemic. Front Public Health 2020; 8: 577018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Anderson TL. Understanding deviance: connecting classical | contemporary perspectives. Oxfordshire, UK: Taylor Francis, 2014. [Google Scholar]
- 3. Mehraeen E, Safdari R, SeyedAlinaghi S, et al. A mobile-based self-management application-usability evaluation from the perspective of HIV-positive people. Health Policy Technol 2020; 9(3): 294–301. [Google Scholar]
- 4. Mehraeen E, Safdari R, SeyedAlinaghi SA, et al. Identifying and validating requirements of a mobile-based self-management system for people living with HIV. Stud Health Technol Inform 2018; 248: 140–147. [PubMed] [Google Scholar]
- 5. Abdelhafiz AS, Alorabi M. Social stigma: the hidden threat of COVID-19. Front Public Health 2020; 8: 429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alsawalqa RO. Cyberbullying, social stigma, and self-esteem: the impact of COVID-19 on students from East and Southeast Asia at the University of Jordan. Heliyon 2021; 7(4): e06711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mehraeen E, Najafi Z, Hayati B, et al. Current treatments and therapeutic options for COVID-19 patients: a systematic review. Infect Disord Drug Targets 2022; 22(1): e260721194968. [DOI] [PubMed] [Google Scholar]
- 8. SeyedAlinaghi S, Karimi A, Barzegary A, et al. Mucormycosis infection in patients with COVID-19: a systematic review. Health Sci Rep 2022; 5(2): e529. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9. Mehraeen E, Dadras O, Afsahi AM, et al. Vaccines for COVID-19: a systematic review of feasibility and effectiveness. Infect Disord Drug Targets 2022; 22(2): e230921196758. [DOI] [PubMed] [Google Scholar]
- 10. Misra S, Le PD, Goldmann E, et al. Psychological impact of anti-Asian stigma due to the COVID-19 pandemic: a call for research, practice, and policy responses. Psychol Trauma 2020; 12(5): 461–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Adja KYC, Golinelli D, Lenzi J, et al. Pandemics and social stigma: who’s next? Italy’s experience with COVID-19. Public Health 2020; 185: 39–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fan W, Qian Y, Jin Y. Stigma, perceived discrimination, and mental health during China’s COVID-19 outbreak: a mixed-methods investigation. J Health Soc Behav 2021; 62(4): 562–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mehraeen E, Salehi MA, Behnezhad F, et al. Transmission modes of COVID-19: a systematic review. Infect Disord Drug Targets 2021; 21(6): e170721187995. [DOI] [PubMed] [Google Scholar]
- 14. Muschick P. Coronavirus and allergies: don’t sneeze-shame. Allentown, PA: The Morning Call, 2020. [Google Scholar]
- 15. Wells G, Shea BJ, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. Ottawa Hospital Research Institute, https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2021, assecced 17 June 2023).
- 16. Abuhammad S, Alzoubi KH, Al-Azzam S, et al. Stigma toward healthcare providers from patients during COVID-19 era in Jordan. Public Health Nurs 2022; 39(5): 926–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Abuhammad S, Alzoubi KH, Khabour O. Fear of COVID-19 and stigmatization towards infected people among Jordanian people. Int J Clin Pract 2021; 75(4): e13899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Adhikari SP, Rawal N, Shrestha DB, et al. Prevalence of anxiety, depression, and perceived stigma in healthcare workers in Nepal during later phase of first wave of COVID-19 pandemic: a web-based cross-sectional survey. Cureus 2021; 13(6): e16037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Adom D, Mensah JA, Osei M. The psychological distress and mental health disorders from COVID-19 stigmatization in Ghana. Soc Sci Human Open 2021; 4(1): 100186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Akour A, AlMuhaissen SA, Nusair MB, et al. The untold story of the COVID-19 pandemic: perceptions and views towards social stigma and bullying in the shadow of COVID-19 illness in Jordan. SN Soc Sci 2021; 1(9): 240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Al-Ghuraibi MA, Aldossry TM. Social stigma as an outcome of the cultural repercussions toward COVID-19 in Saudi Arabia. Cogent Soc Sci 2022; 8(1): 2053270. [Google Scholar]
- 22. Alajmi AF, Al-Olimat HS, Abu Ghaboush R, et al. Social avoidance and stigma among healthcare workers serving COVID-19 patients in Saudi Arabia. SAGE Open. 2022; 12(2): 381–390. [Google Scholar]
- 23. Alkathiri MA, Almohammed OA, Alqahtani F, et al. Associations of depression and anxiety with stigma in a sample of patients in Saudi Arabia who recovered from COVID-19. Psychol Res Behav Manag 2022; 15: 381–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Almoayad F, Mahboub S, Amer LB, et al. Stigmatisation of COVID-19 in Riyadh, Saudi Arabia: a cross-sectional study. Sultan Qaboos Univ Med J 2021; 21(4): 525–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Asiyah SN, Kumalasari MLF, Hadi MI, et al. The model of community stigma during the Covid-19 pandemic period in East Java Indonesia. Arch Psychiatry Res 2022; 58(1): 63–72. [Google Scholar]
- 26. Assefa N, Soura A, Hemler EC, et al. Covid-19 knowledge, perception, preventive measures, stigma, and mental health among healthcare workers in three Sub-Saharan African countries: a phone survey. Am J Trop Med Hyg 2021; 105(2): 342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Atinga RA, Alhassan NMI, Ayawine A. Recovered but constrained: narratives of Ghanaian COVID-19 survivors experiences and coping pathways of stigma, discrimination, social exclusion and their sequels. Int J Health Policy Manag 11(9): 1801–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Azizpour I, Mehri S, Moghaddam HR, et al. The impact of psychological factors on bereavement among frontline nurses fighting Covid-19. Int J Afr Nurs Sci 2021; 15: 100341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bhatnagar S, Kumar S, Rathore P, et al. Surviving COVID-19 is half the battle; living life with perceived stigma is other half: a cross-sectional study. Indian J Psychol Med 2021; 43(5): 428–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Caricati L, D’Agostino G, Sollami A, et al. A study on COVID-19-related stigmatization, quality of professional life and professional identity in a sample of HCWs in Italy. Acta Biomed 2022; 93(S2): e2022150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cassiani-Miranda CA, Campo-Arias A, Tirado-Otálvaro AF, et al. Stigmatisation associated with COVID-19 in the general Colombian population. Int J Soc Psychiatry 2021; 67(6): 728–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cénat JM, Noorishad PG, Kokou-Kpolou CK, et al. Prevalence and correlates of depression during the COVID-19 pandemic and the major role of stigmatization in low- and middle-income countries: a multinational cross-sectional study. Psychiatry Res 2021; 297: 113714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chandran N, Vinuprasad VG, Sreedevi C, et al. COVID-19-related stigma among the affected individuals: a cross-sectional study from Kerala, India. Indian J Psychol Med 2022; 44(3): 279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chen X, Liao Z, Huang S, et al. Stigmatizing attitudes toward COVID-19 among patients, their relatives and healthy residents in Zhangjiajie. Front Public Health 2022; 10: 808461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chew CC, Lim XJ, Chang CT, et al. Experiences of social stigma among patients tested positive for COVID-19 and their family members: a qualitative study. BMC Public Health 2021; 21(1): 1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chory A, Nyandiko W, Ashimosi C, et al. Social stigma related to COVID-19 disease described by primary and secondary school teachers and adolescents living with HIV in Western Kenya. Front Public Health 2021; 9: 757267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dar SA, Khurshid SQ, Wani ZA, et al. Stigma in coronavirus disease-19 survivors in Kashmir, India: a cross-sectional exploratory study. PLoS One 2020; 15(11): e0240152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Earnshaw VA, Brousseau NM, Hill EC, et al. Anticipated stigma, stereotypes, and COVID-19 testing. Stig Health 2020; 5(4): 390–393. [Google Scholar]
- 39. Facente SN, De Zuzuarregui M, Frank D, et al. Anticipated and experienced stigma after testing positive for SARS-CoV-2: a qualitative study. Health Promot Pract 2022: 15248399221115063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gopichandran V, Subramaniam S. A qualitative inquiry into stigma among patients with Covid-19 in Chennai, India. Indian J Med Ethics 2021; 6(3): 1–21. [DOI] [PubMed] [Google Scholar]
- 41. Grivel MM, Lieff SA, Meltzer GY, et al. Sociodemographic and behavioral factors associated with COVID-19 stigmatizing attitudes in the U.S. Stig Health 2021; 6(4): 371–379. [Google Scholar]
- 42. Grover S, Sahoo S, Mishra E, et al. Fatigue, perceived stigma, self-reported cognitive deficits and psychological morbidity in patients recovered from COVID-19 infection. Asian J Psychiatr 2021; 64: 102815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gutierrez AM, Schneider SC, Islam R, et al. Experiences of stigma in the United States during the COVID-19 pandemic. Stig Health Advance online publication, 2022. [Google Scholar]
- 44. Haddad C, Malhab SB, Malaeb D, Sacre H, et al. Stigma toward people with COVID-19 among the Lebanese population: a cross-sectional study of correlates and mediating effects. BMC Psychol 2021; 9(1): 164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hossain MB, Alam MZ, Islam MS, et al. COVID-19 public stigma in the context of government-based structural stigma: a cross-sectional online survey of adults in Bangladesh. Stig Health 2021; 6(2): 123–133. [Google Scholar]
- 46. Jain S, Das AK, Talwar V, et al. Social stigma of covid-19 experienced by frontline healthcare workers of department of anaesthesia and critical care of a tertiary healthcare institution in Delhi. Indian J Crit Care Med 2021; 25(11): 1241–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jayakody S, Hewage SA, Wickramasinghe ND, et al. “Why are you not dead yet?” – dimensions and the main driving forces of stigma and discrimination among COVID-19 patients in Sri Lanka. Public Health 2021; 199: 10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Jiang T, Zhou X, Lin L, et al. COVID-19-related stigma and its influencing factors: a nationwide cross-sectional study during the early stage of the pandemic in China. BMJ Open 2021; 11(8): e048983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kang E, Lee SY, Kim MS, et al. The psychological burden of COVID-19 stigma: evaluation of the mental health of isolated mild condition COVID-19 patients. J Korean Med Sci 2021; 36(3): e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kang S, Kang J. Age differences in psychological antecedents and behavioral consequences of stigmatization associated with COVID-19 among Koreans. Int J Environ Res Public Health 2022; 19(14): 8594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Khalid MF, Alam M, Rehman F, et al. Stigmatization of healthcare workers during the COVID-19 pandemic. Pakistan J Med Health Sci 2021; 15(6): 1379–1383. [Google Scholar]
- 52. Koyama Y, Nawa N, Yamaoka Y, et al. Association between social engagements and stigmatization of COVID-19 infection among community population in Japan. Int J Environ Res Public Health 2022; 19(15): 9050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Latifah L, Nurcahyani YD, Yunitawati D, et al. Stigma and mental health during covid-19 new normal transition in Indonesia. Indian J Forensic Med Toxicol 2021; 15(4): 1629–1635. [Google Scholar]
- 54. Li MY, Long J, Wang XY, et al. A comparison of COVID-19 stigma and AIDS stigma during the COVID-19 pandemic: a cross-sectional study in China. Front Psychiatry 2021; 12: 782501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lin B, Zhong G, Liang Z, et al. Perceived-stigma level of COVID-19 patients in China in the early stage of the epidemic: a cross-sectional research. PLoS One 2021; 16(10): e0258042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lohiniva AL, Dub T, Hagberg L, et al. Learning about COVID-19-related stigma, quarantine and isolation experiences in Finland. PLoS One 2021; 16(4): e0247962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mostafa A, Sabry W, Mostafa NS. COVID-19-related stigmatization among a sample of Egyptian healthcare workers. PLoS One 2020; 15(12): e0244172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Mustikasari M, Fadhillah H, Sunadi A, et al. The impact of COVID-19 on psychological and social stigma for Indonesian nurses: a cross-sectional survey. Front Psychiatry 2022; 13: 895788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Nashwan AJ, Valdez GFD, Al-Fayyadh S, et al. Stigma towards health care providers taking care of COVID-19 patients: a multi-country study. Heliyon 2022; 8(4): e09300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Preusting LC, Raadsen MP, Abourashed A, et al. COVID-19 related stigma and healthprotective behaviours among adolescents in the Netherlands: an explorative study. PLoS One 2021; 16(6): e0253342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ramaci T, Barattucci M, Ledda C, et al. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability 2020; 12(9): 3834. [Google Scholar]
- 62. Sachdeva A, Nandini H, Kumar V, et al. From stress to stigma – mental health considerations of health care workers involved in COVID19 management. Indian J Tuberc 2021; 69(4): 590–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Smith LE, Potts HWW, Amlȏt R, et al. Holding a stigmatizing attitude at the start of the COVID-19 outbreak: a cross-sectional survey. Br J Health Psychol 2022; 27(2): 588–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Soleimani F, Aligholipour M, Aghal M, et al. COVID 19 related perceived discrimination in medical settings, March and April 2020. Inquiry 2021; 58: 00469580211020884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Sorokin MY, Kasyanov ED, Rukavishnikov GV, et al. Stress and stigmatization in health-care workers during the COVID-19 pandemic. Indian J Psychiatry 2020; 62(9): S445–S453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Sousa AR, Cerqueira SSB, Santana TDS, et al. Stigma experienced by men diagnosed with COVID-19. Rev Bras Enferm 2021; 75(Suppl 1): e20210038. [DOI] [PubMed] [Google Scholar]
- 67. Taşdelen R, Ayik B, Kaya H, et al. Psychological reactions of Turkish healthcare workers during Covid-19 outbreak: the impact of stigmatization. Noro Psikiyatr Arsivi 2022; 59(2): 133–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Taylor S, Landry CA, Rachor GS, et al. Fear and avoidance of healthcare workers: an important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord 2020; 75: 102289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Teksin G, Uluyol OB, Onur OS, et al. Stigma-related factors and their effects on health-care workers during COVID-19 pandemics in Turkey: a multicenter study. Sisli Etfal Hastan Tip Bul 2020; 54(3): 281–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Wahyuhadi J, Efendi F, Al Farabi MJ, et al. Association of stigma with mental health and quality of life among Indonesian COVID-19 survivors. PLoS One 2022; 17(2): e0264218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Warren AM, Khetan R, Bennett M, et al. The relationship between stigma and mental health in a population of individuals with COVID-19. Rehab Psychol 2022; 67(2): 226–230. [DOI] [PubMed] [Google Scholar]
- 72. Yadav AK, Mangal V, Devarakonda R, et al. Perceived stigma among the patients of coronavirus disease-19 admitted at a dedicated COVID-19 hospital in Northern India: a cross-sectional study. Ind Psychiatry J 2021; 30(1): 118–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Yuan Y, Zhao YJ, Zhang QE, et al. COVID-19-related stigma and its sociodemographic correlates: a comparative study. Global Health 2021; 17(1): 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Yufika A, Pratama R, Anwar S, et al. Stigma against COVID-19 among health care workers in Indonesia. Disaster Med Public Health Prep 2021; 16(5): 1942–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Zandifar A, Badrfam R, Khonsari NM, et al. Prevalence and associated factors of posttraumatic stress symptoms and stigma among health care workers in contact with COVID-19 patients. Iran J Psychiatry 2020; 15(4): 340–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Zhang TM, Yao H, Fang Q, et al. Public stigma of covid-19 and its correlates in the general population of China. Int J Environ Res Public Health 2021; 18(21): 11718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Zhao L, Wang Z, Guan J, et al. Coronavirus disease 2019–related stigma in China: a descriptive study. Front Psychol 2021; 12: 694988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Delgado A. COVID-19 with stigma: new evidence from mobility data and “Go to Travel” campaign. Heliyon 2023; 9(5): e15704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ranganathan P, Tandon S, Khan S, et al. Investigating stigma during the COVID-19 pandemic: living conditions, social determinants and experiences of infection among employees at a tertiary referral cancer centre. J Cancer Policy 2023; 36: 100412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Peters L, Burkert S, Brenner C, et al. Experienced stigma and applied coping strategies during the COVID-19 pandemic in Germany: a mixed-methods study. BMJ Open 2022; 12(8): e059472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Pantelic M, Ziauddeen N, Boyes M, et al. The prevalence of stigma in a UK community survey of people with lived experience of long COVID. Lancet 2022; 400: S84. [Google Scholar]
- 82. Osman DM, Khalaf FR, Ahmed GK, et al. Worry from contracting COVID-19 infection and its stigma among Egyptian health care providers. J Egypt Public Health Assoc 2022; 97(1): 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Adhikari T, Aggarwal S, Nair S, et al. Factors associated with COVID-19 stigma during the onset of the global pandemic in India: a cross-sectional study. Front Public Health 2022; 10: 992046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Alchawa M, Naja S, Ali K, et al. COVID-19 perceived stigma among survivors: a cross-sectional study of prevalence and predictors. Eur J Psychiatry 2023; 37(1): 24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Esiaka D, Nwakasi C, Mahmoud K, et al. Perceived risk of COVID-19 diagnosis and stigma among Nigerians. Sci Afr 2022; 18: e01411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Faghankhani M, Nourinia H, Rafiei-Rad AA, et al. COVID-19 related stigma among the general population in Iran. BMC Public Health 2022; 22(1): 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Gaber DM, Ahmed MM, Sayed AM, et al. Perception of COVID-19-related stigma and associated psychological challenges among healthcare workers at Cairo University hospitals. J Int Med Res 2023; 51(1): 03000605221148833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Sangma RD, Kumar P, Nerli LM, et al. Social stigma and discrimination in Coronavirus Disease-2019 survivors and its changing trend: a longitudinal study at tertiary care center Gujarat, India. Asian J Social Health 2022; 5(2): 68. [Google Scholar]
- 89. Sattler S, Maskileyson D, Racine E, et al. Stigmatization in the context of the COVID-19 pandemic: a survey experiment using attribution theory and the familiarity hypothesis. BMC Public Health 2023; 23(1): 521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Sawaguchi E, Nakamura S, Watanabe K, et al. COVID-19-related stigma and its relationship with mental wellbeing: a cross-sectional analysis of a cohort study in Japan. Front Public Health 2022; 10: 1010720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Scholz U, Bierbauer W, Lüscher J. Social stigma, mental health, stress, and health-related quality of life in people with long COVID. Int J Environ Res Public Health 2023; 20(5): 3927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Lim T, Zelaya C, Latkin C, et al. Individual-level socioeconomic status and community-level inequality as determinants of stigma towards persons living with HIV who inject drugs in Thai Nguyen, Vietnam. J Int AIDS Soc 2013; 16: 18637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Adongo PB, Tabong PT-N, Asampong E, et al. Beyond knowledge and awareness: addressing misconceptions in Ghana’s preparation towards an outbreak of Ebola virus disease. PLoS One 2016; 11(2): e0149627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Tenkorang EY. Ebola-related stigma in Ghana: individual and community level determinants. Soc Sci Med 2017; 182: 142–149. [DOI] [PubMed] [Google Scholar]
- 95. Shi L, Que J-Y, Lu Z-A, et al. Prevalence and correlates of suicidal ideation among the general population in China during the COVID-19 pandemic. Eur Psychiatry 2021; 64(1): e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Naeem SB, Bhatti R. The Covid-19 ‘infodemic’: a new front for information professionals. Health Inform Libr J 2020; 37(3): 233–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Que J, Yuan K, Gong Y, et al. Raising awareness of suicide prevention during the COVID-19 pandemic. Neuropsychopharmacol Rep 2020; 40(4): 392–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Fischer LS, Mansergh G, Lynch J, et al. Addressing disease-related stigma during infectious disease outbreaks. Disaster Med Public Health Prep 2019; 13(5–6): 989–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Nyakarahuka L, Skjerve E, Nabadda D, et al. Knowledge and attitude towards Ebola and Marburg virus diseases in Uganda using quantitative and participatory epidemiology techniques. PLoS Negl Trop Dis 2017; 11(9): e0005907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Gollust SE, Nagler RH, Fowler EF. The emergence of COVID-19 in the US: a public health and political communication crisis. J Health Politics Policy Law 2020; 45(6): 967–981. [DOI] [PubMed] [Google Scholar]
- 101. Holzemer WL, Uys L, Makoae L, et al. A conceptual model of HIV/AIDS stigma from five African countries. J Adv Nurs 2007; 58(6): 541–551. [DOI] [PubMed] [Google Scholar]
- 102. Weiss MG, Doongaji DR, Siddhartha S, et al. The explanatory model interview catalogue (EMIC). Br J Psychiatry 1992; 160(6): 819–830. [DOI] [PubMed] [Google Scholar]
- 103. Sirois FM, Owens J. Factors associated with psychological distress in health-care workers during an infectious disease outbreak: a rapid systematic review of the evidence. Front Psychiatry 2021; 11: 589545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Volinn IJ. Issues of definitions and their implications: AIDS and leprosy. Soc Sci Med 1989; 29(10): 1157–1162. [DOI] [PubMed] [Google Scholar]
- 105. Aqeel U, Ali MD, Iqbal Z, et al. Knowledge, attitudes, and practices toward coronavirus disease-19 infection among residents of Delhi NCR, India: a cross-sectional survey based study. Asian J Pharm Clin Res 2020; 13: 110–116. [Google Scholar]
- 106. Gregorio ER, Jr, Medina JRC, Lomboy MFTC, et al. Knowledge, attitudes, and practices of public secondary school teachers on Zika Virus disease: a basis for the development of evidence-based Zika educational materials for schools in the Philippines. PloS One 2019; 14(3): e0214515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Marbán-Castro E, Villén-Gonzalvo A, Enguita-Fernàndez C, et al. Uncertainties, fear and stigma: perceptions of Zika virus among pregnant women in Spain. Int J Environ Res Public Health 2020; 17(18): 6643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Park HY, Park WB, Lee SH, et al. Posttraumatic stress disorder and depression of survivors 12 months after the outbreak of Middle East respiratory syndrome in South Korea. BMC Public Health 2020; 20: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Yuan K, Gong Y-M, Liu L, et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol Psychiatry 2021; 26(9): 4982–4998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Jain M, Kar SK, Yadav M. A questionnaire survey of stigma related to human immunodeficiency virus infection/acquired immunodeficiency syndrome among healthy population: Survey of stigma related to HIV infection/AIDS among healthy population. Commun Acquir Infect 2017; 4: 2017. [Google Scholar]
- 111. Turan JM, Elafros MA, Logie CH, et al. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med 2019; 17(1): 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Lee S, Chan LY, Chau AM, et al. The experience of SARS-related stigma at Amoy Gardens. Soc Sci Med 2005; 61(9): 2038–2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Person B, Sy F, Holton K, et al. Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis 2004; 10(2): 358–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Miller CT, Kaiser CR. A theoretical perspective on coping with stigma. J Soc Iss 2001; 57(1): 73–92. [Google Scholar]
- 115. Des Jarlais DC, Galea S, Tracy M, et al. Stigmatization of newly emerging infectious diseases: AIDS and SARS. Am J Public Health 2006; 96(3): 561–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-smo-10.1177_20503121231208273 for Social stigma during COVID-19: A systematic review by SeyedAhmad SeyedAlinaghi, Amir Masoud Afsahi, Ramin Shahidi, Arian Afzalian, Pegah Mirzapour, Mohammad Eslami, Sepide Ahmadi, Parisa Matini, Soudabeh Yarmohammadi, Seyed Saeed Tamehri Zadeh, Pooria Asili, Parinaz Paranjkhoo, Maryam Ramezani, Sahar Nooralioghli Parikhani, Foziye Sanaati, Iman Amiri Fard, Elham Emamgholizade Baboli, Somaye Mansouri, Ava Pashaei, Esmaeil Mehraeen and Daniel Hackett in SAGE Open Medicine