Abstract
Background
Weight gain is often considered a side effect of combination hormonal contraceptives, and many women and clinicians believe that an association exists. Concern about weight gain can limit the use of this highly effective method of contraception by deterring the initiation of its use and causing early discontinuation among users. However, a causal relationship between combination contraceptives and weight gain has not been established.
Objectives
The aim of the review was to evaluate the potential association between combination contraceptive use and changes in weight.
Search methods
In November 2013, we searched the computerized databases CENTRAL (The Cochrane Library), MEDLINE, POPLINE, EMBASE, and LILACS for studies of combination contraceptives, as well as ClinicalTrials.gov and International Clinical Trials Registry Platform (ICTRP). For the initial review, we also wrote to known investigators and manufacturers to request information about other published or unpublished trials not discovered in our search.
Selection criteria
All English‐language, randomized controlled trials were eligible if they had at least three treatment cycles and compared a combination contraceptive to a placebo or to a combination contraceptive that differed in drug, dosage, regimen, or study length.
Data collection and analysis
All titles and abstracts located in the literature searches were assessed. Data were entered and analyzed with RevMan. A second author verified the data entered. For continuous data, we calculated the mean difference and 95% confidence interval (CI) for the mean change in weight between baseline and post‐treatment measurements using a fixed‐effect model. For categorical data, such as the proportion of women who gained or lost more than a specified amount of weight, the Peto odds ratio with 95% CI was calculated.
Main results
We found 49 trials that met our inclusion criteria. The trials included 85 weight change comparisons for 52 distinct contraceptive pairs (or placebos). The four trials with a placebo or no intervention group did not find evidence supporting a causal association between combination oral contraceptives or a combination skin patch and weight change. Most comparisons of different combination contraceptives showed no substantial difference in weight. In addition, discontinuation of combination contraceptives because of weight change did not differ between groups where this was studied.
Authors' conclusions
Available evidence was insufficient to determine the effect of combination contraceptives on weight, but no large effect was evident. Trials to evaluate the link between combination contraceptives and weight change require a placebo or non‐hormonal group to control for other factors, including changes in weight over time.
Plain language summary
Effect of birth control pills and patches on weight
Weight gain is thought to be a side effect of birth control methods. Many women and healthcare providers believe that pills and patches cause weight gain. Concern about weight gain can limit the use of these effective birth control methods. Fear of weight gain keeps some women from starting the pill or patch. Women may stop using the pill because they think it caused weight gain. This review looked at trials of birth control pills or patches where the woman's weight was measured.
In November 2013, we did a computer search for studies of pills or patches containing two types of hormones. For the initial review, we also wrote to researchers and manufacturers to find other trials. We included randomized trials in the English language if they had at least three treatment cycles. The studies also had to compare two types of birth control methods or one type with a 'dummy' method.
We found 49 trials. These trials compared 52 different pairs of birth control methods, or a birth control method and a 'dummy' method. The four trials with a dummy or no method group did not show that these pills or patches led to weight change. Most studies of different birth control methods showed no large weight difference. Also, women did not stop using the pill or patch because of weight change. The evidence was not strong enough to be sure that these methods did not cause some weight change. However, we found no major effect on weight. To look at the link between these birth control methods and weight change, studies should have a 'dummy' method or a group not using hormones. Having that type of control group would help remove other factors, such as weight change over time.
Background
Weight gain is often considered a side effect of using combination contraceptives (that is, an estrogen plus a progestin) (IOM 1996; Nelson 2007), and many women and clinicians believe that an association exists. Almost three‐quarters of women in a random survey conducted in the United Kingdom reported believing that weight gain was related to oral contraceptive use (Turner 1994). In a Canadian survey of women filling an oral contraceptive (OC) prescription (Gaudet 2004), 68% had counseling from their physician on weight gain and the pill. Of those who had counseling, 36% said their weight would stay the same while on the pill compared to 50% of those who had no counseling. In the United States, 45% of adolescents starting OC use believed that oral contraceptive use increased the risk of weight gain (Emans 1987). Also, in a large German convenience sample, about 27% of ever users reported gaining weight from oral contraceptive use (Oddens 1999). In a representative sample of 3600 females in France, aged 15 to 45 years, 1665 were taking OCs (Le 2003). Of these women using the pill, 30% claimed to have gained weight on their most recent pill.
Concern about weight gain can deter the initiation of combination contraceptives and cause early discontinuation among users. Weight gain was the most frequently cited reason for oral contraceptive discontinuation in a national study of adult women in the United States (Rosenberg 1998). A second survey found that about 20% of women claimed that weight gain was a reason for oral contraceptive discontinuation or failure to initiate use (Wysocki 2000). In a convenience sample of oral contraceptive users in five European nations, women who reported weight gain had a relative risk of 1.4 (95% CI 1.2 to 1.6) of method discontinuation before two years of use compared to those who did not report a gain in weight (Rosenberg 1995). Furthermore, even the perception of weight gain can lead to contraceptive discontinuation. A United States study found that women who stopped using OCs were more likely to report weight gain than those who continued using the method, even with no significant difference in measured weight gain between the two groups (Emans 1987). Thus, concern about weight gain limits the use of a highly effective method of contraception.
Nevertheless, a causal relationship between combination contraceptives and weight gain has not been established. Several mechanisms by which combination contraceptives could lead to weight gain have been hypothesized. In general, weight gain is due to an increase in one or more factors of fluid retention, muscle mass, and fat deposition. Fluid retention could be induced by the mineralocorticoid activity that occurs when ethinyl estradiol, the estrogen in combination oral contraceptives, enters the renin‐angiotensin‐aldosterone system (Corvol 1983). Estrogen has been associated with increased subcutaneous fat, especially in the breasts, hips, and thighs (Nelson 2007). The anabolic properties of combination contraceptives could result in increased food intake through a physiological effect on satiety and appetite. Androgens may stimulate nitrogen retention and increase muscle mass, although it is unlikely that oral contraceptives would cause such weight gain (Nelson 2007).
The possible causal association between combination contraceptives and weight gain is difficult to study for several reasons. During adolescence, some weight gain is developmentally normal and appropriate. Also, women tend to gain weight over time (Flegal 2000). A contemporaneous control group is needed, but a randomized controlled trial comparing a combination contraceptive method with a placebo or non‐hormonal method for contraception raises ethical issues. Few such studies have been conducted. Comparing combination contraceptive products is complicated by the variety of formulations and regimens. In addition, most combination contraceptive studies have been of short duration (that is, six cycles or fewer); more time might be required for the weight gain to become evident. Finally, no consensus exists regarding what constitutes excessive weight gain. Ideally, studies would set an a priori definition of clinically important weight gain, but this is rarely specified, perhaps because weight change is not a primary outcome in most comparison trials of combination contraception. Most studies that present a dichotomous classification for weight gain selected either 2.0 or 2.3 kilograms as the cut point; however, the justification for this decision is not apparent. Even if clinically important weight gain was well specified, any gain in weight could still be relevant since the mere perception of weight gain is associated with discontinuation of oral contraception.
Objectives
The aim of the review was to evaluate the potential association between combination contraceptive use and changes in weight. The primary hypothesis was that combination contraceptives do not result in weight changes greater than that of a placebo. The secondary hypothesis was that different formulations and regimens of combination contraceptives are not associated with differences in weight changes.
Methods
Criteria for considering studies for this review
Types of studies
All randomized controlled trials reported in English (Juni 2002; Moher 2000) that compared a combination contraceptive to a placebo, no intervention, or a combination contraceptive that differed in drug, dosage, regimen, or study length.
Types of participants
Women of reproductive age without medical contraindications to combination contraceptives.
Types of interventions
Any combination contraceptive compared to a placebo, no intervention, or another combination contraceptive. Trial drug interventions must have included at least three consecutive cycles to be eligible.
Types of outcome measures
Trials must have collected data on change in body weight to be eligible for inclusion. Weight change could have been measured as either the change in the study group's mean weight or as the proportion of the study group who lost or gained more than a specified amount.
Search methods for identification of studies
Electronic searches
In November 2013, we searched the computerized databases Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library), MEDLINE, POPLINE, EMBASE, and LILACS for studies of combination contraceptives. We also searched for trials via ClinicalTrials.gov and the search portal of the International Clinical Trials Registry Platform (ICTRP). The strategies are given below.
Searching other resources
For the initial review, we wrote to known investigators and manufacturers to request information about other published or unpublished trials not discovered in our search.
Data collection and analysis
Selection of studies
All titles and abstracts identified during the literature searches were assessed for inclusion, and all potentially relevant articles were photocopied. For the initial review, we wrote to the manufacturers of combination contraception and authors of the included trials to seek other published or unpublished trials.
Data extraction and management
The abstracted data were entered into RevMan and were double‐checked by a second author. The analysis depended on the data available. For the mean change in weight between baseline and post‐treatment measurements, the mean difference (MD) with 95% confidence interval (CI) was calculated using a fixed‐effect model. Alternatively, the Peto odds ratio (OR) with 95% CI was calculated using the proportion of women who gained or lost more than a specified amount of weight.
Significant weight change could be considered a negative side effect of contraceptive use. We used a consistent direction for the graph labels even though the outcomes differed. Therefore, the intervention ‘favors treatment’ if the change is greater in the control group. The intervention ‘favors control’ if the change is greater in the treatment group.
Assessment of risk of bias in included studies
The validity of trials was critically appraised by assessing potential biases; however, summary quality scores were not calculated since the available evidence does not support their use (Higgins 2011). The appraisal of potential biases concentrated on the study design, blinding, randomization method, group allocation concealment, and loss to follow up and early discontinuation.
Measures of treatment effect
Despite some trials reporting weight change data for multiple cycles, only one weight change measure was abstracted for each intervention group. We chose the cycle 12, cycle 6, or last treatment cycle data (in this order of preference) to facilitate comparisons between trials. For trials that included more than two interventions, comparisons were made between the control group and the other groups. If the authors did not identify a control group, all possible combinations were included in the review. We did not use any technique to control for multiple testing.
Significance testing has been criticized for forcing the decision to recognize a difference between two interventions to rest on an arbitrary alpha‐level. Rather than determine differences solely based on a dichotomous classification of the P value, analyses using interval estimation consider both the location of the point estimate and the spread of the CI (Rothman 1998). While this process introduces more subjectivity, borderline 'statistically significant' results are not overlooked and clinically insignificant results are not ascribed undue importance. Although interval estimation is a preferable method, given the reliance on significance testing, we presented results based on both considerations.
Dealing with missing data
For the initial review, we wrote to the authors of 94 trials that either did not report weight data or reported insufficient details. At that point we revised and broadened the search strategy and decided that continuing to contact the authors of trials that appeared to be eligible except for a lack of weight data was no longer feasible. The 14 trials with additional, unpublished data supplied by the authors contacted before the protocol change were included in the present review.
Since point estimates that are not accompanied by a measure of sampling variation have limited interpretation, trial reports that did not include the standard error, standard deviation, or CI for the mean change in weight were not included in the review. For trials that did not report the denominators used to calculate the mean weight difference, or the percentage of women experiencing weight change, we estimated these numbers based on denominators used for other outcomes or the number of women who completed the trial.
Data synthesis
Studies were combined for a meta‐analysis only when identical drugs, dosages, regimens, and delivery systems were compared. No sensitivity analyses were planned since few trials were anticipated to be eligible for meta‐analysis. The data abstracted for the review were dependent on the analytic method used in the trial report (for example, intent to treat, per protocol, or a modification of either type).
Results
Description of studies
Results of the search
Initial review
The initial search strategy in 2002 yielded 570 reports of randomized controlled trials that compared a combination contraceptive to a placebo or to another combination contraceptive. Of those, 476 articles were not eligible for inclusion due to a study length less than three treatment cycles in duration or a lack of reported weight change. An additional 53 articles with weight data were excluded since they lacked an estimate of the sampling variability for the mean difference in weight. The 41 eligible articles, including the 14 articles with additional unpublished data from the authors, reported on 44 trials. One article (Oelkers 2000) described two trials, and two articles (Coney 2001; Kaunitz 2000) each reported pooled results from two eligible trials with similar or identical protocols. Since they could not be disaggregated, we treated the pooled results as if they were from one larger trial, for a total of 42 trials.
Updates
2005: 12 new RCTs of combination contraceptives also included a weight measurement. Only two trials were of sufficient duration and had reported weight change data with sampling variability, which yielded 44 trials.
2008: 13 trials had weight measurements, but only three had sufficient data for inclusion, for a new total of 47 trials.
2011: Of five possible trials, two met our inclusion criteria. The new total was 49 trials.
2013: The search yielded 134 unduplicated citations from the electronic databases. We reviewed the full text of eight articles; none met our inclusion criteria. In addition, we found 32 unduplicated listings in ClinicalTrials.gov and ICTRP. We identified one ongoing trial that was relevant (Mahidol 2013).
Included studies
Of the 49 eligible trials, four included a placebo group or no hormonal method. Three of these trials evaluated oral contraceptives (Coney 2001; Goldzieher 1971; Procter‐Gray 2008) and one studied a contraceptive skin patch (Sibai 2001). The products evaluated in the 49 trials included 18 progestins and three estrogens. Trials examined combination oral contraceptives except for the following comparisons: two combination injectables (Sang 1995); two combination vaginal rings (Weisberg 1999); a combination skin patch (Sibai 2001; Stewart 2005); and a combination ring with an oral contraceptive (Milsom 2006; Oddsson 2005). Seven trials included more than two intervention groups; three of these trials did not specify a control group.
The sample sizes for the trials ranged from 20 to 5654 randomized participants with a median of 196 participants. The study location was not described for 13 trials; the other studies were conducted in locations worldwide. The number of trial sites ranged from a single site (12 trials) to 131 sites, except for 10 trials that did not specify the number of sites. The duration of the trials ranged from 3 to 24 treatment cycles with most trials designed to be either 6 or 12 treatment cycles in length. The eligibility criteria for the participants varied among the trials with most trials recruiting healthy women of reproductive age without contraindications to hormonal contraceptive use. However, six of the articles did not describe any inclusion or exclusion criteria.
Risk of bias in included studies
The quality of the reporting of the trials on this topic was generally poor, and poor quality is associated with empirical evidence of bias (Schulz 1995).
Allocation
The method of generating the randomization sequence was not reported for 31 trials. The remaining 18 trials included at least some detail of the process (for example, use of a random numbers table, pre‐distributed lists, or computer‐generated sequence). Most trial reports (N = 45) did not describe a method of allocation concealment (Schulz 2002a). Cachrimanidou 1993 and Kashanian 2010 reported the use of sealed envelopes but did not provide details on whether the envelopes were impervious to deciphering (for example, use of opaque, sequentially‐numbered envelopes). Only three articles reported adequate allocation concealment: Miller 2001 used sealed, sequentially‐numbered, opaque envelopes containing carbon paper, which allowed the participant to sign the allocation card before study staff opened the envelope and learned the group assignment; Milsom 2006 and Oddsson 2005 had interactive voice response systems for the randomization process.
Only four articles reported the number of women recruited for the trial (Cachrimanidou 1993; Kashanian 2010; Oddsson 2005; Wiegratz 2002). One article stated that not all randomized women were included in the study results but did not specify the number of randomized women (Worsley 1980). A second trial report included sample sizes for the weight outcome but did not state whether these data included all randomized women (Sibai 2001). Although they reported the total number of randomized women, seven trial reports did not provide the number of randomized women stratified by study group.
Blinding
About half of the eligible trials were open; two were single‐blinded, 10 were double‐blinded, and one was triple‐blinded. Blinding was not mentioned in 15 trials. Participants, investigators, and outcome assessors were blinded as to group assignment in the triple‐blinded study (Oelkers 1995), and participants appeared to have been blinded in two of the double‐blinded trials (Coney 2001; Goldzieher 1971) using active and placebo pills that were identical in appearance. Since the Goldzieher 1971 trial reported that the randomization code was not broken during the study, the blinding of the investigators can be inferred. Two trials did not inform the assessors of group assignment, but the investigators and participants were not blinded (Kashanian 2010; Procter‐Gray 2008). The remaining blinded trials were unclear about who was blinded, and none of the trials included details regarding whether blinding appeared to have been implemented successfully (Schulz 2002b).
Incomplete outcome data
Eleven trials did not report the denominators used to derive the mean weight difference (Coenen 1996) or the percentage of women with weight change greater than a specified amount (Brill 1991; Dionne 1974; Endrikat 1999; Endrikat 2001a; Goldzieher 1971; Halbe 1998; Koetsawang 1995; Lachnit‐Fixson 1984; Oelkers 1995; Rosenbaum 2000). Discrepancies existed in at least 13 trials, since more women were missing in the weight estimate than could be explained with the possible reasons in the article (for example, non‐starters, early discontinuation, those lost to follow up, or exclusion).
Deducing which participants were included in the reported weight change estimate was hindered for most trials due to the lack of details regarding the method of analysis. An intention‐to‐treat analysis was described for three trials (Oddsson 2005; Procter‐Gray 2008; Wiegratz 2002); a per‐protocol analysis (also called valid‐case) was reported for three trials (Endrikat 1999; Serfaty 1998; Winkler 1996); and an analysis based on all participants who started treatment was reported for five trials (Coney 2001; Endrikat 2001b; Gruber 2006; Kaunitz 2000; Milsom 2006). Two trials (Endrikat 2001a; Stewart 2005) described intention‐to‐treat or valid‐case analyses but did not specify which was used for the weight change data. Two trials (Spellacy 1970; Van der Does 1995) had complete study participation and based the weight estimates on measurements from all participants. Kashanian 2010 excluded from the analysis two women who discontinued the intervention. The remaining 33 trials did not specify the analytic method used for the weight change data.
Other potential sources of bias
Change in body weight was a primary outcome for only one trial (Sibai 2001). Most trials either recorded weight at the baseline and follow‐up clinic visits or did not describe the method used for measuring weight. Liukko 1987 reported that the clinic visits, in which weight was measured, were scheduled around day 22 of the cycle. Milsom 2006 and Procter‐Gray 2008 described the methods used to standardize weight measurements. Four trials instructed participants to weigh and record their weight at home (Rosenbaum 2000), at home without clothing every second day (Oelkers 2000, Study 2) and in a fasting state (Oelkers 1995), or at home without clothing on a weekly basis (Oelkers 2000, Study 3).
Most trial reports either did not include data on loss to follow up (19 trials) or reported it combined with early discontinuation (nine trials). Loss to follow up ranged from zero to 17% for the 20 trials with loss to follow up reported separately from early discontinuation and from 10% to 35% for those that only reported losses from all causes. Early discontinuation ranged from zero to 39% for the 31 trials that reported this study factor separately. Eight trial reports did not include information on early discontinuation. Furthermore, 18 trial reports described excluding randomized women from study participation or analysis. Exclusions after randomization are not consistent with an intention‐to‐treat analysis and could have led to biased results (Weiss 1998).
Effects of interventions
The trials included 85 weight change comparisons for 52 distinct contraceptive pairs (or a placebo) that were eligible for the present review. We combined data from two or more trials for four of the 84 comparisons since they were identical in drug, dosage, regimen, and study length. The comparisons of a combination contraceptive with a placebo or no hormonal method showed no significant differences in weight change. These included five comparisons between an oral contraceptive and placebo (Coney 2001; Goldzieher 1971) or no intervention (Procter‐Gray 2008) and one comparison between a combination skin patch and placebo (Sibai 2001).
The study groups differed significantly in six comparisons of two pills and one comparison of the vaginal ring with an OC.
-
Three studies showed differences in the numbers of women with a weight change of more than 2 kg.
For gaining more than 2 kg, the OR was 3.29 (95% CI 1.84 to 5.88) for women assigned to oral desogestrel 150 μg and ethinyl estradiol (EE) 30 μg compared to those with oral levonorgestrel 50‐75‐125 μg and EE 30‐40‐30 μg (Lachnit‐Fixson 1984) (Analysis 11.1).
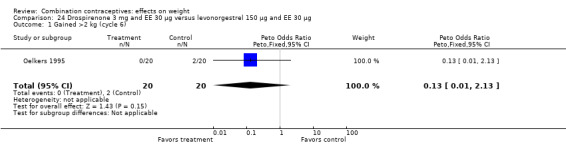
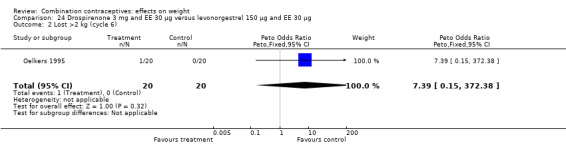
For losing more than 2 kg, the OR was 9.22 (95% CI 1.79 to 55.04) for oral drospirenone 3 mg and EE 15 μg compared to oral levonorgestrel 150 μg and EE 30 μg (Oelkers 1995) (Analysis 20.2).
The OR for losing more than 2 kg was 1.65 (95% CI 1.13 to 2.41) for the oral desogestrel 150 μg and EE 20 μg group compared to the oral gestodene 75 μg and EE 20 μg group (Serfaty 1998) (Analysis 9.2).
-
Four studies showed differences in the mean weight change between groups. One group had a slight increase while the other group showed a small decrease or no change.
The mean difference in Kaunitz 2000 was 0.26 kg (95% CI 0.12 to 0.40) (Analysis 46.1). Women assigned to oral norethindrone 500‐750‐1000 μg and EE 35 μg group had a slight mean increase, and those in the oral desogestrel 100‐125‐150 μg and EE 25 μg group had a slight decrease.
In Loudon 1990, the mean difference was 0.70 kg (95% CI 0.14 to 1.26) (Analysis 35.1). The group with oral levonorgestrel 150 μg and EE 30 μg gained, on average, while those with oral gestodene 75 μg and EE 30 μg lost a little weight.
The mean difference was ‐0.67 kg (95% CI ‐1.16 to ‐0.18) in Gruber 2006 (Analysis 23.1). On average, the women assigned to drospirenone 3 mg and EE 20 μg had a slight decrease, and the group with desogestrel 150 μg and EE 20 μg had a small increase.
Tn Milsom 2006, the mean difference was 0.40 kg (95% CI 0.03 to 0.77) (Analysis 52.1). Women assigned to the vaginal ring gained on average while the group with the combination oral contraceptive (COC) containing drospirenone 3 mg and EE 30 µg had no change overall.
11.1. Analysis.
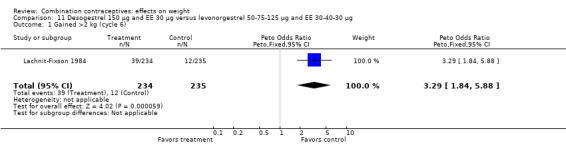
Comparison 11 Desogestrel 150 µg and EE 30 µg versus levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg, Outcome 1 Gained >2 kg (cycle 6).
20.2. Analysis.
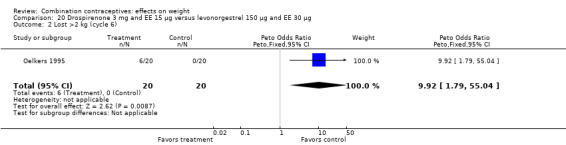
Comparison 20 Drospirenone 3 mg and EE 15 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 2 Lost >2 kg (cycle 6).
9.2. Analysis.
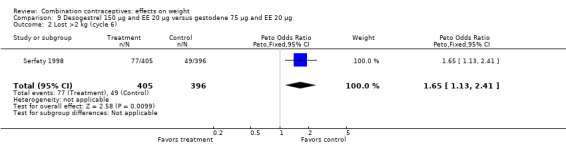
Comparison 9 Desogestrel 150 µg and EE 20 µg versus gestodene 75 µg and EE 20 µg, Outcome 2 Lost >2 kg (cycle 6).
46.1. Analysis.
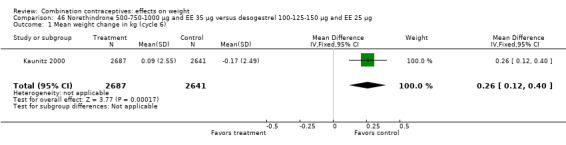
Comparison 46 Norethindrone 500‐750‐1000 µg and EE 35 µg versus desogestrel 100‐125‐150 µg and EE 25 µg, Outcome 1 Mean weight change in kg (cycle 6).
35.1. Analysis.
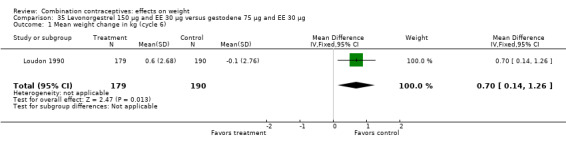
Comparison 35 Levonorgestrel 150 µg and EE 30 µg versus gestodene 75 µg and EE 30 µg, Outcome 1 Mean weight change in kg (cycle 6).
23.1. Analysis.
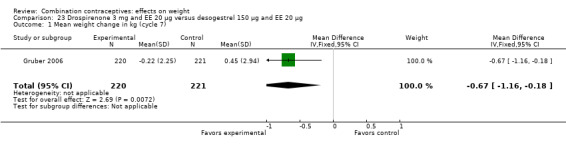
Comparison 23 Drospirenone 3 mg and EE 20 μg versus desogestrel 150 μg and EE 20 μg, Outcome 1 Mean weight change in kg (cycle 7).
52.1. Analysis.
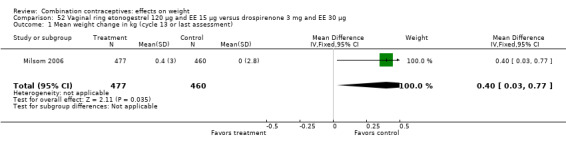
Comparison 52 Vaginal ring etonogestrel 120 µg and EE 15 µg versus drospirenone 3 mg and EE 30 µg, Outcome 1 Mean weight change in kg (cycle 13 or last assessment).
Six additional comparisons had a point estimate and 95% CI that were consistent with at least a minimal difference between the two groups. Odds ratios for three of the six studies were as follows:
OR 1.54 (95% CI 0.92 to 2.60) for gaining more than 2 kg with oral gestodene 75 μg and EE 30 μg versus oral norgestimate 250 μg and EE 35 μg (Brill 1991) (Analysis 29.1);
OR 1.75 (95% CI 0.98 to 3.11) for gaining more than 2.5 kg with oral lynestrenol 2 mg and EE 40 μg versus oral lynestrenol 1 mg and EE 40 μg (Koetsawang 1977) (Analysis 42.1);
OR 1.69 (95% CI 0.89 to 3.20) of losing more than 2 kg with oral norethisterone 500 μg and EE 20 μg versus oral levonorgestrel 150 μg and EE 30 μg (Endrikat 2001b) (Analysis 45.2).
29.1. Analysis.
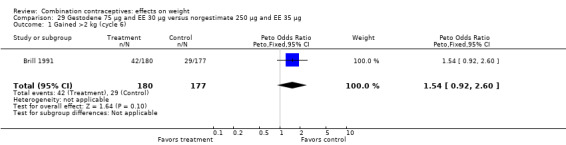
Comparison 29 Gestodene 75 µg and EE 30 µg versus norgestimate 250 µg and EE 35 µg, Outcome 1 Gained >2 kg (cycle 6).
42.1. Analysis.
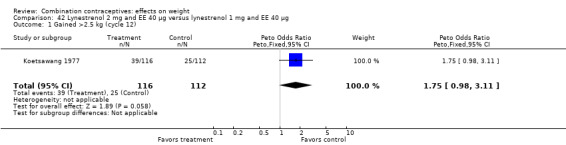
Comparison 42 Lynestrenol 2 mg and EE 40 µg versus lynestrenol 1 mg and EE 40 µg, Outcome 1 Gained >2.5 kg (cycle 12).
45.2. Analysis.
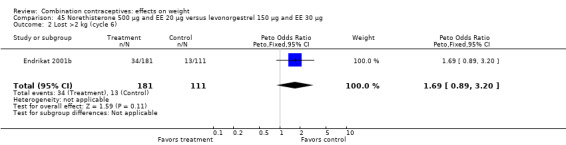
Comparison 45 Norethisterone 500 µg and EE 20 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 2 Lost >2 kg (cycle 6).
Mean differences in kg were as follows for the other three studies:
MD 1.30 (95% CI ‐0.32 to 2.92) between oral levonorgestrel 50, 75, 125 μg and EE 30, 40, 30 μg group and oral desogestrel 50‐100‐150 μg and EE 35‐30‐30 μg group (Van der Does 1995) (Analysis 38.2);
MD 1.80 (95% CI ‐0.73 to 4.33) between a standard versus prolonged oral norgestrel and EE regimen (Miller 2001) (Analysis 48.1);
MD 1.14 (95% CI ‐0.54 to 2.82) between oral dl‐norgestrel 500 μg and EE 50 μg group and oral norethisterone acetate 1 mg and EE 50 μg group (Worsley 1980) (Analysis 18.1).
38.2. Analysis.
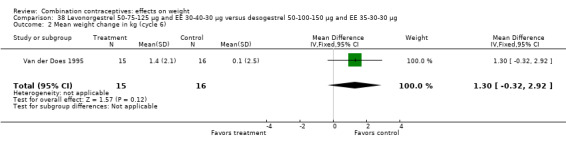
Comparison 38 Levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg versus desogestrel 50‐100‐150 µg and EE 35‐30‐30 µg, Outcome 2 Mean weight change in kg (cycle 6).
48.1. Analysis.
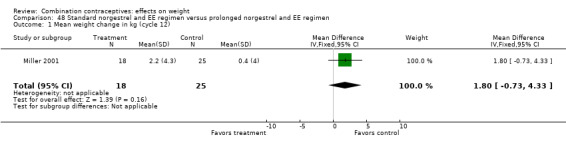
Comparison 48 Standard norgestrel and EE regimen versus prolonged norgestrel and EE regimen, Outcome 1 Mean weight change in kg (cycle 12).
18.1. Analysis.
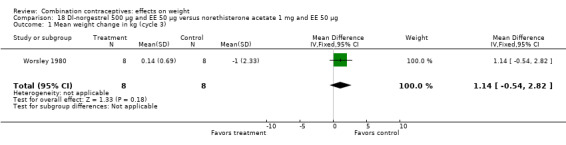
Comparison 18 Dl‐norgestrel 500 µg and EE 50 µg versus norethisterone acetate 1 mg and EE 50 µg, Outcome 1 Mean weight change in kg (cycle 3).
Twenty‐one trial reports provided quantitative data on the primary reasons for early discontinuation. Ten of these trial reports included weight change as a distinct category for early discontinuation from trial participation (Table 1). The proportions of women who discontinued due to weight changes were small (zero to 5%) and did not differ between the study groups. Sang 1995 included the mean weight gain for the women who cited weight gain as the primary or secondary reason for early discontinuation. In the group with injectable medroxyprogesterone acetate 25 mg and estradiol cypionate 5 mg, the 18 women who attributed weight gain to the contraceptive had a mean gain of 2.8 kg compared to 3.1 kg for the 16 women in the group assigned to the injectable norethisterone enanthate 50 mg and estradiol valerate 5 mg (Sang 1995).
1. Discontinuation due to weight change.
| Study ID | Intervention group | n | N (randomized women) |
| Cachrimanidou 1993 | Prolonged desogestrel / ethinyl estradiol (EE) regimen | 10 | 200 |
| Standard desogestrel / EE regimen | 1 | 100 | |
| Coenen 1996 | Norgestimate 250 μg / EE 35 μg | 1 | 25 |
| Gestodene 75 μg / EE 30 μg | 0 | 25 | |
| Desogestrel 150 μg / EE 30 μg | 0 | 25 | |
| Desogestrel 150 μg / EE 20 μg | 0 | 25 | |
| Coney 2001 | Levonorgestrel 100 μg / EE 20 μg | 2 | 359 |
| Placebo | 0 | 362 | |
| Dionne 1974 | Levonorgestrel 250 μg / EE 50 μg | 3 | 73 |
| Levonorgestrel 150 μg / EE 30 μg | 1 | 77 | |
| Halbe 1998 | Gestodene 75 μg / EE 30 μg | 4 | 279 |
| Desogestrel 150 μg / EE 30 μg | 0 | 316 | |
| Kirkman 1994 | Gestodene 75 μg / EE 30 μg | 4 | 505 |
| Desogestrel 150 μg / EE 20 μg | 2 | 501 | |
| Miller 2001 | Standard norgestrel / EE regimen | 0 | 44 |
| Prolonged norgestrel / EE regimen | 1 | 46 | |
| Oddsson 2005 | Vaginal ring etonogestrel 120 µg / EE 15 µg | 2 | 512 |
| Levonorgestrel 150 µg / EE 30 µg | 6 | 518 | |
| Sang 1995 | Injectable medroxyprogesterone acetate 25 mg / estradiol cypionatge (EC) 5 mg | 14 | 1955 |
| Injectable norethisterone enanthate 50 mg / estradiol valerate (EV) 5 mg | 10 | 1960 | |
| Wiik 1993 | Norethisterone 500‐1000 μg / EE 35 μg | 3 | 100 |
| Levonorgestrel 50‐75‐125 μg / EE 30‐40 μg | 1 | 96 |
Discussion
Summary of main results
The four trials that included a placebo group or 'no intervention' group (Coney 2001; Goldzieher 1971; Procter‐Gray 2008; Sibai 2001) did not find evidence supporting the putative association between combination contraceptive use and weight change. The lack of an association in those trials could be due to the limited number of contraceptives evaluated. Goldzieher 1971, conducted more than three decades ago, studied three high‐estrogen dose oral contraceptives. Coney 2001 and Procter‐Gray 2008 evaluated one oral contraceptive each. Sibai 2001 studied one skin patch. Given the numerous combination contraceptive drugs, doses, and regimens, the possibility that one or more combination contraceptives could cause weight change cannot be eliminated with the data from the four placebo‐controlled randomized trials conducted to date.
Of the 79 weight change comparisons evaluating two combination contraceptives, seven showed a difference in the mean weight change or the proportion of women gaining or losing more than a set amount of weight. Even if no association existed between combination contraceptives and weight, one would expect several significant results (Type I errors) since numerous comparisons were made. Regardless of statistical significance, the clinical significance seems negligible. The point estimates for the mean difference in weight between the comparison groups were small. The largest notable difference was 1.80 kg (95% CI ‐0.73 to 4.33) after 12 treatment cycles (Miller 2001). The ORs for the proportions of women who gained or lost more than a set amount were generally either weak or too imprecise to convey much meaning. The CI from Oelkers 1995 was very wide since no one in the levonorgestrel and EE group lost more than the specified 2 kg.
If a mechanism for weight gain were estrogen‐dependent, two contraceptives containing the same progestin and estrogen types but different hormone doses might show more weight gain with the higher‐estrogen contraceptive. In this review, 11 of the 51 comparison pairs included two oral contraceptives with identical progestin and estrogen types but different hormone doses or regimens. Only Miller 2001 detected a possible difference in weight change between the groups, and the higher weight gain was for the group assigned less estrogen. While a dose‐related effect would have supported the hypothesized causal link between estrogen and weight gain, the lack of this finding does not disprove the possible association. The studies could have been underpowered to detect a dose‐gradient response between the estrogen content and weight gain.
Overall completeness and applicability of evidence
Only one trial examined weight change as a primary outcome, so most trials did not use rigorous methods for measuring weight. The reliability of the measurements could be affected by numerous factors, such as the use of calibrated scales, the time of day and cycle when measurements were collected, the use of a fasting state, and the amount of clothing on the participant. The degree of error in measuring weight change is likely to be similar between study groups and to dilute the effect estimate toward the null value of no difference.
The trials also could have failed to detect differences in weight if the rates for early discontinuation or loss to follow up had systematically differed between intervention groups for women who gained or lost weight. Ten trials reported the proportion of women for whom weight change was the primary reason for early discontinuation, and did not find differences by study group. Also, the one trial that reported the mean weight gain for the women who discontinued early for this reason found similar mean weight changes for the two combination injectable groups. The interpretation of the trial results would have been strengthened by including weight change data for women who did not complete the trial.
Quality of the evidence
More than 25% of the trials had high risk of bias due to lack of blinding or incomplete outcome data (Figure 1). The majority of studies had unclear risk of bias due to missing information on randomization sequence generation or allocation concealment. However, most of those trials were published before CONSORT (Moher 2001; CONSORT 2009) (Figure 2).
1.
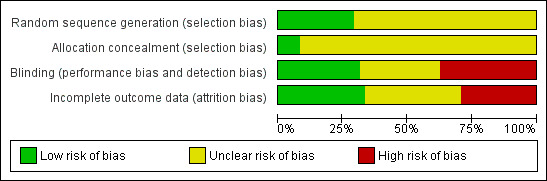
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
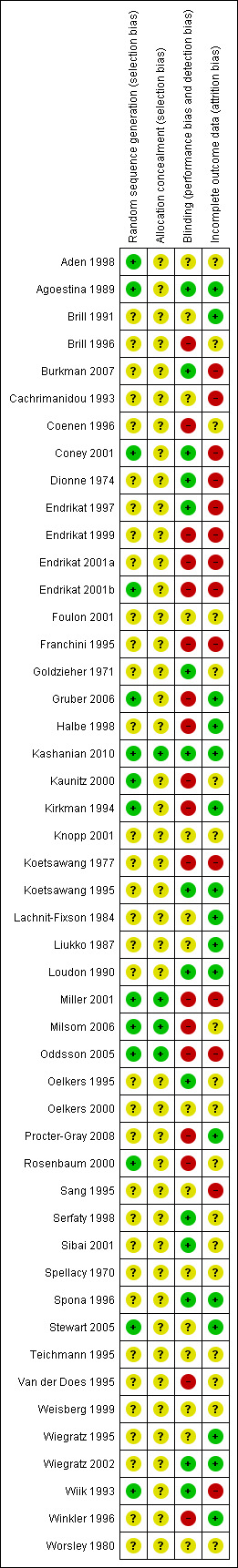
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Authors' conclusions
Implications for practice.
The four trials with a placebo or no intervention group did not find evidence supporting a causal association between combination contraceptives and weight change. Also, most comparisons of different combination contraceptives showed no substantial difference in weight or difference in discontinuation rates due to weight change. Available evidence is insufficient to determine the effect of combination contraceptives on weight, but no large effect is evident. The medical usefulness of weighing women who use combination contraceptives appears to be limited. Appropriate and accurate counseling about typical weight gain over time may help reduce discontinuation of contraceptives due to perceptions of weight gain.
Implications for research.
Randomized controlled trials to evaluate the link between combination contraceptives and weight change require a placebo or non‐hormonal group to control for other factors, including changes in weight over time. In addition, improved reporting of study methods and results would permit the inclusion of more trials and strengthen the interpretation. Trials should also attempt to collect and report weight data for those who discontinue early or are excluded from the trial.
What's new
| Date | Event | Description |
|---|---|---|
| 1 January 2014 | New citation required but conclusions have not changed | Searches updated |
| 18 December 2013 | New search has been performed | No new trials met inclusion criteria. Added one ongoing trial (Mahidol 2013). Added Figure 1 and Figure 2 to summarize risk of bias. |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 2, 2003
| Date | Event | Description |
|---|---|---|
| 31 May 2011 | New search has been performed | MEDLINE search was updated. No additional trials found. |
| 28 February 2011 | New citation required but conclusions have not changed | Two new trials included (Kashanian 2010; Procter‐Gray 2008) |
| 25 February 2011 | New search has been performed | Searches were updated. Searches added for ClinicalTrials.gov and ICTRP. |
| 17 June 2008 | New citation required but conclusions have not changed | Three new trials were added (Gruber 2006; Burkman 2007; Milsom 2006). Several recent trials were excluded. |
| 16 June 2008 | New search has been performed | Searches were updated in May and June 2008. |
| 9 May 2008 | Amended | Converted to new review format. |
| 29 September 2005 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Carol Manion of FHI 360 helped with the literature searches. For the original review, Anne Eisinga of the Cochrane Fertility Regulation Group also provided assistance.
Appendices
Appendix 1. Search 2013
MEDLINE via PubMed (01 Jan 2011 to 01 Jan 2014)
("Contraceptive Agents, Female"[Mesh] OR "Contraceptive Devices, Female"[Mesh] OR contracept*[tiab]) AND ("Body Weight"[Mesh] OR weight[tiab] OR "Body Mass Index"[Mesh]) NOT (cancer*[ti] OR polycystic [ti] OR exercise [ti] OR physical activity[ti] OR postmenopaus*[ti]) Filter Activated: Clinical Trial
CENTRAL (01 Jan 2011 to 11 Nov 2013)
contracept* in Title, Abstract, or Keywords AND (weigh* OR body mass index) in Abstract
POPLINE (01 Jan 2011 to 06 Nov 2013)
All fields: (contraceptive agents OR contraceptive devices) AND weight
Filter by keywords: research report
EMBASE (01 Jan 2011 to 11 Nov 2013)
'weight'/exp OR weight AND contracept* AND ([controlled clinical trial]/lim OR [randomized controlled trial]/lim) AND ([article]/lim OR [article in press]/lim OR [conference abstract]/lim OR [conference paper]/lim OR [erratum]/lim) AND ([obstetrics and gynecology]/lim OR [public health]/lim) AND [humans]/lim AND [embase]/lim AND [2011‐2014]/py
LILACS (01 Jan 2011 to 06 Nov 2013)
(contraceptive agents, female or agentes anticonceptivos femeninos or anticoncepcionais femeninos) AND (weight or weight gain or weight loss or peso or aumento de peso or ganho de peso or peridida de peso or perda de peso)
ClinicalTrials.gov (01 Jan 2011 to 11 Nov 2013)
Intervention: contraceptive OR contraception Outcomes: weight OR body mass index Studies with female participants Study type: interventional
ICTRP (01 Jan 2011 to 07 Nov 2013)
1) contracept* AND weight
2) contracept* AND body mass index
Appendix 2. Previous search
MEDLINE via PubMed (31 May 2011)
("Contraceptive Agents, Female"[Mesh] OR "Contraceptive Devices, Female"[Mesh] OR contracept*[tiab]) AND ("Body Weight"[Mesh] OR weight[tiab] OR "Body Mass Index"[Mesh]) NOT (cancer*[ti] OR polycystic [ti] OR exercise [ti] OR physical activity[ti] OR postmenopaus*[ti]) Limits Activated: Humans, Clinical Trial, Randomized Controlled Trial
POPLINE (24 Jan 2011)
(contraceptive agents / contraceptive devices) & (random* / blind* / placebo* / crossover*) & weight
CENTRAL (22 Feb 2011)
contracept* in Title, Abstract, or Keywords AND (weigh* OR body mass index) in Abstract
EMBASE (22 Feb 2011)
s weight(w)gain and s contracept? OR contraceptive agent? and s3 and pd=20080523:20110222 and s human and s clinical trial
LILACS (25 Feb 2011)
(contraceptive agents, female or agentes anticonceptivos femeninos or anticoncepcionais femeninos) AND (weight or weight gain or weight loss or peso or aumento de peso or ganho de peso or peridida de peso or perda de peso)
ClinicalTrials.gov (24 Jan 2011)
Intervention: contraceptive OR contraception Outcomes: weight OR body mass index Studies with female participants Study type: interventional
ICTRP (09 Feb 2011)
1) contracept* AND weight
2) contracept* AND body mass index
Data and analyses
Comparison 1. Dimethisterone 25 mg and ethinyl estradiol (EE) 100 µg versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2.3 kg (cycle 4) | 1 | 113 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.02 [0.46, 2.26] |
1.1. Analysis.
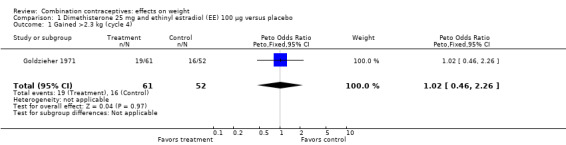
Comparison 1 Dimethisterone 25 mg and ethinyl estradiol (EE) 100 µg versus placebo, Outcome 1 Gained >2.3 kg (cycle 4).
Comparison 2. Ethynodiol diacetate 1 mg and mestranol 100 µg versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2.3 kg (cycle 4) | 1 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.57 [0.24, 1.33] |
2.1. Analysis.
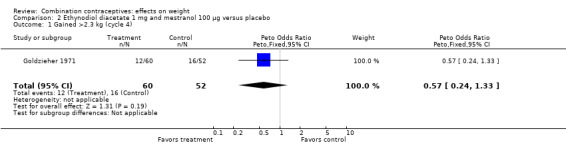
Comparison 2 Ethynodiol diacetate 1 mg and mestranol 100 µg versus placebo, Outcome 1 Gained >2.3 kg (cycle 4).
Comparison 3. Levonorgestrel 100 µg and EE 20 µg versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 6) | 1 | 473 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.23, 0.83] |
3.1. Analysis.
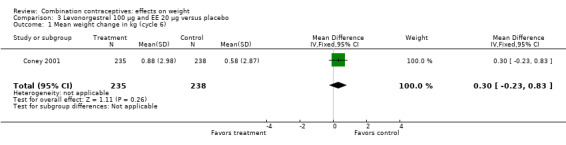
Comparison 3 Levonorgestrel 100 µg and EE 20 µg versus placebo, Outcome 1 Mean weight change in kg (cycle 6).
Comparison 4. Norgestrel 300 µg and EE 30 µg versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg per year | 1 | 150 | Mean Difference (IV, Fixed, 95% CI) | ‐0.54 [‐1.39, 0.31] |
4.1. Analysis.
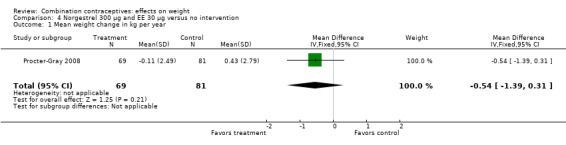
Comparison 4 Norgestrel 300 µg and EE 30 µg versus no intervention, Outcome 1 Mean weight change in kg per year.
Comparison 5. Norethindrone 1 mg and mestranol 50 µg versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2.3 kg (cycle 4) | 1 | 123 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.50 [0.22, 1.17] |
5.1. Analysis.
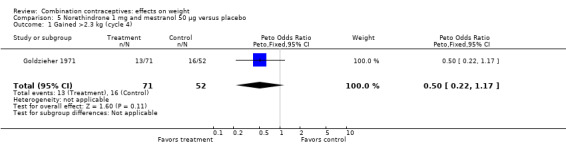
Comparison 5 Norethindrone 1 mg and mestranol 50 µg versus placebo, Outcome 1 Gained >2.3 kg (cycle 4).
Comparison 6. Skin patch norelgestromin 150 µg and EE 20 µg versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >5% baseline weight (cycle 9) | 1 | 136 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.95 [0.30, 2.98] |
| 2 Lost >5% baseline weight (cycle 9) | 1 | 136 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.27 [0.04, 1.82] |
6.1. Analysis.
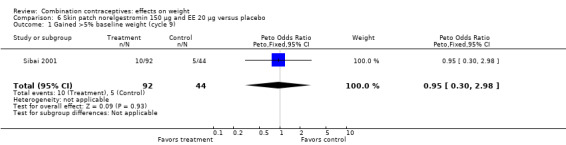
Comparison 6 Skin patch norelgestromin 150 µg and EE 20 µg versus placebo, Outcome 1 Gained >5% baseline weight (cycle 9).
6.2. Analysis.
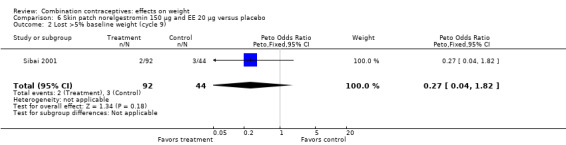
Comparison 6 Skin patch norelgestromin 150 µg and EE 20 µg versus placebo, Outcome 2 Lost >5% baseline weight (cycle 9).
Comparison 7. Skin patch norelgestromin 150 µg and EE 20 µg: extended versus cyclic regimen.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change (112 days or cycle 4) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.79, 0.55] |
7.1. Analysis.
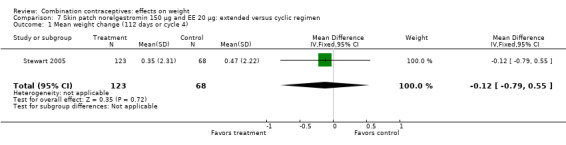
Comparison 7 Skin patch norelgestromin 150 µg and EE 20 µg: extended versus cyclic regimen, Outcome 1 Mean weight change (112 days or cycle 4).
Comparison 8. Desogestrel 150 µg and EE 20 µg versus desogestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean body mass percentage change (cycle 6) | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐1.54, 1.74] |
8.1. Analysis.
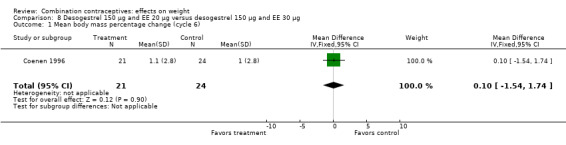
Comparison 8 Desogestrel 150 µg and EE 20 µg versus desogestrel 150 µg and EE 30 µg, Outcome 1 Mean body mass percentage change (cycle 6).
Comparison 9. Desogestrel 150 µg and EE 20 µg versus gestodene 75 µg and EE 20 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 801 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.84 [0.58, 1.22] |
| 2 Lost >2 kg (cycle 6) | 1 | 801 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.65 [1.13, 2.41] |
| 3 Gained >2 kg (cycle 12) | 1 | 1476 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.13 [0.85, 1.49] |
| 4 Lost >2 kg (cycle 12) | 1 | 1476 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.95 [0.68, 1.33] |
9.1. Analysis.
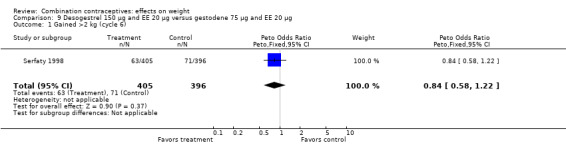
Comparison 9 Desogestrel 150 µg and EE 20 µg versus gestodene 75 µg and EE 20 µg, Outcome 1 Gained >2 kg (cycle 6).
9.3. Analysis.
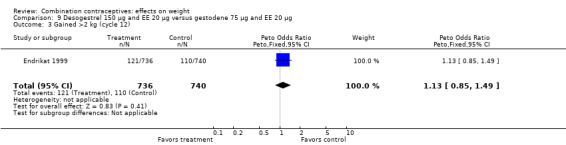
Comparison 9 Desogestrel 150 µg and EE 20 µg versus gestodene 75 µg and EE 20 µg, Outcome 3 Gained >2 kg (cycle 12).
9.4. Analysis.
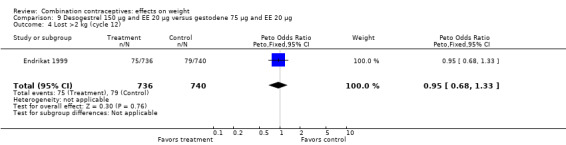
Comparison 9 Desogestrel 150 µg and EE 20 µg versus gestodene 75 µg and EE 20 µg, Outcome 4 Lost >2 kg (cycle 12).
Comparison 10. Desogestrel 150 µg and EE 20 µg versus norgestimate 250 µg and EE 35 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean body mass percentage change (cycle 6) | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐1.45, 2.65] |
10.1. Analysis.
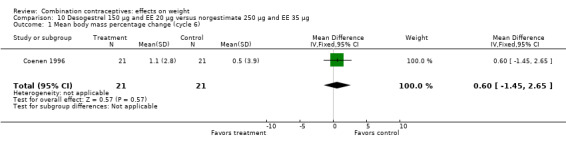
Comparison 10 Desogestrel 150 µg and EE 20 µg versus norgestimate 250 µg and EE 35 µg, Outcome 1 Mean body mass percentage change (cycle 6).
Comparison 11. Desogestrel 150 µg and EE 30 µg versus levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 469 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 3.29 [1.84, 5.88] |
Comparison 12. Standard desogestrel and EE regimen versus prolonged gestodene and EE regimen.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 7) | 1 | 890 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.20 [0.86, 1.68] |
12.1. Analysis.
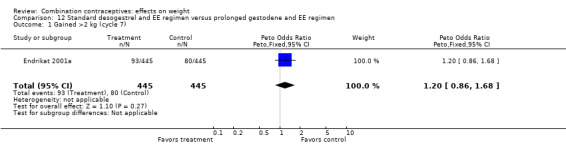
Comparison 12 Standard desogestrel and EE regimen versus prolonged gestodene and EE regimen, Outcome 1 Gained >2 kg (cycle 7).
Comparison 13. Prolonged desogestrel and EE regimen versus standard desogestrel and EE regimen.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 12) | 1 | 196 | Mean Difference (IV, Fixed, 95% CI) | 0.57 [‐0.42, 1.56] |
13.1. Analysis.
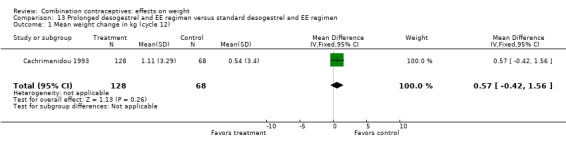
Comparison 13 Prolonged desogestrel and EE regimen versus standard desogestrel and EE regimen, Outcome 1 Mean weight change in kg (cycle 12).
Comparison 14. Dienogest 2 mg, EE 10 µg and estradiol valerate 2 mg versus levonorgestrel 100 µg and EE 20 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >5% baseline weight (cycle 3) | 1 | 49 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.20 [0.32, 4.51] |
| 2 Lost >5% baseline weight (cycle 3) | 1 | 49 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.10 [0.14, 358.08] |
14.1. Analysis.
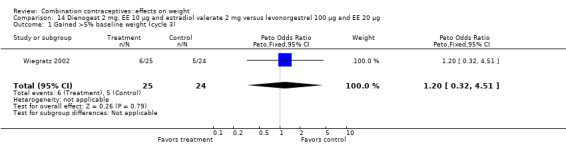
Comparison 14 Dienogest 2 mg, EE 10 µg and estradiol valerate 2 mg versus levonorgestrel 100 µg and EE 20 µg, Outcome 1 Gained >5% baseline weight (cycle 3).
14.2. Analysis.
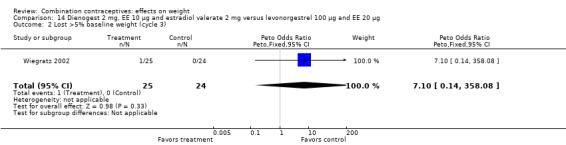
Comparison 14 Dienogest 2 mg, EE 10 µg and estradiol valerate 2 mg versus levonorgestrel 100 µg and EE 20 µg, Outcome 2 Lost >5% baseline weight (cycle 3).
Comparison 15. Dienogest 2 mg and EE 20 µg versus levonorgestrel 100 µg and EE 20 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >5% baseline weight (cycle 3) | 1 | 49 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.95 [0.24, 3.76] |
| 2 Lost >5% baseline weight (cycle 3) | 1 | 49 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.40 [0.45, 121.93] |
15.1. Analysis.
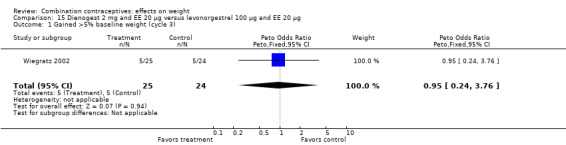
Comparison 15 Dienogest 2 mg and EE 20 µg versus levonorgestrel 100 µg and EE 20 µg, Outcome 1 Gained >5% baseline weight (cycle 3).
15.2. Analysis.
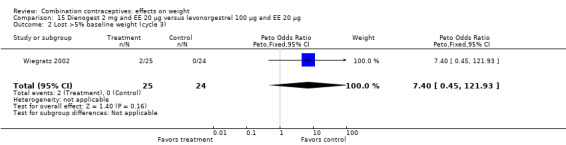
Comparison 15 Dienogest 2 mg and EE 20 µg versus levonorgestrel 100 µg and EE 20 µg, Outcome 2 Lost >5% baseline weight (cycle 3).
Comparison 16. Dienogest 2 mg and EE 30 µg versus levonorgestrel 100 µg and EE 20 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >5% baseline weight (cycle 3) | 1 | 48 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.77 [0.18, 3.21] |
| 2 Lost >5% baseline weight (cycle 3) | 1 | 48 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.39 [0.15, 372.38] |
16.1. Analysis.
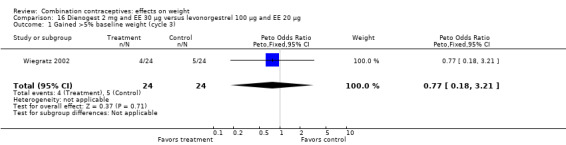
Comparison 16 Dienogest 2 mg and EE 30 µg versus levonorgestrel 100 µg and EE 20 µg, Outcome 1 Gained >5% baseline weight (cycle 3).
16.2. Analysis.
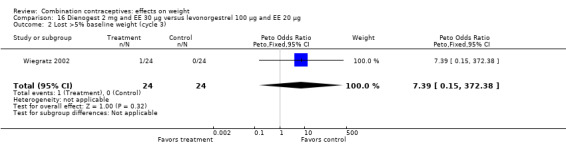
Comparison 16 Dienogest 2 mg and EE 30 µg versus levonorgestrel 100 µg and EE 20 µg, Outcome 2 Lost >5% baseline weight (cycle 3).
Comparison 17. Dl‐norgestrel 500 µg and EE 50 µg versus levonorgestrel 250 µg and EE 50 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 3) | 1 | 21 | Mean Difference (IV, Fixed, 95% CI) | 0.22 [‐1.30, 1.74] |
17.1. Analysis.
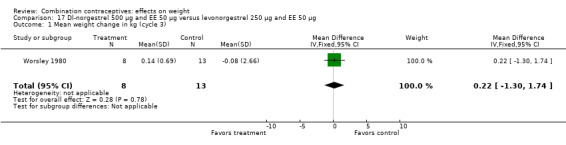
Comparison 17 Dl‐norgestrel 500 µg and EE 50 µg versus levonorgestrel 250 µg and EE 50 µg, Outcome 1 Mean weight change in kg (cycle 3).
Comparison 18. Dl‐norgestrel 500 µg and EE 50 µg versus norethisterone acetate 1 mg and EE 50 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 3) | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | 1.14 [‐0.54, 2.82] |
Comparison 19. Drospirenone 2 mg and EE 30 µg versus drospirenone 3 mg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
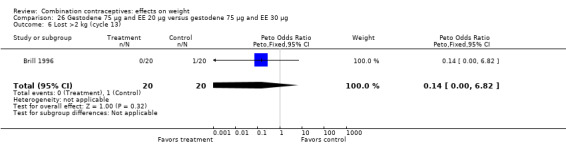
| 1 Gained >2 kg (cycle 3) | 2 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.14 [0.00, 6.82] |
| 2 Lost >2 kg (cycle 3) | 1 | 66 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.99 [0.20, 19.82] |
19.1. Analysis.
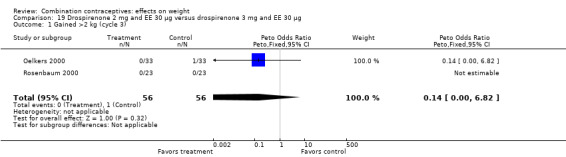
Comparison 19 Drospirenone 2 mg and EE 30 µg versus drospirenone 3 mg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 3).
19.2. Analysis.
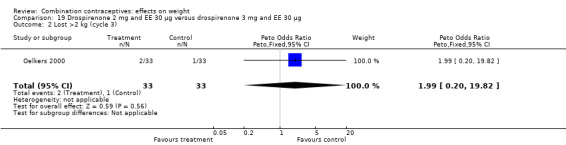
Comparison 19 Drospirenone 2 mg and EE 30 µg versus drospirenone 3 mg and EE 30 µg, Outcome 2 Lost >2 kg (cycle 3).
Comparison 20. Drospirenone 3 mg and EE 15 µg versus levonorgestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.50 [0.05, 5.06] |
| 2 Lost >2 kg (cycle 6) | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 9.92 [1.79, 55.04] |
20.1. Analysis.
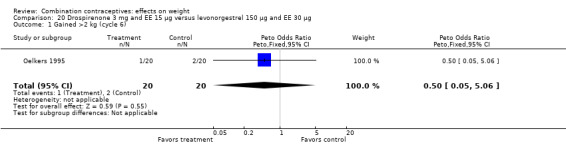
Comparison 20 Drospirenone 3 mg and EE 15 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 6).
Comparison 21. Drospirenone 3 mg and EE 20 µg versus levonorgestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.01, 2.13] |
| 2 Lost >2 kg (cycle 6) | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.39 [0.15, 372.38] |
21.1. Analysis.
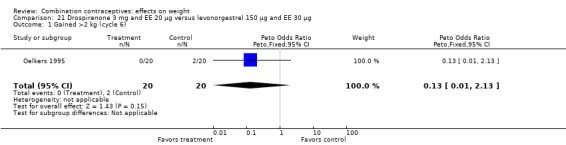
Comparison 21 Drospirenone 3 mg and EE 20 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 6).
21.2. Analysis.
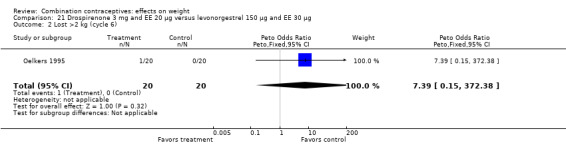
Comparison 21 Drospirenone 3 mg and EE 20 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 2 Lost >2 kg (cycle 6).
Comparison 22. Drospirenone 3 mg and EE 30 µg versus desogestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 13) | 1 | 56 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.86 [0.29, 2.56] |
| 2 Lost >2 kg (cycle 13) | 1 | 56 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.38 [0.29, 6.62] |
22.1. Analysis.
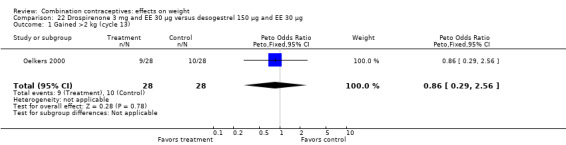
Comparison 22 Drospirenone 3 mg and EE 30 µg versus desogestrel 150 µg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 13).
22.2. Analysis.
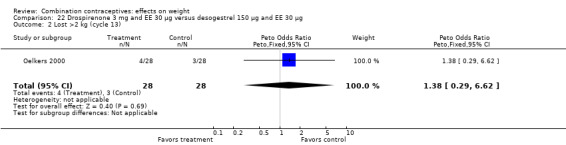
Comparison 22 Drospirenone 3 mg and EE 30 µg versus desogestrel 150 µg and EE 30 µg, Outcome 2 Lost >2 kg (cycle 13).
Comparison 23. Drospirenone 3 mg and EE 20 μg versus desogestrel 150 μg and EE 20 μg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 7) | 1 | 441 | Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.16, ‐0.18] |
Comparison 24. Drospirenone 3 mg and EE 30 µg versus levonorgestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.01, 2.13] |
| 2 Lost >2 kg (cycle 6) | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.39 [0.15, 372.38] |
24.1. Analysis.
Comparison 24 Drospirenone 3 mg and EE 30 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 6).
24.2. Analysis.
Comparison 24 Drospirenone 3 mg and EE 30 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 2 Lost >2 kg (cycle 6).
Comparison 25. Ethynodiol diacetate 1 mg and mestranol 100 µg versus chlormadinone acetate 1.5 mg and mestranol 100 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 6) | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐1.43, 2.03] |
25.1. Analysis.
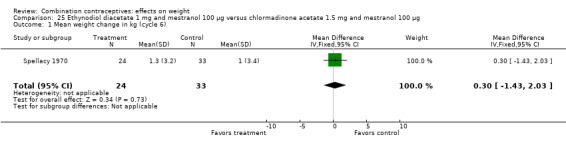
Comparison 25 Ethynodiol diacetate 1 mg and mestranol 100 µg versus chlormadinone acetate 1.5 mg and mestranol 100 µg, Outcome 1 Mean weight change in kg (cycle 6).
Comparison 26. Gestodene 75 µg and EE 20 µg versus gestodene 75 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 39 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.05 [0.06, 17.51] |
| 2 Lost >2 kg (cycle 6) | 1 | 39 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.79 [0.15, 393.02] |
| 3 Gained >2 kg (cycle 12) | 1 | 452 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.06 [0.63, 1.81] |
| 4 Lost >2 kg (cycle 12) | 1 | 452 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.13 [0.63, 2.03] |
| 5 Gained >2 kg (cycle 13) | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.71 [0.14, 3.57] |
| 6 Lost >2 kg (cycle 13) | 1 | 40 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.14 [0.00, 6.82] |
26.1. Analysis.
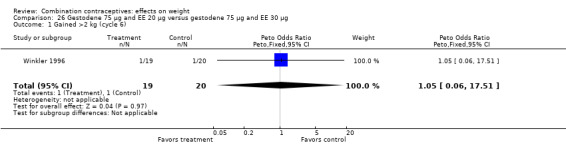
Comparison 26 Gestodene 75 µg and EE 20 µg versus gestodene 75 µg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 6).
26.2. Analysis.
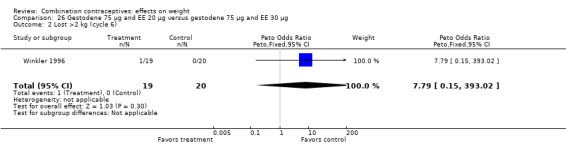
Comparison 26 Gestodene 75 µg and EE 20 µg versus gestodene 75 µg and EE 30 µg, Outcome 2 Lost >2 kg (cycle 6).
26.3. Analysis.
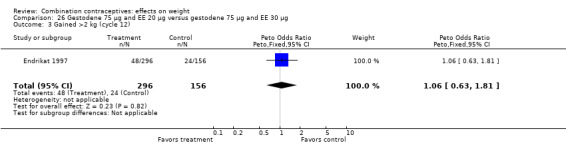
Comparison 26 Gestodene 75 µg and EE 20 µg versus gestodene 75 µg and EE 30 µg, Outcome 3 Gained >2 kg (cycle 12).
26.4. Analysis.
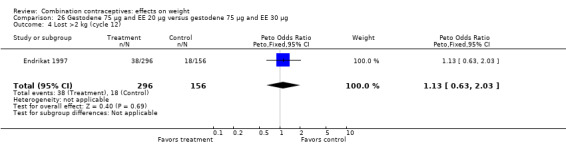
Comparison 26 Gestodene 75 µg and EE 20 µg versus gestodene 75 µg and EE 30 µg, Outcome 4 Lost >2 kg (cycle 12).
26.5. Analysis.
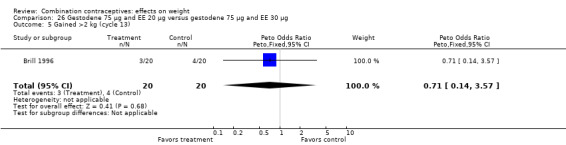
Comparison 26 Gestodene 75 µg and EE 20 µg versus gestodene 75 µg and EE 30 µg, Outcome 5 Gained >2 kg (cycle 13).
26.6. Analysis.
Comparison 26 Gestodene 75 µg and EE 20 µg versus gestodene 75 µg and EE 30 µg, Outcome 6 Lost >2 kg (cycle 13).
Comparison 27. Gestodene 75 µg and EE 30 µg versus desogestrel 150 µg and EE 20 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean body mass percentage change (cycle 6) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 0.7 [‐1.32, 2.72] |
| 2 Mean weight change in kg (cycle 6) | 1 | 805 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [0.00, 0.40] |
| 3 Mean weight change in kg (cycle 12) | 2 | 462 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.50, 0.51] |
27.1. Analysis.
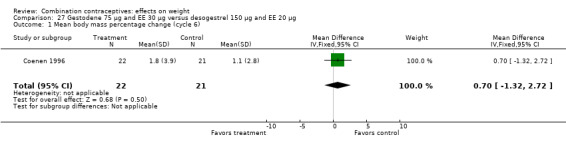
Comparison 27 Gestodene 75 µg and EE 30 µg versus desogestrel 150 µg and EE 20 µg, Outcome 1 Mean body mass percentage change (cycle 6).
27.2. Analysis.
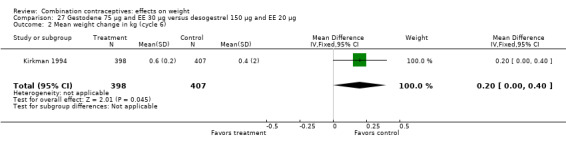
Comparison 27 Gestodene 75 µg and EE 30 µg versus desogestrel 150 µg and EE 20 µg, Outcome 2 Mean weight change in kg (cycle 6).
27.3. Analysis.
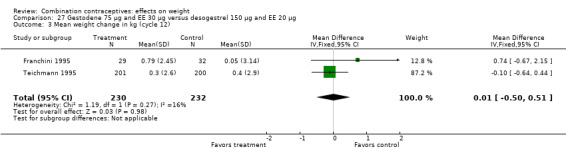
Comparison 27 Gestodene 75 µg and EE 30 µg versus desogestrel 150 µg and EE 20 µg, Outcome 3 Mean weight change in kg (cycle 12).
Comparison 28. Gestodene 75 µg and EE 30 µg versus desogestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 3 | 1524 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.18 [0.87, 1.60] |
| 2 Lost >2 kg ( cycle 6) | 2 | 1172 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.34 [0.90, 2.00] |
| 3 Mean body mass percentage change (cycle 6) | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 0.8 [‐1.18, 2.78] |
28.1. Analysis.
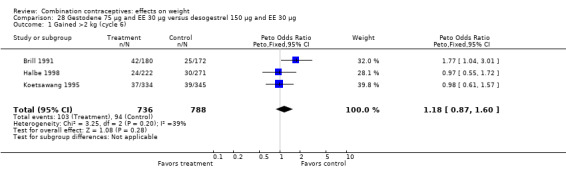
Comparison 28 Gestodene 75 µg and EE 30 µg versus desogestrel 150 µg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 6).
28.2. Analysis.
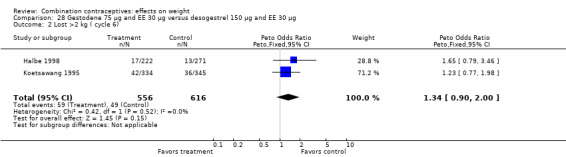
Comparison 28 Gestodene 75 µg and EE 30 µg versus desogestrel 150 µg and EE 30 µg, Outcome 2 Lost >2 kg ( cycle 6).
28.3. Analysis.
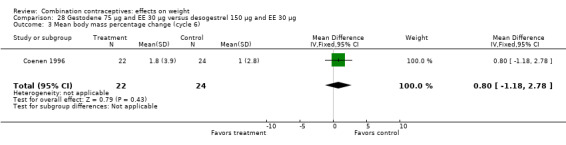
Comparison 28 Gestodene 75 µg and EE 30 µg versus desogestrel 150 µg and EE 30 µg, Outcome 3 Mean body mass percentage change (cycle 6).
Comparison 29. Gestodene 75 µg and EE 30 µg versus norgestimate 250 µg and EE 35 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 357 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.54 [0.92, 2.60] |
| 2 Mean body mass percentage change (cycle 6) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 1.3 [‐1.03, 3.63] |
29.2. Analysis.
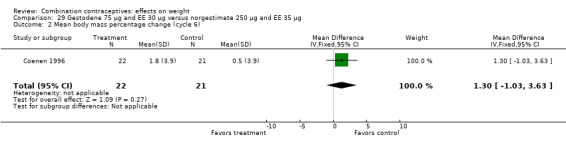
Comparison 29 Gestodene 75 µg and EE 30 µg versus norgestimate 250 µg and EE 35 µg, Outcome 2 Mean body mass percentage change (cycle 6).
Comparison 30. Gestodene 50‐70‐100 µg and EE 30‐40‐30 µg versus desogestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 12) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 1.25 [‐1.22, 3.72] |
30.1. Analysis.
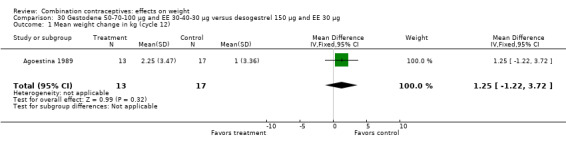
Comparison 30 Gestodene 50‐70‐100 µg and EE 30‐40‐30 µg versus desogestrel 150 µg and EE 30 µg, Outcome 1 Mean weight change in kg (cycle 12).
Comparison 31. Gestodene 50‐70‐100 µg and EE 30‐40‐30 µg versus norgestimate 250 µg and EE 35 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 12) | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐1.09, 0.59] |
31.1. Analysis.
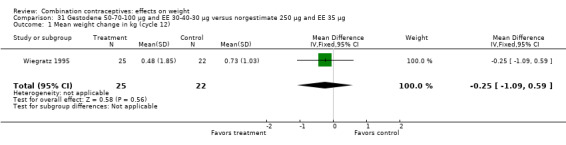
Comparison 31 Gestodene 50‐70‐100 µg and EE 30‐40‐30 µg versus norgestimate 250 µg and EE 35 µg, Outcome 1 Mean weight change in kg (cycle 12).
Comparison 32. Prolonged gestodene and EE regimen versus standard gestodene and EE regimen.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 3) | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐1.23, 1.23] |
32.1. Analysis.
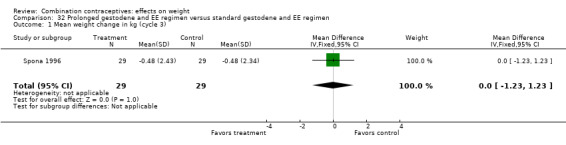
Comparison 32 Prolonged gestodene and EE regimen versus standard gestodene and EE regimen, Outcome 1 Mean weight change in kg (cycle 3).
Comparison 33. Levonorgestrel 100 µg and EE 20 µg versus levonorgestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 418 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.26 [0.74, 2.15] |
| 2 Lost >2 kg (cycle 6) | 1 | 418 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.31 [0.70, 2.44] |
33.1. Analysis.
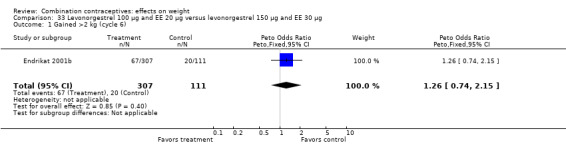
Comparison 33 Levonorgestrel 100 µg and EE 20 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 6).
33.2. Analysis.
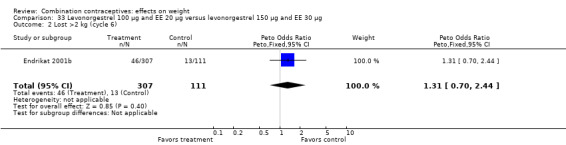
Comparison 33 Levonorgestrel 100 µg and EE 20 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 2 Lost >2 kg (cycle 6).
Comparison 34. Levonorgestrel 150 µg and EE 30 µg versus desogestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2.5 kg (cycle 24) | 1 | 17 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 8.66 [0.77, 97.74] |
| 2 Lost >2.5 kg (cycle 24) | 1 | 17 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.88 [0.17, 21.18] |
34.1. Analysis.
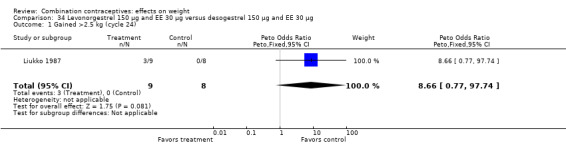
Comparison 34 Levonorgestrel 150 µg and EE 30 µg versus desogestrel 150 µg and EE 30 µg, Outcome 1 Gained >2.5 kg (cycle 24).
34.2. Analysis.
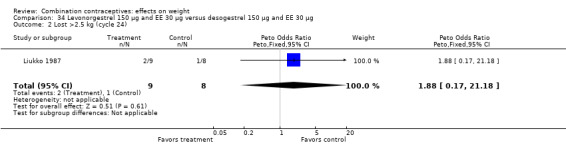
Comparison 34 Levonorgestrel 150 µg and EE 30 µg versus desogestrel 150 µg and EE 30 µg, Outcome 2 Lost >2.5 kg (cycle 24).
Comparison 35. Levonorgestrel 150 µg and EE 30 µg versus gestodene 75 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 6) | 1 | 369 | Mean Difference (IV, Fixed, 95% CI) | 0.7 [0.14, 1.26] |
Comparison 36. Levonorgestrel 250 µg and EE 50 µg versus levonorgestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2.7 kg (cycle 6) | 1 | 109 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.92 [0.74, 4.96] |
36.1. Analysis.
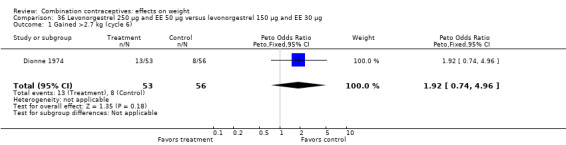
Comparison 36 Levonorgestrel 250 µg and EE 50 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 1 Gained >2.7 kg (cycle 6).
Comparison 37. Levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg versus levonorgestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 6) | 1 | 314 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.06, 0.03] |
37.1. Analysis.
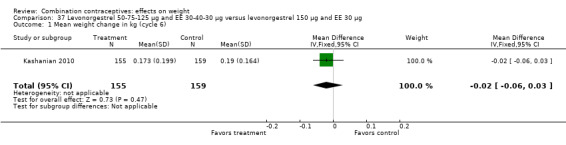
Comparison 37 Levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 1 Mean weight change in kg (cycle 6).
Comparison 38. Levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg versus desogestrel 50‐100‐150 µg and EE 35‐30‐30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean BMI change (cycle 6) | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.35 [‐0.13, 0.83] |
| 2 Mean weight change in kg (cycle 6) | 1 | 31 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [‐0.32, 2.92] |
38.1. Analysis.
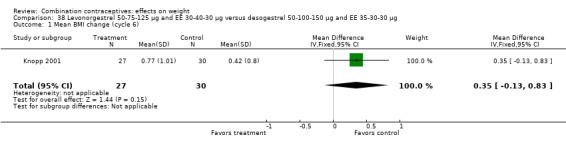
Comparison 38 Levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg versus desogestrel 50‐100‐150 µg and EE 35‐30‐30 µg, Outcome 1 Mean BMI change (cycle 6).
Comparison 39. Levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg versus desogestrel 150 µg and EE 20 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 3) | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 0.78 [‐0.28, 1.84] |
39.1. Analysis.
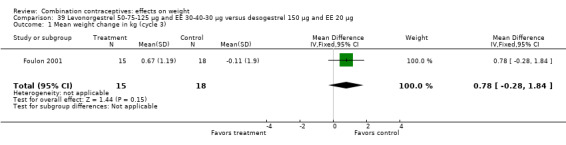
Comparison 39 Levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg versus desogestrel 150 µg and EE 20 µg, Outcome 1 Mean weight change in kg (cycle 3).
Comparison 40. Levonorgestrel 250 µg and EE 50 µg versus norethisterone acetate 1 mg and EE 50 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 3) | 1 | 21 | Mean Difference (IV, Fixed, 95% CI) | 0.92 [‐1.25, 3.09] |
40.1. Analysis.
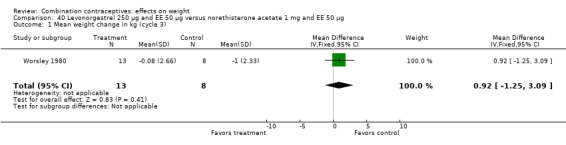
Comparison 40 Levonorgestrel 250 µg and EE 50 µg versus norethisterone acetate 1 mg and EE 50 µg, Outcome 1 Mean weight change in kg (cycle 3).
Comparison 41. Levonorgestrel and EE 6‐6‐9 day regimen versus levonorgestrel 6‐5‐10 day regimen.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 3) | 1 | 28 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐1.15, 1.33] |
41.1. Analysis.
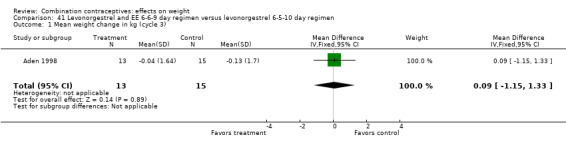
Comparison 41 Levonorgestrel and EE 6‐6‐9 day regimen versus levonorgestrel 6‐5‐10 day regimen, Outcome 1 Mean weight change in kg (cycle 3).
Comparison 42. Lynestrenol 2 mg and EE 40 µg versus lynestrenol 1 mg and EE 40 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2.5 kg (cycle 12) | 1 | 228 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.75 [0.98, 3.11] |
| 2 Lost >2.5 kg (cycle 12) | 1 | 228 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.66 [0.25, 1.77] |
42.2. Analysis.
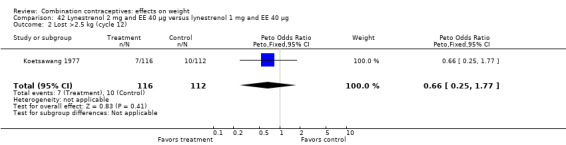
Comparison 42 Lynestrenol 2 mg and EE 40 µg versus lynestrenol 1 mg and EE 40 µg, Outcome 2 Lost >2.5 kg (cycle 12).
Comparison 43. Norethisterone 500‐1000 µg and EE 35 µg versus levonorgestrel 50‐75‐125 µg and EE 30‐40 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 6) | 1 | 144 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.70, 0.90] |
43.1. Analysis.
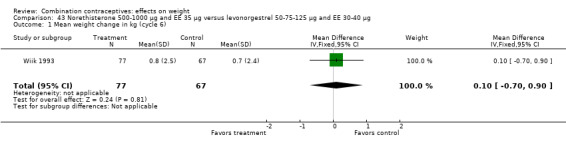
Comparison 43 Norethisterone 500‐1000 µg and EE 35 µg versus levonorgestrel 50‐75‐125 µg and EE 30‐40 µg, Outcome 1 Mean weight change in kg (cycle 6).
Comparison 44. Norgestimate 250 µg and EE 35 µg versus desogestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 349 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.15 [0.65, 2.06] |
| 2 Mean body mass percentage change (cycle 6) | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | ‐0.5 [‐2.51, 1.51] |
44.1. Analysis.
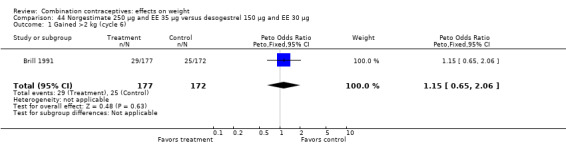
Comparison 44 Norgestimate 250 µg and EE 35 µg versus desogestrel 150 µg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 6).
44.2. Analysis.
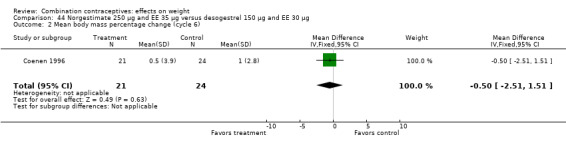
Comparison 44 Norgestimate 250 µg and EE 35 µg versus desogestrel 150 µg and EE 30 µg, Outcome 2 Mean body mass percentage change (cycle 6).
Comparison 45. Norethisterone 500 µg and EE 20 µg versus levonorgestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gained >2 kg (cycle 6) | 1 | 292 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.09 [0.60, 1.99] |
| 2 Lost >2 kg (cycle 6) | 1 | 292 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.69 [0.89, 3.20] |
45.1. Analysis.
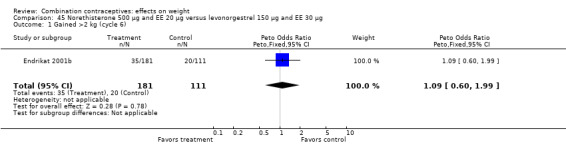
Comparison 45 Norethisterone 500 µg and EE 20 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 1 Gained >2 kg (cycle 6).
Comparison 46. Norethindrone 500‐750‐1000 µg and EE 35 µg versus desogestrel 100‐125‐150 µg and EE 25 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 6) | 1 | 5328 | Mean Difference (IV, Fixed, 95% CI) | 0.26 [0.12, 0.40] |
Comparison 47. Norgestimate 180‐215‐250 µg and EE 25 µg versus norethindrone acetate 1 mg and EE 20 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight gain >=5% (cycle 6) | 1 | 2157 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.15 [0.91, 1.45] |
| 2 Weight gain >=5% (cycle 13) | 1 | 453 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.09 [0.69, 1.74] |
| 3 Weight loss >=5% (cycle 6) | 1 | 2157 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.99 [0.72, 1.37] |
| 4 Weight loss >=5% (cycle 13) | 1 | 453 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.32 [0.74, 2.34] |
47.1. Analysis.
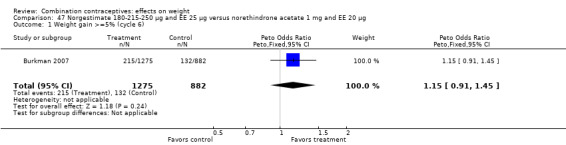
Comparison 47 Norgestimate 180‐215‐250 µg and EE 25 µg versus norethindrone acetate 1 mg and EE 20 µg, Outcome 1 Weight gain >=5% (cycle 6).
47.2. Analysis.
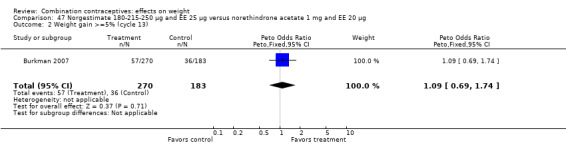
Comparison 47 Norgestimate 180‐215‐250 µg and EE 25 µg versus norethindrone acetate 1 mg and EE 20 µg, Outcome 2 Weight gain >=5% (cycle 13).
47.3. Analysis.
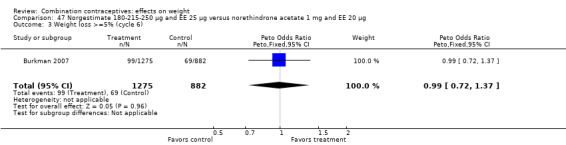
Comparison 47 Norgestimate 180‐215‐250 µg and EE 25 µg versus norethindrone acetate 1 mg and EE 20 µg, Outcome 3 Weight loss >=5% (cycle 6).
47.4. Analysis.
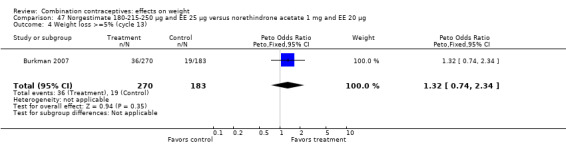
Comparison 47 Norgestimate 180‐215‐250 µg and EE 25 µg versus norethindrone acetate 1 mg and EE 20 µg, Outcome 4 Weight loss >=5% (cycle 13).
Comparison 48. Standard norgestrel and EE regimen versus prolonged norgestrel and EE regimen.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 12) | 1 | 43 | Mean Difference (IV, Fixed, 95% CI) | 1.8 [‐0.73, 4.33] |
Comparison 49. Injectable medroxyprogesterone acetate 25 mg and EC 5 mg versus norethisterone enanthate 50 mg and EV 5 mg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 12) | 1 | 3029 | Mean Difference (IV, Fixed, 95% CI) | 0.13 [‐0.04, 0.30] |
49.1. Analysis.
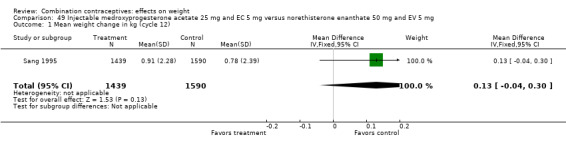
Comparison 49 Injectable medroxyprogesterone acetate 25 mg and EC 5 mg versus norethisterone enanthate 50 mg and EV 5 mg, Outcome 1 Mean weight change in kg (cycle 12).
Comparison 50. Vaginal ring with norethindrone acetate 1 mg and EE 15 µg versus norethindrone acetate 1 mg and EE 20 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gain >2 kg (cycle 4) | 1 | 51 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.69 [0.13, 3.58] |
| 2 Lost >2 kg (cycle 4) | 1 | 51 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.69 [0.35, 8.07] |
50.1. Analysis.
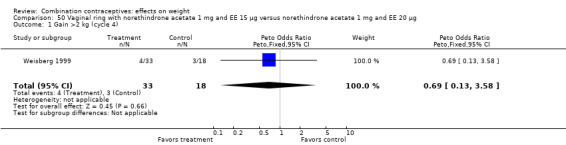
Comparison 50 Vaginal ring with norethindrone acetate 1 mg and EE 15 µg versus norethindrone acetate 1 mg and EE 20 µg, Outcome 1 Gain >2 kg (cycle 4).
50.2. Analysis.
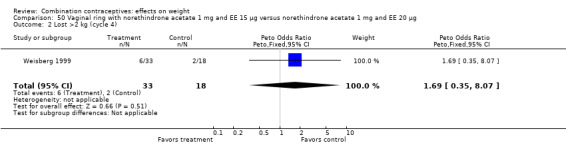
Comparison 50 Vaginal ring with norethindrone acetate 1 mg and EE 15 µg versus norethindrone acetate 1 mg and EE 20 µg, Outcome 2 Lost >2 kg (cycle 4).
Comparison 51. Vaginal ring etonogestrel 120 µg and EE 15 µg versus levonorgestrel 150 µg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gain >=7% body weight (cycle 13) | 1 | 1030 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.84 [0.55, 1.28] |
| 2 Lost >=7% body weight (cycle 13) | 1 | 1030 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.39 [0.83, 2.32] |
51.1. Analysis.
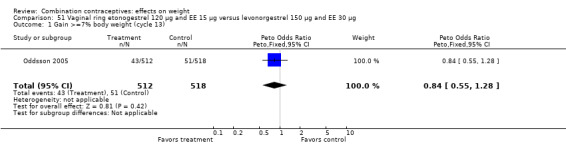
Comparison 51 Vaginal ring etonogestrel 120 µg and EE 15 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 1 Gain >=7% body weight (cycle 13).
51.2. Analysis.
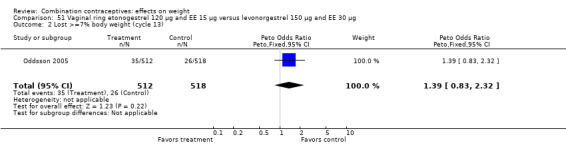
Comparison 51 Vaginal ring etonogestrel 120 µg and EE 15 µg versus levonorgestrel 150 µg and EE 30 µg, Outcome 2 Lost >=7% body weight (cycle 13).
Comparison 52. Vaginal ring etonogestrel 120 µg and EE 15 µg versus drospirenone 3 mg and EE 30 µg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean weight change in kg (cycle 13 or last assessment) | 1 | 937 | Mean Difference (IV, Fixed, 95% CI) | 0.4 [0.03, 0.77] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aden 1998.
| Methods | Study location not described. Cross‐over trial but weight data available from first treatment period only. Two pre‐treatment 'washout' cycles and three treatment cycles. | |
| Participants | Healthy women age 21 to 32 years with regular menses. Excluded recent hormonal contraceptive use; recent use of certain drugs. | |
| Interventions | Levonorgestrel 50‐75‐150 µg and EE 30‐40‐30 µg versus levonorgestrel 50‐75‐150 µg and EE 30‐40‐30 µg. 29 women randomized; initial number assigned to each study group not reported. | |
| Outcomes | Adverse events, hormonal measurements. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Three women discontinued early. Primary reasons for discontinuation described and did not include weight gain. Loss to follow up not reported. |
Agoestina 1989.
| Methods | One site in Indonesia. 12 treatment cycles. | |
| Participants | Inclusion and exclusion criteria not described. | |
| Interventions | Gestodene 50‐70‐100 µg and EE 30‐40‐30 µg (N=13) versus desogestrel 150 µg and EE 30 µg (N=17). | |
| Outcomes | Lipoprotein, liver function, blood coagulation, adverse events, body weight, blood pressure. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Double‐blinded" but did not report who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Three women discontinued early or were lost to follow up. Primary reasons for discontinuation not described. |
Brill 1991.
| Methods | Multicenter trial in Germany. Six treatment cycles. | |
| Participants | Healthy, sexually‐active women age 16 to 45 years with regular menses. Excluded contraindications to oral contraceptive use; recent oral contraceptive use; certain drug use; abnormal Pap smear. | |
| Interventions | Gestodene 75 µg and EE 30 µg (N=209) versus desogestrel 150 µg and EE 30 µg (N=201) versus norgestimate 250 µg and EE 35 µg (N=195). | |
| Outcomes | Contraceptive efficacy, cycle control, body weight, blood pressure, adverse events. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 29 women in the gestodene, 29 women in the desogestrel and 18 women in the norgestimate group discontinued early or were lost to follow up. Primary reasons for discontinuation described and did not include weight gain. |
Brill 1996.
| Methods | One site. Three pill‐free pretreatment cycles and 13 treatment cycles. | |
| Participants | Women age 18 to 35 years with regular menses. Excluded smokers over age 30 years; pregnancy; liver disease; vascular disease; tumors; certain other diseases; obesity; heavy alcohol use; other hormone preparations or intrauterine device use. | |
| Interventions | Gestodene 75 µg and EE 20 µg (N=32) versus gestodene 75 µg and EE 30 µg (N=32). | |
| Outcomes | Lipid levels, hormone levels, efficacy, cycle control, safety. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 woman in EE 20 µg and 5 in EE 30 µg group withdrew before starting treatment. 4 in EE 20 µg and 1 in EE 30 µg group discontinued early due to adverse events. Primary reasons for discontinuation not described. 3 women in EE 20 µg group were excluded for protocol violations. Lost to follow up not reported. |
Burkman 2007.
| Methods | 100 sites in USA and 10 in Canada. First 1/3 of participants were to have 13 treatment cycles and the remaining 2/3 were to have 6 treatment cycles. | |
| Participants | Sexually active, healthy women aged 18 to 45 years at risk for pregnancy with regular menstrual cycles, blood pressure <140/90. Excluded recent pregnancy or lactation; contraindications to OCs; certain diseases; smokers aged 35 or more years; certain drugs or devices; recent DMPA use; and recent alcohol or substance abuse. | |
| Interventions | Norethindrone acetate (NETA) 1.0 mg plus EE 20 µg, with 75 mg ferrous fumarate on days 22‐28 (N=853 for 6 cycles, 318 for 13 cycles) versus norgestimate (NGM) 180‐215‐250 µg plus EE 25 µg (N=1236 for 6 cycles, 487 for 13 cycles). | |
| Outcomes | Weight change was primary outcome; contraceptive efficacy, cycle control, and safety were in earlier report (Hampton 2001). 'Breakthrough' bleeding or spotting defined as bleeding or spotting that occurred during the active pill days unless it was contiguous with menses. 'Amenorrhea' defined as two consecutive cycles without any bleeding or spotting. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Allocated with block sizes of 11 |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinded (participants and at least the assessors at cycle 3). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Lost to follow up reportedly 6.5% in NGM/EE group and 5.8% in NETA/EE group. Noncompleters were 21% of 6‐cycle groups; 42% to 40% of 13‐cycle groups, respectively. |
Cachrimanidou 1993.
| Methods | Three sites in Sweden. 12 treatment cycles. | |
| Participants | Healthy women age 18 to 39 years at risk of pregnancy. Excluded "generally accepted" contraindications of OC use. | |
| Interventions | Prolonged regimen (desogestrel 150 µg and EE 30 µg; nine pill weeks and one pill‐free week; N=198) versus standard regimen (desogestrel 96 µg and EE 30 µg; three pill weeks and one pill‐free week; N=96). | |
| Outcomes | Lipoprotein, liver function, blood coagulation, adverse events, body weight, blood pressure. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | Allocated with sealed envelopes. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 83 women in the prolonged regimen and 32 women in the standard regimen group discontinued early. Primary reasons for discontinuation described; 10 women in the prolonged and one woman in the standard regimen group cited weight gain. Loss to follow up not reported. |
Coenen 1996.
| Methods | Unspecified location. One pre‐treatment cycle and six treatment cycles. | |
| Participants | Healthy women age 18 to 38 years with regular menses. Excluded obesity; pregnancy; recent pregnancy; lactation; contraindications to oral contraceptives; certain medications; heavy smoking. | |
| Interventions | Norgestimate 250 µg and EE 35 µg (N=25) versus gestodene 75 µg and EE 30 µg (N=25) versus desogestrel 150 µg and EE 30 µg (N=25) versus desogestrel 150 µg and EE 20 µg (N=25). | |
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 women who became pregnant during pretreatment cycle were excluded and replaced.
4 women in the norgestimate, 3 women in the gestodene, 1 woman in the desogestrel/EE 30 µg, and 4 women in the desogestrel/EE 20 µg group discontinued early. Primary reasons for discontinuation described; 1 women in the norgestimate group cited weight change. Loss to follow up not reported. |
Coney 2001.
| Methods | 32 sites in USA, Canada and Australia. Article reports pooled data from two randomized controlled trials with similar protocols. Six treatment cycles. Placebo tablets identical in appearance to oral contraceptive pills. | |
| Participants | Healthy women age 14 or more years with regular menses and moderate facial acne. Excluded recent abnormal cervical cytology; pregnancy; willing to use non‐hormonal contraception if at risk of pregnancy; contraindications to oral contraceptive use; recent oral or injectable hormones; recent use of certain drugs. | |
| Interventions | Levonorgestrel 100 µg and EE 20 µg (N=359) versus placebo (N=362). | |
| Outcomes | Lipoprotein, liver function, blood coagulation, adverse events, body weight, blood pressure. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme with block size of four stratified by study site. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Double‐blinded" but did not report who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 22 women in the levonorgestrel and 15 women in the placebo group withdrew before starting treatment. 124 in the oral contraceptive and 125 in the placebo group discontinued early or were lost to follow up. Primary reasons for discontinuation described; two women in the levonorgestrel group cited body weight. |
Dionne 1974.
| Methods | Location not described. 6 treatment cycles. | |
| Participants | Inclusion and exclusion criteria not described. Post‐partum or post‐abortal women were given oral contraceptive (levonorgestrel 250 µg and EE 50 µg) until re‐establishment of regular menses. | |
| Interventions | Levonorgestrel 250 µg and EE 50 µg (N=73) versus levonorgestrel 150 µg and EE 30 µg (N=77). | |
| Outcomes | Cycle control, side effects, discontinuation. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Double‐blinded" but did not report who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 20 women in the higher dose pill and 21 women in the lower dose pill group discontinued early or were lost to follow up. Reasons for discontinuation described; two women in the higher dose group cited weight gain and one women in each group cited weight loss. |
Endrikat 1997.
| Methods | 10 sites in Germany. 12 treatment cycles. | |
| Participants | Healthy, sexually active women age 18 to 39 years. Excluded recent depot‐contraceptive use; pregnancy; liver, vascular, and metabolic diseases; tumors; unclassified genital bleeding. | |
| Interventions | Gestodene 75 µg and EE 20 µg (N=428) versus gestodene 75 µg and EE 30 µg (N=221). | |
| Outcomes | Contraceptive reliability, cycle control, tolerance (including body weight). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Double‐blinded" but did not report who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 93 women in the EE 20 µg and 40 women in the EE 30 µg group discontinued early. Primary reasons for discontinuation included weight gain but no data reported. 16 women in the EE 20 µg and 12 women in the EE 30 µg group were excluded by the sponsor. Lost to follow up not reported. |
Endrikat 1999.
| Methods | 123 sites in France, Austria, the UK, The Netherlands, Switzerland and Italy. 12 treatment cycles. | |
| Participants | Healthy women age 18 to 35 years with regular menses. Excluded current use of oral contraceptive containing 150 µg desogestrel and 20 µg EE; contraindications to oral contraceptive use; recent depot‐contraceptives use; unclassified genital bleeding; excessive smoking. | |
| Interventions | Gestodene 75 µg and EE 20 µg (N=786) versus desogestrel 150 µg and EE 20 µg (N=777). | |
| Outcomes | Contraceptive efficacy, cycle control, adverse events. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 228 women in the gestodene and 221 women in the desogestrel group discontinued early or were lost to follow up. Primary reasons for discontinuation described and did not include weight gain. 87 women were excluded from analysis for protocol violations. |
Endrikat 2001a.
| Methods | 67 sites in Austria, Belgium, France, Italy, Switzerland, and the UK. Seven treatment cycles following at least one pill‐free 'wash‐out' cycle. | |
| Participants | Healthy women age 18 to 35 years. Excluded "established" oral contraceptive contraindications; recent depot‐contraceptive use; select diseases; menses‐related migraines. | |
| Interventions | Prolonged regimen (gestodene 75 µg and EE 20 µg; 23 pill and 5 placebo days) versus standard regimen (desogestrel 150 µg and EE 20 µg; 21 pill and 7 placebo days). 1101 women randomized; initial number assigned to each study group not reported. | |
| Outcomes | Contraceptive efficacy, cycle control, discontinuation, adverse events, blood pressure, weight. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 42 women withdrew before starting treatment. 145 women in the gestodene and 127 women in the desogestrel group discontinued early or were lost to follow up. Primary reasons for discontinuation described and did not include weight gain. 81 women in the gestodene and 88 women in the desogestrel group were excluded due to protocol violations. |
Endrikat 2001b.
| Methods | 30 sites in Germany. 13 treatment cycles. | |
| Participants | Healthy, normal weight women age 18 to 35 years. Excluded high blood pressure; heavy smoking; established contraindications to oral contraceptive use; recent depot‐contraceptive use; unexplained vaginal bleeding; migraine headaches during menstruation. | |
| Interventions | Levonorgestrel 100 µg and EE 20 µg (N=380) versus norethisterone 500 µg and EE 20 µg (N=255) versus levonorgestrel 150 µg and EE 30 µg (N=125; study standard). 767 women were randomized; however, the sum of the number of women assigned to each group totaled 760 women. The remaining seven women were not described. | |
| Outcomes | Cycle control, contraceptive efficacy, discontinuations, blood pressure, adverse events, weight. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 73 women in the levonorgestrel/EE 20 µg, 74 women in the norethisterone, and 13 women in the levonorgestrel/EE 30 µg group discontinued early or were lost to follow up. Primary reasons for discontinuation not described. |
Foulon 2001.
| Methods | One site in France. Three treatment cycles. | |
| Participants | Healthy, non‐obese women age 19 to 27 years with regular menses and normal lipid values. Excluded cardiovascular, thyroid, hepatic, renal or pancreatic diseases; certain drugs. | |
| Interventions | Desogestrel 150 µg and EE 20 µg (N=20) versus levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg (N=17). | |
| Outcomes | Lipoprotein levels, body mass index, blood pressure. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Early discontinuation and loss to follow up not reported. |
Franchini 1995.
| Methods | One site in Italy. Twelve treatment months. | |
| Participants | Women age 18 to 43 years. Excluded recent oral contraceptive or certain drug use; current cardiovascular or metabolic disease; agonistic activity. | |
| Interventions | Desogestrel 150 µg and EE 20 µg versus gestodene 75 µg and EE 30 µg. 80 women randomized; initial number assigned to each study group not reported. | |
| Outcomes | Weight, body composition changes. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 19 women discontinued early. Adverse events cited as primary reason for discontinuation were not described in detail. No women were lost to follow up. |
Goldzieher 1971.
| Methods | One site in USA. Cross‐over design implemented after fourth cycle; however, data after fourth cycle not presented in this review. Six treatment cycles. Pre‐packaged, identical capsules. All placebo cases were tagged on their code designations to receive a contraceptive vaginal cream or foam. To preserve the blinding, 10% of the other groups were randomly marked to receive cream or foam as well. | |
| Participants | Women willing to use vaginal contraceptive foam or cream. Excluded previous oral contraceptive use. | |
| Interventions | EE 100 µg with last five of the 20 pills also containing dimethisterone 25 mg (N=79) versus mestranol 100 µg and ethynodiol diacetate 1 mg (N=78) versus mestranol 50 mg and norethindrone 1 mg (N=81) versus chlormadinone acetate 500 µg daily (N=84) versus placebo (N=76). | |
| Outcomes | Nausea, vomiting, abdominal discomfort, mastalgia, headache, nervousness, depression, body weight, blood pressure. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blinded; participants and investigators blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Early discontinuation and loss to follow up not reported. 18 women were excluded for protocol violations. |
Gruber 2006.
| Methods | 25 centers in 4 countries (Italy, UK, Czech Republic, and Belgium). 7 treatment cycles. No a priori sample size calculation. | |
| Participants | Healthy women aged 18 to 35 years, except for smokers over 30 years. Exclusion: contraindications for COC use; use of DMPA in past 6 months or OC with desogestrel or drospirenone in last cycle; childbirth, abortion, or lactation in last 3 cycles; suspect cervical smear. | |
| Interventions | Drospirenone 3 mg and EE 20 µg (N=222) versus desogestrel 150 µg and EE 20 µg (N=223). | |
| Outcomes | Mean body weight change (no methods reported), bleeding patterns, and contraceptive efficacy. | |
| Notes | Full analysis defined as having at least one dose of study medication and one study observation rather than intent‐to‐treat. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization via "computer‐generated randomization schedule". |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow up: 2.3% drospirenone group and 3.6% desogestrel group. |
Halbe 1998.
| Methods | 8 sites in Brazil. Six treatment cycles. | |
| Participants | Healthy, reproductive‐age women with regular menses and at risk for pregnancy. Excluded contraindications to oral contraceptive use, lactation, certain drugs, malnutrition. | |
| Interventions | Desogestrel 150 µg and EE 30 µg (N=316) versus gestodene 75 µg and EE 30 µg (N=279). | |
| Outcomes | Contraceptive efficacy, cycle control, skin conditions, blood pressure, body weight, adverse events. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 34 women in the desogestrel and 44 women in the gestodene group discontinued early. 19 of these early discontinuations occurred before initiating treatment. Primary reasons for discontinuation described; four women in the gestodene group cited weight gain. Eight women in each group were lost to follow up. |
Kashanian 2010.
| Methods | Public health centers in Iran. Six treatment cycles. Sample size information referred to both 80% and 85% power. Correspondence with researcher indicated 80% power. Sample size of 300 was considered sufficient for power to detect difference in "common side effects". Presuming 10% drop‐out rate, sample of 330 was determined adequate. | |
| Participants | 342 women seeking contraception at public health centers. Inclusion criteria: married, age 17 to 40 years, regular menstruation, no signs or symptoms similar to adverse effects of pills before using them, no prior OCP use. Exclusion criteria: contraindication to pills, systemic disorders or drug use, breastfeeding, delivered < 3 weeks previously; use of injectable contraceptive in past 6 months or implant in past 3 months; abnormal Pap smear, abnormal blood cholesterol and triglycerides, and being illiterate. Further exclusion criteria during the study: omitting one or more pills during the cycles, stopping taking pills, using other contraceptives along with OCPs, acute severe diarrhea and vomiting, and pregnancy. | |
| Interventions | Levonorgestrel 150 µg and EE 30 µg versus levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg | |
| Outcomes | Weight change (weight measured monthly by investigator), side effects, satisfaction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization method not clear in report; blocks of 4 mentioned. Correspondence with researcher indicated use of Random Allocation Software with "simple block randomization." |
| Allocation concealment (selection bias) | Low risk | "Sealed, sequentially distributed envelopes" with letters A, B, C, D (2 letters assigned to each treatment group). Participant chose an envelope, which investigator opened. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding not mentioned in report, but investigator communicated that the outcome assessors were blinded to group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow up: monophasic 6% (10/171); triphasic 9% (16/171). In addition, 2 from the monophasic group who discontinued the intervention were excluded from the analysis. |
Kaunitz 2000.
| Methods | 131 sites. Pooled results from two trials with identical study designs. Six treatment cycles. | |
| Participants | Normal‐weight women age 18 to 50 years at risk of pregnancy with regular menses. Excluded contraindications to oral contraceptives; breastfeeding; certain medication use; recent injectable contraception or IUD use; heavy alcohol use; heavy smoking among those over age 35 years; drug abuse history; abnormal pap smear. | |
| Interventions | Triphasics: desogestrel 100‐125‐150 µg and EE 25 µg versus norethindrone 500‐750‐1000 µg and EE 35 µg. 5654 women randomized; initial number assigned to each study group not reported. | |
| Outcomes | Contraceptive efficacy, cycle control, adverse events, biochemical changes, weight and body mass index, blood pressure. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme stratified by study site. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1040 women discontinued early. Adverse events cited as primary reason for discontinuation were not described in detail. Loss to follow up not reported. |
Kirkman 1994.
| Methods | 66 sites in Denmark, Italy, New Zealand and the United Kingdom. Six treatment cycles. | |
| Participants | Healthy women over age 30 years. Excluded irregular menses; smoking among those over age 34 years; lactation; high blood pressure; certain drug use. | |
| Interventions | Gestodene 75 µg and EE 30 µg (N=505) versus desogestrel 150 µg and EE 20 µg (N=501). | |
| Outcomes | Contraceptive efficacy, cycle control, body weight, blood pressure, discontinuation. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization by pre‐distributed schedules. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 52 women in the gestodene and 49 women in the desogestrel group discontinued early. Weight gain cited as primary reason for discontinuation by four women in the gestodene and two women in the desogestrel group. 7 women in the gestodene and 3 women in the desogestrel group were lost to follow up. 9 women in the gestodene and 12 women in the desogestrel group were excluded for protocol violations. |
Knopp 2001.
| Methods | Study location not described. Nine treatment cycles. | |
| Participants | Healthy women age 21 to 35 years with normal lipid levels and regular menses. Excluded diseases affecting lipoprotein metabolism; recent OC, injectable hormones or certain drug use; certain diseases; high blood pressure; recent smoking; recent alcohol or drug abuse; pregnancy; lactation. | |
| Interventions | Desogestrel 50‐100‐150 µg and EE 35‐30‐30 µg (N=33) versus levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg (N=34). | |
| Outcomes | Plasma lipids, glucose, insulin, hemostasis, sex hormone binding globulin. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Early discontinuation and loss to follow up not reported. One woman from desogestrel group excluded for protocol violation before starting treatment. |
Koetsawang 1977.
| Methods | One site in India. 12 treatment cycles. | |
| Participants | Healthy women with proven fertility. Excluded recent hormone use. | |
| Interventions | Lynestrenol 2 mg and EE 40 µg (N=150) versus lynestrenol 1 mg and EE 40 µg (N=150). | |
| Outcomes | Contraceptive efficacy, cycle control, nausea, weight, headache, dysmenorrhea. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 30 women in the lynestrenol 2 mg and 33 women in the lynestrenol 1 mg group discontinued early. Discontinuations due to side effects not described. 4 women in the lynestrenol 2 mg and 5 women in the lynestrenol 1 mg group were lost to follow up. |
Koetsawang 1995.
| Methods | Six sites in Thailand. Six treatment cycles. | |
| Participants | Healthy women of fertile age with regular menses. Excluded contraindications to oral contraceptive use; lactation; certain drug use. | |
| Interventions | Desogestrel 150 µg and EE 30 µg (N=394) versus gestodene 75 µg and EE 30 µg (N=389). | |
| Outcomes | Contraceptive efficacy, cycle control, side effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization by random number table. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 23 women in the desogestrel and 31 women in the gestodene group discontinued early. Adverse events cited as primary reason for discontinuation not described in detail. 22 women in the desogestrel and 21 women in the gestodene group were lost to follow up. Four women in the desogestrel and three women in the gestodene group were excluded for protocol violations. |
Lachnit‐Fixson 1984.
| Methods | Multicenter trial in Austria, Germany, The Netherlands and the UK. Six treatment cycles. | |
| Participants | Inclusion and exclusion criteria not described. | |
| Interventions | Desogestrel 150 µg and EE 30 µg (N=277) versus triphasic: levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg (N=278). | |
| Outcomes | Contraceptive efficacy, cycle control, body weight, blood pressure, side effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 86 women discontinued early or were lost to follow up. Primary reasons for discontinuation not described. |
Liukko 1987.
| Methods | Study location not described. 24 treatment months. | |
| Participants | Healthy normal‐weight women with regular menses. Excluded history of hypertension; recent pregnancy; recent hormonal therapy. | |
| Interventions | Levonorgestrel 150 µg and EE 30 µg (N=10) versus desogestrel 150 µg and EE 30 µg (N=10). | |
| Outcomes | Body weight, blood pressure, plasma renin activity. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One woman in the levonorgestrel and two women in the desogestrel group discontinued early. Primary reasons for discontinuation described and did not include weight gain. No women were lost to follow up. |
Loudon 1990.
| Methods | 31 sites in the United Kingdom. Six treatment months. | |
| Participants | Women age 16 to 35 years. Excluded high blood pressure; amenorrhea; post‐partum women without resumption of menses; thrombotic disorders; history of sickle‐cell anemia, lipid metabolism disorders, or herpes; liver diseases; abnormal vaginal bleeding of unknown origin; certain neoplasias; pregnancy; lactation. | |
| Interventions | Gestodene 75 µg and EE 30 µg (N=229) versus levonorgestrel 150 µg and EE 30 µg (N=227). | |
| Outcomes | Cycle control, body weight, blood pressure, other side effects, withdrawals. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Double‐blinded" but did not report who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 24 women in the gestodene and 30 women in the levonorgestrel group discontinued early. Primary reasons for discontinuation not described in detail. Four women in the gestodene and five women in the levonorgestrel group were lost to follow up. 32 women withdrew before starting intervention. |
Miller 2001.
| Methods | Four sites in USA. 12 treatment cycles. | |
| Participants | Women age 18 to 45 years who could speak and read English and who did not intend to become pregnant within one year. Excluded "standard" contraindications to OC use. | |
| Interventions | Standard regimen (28‐day cycle with 21 active pills; N=44) versus prolonged regimen (49‐day cycle with 42 active pills; N=46). Both groups used same oral contraceptive (levonorgestrel 300 µg and EE 30 µg). | |
| Outcomes | Cycle control, body weight, blood pressure, other side effects, withdrawals. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized using random number table and permuted blocks of six. |
| Allocation concealment (selection bias) | Low risk | Allocation concealed with sequentially numbered, opaque envelopes. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 women in each group withdrew before starting treatment. 9 women in the standard regimen and 5 women in the prolonged regimen group discontinued early. Primary reasons for discontinuation described; 1 woman in prolonged regimen group cited weight gain. 9 women in the standard and 11 women in the prolonged regimen group were lost to follow up. |
Milsom 2006.
| Methods | Open‐label, randomized trial in 10 European countries from May 2002 to April 2004. | |
| Participants | 1017 women, at least 18 years old, seeking contraception. Exclusion criteria: contraindication for hormonal contraception, abortion or breastfeeding in past 2 months, injectable hormonal contraceptive use in past 6 months, abnormal cervical smear during screening, and use in past 2 months of drugs that interfere with metabolism of hormonal contraceptives. | |
| Interventions | Vaginal ring releasing etonogestrel 120 µg + EE 15 µg daily versus COC containing drospirenone 3 mg + EE 30 µg; 13 treatment cycles. | |
| Outcomes | Body weight (methods reported for standardized measurements) and body composition; contraceptive efficacy, compliance, acceptability, tolerability (adverse events), continuation in earlier report (Ahrendt 2006) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization conducted via an interactive voice response system. |
| Allocation concealment (selection bias) | Low risk | Interactive voice response system. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss after randomization and before treatment: 1017 ‐ 983 = 34. Loss after treatment: ring 29% (144/499) and COC 25% (123/484). Lost to follow up: 2% ring and 3% COC. |
Oddsson 2005.
| Methods | 11 countries in Europe and South America. 13 treatment cycles. | |
| Participants | 1030 "healthy" women, 18 or more years old. Excluded if OC contraindicated, DMPA use in previous 6 months, postpartum or postabortion within 2 months of start, breastfeeding within 2 months, abnormal cervical smear, or drugs that could interfere with contraceptive metabolism. | |
| Interventions | Vaginal ring releasing 120 µg etonogestrel and 15 µg ethinylestradiol daily (N=512) versus OC with 150 µg levonorgestrel and 30 µg ethinylestradiol (N=518). | |
| Outcomes | Contraceptive efficacy, compliance, weight change (≥7% or ≤7%). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomized with interactive voice response system, which gave treatment group and medication number. |
| Allocation concealment (selection bias) | Low risk | Interactive voice response system |
| Blinding (performance bias and detection bias) All outcomes | High risk | Open‐label |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 1090 were randomized, but only 1079 began treatment. 298 discontinued (149 from each group): 33 lost to follow up in each group, 58 adverse events in ring group and 45 in OC group. |
Oelkers 1995.
| Methods | Study location not described. One pill‐free pretreatment cycle, six treatment cycles, and one pill‐free post‐treatment cycle. | |
| Participants | Women age 18 to 34 years. Excluded smoking among those age 30 years or older. | |
| Interventions | Drospirenone 3 mg and EE 30 µg (N=20) versus drospirenone 3 mg and EE 20 µg (N=20) versus drospirenone 3 mg and EE 15 µg (N=20) versus levonorgestrel 150 µg and EE 30 µg (N=20; control group). | |
| Outcomes | Renin‐aldosterone system, well‐being, cycle control, body weight, blood pressure, glucose tolerance, lipid metabolism. Cycle average weights based on self‐measured weighing conducted every second day in unclothed, fasting‐state. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Triple‐blinded; participant, investigator and outcome assessor blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Early discontinuation and loss to follow up not reported. |
Oelkers 2000.
| Methods | Study 2:
Three centers in The Netherlands and Belgium. One pill‐free pre‐treatment cycle and three treatment cycles. Study 3: One site in The Netherlands. Two pill‐free pretreatment cycles, 13 treatment cycles and one follow up cycle. |
|
| Participants | Study 2 and 3: Women age 18 to 35 years (18 to 30 years for smokers) with regular menses. Excluded pregnancy. | |
| Interventions | Study 2:
Drospirenone 2 mg and EE 30 µg (N=35) versus drospirenone 3 mg and EE 30 µg (N=35). Study 3: Drospirenone 3 mg and EE 30 µg (N=30) versus desogestrel 150 µg and EE 30 µg (N=30). |
|
| Outcomes | Study 2 and 3: Renin‐angiotensin‐aldosterone system, body weight. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Study 2, no information; study 3, unblinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Early discontinuation and loss to follow up not reported. |
Procter‐Gray 2008.
| Methods | Five sites in USA. Participants recruited Aug 1998 to Sep 2003 and followed at 1 and 2 years. | |
| Participants | 150 female runners. Inclusion criteria: 18 to 26 years old, run at least 40 miles per week during peak training times, and compete in running races. Exclusion criteria: had used OC, other hormone therapy, or other hormonal contraception in past 6 months; unwilling to be randomized to take OC or not to take OC for 2 years; any medical contraindication to OC use. | |
| Interventions | Norgestrel 300 µg and EE 30 µg (N=69) versus no intervention (N=81). | |
| Outcomes | Bone mass, stress fractures, weight and body composition. | |
| Notes | Crossover from assigned protocol > 25% in each group; researchers conducted primary analysis by assigned group and secondary analysis by treatment received. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization done by investigator not involved in study, using random‐number table. Stratified by clinical site. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded participants and prescribing physicians; assessors not informed of treatment assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow up: 17% overall; treatment 22% (15/69); control 14% (11/81). |
Rosenbaum 2000.
| Methods | Six sites in Germany and Belgium. Pill‐free cycle followed by three treatment cycles and a follow‐up cycle. | |
| Participants | Women age 18 to 35 years (18 to 30 years for smokers) with regular menses. Excluded "usual" contraindications to oral contraception. | |
| Interventions | Drospirenone 2 mg and EE 30 µg (N=26) versus drospirenone 3 mg and EE 30 µg (N=26). | |
| Outcomes | Hormonal and peripheral measurements, cycle control, safety. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No one in the drospirenone 2 mg and one woman in the drospirenone 3 mg group discontinued early. The primary reasons for discontinuation described and did not include weight gain. Three women in the drospirenone 2 mg and two women in the drospirenone 3 µg group were excluded for protocol violations. No women were lost to follow up. |
Sang 1995.
| Methods | 15 sites in China. 12 treatment months. | |
| Participants | Healthy women age 18 to 35 years with regular menses and proven fertility. Excluded lactation; pregnancy; diabetes; abnormal Pap smears; unexplained vaginal bleeding; hypertension; liver disease; hypertension; thromboembolism; malignancy; abnormal nipple discharge; selected drug use; recent injectable or oral contraceptive. | |
| Interventions | Norethisterone enanthate 50 mg and estradiol valerate 5 mg (N=1960) versus medroxyprogesterone acetate 25 mg and estradiol cypionate 5 mg (N=1955). Also included a study arm with Injectable No. 1, which was not included in the present review since the drug regimen was changed during the trial due to unacceptable efficacy rates. | |
| Outcomes | Contraceptive efficacy, discontinuation, weight, blood pressure, side effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization using random numbers table. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 353 women in the norethisterone enanthate and 498 women in the medroxyprogesterone acetate group discontinued early. Primary reasons for discontinuation described; 10 women in the norethisterone enanthate and 14 women in the medroxyprogesterone acetate group cited weight gain. 17 women in the norethisterone enanthate and 18 women in the medroxyprogesterone acetate group were lost to follow up. |
Serfaty 1998.
| Methods | 52 sites in Paris, France. Six treatment cycles. | |
| Participants | Healthy, normal‐weight women age 18 to 45 years (18 to 35 years for smokers) with regular menses and normal plasma lipid and carbohydrate levels. Excluded contraindications to oral contraception; recent injectable, implant, or intrauterine contraceptive use; recent birth or abortion; use of certain drugs. | |
| Interventions | Desogestrel 150 µg and EE 20 µg (N=515) versus gestodene 75 µg and EE 20 µg (N=511). | |
| Outcomes | Contraceptive efficacy, cycle control, premenstrual syndrome, adverse events, weight, blood pressure. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized in blocks of four. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Six women in the desogestrel and four women in the gestodene group withdrew before starting treatment. 85 women in the desogestrel (17%) and 97 (19%) women in the gestodene group discontinued early, were lost to follow up or were excluded for protocol violation. Primary reasons for discontinuation were not described. |
Sibai 2001.
| Methods | Study location not described. Nine treatment cycles. | |
| Participants | Inclusion and exclusion criteria not described. | |
| Interventions | Contraceptive skin patch releasing norelgestromin 150 µg and EE 20 µg daily (N=92) versus placebo (N=44). Initial number assigned to each study group not reported. | |
| Outcomes | Body weight. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Double‐blinded" but did not report who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Early discontinuation and loss to follow up not reported. Unclear if the number of participants with weight outcomes was the number of women randomized. |
Spellacy 1970.
| Methods | One site in the USA. Six treatment cycles. | |
| Participants | Inclusion and exclusion criteria not described. | |
| Interventions | Ethynodiol diacetate 1.0 mg and mestranol 100 µg (N=24) versus 15 pills of mestranol 100 mg, 8 pills of mestranol 100 mg and chlormadinone acetate 1.5 mg and 5 placebo pills (N=33). | |
| Outcomes | Blood pressure. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Early discontinuation and loss to follow up not reported. |
Spona 1996.
| Methods | Two sites in UK and Austria. One pill‐free cycle, five treatment cycles and one follow‐up cycle. | |
| Participants | Healthy, non‐obese women age 19 to 35 years with demonstrable ovulatory pretreatment cycle. Excluded heavy smokers; pregnancy; certain diseases; history of migraine with aura; other contraindications for oral contraceptive use. | |
| Interventions | Standard regimen (21 pill days and 7 pill‐free days; N=30) versus prolonged regimen (23 pill days and 5 pill‐free days; N=30). Both groups used the same oral contraceptive (gestodene 75 µg and EE 20 µg). | |
| Outcomes | Follicular development, endogenous hormone levels, cycle control, adverse effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization list using blocks of ten and four. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Double‐blinded" but did not report who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One woman in the standard regimen and no women in the prolonged regimen group discontinued early. Primary reasons for discontinuation described and did not include weight change. No women were lost to follow up. |
Stewart 2005.
| Methods | 9 clinical research sites. 112 days (4 cycles). | |
| Participants | 239 healthy, regularly menstruating women, aged 18 to 45 years. | |
| Interventions | Patch delivered daily 150 µg norelgestromin and 20 µg ethinyl E2. Extended regimen (N=239) of weekly patch for 12 weeks, 1 patch‐free week, then weekly patch for 3 weeks versus cyclic regimen (N=81) of 4 cycles (28 days each) of 1 patch weekly for 3 weeks then 1 patch‐free week. Exclusion criteria included contraindication for steroid hormones, dermal hypersensitivity, extended OC within prior 3 months. | |
| Outcomes | Total bleeding or spotting days plus headaches and overall assessment; weight change. | |
| Notes | Four subjects had no information after randomization (3 extended and 1 cyclic). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization done by pharmaceutical sponsor; permuted blocks of 6. Assigned 2:1. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow up: 2% in extended group and 4% in cyclic regimen. Completed study: 123/155 (79%) in extended group and 68/80 (85%) in cyclic regimen. |
Teichmann 1995.
| Methods | One site in Poland. One pill‐free pretreatment cycle and 12 treatment cycles. | |
| Participants | Healthy, non‐obese, sexually active women age 19 to 40 years with regular menses. Excluded abnormal lipid levels; certain drug use; smoking; "generally accepted" contraindications for oral contraceptives. | |
| Interventions | Gestodene 75 µg and EE 30 µg versus desogestrel 150 µg and EE 20 µg. 500 women randomized; initial number assigned to each study group not reported. | |
| Outcomes | Follicle growth, discontinuation. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 84 women withdrew before starting treatment. 45 women in the gestodene and 54 women in the desogestrel group discontinued early. Primary reasons for discontinuation described and weight gain not cited. Loss to follow up not reported. Three women were excluded for protocol violations. |
Van der Does 1995.
| Methods | One site in the Netherlands. Six treatment cycles. | |
| Participants | Healthy women age 20 to 35 years with regular menses. Excluded recent oral contraceptive use; recent pregnancy; lactation. | |
| Interventions | Triphasics: levonorgestrel 50‐75‐125 µg and EE 30‐40‐30 µg (N=15) versus desogestrel 50‐100‐150 µg and EE 35‐30‐30 µg (N=16). | |
| Outcomes | Follicle growth, hormone levels. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Early discontinuation and loss to follow up not reported. |
Weisberg 1999.
| Methods | Three sites in Australia and USA. Four treatment cycles. | |
| Participants | Women age 18 to 35 years with regular menses. Excluded "usual" contraindications to oral contraceptives; recent oral or injectable contraceptives; vaginal or cervical irritation; pregnancy. | |
| Interventions | Contraceptive vaginal ring releasing norethindrone acetate 1 mg and EE 15 µg (N=37) versus norethindrone acetate 1 mg and EE 20 µg (N=24). | |
| Outcomes | Serum hormone levels, side effects, weight. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Nine women discontinued early or were excluded for protocol violations. Primary reasons for discontinuation described and weight gain not cited. Loss to follow up not reported. |
Wiegratz 1995.
| Methods | Study location not described. 12 treatment cycles. | |
| Participants | Healthy women age 18 to 36 years with regular menses. Excluded recent hormonal contraceptives; certain drug use. | |
| Interventions | Gestodene 50‐70‐100 µg and EE 30‐40‐30 µg versus norgestimate 250 µg and EE 35 µg. 52 women randomized; initial number assigned to each study group not reported. | |
| Outcomes | Serum hormone levels, side effects. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Six women discontinued early. Primary reasons for discontinuation described and weight gain not cited. No women were lost to follow up. |
Wiegratz 2002.
| Methods | Two sites in Germany. Six treatment cycles. | |
| Participants | Women age 18 to 35 years with regular menses. Excluded contraindications for oral contraceptive use; recent hormonal drugs. | |
| Interventions | Dienogest 2 mg and EE 30 µg versus dienogest 2 mg and EE 20 µg versus dienogest 2 mg, estradiol valerate 2 mg and EE 10 µg versus levonorgestrel 100 µg and EE 20 µg. 100 women randomized; initial number assigned to each study group not reported. | |
| Outcomes | Lipid metabolism. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Double‐blinded" but did not report who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 110 women screened and 100 randomized. Eight women discontinued early. Primary reasons for discontinuation not described. One woman lost to follow up. Intent‐to treat analysis used. |
Wiik 1993.
| Methods | Ten sites in Norway and Finland. Six treatment cycles. | |
| Participants | Healthy, normal‐weight women age 18 to 30 years. Excluded recent oral contraceptive use; certain diseases; high cholesterol levels. | |
| Interventions | Norethisterone 500‐1000 µg and EE 35 µg (N=100) versus levonorgestrel 50‐75‐125 µg and EE 30‐40 µg (N=96). | |
| Outcomes | Serum lipids, discontinuation, side effects, weight. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomization scheme. |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Single‐blinded" but did not report who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 17 women in the norethisterone and seven in the levonorgestrel group discontinued early. Primary reasons for discontinuation described; four women in the norethisterone and one woman in the levonorgestrel group cited weight gain. Nine women in the norethisterone and 14 in the levonorgestrel group were lost to follow up. |
Winkler 1996.
| Methods | One site. Two pre‐treatment cycles, six treatment cycles and one post‐treatment cycle. | |
| Participants | Healthy women age 18 to 30 years. Excluded contraindications to oral contraceptive use; heavy smoking. | |
| Interventions | Gestodene 75 µg and EE 30 µg (N=20) versus gestodene 75 µg and EE 20 µg (N=20). | |
| Outcomes | Hemostatic measurements. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Two women in both groups discontinued early. Primary reasons for discontinuation described and weight change not cited. No women were lost to follow up. |
Worsley 1980.
| Methods | One site. Three treatment cycles. | |
| Participants | Inclusion and exclusion criteria not described. | |
| Interventions | Norethisterone acetate 1 mg and EE 50 µg versus levonorgestrel 250 µg and EE 50 µg versus dl‐norgestrel 500 µg and EE 50 µg. Number of women randomized not reported. | |
| Outcomes | Psychological tests, blood pressure, weight. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Early discontinuation and loss to follow up not reported. |
COC = combination oral contraceptive DMPA = depot‐medroxyprogesterone acetate EE = ethinyl estradiol OC = oral contraceptive
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahrendt 2009 | No weight change data presented. Researchers presented the numbers that reported an increase in weight as adverse events. Weight was reportedly measured at screening and final assessment. |
| Bonny 2006 | Participants chose DMPA or OC, then DMPA group was randomly assigned to estrogen supplement or placebo supplement. |
| Boonyarangkul 2007 | No change data presented. Researchers presented weights at baseline and maximum weight gain. |
| Elkind‐Hirsch 2007 | No change data presented. Researchers compared body mass index within group at pre‐treatment and post‐treatment. |
| Endrikat 2007 | Single‐arm study |
| Fan 2010 | Weight change was shown in figure without actual numbers. Abstract provided means without variance. Researchers reported that BMI was also measured but no data were provided. |
| Gaspard 2003 | No information on sampling variation for mean weight changes. |
| Grinspoon 2003 | Researchers reported no significant change in weight. No weight data provided for calculating. |
| Junge 2011 | No weight change data presented. Investigators reported mean weight (and SD) at baseline and end of study. |
| Machado 2006 | Study duration was only one cycle. |
| Miller 2003 | No weight change data presented. Researchers compared weights for groups at baseline and at exit. |
| Miller 2005 | No weight change data presented. Researchers reported weights for regimens at baseline and at exit. |
| Mohamed 2011 | No weight change data presented. Investigators reported an increase in weight as adverse event. |
| O'Connell 2005 | Mean change in body mass index was reported, but no variance was provided. |
| O'Connell 2007 | Trial of OCs as treatment for dysmenorrhea. |
| Sabatini 2006 | Insufficient change data presented. Reported maximum weight gain per group rather than mean. |
| Sanam 2011 | No Ns given for analysis. Unable to obtain further information from investigator. Report is inconsistent regarding weight change: text states 2.5 kg increase in mean weight for one group, while table shows 3.3 kg change for same group. |
| Sangthawan 2005 | Weight data provided for baseline only. Questionnaire asked about perception of weight change (scored 0 to 4). |
| Skouby 2005 | Weight data only provided for baseline. |
| Suthipongse 2004 | No change data presented. Researchers compared weights for groups at baseline and at exit. |
| Taneepanichskul 2002 | No change data presented. Researchers presented weights per group at baseline and at end of study. Sample sizes differed for baseline and end of study data. |
| Tantbirojn 2002 | No change data presented. Researchers presented weights per group at admission and at end of study. No sample sizes provided per group. |
| Veres 2004 | Researchers reported there was no significant change in weight. Data were not provided. |
| Westhoff 2007 | Weight change not quantified, but reported as gained, lost or no change. |
| Westhoff 2010 | Body mass index was used for stratifying; outcomes did not include weight or BMI change. |
| Westhoff 2012 | No weight change data; investigators reported slight differences in weight increase between the groups. Data were not provided. Adverse events included percent reporting weight gain. |
| Winkler 2004 | Researchers reported there was no significant change in weight. Data were not provided. |
| Yildizhan 2009 | Researchers reported there was no significant change in BMI. Means were shown but not change data. |
Characteristics of ongoing studies [ordered by study ID]
Mahidol 2013.
| Trial name or title | Comparison of body weight change during contraception with Belara and Yasmin |
| Methods | Family Planning Unit, Mahidol University, Bangkok, Thailand RCT; blinding of subject, caregiver, investigator, outcome assessor |
| Participants | 100 women, 19 to 45 years old Inclusion criteria: reproductive age; BMI < 28.5 kg/m2; regular menstruation; no pelvic organ disorder; wants contraception with oral contraceptive pills. Exclusion criteria: abnormal blood pressure; abnormal vaginal bleeding; pregnant; on medication effecting contraceptive pills, i.e., anti‐fungal, anti‐retroviral, anti‐convulsant drug; contraindication for OCP; used steroid in 3 months before enrollment; smoking; eating disorder. |
| Interventions | 2 mg chlormadinone acetate and 30 µg ethinyl estradiol versus 3 mg drospirenone and 30 µg ethinyl estradiol Duration: 6 cycles |
| Outcomes | Body weight change at 3 and 6 months of use |
| Starting date | Study start June 2012; estimated completion July 2014 |
| Contact information | no information |
| Notes |
Contributions of authors
F Helmerhorst developed the idea. M Gallo extracted data for the original review in 2003 and drafted the review. D Grimes did the second data extraction for the initial review and the updates through 2011. For the 2005 to 2013 updates, L Lopez reviewed the search results, did the primary data extraction, and incorporated the results. In 2013, F Carayon helped review search results, entered information, and checked the review. D Grimes, K Schulz, and F Helmerhorst revised and approved the initial review and reviewed the updates.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institute of Child Health and Human Development, USA.
Support for conducting the review and updates at FHI 360
-
U.S. Agency for International Development, USA.
Support for conducting the review and updates (through 2011) at FHI 360
Declarations of interest
DA Grimes has consulted with the pharmaceutical companies Bayer Healthcare Pharmaceuticals and Merck & Co, Inc.
FM Helmerhorst has supervised studies sponsored or assigned by various pharmaceutical companies that manufacture oral contraceptives.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Aden 1998 {published and unpublished data}
- Aden U, Jung‐Hoffmann C, Kuhl H. A randomized cross‐over study on various hormonal parameters of two triphasic oral contraceptives. Contraception 1998;58:75‐81. [DOI] [PubMed] [Google Scholar]
Agoestina 1989 {published and unpublished data}
- Agoestina T, Sabarudin U, Hoppe G. A study comparing a gestoden triphasic formulation with a fixed combination OC. Advances in Contraception 1989;5:71‐84. [DOI] [PubMed] [Google Scholar]
Brill 1991 {published data only}
- Brill K, Muller C, Schnitker J, Albring M. The influence of different modern low‐dose oral contraceptives on intermenstrual bleeding. Advances in Contraception 1991;7:51‐61. [Google Scholar]
Brill 1996 {published and unpublished data}
- Brill K, Then A, Beisiegel U, Jene A, Wunsch C, Leidenberger F. Investigation of the influence of two low‐dose monophasic oral contraceptives containing 20 micrograms ethinylestradiol/75 micrograms gestodene and 30 micrograms ethinylestradiol/75 micrograms gestodene, on lipid metabolism in an open randomized trial. Contraception 1996;54:291‐7. [DOI] [PubMed] [Google Scholar]
Burkman 2007 {published data only}
- Burkman RT, Fisher AC, LaGuardia KD. Effects of low‐dose oral contraceptives on body weight. Journal of Reproductive Medicine 2007;52:1030‐4. [PubMed] [Google Scholar]
- Hampton RM, Short M, Bieber E, Bouchard C, Ayotte N, Shangold G, et al. Comparison of a novel norgestimate/ethinyl estradiol oral contraceptive (Ortho Tri‐Cyclen Lo) with the oral contraceptive Loestrin Fe 1/20. Contraception 2001;63:289‐95. [DOI] [PubMed] [Google Scholar]
Cachrimanidou 1993 {published data only}
- Cachrimanidou AC, Hellberg D, Nilsson S, Waldenstrom U, Olsson SE, Sikstrom B. Long‐interval treatment regimen with a desogestrel‐containing oral contraceptive. Contraception 1993;48:205‐16. [DOI] [PubMed] [Google Scholar]
Coenen 1996 {published data only}
- Coenen CM, Thomas CM, Borm GF, Hollanders JM, Rolland R. Changes in androgens during treatment with four low‐dose contraceptives. Contraception 1996;53:171‐6. [DOI] [PubMed] [Google Scholar]
Coney 2001 {published data only}
- Coney P, Washenik K, Langley RGB, DiGiovanna JJ, Harrison DD. Weight change and adverse event incidence with a low‐dose oral contraceptive: two randomized, placebo‐controlled trials. Contraception 2001;63:297‐302. [DOI] [PubMed] [Google Scholar]
Dionne 1974 {published data only}
- Dionne P, Vickerson F. A double‐blind comparison of two oral contraceptives containing 50 µg. and 30 µg. ethinyl estradiol. Current Therapeutic Research, Clinical and Experimental 1974;16:281‐8. [PubMed] [Google Scholar]
Endrikat 1997 {published data only}
- Endrikat J, Muller U, Dusterberg B. A twelve‐month comparative clinical investigation of two low‐dose oral contraceptives containing 20 µg ethinylestradiol/75 µg gestodene and 30 µg ethinylestradiol/75 µg gestodene, with respect to efficacy, cycle control, and tolerance. Contraception 1997;55:131‐7. [DOI] [PubMed] [Google Scholar]
Endrikat 1999 {published data only}
- Endrikat J, Dusterberg B, Ruebig A, Gerlinger C, Strowitzki T. Comparison of efficacy, cycle control, and tolerability of two low‐dose oral contraceptives in a multicenter clinical study. Contraception 1999;60:269‐74. [DOI] [PubMed] [Google Scholar]
- Endrikat J, Jaques MA, Mayerhofer M, Pelissier C, Muller U, Dusterberg B. A twelve‐month comparative clinical investigation of two low‐dose oral contraceptives containing 20 micrograms ethinylestradiol/75 micrograms gestodene and 20 micrograms ethinylestradiol/150 micrograms desogestrel, with respect to efficacy, cycle control and tolerance. Contraception 1995;52:229‐35. [DOI] [PubMed] [Google Scholar]
Endrikat 2001a {published data only}
- Endrikat J, Cronin M, Gerlinger C, Ruebig A, Schmidt W, Dusterberg B. Open, multicenter comparison of efficacy, cycle control, and tolerability of a 23‐day oral contraceptive regimen with 20 µg ethinyl estradiol and 75 µg gestodene and a 21‐day regimen with 20 µg ethinyl estradiol and 150 µg desogestrel. Contraception 2001;64:201‐7. [DOI] [PubMed] [Google Scholar]
Endrikat 2001b {published and unpublished data}
- Endrikat J, Hite R, Bannemerschult R, Gerlinger C, Schmidt W. Multicenter, comparative study of cycle control, efficacy and tolerability of two low‐dose oral contraceptives containing 20 µg ethinylestradiol/100 µg levonorgestrel and 20 µg ethinylestradiol/500 µg norethisterone. Contraception 2001;64:3‐10. [DOI] [PubMed] [Google Scholar]
Foulon 2001 {published and unpublished data}
- Foulon T, Payen N, Laporte F, Bijaoui S, Dupont G, Roland F, et al. Effects of two low‐dose oral contraceptives containing ethinylestradiol and either desogestrel or levonorgestrel on serum lipids and lipoproteins with particular regard to LDL size. Contraception 2001;64:11‐6. [DOI] [PubMed] [Google Scholar]
Franchini 1995 {published and unpublished data}
- Franchini M, Caruso C, Nigrelli S, Poggiali C. Evaluation of body composition during low‐dose estrogen oral contraceptives treatment. Acta Europaea Fertilitatis 1995;26:69‐73. [PubMed] [Google Scholar]
Goldzieher 1971 {published data only}
- Goldzieher JW, Moses LE, Averkin E, Scheel C, Taber BZ. A placebo‐controlled double‐blind crossover investigation of the side effects attributed to oral contraceptives. Fertility and Sterility 1971;22:609‐23. [PubMed] [Google Scholar]
Gruber 2006 {published data only}
- Gruber DM, Huber JC, Melis GB, Stagg C, Parke S, Marr J. A comparison of the cycle control, safety, and efficacy profile of a 21‐day regimen of ethinylestradiol 20µg and drospirenone 3mg with a 21‐day regimen of ethinylestradiol 20µg and desogestrel 150µg. Treatments in Endocrinology 2006;5:115‐21. [DOI] [PubMed] [Google Scholar]
Halbe 1998 {published data only}
- Halbe HW, Melo NR, Bahamondes L, Petracco A, Lemgruber M, Andrade RP, et al. Efficacy and acceptability of two monophasic oral contraceptives containing ethinylestradiol and either desogestrel or gestodene. European Journal of Contraception & Reproductive Health Care 1998;3:113‐20. [DOI] [PubMed] [Google Scholar]
Kashanian 2010 {published data only}
- Kashanian M, Shahpourian F, Zare O. A comparison between monophasic levonorgestrel‐ethinyl estradiol 150/30 and triphasic levonorgestrel‐ethinyl estradiol 50‐75‐125/30‐40‐30 contraceptive pills for side effects and patient satisfaction: a study in Iran. European Journal of Obstetrics, Gynecology, and Reproductive Biology. 2010/02/27 2010; Vol. 150, issue 1:47‐51. [DOI] [PubMed]
Kaunitz 2000 {published and unpublished data}
- Kaunitz AM. Efficacy, cycle control, and safety of two triphasic oral contraceptives: Cyclessa (desogestrel/ethinyl estradiol) and Ortho‐Novum 7/7/7 (norethindrone/ethinyl estradiol): a randomized clinical trial. Contraception 2000;61:295‐302. [DOI] [PubMed] [Google Scholar]
Kirkman 1994 {published data only}
- Kirkman RJ, Pedersen JH, Fioretti P, Roberts HE. Clinical comparison of two low‐dose oral contraceptives, Minulet and Mercilon, in women over 30 years of age. Contraception 1994;49:33‐46. [DOI] [PubMed] [Google Scholar]
- Kirkman RJE. Clinical comparison of two low‐dose oral contraceptives in women older than 30 years. Advances in Contraception 1991;7:63‐76. [Google Scholar]
Knopp 2001 {published data only}
- Knopp RH, Broyles FE, Cheung M, Moore K, Marcovina S, Chandler WL. Comparison of the lipoprotein, carbohydrate, and hemostatic effects of phasic oral contraceptives containing desogestrel or levonorgestrel. Contraception 2001;63:1‐11. [DOI] [PubMed] [Google Scholar]
Koetsawang 1977 {published data only}
- Koetsawang S, Srisupandit S, Srivannaboon S, Bhiraleus P. Comparative clinical trial of two oral contraceptives with a low‐‐ estrogen content. Journal of the Medical Association of Thailand 1977;60:368‐73. [PubMed] [Google Scholar]
Koetsawang 1995 {published data only}
- Koetsawang S, Charoenvisal C, Banharnsupawat L, Singhakovin S, Kaewsuk O, Punnahitanont S. Multicenter trial of two monophasic oral contraceptives containing 30 mcg ethinylestradiol and either desogestrel or gestodene in Thai women. Contraception 1995;51:225‐9. [DOI] [PubMed] [Google Scholar]
Lachnit‐Fixson 1984 {published data only}
- Lachnit‐Fixson U, Aydinlik S, Lehnert J. Clinical comparison between a monophasic preparation and a triphasic preparation. In: Rolland R, Harrison RF, Bonnar J, Thompson W editor(s). Advances in fertility control and the treatment of sterility: the proceedings of a special symposium held at the XIth World Congress on Fertility and Sterility, Dublin, June 1983. Hingham, MA: MTP Press, 1984:71‐9. [Google Scholar]
Liukko 1987 {published data only}
- Liukko P, Erkkola R, Gronroos M, Lammintausta R. Plasma renin activity, blood pressure and body weight during two years' oral contraception with two different low‐estrogen combinations. Annales Chirurgiae et Gynaecologiae Supplementum 1987;202:45‐9. [PubMed] [Google Scholar]
- Liukko P, Erkkola R, Lammintausta R, Gronroos M, Kloosterboer HJ. Blood glucose, serum insulin, serum growth hormone and serum glycosylated proteins during two years' oral contraception with low‐ estrogen combinations. Annales Chirurgiae et Gynaecologiae Supplementum 1987;202:50‐53. [PubMed] [Google Scholar]
Loudon 1990 {published data only}
- Loudon NB, Kirkman RJE, Dewsbury JA. A double‐blind comparison of the efficacy and acceptability of Femodene and Microgynon‐30. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1990;34:257‐66. [DOI] [PubMed] [Google Scholar]
Miller 2001 {published data only}
- Miller L, Notter KM. Menstrual reduction with extended use of combination oral contraceptive pills: randomized controlled trial. Obstetrics and Gynecology 2001;98:771‐8. [DOI] [PubMed] [Google Scholar]
Milsom 2006 {published data only}
- Ahrendt H‐J, Nisand I, Bastianelli C, Gómez AM, Gemzell‐Danielsson K, Urdl W, et al. Efficacy, acceptability and tolerability of the combined contraceptive ring, NuvaRing, compared with an oral contraceptive containing 3 µg of ethinyl estradiol and 3 mg of drospirenone. Contraception 2006;74:451‐7. [DOI] [PubMed] [Google Scholar]
- Milsom I, Lete I, Bjertnaes A, Rokstad K, Lindh I, Gruber CJ, et al. Effects on cycle control and bodyweight of the combined contraceptive ring, NuvaRing, versus an oral contraceptive containing 30 µg ethinyl estradiol and 3 mg drospirenone. Human Reproduction 2006;21:2304‐11. [DOI] [PubMed] [Google Scholar]
Oddsson 2005 {published data only}
- Oddsson K, Leifels‐Fischer B, Melo NR, Wiel‐Masson D, Benedetto C, Verhoeven CHJ, et al. Efficacy and safety of a contraceptive vaginal ring (NuvaRing) compared with a combined oral contraceptive: a 1‐year randomized trial. Contraception 2005;71:176‐82. [DOI] [PubMed] [Google Scholar]
Oelkers 1995 {published data only}
- Oelkers W, Foidart JM, Dombrovicz N, Welter A, Heithecker R. Effects of a new oral contraceptive containing an antimineralocorticoid progestogen, drospirenone, on the renin‐aldosterone system, body weight, blood pressure, glucose tolerance, and lipid metabolism. Journal of Clinical Endocrinology and Metabolism 1995;80:1816‐21. [DOI] [PubMed] [Google Scholar]
Oelkers 2000 {published data only}
- Oelkers W, Helmerhorst FM, Wuttke W, Heithecker R. Effect of an oral contraceptive containing drospirenone on the renin‐angiotensin‐aldosterone system in healthy female volunteers. Gynecological Endocrinology 2000;14:204‐13. [DOI] [PubMed] [Google Scholar]
Procter‐Gray 2008 {published data only}
- Cobb KL, Bachrach LK, Sowers M, Nieves J, Greendale GA, Kent KK, et al. The effect of oral contraceptives on bone mass and stress fractures in female runners. Medicine & Science in Sports & Exercise. 2007/09/07 2007; Vol. 39, issue 9:1464‐73. [DOI] [PubMed]
- Procter‐Gray E, Cobb KL, Crawford SL, Bachrach LK, Chirra A, Sowers M, et al. Effect of oral contraceptives on weight and body composition in young female runners. Medicine & Science in Sports & Exercise. 2008/06/27 2008; Vol. 40, issue 7:1205‐12. [DOI] [PubMed]
Rosenbaum 2000 {published data only}
- Rosenbaum P, Schmidt W, Helmerhorst FM, Wuttke W, Rossmanith W, Freundl F, et al. Inhibition of ovulation by a novel progestogen (drospirenone) alone or in combination with ethinylestradiol. European Journal of Contraception & Reproductive Health Care 2000;5:16‐24. [DOI] [PubMed] [Google Scholar]
Sang 1995 {published and unpublished data}
- Sang GW, Shao QX, Ge RS, Ge JL, Chen JK, Song S, et al. A multicentred phase III comparative clinical trial of Mesigyna, Cyclofem and injectable No. 1 given monthly by intramuscular injection to Chinese women. Contraception 1995;51:167‐83. [DOI] [PubMed] [Google Scholar]
Serfaty 1998 {published data only}
- Serfaty D, Vree ML. A comparison of the cycle control and tolerability of two ultra low‐ dose oral contraceptives containing 20 micrograms ethinylestradiol and either 150 micrograms desogestrel or 75 micrograms gestodene. European Journal of Contraception & Reproductive Health Care 1998;3:179‐89. [DOI] [PubMed] [Google Scholar]
Sibai 2001 {published data only}
- Sibai B, Odlind V, Meador M, Shangold G, Fisher A, Creasy G. A comparative assessment of ORTHO EVRA™/EVRA™ to placebo patch effects on body weight. Fertility and Sterility 2001;76:S188. [Google Scholar]
- Sibai BM, Odlind V, Meador ML, Shangold GA, Fisher AC, Creasy GW. A comparative and pooled analysis of the safety and tolerability of the contraceptive patch (Ortho Evra/Evra). Fertility and Sterility 2002;77 Suppl 2:19‐26. [DOI] [PubMed] [Google Scholar]
Spellacy 1970 {published data only}
- Spellacy WN, Birk SA. The development of elevated blood pressure while using oral contraceptives: a preliminary report of a prospective study. Fertility and Sterility 1970;21:301‐6. [PubMed] [Google Scholar]
Spona 1996 {published and unpublished data}
- Spona J, Elstein M, Feichtinger W, Sullivan H, Ludicke F, Muller U, et al. Shorter pill‐free interval in combined oral contraceptives decreases follicular development. Contraception 1996;54:71‐7. [DOI] [PubMed] [Google Scholar]
Stewart 2005 {published data only}
- Stewart FH, Kaunitz AM, LaGuardia KD, Karvois DL, Fisher AC, Friedman AJ. Extended use of transdermal norelgestromin/ethinyl estradiol: a randomized trial. Obstetrics and Gynecology 2005;105:1389‐96. [DOI] [PubMed] [Google Scholar]
Teichmann 1995 {published and unpublished data}
- Teichmann AT, Brill K, Albring M, Schnitker J, Wojtynek P, Kustra E. The influence of the dose of ethinylestradiol in oral contraceptives on follicle growth. Gynecology and Endocrinology 1995;9:299‐305. [DOI] [PubMed] [Google Scholar]
Van der Does 1995 {published and unpublished data}
- Does J, Exalto N, Dieben T, Bennink HC. Ovarian activity suppression by two different low‐dose triphasic oral contraceptives. Contraception 1995;52:357‐61. [DOI] [PubMed] [Google Scholar]
Weisberg 1999 {published data only}
- Weisberg E, Fraser IS, Mishell DR, Lacarra M, Darney P, Jackanicz TM. A comparative study of two contraceptive vaginal rings releasing norethindrone acetate and differing doses of ethinyl estradiol. Contraception 1999;59:305‐10. [DOI] [PubMed] [Google Scholar]
Wiegratz 1995 {published and unpublished data}
- Wiegratz I, Jung‐Hoffman C, Kuhl H. Effect of two oral contraceptives containing ethinylestradiol and gestodene or norgestimate upon androgen parameters and serum binding proteins. Contraception 1995;51:341‐6. [DOI] [PubMed] [Google Scholar]
Wiegratz 2002 {published and unpublished data}
- Wiegratz I, Lee JH, Kutschera E, Bauer HH, Hayn C, Moore C, et al. Effect of dienogest‐containing oral contraceptives on lipid metabolism. Contraception 2002;65:223‐9. [DOI] [PubMed] [Google Scholar]
Wiik 1993 {published data only}
- Wiik P, Nordby J, Paulsen JE. Effect of norethisterone and levonorgestrel in low‐dose multiphasic oral contraceptives on serum lipids. Acta Obstetricia et Gynecologica Scandinavica 1993;72:550‐5. [DOI] [PubMed] [Google Scholar]
Winkler 1996 {published and unpublished data}
- Winkler UH, Schindler AE, Endrikat J, Dusterberg B. A comparative study of the effects of the hemostatic system of two monophasic gestodene oral contraceptives containing 20 micrograms and 30 micrograms ethinylestradiol. Contraception 1996;53:75‐84. [DOI] [PubMed] [Google Scholar]
Worsley 1980 {published data only}
- Worsley A. A prospective study of the effects of the progestagen content of oral contraceptives on measures of affect, automatization, and perceptual restructuring ability. Psychopharmacology (Berl) 1980;67:289‐96. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ahrendt 2009 {published data only}
- Ahrendt HJ, Makalova D, Parke S, Mellinger U, Mansour D. Bleeding pattern and cycle control with an estradiol‐based oral contraceptive: a seven‐cycle, randomized comparative trial of estradiol valerate/dienogest and ethinyl estradiol/levonorgestrel. Contraception. 2009/10/20 2009; Vol. 80, issue 5:436‐44. [DOI] [PubMed]
Bonny 2006 {published data only}
- Bonny AE, Ziegler J, Harvey R, Debanne SM, Secic M, Cromer BA. Weight gain in obese and nonobese adolescent girls initiating depot medroxyprogesterone, oral contraceptive pills, or no hormonal contraceptive method. Archives of Pediatrics & Adolescent Medicine 2006;160:40‐5. [DOI] [PubMed] [Google Scholar]
Boonyarangkul 2007 {published data only}
- Boonyarangkul A, Taneepanischskul S. Comparison of cycle contral and side effects between transdermal contraceptive patch and an oral contraceptive in women older than 35 years. Journal of the Medical Association of Thailand 2007;90:1715‐9. [PubMed] [Google Scholar]
Elkind‐Hirsch 2007 {published data only}
- Elkind‐Hirsch KE, Darensbourg C, Ogden B, Ogden LF, Hindelang P. Contraceptive vaginal ring use for women has less adverse metabolic effects than an oral contraceptive. Contraception 2007;76:348‐56. [DOI] [PubMed] [Google Scholar]
Endrikat 2007 {published data only}
- Endrikat J, Sandri M, Gerlinger C, Rubig A, Schmidt W, Fortier M. A Canadian multicentre prospective study on the effects of an oral contraceptive containing 3 mg drospirenone and 30 μg ethinyl oestradiol on somatic and psychological symptoms related to water retention and on body weight. European Journal of Contraception & Reproductive Health Care 2007;12:220‐8. [DOI] [PubMed] [Google Scholar]
Fan 2010 {published data only}
- Fan GS, Bian ML, Cheng LN, Cao XM, Huang ZR, Han ZY, et al. Efficacy and safety of drospirenone‐ethinylestradiol on contraception in healthy Chinese women: a multicenter randomized controlled trial [article in Chinese]. Zhonghua Fu Chan Ke Za Zhi 2009;44(1):38‐44. [PubMed] [Google Scholar]
- Fan GS, Bian ML, Cheng LN, Cao XM, Huang ZR, Han ZY, et al. Efficacy and safety of the combined oral contraceptive ethinylestradiol/drospirenone (Yasmin) in healthy Chinese women: a randomized, open‐label, controlled, multicentre trial. Clinical Drug Investigation. 2010/03/06 2010; Vol. 30, issue 6:387‐96. [DOI] [PubMed]
Gaspard 2003 {published data only}
- Gaspard U, Scheen A, Endrikat J, Buicu C, Lefebvre P, Gerlinger C, et al. A randomized study over 13 cycles to assess the influence of oral contraceptives containing ethinylestradiol combined with drospirenone or desogestrel on carbohydrate metabolism. Contraception 2003;67:423‐9. [DOI] [PubMed] [Google Scholar]
Grinspoon 2003 {published data only}
- Grinspoon SK, Friedman AJ, Miller KK, Lippman J, Olson WH, Warren MP. Effects of a triphasic combination oral contraceptive containing norgestimate/ethinyl estradiol on biochemical markers of bone metabolism in young women with osteopenia secondary to hypothalamic amenorrhea. Journal of Clinical Endocrinology and Metabolism 2003;88:3651‐6. [DOI] [PubMed] [Google Scholar]
Junge 2011 {published data only}
Machado 2006 {published data only}
- Machado RB, Tachotti F, Cavenague G, Maia E. Effects of two different oral contraceptives on total body water: a randomized study. Contraception 2006;73:344‐7. [DOI] [PubMed] [Google Scholar]
Miller 2003 {published data only}
- Miller L, Hughes JP. Continuous combination oral contraceptive pills to eliminate withdrawal bleeding: a randomized trial. Obstetrics and Gynecology 2003;101:653‐61. [DOI] [PubMed] [Google Scholar]
Miller 2005 {published data only}
- Miller L, Verhoeven CH, Hout J. Extended regimens of the contraceptive vaginal ring: a randomized trial. Obstetrics and Gynecology 2005;106:473‐82. [DOI] [PubMed] [Google Scholar]
Mohamed 2011 {published data only}
- Mohamed A M, El‐Sherbiny W S, Mostafa W A. Combined contraceptive ring versus combined oral contraceptive (30‐mug ethinylestradiol and 3‐mg drospirenone). International Journal of Gynaecology and Obstetrics 2011;114(2):145‐8. [DOI] [PubMed] [Google Scholar]
O'Connell 2005 {published data only}
- O'Connell KJ, Osborne LM, Westhoff C. Measured and reported weight change for women using a vaginal contraceptive ring vs. a low‐dose oral contraceptive. Contraception 2005;72:323‐7. [DOI] [PubMed] [Google Scholar]
- Westhoff C, Osborne LM, Schafer JE, Morroni C. Bleeding patterns after immediate initiation of an oral compared with a vaginal hormonal contraceptive. Obstetrics and Gynecology 2005;106:89‐96. [DOI] [PubMed] [Google Scholar]
O'Connell 2007 {published data only}
- O'Connell K, Davis AR, Kerns J. Oral contraceptives: side effects and depression in adolescent girls. Contraception 2007;75:299‐304. [DOI] [PubMed] [Google Scholar]
Sabatini 2006 {published data only}
- Sabatini R, Cagiano R. Comparison profiles of cycle control, side effects and sexual satisfaction of three hormonal contraceptives. Contraception 2006;74:220‐3. [DOI] [PubMed] [Google Scholar]
Sanam 2011 {published data only}
- Sanam M, Ziba O. Desogestrel+ethinylestradiol versus levonorgestrel+ethinylestradiol. Which one has better affect on acne, hirsutism, and weight change. Saudi Medical Journal 2011;32(1):23‐6. [PubMed] [Google Scholar]
Sangthawan 2005 {published data only}
- Sangthawan M, Taneepanichskul S. A comparative study of monophasic oral contraceptives containing either drospirenone 3 mg or levonorgestrel 150 µg on premenstrual symptoms. Contraception 2005;71:1‐7. [DOI] [PubMed] [Google Scholar]
Skouby 2005 {published data only}
- Skouby SO, Endrikat J, Dusterberg B, Schmidt W, Gerlinger C, Wessel J, et al. A 1‐year randomized study to evaluate the effects of a dose reduction in oral contraceptives on lipids and carbohydrate metabolism: 20 µg ethniyl estradiol combined with 100 µg levonorgestrel. Contraception 2005;71:111‐7. [DOI] [PubMed] [Google Scholar]
Suthipongse 2004 {published data only}
- Suthipongse W, Taneepanichskul S. An open‐label randomized comparative study of oral contraceptives between medications containing 3 µg drospirenone/30 µg ethinylestradiol and 150 µg levonogestrel/30 µg ethinylestradiol in Thai women. Contraception 2004;69:23‐6. [DOI] [PubMed] [Google Scholar]
Taneepanichskul 2002 {published data only}
- Taneepanichskul S, Kriengsinyot R, Jaisamrarn U. A comparison of cycle control, efficacy, and side effects among healthy Thai women between two low‐dose oral contraceptives containing 20 µg ethinylestradiol/75 µg gestodene (Meliane) and 30 µg ethinylestradiol/75 µg gestodene (Gynera). Contraception 2002;66:407‐9. [DOI] [PubMed] [Google Scholar]
Tantbirojn 2002 {published data only}
- Tantbirojn P, Taneepanichskul S. Clinical comparative study of oral contraceptives containing 30 µg ethinylestradiol/150 µg levonorgestrel, and 35 µg ethinylestradiol/250 µg norgestimate in Thai women. Contraception 2002;66:401‐5. [DOI] [PubMed] [Google Scholar]
Veres 2004 {published data only}
- Veres S, Miller L, Burington B. A comparison between the vaginal ring and oral contraceptives. Obstetrics and Gynecology 2004;104:555‐63. [DOI] [PubMed] [Google Scholar]
Westhoff 2007 {published data only}
- Westhoff C, Heartwell S, Edwards S, Zieman M, Cushman L, Robilotto C, et al. Initiation of oral contraceptives using a quick start compared with a conventional start. Obstetrics and Gynecology 2007;109:1270‐6. [DOI] [PubMed] [Google Scholar]
- Westhoff CL, Heartwell S, Edwards S, Zieman M, Stuart G, Cwiak C, et al. Oral contraceptive discontinuation: do side effects matter?. American Journal of Obstetrics and Gynecology 2007;196:412.e1‐6; discussion 412.e6‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Westhoff 2010 {published data only}
- Westhoff CL, Torgal AH, Mayeda ER, Stanczyk FZ, Lerner JP, Benn EK, et al. Ovarian suppression in normal‐weight and obese women during oral contraceptive use: a randomized controlled trial. Obstetrics and Gynecology 2010;116(2 Pt 1):275‐83. [DOI] [PubMed] [Google Scholar]
Westhoff 2012 {published data only}
- Westhoff C, Kaunitz AM, Korver T, Sommer W, Bahamondes L, Darney P, et al. Efficacy, safety, and tolerability of a monophasic oral contraceptive containing nomegestrol acetate and 17β‐estradiol: a randomized controlled trial. Obstetrics and Gynecology 2012;119(5):989‐99. [DOI] [PubMed] [Google Scholar]
Winkler 2004 {published data only}
- Winkler UH, Ferguson H, Mulders JAPA. Cycle control, quality of life and acne with two low‐dose oral contraceptives containing 20 µg ethinylestradiol. Contraception 2004;79:469‐76. [DOI] [PubMed] [Google Scholar]
Yildizhan 2009 {published data only}
- Yildizhan R, Yildizhan B, Adali E, Yoruk P, Birol F, Suer N. Effects of two combined oral contraceptives containing ethinyl estradiol 30 microg combined with either gestodene or drospirenone on hemostatic parameters, lipid profiles and blood pressure. Archives of Gynecology and Obstetrics. 2009/01/07 2009; Vol. 280, issue 2:255‐61. [DOI] [PubMed]
References to ongoing studies
Mahidol 2013 {published data only}
- Mahidol University. Comparison of body weight change during contraception with Belara and Yasmin. http://clinicaltrials.gov/show/NCT01608698 (accessed 05 Dec 2013).
Additional references
CONSORT 2009
- CONSORT group. CONSORT: Transparent reporting of trials. http://www.consort‐statement.org/ (accessed 15 Jul 2009).
Corvol 1983
- Corvol P, Elkik F, Feneant M, Oblin ME, Michaud A, Claire M, et al. Effect of progesterone and progestins on water and salt metabolism. In: CW Bardin, E Milgrom, P Mauvais‐Jarvis editor(s). Progesterone and Progestins. New York: Raven Press, 1983. [Google Scholar]
Emans 1987
- Emans SJ, Grace E, Woods ER, Smith DE, Kelin K, Merola J. Adolescents' compliance with the use of oral contraceptives. JAMA 1987;257:3377‐81. [PubMed] [Google Scholar]
Flegal 2000
- Flegal KM, Troiano RP. Changes in the distribution of body mass index of adults and children in the US population. International Journal of Obesity and Related Metabolic Disorders 2000;24:807‐18. [DOI] [PubMed] [Google Scholar]
Gaudet 2004
- Gaudet LM, Kives S, Hahn, Reid RL. What women believe about oral contraceptives and the effect of counseling. Contraception 2004;69:31‐6. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. The Cochrane Collaboration 2011; Vol. available from www.cochrane‐handbook.org.
IOM 1996
- Institute of Medicine. Contraceptive research and development: looking to the future. Washington, DC: National Academy Press, 1996. [Google Scholar]
Juni 2002
- Juni P, Holenstein F, Sterne J, Bartlett C, Egger M. Direction and impact of language bias in meta‐analyses of controlled trials: empirical study. International Journal of Epidemiology 2002;31:115‐23. [DOI] [PubMed] [Google Scholar]
Le 2003
- Le MG, Laveissiere MN, Pelissier C. Factors associated with weight gain in women using oral contraceptives: results of a French 2001 opinion poll survey conducted on 1665 women. Gynecologie, Obstetrique & Fertilite 2003;31:230‐9. [DOI] [PubMed] [Google Scholar]
Moher 2000
- Moher D, Pham B, Klassen TP, Schulz KF, Berlin JA, Jadad AR, et al. What contributions do languages other than English make on the results of meta‐analyses?. Journal of Clinical Epidemiology 2000;53:964‐72. [DOI] [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomized trials. Lancet 2001;357:1191‐4. [PubMed] [Google Scholar]
Nelson 2007
- Nelson AL. Combined oral contraceptives. In: Hatcher RA, Trussell J, Nelson AL, Cates W, Stewart FH, Kowal D, et al. editor(s). Contraceptive Technology. 19th Edition. New York: Ardent Media, Inc., 2007:193‐270. [Google Scholar]
Oddens 1999
- Oddens BJ. Women's satisfaction with birth control: a population survey of physical and psychological effects of oral contraceptives, intrauterine devices, condoms, natural family planning, and sterilization among 1466 women. Contraception 1999;59:277‐86. [DOI] [PubMed] [Google Scholar]
Rosenberg 1995
- Rosenberg MJ, Waugh MS, Meehan TE. Use and misuse of oral contraceptives: risk indicators for poor pill taking and discontinuation. Contraception 1995;51:283‐8. [DOI] [PubMed] [Google Scholar]
Rosenberg 1998
- Rosenberg M. Weight change with oral contraceptive use and during the menstrual cycle. Results of daily measurements. Contraception 1998;58:345‐9. [DOI] [PubMed] [Google Scholar]
Rothman 1998
- Rothman KJ, Greenland S. Approaches to statistical analysis. In: RJ Rothman, S Greenland editor(s). Modern Epidemiology. 2nd Edition. New York: Lippincott Williams and Wilkins, 1998:183‐99. [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
Schulz 2002a
- Schulz KF, Grimes DA. Allocation concealment in randomised trials: defending against deciphering. Lancet 2002;359:614‐700. [DOI] [PubMed] [Google Scholar]
Schulz 2002b
- Schulz KF, Grimes DA. Blinding in randomised trials: hiding who got what. Lancet 2002;359:696‐700. [DOI] [PubMed] [Google Scholar]
Turner 1994
- Turner R. Most British women use reliable contraceptive methods, but many fear health risks from use. Family Planning Perspectives 1994;26:183‐4. [Google Scholar]
Weiss 1998
- Weiss NS. Clinical epidemiology. In: RJ Rothman, S Greenland editor(s). Modern Epidemiology. 2nd Edition. New York: Lippincott Williams and Wilkins, 1998:519‐28. [Google Scholar]
Wysocki 2000
- Wysocki S. A survey of American women regarding the use of oral contraceptives and weight gain [abstract]. International Journal of Gynecology and Obstetrics 2000; Vol. 70:114.
References to other published versions of this review
Gallo 2004
- Gallo M, Grimes D, Schulz K, Helmerhorst F. Combination contraceptives: effects on weight. Obstetrics and Gynecology 2004;103:359‐73. [DOI] [PubMed] [Google Scholar]


