Abstract
Background
Artificial intelligence (AI) has demonstrated significant potential in supporting emergency medical services personnel during out-of-hospital cardiac arrest (OHCA) care; however, the extent of research evaluating this topic is unknown. This scoping review examines the breadth of literature on the application of AI in early OHCA care.
Methods
We conducted a search of PubMed®, Embase, and Web of Science in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews guidelines. Articles focused on non-traumatic OHCA and published prior to January 18th, 2023 were included. Studies were excluded if they did not use an AI intervention (including machine learning, deep learning, or natural language processing), or did not utilize data from the prehospital phase of care.
Results
Of 173 unique articles identified, 54 (31%) were included after screening. Of these studies, 15 (28%) were from the year 2022 and with an increasing trend annually starting in 2019. The majority were carried out by multinational collaborations (20/54, 38%) with additional studies from the United States (10/54, 19%), Korea (5/54, 10%), and Spain (3/54, 6%). Studies were classified into three major categories including ECG waveform classification and outcome prediction (24/54, 44%), early dispatch-level detection and outcome prediction (7/54, 13%), return of spontaneous circulation and survival outcome prediction (15/54, 20%), and other (9/54, 16%). All but one study had a retrospective design.
Conclusions
A small but growing body of literature exists describing the use of AI to augment early OHCA care.
Keywords: Out-of-hospital cardiac arrest, Prehospital care, Emergency medical services, Medical dispatch, Artificial intelligence, Machine learning, Deep learning
Introduction
Over 250,000 people are treated by emergency medical services (EMS) for out-of-hospital cardiac arrest (OHCA) annually in the United States.1 While the incidence of successful prehospital return of spontaneous circulation (ROSC) has been reported at approximately 27%, the chances of survival are low at around 9% and 7% for survival to hospital discharge and neurologically intact survival, respectively.1 Despite significant research into prehospital resuscitation, survival outcomes after OHCA have remained low.2
The role of artificial intelligence (AI), including machine learning (ML), deep learning (DL), and natural language processing (NLP), as decision-support for EMS personnel in the management of OHCA is rapidly evolving. In the dynamic out-of-hospital setting where critical management decisions must be based off limited information, AI may assist EMS clinicians in quickly and objectively synthesizing patient data to guide care. Prior studies have demonstrated the feasibility of AI in assisting dispatchers in the early recognition of OHCA, and EMS clinicians and emergency department (ED) physicians in OHCA prognostication based solely on prehospital factors. To date, little research has evaluated the literature scope pertaining to the use of AI in emergency care3 and in cardiac arrest care4, 5, and no studies have mapped the extent of literature on the use of AI as decision-support in the prehospital OHCA management.
We aimed to perform a scoping review on the use of AI as decision-support for OHCA management in the prehospital and early phases of care. The intent of this review is to inform EMS clinicians, physicians, and researchers on the current scope of literature on the use of AI as decision-support in early OHCA care.
Methods
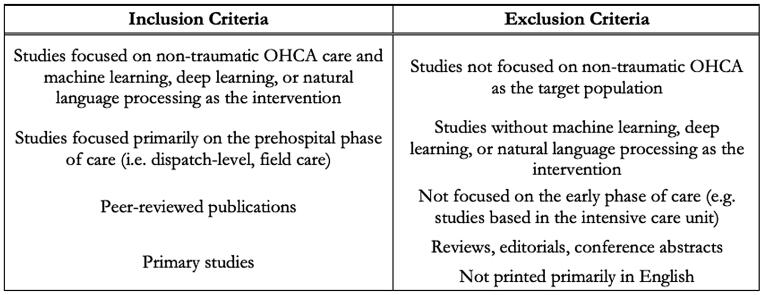
We performed a search of peer-reviewed articles indexed in Embase, PubMed®, and Web of Science on January 18th, 2023. Articles published up to the search date were eligible for inclusion. Key search terms included ‘artificial intelligence’, ‘machine learning’, ‘deep learning’, ‘natural language processing’, and ‘out-of-hospital cardiac arrest’ (Fig. 1). After removal of duplicate publications, a single investigator (J.T.) who is an emergency medicine physician specializing in EMS screened titles and abstracts for relevancy based on predefined criterion (Supplementary Fig. 1). Selected articles underwent full-text screening. We conducted this review in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews guidelines (See Fig. 2 for PRISMA checklist).6
Fig. 1.
Inclusion/exclusion criteria.
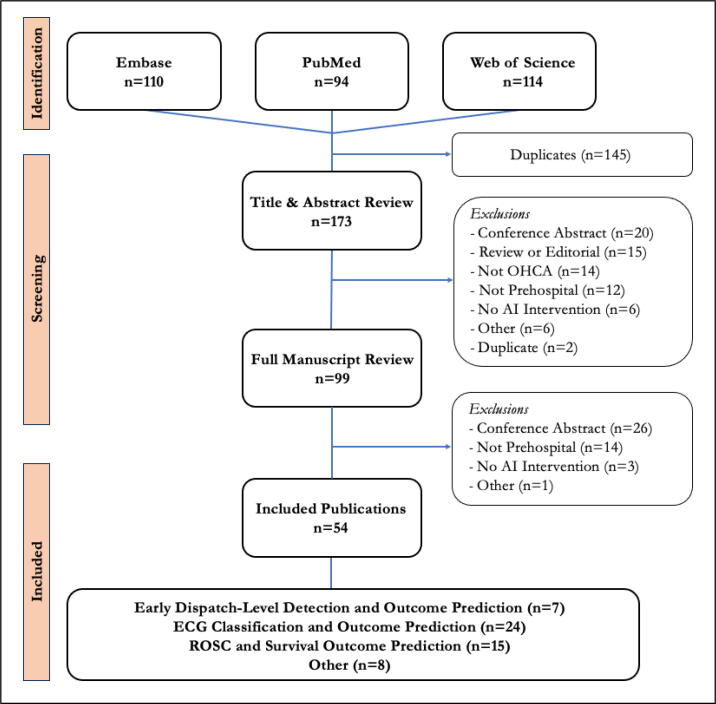
Fig. 2.
Selection Flow Chart. AI = artificial intelligence, ECG = electrocardiogram, OHCA = out of hospital cardiac arrest, ROSC = return of spontaneous circulation.
Studies were included if they used subsets of AI including ML, DL, or NLP as decision-support in the early phases of non-traumatic OHCA care. ML requires the input of structured data and learns in a supervised or unsupervised manner to make predictions. DL, a subset of ML, automatically inputs structured or raw data into multiple layers known as neural networks to organize and classify information and output predictions. Both ML and DL frameworks utilize classification algorithms of varying complexity (i.e., random forest, convolutional neural networks) to recognize, understand, and group data elements into categories which can then be interpreted by a human operator. NLP refers to the ability of a computer to understand and interpret text or spoken human language.
The search focused on peer-reviewed, primary studies published in academic journals. Studies were restricted to those published in the English language and based on human subject research. Studies were excluded if they did not restrict the patient population to non-traumatic OHCA, did not include ML, DL, and/or NLP as the AI intervention, or did not utilize input data from the prehospital setting or data obtained immediately upon arrival to the ED. Of note, studies utilizing non-prehospital data that are applicable and could be easily collected in the prehospital setting were included (i.e., electrocardiogram [ECG] waveform data). Conference abstracts, review articles, editorials, and gray literature were excluded.
Studies were filed into the citation-manager Zotero (Version 6.0.23; Corporation for Digital Scholarship, Vienna, Virginia, USA) and data were extracted by a single investigator (J.T.) into an Excel spreadsheet (Version 16.66.1; Microsoft Corp, Redmond Washington, USA). We extracted year, country of origin, AI branch (i.e., ML, DL, or NLP), classification algorithm (i.e., random forest, support vector machine), number of input predictors, data input type (i.e., clinical variables, ECG segment), database used, database size, and primary study outcomes. Country of origin was defined as the country were the authors declared their institutional affiliation. The category ‘Multinational Collaboration’ was created for studies with authors from two or more countries. We summarized descriptive statistics as frequencies and percentages. No personal or individual identifiers of human study subjects was retrieved in this literature review.
Results
The initial search yielded 318 total articles (Fig. 2). After removal of duplicate publications, 173 articles remained. After screening of titles and abstracts, 99 articles remained. Full manuscript review yielded 54 (31%) articles for inclusion.
Overall study characteristics
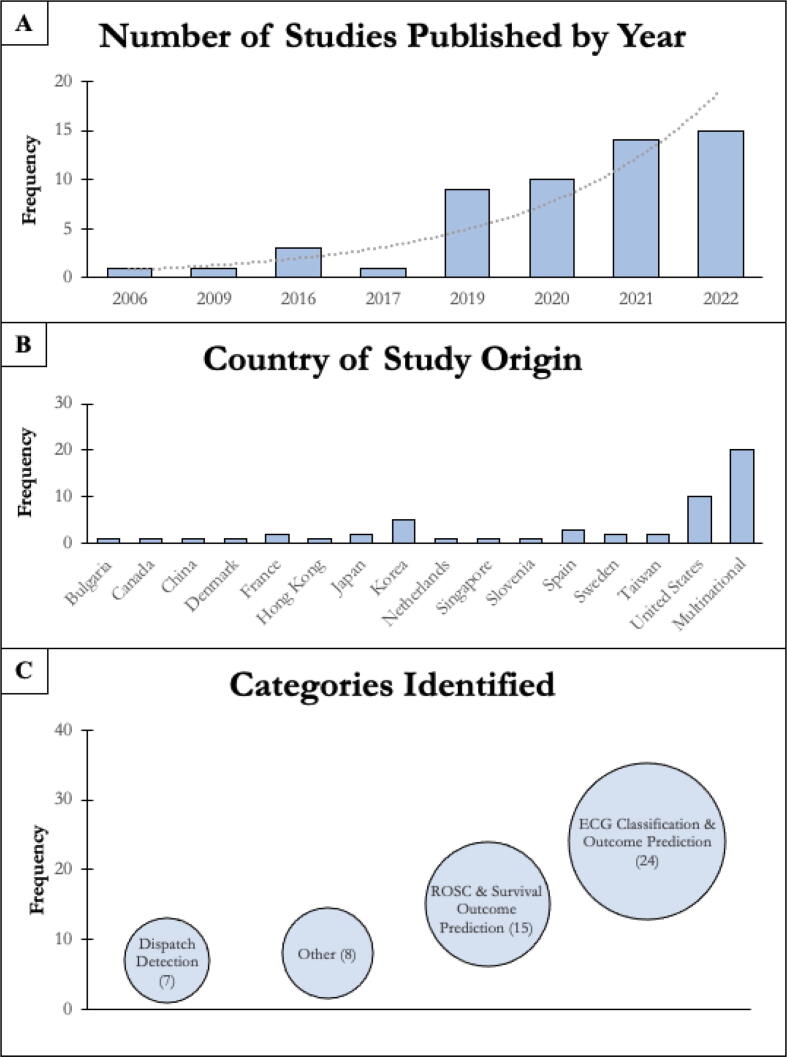
Of 54 included studies (Fig. 3), 15 (28%) were from the year 2022 and there was an annual increase in publications starting in 2019. The majority of studies were carried out by multinational collaborations (20/54, 38%), with additional studies from the United States (10/54, 19%), Korea (5/54, 10%), and Spain (3/54, 6%). We classified studies into four main categories based on their use of AI including ECG waveform classification and outcome prediction (24/54, 44%), early dispatch-level detection and outcome prediction (7/54, 13%), return of spontaneous circulation (ROSC) and/or survival outcome prediction (15/54, 20%), and other uses (9/54, 16%). All studies had a retrospective design except one by Blomberg et al.7 See Table 3 for study list.
Fig. 3.
Characteristics of all included studies in this scoping review. *A) Studies from the year 2023 were omitted. ECG = electrocardiogram; ROSC = return of spontaneous circulation.
Table 3.
Studies included in this scoping review (n = 54).
| Category | Title | Primary Author & Year | Country of Origin | Study Design | AI branch | Data Source |
|---|---|---|---|---|---|---|
| Dispatch | Machine learning as a supportive tool to recognize cardiac arrest in emergency calls | Blomberg et al. 2019 | Denmark, United States | Retrospective Observational | ML | Dispatch Audio |
| Dispatch | Effect of Machine Learning on Dispatcher Recognition of Out-of-Hospital Cardiac Arrest During Calls to Emergency Medical Services: A Randomized Clinical Trial | Blomberg et al. 2021 | Denmark, United States | Randomized Clinical Trial | ML | Dispatch Audio |
| Dispatch | Machine learning can support dispatchers to better and faster recognize out-of-hospital cardiac arrest during emergency calls: A retrospective study | Byrsell et al. 2021 | Sweden | Retrospective Observational | ML, DL | Dispatch Audio |
| Dispatch | Early recognition of a caller’s emotion in out-ofhospital cardiac arrest dispatching: An artificial intelligence approach | Chin et al. 2021 | Taiwan | Retrospective Observational | ML | Dispatch Audio |
| Dispatch | Privacy-Preserving Prediction of Victim's Mortality and Their Need for Transportation to Health Facilities | Arcolezi et al. 2022 | France | Retrospective Observational | ML, DL | Dispatch Audio |
| Dispatch | Out-of-Hospital Cardiac Arrest Detection by Machine Learning Based on the Phonetic Characteristics of the Caller's Voice. | Rafi et al. 2022 | France | Retrospective Observational | ML, DL | Dispatch Audio |
| Dispatch | When the machine is wrong. Characteristics of true and false predictions of Out-of-Hospital Cardiac Arrests in Emergency Calls using a machine-learning model | Blomberg et al. 2023 | Denmark | Retrospective Observational | ML | Dispatch Audio |
| ECG | A method to predict ventricular fibrillation shock outcome during chest compressions | Coult et al. 2021 | United States | Retrospective Observational | ML | ECG Waveform, Thoracic impedance |
| ECG | Ventricular Fibrillation Waveform Analysis During Chest Compressions to Predict Survival From Cardiac Arrest | Coult et al. 2019 | United States | Retrospective Observational | ML | ECG Waveform, Thoracic impedance, Clinical Variables |
| ECG | Towards the Prediction of Rearrest during Out-of-Hospital Cardiac Arrest | Elola et al. 2020 | Spain, United States | Retrospective Observational | ML | ECG Waveform |
| ECG | Multimodal Algorithms for the Classification of Circulation States During Out-of-Hospital Cardiac Arrest | Elola et al. 2020 | Spain, Norway | Retrospective Observational | ML | ECG Waveform, Thoracic impedance, EtCO2 |
| ECG | Capnography: A support tool for the detection of return of spontaneous circulation in out-of-hospital cardiac arrest | Elola et al. 2019 | Spain, China, United States | Retrospective Observational | ML | ECG Waveform, Thoracic impedance |
| ECG | Deep Neural Networks for ECG-Based Pulse Detection during Out-of-Hospital Cardiac Arrest | Elola et al. 2019 | Spain, United States | Retrospective Observational | DL | ECG Waveform, Thoracic impedance, EtCO2 |
| ECG | Machine Learning Techniques for the Detection of Shockable Rhythms in Automated External Defibrillators | Figuera et al. 2016 | Spain, Norway | Retrospective Observational | ML | ECG Waveform |
| ECG | Enhancing the accuracy of shock advisory algorithms in automated external defibrillators during ongoing cardiopulmonary resuscitation using a deep convolutional Encoder-Decoder filtering model | Hajeb et al. 2022 | United States | Retrospective Observational | DL | ECG Waveform |
| ECG | Deep Neural Network Approach for Continuous ECG-Based Automated External Defibrillator Shock Advisory System During Cardiopulmonary Resuscitation. | Hajeb et al. 2021 | United States | Retrospective Observational | DL | ECG Waveform |
| ECG | Combining Amplitude Spectrum Area with Previous Shock Information Using Neural Networks Improves Prediction Performance of Defibrillation Outcome for Subsequent Shocks in Out-Of-Hospital Cardiac Arrest Patients. | He et al. 2016 | China | Retrospective Observational | DL | ECG Waveform |
| ECG | Rhythm Analysis during Cardiopulmonary Resuscitation Using Convolutional Neural Networks. | Isasi et al. 2020 | Spain, Norway | Retrospective Observational | DL | ECG Waveform, Thoracic impedance |
| ECG | Shock decision algorithm for use during load distributing band cardiopulmonary resuscitation | Isasi et al. 2021 | Spain, Norway | Retrospective Observational | ML | ECG Waveform, Thoracic impedance |
| ECG | ECG derived feature combination versus single feature in predicting defibrillation success in out-of-hospital cardiac arrested patients | Ivanovic et al. 2019 | Serbia, Germany, Italy | Retrospective Observational | ML | ECG Waveform |
| ECG | Predicting defibrillation success in out-of-hospital cardiac arrested patients: Moving beyond feature design | Ivanovic et al. 2020 | Serbia, Germany, Italy | Retrospective Observational | ML | ECG Waveform |
| ECG | Shock Decision Algorithms for Automated External Defibrillators Based on Convolutional Networks | Jaureguibeitia et al. 2020 | Spain | Retrospective Observational | DL | ECG Waveform, Thoracic impedance |
| ECG | Optimization of End-to-End Convolutional Neural Networks for Analysis of Out-of-Hospital Cardiac Arrest Rhythms during Cardiopulmonary Resuscitation. | Jekova & Krasteva 2021 | Bulgaria | Retrospective Observational | DL | ECG Waveform |
| ECG | Fully Convolutional Deep Neural Networks with Optimized Hyperparameters for Detection of Shockable and Non-Shockable Rhythms. | Krasteva et al. 2020 | Bulgaria, France | Retrospective Observational | DL | ECG Waveform |
| ECG | Prediction of countershock success using single features from multiple ventricular fibrillation frequency bands and feature combinations using neural networks | Neurauter et al. 2006 | Austria, Norway, United States | Retrospective Observational | DL | ECG Waveform |
| ECG | Mixed convolutional and long short-term memory network for the detection of lethal ventricular arrhythmia. | Picon et al. 2019 | Spain | Retrospective Observational | ML, DL | ECG Waveform |
| ECG | ECG-Based Classification of Resuscitation Cardiac Rhythms for Retrospective Data Analysis | Rad et al. 2017 | Spain, Norway, United States | Retrospective Observational | ML | ECG Waveform |
| ECG | Machine learning and feature engineering for predicting pulse presence during chest compressions | Sashidhar et al. 2021 | United States | Retrospective Observational | ML | ECG Waveform, Thoracic impedance |
| ECG | Integration of attributes from non-linear characterization of cardiovascular time-series for prediction of defibrillation outcomes | Shandilya et al. 2016 | United States | Retrospective Observational | ML | ECG Waveform. EtCO2 |
| ECG | Pilot study on VF-waveform based algorithms for early detection of acute myocardial infarction during out-of-hospital cardiac arrest | Thannhauser et al. 2022 | Netherlands | Retrospective Observational | ML | ECG Waveform |
| ECG | A Machine Learning Model for the Prognosis of Pulseless Electrical Activity during Out-of-Hospital Cardiac Arrest. | Urteaga et al. 2021 | Spain, United States | Retrospective Observational | ML | ECG Waveform, Thoracic impedance |
| Other | Machine Learning Analysis to Identify Data Entry Errors in Prehospital Patient Care Reports: A Case Study of a National Out-of-Hospital Cardiac Arrest Registry. | Choi et al. 2022 | Korea | Retrospective Observational | ML, NLP | Clinical Variables |
| Other | Machine learning-based dispatch of drone-delivered defibrillators for out-of-hospital cardiac arrest. | Chu et al. 2020 | Canada | Retrospective Observational | ML | Other |
| Other | Identification of Factors Associated with Return of Spontaneous Circulation after Pediatric Out-of-Hospital Cardiac Arrest Using Natural Language Processing | Harris et al. 2022 | United States | Retrospective Observational | NLP | Clinical Variables |
| Other | Racial and Socioeconomic Disparities in Out-Of-Hospital Cardiac Arrest Outcomes: Artificial Intelligence-Augmented Propensity Score and Geospatial Cohort Analysis of 3,952 Patients. | Monlezun et al. 2021 | United States | Retrospective Observational | ML | Demographic Variables |
| Other | Identification of out-of-hospital cardiac arrest clusters using unsupervised learning. | Moon et al.2022 | Korea | Retrospective Observational | ML | Other |
| Other | Machine learning model for predicting out-of-hospital cardiac arrests using meteorological and chronological data | Nakashima et al. 2020 | United States, Japan | Retrospective Observational | ML | Other |
| Other | Association between type of bystander cardiopulmonary resuscitation and survival in out-of-hospital cardiac arrest: A machine learning study | Jerkeman et al. 2022 | Sweden | Retrospective Observational | ML | Clinical Variables |
| Other | Can a voice assistant help bystanders save lives? A feasibility pilot study chatbot in beta version to assist OHCA bystanders. | Otero-Agra et al. 2022 | Spain | Retrospective Observational | ML, DL | Other |
| ROSC Prediction | Prediction of ROSC After Cardiac Arrest Using Machine Learning | Liu et al. 2020 | Singapore, Taiwan, Thailand, Korea, Japan, United Arab Emirates | Retrospective Observational | ML | Clinical Variables |
| ROSC Prediction | Development and validation of an interpretable prehospital return of spontaneous circulation (P-ROSC) score for patients with out-of-hospital cardiac arrest using machine learning: A retrospective study | Liu et al. 2022 | Singapore, Korea, Taiwan, Japan | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction | Identifying the relative importance of predictors of survival in out of hospital cardiac arrest: a machine learning study | Al-Dury et al. 2020 | Sweden, Norway | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction | A machine learning approach for modeling decisions in the out of hospital cardiac arrest care workflow. | Harford et al.2022 | United States | Retrospective Observational | ML, DL | Clinical Variables |
| Survival Prediction | A machine learning based model for Out of Hospital cardiac arrest outcome classification and sensitivity analysis. | Harford et al.2019 | United States | Retrospective Observational | ML, DL | Clinical Variables |
| Survival Prediction | Early outcome prediction for out-of-hospital cardiac arrest with initial shockable rhythm using machine learning models. | Hirano et al. 2021 | Japan | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction | Visual assessment of interactions among resuscitation activity factors in out-of-hospital cardiopulmonary arrest using amachine learning model | Kawai2022 | Japan | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction | Developing a Time-Adaptive Prediction Model for Out-of-Hospital Cardiac Arrest: Nationwide Cohort Study in Korea. | Kim et al. 2021 | Korea, United States | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction | Deep-learning-based out-of-hospital cardiac arrest prognostic system to predict clinical outcomes | Kwon et al.2019 | Korea | Retrospective Observational | ML, DL | Clinical Variables |
| Survival Prediction | Tree-Based Algorithms and Association Rule Mining for Predicting Patients’ Neurological Outcomes After First-Aid Treatment for an Out-of-Hospital Cardiac Arrest During COVID-19 Pandemic: Application of Data Mining | Lin et al. 2022 | Taiwan | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction | Predicting Survived Events in Nontraumatic Out-of-Hospital Cardiac Arrest: A Comparison Study on Machine Learning and Regression Models | Lo & Siu2021 | Hong Kong | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction | Prediction of Neurologically Intact Survival in Cardiac Arrest Patients without Pre-Hospital Return of Spontaneous Circulation: Machine Learning Approach | Seo et al. 2021 | Korea | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction | Development and validation of the SARICA score to predict survival after return of spontaneous circulation in out of hospital cardiac arrest using an interpretable machine learning framework. | Wong et al. 2022 | Singapore | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction/ROSC | Intelligent analysis in predicting outcome of out-of-hospital cardiac arrest | Krizmaric et al. 2009 | Slovenia | Retrospective Observational | ML | Clinical Variables |
| Survival Prediction/ROSC | Evaluation of optimal scene time interval for out-of-hospital cardiac arrest using a deep neural network. | Shin et al. 2023 | Korea | Retrospective Observational | ML, DL | Clinical Variables |
ROSC and survival outcome prediction
Fifteen studies were identified that used AI for ROSC and survival outcome prediction (Table 1). The majority were from 2022 (5/15, 34%)8, 9, 10, 11, 12 and all but one were published in the past five years. Most studies were carried out by multinational collaborations (4/15, 27%)12, 13, 14, 15 and from Korea (3/15, 20%)16, 17, 18, Japan (2/15, 14%)9, 19, and the United States (2/15, 14%)8, 20. Eleven studies (73%) focused on survival prediction13, 14, 8, 9, 10, 11, 17, 18, 19, 20, 21, two studies (13%) focused on ROSC prediction12, 15, and two studies (13%) focused on both16, 22. Most studies excluded patients < 18 years of age or did not specify an age cutoff, while a single study by Al-Dury et al.13 explicitly included both adults and children. The number of patients included in each study ranged from 194 to 170,678 with the majority of studies including > 5,000 patients from large OHCA databases.
Table 1.
Characteristics of studies aimed at prediction of return of spontaneous circulation outcomes and survival. ROSC = return of spontaneous circulation.
|
Prediction of ROSC and Survival (n = 15) | |
|---|---|
| Dates | Frequency (%) |
| 2023 | 1 (7) |
| 2022 | 5 (34) |
| 2021 | 4 (27) |
| 2020 | 2 (14) |
| 2019 | 2 (14) |
| 2009 | 1 (7) |
| Country of Study Origin | |
| Hong Kong | 1 (7) |
| Japan | 2 (14) |
| Korea | 3 (20) |
| Singapore | 1 (7) |
| Slovenia | 1 (7) |
| Taiwan | 1 (7) |
| United States | 2 (14) |
| Multinational Collaboration | 4 (27) |
| Patient Demographic | |
| Adults (<18 years) | 10 (67) |
| Adults & Pediatrics | 1 (7) |
| Not Specified | 4 (27) |
| AI Branch | |
| Machine Learning | 11 |
| Machine Learning & Deep Learning | 4 |
| Classification Algorithm | |
| Artificial Neural Networks | 1 |
| Autoscore | 2 |
| Classification and Regression Tree | 1 |
| Decision Tree | 4 |
| Deep Neural Networks | 2 |
| Embedded Fully Convolutional Network | 2 |
| Gradient Boosting | 2 |
| K-Nearest Neighbor | 5 |
| Lagrangian Support Vector Machine | 1 |
| LightGBM | 4 |
| Logistic Regression | 7 |
| Multilayer Perceptron | 3 |
| Naïve Bayes | 1 |
| Neural Networks | 1 |
| Random Forest | 15 |
| Reduced Support Vector Machine | 1 |
| Regularized Logistic Regression | 1 |
| Support Vector Machine | 6 |
| Voting Classifier | 1 |
| XGBoost | 4 |
Among studies with models aimed at predicting survival and/or ROSC, eleven utilized ML17, 19, 9, 10, 11, 13, 14, 15, 21, 22, 23 and four used both ML and DL8, 16, 18, 20. All of these studies utilized a random forest classification algorithm as one type of the ML classification algorithms and additional ML and DL classification methods included logistic regression8, 9, 16, 18, 19, 20, 21, support vector machine9, 18, 19, 20, 22, k-nearest neighbor8, 9, 16, 20, 22, decision tree8, 9, 16, 20, light gradient boosted machine (LightGBM)8, 9, 14, 20, extreme gradient boosting (XGboost)8, 9, 17, 20, multilayer perceptron18, 19, 21, Autoscore10, 15, deep neural networks8, 20, embedded fully convolutional network8, 20, gradient boosting8, 20, artificial neural networks14, classification and regression tree11, Lagrangian support vector machine16, naïve bayes22, neural networks22, reduced support vector machine16, regularized logistic regression17, and voting classifier17. All studies utilized more than one classification algorithm with the exception of one study by Liu et al.15 which used a single ML classification algorithm (random forest) and compared it to an existing prediction score.
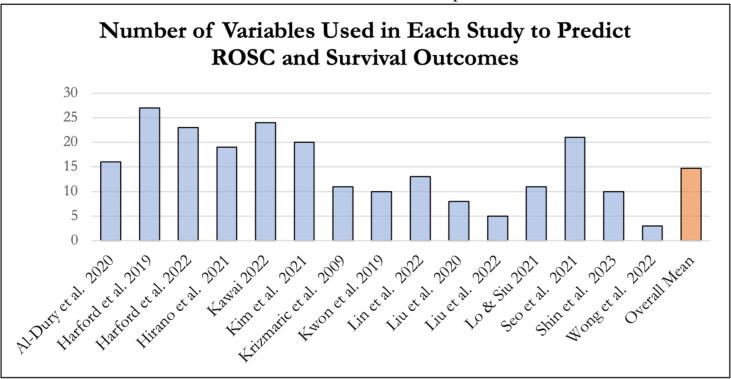
The number of predictors utilized in the various classification algorithms employed by each study to predict ROSC and survival ranged from three to 27 with an overall mean of 14.7 (Fig. 4). In these studies, 12 of 15 models12, 13, 8, 9, 10, 15, 16, 17, 19, 20, 21, 22 utilized only predictors from the prehospital setting, while the remaining three models12, 14, 18 also incorporated one to two predictor variables obtained upon ED arrival including initial ED vitals, initial ED ECG, consciousness level upon ED arrival, and time from ED arrival to ROSC.
Fig. 4.
Number of inputted variables used in each study to predict return of spontaneous circulation and survival outcomes. ROSC = return of spontaneous circulation.
Early dispatch-level detection and outcome prediction
Seven studies were identified that used AI for the early detection of OHCA and outcome prediction at the dispatch-level from audio-based input (Table 2). All were published in the past five years. The studies were conducted by investigators in multinational collaborations (2/7, 29%)22, 28, France (2/7, 29%)24, 25, with additional studies from Denmark26, Sweden27, and Taiwan28. Four studies7, 26, 27, 29 focused on the early detection of OHCA based on linguistic (e.g., spoken words) features in the dispatch-call audio while Rafi et al.24 focused on the phonetic (e.g., vocal acoustic characteristics) features of the callers voice in the dispatch-call audio. Chin et al.28 characterized callers’ emotional state during dispatch calls for OHCA and Arcolezi et al.25 predicted the need for transport and mortality outcomes from the dispatch call audio. The exact number and types of inputted predictors varied greatly and/or were not well described in these studies. One study by Blomberg et al.7 was a randomized controlled trial while the remaining were of retrospective observational design. The number of audio calls analyzed in each study ranged from 337 to 169,236 with the majority obtaining call audio from large, regional OHCA databases.
Table 2.
Characteristics of studies aimed at the early dispatch-level detection of out-of-hospital cardiac arrest and outcome prediction.
|
Early Dispatch-level Detection and Outcome Prediction for OHCA (n = 7) | |
|---|---|
| Year | Frequency (%) |
| 2023 | 1 (15) |
| 2022 | 2 (29) |
| 2021 | 3 (43) |
| 2019 | 1 (15) |
| Country of Study Origin | |
| Denmark | 1 (15) |
| France | 2 (29) |
| Sweden | 1 (15) |
| Taiwan | 1 (15) |
| Multinational Collaboration | 2 (29) |
| Patient Demographic | |
| Adults & Pediatrics | 7 (100) |
| AI Branch | |
| Machine Learning | 4 |
| Machine Learning & Deep Learning | 3 |
| Classification Algorithm | |
| Attentive Interpretable Tabular Learning | 1 |
| Automatic speech recognition | 1 |
| Binary logistic regression | 1 |
| Convolutional Neural Network | 1 |
| LightGBM | 1 |
| Neural network | 1 |
| Random forest | 1 |
| XGBoost | 1 |
| Not specified | 4 |
Among these dispatch-level studies, four utilized ML7, 26, 28, 29 and three employed both ML and DL24, 25, 27. ML and DL classification algorithms included attentive interpretable tabular learning (TabNet)25, automatic speech recognition27, binary logistic regression24, convolutional neural network24, lightGBM25, Neural network24, Random forest24, XGBoost25. Four studies did not describe the specific classification algorithm used.7, 26, 28, 29
Electrocardiogram waveform classification and prediction of outcomes
Twenty-four studies were identified that used AI for ECG waveform classification in OHCA and outcome prediction. The majority were published in the past five years and five from prior years. The majority were carried out through collaborations between multinational groups in Europe and the United States utilizing ECG waveform data from multicenter databases. Among these studies, six (25%) aimed to predict defibrillation outcomes in ventricular fibrillation (VF)30, 31, 32, 33, 34, 35, five (21%) focused on rhythm classification36, 37, 38, 39, 40, five (21%) developed algorithms to advise defibrillation versus no defibrillation41, 42, 43, 44, 45, four (17%) focused specific on the classification of pulseless electrical activity (PEA) (i.e., PEA vs pseudo-PEA vs pulsed rhythm, or favorable-PEA vs non-favorable-PEA)46, 47, 48, 49, two (8%) aimed to predict survival outcomes30, 50 and two (8%) aimed to suppress CPR artifact to improve ECG segment analysis36, 37. Additional studies aimed to develop ECG based classification algorithms to predict rearrest in the immediate post-ROSC period51, predict the presence of a pulse during CPR52, and predict myocardial infarction/acute coronary artery occlusion during CPR53
Among the studies of ECG segment analysis, fourteen used ML35, 36, 30, 31, 32, 38, 39, 40, 47, 48, 49, 50, 51, 52, nine used DL33, 34, 37, 38, 41, 42, 43, 44, 45, 46, and one used both ML and DL38. All studies utilized ECG waveform characteristics (i.e., VF amplitude/frequency, QRS size/amplitude) obtained from manual defibrillators, automated external defibrillators, and/or Holter monitors. Several studies additionally utilized thoracic impedance data30, 36, 42, 43, 47, 48, 49, 50, 51, 52 obtained from the manual defibrillator and end tidal carbon monoxide values35, 48, 49. Coult et al.50 also added clinical variables including age (<60 or ≥60 years) and sex. The analyzed ECG segments ranged from 1-second to greater than 40-seconds and were primarily segments from continuous ECG waveform captured during OHCA resuscitation (10/24, 42%)36, 37, 40, 41, 42, 43, 44, 45. Other studies analyzed more specific ECG segments including VF segments before and after defibrillator (9/24, 38%)38, 50, 31, 32, 33, 34, 35, pulseless electrical activity (PEA) segments (4/24, 17%)46, 47, 48, 49, and immediate post-ROSC ECG segments (1/24, 4%)51
Other
Eight studies were identified that utilized AI to augment other aspects OHCA care. Three of these studies described their use of ML for spatial and temporal OHCA cluster detection and outcome prediction using clinical, demographic, or environmental factors.54, 55, 56 Three retrospective studies employed ML to analyze OHCA patient care reports to evaluate data integrity and predict outcomes, one of which also used NLP.57, 58, 59 Finally, two studies described the use of ML and DL to augment the lay rescuer and prehospital response to OHCA including chatbots to guide lay rescuer OHCA response60 and the use of drones to deliver automated external defibrillators61
Discussion
To date, there is a small but growing body of research evaluating the AI to support dispatchers, EMS clinicians, and physicians in OHCA care. The number of published studies detailing the feasibility and potential applications of AI have steadily increased since 2019. To our knowledge, we are the first to have evaluated the scope of literature on AI as decision-support in early OHCA resuscitation. We identified three main categories of studies that use AI to detect and predict outcomes in OHCA care: early dispatch-level detection of OHCA, prediction of ROSC and/or survival, and ECG waveform classification. In the prehospital setting where the dynamic nature requires rapid gathering and interpretation of limited information, harnessing the power of AI to quickly analyze data and predict outcomes may enhance our ability to deliver the most effective OHCA care.
The prediction of ROSC and survival early in the care continuum has the potential to guide resuscitation decisions for OHCA patients; yet accurate outcome prediction based on limited prehospital data represents a major challenge. In this scoping review, most of the studies evaluated the performance of different AI classification algorithms to predict the binary outcome(s) of survival and/or neurologically intact survival. The majority of studies compared the predictive performance of multiple different ML or DL classification algorithms. Two different studies by Liu et al. additionally compared a single ML classification algorithm to previously validated predictive models based on standard logistic regression including the ROSC After Cardiac Arrest score (RACA) and Utstein reporting-based ROSC score (UB-ROSC).12, 15 Kim et al. developed a time-adaptive ML algorithm to predict percent survival and neurologically intact survival minute-by-minute for OHCA patients up to 60 minutes.14
When assessing factors in each study predicting ROSC and survival, there was significant heterogeneity. While some studies included as few as three predictors, others included as many as 27. Other studies utilized data available at the time of ambulance arrival while further studies included data up to the time of care transfer to ED staff. Al-Dury et al.13 evaluated the relative importance of factors for predicting survival present at the time of ambulance arrival and found that initial rhythm (most important), age, time to CPR initiation, EMS response time, and location of cardiac arrest were the top five most important. Lin et al.11 assessed the relative importance of factors available during the entire out-of-hospital course and upon ED arrival and found that prehospital ROSC, age, EMS response time, scene time, and transport time were the five most important factors, with prehospital ROSC being the most important. Overall, the use of AI to prognosticate outcomes at different time points may benefit different care teams including EMS providers (i.e., informing transport or field termination of resuscitation ) and ED physicians (i.e., informing the length of additional resuscitation or care discussions with families).
Despite the growing number of studies evaluating AI to predict ROSC and survival outcomes in OHCA, the generalizability of the predictive models developed to date may be limited. Most of these studies utilized classification algorithms that were developed and validated with data from EMS systems in Asia.10, 11, 13, 14, 15, 16, 17, 18, 19 It is known that EMS systems vary widely both at the international level and within the United States.62 As such, these models may not be applicable within the North American and European EMS systems.
Improving timely recognition of OHCA during the initial medical dispatch call is another factor that may improve OHCA outcomes. Early detection of OHCA is critical as it may enable telephone CPR and dispatch of appropriate EMS resources. This scoping review identified multiple studies which described ML and DL frameworks which analyze linguistic and phonetic characteristics of speech during the dispatch call and provided decision-support for dispatch in the detection of OHCA. Blomberg et al.7 conducted the first randomized controlled trial evaluating the use of ML as real-time decision support for OHCA recognition for dispatchers. Though the model had previously shown success in training and validation during a prior retrospective observational study29, it did not result in a significant improvement in dispatcher OHCA recognition when used in real-time. The absence of a significant improvement was attributed to human factors in the interaction with the decision support tool. This study highlighted the first prospective implementation of ML to guide early OHCA care. Overall, this scoping review revealed that current literature consists of retrospective analyses with positive conclusions and a single randomized control trial with a neutral outcome. As such, these findings demonstrate the need for future prospective studies to better elucidate the factors impacting the use of AI in real-time to support dispatch and prehospital care.
This scoping review further identified studies which used AI to analyze ECG waveform segments from OHCA resuscitations. These studies were heterogenous in both their objectives and approaches; nonetheless the overarching aims were to limit CPR interruptions through rapid analysis of ECG segments (both with and without CPR artifact) with a variety of classification algorithms. While some studies used ML algorithms to classify ECG segments obtained during CPR pauses46, 47, 48, 49, other studies allowed classified rhythms with on-going CPR through removal of artifact via filtering.30, 36, 38, 42, 50, 52 Other studies utilized feature extraction and rhythm classification via DL from ECG segments taken during CPR which eliminated the need for CPR artifact filtering.37, 41, 44, 45, 53 Additional studies attempted to characterize specific features of VF in order to predict defibrillation performance31, 32, 33, 34, 35 while others targeted overall rhythm classification39, 40 Finally, Coult et al.50 conducted a study using ECG waveform and thoracic impedance data obtained from the defibrillator and combined it with clinical variables in an attempt to predict survival outcomes.
Limitations
The results of this scoping review must be considered within the context of multiple limitations. This review may not encompass literature published by nursing and allied health professionals given that databases such as the Cumulated Index to Nursing and Allied Health Literature were not included. Similarly, more technical engineering studies in databases such as Institute of Electrical and Electronics Engineers may not have been included. Further, findings may lack external validity due to the limited number of countries from which studies were published. Conference abstracts, which lack complete methodology and outcome descriptions, were also excluded and this may have limited the breadth of emerging research. Finally, a single experienced reviewer screened manuscripts which may have led to bias toward over- or under-inclusion of articles; however, a previous study showed that it is unlikely to have significantly changed the overall results.63
Conclusions
A growing body of literature exists describing the use of AI to support providers in the early care of OHCA. The main categories that were identified included studies that aimed to improve the early dispatch-level detection of OHCA, predict ROSC and survival outcomes, and classify of ECG rhythms. Only one prospective trial was identified, and future trials are needed to evaluate the integration of AI with human decision-making and gestalt. Nonetheless, these 54 studies demonstrate the potential applicability of AI algorithms to support dispatchers, EMS providers and physicians, and ED-based physicians in the OHCA care.
CRediT authorship contribution statement
Jake Toy: Conceptualization, Methodology, Data curation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing. Nichole Bosson: Supervision, Writing – review & editing. Shira Schlesinger: Supervision, Writing – review & editing. Marianne Gausche-Hill: Supervision, Writing – review & editing. Samuel Stratton: Conceptualization, Methodology, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: [Jake Toy, DO, Declarations of interest: none. Nichole Bosson, MD, MPH, Declarations of interest: none. Shira Schlesinger, MD, MPH, Declarations of interest: none, Marianne Gausche-Hill, MD, Declarations of interest: Member of the CARES Advisory Board beginning in September 2023. Sam Stratton, MD, Declarations of interest: none].
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100491.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.2021 CARES Annual Report. Accessed December 9, 2022. https://mycares.net/sitepages/uploads/2022/2021_flipbook/index.html?page=1.
- 2.Part 12: From Science to Survival | Circulation. Accessed October 28, 202. https://www.ahajournals.org/doi/10.1161/circ.102.suppl_1.I-358.
- 3.Kirubarajan A., Taher A., Khan S., Masood S. Artificial intelligence in emergency medicine: A scoping review. J Am Coll Emerg Physicians Open. 2020;1:1691–1702. doi: 10.1002/emp2.12277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alamgir A., Mousa O., Shah Z. Artificial intelligence in predicting cardiac arrest: scoping review. JMIR Med Inform. 2021;9:e30798. doi: 10.2196/30798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Viderman D., Abdildin Y.G., Batkuldinova K., Badenes R., Bilotta F. Artificial Intelligence in Resuscitation: A Scoping Review. J Clin Med. 2023;12:2254. doi: 10.3390/jcm12062254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation | Annals of Internal Medicine. Accessed April 3, 2023. https://www.acpjournals.org/doi/10.7326/M18-0850. [DOI] [PubMed]
- 7.Blomberg S.N., Christensen H.C., Lippert F., et al. Effect of machine learning on dispatcher recognition of out-of-hospital cardiac arrest during calls to emergency medical services: A randomized clinical trial. JAMA Netw Open. 2021;4:e2032320. doi: 10.1001/jamanetworkopen.2020.32320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harford S., Del Rios M., Heinert S., et al. A machine learning approach for modeling decisions in the out of hospital cardiac arrest care workflow. BMC Med Inf Decis Making. 2022;22:21. doi: 10.1186/s12911-021-01730-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kawai Y., Okuda H., Kinoshita A., et al. Visual assessment of interactions among resuscitation activity factors in out-of-hospital cardiopulmonary arrest using a machine learning model. PLoS One. 2022;17:e0273787. doi: 10.1371/journal.pone.0273787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong X.Y., Ang Y.K., Li K., et al. Development and validation of the SARICA score to predict survival after return of spontaneous circulation in out of hospital cardiac arrest using an interpretable machine learning framework. Resuscitation. 2022;170:126–133. doi: 10.1016/j.resuscitation.2021.11.029. [DOI] [PubMed] [Google Scholar]
- 11.Lin W.C., Huang C.H., Chien L.T., et al. Tree-based algorithms and association rule mining for predicting patients’ neurological outcomes after first-aid treatment for an out-of-hospital cardiac Arrest During COVID-19 pandemic: application of data mining. Int J Gen Med. 2022;15:7395–7405. doi: 10.2147/IJGM.S384959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu N., Liu M., Chen X., et al. Development and validation of an interpretable prehospital return of spontaneous circulation (P-ROSC) score for patients with out-of-hospital cardiac arrest using machine learning: A retrospective study. eClinicalMedicine101422. 2022;48 doi: 10.1016/j.eclinm.2022.101422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Dury N., Ravn-Fischer A., Hollenberg J., et al. Identifying the relative importance of predictors of survival in out of hospital cardiac arrest: a machine learning study. Scand J Trauma Resusc Emerg Med. 2020;28:60. doi: 10.1186/s13049-020-00742-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim J.W., Ha J., Kim T., et al. Developing a time-adaptive prediction model for out-of-hospital cardiac arrest: nationwide cohort Study in Korea. J Med Internet Res. 2021;23:e28361. doi: 10.2196/28361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu N, Ho AFW, Pek PP, et al. Prediction of ROSC After Cardiac Arrest Using Machine Learning. Stud Health Technol Inform. 2020;270((Liu N.) Health Services Research Centre, Singapore Health Services, Singapore):1357–1358. 10.3233/SHTI200440. [DOI] [PubMed]
- 16.Shin S.J., Bae H.S., Moon H.J., et al. Evaluation of optimal scene time interval for out-of-hospital cardiac arrest using a deep neural network. Am J Emerg Med. 2023;63:29–37. doi: 10.1016/j.ajem.2022.10.011. [DOI] [PubMed] [Google Scholar]
- 17.Seo D.W., Yi H., Bae H.J., et al. Prediction of neurologically intact survival in cardiac arrest patients without pre-hospital return of spontaneous circulation: machine learning approach. J Clin Med. 2021;10 doi: 10.3390/jcm10051089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kwon J.M., Jeon K.H., Kim H.M., et al. Deep-learning-based out-of-hospital cardiac arrest prognostic system to predict clinical outcomes. Resuscitation. 2019;139:84–91. doi: 10.1016/j.resuscitation.2019.04.007. [DOI] [PubMed] [Google Scholar]
- 19.Hirano Y., Kondo Y., Sueyoshi K., Okamoto K., Tanaka H. Early outcome prediction for out-of-hospital cardiac arrest with initial shockable rhythm using machine learning models. Resuscitation. 2021;158:49–56. doi: 10.1016/j.resuscitation.2020.11.020. [DOI] [PubMed] [Google Scholar]
- 20.Harford S., Darabi H., Del Rios M., et al. A machine learning based model for Out of Hospital cardiac arrest outcome classification and sensitivity analysis. Resuscitation. 2019;138:134–140. doi: 10.1016/j.resuscitation.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 21.Lo Y.H., Siu Y.C.A. Predicting survived events in nontraumatic out-of-hospital cardiac arrest: A comparison study on machine learning and regression models. J Emerg Med. 2021;61:683–694. doi: 10.1016/j.jemermed.2021.07.058. [DOI] [PubMed] [Google Scholar]
- 22.Krizmaric M., Verlic M., Stiglic G., Grmec S., Kokol P. Intelligent analysis in predicting outcome of out-of-hospital cardiac arrest. Comput Methods Programs Biomed. 2009;95:S22–S32. doi: 10.1016/j.cmpb.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 23.Liu N., Ho A.F.W., Pek P.P., et al. Prediction of ROSC after cardiac arrest using machine learning. Stud Health Technol Inform. 2020;270:1357–1358. doi: 10.3233/SHTI200440. [DOI] [PubMed] [Google Scholar]
- 24.Rafi S., Gangloff C., Paulhet E., et al. Out-of-hospital cardiac arrest detection by machine learning based on the phonetic characteristics of the caller’s voice. Stud Health Technol Inform. 2022;294:445–449. doi: 10.3233/SHTI220498. [DOI] [PubMed] [Google Scholar]
- 25.Arcolezi H.H., Cerna S., Couchot J.F., Guyeux C., Makhoul A. Privacy-preserving prediction of victim’s mortality and their need for transportation to health facilities. IEEE Trans Ind Inform. 2022;18:5592–5599. doi: 10.1109/TII.2021.3123588. [DOI] [Google Scholar]
- 26.Blomberg SN, Jensen TW, Porsborg Andersen M, et al. When the machine is wrong. Characteristics of true and false predictions of Out-of-Hospital Cardiac Arrests in Emergency Calls using a machine-learning model. Resuscitation. Published online January 9, 2023:109689. 10.1016/j.resuscitation.2023.109689. [DOI] [PubMed]
- 27.Byrsell F., Claesson A., Ringh M., et al. Machine learning can support dispatchers to better and faster recognize out-of-hospital cardiac arrest during emergency calls: A retrospective study. Resuscitation. 2021;162:218–226. doi: 10.1016/j.resuscitation.2021.02.041. [DOI] [PubMed] [Google Scholar]
- 28.Chin K.C., Hsieh T.C., Chiang W.C., et al. Early recognition of a caller’s emotion in out-of-hospital cardiac arrest dispatching: An artificial intelligence approach. Resuscitation. 2021;167:144–150. doi: 10.1016/j.resuscitation.2021.08.032. [DOI] [PubMed] [Google Scholar]
- 29.Blomberg S.N., Folke F., Ersbøll A.K., et al. Machine learning as a supportive tool to recognize cardiac arrest in emergency calls. Resuscitation. 2019;138:322–329. doi: 10.1016/j.resuscitation.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 30.Coult J., Rea T.D., Blackwood J., Kudenchuk P.J., Liu C., Kwok H. A method to predict ventricular fibrillation shock outcome during chest compressions. Comput Biol Med. 2021;129:104136. doi: 10.1016/j.compbiomed.2020.104136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ivanović M.D., Hannink J., Ring M., et al. Predicting defibrillation success in out-of-hospital cardiac arrested patients: Moving beyond feature design. Artif Intell Med. 2020;110:101963. doi: 10.1016/j.artmed.2020.101963. [DOI] [PubMed] [Google Scholar]
- 32.Ivanović M.D., Ring M., Baronio F., et al. ECG derived feature combination versus single feature in predicting defibrillation success in out-of-hospital cardiac arrested patients. Biomed Phys Eng Express. 2019;5 doi: 10.1088/2057-1976/aaebec. [DOI] [Google Scholar]
- 33.He M., Lu Y., Zhang L., Zhang H., Gong Y., Li Y. Combining amplitude spectrum area with previous shock information using neural networks improves prediction performance of defibrillation outcome for subsequent shocks in out-of-hospital cardiac arrest patients. PLoS One. 2016;11:e0149115. doi: 10.1371/journal.pone.0149115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neurauter A., Eftestøl T., Kramer-Johansen J., et al. Prediction of countershock success using single features from multiple ventricular fibrillation frequency bands and feature combinations using neural networks. Resuscitation. 2007;73:253–263. doi: 10.1016/j.resuscitation.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 35.Shandilya S., Kurz M.C., Ward K.R., Najarian K. Integration of attributes from non-linear characterization of cardiovascular time-series for prediction of defibrillation outcomes. PLoS One. 2016;11 doi: 10.1371/journal.pone.0141313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Isasi I., Irusta U., Aramendi E., Olsen J.A., Wik L. Shock decision algorithm for use during load distributing band cardiopulmonary resuscitation. Resuscitation. 2021;165:93–100. doi: 10.1016/j.resuscitation.2021.05.028. [DOI] [PubMed] [Google Scholar]
- 37.Hajeb-M S., Cascella A., Valentine M., Chon K.H. Enhancing the accuracy of shock advisory algorithms in automated external defibrillators during ongoing cardiopulmonary resuscitation using a deep convolutional Encoder-Decoder filtering model. Expert Syst Appl. 2022;203 doi: 10.1016/j.eswa.2022.117499. [DOI] [Google Scholar]
- 38.Picon A., Irusta U., Álvarez-Gila A., et al. Mixed convolutional and long short-term memory network for the detection of lethal ventricular arrhythmia. PLoS One. 2019;14:e0216756. doi: 10.1371/journal.pone.0216756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rad A.B., Eftestol T., Engan K., et al. ECG-based classification of resuscitation cardiac rhythms for retrospective data analysis. IEEE Trans Biomed Eng. 2017;64:2411–2418. doi: 10.1109/TBME.2017.2688380. [DOI] [PubMed] [Google Scholar]
- 40.Figuera C., Irusta U., Morgado E., et al. Machine learning techniques for the detection of Shockable rhythms in automated external defibrillators. PLoS One. 2016;11:e0159654. doi: 10.1371/journal.pone.0159654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jekova I., Krasteva V. Optimization of end-to-end convolutional neural networks for analysis of out-of-hospital cardiac arrest rhythms during cardiopulmonary resuscitation. Sensors. 2021;21 doi: 10.3390/s21124105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Isasi I., Irusta U., Aramendi E., Eftestøl T., Kramer-Johansen J., Wik L. Rhythm analysis during cardiopulmonary resuscitation using convolutional neural networks. Entropy Basel Switz. 2020;22 doi: 10.3390/e22060595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jaureguibeitia X., Zubia G., Irusta U., et al. Shock decision algorithms for automated external defibrillators based on convolutional networks. IEEE Access. 2020;8:154746–154758. doi: 10.1109/ACCESS.2020.3018704. [DOI] [Google Scholar]
- 44.Krasteva V., Ménétré S., Didon J.P., Jekova I. Fully convolutional deep neural networks with optimized hyperparameters for detection of shockable and non-Shockable rhythms. Sensors. 2020;20 doi: 10.3390/s20102875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hajeb-M S., Cascella A., Valentine M., Chon K.H. Deep neural network approach for continuous ECG-Based automated external defibrillator shock advisory system during cardiopulmonary resuscitation. J Am Heart Assoc. 2021;10:e019065. doi: 10.1161/JAHA.120.019065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Elola A., Aramendi E., Irusta U., et al. Deep neural networks for ECG-based pulse detection during out-of-hospital cardiac arrest. Entropy Basel Switz. 2019;21 doi: 10.3390/e21030305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Urteaga J., Aramendi E., Elola A., Irusta U., Idris A. A machine learning model for the prognosis of pulseless electrical activity during out-of-hospital cardiac arrest. Entropy Basel Switz. 2021;23 doi: 10.3390/e23070847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elola A., Aramendi E., Irusta U., Berve P.O., Wik L. Multimodal algorithms for the classification of circulation states during out-of-hospital cardiac arrest. IEEE Trans Biomed Eng. 2021;68:1913–1922. doi: 10.1109/TBME.2020.3030216. [DOI] [PubMed] [Google Scholar]
- 49.Elola A., Aramendi E., Irusta U., et al. Capnography: A support tool for the detection of return of spontaneous circulation in out-of-hospital cardiac arrest. Resuscitation. 2019;142:153–161. doi: 10.1016/j.resuscitation.2019.03.048. [DOI] [PubMed] [Google Scholar]
- 50.Coult J., Blackwood J., Sherman L., Rea T.D., Kudenchuk P.J., Kwok H. Ventricular fibrillation waveform analysis during chest compressions to predict survival from cardiac arrest. Circ Arrhythm Electrophysiol. 2019;12:e006924. doi: 10.1161/CIRCEP.118.006924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Elola A., Aramendi E., Rueda E., Irusta U., Wang H., Idris A. Towards the prediction of rearrest during out-of-hospital cardiac arrest. Entropy Basel Switz. 2020;22 doi: 10.3390/e22070758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sashidhar D., Kwok H., Coult J., et al. Machine learning and feature engineering for predicting pulse presence during chest compressions. R Soc Open Sci. 2021;8:210566. doi: 10.1098/rsos.210566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thannhauser J, Nas J, van der Sluijs K, et al. Pilot study on VF-waveform based algorithms for early detection of acute myocardial infarction during out-of-hospital cardiac arrest. Resuscitation. 2022;174((Thannhauser J., Jos.Thannhauser@Radboudumc.nl; Nas J.; van der Sluijs K.; de Boer M.-J.; van Royen N.; Bonnes J.; Brouwer M.) Department of Cardiology, Radboudumc, Nijmegen, Netherlands):62–67. 10.1016/j.resuscitation.2022.03.025. [DOI] [PubMed]
- 54.Monlezun D.J., Samura A.T., Patel R.S., Thannoun T.E., Balan P. Racial and socioeconomic disparities in out-of-hospital cardiac arrest outcomes: artificial intelligence-augmented propensity score and geospatial cohort analysis of 3,952 Patients. Cardiol Res Pract. 2021;2021:3180987. doi: 10.1155/2021/3180987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moon H.J., Shin Y.J., Cho Y.S. Identification of out-of-hospital cardiac arrest clusters using unsupervised learning. Am J Emerg Med. 2022;62:41–48. doi: 10.1016/j.ajem.2022.09.035. [DOI] [PubMed] [Google Scholar]
- 56.Nakashima T., Ogata S., Noguchi T., et al. Machine learning model for predicting out-of-hospital cardiac arrests using meteorological and chronological data. Heart Br Card Soc. 2021;107:1084–1091. doi: 10.1136/heartjnl-2020-318726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harris M, Crowe RP, Anders J, D’Acunto S, Adelgais KM, Fishe JN. Identification of Factors Associated with Return of Spontaneous Circulation after Pediatric Out-of-Hospital Cardiac Arrest Using Natural Language Processing. Prehosp Emerg Care. Published online May 23, 2022:1-8. 10.1080/10903127.2022.2074180. [DOI] [PubMed]
- 58.Choi DH, Park JH, Choi YH, Song KJ, Kim S, Shin SD. Machine Learning Analysis to Identify Data Entry Errors in Prehospital Patient Care Reports: A Case Study of a National Out-of-Hospital Cardiac Arrest Registry. Prehosp Emerg Care. Published online November 16, 2022:1–9. 10.1080/10903127.2022.2137745. [DOI] [PubMed]
- 59.Jerkeman M., Lundgren P., Omerovic E., et al. Association between type of bystander cardiopulmonary resuscitation and survival in out-of-hospital cardiac arrest: A machine learning study. Resusc Plus. 2022;10:100245. doi: 10.1016/j.resplu.2022.100245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Otero-Agra M., Jorge-Soto C., Cosido-Cobos Ó.J., et al. Can a voice assistant help bystanders save lives? A feasibility pilot study chatbot in beta version to assist OHCA bystanders. Am J Emerg Med. 2022;61:169–174. doi: 10.1016/j.ajem.2022.09.013. [DOI] [PubMed] [Google Scholar]
- 61.Chu J., Leung K.H.B., Snobelen P., et al. Machine learning-based dispatch of drone-delivered defibrillators for out-of-hospital cardiac arrest. Resuscitation. 2021;162:120–127. doi: 10.1016/j.resuscitation.2021.02.028. [DOI] [PubMed] [Google Scholar]
- 62.Spigner M.F., Benoit J.L., Menegazzi J.J., McMullan J.T. Prehospital protocols for post-return of spontaneous circulation are highly variable. Prehosp Emerg Care. 2021;25:191–195. doi: 10.1080/10903127.2020.1754979. [DOI] [PubMed] [Google Scholar]
- 63.Waffenschmidt S., Knelangen M., Sieben W., Bühn S., Pieper D. Single screening versus conventional double screening for study selection in systematic reviews: a methodological systematic review. BMC Med Res Method. 2019;19:132. doi: 10.1186/s12874-019-0782-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.