Abstract
Introduction
Failure to restore spontaneous circulation remains a major cause of death for cardiac arrest (CA) patients. Mechanical circulatory support, specifically extracorporeal cardiopulmonary resuscitation (ECPR), has emerged as a feasible and efficacious rescue strategy for selected refractory CA patients.
Methods
Mechanical Circulatory Support was one of six focus topics for the Wolf Creek XVII Conference held on June 14–17, 2023 in Ann Arbor, Michigan, USA. Conference invitees included international thought leaders and scientists in the field of CA resuscitation from academia and industry. Participants submitted via online survey knowledge gaps, barriers to translation and research priorities for each focus topic. Expert panels used the survey results and their own perspectives and insights to create and present a preliminary unranked list for each category that was debated, revised and ranked by all attendees to identify the top 5 for each category.
Results
Top 5 knowledge gaps included optimal patient selection, pre-ECPR treatments, logistical and programmatic characteristics of ECPR programs, generalizability and effectiveness of ECPR, and prevention of reperfusion injury. Top 5 barriers to translation included cost/resource limitations, technical challenges, collaboration across multiple disciplines, limited patient population, and early identification of eligible patients. Top 5 research priorities focused on comparing the outcomes of prehospital/rapid transport strategies vs in-hospital ECPR initiation, implementation of high-performing ECPR system vs standard care, rapid patient identification tools vs standard clinical judgment, post-cardiac arrest bundled care vs no bundled care, and standardized ECPR clinical protocol vs routine care.
Conclusion
This overview can serve as an innovative guide to transform the care and outcome of patients with refractory CA.
Keywords: Cardiac arrest, Mechanical circulatory support, Extracorporeal cardiopulmonary resuscitation, Wolf Creek Conference
Introduction
Cardiac arrest (CA) is a prevalent public health problem with high incidence of mortality and neurologic impairment.1, 2, 3, 4, 5 Approximately 70% of CA is associated with primary myocardial failure, which is often caused by acute coronary occlusion and malignant cardiac arrhythmia.6 Timely restoration of cardiac function and return of spontaneous circulation (ROSC) during cardiopulmonary resuscitation (CPR) remains a major challenge for refractory CA.
Failure to achieve ROSC within 30 minutes from onset of CA has been associated with almost 100% mortality.7, 8 To overcome this life-threatening circulatory failure, short-term mechanical circulatory support provided by venoarterial extracorporeal membrane oxygenation (VA-ECMO) and extracorporeal cardiopulmonary resuscitation (ECPR) during refractory CA have become rescue strategies in selected centers.9, 10, 11, 12, 13 Recent randomized controlled trials have demonstrated ECPR to improve the survival and neurologic outcome of selected refractory out-of-hospital CA (OHCA) patients with initial shockable rhythm.14, 15, 16 The 2022 International Liaison Committee on Resuscitation Consensus on Science with Treatment Recommendation suggests that ECPR may be considered as a rescue therapy for selected patients with OHCA and in-hospital CA (IHCA) when conventional CPR is failing to restore spontaneous circulation in settings where this can be implemented.17 However, ECPR remains a resource-intensive system of care that is not readily available at most healthcare centers.18, 19, 20 Key questions regarding ECPR implementation include optimal patient selection, strategies to shorten time from CA to extracorporeal support, and resource utilization.
The main focus of the Wolf Creek Conference XVII Mechanical Support Panel on June 16, 2023, in Ann Arbor, Michigan, was to highlight the current state and propose a potential future state for ECPR, as well as to identify its top knowledge gaps, barriers to translation, and research priorities. The panel was co-chaired by Drs. Cindy Hsu and Jason Bartos, with Drs. George Trummer, Jan Belohlavek, and Demetris Yannopoulos as panelists. This manuscript provides an overview of the current and potential future state of the field and prioritized results of the discussions between the panelists (authors of this manuscript) and the conference participants.
Methods
Since its inception in 1975, the Wolf Creek Conference has a well-established tradition of providing a unique forum for robust intellectual exchange between thought leaders and scientist from academia and industry that focuses on advancing the science and practice of CA resuscitation.21 The Wolf Creek XVII Conference was hosted by the Max Harry Weil Institute for Critical Care Research and Innovation in Ann Arbor, Michigan, USA on June 15–17, 2023.22
Mechanical Circulatory Support was one of 6 focus topics for the Wolf Creek XVII Meeting hosted by the Max Harry Weil Institute for Critical Care Research and Innovation in Ann Arbor, Michigan, USA on June 15–17, 2023. Meeting invitees included international academic and industry scientists as well as thought leaders in the field of CA resuscitation. All participants were required to complete conflict of interest disclosures. Prior to the meeting, all participants were asked via online survey to list up to three knowledge gaps, barriers to translation and research priorities for each topic. Participants were instructed that the topic of mechanical circulatory support would focus on rescue strategies for refractory CA using invasive mechanical devices such as ECPR, percutaneous left ventricular assist devices, and aortic balloon occlusion.
Knowledge gaps were defined as areas where our understanding or knowledge is incomplete or limited. These gaps can arise due to various factors, such as lack of research, inadequate information, limited access to data or resources, or simply because the topic is new or complex. Barriers to translation were defined as obstacles that can prevent the successful transfer of knowledge or innovations from research or development settings to practical applications in the real world. Research priorities were defined as the areas of study that are considered most important or urgent by the scientific community or society as a whole. These priorities are often determined by a range of factors such as knowledge gaps, scientific breakthroughs, new challenges, societal needs or funding opportunities.
Panels of experts in each topic used the survey results and their own perspectives and insights to create an initial unranked list of up to ten items for each category. For this panel, the survey responses for each question were entered in ChatGPT (OpenAI, Microsoft Corporation) with the prompt, “You are a qualitative researcher. Please code the following open-ended survey responses into relevant categories using a modified delphi approach.” ChatGPT was also provided with the original question for the responses. CHH and JAB then iteratively revised and collapsed the categories generated by ChatGPT into top 10 categories for each of the three questions. The top research priorities were restructured in patient/population, intervention, comparison, outcomes (PICO) format whenever feasible.
During the conference, expert panelists provided an overview of the current state and potential future state of the field to lay the groundwork for an informed debate. This was followed by presentation and initial ranking of the knowledge gaps, barriers to translation, and research priorities by all attendees using electronic voting, discussion and revision by the panel and attendees, and then re-ranking. The top 5 items in each category underwent final review on the last day of the conference. An overview of the current and potential future state of the field and prioritized results for Mechanical Circulatory Support are presented and discussed in this manuscript. The complete results and rankings from all three categories are listed in Supplemental Materials.
Current state
What is currently in use?
The integration of mechanical circulatory support devices during CPR is performed to counteract the ongoing circulatory failure caused by refractory CA. Potential devices for this purpose include VA-ECMO and microaxial blood pumps. All these systems require central arterial and venous vascular access.23, 24 Microaxial pumps can provide high rates of blood flow (3.5–5 l/min) and therefore can temporarily replace circulatory function. However, the concomitant pulmonary failure from refractory CA is not supported by microaxial pumps. Moreover, the use of microaxial pumps in biventricular dysfunction may become inadequate due to cardiac non-contractility. Therefore, VA-ECMO is the most suitable option for ECPR due to its ability to fully support the cardiac and pulmonary systems.
What is being clinically studied?
The availability of extracorporeal devices and experienced staff to implement ECPR is still limited to specialized centers. Beyond that, the course of VA-ECMO support has not been standardized yet with respect to specific elements like circuit priming, blood flow, and specified conditions of gas exchange.25, 26, 27, 28, 29, 30, 31 Until recently, the outcomes of ECPR for refractory OHCA and IHCA have been limited to retrospective or prospective observational studies, case series, or case reports.
Three randomized trials on the outcome of OHCA were recently published.14, 32, 33 These trials provide promising survival rates between 20% and 43% in patients who received ECPR. Furthermore, these trials indicate that ECPR requires well defined patient selection criteria, sophisticated program structures to provide extracorporeal circulation in the scenario of ECPR, and a well-designed integration along the interfaces to prehospital and in-hospital advanced cardiac life support (ACLS).
What is in development?
Post-cardiac arrest syndrome is a summation of detrimental processes following CA, low-flow state, and ROSC.34 The underlying pathophysiologic comprehension of this syndrome refers to a generalized ischemia/reperfusion injury. Other than in CPR, the implementation of ECPR enables the control over blood circulation and gas exchange and therefore the conditions and composition of reperfusion. “Controlled Automated Reperfusion of the Whole Body” (CARL) is such an approach currently under investigation in a first clinical trial.35, 36, 37
Potential future state
The ongoing vision of improved survival and neurologic recovery following CA in combination with state of the art medical engineering motivates the medical community to continue to innovate and improve the methods of ECPR. ECPR is currently performed in various institutions across the world with innumerable variations in each aspect of the ECPR system that are driven by local logistics and professional society guidelines. Ideally, these institutions and organizations would collaborate to compare outcomes and improve the integration of ECPR within the chain of survival. Potential areas for improvement include: (a) timely consideration of ECPR and activation of ECPR teams during ACLS, (b) selection criteria for ECPR, (c) training and skill maintenance of ECPR providers, (d) development of robust reporting standards for ECPR clinical trials, (e) improved strategies for post-cardiac arrest care incorporating the risks and opportunities of ECPR, and (f) development of reliable prognostication strategies to focus resources on those likely to recover. ECPR has the potential to become the standard of care in selected groups of CA patients if the essential components for a successful system of care can be identified and implemented at other centers.
Knowledge gaps
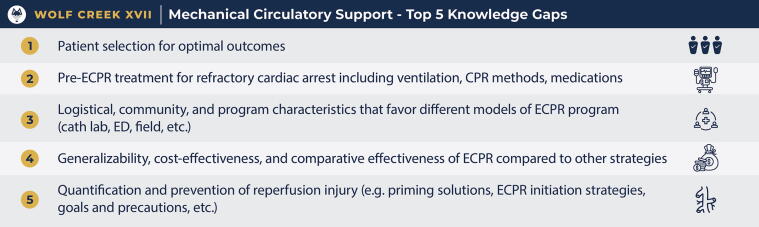
The following top 5 knowledge gaps were identified by conference participants and discussed during the Mechanical Circulatory Support Panel (Fig. 1).
-
1.
Patient selection for optimal outcomes
Figure 1.
Mechanical circulatory support: Top 5 knowledge gaps as ranked by attendees at Wolf Creek XVII, June 15-17, 2023, Ann Arbor, MI
Since ECPR is resource-intensive and rare, patient selection is crucial to maximize outcome. The proof-of-concept ECPR systems of care should ideally be performed in well-defined groups of patients. Indications and contraindications for ECPR are still debated, including whether ECPR should be implemented in patients with initial nonshockable rhythm or unwitnessed CA.15, 38 However, in order to achieve time from CA to VA-ECMO of less than 60 minutes, prompt ECPR initiation would require early dispatch (i.e. 10–20 min after start of CPR) of the ECPR team (i.e. prehospital, emergency department, cardiac catheterization lab).8, 10, 39, 40, 41 This requirement can be challenging because accurate prehospital information about the OHCA patients may not be readily available.
-
2.
Pre-ECPR treatment for refractory cardiac arrest including ventilation, CPR methods, medications
CPR is a community-based intervention and an integral component within the chain of survival. ECPR should be integrated with prompt initiation and continuation of high quality CPR. However, the best strategies for CPR, ventilation, and vasoactive support to optimize brain and cardiac perfusion during refractory CA require further investigation.42
-
3.
Logistical, community and program characteristics that favor different models of ECPR program (Cath lab, ED, field, etc.)
OHCA more commonly occurs in private residences than in public locations, and IHCA may also occur at different locations in hospitals.2, 43 The integration and initiation of extracorporeal support during CPR is therefore faced with logistic challenges. Beyond that, the structure of healthcare systems may vary between countries, regions, or cities, which adds more complexity to logistical, community, and program characteristics. Nevertheless, scenarios of ECPR in IHCA or OHCA settings are described but require adaptation to local conditions and resources.44, 45
-
4.
Generalizability, cost effectiveness, and comparative effectiveness of ECPR compared to other strategies
Within the given heterogeneity of patients in refractory CA, it is challenging to determine the effect of ECPR on specific populations. Since ECPR is a rescue strategy at the end of the chain of survival, the CA patients generally represent those who would not have otherwise survived without ECPR. On the other hand, patient selection for ECPR impacts the outcomes observed which may provide important insights into the effects of ECPR.15 Documentation of ECPR along established reporting standards (i.e. Utstein style) could help to create a more comprehensive database useful for drawing conclusions of the effect of ECPR. In addition, the cost and cost-effectiveness of ECPR will need further elucidation in order to demonstrate its feasibility and sustainability within different health systems.
-
5.
Quantification and prevention of reperfusion injury (e.g. priming solution, ECPR initiation strategies, goals and precautions, etc.)
The pathophysiology of CPR is closely related to a generalized ischemia/reperfusion injury of the whole body. Since ECPR provides the opportunity to gain control over blood circulation, monitoring, and gas exchange, the conditions and composition of reperfusion may be adapted to limit post-cardiac arrest syndrome.34 Components of VA-ECMO that have not been standardized for ECPR patients include optimal priming and perfusate composition, blood flow, and specified conditions of gas exchange.
Barriers to translation
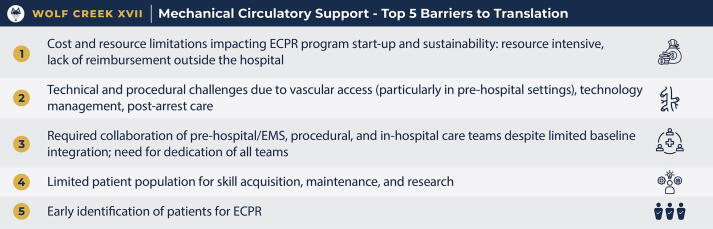
The following top 5 barriers to translation were identified by conference participants and discussed during the Mechanical Circulatory Support Panel (Fig. 2).
-
1.
Cost and resource limitations impacting ECPR program start-up and sustainability: resource intensive, lack of reimbursement outside the hospital
Figure 2.
Mechanical circulatory support: Top 5 barriers to translation as ranked by attendees at Wolf Creek XVII, June 15-17, 2023, Ann Arbor, MI
Cost and resource limitations were identified as the top barrier to translation for successful implementation and sustainability of ECPR systems of care. This barrier is often associated with disparities in access to healthcare that are disproportionately affected by the clinical characteristics and geographic location of CA patients. Furthermore, the variability in reimbursement for prehospital care poses another barrier to sustainability of ECPR programs.
-
2.
Technical and procedural challenges due to vascular access (particularly in pre-hospital settings), technology management, post-cardiac arrest care
The relative low incidence and unpredictable timing of ECPR pose significant challenges to the training and skill competency maintenance for both proceduralists who initiate ECPR for the refractory CA patients and those who care for these patients in the emergency departments and intensive care units. These same barriers apply to all members of the medical team such as emergency medical services, nurses, respiratory therapists, and perfusionists.
-
3.
Required collaboration of prehospital/EMS, procedural, and in-hospital care teams despite limited baseline integration. Need for dedication of all teams
ECPR is a system of care that begins in the prehospital setting. Successful implementation of an ECPR system must integrate prehospital teams, emergency departments, intensive care units, and related subspecialists who manage ECPR patients after initiation of VA-ECMO. The success of an ECPR program is dependent on the seamless integration of these multidisciplinary teams.
-
4.
Limited patient population for skill acquisition, maintenance, and research
Similar to technical and procedural challenges, the infrequent ECPR incidence poses a challenge to supporting the training and sustainability of a successful ECPR system of care. With the exception of high volume health centers, it is unlikely that there are enough refractory CA patients to consistently sustain the training efforts. As such, the development of novel training strategies will be critically important.
-
5.
Early identification of patients for ECPR
As ECPR is a time-sensitive intervention, and shorter time from CA to VA-ECMO initiation has been associated with better outcome,46 early identification of eligible patients is critical for patient outcome. This applies to both OHCA and IHCA settings. For OHCA, prehospital identification and notification of refractory CA patients who may meet inclusion criteria within suitable transport time is important. Similarly for IHCA, prompt notification and activation of the ECMO team of eligible patients may shorten their time to extracorporeal support and impact their outcome.
Research priorities
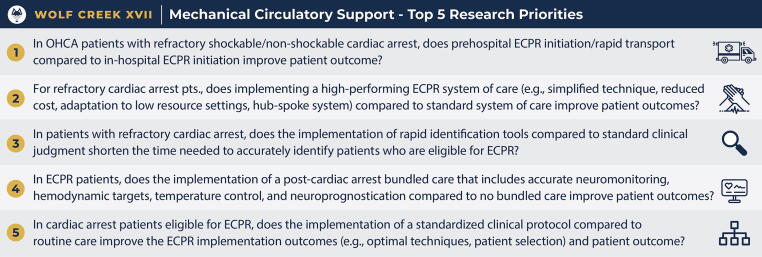
The following top 5 research priorities in PICO format were identified by conference participants and discussed during the Mechanical Circulatory Support Panel (Fig. 3).
-
1.
In OHCA patients with refractory shockable/nonshockable cardiac arrest, does prehospital ECPR initiation/rapid transport compared to in-hospital ECPR initiation improve patient outcome?
Figure 3.
Mechanical circulatory support: Top 5 research priorities as ranked by attendees at Wolf Creek XVII, June 15-17, 2023, Ann Arbor, MI
Comparing prehospital ECPR activation vs in-hospital activation for OHCA was identified as the top research priority. In-hospital activation could occur in the emergency departments, catheterization labs, or intensive care units. An ideal study would also identify prehospital strategies that could shorten the time from CA to initiation of VA-ECMO, which has been associated with better outcomes in observational studies.45
-
2.
For refractory CA patients, does implementing a high-performing ECPR system of care (e.g., simplified technique, reduced cost, adaptation to low resource settings, hub-spoke system) compared to standard system of care improve patient outcomes?
Discussions on this research priority focused on identifying the elements of a high-performing ECPR system of care that are essential and scalable to other centers. The conference participants and panelists discussed that the ARREST trial has already demonstrated the efficacy of a high-performing ECPR program’s ability to improve survival with good neurologic outcomes for refractory OHCA patients with initial shockable rhythm. The outcomes from the Minnesota ECPR system of care have already demonstrated superior outcomes compared to historical data from other OHCA trials.8 The INCEPTION trial33 demonstrated that ECPR may not be effective in real world clinical settings if performed at centers with variable experience.
-
3.
In patients with refractory cardiac arrest, does the implementation of rapid identification tools compared to standard clinical judgment shorten the time needed to accurately identify patients who are eligible for ECPR?
The eligibility criteria for ECPR patients and how to rapidly identify these patients emerged as another research priority. The identification of refractory CA patients with initial shockable rhythm is a reasonable starting point for the development, iterative refinement, and implementation of rapid identification tools, as these patients have been demonstrated to benefit from ECPR in a randomized controlled trial.14 The eligibility criteria of refractory CA patients with initial nonshockable rhythm will require further investigation to first identify which of these patients may benefit from ECPR, then to develop and test rapid identification strategies.
-
4.
In ECPR patients, does the implementation of a post-cardiac arrest bundle of care that includes accurate neuromonitoring, hemodynamic targets, temperature control, and neuroprognostication compared to no bundled care improve patient outcome?
The post-cardiac arrest care of ECPR patients remains an important modifiable variable that could impact the clinical outcome of these critically ill patients. This research priority aims to identify a bundle of care that could improve the outcome of ECPR patients. Some potential elements of the bundled care may include protocolized temperature management strategy, circuit and ventilator parameters, hemodynamic optimization, and neuroprognostication.
-
5.
In cardiac arrest patients eligible for ECPR, does the implementation of a standardized clinical protocol compared to routine care improve the ECPR implementation outcomes (e.g., optimal techniques, patient selection) and patient outcome?
This research priority incorporates elements from the previous four priorities. In order to answer this research question, the appropriate ECPR eligibility criteria will need to first be established. The development and implementation of a standardized clinical protocol to identify these eligible patients, initiate ECPR, and to provide consistent post-cardiac arrest care may facilitate the implementation of ECPR programs and ultimately their patient outcome.
Dissenting opinions
The conference participants discussed the limitations of PICO format in identifying research priorities, as some priorities cannot be written in this format. There were also discussions regarding what would be considered a “standard” system of care and how “clinical judgment” is defined.
Conclusions
The 2023 Wolf Creek Conference XVII Mechanical Circulatory Support Panel identified the top knowledge gaps, barriers to translation, and research priorities for ECPR in refractory CA. The themes that emerged from the discussions during this panel included strategies to rapidly and accurately identify eligible patients to shorten the time from CA to initiation of extracorporeal support; identification of physiologic and programmatic elements that are critical to successful ECPR programs; development of implementation strategies to facilitate ECPR skill acquisition, maintenance, and multidisciplinary collaborations; development of novel training methods to sustain low frequency, high-stake procedures and knowledge retention; and strategies to eliminate healthcare disparities that are associated with inequitable access to ECPR systems of care. We hope that this overview can serve as an innovative guide to those who hope to transform the care and outcome of patients with refractory CA.
CRediT authorship contribution statement
Cindy H. Hsu: Conceptualization, Methodology, Formal analysis, Writing – original draft, Writing – review & editing, Supervision. George Trummer: Writing – original draft, Writing – review & editing. Jan Belohlavek: Writing – review & editing. Demetris Yannopoulos: Writing – review & editing. Jason A. Bartos: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Supervision.
Declaration of Competing Interest
Cindy H. Hsu was the lead investigator of the EROCA trial and Editorial Board Member of Resuscitation Plus. Jason A. Bartos and Demetris Yannopoulos were the lead investigators of the ARREST trial. Jan Belohlavek was the lead investigator of the Prague OHCA study. George Trummer was the lead investigator for the Controlled Automated Reperfusion of the whoLe body (CARL). None of the authors have any financial conflicts of interests.
Acknowledgement
We acknowledge the staff of the Max Harry Weil Institute for Critical Care Research and Innovation for their technical and administrative support for the Wolf Creek Conference XVII Mechanical Circulatory Support Panel.
Footnotes
Supplementary material to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100493.
Appendix A. Supplementary material
The following are the Supplementary material to this article:
References
- 1.Gräsner J.-T., Herlitz J., Tjelmeland I.B.M., et al. European Resuscitation Council Guidelines 2021: Epidemiology of cardiac arrest in Europe. Resuscitation. 2021;161:61–79. doi: 10.1016/j.resuscitation.2021.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Tsao C.W., Aday A.W., Almarzooq Z.I., et al. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 3.Kiguchi T., Okubo M., Nishiyama C., et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR) Resuscitation. 2020;152:39–49. doi: 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 4.Perkins G.D., Callaway C.W., Haywood K., et al. Brain injury after cardiac arrest. Lancet. 2021;398:1269–1278. doi: 10.1016/S0140-6736(21)00953-3. [DOI] [PubMed] [Google Scholar]
- 5.Nishiyama C., Kiguchi T., Okubo M., et al. Three-year trends in out-of-hospital cardiac arrest across the world: Second report from the International Liaison Committee on Resuscitation (ILCOR) Resuscitation. 2023;186 doi: 10.1016/j.resuscitation.2023.109757. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) State-specific mortality from sudden cardiac death--United States, 1999. MMWR Morb Mortal Wkly Rep. 2002;51:123–126. [PubMed] [Google Scholar]
- 7.Reynolds J.C., Grunau B.E., Elmer J., et al. Prevalence, natural history, and time-dependent outcomes of a multi-center North American cohort of out-of-hospital cardiac arrest extracorporeal CPR candidates. Resuscitation. 2017;117:24–31. doi: 10.1016/j.resuscitation.2017.05.024. [DOI] [PubMed] [Google Scholar]
- 8.Bartos J.A., Grunau B., Carlson C., et al. Improved survival with extracorporeal cardiopulmonary resuscitation despite progressive metabolic derangement associated with prolonged resuscitation. Circulation. 2020;141:877–886. doi: 10.1161/CIRCULATIONAHA.119.042173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yannopoulos D., Bartos J.A., Martin C., et al. Minnesota resuscitation consortium’s advanced perfusion and reperfusion cardiac life support strategy for out-of-hospital refractory ventricular fibrillation. J Am Heart Assoc. 2016:5. doi: 10.1161/JAHA.116.003732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bartos J.A., Frascone R.J., Conterato M., et al. The Minnesota mobile extracorporeal cardiopulmonary resuscitation consortium for treatment of out-of-hospital refractory ventricular fibrillation: Program description, performance, and outcomes. EClinicalMedicine. 2020;29–30 doi: 10.1016/j.eclinm.2020.100632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bosson N., Kazan C., Sanko S., et al. Implementation of a regional extracorporeal membrane oxygenation program for refractory ventricular fibrillation out-of-hospital cardiac arrest. Resuscitation. 2023;187 doi: 10.1016/j.resuscitation.2023.109711. [DOI] [PubMed] [Google Scholar]
- 12.Tonna J.E., Johnson N.J., Greenwood J., et al. Practice characteristics of Emergency Department extracorporeal cardiopulmonary resuscitation (eCPR) programs in the United States: The current state of the art of Emergency Department extracorporeal membrane oxygenation (ED ECMO) Resuscitation. 2016;107:38–46. doi: 10.1016/j.resuscitation.2016.07.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stub D., Bernard S., Pellegrino V., et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial) Resuscitation. 2015;86:88–94. doi: 10.1016/j.resuscitation.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 14.Yannopoulos D., Bartos J., Raveendran G., et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396:1807–1816. doi: 10.1016/S0140-6736(20)32338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Belohlavek J., Yannopoulos D., Smalcova J., et al. Intraarrest transport, extracorporeal cardiopulmonary resuscitation, and early invasive management in refractory out-of-hospital cardiac arrest: an individual patient data pooled analysis of two randomised trials. EClinicalMedicine. 2023;59 doi: 10.1016/j.eclinm.2023.101988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Havranek S., Fingrova Z., Rob D., et al. Initial rhythm and survival in refractory out-of-hospital cardiac arrest. Post-hoc analysis of the Prague OHCA randomized trial. Resuscitation. 2022;181:289–296. doi: 10.1016/j.resuscitation.2022.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Updated: C·. Extracorporeal cardiopulmonary resuscitation (ECPR) for cardiac arrest: ALS TFSR. n.d. https://costr.ilcor.org/document/extracorporeal-cardiopulmonary-resuscitation-ecpr-for-cardiac-arrest-als-tfsr (accessed August 27, 2023).
- 18.Gottula A.L., Shaw C.R., Gorder K.L., et al. Eligibility of out-of-hospital cardiac arrest patients for extracorporeal cardiopulmonary resuscitation in the United States: A geographic information system model. Resuscitation. 2022;180:111–120. doi: 10.1016/j.resuscitation.2022.09.017. [DOI] [PubMed] [Google Scholar]
- 19.Grunau B., Scheuermeyer F.X., Stub D., et al. Potential candidates for a structured Canadian ECPR program for out-of-hospital cardiac arrest. CJEM. 2016;18:453–460. doi: 10.1017/cem.2016.8. [DOI] [PubMed] [Google Scholar]
- 20.Choi D.-H., Kim Y.-J., Ryoo S.M., et al. Extracorporeal cardiopulmonary resuscitation among patients with out-of-hospital cardiac arrest. Clin Exp Emerg Med. 2016;3:132–138. doi: 10.15441/ceem.16.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolf Creek XVII: Part 2. Resuscitation Plus 2023.
- 22.Wolf Creek XVII: Part 1. Resuscitation Plus 2023.
- 23.Bartos J.A. The rise of the machines: ECLS and other temporary mechanical support for patients with cardiac arrest. Resuscitation. 2020;151:208–210. doi: 10.1016/j.resuscitation.2020.04.017. [DOI] [PubMed] [Google Scholar]
- 24.Thiele H., Ohman E.M., de Waha-Thiele S., Zeymer U., Desch S. Management of cardiogenic shock complicating myocardial infarction: an update 2019. Eur Heart J. 2019;40:2671–2683. doi: 10.1093/eurheartj/ehz363. [DOI] [PubMed] [Google Scholar]
- 25.Yannopoulos D., Bartos J.A., Raveendran G., et al. Coronary artery disease in patients with out-of-hospital refractory ventricular fibrillation cardiac arrest. J Am Coll Cardiol. 2017;70:1109–1117. doi: 10.1016/j.jacc.2017.06.059. [DOI] [PubMed] [Google Scholar]
- 26.Bartos J.A., Carlson K., Carlson C., et al. Surviving refractory out-of-hospital ventricular fibrillation cardiac arrest: Critical care and extracorporeal membrane oxygenation management. Resuscitation. 2018;132:47–55. doi: 10.1016/j.resuscitation.2018.08.030. [DOI] [PubMed] [Google Scholar]
- 27.Kalra R., Bartos J.A., Kosmopoulos M., et al. Echocardiographic evaluation of cardiac recovery after refractory out-of-hospital cardiac arrest. Resuscitation. 2020;154:38–46. doi: 10.1016/j.resuscitation.2020.06.037. [DOI] [PubMed] [Google Scholar]
- 28.Gutierrez A., Carlson C., Kalra R., Elliott A.M., Yannopoulos D., Bartos J.A. Outcomes associated with delayed enteral feeding after cardiac arrest treated with veno-arterial extracorporeal membrane oxygenation and targeted temperature management. Resuscitation. 2021;164:20–26. doi: 10.1016/j.resuscitation.2021.04.029. [DOI] [PubMed] [Google Scholar]
- 29.Tonna J.E., Selzman C.H., Bartos J.A., et al. The association of modifiable mechanical ventilation settings, blood gas changes and survival on extracorporeal membrane oxygenation for cardiac arrest. Resuscitation. 2022;174:53–61. doi: 10.1016/j.resuscitation.2022.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alexy T., Kalra R., Kosmopoulos M., et al. Initial hospital length of stay and long-term survival of patients successfully resuscitated using extracorporeal cardiopulmonary resuscitation for refractory out-of-hospital cardiac arrest. Eur Heart J Acute Cardiovasc Care. 2023;12:175–183. doi: 10.1093/ehjacc/zuac141. [DOI] [PubMed] [Google Scholar]
- 31.Gutierrez A., Kalra R., Elliott A.M., Marquez A., Yannopoulos D., Bartos J.A. Acute lung injury and recovery in patients with refractory VT/VF cardiac arrest treated with prolonged CPR and veno-arterial extracorporeal membrane oxygenation. Resuscitation. 2023;182 doi: 10.1016/j.resuscitation.2022.11.017. [DOI] [PubMed] [Google Scholar]
- 32.Belohlavek J., Smalcova J., Rob D., et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: a randomized clinical trial. J Am Med Assoc. 2022;327:737–747. doi: 10.1001/jama.2022.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Suverein M.M., Delnoij T.S.R., Lorusso R., et al. Early extracorporeal CPR for refractory out-of-hospital cardiac arrest. N Engl J Med. 2023;388:299–309. doi: 10.1056/NEJMoa2204511. [DOI] [PubMed] [Google Scholar]
- 34.Neumar R.W., Nolan J.P., Adrie C., et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the international liaison committee on resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452–2483. doi: 10.1161/CIRCULATIONAHA.108.190652. [DOI] [PubMed] [Google Scholar]
- 35.Beyersdorf F., Trummer G., Benk C., Pooth J.-S. Application of cardiac surgery techniques to improve the results of cardiopulmonary resuscitation after cardiac arrest: Controlled automated reperfusion of the whole body. JTCVS Open. 2021;8:47–52. doi: 10.1016/j.xjon.2021.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trummer G., Benk C., Beyersdorf F. Controlled automated reperfusion of the whole body after cardiac arrest. J Thorac Dis. 2019;11:S1464–S1470. doi: 10.21037/jtd.2019.04.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kreibich M., Trummer G., Beyersdorf F., et al. Improved outcome in an animal model of prolonged cardiac arrest through pulsatile high pressure controlled automated reperfusion of the whole body. Artif Organs. 2018;42:992–1000. doi: 10.1111/aor.13147. [DOI] [PubMed] [Google Scholar]
- 38.Bougouin W., Dumas F., Lamhaut L., et al. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: a registry study. Eur Heart J. 2020;41:1961–1971. doi: 10.1093/eurheartj/ehz753. [DOI] [PubMed] [Google Scholar]
- 39.Scquizzato T., Hutin A., Landoni G. Extracorporeal cardiopulmonary resuscitation: prehospital or in-hospital cannulation? J Cardiothorac Vasc Anesth. 2023;37:755–757. doi: 10.1053/j.jvca.2023.01.015. [DOI] [PubMed] [Google Scholar]
- 40.Hsu C.H., Meurer W.J., Domeier R., et al. Extracorporeal cardiopulmonary resuscitation for refractory out-of-hospital cardiac arrest (EROCA): Results of a randomized feasibility trial of expedited out-of-hospital transport. Ann Emerg Med. 2021 doi: 10.1016/j.annemergmed.2020.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lamhaut L., Hutin A., Puymirat E., et al. A pre-hospital extracorporeal cardio pulmonary resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: An observational study and propensity analysis. Resuscitation. 2017;117:109–117. doi: 10.1016/j.resuscitation.2017.04.014. [DOI] [PubMed] [Google Scholar]
- 42.Bartos J.A., Clare Agdamag A., Kalra R., et al. Supraglottic airway devices are associated with asphyxial physiology after prolonged CPR in patients with refractory Out-of-Hospital cardiac arrest presenting for extracorporeal cardiopulmonary resuscitation. Resuscitation. 2023;186 doi: 10.1016/j.resuscitation.2023.109769. [DOI] [PubMed] [Google Scholar]
- 43.Perman S.M., et al. J Am Heart Assoc. 2016;5(10) doi: 10.1161/JAHA.116.003638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ciullo A.L., Wall N., Taleb I., et al. Effect of portable, in-hospital extracorporeal membrane oxygenation on clinical outcomes. J Clin Med Res. 2022:11. doi: 10.3390/jcm11226802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tonna J.E., Selzman C.H., Girotra S., et al. Resuscitation using ECPR during in-hospital cardiac arrest (RESCUE-IHCA) mortality prediction score and external validation. JACC Cardiovasc Interv. 2022;15:237–247. doi: 10.1016/j.jcin.2021.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Higashi A., Nakada T.-A., Imaeda T., Abe R., Shinozaki K., Oda S. Shortening of low-flow duration over time was associated with improved outcomes of extracorporeal cardiopulmonary resuscitation in in-hospital cardiac arrest. J Intensive Care Med. 2020;8:39. doi: 10.1186/s40560-020-00457-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.