Abstract
Children frequently present with symptoms of palpitations. These symptoms can occur in isolation or in association with other presentations such as chest pain, presyncope, or syncope. Usually, their symptoms are episodic in occurrence; therefore, establishment of symptom-rhythm correlation is challenging but critical for accurate diagnosis and management. We reviewed the use of smartphone-based wireless electrocardiogram monitoring with AliveCor Kardia, to establish symptom-rhythm correlation in a paediatric case series at a single Canadian tertiary care centre.
Résumé
Les enfants présentent fréquemment des symptômes de palpitations. Ces symptômes peuvent se produire isolément ou en association avec d’autres manifestations comme la douleur thoracique, la présyncope ou la syncope. Habituellement, les symptômes sont épisodiques, d’où la difficulté d’établir une corrélation entre les symptômes et le rythme cardiaque, un exercice pourtant essentiel pour poser un diagnostic précis et assurer la prise en charge du patient. Nous avons passé en revue les données relatives à la surveillance électrocardiographique sans fil effectuée au moyen d’un téléphone intelligent via la technologie Kardia d’AliveCor afin d’établir une telle corrélation dans une série de cas pédiatriques issue d’un même centre de soins tertiaires canadien.
Children frequently present with symptoms of palpitations. These symptoms can occur in isolation or in association with other symptoms such as chest pain, presyncope, or syncope that can be challenging for them to describe.1 As such, symptom-rhythm correlation is critical for accurate diagnosis, prognosis, and treatment recommendations. Success with conventional methods to establish symptom-rhythm correlation, such as Holter monitors or event recorders, is dependent on the duration of monitoring and occurrence of symptoms during the monitoring period.1 For longer duration monitoring, invasive implantable loop recorders are often used, which, for children, requires anaesthesia and sedation.
Symptom-rhythm correlation is challenging to obtain in children due to the paroxysmal nature of the arrhythmia, which may be of short duration. The yield of in-clinic electrocardiograms (ECGs) or Holter monitors to obtain this information is low.2 Furthermore, it can be difficult to maintain compliance with cardiac monitoring in a young child for longer ambulatory rhythm recording. Wireless ECG monitoring has been developed to allow recording of a single-lead ECG for 30 seconds using a smartphone app. AliveCor Kardia is a small portable device that connects to a smartphone via an application using ultrasonic proprietary technology.3 The 2 sensors on top detect the electrical signals and then filter them to create a single-lead ECG that is equivalent to lead I on a 12-lead ECG.4 The United States Food and Drug Administration has approved AliveCor in adults to identify atrial fibrillation.5 Multiple studies have already shown promising results when using AliveCor in the paediatric population.6 We reviewed the use of AliveCor in a single tertiary care paediatric cardiac centre to obtain symptom-rhythm correlation in children under 18 years of age, presenting with symptoms that are potentially consistent with an arrhythmia.
Cases
In 2021, the IWK Children’s Heart Centre purchased 10 AliveCor Kardia monitors for use in confirming symptom-rhythm correlation in paediatric patients presenting with symptoms potentially related to or attributable to an arrhythmia. Patients were given the device for 2-4 weeks, depending on the frequency of symptoms. Some families opted to purchase their own device to have it available for longer time, including a family who were able to document supraventricular tachycardia (SVT) in 2 brothers. Since recommending AliveCor Kardia to patients with palpitations suspicious for arrhythmias, we have had 5 patients who have used the device to successfully capture their heart rhythm during a symptomatic episode, and in whom the rhythms were confirmed to be consistent with a diagnosis of SVT. All patients had undergone previous testing, which had not revealed the diagnosis. In these patients, the AliveCor Kardia monitor aided in earlier diagnosis and treatment. Our sixth case involved the use of AliveCor Kardia for rhythm monitoring in an infant with a refractory form of SVT. In this case, the child’s family used the device at home to monitor breakthrough episodes of SVT while being managed with multiple antiarrhythmic medications. Details of these 6 cases are presented in Table 1.
Table 1.
Summary of cases
| Case | Age | Clinical presentation | Investigations | Emergency visit | ECG | AliveCor | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 11 y | Brief episodes of tachycardia, dizziness, and nausea every 1-2 wk | Multiple normal Holters and event recorders | Yes | Normal | SVT | Intolerance of medical therapy. Referred for ablation |
| 2 | 13 y∗ | Intermittent palpitations twice a year | Multiple normal Holters | Yes | Normal | SVT (atrioventricular nodal re-entry tachycardia) initially and confirmed sinus tachycardia after ablation for recurrence of symptoms | Intolerance of medical therapy. Successful ablation |
| 3 | 2 mo∗ | History of incessant multifocal atrial ectopic tachycardia and atrial flutter | Multiple normal Holters | Yes, hospitalized for months to treat arrhythmia and structural heart disease | Ectopic atrial rhythm | SVT (atrial flutter and atrial ectopic tachycardia) | Captured SVT previously noted to be atrial flutter and reassuring sinus rhythm. Managed with multiple antiarrhythmic agents |
| 4 | 12 y | Palpitations with chest pain, excessive sweating, and presyncope | None | No | Normal | SVT (atrioventricular re-entry type SVT) | Vagal manoeuvres |
| 5 | 14 y | Palpitations occasionally triggered by exercise. Occasional presyncope. SVT was captured on an event recorder initially but continued to have symptoms after ablation | Multiple normal Holters, exercise stress test, and event recorder | Yes | Normal | SVT (atrioventricular nodal re-entry tachycardia) recurred after first ablation | Restarted on medication and then had successful second ablation |
| 6 | 12 y | Intermittent palpitations with chest pain 1-2 times a month mainly with light exercise | Holters, multiple event recorders, and exercise test | Yes | Normal | SVT | Managed with nadolol |
ECG, electrocardiogram; SVT, supraventricular tachycardia.
Discussed in further details.
Most of the cases had a typical presentation for SVT; however, we believe that 2 cases had a unique course for their supraventricular arrhythmia including their management.
Case 2 in Table 1 is a teenage girl who at 10 years of age presented with an episode of palpitations after swimming, which resolved spontaneously. She had a past medical history of asthma and attention deficit and hyperactivity disorder treated with atomoxetine. Her physical examination and ECG were normal. At 12 years of age, she had intermittent palpitations occurring twice a year and was fully investigated with standard tests. Multiple Holters failed to establish any symptom-rhythm correlation. She had multiple visits to the emergency department for palpitations; however, her symptoms had consistently subsided before reaching the hospital. Therefore, the family purchased an AliveCor Kardia device.
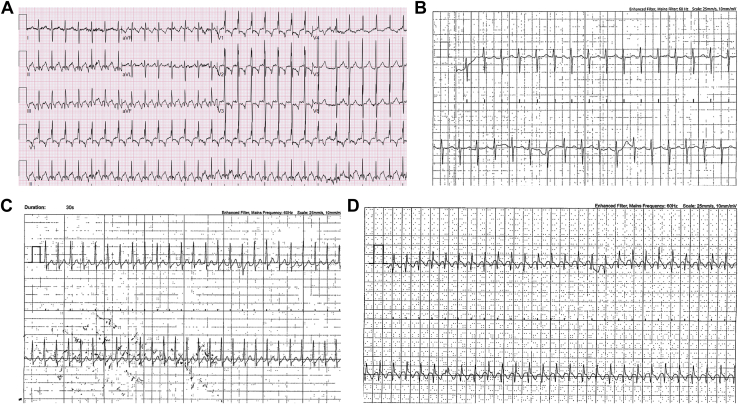
A year later, she developed sudden onset of palpitations while hiking with schoolmates, and she used her AliveCor Kardia device to document an episode of SVT (Fig. 1D) with a rate of 200 beats per minute. She ultimately underwent invasive electrophysiology study and slow pathway modification with radiofrequency ablation for typical atrioventricular (AV) nodal re-entry tachycardia. After the ablation, she had several recurrences of palpitations, but her AliveCor was able to document sinus tachycardia, which provided reassurance to the patient and her care providers.
Figure 1.
(A) 12-lead ECG demonstrating 2:1 atrial flutter and (B) AliveCor tracing showing possible 2:1 atrial flutter with a fixed heart rate of 140 bpm in a 2-month-old baby with incessant SVT (C) AliveCor tracing in a 12-year-old boy showing SVT, which later was diagnosed as AVRT. (D) AliveCor tracing in a 13-year-old girl showing SVT, which was later shown to be AVNRT. AVNRT, atrioventricular nodal re-entrant tachycardia; AVRT, atrioventricular reciprocating tachycardia; ECG, electrocardiogram; SVT, supraventricular tachycardia.
Another case was of an infant who presented at a regional centre at 2 days of age with incessant tachycardia (heart rate [HR] 180-190 bpm). Atrial flutter was documented on ECG with variable AV conduction (Fig. 1A), and he was treated with a β-blocker. He was subsequently diagnosed with coarctation of the aorta requiring surgical repair at 2 weeks of age. His serial ECGs and hospital telemetry after coarctation repair showed multifocal atrial tachycardia. He was discharged home on propranolol and digoxin with reasonable rhythm and rate control.
Unfortunately, he developed a recoarctation of the aorta and was readmitted at 2 months of age after cardiac catheterization for balloon dilatation of his aorta. During this hospital stay, he continued to have breakthrough episodes of atrial flutter (HR 170-180 bpm) with variable AV node conduction requiring oesophageal overdrive pacing and cardioversion. Digoxin was discontinued, and then flecainide was added with the goal of rhythm control. He was discharged home on flecainide, propranolol, sotalol, and acetylsalicylic acid.
He was followed as an outpatient and had Holters that showed sinus rhythm with rare intermittent ectopic atrial rhythm and/or atrial flutter. His medical therapy was modified accordingly. Because of family circumstances and logistics, the family purchased an AliveCor monitor and was able to capture his rhythm by placing the device on his chest. They sent multiple transmissions that documented either sinus rhythm or SVT (Fig. 1B). He continued to be managed with flecainide, propranolol, and sotalol. In his case, the device helped the cardiology team monitor his rhythm frequently to optimize his rate control and ultimately rhythm control, thereby avoiding the need for additional Holters and hospital visits. At his last visit at 16 months of age, he remained asymptomatic on single-agent therapy with sotalol, with no recently documented sustained arrhythmia.
Discussion
This small case series demonstrates the application of smartphone-based wireless ECG monitoring using AliveCor Kardia in children, resulting in a high-quality single-lead ECG. It also affirms earlier studies and demonstrates that AliveCor can be used both for initial diagnosis in paediatric patients with palpitations and as a management support tool in subsequent follow-up. Studies have already begun to look at the utility of using this device more broadly in the paediatric population. Nguyen et al.6 found that the AliveCor device was able to consistently and accurately detect HR and rhythm in the mid to upper 200 bpm range.
AliveCor is a suitable technology for patients with infrequent paroxysmal arrhythmias that are difficult to capture with conventional ambulatory ECG recorders such as Holters or event recorders. The most common arrhythmia in children is SVT. The 2 most common forms of SVT are AV re-entry tachycardia and AV nodal re-entry tachycardia. AliveCor has been shown to produce high-quality ECGs and may even be able to differentiate between these 2 common forms of SVT. Ferdman et al7 used AliveCor to distinguish AV re-entrant tachycardia from AV nodal re-entrant tachycardia by recording a strip with the AliveCor in 3 different positions on the chest. This is a promising study as AliveCor could be used not only to capture SVT but also to determine the specific type of SVT, which may aid in determination of the treatment and prognosis.
This case series demonstrates the utility of this device in different ages, including infants, for both diagnosis and management monitoring. Our patients ranged in age from 2 months to 14 years. This device has been shown to be used easily and independently by teenagers. In addition, our local experience shows that it can also be used on infants if parents or other caregivers are able to place the device on the child’s chest. This is valuable as attempting to obtain a Holter monitor or maintain lead attachments for an event monitor on an active infant can be very challenging.
Parents and families are sometimes frustrated by diagnostic uncertainty, prevailing even after multiple diagnostic tests. Our clinical case series confirms earlier reports that the AliveCor monitor is user friendly and was able to establish symptom-rhythm correlation, thereby providing more definitive answers to patients and their families about the nature of the patients’ symptoms. This can provide much needed reassurance if symptoms are found to be unrelated to an arrhythmia or allow more timely treatment of arrhythmias if a rhythm disturbance is diagnosed. This finding was confirmed by Peritz et al,4 who used AliveCor monitoring in 6 symptomatic athletes complaining of palpitations during exercise. These athletes were able to record and send an ECG strip wirelessly immediately to the team cardiologist confirming their normal sinus rhythm and allowing them to continue playing.4
Conclusion
Smart phone–based wireless ECG monitoring, such as AliveCor, is an excellent option for paediatric patients with infrequent symptoms or who are unsuccessful in establishing symptom-rhythm correlation via conventional investigation methods using Holter monitors or event recorders. Given that AliveCor is portable and equipped with wireless technology, patients have a higher likelihood of capturing even brief arrhythmias. This small case series also reiterated that AliveCor was able to capture and help with the diagnosis of arrhythmias and guide timely management. AliveCor was also beneficial and convenient for parents with infants for therapeutic monitoring of their underlying rhythm disorder. As this type of technology continues to improve and becomes more readily available, AliveCor and similar direct-to-consumer monitors may become an even more important tool in the diagnosis and management of infrequent arrhythmias in the paediatric population.
Acknowledgments
Ethics Statement
This research has adhered to IWK research board ethical guidelines.
Funding Sources
No funding was received for this study.
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Salerno J., Seslar S. Supraventricular tachycardia. Arch Pediatr Adolesc Med. 2009;163:268–274. doi: 10.1001/archpediatrics.2008.547. [DOI] [PubMed] [Google Scholar]
- 2.Gropler M.R.F., Dalal A.S., Van Hare G.F., Silva J.N.A. Can smartphone wireless ECGs be used to accurately assess ECG intervals in pediatrics? A comparison of mobile health monitoring to standard 12-lead ECG. PLoS One. 2018;13:1–9. doi: 10.1371/journal.pone.0204403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.AliveCor. https://www.kardia.com Available at:
- 4.Peritz D.C., Howard A., Ciocca M., Chung E.H. Smartphone ECG AIDS real time diagnosis of palpitations in the competitive college athlete. J Electrocardiol. 2015;48:896–899. doi: 10.1016/j.jelectrocard.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Lau J.K., Lowres N., Neubeck L., et al. IPhone ECG application for community screening to detect silent atrial fibrillation: a novel technology to prevent stroke. Int J Cardiol. 2013;165:193–194. doi: 10.1016/j.ijcard.2013.01.220. [DOI] [PubMed] [Google Scholar]
- 6.Nguyen H.H., Van Hare G.F., Rudokas M., Bowman T., Silva J.N.A. SPEAR trial: smartphone pediatric electrocardiogram trial. PLoS One. 2015;10:1–9. doi: 10.1371/journal.pone.0136256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferdman D.J., Liberman L., Silver E.S. A smartphone application to diagnose the mechanism of pediatric supraventricular tachycardia. Pediatr Cardiol. 2015;36:1452–1457. doi: 10.1007/s00246-015-1185-6. [DOI] [PubMed] [Google Scholar]