Abstract
Background
Congenital heart disease is the most common congenital birth defect and presents with differing degrees of complexity. Patients require lifelong specialized care. The transfer from paediatric to adult care is a time of risk that may result in lapses or loss of care. A successful transfer from paediatric to adult care is integral for improved patient outcomes.
Methods
In this retrospective study, we used the paediatric cardiology database and the electronic records at the adult congenital heart disease (ACHD) clinic to identify referrals and successful transfer between 2008 and 2017. Successful transfer was defined as a patient referred to the ACHD clinic who was seen in the clinic and has ongoing follow-up. We also sought to identify predictors of a successful transfer.
Results
A total of 555 patients were referred to the ACHD clinic (2008-2017). Of all patients referred, 62% had a successful transfer and an ongoing specialist care. The remaining 38% either did not show for first appointments or missed 3 consecutive visits. Independent predictors of a successful transfer were the presence of moderate or complex ACHD, residing within the city limits, older age at the time of referral, and a more recent year of referral.
Conclusions
Over one-third of patients did not achieve successful transfer, namely attendance at first clinic visit plus early retention in care. We were able to identify several variables that predict successful transfer. Further research is required to identify interventions that can be implemented to reduce lapses in patient care.
Résumé
Contexte
La cardiopathie congénitale, qui est la malformation congénitale la plus courante, présente divers degrés de complexité. Les patients qui en sont atteints nécessitent des soins spécialisés tout au long de leur vie. La transition entre les soins pédiatriques et les soins pour adultes est un moment risqué qui peut occasionner un relâchement ou une interruption des soins. Le succès de ce transfert des soins pédiatriques aux soins pour adultes est essentiel à l’amélioration des résultats pour les patients.
Méthodologie
Pour cette étude rétrospective, nous avons utilisé la base de données de cardiologie pédiatrique et les dossiers électroniques de la clinique de cardiopathie congénitale de l’adulte (CCA) pour relever les cas de réorientation et de transfert réussi survenus entre 2008 et 2017. On entendait par « transfert réussi » le fait qu’un patient orienté vers la clinique de CCA ait été vu en consultation à la clinique et qu’il fasse l’objet d’un suivi. Nous avons aussi cherché à identifier les facteurs prédictifs d’un transfert réussi.
Résultats
Au total, 555 patients ont été orientés à la clinique de CCA entre 2008 et 2017. Chez 62 % de tous ces patients orientés, le transfert a été réussi et les soins spécialisés ont été poursuivis. Les patients représentant les 38 % restants ne se sont pas présentés soit à leur premier rendez-vous, soit à trois visites subséquentes consécutives. Les facteurs prédictifs indépendants du transfert réussi étaient la présence d’une CCA modérée ou complexe, le fait de résider à l’intérieur des limites de la ville, un âge plus avancé au moment de la réorientation et le caractère plus récent de la réorientation.
Conclusions
Chez plus du tiers des patients, le transfert n’a pas été réussi, c’est-à-dire que ces patients ne se sont pas présentés à leur première visite à la clinique et que leurs soins n’ont pas été poursuivis rapidement après le transfert. Nous avons pu cerner plusieurs variables qui prédisent les transferts réussis. D’autres recherches seront nécessaires pour trouver les interventions à mettre en œuvre pour réduire les interruptions dans les soins aux patients.
Nearly 8 of 1000 live births are affected by congenital heart disease (CHD), making it the most common birth defect.1 Approximately 90% of children born with CHD survive into adulthood due to advances in paediatric cardiology and cardiac surgery.2 Adult patients with CHD require lifelong follow-up and management to improve outcomes.3,4 In Canada, there are 15 major centres providing specialized care to patients with adult congenital heart disease (ACHD). Because of the geography and distribution of the population, resources among these specialized centres differ. Certain centres have advanced congenital cardiac surgery and transplant facilities, but all centres provide diagnostic investigations and outpatient clinic visits. Approximately 2000 adult patients are followed in the ACHD clinic in Winnipeg, Manitoba, with greater than 6000 ACHD estimated in our catchment area with our population of 1,380,000, based on birth rates and survival to adulthood.
Patients living with CHD require lifelong management with appropriate follow-up. It has been shown that successful transfer of care is associated with improved outcomes including well-being and survival. Furthermore, patients with CHD are at an increased risk of poor outcomes when compared with the age-matched non-CHD population.5,6 A meta-analysis demonstrated that 3.6%-62.7% of patients with ACHD do not complete the transfer process resulting in long gaps in care, and in more extreme situations, there is a complete discontinuation in care.6
Transfer of care in CHD has typically been characterized as a one-time event where the responsibility for patient care moves from one health care team to another in late adolescence or early adulthood. Transition of care is a large process that may occur over years in adolescence and early adulthood in which the management of patient care shifts from the family and paediatric team to the patient and adult team.7 The model of transfer of care from paediatric to adult care may differ depending on the centre but is part of the overall transition process. At our centre, a “successful transfer” process involves the transfer of care to the ACHD clinic with follow-up in a timely manner as specified by the paediatric cardiologist, as well as ongoing follow-up at the ACHD clinic. With this study we sought to examine the variables that predict successful transfer from the paediatric cardiology clinic to the ACHD clinic.
Methods
We conducted a retrospective review of all patients with CHD referred from the paediatric cardiology clinic to the ACHD clinic at our academic centre (Winnipeg, Manitoba, Canada) between 2008 and 2017.
Current standard of care at our institution
The paediatric cardiology clinic and ACHD clinic in Winnipeg are the only clinics providing specialized cardiac care for CHD across the entire province of Manitoba, with extended catchment areas to parts of western Ontario, eastern Saskatchewan, and the Nunavut. At our centre, the standard transfer process involves referring paediatric patients to the ACHD clinic through a standard referral letter. The paediatric cardiology team explains the patient’s medical history and recommends the appropriate time for follow-up in the letter. Once the letter and patient file has been received, the ACHD clinic contacts the patient through both a phone call and mail to set up an appointment. In the situation where a patient missed his or her appointment, the ACHD clinic attempts to reschedule an appointment. The paediatric clinic is also contacted when a patient fails to attend his or her first appointment in the ACHD clinic. The paediatric clinic will also send a reminder to the patient to attend his or her appointment. Over the course of a year, 3 additional attempts are made to reschedule the appointment. After 3 failed attempts to reschedule an appointment, the patient requires a new referral from the paediatric team or other physician.
To support the transfer process our centre instituted annual transfer information sessions between 2010 and 2015. These sessions were done once annually and were patient lead and focused. Paediatric patients and their families, identified by the nursing staff at the paediatric clinic, who were planned for transfer to adult care that year were invited to join a meeting held in person in Winnipeg. Patient selection was at the discretion of the paediatric team and typically included 20 patients (and family) with moderate or complex disease with upcoming adult clinic visits, primarily within the next year, as well as patients with social or other reasons for increased health care support. The voluntary session was led by patients with ACHD who successfully transferred from the paediatric to adult clinic and joined by a paediatric cardiology nurse and a member of the ACHD team, where they would share their experience in a question-and-answer session. The format of the session was nonstandardized. A tour of the ACHD facility was also offered after the meeting. These voluntary sessions were developed to help promote patient engagement in their care and successful transfer of care.
Study population
The paediatric heart centre database was used to identify all the eligible referrals to the ACHD clinic, and the electronic patient record at the adult clinic was used to determine the establishment of care and success of transfer of care. Patients were included if they had documented CHD (International Classification of Diseases [9th revision] codes 745-747 or International Classification of Diseases [10th revision] Q20-Q26), and patients without one of these diagnoses were excluded from analysis. Patients were excluded from the study if (1) they relocated to a different province and transferred to another ACHD centre or (2) the date of transfer extended beyond the study period. Disease complexity was divided into simple, moderate, or complex, defined by previously established criteria.8
Study variables
The primary aim of the study was to identify variables that affect successful transfer to the ACHD clinic. Transfer was considered successful if the following criteria were met by the patient: (1) attendance at the ACHD clinic within 1 year of the time frame recommended by the paediatric cardiology team (this allowed time for 3 attempts at rescheduling missed appointments), and (2) retention in care, defined as not missing 3 consecutive ACHD visits, no interruptions in planned care. The following data were collected to investigate whether they were predictors of successful transfer: sex, age at transfer and first adult visit, postal code (to determine whether the patient resided within city limits), cardiac anatomy, and complexity. Patients with more than 1 congenital heart defect were categorized by the most complex lesion.
Statistical analysis
The characteristics of the study population were summarized using means and standard deviations for continuous variables and absolute numbers and percentages for categorical variables. Factors associated with “successful transfer” were assessed via a multivariable logistic regression model including clinically relevant variables (age, sex, residence outside the city, lesion, and year of referral). The final model included age at referral, sex, disease complexity, year of referral, and residing in an urban (within city limits) vs rural (outside city limits) setting. All P values presented were 2-tailed; P values <0.05 were considered statistically significant. All statistical analysis was performed using SAS Version 9.4 (SAS Institute, Cary, NC).
Results
Participant characteristics
We identified 656 patients who were referred to the ACHD clinic during the study period (2008-2017). One hundred one patients had delayed referral for simple disease, or prior referral and follow-up by general cardiology, electrophysiology, or heart failure specialists, with no shared care with the ACHD clinic. These patients were excluded from the study, leaving 555 patients eligible to be evaluated for successful transfer to the ACHD clinic. Demographics of the patient population are listed in Table 1.
Table 1.
Characteristics of patients referred to the ACHD clinic—January 2008 to July 2017
| Characteristic | Total sample (N = 555) | Successful transfer∗ (N = 346) |
|---|---|---|
| Demographics | ||
| Age at referral (SD) | 17.0 (1) | 17.1 (1) |
| Age seen in ACHD (SD) | – | 19.2 (2) |
| Female sex (%) | 250 (45) | 152 (61) |
| Male sex (%) | 305 (55) | 194 (64) |
| Living outside the city (%) | 281 (51) | 166 (48) |
| CHD complexity | ||
| Simple (%) | 218 (39) | 113 (52) |
| Moderate (%) | 241 (43) | 154 (64) |
| Complex (%) | 96 (17) | 79 (82) |
Continuous variables expressed as mean (SD); categorical variables expressed as N (%).
ACHD, adult congenital heart disease; CHD, congenital heart disease; N, number; SD, standard deviation.
Successful transfer defined as being seen in the ACHD clinic and receiving ongoing care.
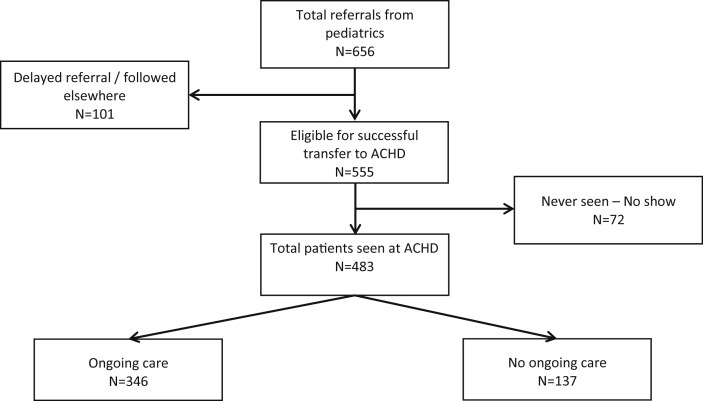
Rate of successful transfer
Of 555 patients who were referred to the ACHD clinic, 346 (62%) had successful transfer (Fig. 1), namely, attendance at the first ACHD clinic visit plus retention in care. Of the remaining 209 patients, 72 (13%) did not attend any appointments in the ACHD clinic and 137 (25%) attended at least 1 ACHD visit before missing at least 3 consecutive clinic visits (ie, no retention in care).
Figure 1.
Flow sheet of patients referred from paediatric to ACHD care—January 2008 to July 2017. ACHD, adult congenital heart disease; N, number of patients.
Exploration of potential correlates of successful transfer
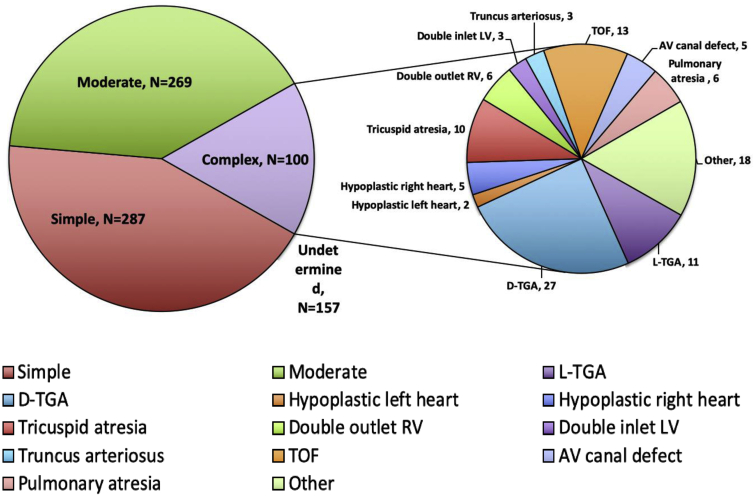
Patients were categorized according to their primary heart defect (Fig. 2) and complexity, divided into simple, moderate, and complex lesions.8 Of 218 patients with simple CHD, 113 (52%) had successful transfer. Of 241 patients with moderate CHD, 154 (64%) had successful transfer. Of 96 patients with complex CHD, 79 (82%) had successful transfer.
Figure 2.
All referrals to the ACHD clinic by disease complexity—January 2008 to July 2017. Detailed breakdown of the congenital heart disease by degree of complexity and underlying diagnosis. ACHD, adult congenital heart disease; AV, atrioventricular; D-TGA, dextro-transposition of the great arteries; L-TGA, levo-transposition of the great arteries; LV, left ventricle; N, number; RV, right ventricle; TOF, tetralogy of Fallot.
Of the 250 female patients referred for transfer, 152 (61%) had successful transfer. Of the 305 male patients referred for transfer, 194 (64%) had successful transfer. The mean age of referral for patients who successfully transferred into the ACHD clinic was 17.1 with a standard deviation of 1 year.
Our single-centre catchment area is wide, spanning 1,545,017 km2, with some patients requiring prolonged ground or air transportation to attend investigations and clinic visits, which may not be coordinated on the same day. Of 281 patients living in nonurban communities, 166 (48%) had successful transfer (Table 1).
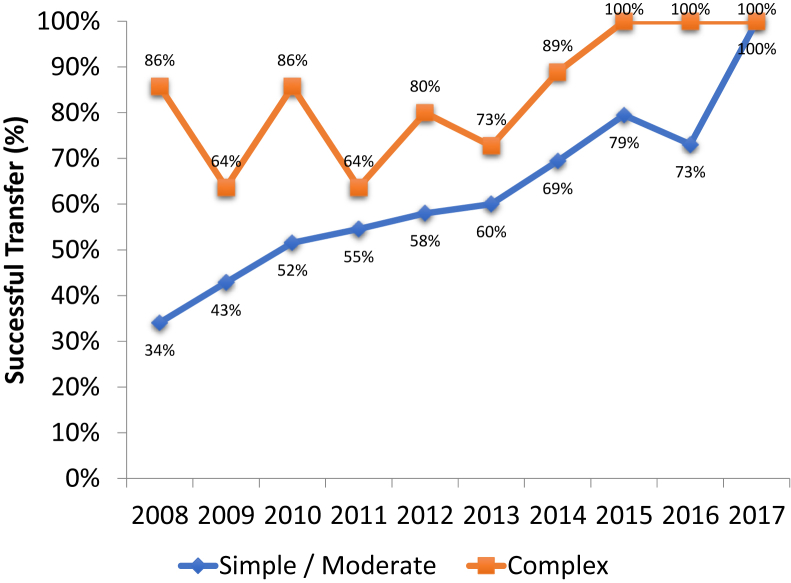
The most recent years of referral were associated with higher rate of transfer success. This coincided with the institution of the transfer information sessions, though a causation could not be established. In the period during which the transfer information sessions were implemented, a continued upward trend of success was noted. The rate had improved from 73% by the end of the year 2014, to around 100% by the end of 2017 (Fig. 3).
Figure 3.
Successful transfer from paediatric to adult care—January 2008 to July 2017. This graph depicts the rates of successful transfer of patients with simple/moderate and complex cardiac defects from paediatric cardiology to the adult congenital heart disease clinic over the years.
Multivariate analysis demonstrated that the presence of moderate and complex disease was associated with a higher rate of successful transfer. An older age at the time of referral was associated with increased rate of successful transfer, whereas patients living in nonurban communities had lower rates of successful transfer (Table 2). There was no difference in the rates of successful transfer between male and female patients.
Table 2.
Predictors of successful transfer based on multivariable regression∗—January 2008 to July 2017
| Characteristic | Odds ratio | 95% confidence interval | P value |
|---|---|---|---|
| Demographics | |||
| Age at referral (per year) | 1.26 | 1.03-1.54 | 0.022 |
| Sex (female) | 0.89 | 0.61-1.29 | 0.520 |
| Living within the city limits | 1.49 | 1.03-2.17 | 0.034 |
| Patient type | |||
| Moderate vs simple | 1.50 | 1.01-2.23 | 0.044 |
| Complex vs simple | 3.88 | 2.10-7.16 | <0.001 |
| Year of referral (per year) | 1.26 | 1.16-1.35 | <0.001 |
ACHD, adult congenital heart disease.
Successful transfer defined as being seen in the ACHD clinic and receiving ongoing care. Over the study period, a total of 346 of 555 (62.3%) patients who were referred had successful transfer.
Discussion
There is no true cure for CHD, and consequently the care and management of CHD is a lifelong process. It has been well established that ongoing specialist care at an ACHD clinic is associated with improved survival.9 Studies to date have demonstrated that many paediatric patients do not have a successful transfer from paediatric to ACHD care, which can result in adverse patient outcomes.10, 11, 12 The transfer from paediatric to adult care is a critical time for patients with CHD. Our findings suggest that a more robust process than direct referral from the paediatric to adult clinic is required to maintain patient engagement and continuity of care.
Over one-third of the patients in this study did not achieve successful transfer according to our definition. We demonstrated that complex congenital heart lesions and older age at the time of referral favour successful transfer from paediatric to ACHD care. In contrast, patients living in rural communities were less likely to experience successful transfer compared with their counterparts living within the city. Although our transfer information sessions were instituted to help improve transfer success, their overall efficacy is challenging to measure and a more robust program is required to maintain patient engagement.
At the Hospital for Sick Children in Toronto, ON, Canada, Reid et al.10 selected 360 patients with complex CHD (aged 19-21) to investigate medical care after their transfer from paediatric care. They found that 53% of this population had an unsuccessful transfer. In this study it was found that successful transfer of care was more common in: patients who were older at the last peadiatric heart disease clinic visit, patients who believed ongoing clinical care was important and patients who had documented recommendations for ongoing adult follow up by their paediatric cardiologist.10
A study conducted in Quebec by Mackie et al.11 found similar rates of cardiology follow-up in adulthood. After the 18th birthday of patients with CHD, 61% of patients were lost to follow-up. Unsuccessful transfer to adult care was significantly associated with male sex and cardiology visits outside a university hospital setting. In addition, Mackie et al. found that low complexity heart lesions predicted against successful transfer of care.
The findings from our study are in agreement with Mackie et al.11 and Reid et al.10 However, their definition of successful transfer was attendance to at least 1 cardiac follow-up appointment. The definition used in our study mandates that patients have no interruptions in long-term follow-up. The definition of successful transfer used in other studies is an event that occurs where the responsibility of patients is moved from the paediatric clinic to an adult clinic. For our study we expanded the definition of successful transfer to emphasize the initial ACHD clinic visit, but also the importance in continuity of specialized care. The purpose of using our expanded definition was to identify variables that impact continuity in patient care. This will help providers identify patients at risk of being lost to follow-up. As studies have demonstrated increased mortality in patients without long-term ACHD follow-up, our experience, though suboptimal, is not unique.5 The results from our study suggest that patients with complex congenital heart lesions are more likely to have successful transfer from paediatric to adult care, which was also demonstrated by Mackie et al.11 Lower complexity heart lesions may not require routine specialized CHD follow-up in adulthood but may still require general cardiology follow-up.
A recent study by Mondal et al.13 from McMaster found that the proximity of the ACHD clinic to the patient’s residence is an important variable in the successful transfer of care. This is in line with the findings from our study. Patients living in rural communities were less likely to have successful follow-up. Possible explanations for this include patients living outside the city experience transportation/accommodation costs related to attending ACHD visits in addition to time off work for themselves and/or their family members escorting them to their appointments.14 Using telehealth or virtual clinic visits to bridge the discordance in follow-up may be a possible future solution to this problem, ensuring more equitable access to specialized care.
In addition to the previous variables affecting successful transfer, we identified age as a factor that potentially impacts successful transfer. Currently, there is no consensus on the optimal age for transfer in patients with CHD. In our multivariable model after controlling for complexity of disease, sex, and geographical location, older age at the initiation of the transfer process was associated with successful transfer. A systematic review of papers published between January 2001 and May 2013 by Heery et al.15 revealed that younger patients were more likely to be lost to follow-up because they had poor understanding of their disease and the importance of lifelong follow-up. Older patients may possess greater maturity and engage in medical care.16 Also, older patients are seen sooner in the ACHD clinic because they are closer to adulthood. Younger patients may have a longer gap between the time of referral and the initial clinic visit (eg, referral at 15 years to be seen in the ACHD clinic at 19 years). As a result, these patients may forget about their appointment, may not remember the reason for ongoing care, and have new residence or contact information not available to the ACHD clinic. These are potential reasons why an older age at the time of referral (18-19 years) may be associated with higher rates of successful transfers to ACHD care. It is also possible that referral at younger age with planned adult follow-up may be more common in simple lesions, which may be a confounding factor in lapses in care.
A systematic review by Yassaee et al.17 found evidence to suggest that the relationship is also seen in patients with noncardiac chronic conditions. Paediatric patients at older ages are likely to have greater understanding of their disease process and greater developmental maturity. The lack of maturity was found to be a negative predictor of successful transfer in paediatric patients with inflammatory bowel disease.18 Therefore, the transfer process should factor in these variables in addition to age when assessing a patient’s readiness to transfer. Although age alone is likely not the only factor at play in achieving successful transfer, individualized care plans considering patient maturity, needs, and understanding are all important components of patient engagement.
Transition programs and future research
Because of the importance of continued care, many centres are promoting and creating transition programs, clinics, and services.13,19, 20, 21, 22 The ideal program has not yet been established and may be centre and patient population specific. Mackie et al.23,24 demonstrated that with nurses lead, 1 on 1 education sessions, participants were 1.8 times more likely to have their adult CHD appointment within 1 month relative to those in usual care, indicating higher probability for successful transfer to adult care. The results of this study along with existing literature may help clinicians identify patients in the process of transferring to the ACHD at risk of being lost to follow-up.10,11,13,15 Further research is required to identify targeted strategies and interventions that can be implemented to reduce lapses in patient care. Such strategies may include the use of virtual care for patients with residence far from a care centre or implementing a transition process spanning several years at the paediatric clinic before formal transfer to ACHD care.
Study limitations
Our study was a retrospective chart review and subject to the limitations thereof. Information on why patients did not attend their first or subsequent ACHD visits was incomplete and did not capture reasons such as ongoing out of province care, relocation, or death. The overall study period was relatively short and cannot provide the true picture of lost to follow-up over a patient’s lifespan, and some of the improved success rates in later years may overestimate true retention in care as those patients have not yet had as much opportunity for lapses in care. Transfer information sessions were not standardized, and their overall effect is challenging to characterize.
Conclusions
For patients transferring from paediatric to adult care in our centre, we found a suboptimal rate of successful transfer and ongoing care. Despite this, our findings demonstrate that complex cardiac defects and older age at the time of referral predict successful transfer to ACHD clinics. On the contrary, living in rural communities predicts against successful transfer. Further research is required to expand determinants of successful transfer and to develop programs aimed to improve CHD care for all patients, over their lifetime.
Ethics Statement
This research was approved by the institutional research ethics board.
Acknowledgments
Funding Sources
No funding was received for this study.
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Hoffman J.I., Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–1900. doi: 10.1016/s0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 2.Moons P., Bovijn L., Budts W., Belmans A., Gewillig M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation. 2010;122:2264–2272. doi: 10.1161/CIRCULATIONAHA.110.946343. [DOI] [PubMed] [Google Scholar]
- 3.Wray J., Frigiola A., Bull C. Loss to specialist follow-up in congenital heart disease; out of sight, out of mind. Heart. 2013;99:485. doi: 10.1136/heartjnl-2012-302831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Webb G.D., Williams R.G. 32nd Bethesda Conference: “care of the adult with congenital heart disease”. J Am Coll Cardiol. 2001;37:1162–1165. doi: 10.1016/s0735-1097(01)01280-3. [DOI] [PubMed] [Google Scholar]
- 5.Yeung E., Kay J., Roosevelt G.E., Brandon M., Yetman A.T. Lapse of care as a predictor for morbidity in adults with congenital heart disease. Int J Cardiol. 2008;125:62–65. doi: 10.1016/j.ijcard.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 6.Moons P., Skogby S., Bratt E.L., et al. Discontinuity of cardiac follow-up in young people with congenital heart disease transitioning to adulthood: a systematic review and meta-analysis. J Am Heart Assoc. 2021;10 doi: 10.1161/JAHA.120.019552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blum R.W., Garell D., Hodgman C.H., et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. a position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993;14:570–576. doi: 10.1016/1054-139x(93)90143-d. [DOI] [PubMed] [Google Scholar]
- 8.Warnes C.A., Liberthson R., Danielson G.K., et al. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001;37:1170–1175. doi: 10.1016/s0735-1097(01)01272-4. [DOI] [PubMed] [Google Scholar]
- 9.Mylotte D., Pilote L., Ionescu-Ittu R., et al. Specialized adult congenital heart disease care. Circulation. 2014;129:1804–1812. doi: 10.1161/CIRCULATIONAHA.113.005817. [DOI] [PubMed] [Google Scholar]
- 10.Reid G.J., Irvine M.J., McCrindle B.W., et al. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics. 2004;113:e197–205. doi: 10.1542/peds.113.3.e197. [DOI] [PubMed] [Google Scholar]
- 11.Mackie A.S., Ionescu-Ittu R., Therrien J., et al. Children and adults with congenital heart disease lost to follow-up: who and when? Circulation. 2009;120:302–309. doi: 10.1161/CIRCULATIONAHA.108.839464. [DOI] [PubMed] [Google Scholar]
- 12.Wacker A., Kaemmerer H., Hollweck R., et al. Outcome of operated and unoperated adults with congenital cardiac disease lost to follow-up for more than five years. Am J Cardiol. 2005;95:776–779. doi: 10.1016/j.amjcard.2004.11.036. [DOI] [PubMed] [Google Scholar]
- 13.Mondal T.K., Muddaluru V., Jaafar A., et al. Transition of adolescents with congenital heart disease from pediatric to adult congenital cardiac care: lessons from a retrospective cohort study. J Trans Med. 2020;2:20190003. [Google Scholar]
- 14.Syed S.T., Gerber B.S., Sharp L.K. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38:976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heery E., Sheehan A.M., While A.E., Coyne I. Experiences and outcomes of transition from pediatric to adult health care services for young people with congenital heart disease: a systematic review. Congenit Heart Dis. 2015;10:413–427. doi: 10.1111/chd.12251. [DOI] [PubMed] [Google Scholar]
- 16.Mackie A.S., Rempel G.R., Islam S., et al. Psychosocial maturity, autonomy, and transition readiness among young adults with congenital heart disease or a heart transplant. Congenit Heart Dis. 2016;11:136–143. doi: 10.1111/chd.12300. [DOI] [PubMed] [Google Scholar]
- 17.Yassaee A., Hale D., Armitage A., Viner R. The impact of age of transfer on outcomes in the transition from pediatric to adult health systems: a systematic review of reviews. J Adolesc Health. 2019;64:709–720. doi: 10.1016/j.jadohealth.2018.11.023. [DOI] [PubMed] [Google Scholar]
- 18.Abraham B.P., Kahn S.A. Transition of care in inflammatory bowel disease. Gastroenterol Hepatol (N Y) 2014;10:633–640. [PMC free article] [PubMed] [Google Scholar]
- 19.Goossens E., Stephani I., Hilderson D., et al. Transfer of adolescents with congenital heart disease from pediatric cardiology to adult health care: an analysis of transfer destinations. J Am Coll Cardiol. 2011;57:2368–2374. doi: 10.1016/j.jacc.2010.11.068. [DOI] [PubMed] [Google Scholar]
- 20.Stout K.K., Daniels C.J., Aboulhosn J.A., et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73:1494–1563. doi: 10.1016/j.jacc.2018.08.1028. [DOI] [PubMed] [Google Scholar]
- 21.Moons P., Bratt E.L., De Backer J., et al. Transition to adulthood and transfer to adult care of adolescents with congenital heart disease: a global consensus statement of the ESC Association of Cardiovascular Nursing and Allied Professions (ACNAP), the ESC Working Group on Adult Congenital Heart Disease (WG ACHD), the Association for European Paediatric and Congenital Cardiology (AEPC), the Pan-African Society of Cardiology (PASCAR), the Asia-Pacific Pediatric Cardiac Society (APPCS), the Inter-American Society of Cardiology (IASC), the Cardiac Society of Australia and New Zealand (CSANZ), the International Society for Adult Congenital Heart Disease (ISACHD), the World Heart Federation (WHF), the European Congenital Heart Disease Organisation (ECHDO), and the Global Alliance for Rheumatic and Congenital Hearts (Global ARCH) Eur Heart J. 2021;42:4213–4223. doi: 10.1093/eurheartj/ehab388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beauchesne M.F., Bercier D., Julien-Baker F., et al. Community pharmacy-based medication assessment program for asthma and chronic obstructive pulmonary disease. Can Pharm J (Ott) 2012;145:70–71. doi: 10.3821/145.2.cpj70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mackie A.S., Rempel G.R., Kovacs A.H., et al. Transition intervention for adolescents with congenital heart disease. J Am Coll Cardiol. 2018;71:1768–1777. doi: 10.1016/j.jacc.2018.02.043. [DOI] [PubMed] [Google Scholar]
- 24.Mackie A.S., Fournier A., Swan L., Marelli A.J., Kovacs A.H. Transition and transfer from pediatric to adult congenital heart disease care in Canada: call for strategic implementation. Can J Cardiol. 2019;35:1640–1651. doi: 10.1016/j.cjca.2019.08.014. [DOI] [PubMed] [Google Scholar]