Abstract
Background
Congenital heart disease, the most common congenital anomaly, often presents in neonates. Because of perceived risks, health care providers may consider deferring immunizations in this population. We sought to understand the perceived risk of immunizations in those providing health care to children with particular heart conditions.
Methods
A survey, which included 6 hypothetical scenarios assessing immunization recommendations, was distributed internationally to relevant health care providers, and responses were compared between the different scenarios.
Results
Majority of responses (n = 142) were from paediatric cardiologists (n = 98; 69%) and nurse practitioners (n = 27; 19%) located in the United States (n = 77; 54%) or Canada (n = 53; 37%) working in academic teaching hospitals (n = 133; 93.7%). Most favoured vaccinations (n = 107; 75.4%) and less likely to proceed with the first immunization in infants with structural heart disease compared with channelopathy (risk ratio: 0.80, confidence interval: 0.73-0.87; P < 0.001). Only 40% would proceed with immunization as normal in an infant with manifest Brugada type I electrocardiogram. Special precautions after the immunization included longer duration of observation (19%) and administering prophylactic antipyretic medication (92%).
Conclusions
Respondents were 20% more likely to defer immunizations in the presence of treatable structural heart disease as compared with channelopathy despite the lack of evidence supporting deferring immunizations in children with structural heart disease. Most were cautious in their response to the scenario involving Brugada syndrome, indicating awareness of the risk of haemodynamic instability in the event of a fever. The majority of respondents still strongly recommend immunizations in this population as the benefits outweigh the potential for adverse events.
Résumé
Contexte
La cardiopathie congénitale – l’anomalie congénitale la plus courante – est souvent observée chez les nouveau-nés. En raison des risques perçus, les dispensateurs de soins de santé peuvent parfois envisager de reporter la vaccination chez ces patients. Notre but était de comprendre le risque perçu à l'égard de la vaccination par les dispensateurs de soins de santé traitant des enfants atteints de certaines cardiopathies.
Méthodologie
Un sondage comprenant six scénarios hypothétiques visant à évaluer les recommandations de vaccination a été distribué à des dispensateurs de soins de santé pertinents dans différents pays, et leurs réponses pour les différents scénarios ont été comparées.
Résultats
La majorité des répondants (n = 142) étaient des cardiologues pédiatriques (n = 98; 69 %) ou des infirmières praticiennes (n = 27; 19 %) des États-Unis (n = 77; 54 %) ou du Canada (n = 53; 37 %) travaillant dans des hôpitaux universitaires (n = 133; 93,7 %). La plupart d’entre eux étaient en faveur de la vaccination (n = 107; 75,4 %), bien que moins enclins à administrer un premier vaccin à des nourrissons présentant une cardiopathie structurelle comparativement à une canalopathie (rapport des risques : 0,80, intervalle de confiance : 0,73-0,87; p < 0,001). Or, seulement 40 % d’entre eux vaccineraient de façon normale un nourrisson présentant un syndrome de Brugada de type 1 à l’ECG. Les précautions particulières prises après la vaccination comprenaient une période d’observation plus longue (19 %) et l’administration d’un antipyrétique à des fins prophylactiques (92 %).
Conclusions
À la lumière des réponses obtenues, la probabilité de report de la vaccination était 20 % plus élevée en présence d’une cardiopathie structurelle traitable comparativement à une canalopathie, malgré le manque de données probantes justifiant ce report chez les enfants atteints d’une cardiopathie structurelle. La plupart des répondants ont répondu de façon prudente au scénario du syndrome de Brugada en évoquant un risque d’instabilité hémodynamique en cas de fièvre. La majorité d’entre eux recommandent quand même fortement la vaccination chez ces patients, car les bienfaits escomptés l’emportent sur les risques d’effets indésirables.
Congenital heart disease (CHD) is the most common congenital anomaly, occurring in approximately 1 in 100 live births.1 Most haemodynamically significant CHD is diagnosed before 2 months of age. Changes in pulmonary physiology in the first few weeks of life lead to development of symptoms in several types of CHD, particularly left to right shunts. This is also a critical time in development, with the physiologic nadir of haemoglobin and the peak occurrence of sudden infant death.
The majority of standard infant immunizations globally are scheduled for initial doses at 6 weeks to 2 months of age, as recommended by the World Health Organization.2, 3, 4 Adverse events occur after all vaccines, including risk of a febrile illness. The most commonly reported adverse effects include fussiness (1 in 3 children), redness and swelling at the injection site (1 in 4 children), low-grade fever (1 in 4 children), drowsiness and poor appetite (1 in 10 children), vomiting (1 in 50 children), and fever above 40.5°C (1 in 16,000 children).5,6 Because of this risk at a time when physiology is changing and CHD may become symptomatic, care providers are often asked if the immunizations should be given as normal or deferred until the CHD has been treated or has stabilized. Although there are guidelines for delaying immunization after exposure to blood products, as occurs with open heart surgery, there are no guidelines and very limited data as to risk-benefit in symptomatic CHD.7,8 Comorbidities commonly associated with CHD, such as DiGeorge syndrome, may additionally increase the risk of vaccine-preventable diseases due to immunocompromise.9,10
Paediatric cardiologists and other specialist health care providers are often consulted about the decision to proceed with the first immunization. The purpose of this study was to gain a better understanding of health care providers’ assessment of the risk of immunizations with certain heart conditions.10 Using a survey method with hypothetical scenarios that present commonly in the first few months of life, we examined the health care provider’s decision to recommend proceeding with the first scheduled immunization.
Methods
Participant survey
A voluntary survey outlining 6 hypothetical scenarios was available to complete in English or French (see Supplemental Appendix S1). Survey responses were collected between December 2, 2019, and June 16, 2020.
The survey was distributed in several ways. The link to the survey was distributed by email and posted on Twitter. The Pediatric and Congenital Electrophysiology Society has an international group of members who were asked to circulate the survey to their colleagues. Individual paediatric cardiologists who received the email were asked to forward the survey to their paediatric cardiology colleagues. The survey was also sent to the Canadian Pediatric Cardiology Association members and emailed to the division chief of every paediatric cardiology program in the United States. The survey was distributed to nurse practitioners via the National Association of Pediatric Nurse Practitioners.
The survey included a section on demographics to ensure that the respondents were involved in counselling caregivers and health professionals about whether to proceed with immunizations in patients with CHD. Respondents were only able to provide answers to the hypothetical scenarios if they answered “yes” to counselling patients or their parents about proceeding with vaccinations and working primarily with paediatric cardiology patients. The survey included a scenario in which there was no justification to alter the recommended schedule to serve as a control group (a small ventricular septal defect).
The survey scenarios were structured to examine whether there is deviation from the immunization recommendations for the first immunization and whether the deviation is to defer, cancel, or observe in hospital. The lesions selected, in addition to the control, were designed to represent clear categories in which a fever or reduced oral intake may be a significant haemodynamic challenge for an infant (left ventricular outflow tract [LVOT] obstruction, congestive heart failure [CHF], cardiomyopathy, and channelopathy).
Survey data were collected and managed using Research Electronic Data Capture (REDCap) housed at BC Children’s Hospital Research Institute. REDCap is a secure, web-based software platform designed to support data capture for research studies.11,12 Respondents were asked to respond only once, and no obvious duplicates were apparent from the demographic responses.
Data analysis
Responses were categorized as proceeding with standard immunization or altering the immunization protocol in a dichotomous manner. Percentages were calculated based on eligible respondents for each scenario. When respondents indicated that they would not be consulted for a specific scenario, they were not included in that analysis. To account for multiple responses from the same individual, generalized estimating equations with a Poisson link function were used to estimate risk ratios (RR) and 95% confidence intervals (CI).13 We further analyzed immunization response for specific combinations of relevant situations (eg, situations 1 and 2 vs 3, 6A, 6B). In the primary analysis, individuals were marked as “yes” to immunization if they said yes to all components. Inclusion of this group addressed those who would proceed with routine immunizations without additional precautions. Secondary analysis included both those who would proceed normally and those who would proceed with immunization with special precautions. We carried out 2 further sensitivity analyses. The first included country of response as a covariate in the above models to account for possible systematic differences in response by country; the second restricted analyses only to paediatric cardiologists and nurse practitioners. Exploratory analyses included stratification by years of service and respondent job type. Statistical significance was set at 0.05, and all models were fit using the geepack in R statistical software version 4.0.3.14
Results
Demographics
A total of 239 survey responses were received. Of these, 29 responses were incomplete and excluded from analysis, leaving 210 responses available for analysis. A total of 142 of the respondents (68%) indicated that they worked primarily with paediatric cardiology patients and are consulted about vaccinations, a requirement for proceeding to the component of the survey regarding the immunization scenarios.
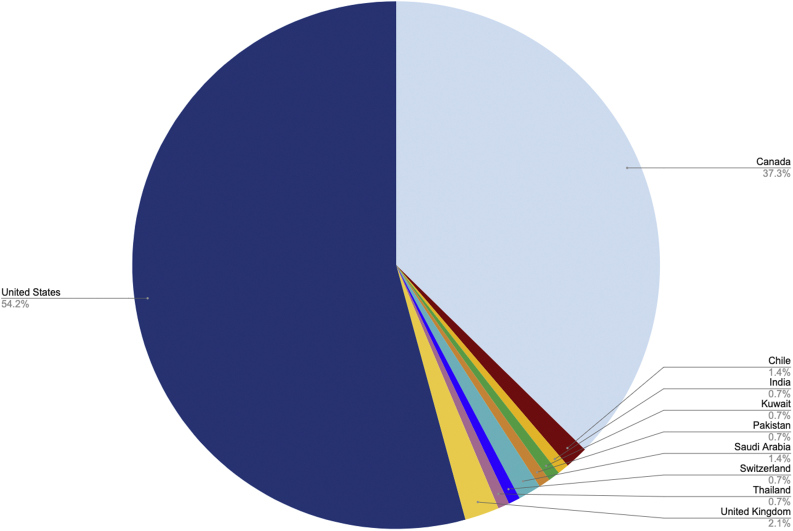
The majority of the survey respondents who completed the survey were located in the United States and Canada (Fig. 1) and comprised primarily paediatric cardiologists (n = 98; 69%) and nurse practitioners (n = 27; 19%), working in academic teaching hospitals (n = 133; 93.7%) (Table 1). Most respondents reported practicing in the United States (n = 77; 54%) and Canada (n = 53; 37%) (Fig. 1) with many of the respondents (43.7%) practicing for >15 years (Table 1). The majority of respondents were strongly in favour of vaccinations (n = 107; 75.4%).
Figure 1.
Country of respondents.
Table 1.
Respondent demographics
| N = 142, n (%) | |
|---|---|
| Primary language | |
| English | 140 (98.6) |
| French | 2 (1.4) |
| Primary practice setting | |
| Academic teaching hospital | 133 (93.7) |
| Nonteaching hospital | 6 (4.2) |
| Private health clinic | 2 (1.4) |
| Other | 1 (0.7) |
| Profession | |
| Paediatric cardiologist | 98 (69) |
| Nurse practitioner | 27 (19) |
| Nurse | 13 (9.2) |
| Paediatrician | 1 (0.7) |
| Other | 3 (2.1) |
| Number of years in practice | |
| 0-5 | 28 (19.7) |
| 6-10 | 30 (21.1) |
| 11-15 | 22 (15.5) |
| >15 | 62 (43.7) |
Scenarios
Immunize as normal
In response to a child in the control scenario, 93% (132 of 142) of respondents indicated that they would immunize as normal with the standard protocol (Table 2). A median of 6% (interquartile range = 4.7-15.7) indicated that they would not be consulted about that particular lesion. Overall, the majority of respondents would immunize as normal in a child with cardiomyopathy, CHF, LVOT, and channelopathies long QT syndrome and Brugada where the electrocardiogram is normal. In the scenario describing an infant with a manifest Brugada type I electrocardiogram, respondents were more cautious in their approach. A slight majority (69 of 142; 48.6%) recommended special precautions, as compared with 32.4% (46 of 142) who would proceed normally with immunization. Eight percent (12 of 142) indicated that they would admit the child to hospital for the immunization.
Table 2.
Summary of hypothetical scenarios and survey responses
| Category | Specific condition | Response | Number of responses | Overall % (out of 142) |
|---|---|---|---|---|
| Control | Control | Do not immunize at this time | 1 | 0.7 |
| Immunize with special precautions | 1 | 0.7 | ||
| Immunize as normal | 132 | 93 | ||
| Not consulted for this particular lesion | 6 | 4.2 | ||
| No response | 2 | 1.4 | ||
| Channelopathy | Brugada, type I ECG | Do not immunize at this time | 1 | 0.7 |
| Immunize with special precautions | 69 | 48.6 | ||
| Immunize as normal | 46 | 32.4 | ||
| Not consulted for this particular lesion | 23 | 16.2 | ||
| No response | 3 | 2.1 | ||
| Channelopathy | Brugada, normal ECG | Do not immunize at this time | 1 | 0.7 |
| Immunize with special precautions | 44 | 31 | ||
| Immunize as normal | 74 | 52.1 | ||
| Not consulted for this particular lesion | 21 | 14.8 | ||
| No response | 2 | 1.4 | ||
| Channelopathy | Long QT syndrome | Do not immunize at this time | 1 | 0.7 |
| Immunize with special precautions | 24 | 16.9 | ||
| Immunize as normal | 93 | 65.5 | ||
| Not consulted for this particular lesion | 23 | 16.2 | ||
| No response | 1 | 0.7 | ||
| Left ventricular outflow tract obstruction | Severe aortic stenosis | Do not immunize at this time | 24 | 16.9 |
| Immunize with special precautions | 41 | 28.9 | ||
| Immunize as normal | 70 | 49.3 | ||
| Not consulted for this particular lesion | 7 | 4.9 | ||
| Congestive heart failure | Large ventricular septal defect | Do not immunize at this time | 11 | 7.7 |
| Immunize with special precautions | 29 | 20.4 | ||
| Immunize as normal | 96 | 67.6 | ||
| Not consulted for this particular lesion | 6 | 4.3 | ||
| Cardiomyopathy | Dilated cardiomyopathy, mild | Do not immunize at this time | 1 | 0.7 |
| Immunize with special precautions | 16 | 11.3 | ||
| Immunize as normal | 115 | 81 | ||
| Not consulted for this particular lesion | 9 | 6.3 | ||
| No response | 1 | 0.7 |
ECG, electrocardiogram.
Compared with the control scenario, recommendations to immunize as normal were 12%-59% lower in other scenarios, depending on the specific condition (Table 3). There was no evidence of a large difference in whether respondents would immunize as normal when we compared treatable structural heart disease vs channelopathy (RR: 1.14, CI: 0.88-1.46; P = 0.16). We conducted sensitivity analyses adjusting for country of response, respondent type, and nonresponders (Supplemental Table S1). Adjusting for country of response, responses from paediatric cardiologists and nurse practitioners only and nonresponders had minimal difference with our primary result.
Table 3.
Risk ratios and 95% confidence intervals of responses to the different types of conditions including those who would proceed with immunization as normal
| Scenario | Respondents who would proceed with immunization as normal plus immunize with special precautions, n/N (%)∗ | Risk ratio vs small ventricular septal defect (95% confidence interval) | P value |
|---|---|---|---|
| Left ventricular outflow tract obstruction | 70/135 (52) | 0.53 (0.45, 0.62) | <0.001 |
| Congestive heart failure | 96/136 (71) | 0.72 (0.65, 0.80) | <0.001 |
| Channelopathy | 93/118 (79) | 0.79 (0.73, 0.87) | <0.001 |
| Cardiomyopathy | 115/132 (87) | 0.89 (0.84, 0.95) | <0.001 |
| Channelopathy | 74/119 (62) | 0.62 (0.54, 0.72) | <0.001 |
| Channelopathy | 46/116 (40) | 0.4 (0.32, 0.50) | <0.001 |
| Treatable structural heart disease | 60/135 (44) | 0.45 (0.37, 0.55) | <0.001 |
| Channelopathy | 44/111 (40) | 0.40 (0.32, 0.50) | <0.001 |
Numerator is those who would immunize normally plus immunize with special precautions, denominator is those who responded to question.
Immunize with additional precautions
We also compared those who would immunize normally including those who would immunize with special precautions against those who would not immunize at this time (Table 4). Respondents were more likely to proceed with immunization with/without special precautions as they would for controls if the child had a channelopathy, but less likely to proceed if the child presented with LVOT, CHF, or a treatable structural heart disease. A higher proportion of respondents would not proceed with the first immunization in infants with structural heart disease as compared with channelopathy (RR: 0.80, CI: 0.73-0.87; P < 0.001). Respondents indicated that they would treat the haemodynamic abnormality before proceeding with the immunization.
Table 4.
Risk ratios and 95% confidence intervals of responses to the different types of conditions including those who would proceed with immunization as normal and those who would proceed with precautions
| Scenario | Respondents who would proceed with immunization as normal plus immunize with special precautions, n/N (%)∗ | Risk ratio vs small ventricular septal defect (95% confidence interval) | P value |
|---|---|---|---|
| Left ventricular outflow tract obstruction | 111/135 (82) | 0.83 (0.77, 0.90) | <0.001 |
| Congestive heart failure | 125/136 (92) | 0.93 (0.88, 0.97) | 0.001 |
| Channelopathy | 117/118 (99) | 0.99 (0.98, 1.00) | 0.04 |
| Cardiomyopathy | 131/132 (99) | 1.00 (0.99, 1.00) | 0.201 |
| Channelopathy | 118/119 (99) | 1.00 (0.99, 1.00) | 0.16 |
| Channelopathy | 115/116 (99) | 0.99 (0.99, 1.00) | 0.11 |
| Treatable structural heart disease | 107/135 (79) | 0.80 (0.73, 0.87) | <0.001 |
| Channelopathy | 110/111 (99) | 1.00 (0.99, 1.00) | 0.06 |
Numerator is those who would immunize normally plus immunize with special precautions, denominator is those who responded to question.
Compared with nonphysicians, physicians did not have a meaningfully higher probability of immunizing (RR: 0.96, CI: 0.85-1.08; P = 0.45). Those working for less than 15 years had a 10% higher rate of positive response to immunization than those working more than 15 years (RR: 1.10, CI: 0.99-1.22; P = 0.075). Of those who chose to proceed with immunization with special precautions, 19% (42 of 224) recommended a longer duration of observation after the immunization and 92% (205 of 224) advised giving prophylactic antipyretic medication. Ten percent (22 of 218) of participants indicated that they have previously had a patient experience an adverse event within 48 hours of an immunization, including death (n = 4), high fever (n = 2), and hospital admission or assessment (n = 18). No further information regarding these cases was included in the survey.
Discussion
In this survey of paediatric cardiologists, nurse practitioners, and other health care providers with a primary clinical focus of paediatric cardiology patients, we presented several clinical scenarios in which an immunization might present a physiologic stressor. The hypothetical case scenarios were designed so that the respondent would need to weigh the risks of the most common adverse events (in particular, fever and poor feeding) against the benefits of immunization. The respondents expressed greatest concern in the presence of structural heart disease. Respondents were 20% more likely to not proceed with immunizations in infants with treatable structural heart disease as compared with channelopathy. Many respondents would treat the haemodynamic abnormality before proceeding with the immunization. Given the severity of the structural heart disease presented, this is intuitively a reasonable approach. However, there are no data to support this recommendation. McAlvin et al.15 reported on 137 infants with single-ventricle physiology who underwent 173 total immunizations over an almost 3-year time period. They did not find an association with adverse events within 48 hours of the diphtheria, tetanus, pertussis immunization. It should be noted that the population studied was already under increased monitoring and surveillance, and there is no mention of the benefits of additional precautions or immunization deferral in this study.15
In the scenario of an infant with Brugada syndrome, the risk of significant haemodynamic instability in the event of fever in this patient population was recognized by respondents, with fewer than 40% proceeding with routine immunization without special precautions. In the preamble to the scenario, there is no mention of antipyretic use or additional monitoring, both of which were recommended by the majority of respondents. The guidelines for the management of Brugada syndrome include immediate treatment of fever with antipyretics; however, the guidelines make no mention of immunizations.16 Most respondents indicated that they would immunize with special precautions (ie, acetaminophen and observation) rather than not immunize at this time. Because many respondents would deviate from proceeding with immunization as normal, it is important to actively pursue discussion about immunization in this patient population in clinic.
The paediatric cardiologist is often consulted regarding the decision to proceed with the first immunization. Given the absence of data and the vast number of immunizations that occur routinely without serious adverse events, clinicians should be encouraging immunizations. There is no evidence that additional observation or antipyretic medication is required or has a benefit in children with CHD undergoing immunization. Children given acetaminophen prophylactically have been found to be less likely to develop fever after immunization.17 Most data suggest that if given prophylactically, acetaminophen is unlikely to reduce the immunogenicity of a vaccine; however, these concerns are still debated by some.18,19 The benefits of vaccinations in reducing infectious childhood diseases far outweigh the potential for adverse events.
Limitations
Our study has several limitations. The majority of our respondents were in favour of immunization, which may have represented a bias in survey respondents—although it may be expected that most child-focused health care providers would favour immunization. We were unable to determine whether the lack of a response from some respondents was a reflection of their unwillingness to immunize normally. In addition, the majority of respondents were from an academic teaching hospital and may not be representative of the approach of those practicing in the community/private setting. Having an important clinical event temporally related to an immunization may have made individuals more likely to respond, as our proportion of those with a clinical experience with an adverse event was higher than expected. In addition, the survey presents only hypothetical scenarios, which can only approximate true clinical situations. Factors such as family beliefs, monitoring concerns, and patient-specific factors are not accounted for in this survey. Nonetheless, given the lack of data and the importance of immunizations as a preventative health measure, these data are an important step in beginning to address a substantial knowledge gap.
Conclusions
Respondents were more likely to defer immunization in those with a treatable structural heart condition as compared with channelopathy. Most respondents were aware of the guidelines and caution relating to fevers in Brugada syndrome. There was an overall high variability of responses in both structural heart conditions and channelopathies, indicating a lack of consensus on optimal vaccination practices in these patients. The vast majority of respondents still strongly recommend immunizations in this population, with minor special precautions. The paucity of data and lack of signal about significant adverse events support widespread immunization of this population. With the exception of some rare heart conditions, the perceived need for additional precautions is relatively simple to address without significant implications on health care resources.
Acknowledgements
We would like to thank the survey respondents for their contribution to this study. MS is supported via salary awards from the BC Children’s Hospital Foundation, the Canadian Child Health Clinician Scientist Program, and the Michael Smith Foundation for Health Research.
Ethics Statement
Ethics approval was obtained from the University of British Columbia Children's and Women's Health Centre Research Ethics Board (H19-02702).
Funding Sources
No funding was received for this study.
Disclosures
MS has been an investigator on projects funded by GlaxoSmithKline, Merck, Moderna, Pfizer, Sanofi-Pasteur, Seqirus, Symvivo, and VBI Vaccines. All funds have been paid to his institute, and he has not received any personal payments.
Footnotes
To access the supplementary material accompanying this article, visit CJC Pediatric and Congenital Heart Disease at https://www.cjcpc.ca// and at https://doi.org/10.1016/j.cjcpc.2021.12.003.
Supplementary Material
References
- 1.Hoffman J.I., Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–1900. doi: 10.1016/s0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 2.Public Health Agency of Canada Canada's provincial and territorial routine (and catch-up) vaccination routine schedule programs for infants and children. www.canada.ca/en/public-health/services/provincial-territorial-immunization-information/provincial-territorial-routine-vaccination-programs-infants-children.html Available at:
- 3.Centers for Disease Control and Prevention Recommended child and adolescent immunization schedule for ages 18 years or younger, United States, 2019. www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html Available at:
- 4.World Health Organization WHO recommendations for routine immunization—summary tables. www.who.int/immunization/policy/immunization_tables/en/ Available at:
- 5.Centers for Disease Control and Prevention Possible side-effects from vaccines. https://www.cdc.gov/vaccines/vac-gen/side-effects.htm Available at:
- 6.Drutz JE. Diphtheria, tetanus, and pertussis immunization in children 6 weeks through 6 years of age. In: Torchia MM, Duryea TK, Edwards MS, eds. UpToDate, Waltham, MA. Available at: https://www.uptodate.com/contents/diphtheria-tetanus-and-pertussis-immunization-in-children-7-through-18-years-of-age. Accessed August 2, 2019.
- 7.Government of Canada Blood products, human immunoglobulin and timing of immunization: Canadian Immunization Guide. www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-1-key-immunization-information/page-11-blood-products-human-immune-globulin-timing-immunization.html#p1c10t1 Available at:
- 8.Kroger A.T., Sumaya C.V., Pickering L.K., Atkinson W.L. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011;60:1–60. [PubMed] [Google Scholar]
- 9.Woodward C.S. Keeping children with congenital heart disease healthy. J Pediatr Health Care. 2011;25:373–378. doi: 10.1016/j.pedhc.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Lantin-Hermoso M.R., Berger S., Bhatt A.B., et al. The care of children with congenital heart disease in their primary medical home. Pediatrics. 2017;140 doi: 10.1542/peds.2017-2607. [DOI] [PubMed] [Google Scholar]
- 11.Harris P.A., Taylor R., Thielke R., et al. A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris P.A., Taylor R., Minor B.L., et al. The REDCap consortium: building an international community of software partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zou G.Y., Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22:661–670. doi: 10.1177/0962280211427759. [DOI] [PubMed] [Google Scholar]
- 14.Højsgaard S., Halekoh U., Yan J. The R Package geepack for generalized estimating equations. J Stat Softw. 2005;15:1–11. [Google Scholar]
- 15.McAlvin B., Clabby M., Kirshbom P., et al. Routine immunizations and adverse events in infants with single-ventricle physiology. Ann Thorac Surg. 2007;84:1316–1319. doi: 10.1016/j.athoracsur.2007.04.114. [DOI] [PubMed] [Google Scholar]
- 16.Priori S., Wilde A., Horie M., et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. Heart Rhythm. 2013;10:1932–1963. doi: 10.1016/j.hrthm.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 17.Jackson L.A., Peterson D., Dunn J., et al. A randomized placebo-controlled trial of acetaminophen for prevention of post-vaccination fever in infants. PLoS One. 2011;6 doi: 10.1371/journal.pone.0020102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saleh E., Moody M.A., Walter E.B. Effect of antipyretic analgesics on immune responses to vaccination. Hum Vaccin Immunother. 2016;12:2391–2402. doi: 10.1080/21645515.2016.1183077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walter E.B., Hornik C.P., Grohskopf L., et al. The effect of antipyretics on immune response and fever following receipt of inactivated influenza vaccine in young children. Vaccine. 2017;35:6664–6671. doi: 10.1016/j.vaccine.2017.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.