Abstract
BACKGROUND
Alpha-1 antitrypsin deficiency is a rare genetic disease and a leading cause of inherited alterations in plasma protein metabolism (APPM).
AIM
To understand the prevalence, burden and progression of liver disease in patients with APPM including alpha-1 antitrypsin deficiency.
METHODS
We conducted a retrospective analysis of anonymized patient-level claims data from a German health insurance provider (AOK PLUS). The APPM cohort comprised patients with APPM (identified using the German Modification of the International Classification of Diseases-10th Revision [ICD-10-GM] code E88.0 between 01/01/2010-30/09/2020) and incident liver disease (ICD-10-GM codes K74, K70.2-3 and K71.7 between 01/01/2012-30/09/2020). The control cohort comprised patients without APPM but with incident liver disease. Outcomes were incidence/prevalence of liver disease in patients with APPM, demographics/baseline characteristics, diagnostic procedures, progression-free survival (PFS), disease progression and mortality.
RESULTS
Overall, 2680 and 26299 patients were included in the APPM (fibrosis, 96; cirrhosis, 2584) and control (fibrosis, 1444; cirrhosis, 24855) cohorts, respectively. Per 100000 individuals, annual incidence and prevalence of APPM and liver disease was 10-15 and 36-51, respectively. In the APPM cohort, median survival was 4.7 years [95% confidence interval (CI): 3.5-7.0] and 2.5 years (95%CI: 2.3-2.8) in patients with fibrosis and cirrhosis, respectively. A higher proportion of patients in the APPM cohort experienced disease progression (92.0%) compared with the control cohort (67.2%). Median PFS was shorter in the APPM cohort (0.9 years, 95%CI: 0.7-1.1) compared with the control cohort (3.7 years, 95%CI: 3.6-3.8; P < 0.001). Patients with cirrhosis in the control cohort had longer event-free survival for ascites, hepatic encephalopathy, hepatic failure and esophageal/gastric varices than patients with cirrhosis in the APPM cohort (P < 0.001). Patients with fibrosis in the control cohort had longer event-free survival for ascites, cirrhosis, hepatic failure and esophageal/gastric varices than patients with fibrosis in the APPM cohort (P < 0.001). In the APPM cohort, the most common diagnostic procedures within 12 mo after the first diagnosis of liver disease were imaging procedures (66.3%) and laboratory tests (51.0%).
CONCLUSION
Among patients with liver disease, those with APPM experience substantial burden and earlier liver disease progression than patients without APPM.
Keywords: Alpha-1 antitrypsin deficiency, Epidemiology, Germany, Liver diseases, Retrospective study
Core Tip: This was a retrospective analysis of anonymized, patient-level, insurance claims data from a German health insurance provider (AOK PLUS), which demonstrated that a diagnosis of alterations in plasma protein metabolism (APPM) (E88.0) in patients with liver disease was associated with a substantial burden and higher rate of liver disease progression compared with patients with liver disease but without APPM. To enable accurate diagnosis and inform disease management, it is important to have specific diagnostic codes that differentiate between genetic liver disease and liver manifestations from other causes.
INTRODUCTION
Alterations in plasma protein metabolism (APPM) can either be inherited or acquired[1]. As hepatocytes are responsible for the majority of protein production (approximately 10-20 g/d)[2], liver disease is frequently observed among patients with APPM[1].
Alpha-1 antitrypsin (AAT) deficiency (AATD) is the most common form of inherited APPM and is caused by mutations in serpin family A member 1 (SERPINA1), which encodes AAT, a serum protein produced primarily by hepatocytes that protects the lungs from protease-mediated degradation[3]. A homozygous mutation (Glu342Lys) in SERPINA1, named protease inhibitor (Pi) ZZ, is estimated to affect approximately 1 in 2000-5000 newborn infants in Europe and North America[4]. Mutations in SERPINA1 cause a reduction in serum AAT levels and promote the development of respiratory diseases, such as emphysema or chronic obstructive pulmonary disease[5]. In addition, AATD can result in liver diseases such as liver cirrhosis or hepatocellular carcinoma (HCC) due to the accumulation of hepatic AAT, which can trigger proteotoxic stress and lead to hepatocyte death and liver injury[6,7]. Approximately 20%-36% of patients with a PiZZ genotype develop significant fibrosis and approximately 10%-15% develop advanced fibrosis[8]. The only available curative treatment for end-stage liver disease in patients with AATD is liver transplantation[9]. Liver transplants in Germany have been allocated based on urgency according to the model for end-stage liver disease scoring system[10].
Given the lack of information on the natural history and epidemiology of AATD, we conducted a retrospective analysis of insurance claims data from Germany to better understand overall prevalence, burden and progression of liver disease in patients with APPM, including AATD. To improve our understanding of the natural history of APPM and liver disease, we compared patients with APPM and liver disease with a control cohort of patients with liver disease but without APPM.
MATERIALS AND METHODS
Data source and sample selection
This retrospective study used anonymized, patient-level, insurance claims data from 01 January 2010 to 30 September 2020, provided by the German regional health insurance provider, AOK PLUS. This data set covers approximately 3.3 million individuals from the federal states of Saxony and Thuringia, accounting for approximately 4.5% of the German statutory health insured (SHI) population in 2020. The age and comorbidity characteristics of patients insured by AOK PLUS are similar to those in the general German population who are insured by sickness funds[11-14].
The cohort of patients with APPM and incident liver disease was identified using the German Modification of the International Classification of Diseases-10th Revision (ICD-10-GM) code E88.0 for disorders of plasma protein metabolism (which includes AATD and other metabolic disorders such as plasminogen deficiency and bisalbuminaemia), and codes K74, K70.2-3 and K71.7 for liver disease.
Patients were included in the APPM cohort if they had APPM (diagnosed between 01 January 2010 and the end of the study) and incident liver disease (diagnosed between 01 January 2012 and the end of the study; Supplementary Figure 1). Patients were excluded if their liver disease was diagnosed in 2010 or 2011, to guarantee a liver disease-free period of 2 years. Continuous insurance coverage (no interruption of insurance for > 30 d) in 2010 and/or 2011 was required. Patients were observed from the date of the first diagnosis of liver disease (index date) until death, loss to follow-up due to end of insurance or end of the study. In patients with incident fibrosis who developed cirrhosis after 01 January 2012, the index date was defined as the date of the first diagnosis of cirrhosis for analyses of the subgroup of patients with cirrhosis. Patients were included in the control cohort if they did not have a diagnosis of APPM, but had incident liver disease. All patients with incident liver disease in both cohorts were further divided into two sub-cohorts: (1) Those with fibrosis at index date (ICD-10-GM codes: K74.0-2 and K70.2); and (2) those with cirrhosis at index date or those with fibrosis who developed cirrhosis during the study period (ICD-10-GM codes: K74.3-7, K70.3 and K71.7).
Outcomes
The study evaluated point prevalence and cumulative incidence of patients with APPM and liver disease, stratified by sex. In addition, demographics and baseline disease characteristics, including the Charlson Comorbidity Index, were measured at index date, with comorbidities identified during the previous 12 mo. Comorbidities were identified based on three-digit ICD-10-GM codes and evidence of confirmatory diagnosis/diagnoses (at least one inpatient or at least two outpatient diagnoses). Diagnostic procedures (liver biopsy, imaging, laboratory tests, AAT phenotyping and liver function tests) in the 12 mo after the index date were identified based on German procedure codes (Operationen-und Prozedurenschlüssel and einheitlicher Bewertungsmaßstab). A composite endpoint of progression-free survival (PFS) was defined as the time from index date until the first date with selected liver disease-related clinical events (acute peritonitis, ascites, cirrhosis, only among patients with fibrosis), esophageal/gastric varices, HCC, hepatic encephalopathy, hepatic failure, liver transplantation or all-cause death (used to assess mortality). Disease progression events were also analyzed separately, and comprised the following (one inpatient or one confirmed outpatient diagnosis): Ascites, esophageal/gastric varices, acute peritonitis, hepatic encephalopathies, gastrointestinal bleeding (e.g., melaena or hematemesis), hepatic failure, malignant neoplasm of the liver and intrahepatic bile ducts and HCC. Procedure-related events were analyzed, which comprised liver incision, liver resection, other operations on the liver, failure or rejection of transplant, and infection due to prosthesis, implant or graft.
Statistical analysis
To calculate the point prevalence of liver disease in patients with APPM, the denominator was the number of individuals insured by AOK PLUS on 01 January of the respective calendar year (2011-2020) and during the preceding 12 mo. The numerator was the number of patients alive on the 1st January of each year, with evidence of confirmatory diagnosis/diagnoses of APPM (made in two different quarters within the same year) and a diagnosis of liver disease during the previous year, and with continuous insurance coverage during that year.
The cumulative incidence of liver disease in patients with APPM was estimated for 2012-2019 by dividing the number of new cases in a calendar year by the total number of insured patients at risk of liver disease (i.e., those with no current evidence of liver disease) at the beginning of the same year. The numerator was the number of patients with APPM diagnosed at any point and with liver disease diagnosed during the year of the index date, but without any liver disease diagnosis within the previous 2 years and with continuous insurance coverage during this period. The denominator was the number of patients alive at the beginning of the respective calendar year for whom no liver disease diagnosis was documented in the 24 mo before index date, and with continuous insurance over this period.
Point prevalence and cumulative incidence were adjusted for age and sex differences compared with the German SHI population.
Patient demographics and baseline characteristics were analyzed using summary statistics (mean, standard deviation, median and interquartile range) for continuous variables and frequency statistics for categorical variables.
Time to disease progression was estimated using the Kaplan-Meier method. Patients were censored if they were lost to follow-up or had reached the end of the study. In addition to the number of patients with a progression event, the following Kaplan-Meier estimates were reported: median follow-up time in patients without an event, the 25th, 50th and 75th percentiles of time without an event, and event rates at years 1, 3 and 5 post-baseline. All time to event analyses were compared via a log-rank test.
Time from index date to all-cause death was estimated for patients with APPM and incident fibrosis or cirrhosis, and separately for patients with APPM and cirrhosis with and without a previous documented diagnosis of fibrosis.
RESULTS
Overview of analyzed patients
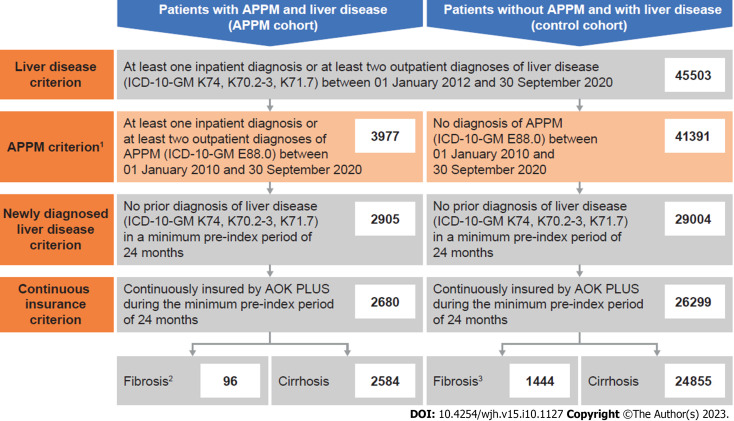
In total, 45503 patients had confirmatory diagnosis(es) of liver disease between 01 January 2012 and the end of the study (Figure 1). Of these, 2680 fulfilled the criteria to be included in the APPM cohort. In total, 96 of these patients had fibrosis and 2584 had cirrhosis at their index date (between 01 January 2012 and the end of the study).
Figure 1.
Selection of patient cohorts. 1In total, 135 patients had only one outpatient alterations in plasma protein metabolism (APPM) diagnosis and therefore did not meet these criteria; 2In total, 42 patients with fibrosis in the APPM cohort progressed to cirrhosis during follow-up; and 3In total, 280 patients with fibrosis in the control cohort progressed to cirrhosis during follow-up. ICD-10-GM: German Modification of the International Classification of Diseases-10th Revision.
In total, 26299 patients were included in the corresponding control cohort with no diagnosis of APPM. Of these, 1444 had fibrosis and 24855 had cirrhosis at their index date (Figure 1).
Epidemiology
Between 2012 and 2019, the annual cumulative incidence of liver disease per 100000 individuals with APPM was 10-15, and was higher in males (15-22) than females (5-9; Supplementary Figure 2). When adjusted for age and sex differences vs the SHI population, the cumulative incidence was 8-13 per 100000 individuals. Between 2011 and 2020, the point prevalence of liver disease per 100000 individuals with APPM was 36-51 and was again higher in males (52-74) than females (22-32; Supplementary Figure 3). When adjusted for age and sex differences compared with the SHI population, the point prevalence was 33-47 per 100000 individuals.
Demographics and baseline characteristics
Demographics and baseline characteristics were similar between cohorts (Table 1). In the APPM and control cohorts, respectively, 840 patients (31.3%) and 8595 patients (32.7%) were female (P = 0.159 between cohorts). Patients in the APPM cohort were significantly younger than in the control cohort, with a median age (interquartile range) of 63 years (54-73) and 65 years (56-76; P < 0.001), respectively. The most common liver-related comorbidities in the APPM and control cohorts, respectively, were “other liver disease” [679 (25.3%) and 6298 (23.9%)], non-alcoholic steatohepatitis [17 (0.6%) and 150 (0.6%)] and chronic hepatitis [12 (0.5%) and 163 (0.6%)]. The proportion of patients with respiratory system-related comorbidities was similar between the APPM [827 (30.9%)] and control [8333 (31.7%)] cohorts.
Table 1.
Demographics and baseline characteristics, n (%)
|
Patients with APPM and liver disease: APPM cohort, n = 2680
|
Patients without APPM and with liver disease: Control cohort, n = 26299 | |||
|
All patients, n = 2680
|
Patients with fibrosis, n = 96
|
Patients with cirrhosis, n = 26261
|
||
| Total observed patient-years | 6118 | 283 | 5944 | 70261 |
| Median follow-up, yr (IQR) | 1.5 (0.4-3.7) | 2.3 (0.8-4.7) | 1.5 (0.4-3.7) | 2.0 (0.5-4.4) |
| Female sex2 | 840 (31.3) | 41 (42.7) | 815 (31.0) | 8595 (32.7) |
| Median age, yr (IQR)3 | 63.0 (54.0-73.0) | 64.5 (53.0-76.5) | 63.0 (54.0-73.0) | 65.0 (56.0-76.0) |
| 0-14 yr | 14 (0.5) | 6 (6.3) | 10 (0.4) | 49 (0.2) |
| 15-29 yr | 10 (0.4) | 0 | 10 (0.4) | 156 (0.6) |
| 30-44 yr | 183 (6.8) | 10 (10.4) | 177 (6.7) | 1420 (5.4) |
| 45-59 yr | 818 (30.5) | 21 (21.9) | 814 (31.0) | 7516 (28.6) |
| 60-74 yr | 1046 (39.0) | 31 (32.3) | 1029 (39.2) | 9564 (36.4) |
| 75-89 yr | 577 (21.5) | 25 (26.0) | 557 (21.2) | 7090 (27.0) |
| ≥ 90 yr | 32 (1.2) | 3 (3.1) | 29 (1.1) | 504 (1.9) |
| With care needs4 | 547 (20.4) | 33 (34.3) | 528 (20.1) | 4934 (18.8) |
| Median CCI5 (IQR) | 3.0 (1.0-5.0) | 4.0 (1.5-6.0) | 3.0 (1.0-5.0) | 3.0 (1.0-5.0) |
| Most common liver-related comorbidities | ||||
| “Other” liver disease6 | 679 (25.3) | 26 (27.1) | 669 (25.5) | 6298 (23.9) |
| Non-alcoholic steatohepatitis | 17 (0.6) | 1 (1.0) | 16 (0.6) | 150 (0.6) |
| Chronic hepatitis | 12 (0.5) | 0 | 12 (0.5) | 163 (0.6) |
| Respiratory system-related comorbidities | 827 (30.9) | 41 (42.7) | 806 (30.7) | 8333 (31.7) |
| Most common comorbidities | ||||
| Hypertension | 1751 (65.3) | 64 (66.7) | 1710 (65.1) | 17278 (65.7) |
| Type 2 diabetes mellitus | 1103 (41.2) | 40 (41.7) | 1082 (41.2) | 10766 (40.9) |
| Dyslipidaemia | 832 (31.0) | 35 (36.5) | 813 (31.0) | 8932 (34.0) |
| Alcohol-related disorders7 | 650 (24.3) | 17 (17.7) | 649 (24.7) | 6127 (23.3) |
| Heart failure | 605 (22.6) | 21 (21.9) | 591 (22.5) | 6071 (23.1) |
Data are n (%) unless otherwise indicated.
In total, 42 patients with fibrosis progressed to cirrhosis during follow-up and are included in both fibrosis and cirrhosis subgroups.
Patients in the alterations in plasma protein metabolism (AAPM) cohort were significantly younger than patients in the control cohort (Wilcoxon rank-sum test: P < 0.001).
There was no statistically significant difference in the proportion of females between cohorts (Wilcoxon rank-sum test: P = 0.159).
Dummy variable for patients who were classified in any of the five care levels which determine the benefits from long-term care insurance in Germany.
Assessed based on diagnoses observed in the 12 mo before the index date.
Captured using the K76 code in the German Modification of the International Classification of Diseases-10th Revision, and includes central hemorrhagic necrosis of the liver, chronic congestive liver, fatty liver (not otherwise classified), hepatorenal syndrome, liver infarction, peliosis hepatis, portal hypertension, veno-occlusive liver disease and other/unspecified liver disease.
Patients with alcohol-related disorders diagnosed before [1172 (43.7%)] and after [1042 (38.9%)] diagnosis of APPM were detected in the cohort with APPM and liver disease.
CCI: Charlson comorbidity index; IQR: Interquartile range.
Minor differences in demographics and baseline characteristics were observed when the APPM cohort was stratified by the presence of fibrosis or cirrhosis. There was a higher proportion of females with fibrosis [41 (42.7%)] compared with cirrhosis [815 (31.0%)] and alcohol-related disorders were more common in patients with cirrhosis [649 (24.7%)] compared with fibrosis [17 (17.7%)].
Diagnostic procedures
The most common diagnostic procedures within 12 mo after the index date in the APPM cohort were imaging procedures [1778 (66.3%)] and laboratory tests [1366 (51.0%); Table 2]. Only 55 patients (2.1%) underwent AAT phenotyping.
Table 2.
Diagnostic procedures within 12 mo after the index date, n (%)
|
Diagnostic procedure
|
Patients with APPM and liver disease: APPM cohort, n = 2680
|
| Imaging procedure1 | 1778 (66.3) |
| Laboratory test2 | 1366 (51.0) |
| Liver biopsy | 207 (7.7) |
| AAT phenotyping | 55 (2.1) |
| Liver function test3 | 13 (0.5) |
Data are n (%).
Included sonographies, computed tomography scans, magnetic resonance imaging procedures, angiographies of the abdomen and magnetic resonance elastographies.
Included albumin and bilirubin measurements.
Liver function test with intravenous application of a 13C-labeled substrate.
AAT: Alpha-1 antitrypsin; APPM: Alterations in plasma protein metabolism.
Disease progression and mortality
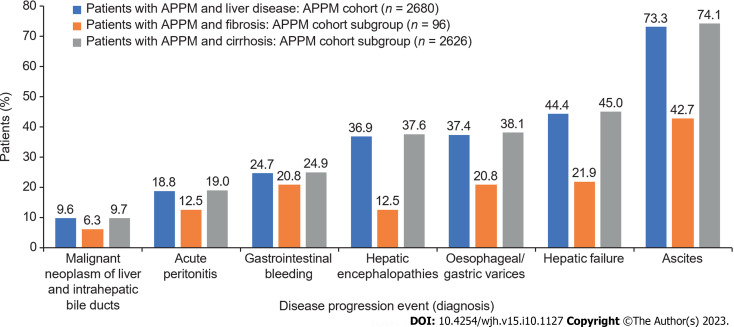
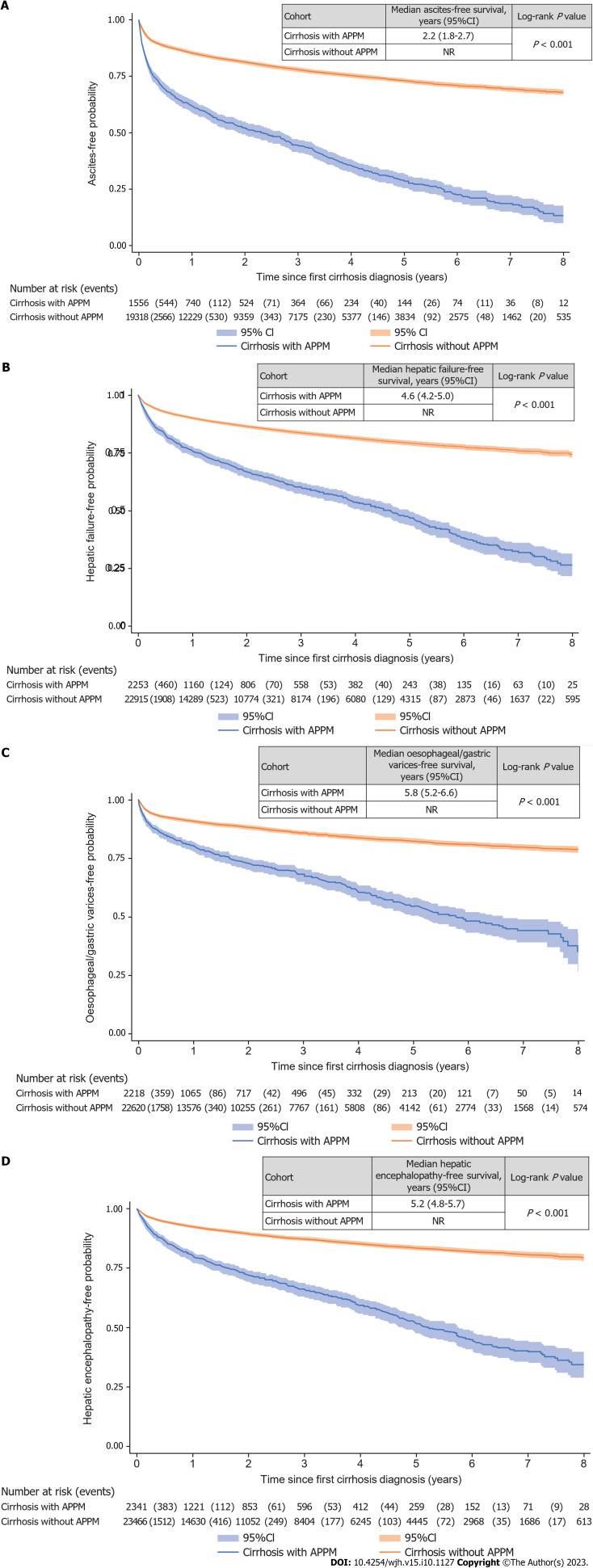
A higher proportion of patients in the APPM cohort experienced disease progression [2465 (92.0%)] compared with the control cohort [17682 (67.2%)]. Median PFS (composite endpoint) was significantly shorter in the APPM cohort [0.9 years (95%CI: 0.7-1.1)] compared with the control cohort [3.7 years (95%CI: 3.6-3.8); P < 0.001; Supplementary Figure 4]. The most common disease progression events were ascites, hepatic failure, esophageal/gastric varices, and hepatic encephalopathies (Figure 2). Patients with cirrhosis but without APPM had significantly longer event-free survival for ascites, hepatic failure, esophageal/gastric varices, and hepatic encephalopathy compared with those with APPM and cirrhosis (all P < 0.001; Figure 3). Similarly, patients with fibrosis but without APPM had significantly longer event-free survival for ascites, cirrhosis, hepatic failure and esophageal/gastric varices compared with those with APPM and fibrosis (all P < 0.001; Supplementary Figure 5). In the subgroup of 96 patients in the APPM cohort with fibrosis, median time from fibrosis to cirrhosis was 2.9 years (95%CI: 1.2-not reached; Supplementary Figure 5B). In the control cohort, median time from fibrosis to cirrhosis was not reached.
Figure 2.
Disease progression events. Disease progression events that occurred after the index date until the end of the study. APPM: Alterations in plasma protein metabolism.
Figure 3.
Event-free survival for disease progression events in patients with cirrhosis with and without alterations in plasma protein metabolism. A: Ascites; B: Hepatic failure; C: Esophageal and gastric varices; D: Hepatic encephalopathy. APPM: Alterations in plasma protein metabolism; CI: Confidence interval; NR: Not reached.
The most common procedures and procedure-related events indicating disease progression were liver resection, liver transplantation, failure and rejection of liver transplant and other operations on the liver (Supplementary Figure 6). A significantly higher proportion of patients with APPM and fibrosis had a liver resection [15 (15.6%) vs 93 (6.4%); P = 0.025] and a liver transplantation [6 (6.3%) vs 3 (0.2%); P < 0.001] compared with patients without APPM but with fibrosis (Table 3). Similarly, a significantly higher proportion of patients with APPM and cirrhosis had a liver resection [87 (3.3%) vs 488 (1.9%); P < 0.001] and a liver transplantation [78 (3.0%) vs 31 (0.1%); P < 0.001] indicating greater disease progression compared with patients without APPM but with cirrhosis (Table 3; Supplementary Figure 6).
Table 3.
Procedures indicating disease progression stratified by fibrosis or cirrhosis
|
Parameter
|
Patients with fibrosis
|
Patients with cirrhosis
|
||||||
|
Liver resection
|
Liver transplantation
|
Liver resection
|
Liver transplantation
|
|||||
|
Patients with APPM, n = 96
|
Patients without APPM, n = 1445
|
Patients with APPM, n = 96
|
Patients without APPM, n = 1445
|
Patients with APPM, n = 2626
|
Patients without APPM, n = 25134
|
Patients with APPM, n = 2626
|
Patients without APPM, n = 25134
|
|
| Patients with event during follow-up | 15 (15.6) | 93 (6.4) | 6 (6.3) | 3 (0.2) | 87 (3.3) | 488 (1.9) | 78 (3.0) | 31 (0.1) |
| Patients included in the KM analysis1 | 85 (88.5) | 1373 (95.0) | 94 (97.9) | 1442 (99.8) | 2606 (99.2) | 24849 (98.9) | 2621 (99.8) | 25034 (99.6) |
| Median follow-up in patients without an event, yr (IQR)2 | 2.3 (0.7-5.0) | 3.0 (1.2-5.2) | 2.3 (0.7-4.7) | 2.8 (1.2-5.1) | 1.5 (0.4-3.7) | 1.9 (0.5-4.4) | 1.5 (0.4-3.7) | 1.9 (0.5-4.4) |
| Failure rate | ||||||||
| After 1 yr | 3 (4.2) | 15 (1.2) | 1 (1.2) | 1 (0.1) | 40 (2.0) | 198 (1.0) | 26 (1.4) | 8 (< 0.1) |
| After 3 yr | 3 (4.2) | 18 (1.5) | 3 (4.8) | 1 (0.1) | 56 (3.4) | 258 (1.5) | 53 (3.6) | 23 (0.2) |
| After 5 yr | 3 (4.2) | 20 (1.9) | 4 (7.3) | 1 (0.1) | 64 (4.7) | 289 (1.9) | 66 (5.6) | 25 (0.2) |
| P value (log-rank test) | 0.025 | < 0.001 | < 0.001 | < 0.001 | ||||
Data are n (%) unless otherwise indicated.
Patients with the event on the index date were excluded from the Kaplan-Meier (KM) analysis. As there were no patients with liver incision in the alterations in plasma protein metabolism cohort, and only one patient in the control cohort, this outcome is not reported.
There were no patients with fibrosis who had an infection/inflammatory reaction due to prothesis/implant/graft. For one patient in the control cohort, the index date and end date were the same; this patient was automatically excluded from the KM analysis. Median follow-up in patients without the event was estimated via the reverse KM method.
IQR: Interquartile range; APPM: Alterations in plasma protein metabolism.
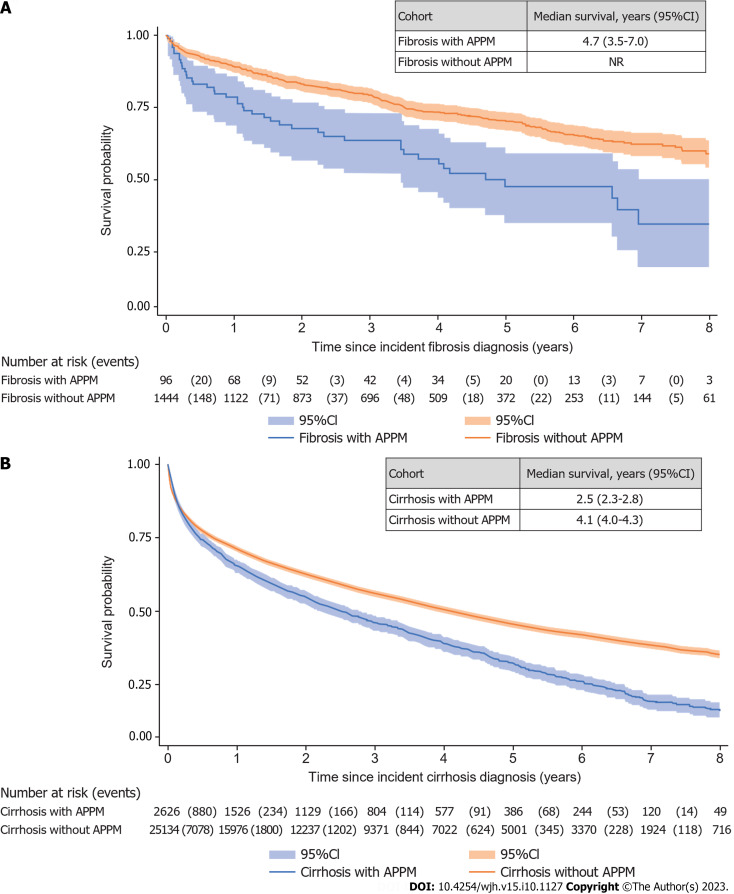
Median survival was shorter in the APPM cohort [2.6 years (95%CI: 2.3-2.8)] than in the control cohort [4.3 years (95%CI: 4.2-4.5)]. Median survival was 4.7 years (95%CI: 3.5-7.0) in patients with APPM and fibrosis and 2.5 years (95%CI: 2.3-2.8) in patients with APPM and cirrhosis (Figure 4). In the 42 patients in the APPM cohort with fibrosis who developed cirrhosis during the follow-up period, median survival was 4.1 years (95%CI: 2.2-7.1). In the 2584 patients in the APPM cohort with cirrhosis and without previous fibrosis, the median survival was 2.5 years (95%CI: 2.2-2.7).
Figure 4.
Survival in patients with fibrosis and cirrhosis. A: Fibrosis; B: Cirrhosis. APPM: Alterations in plasma protein metabolism; CI: Confidence interval; NR: Not reached.
DISCUSSION
This retrospective insurance claims-based study demonstrated that, per 100000 individuals, the annual incidence (2012-2019) and point prevalence (2011-2020) of APPM was 10-15 and 36-51, respectively, with higher rates in males than in females. Patients in the APPM cohort experienced shorter PFS, higher mortality and a higher rate of liver decompensation events compared with patients in the control cohort. In addition, patients with fibrosis in the APPM cohort had significantly shorter cirrhosis-free survival compared with patients with fibrosis in the control cohort (P < 0.001). This may have been because APPM is indicative of a more advanced stage of fibrosis that is more likely to decompensate, or alternatively may reflect how the E88.0 code is used in clinical practice. Liver cirrhosis is often associated with decreased plasma levels of hepatocyte-derived proteins[15]. Some of these proteins, such as albumin and transferrin, are well-established indicators of poor prognosis[1]. Previous studies have demonstrated that patients with cirrhosis and a heterozygous Pi mutation, PiMZ, in SERPINA1 decompensate faster than patients with cirrhosis but without AATD[16,17]. However, only 2.1% of patients in the APPM cohort underwent AAT phenotyping in our study, and therefore we were unable to further evaluate the association between decompensation and AATD genotype. The median age of patients in the APPM cohort was 2 years younger than in the control cohort, yet the APPM cohort had a higher risk of liver disease-related clinical events. This supports that patients with APPM are at a higher risk of liver disease-related clinical events than patients without APPM irrespective of age.
As AATD is also associated with the development of respiratory system comorbidities such as chronic obstructive pulmonary disease[18], it was anticipated that the APPM cohort would have a higher incidence of such comorbidities compared with the control cohort. However, we observed a similar incidence in the APPM and control cohorts (30.9% and 31.7%), which might indicate that the APPM cohort included a substantial number of patients without AATD. The E88.0 code we used to identify patients with APPM cannot be equated with AATD as the code includes a broad range of acquired and inherited APPM disorders, such as plasminogen deficiency. The European Commission Expert Group on Rare Diseases currently recommends the Orphanet nomenclature of rare diseases (ORPHA) codes to identify rare disorders[19]. The adoption of ORPHA codes is expected to facilitate the transition to ICD-11 codes, which include an expanded set of rare disorder codes compared with ICD-10[19]. In addition, developments of the ICD coding system, such as the addition of the E88.0A code for AATD, could improve the identification of patients with AATD in future administrative insurance claims analyses. In a recent registry-based cohort study of the prevalence, incidence and mortality associated with AATD in Denmark using the E88.0A code, a sensitivity analysis demonstrated a predominance of AATD in the E88.0 category for APPM and a near complete shift to the more specific E88.0A code for AATD between 2000 and 2018[20]. The adoption of diagnosis codes specific to patients with AATD may facilitate earlier diagnosis and improved patient management, which may, in turn, contribute to slowing disease progression and decreasing the burden of disease in these patients with a rare, chronic disease.
The limitations of this study are typical of those seen in other insurance claims-based analyses. As noted previously, we were unable to determine the proportion of patients included in the study who had AATD due to the limitations of the ICD-10-GM coding system. In addition, as AATD is a highly underdiagnosed disease[21], we cannot exclude the possibility that some cases may have been included in the control cohort. The general lack of laboratory test results, direct clinical measures and biomarkers in the database confounded our ability to analyze the AATD genotype distribution. Only 96 patients in the APPM cohort and 1444 in the control cohort were recorded as having fibrosis, which was lower than anticipated, likely owing to underdiagnosis (patients are often asymptomatic in the early stages of fibrosis) and/or underreporting[22]. Furthermore, a substantial number of patients with fibrosis developed cirrhosis and liver decompensation events, which suggests that these patients were more likely to be at an advanced stage of fibrosis. Therefore, the development and implementation of structured early screening programs may be useful to increase the early detection of fibrosis in the general population[23]. Fibrosis stage data were not available in the database, which together with the low number of patients in this category constitutes a significant limitation as survival prognosis is thought to be highly linked to fibrosis stage[24]. In addition, regional differences in morbidity and mortality may exist, and our data may not be representative of geographic regions outside of Germany. However, in Germany, approximately 73.3 million people were insured by an SHI fund in 2020, which equates to approximately 88% of the general population. Owing to the uniform structure of SHI funds in all regions of Germany, we consider the data to be representative of the German population[25]. Lastly, as this was a retrospective insurance claims-based study that collected data using ICD-10-GM codes, we were unable to assess body weight/body mass index, which are known risk factors for early progression to advanced liver disease[26], and unable to determine the exact procedures involved in the diagnosis of liver disease.
CONCLUSION
Among patients with liver disease in Germany, those with APPM experience substantial burden and a higher rate of liver disease progression than patients without APPM. To enable accurate diagnosis and inform disease management, it is important to have specific diagnostic codes that differentiate between genetic liver disease and liver manifestations from other causes.
ARTICLE HIGHLIGHTS
Research background
Alpha-1 antitrypsin deficiency (AATD) is a rare genetic disease that can result in the development of liver and/or lung disease, and is a leading cause of inherited alterations in plasma protein metabolism (APPM).
Research motivation
Currently, there is a lack of information on the natural history and epidemiology of AATD.
Research objectives
To understand the prevalence, burden and progression of liver disease in patients with APPM, which includes patients diagnosed with AATD, in Germany.
Research methods
A retrospective analysis of anonymized, patient-level, insurance claims data from a German health insurance provider (AOK PLUS) was conducted. The APPM cohort comprised patients with APPM (01/01/2010-30/09/2020) and incident liver disease (01/01/2012-30/09/2020) and the control cohort comprised patients without APPM but with incident liver disease. Outcomes were incidence/prevalence of liver disease in patients with APPM, demographics/baseline characteristics, disease progression, progression-free survival, mortality, and diagnostic procedures.
Research results
Overall, 2680 and 26299 patients were included in the APPM [fibrosis (96); cirrhosis (2584)] and control [fibrosis (1444); cirrhosis (24855)] cohorts, respectively. The annual incidence and prevalence of APPM and liver disease was 10-15/100000 and 36-51/100000, respectively. Median survival was shorter in the APPM cohort (2.6 years) than in the control cohort (4.3 years). In patients in the APPM cohort with fibrosis and cirrhosis, respectively, median survival was 4.7 years and 2.5 years. More patients in the APPM cohort (92.0%) experienced liver disease progression than in the control cohort (67.2%). Median progression-free survival was shorter in the APPM cohort [0.9 years (95%CI: 0.7-1.1)] compared with the control cohort [3.7 years (95%CI: 3.6-3.8); P < 0.001]. In patients with cirrhosis, event-free survival for ascites, hepatic encephalopathy, hepatic failure, and esophageal/gastric varices was longer in the control cohort than in the APPM cohort (P < 0.001). In patients with fibrosis, event-free survival for ascites, cirrhosis, hepatic failure, and esophageal/gastric varices was longer in the control cohort than in the APPM cohort (P < 0.001). The most common diagnostic procedures within 12 mo after the first diagnosis of liver disease in the APPM cohort were imaging procedures (66.3%) and laboratory tests (51.0%).
Research conclusions
In Germany, patients with APPM and liver disease experience substantial burden and a higher rate of and earlier liver disease progression than patients without APPM.
Research perspectives
The adoption of diagnosis codes specific to AATD should enable differentiation of this disease from other APPM disorders and facilitate earlier diagnosis and patient management. This should contribute to slowing disease progression and decreasing the burden of disease in patients with this rare, chronic disease.
ACKNOWLEDGEMENTS
Medical writing and submission assistance was provided by Matthew Reynolds of Oxford PharmaGenesis, Oxford, United Kingdom and was supported by Takeda Development Center Americas, Inc.
Footnotes
Institutional review board statement: Institutional review board approval was not required for this retrospective analysis of anonymized data.
Informed consent statement: Signed informed consent forms were not required as this was a retrospective analysis of anonymized data.
Conflict-of-interest statement: Dr. Strnad reports grants and other from CSL Behring, grants and other from Grifols, grants and other from Arrowhead Pharmaceuticals, grants and other from Dicerna Pharmaceuticals, grants from Vertex Pharmaceuticals, other from Albireo, other from GlaxoSmithKline, other from Intellia Pharmaceuticals, other from Ono Pharmaceuticals, other from Takeda Pharmaceuticals, during the conduct of the study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: May 22, 2023
First decision: July 8, 2023
Article in press: September 18, 2023
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Germany
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gaspar R, Portugal; Ren WR, China; Zhang Y, China S-Editor: Chen YL L-Editor: Filipodia P-Editor: Cai YX
Contributor Information
Nils Picker, Real-World Evidence, Cytel Inc. Ingress-Health HWM GmbH, Wismar 23966, Germany.
May Hagiwara, R&D, Global Evidence and Outcomes, Takeda Development Center Americas, Inc., Cambridge, MA 02139, United States.
Severin Baumann, Real-World Evidence, Cytel Inc. Ingress-Health HWM GmbH, Wismar 23966, Germany.
Ed G Marins, Global Medical Affairs, Takeda Development Center Americas, Inc., Cambridge, MA 02139, United States.
Thomas Wilke, IPAM Institute, IPAM E.V., Wismar 23966, Germany.
Kaili Ren, Statistics and Quantitative Sciences, Data Science Institute, Takeda Development Center Americas, Inc., Cambridge, MA 02139, United States.
Ulf Maywald, Drug Department, AOK PLUS, Dresden 01058, Germany.
Chitra Karki, R&D, Global Evidence and Outcomes, Takeda Development Center Americas, Inc., Cambridge, MA 02139, United States.
Pavel Strnad, Medical Clinic III, Gastroenterology, Metabolic Diseases and Intensive Care, University Hospital RWTH Aachen, Aachen 52074, Germany. pstrnad@ukaachen.de.
Data sharing statement
The data that support the findings of this study are available from AOK PLUS. Restrictions apply to the availability of these data, which were used under license for this study.
References
- 1.Kuscuoglu D, Janciauskiene S, Hamesch K, Haybaeck J, Trautwein C, Strnad P. Liver - master and servant of serum proteome. J Hepatol. 2018;69:512–524. doi: 10.1016/j.jhep.2018.04.018. [DOI] [PubMed] [Google Scholar]
- 2.Quinlan GJ, Martin GS, Evans TW. Albumin: biochemical properties and therapeutic potential. Hepatology. 2005;41:1211–1219. doi: 10.1002/hep.20720. [DOI] [PubMed] [Google Scholar]
- 3.Ferrarotti I, Carroll TP, Ottaviani S, Fra AM, O'Brien G, Molloy K, Corda L, Medicina D, Curran DR, McElvaney NG, Luisetti M. Identification and characterisation of eight novel SERPINA1 Null mutations. Orphanet J Rare Dis. 2014;9:172. doi: 10.1186/s13023-014-0172-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Brien ML, Buist NR, Murphey WH. Neonatal screening for alpha1-antitrypsin deficiency. J Pediatr. 1978;92:1006–1010. doi: 10.1016/s0022-3476(78)80388-6. [DOI] [PubMed] [Google Scholar]
- 5.Strnad P, McElvaney NG, Lomas DA. Alpha(1)-Antitrypsin Deficiency. N Engl J Med. 2020;382:1443–1455. doi: 10.1056/NEJMra1910234. [DOI] [PubMed] [Google Scholar]
- 6.Townsend SA, Edgar RG, Ellis PR, Kantas D, Newsome PN, Turner AM. Systematic review: the natural history of alpha-1 antitrypsin deficiency, and associated liver disease. Aliment Pharmacol Ther. 2018;47:877–885. doi: 10.1111/apt.14537. [DOI] [PubMed] [Google Scholar]
- 7.Fromme M, Schneider CV, Trautwein C, Brunetti-Pierri N, Strnad P. Alpha-1 antitrypsin deficiency: A re-surfacing adult liver disorder. J Hepatol. 2022;76:946–958. doi: 10.1016/j.jhep.2021.11.022. [DOI] [PubMed] [Google Scholar]
- 8.Hamesch K, Mandorfer M, Pereira VM, Moeller LS, Pons M, Dolman GE, Reichert MC, Schneider CV, Woditsch V, Voss J, Lindhauer C, Fromme M, Spivak I, Guldiken N, Zhou B, Arslanow A, Schaefer B, Zoller H, Aigner E, Reiberger T, Wetzel M, Siegmund B, Simões C, Gaspar R, Maia L, Costa D, Bento-Miranda M, van Helden J, Yagmur E, Bzdok D, Stolk J, Gleiber W, Knipel V, Windisch W, Mahadeva R, Bals R, Koczulla R, Barrecheguren M, Miravitlles M, Janciauskiene S, Stickel F, Lammert F, Liberal R, Genesca J, Griffiths WJ, Trauner M, Krag A, Trautwein C, Strnad P European Alpha1-Liver Study Group. Liver Fibrosis and Metabolic Alterations in Adults With alpha-1-antitrypsin Deficiency Caused by the Pi*ZZ Mutation. Gastroenterology. 2019;157:705–719.e18. doi: 10.1053/j.gastro.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 9.Karatas E, Di-Tommaso S, Dugot-Senant N, Lachaux A, Bouchecareilh M. Overview of alpha-1 antitrypsin deficiency-mediated liver disease. EMJ Hepatol. 2019;7:65–79. [Google Scholar]
- 10.Schlitt HJ, Loss M, Scherer MN, Becker T, Jauch KW, Nashan B, Schmidt H, Settmacher U, Rogiers X, Neuhaus P, Strassburg C. [Current developments in liver transplantation in Germany: MELD-based organ allocation and incentives for transplant centres] Z Gastroenterol. 2011;49:30–38. doi: 10.1055/s-0029-1245946. [DOI] [PubMed] [Google Scholar]
- 11.Flemming R. Patterns of pregabalin prescribing in four German federal states: analysis of routine data to investigate potential misuse of pregabalin. BMJ Open. 2022;12:e060104. doi: 10.1136/bmjopen-2021-060104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Datzmann T, Schmitt J, Fuhrmann S, Roessler M, Meier F, Schoffer O. Implementation and Effectiveness of Novel Therapeutic Substances for Advanced Malignant Melanoma in Saxony, Germany, 2010-2020-Cohort Study Based on Administrative Data. Cancers (Basel) 2021;13:6150. doi: 10.3390/cancers13246150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Markevych I, Tesch F, Datzmann T, Romanos M, Schmitt J, Heinrich J. Outdoor air pollution, greenspace, and incidence of ADHD: A semi-individual study. Sci Total Environ. 2018;642:1362–1368. doi: 10.1016/j.scitotenv.2018.06.167. [DOI] [PubMed] [Google Scholar]
- 14.Trautmann F, Schuler M, Schmitt J. Burden of soft-tissue and bone sarcoma in routine care: Estimation of incidence, prevalence and survival for health services research. Cancer Epidemiol. 2015;39:440–446. doi: 10.1016/j.canep.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Gurbuz B, Guldiken N, Reuken P, Fu L, Remih K, Preisinger C, Brůha R, Leníček M, Petrtýl J, Reissing J, Aly M, Fromme M, Zhou B, Karkossa I, Schubert K, von Bergen M, Stallmach A, Bruns T, Strnad P. Biomarkers of hepatocellular synthesis in patients with decompensated cirrhosis. Hepatol Int. 2023;17:698–708. doi: 10.1007/s12072-022-10473-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen VL, Burkholder DA, Moran IJ, DiBattista JV, Miller MJ, Chen Y, Du X, Oliveri A, Cushing KC, Lok AS, Speliotes EK. Hepatic decompensation is accelerated in patients with cirrhosis and alpha-1 antitrypsin Pi*MZ genotype. JHEP Rep. 2022;4:100483. doi: 10.1016/j.jhepr.2022.100483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balcar L, Tonon M, Semmler G, Calvino V, Hartl L, Incicco S, Jachs M, Bauer D, Hofer BS, Gambino CG, Accetta A, Brocca A, Trauner M, Mandorfer M, Piano S, Reiberger T Baveno Cooperation: an EASL consortium. Risk of further decompensation/mortality in patients with cirrhosis and ascites as the first single decompensation event. JHEP Rep. 2022;4:100513. doi: 10.1016/j.jhepr.2022.100513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sandhaus R, Strange C, Stone G, Runken MC, Blanchette CM, Howden R. Comorbidity Associations with AATD Among Commercially Insured and Medicare Beneficiaries with COPD in the US. Int J Chron Obstruct Pulmon Dis. 2020;15:2389–2397. doi: 10.2147/COPD.S263297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aymé S, Bellet B, Rath A. Rare diseases in ICD11: making rare diseases visible in health information systems through appropriate coding. Orphanet J Rare Dis. 2015;10:35. doi: 10.1186/s13023-015-0251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Acquavella J, Vágó E, Sorensen HT, Horváth-Puhó E, Hess GP. Registry-based cohort study of alpha-1 antitrypsin deficiency prevalence, incidence and mortality in Denmark 2000-2018. BMJ Open Respir Res. 2022;9:e001281. doi: 10.1136/bmjresp-2022-001281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barrecheguren M, Monteagudo M, Simonet P, Llor C, Rodriguez E, Ferrer J, Esquinas C, Miravitlles M. Diagnosis of alpha-1 antitrypsin deficiency: a population-based study. Int J Chron Obstruct Pulmon Dis. 2016;11:999–1004. doi: 10.2147/COPD.S108505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karlsen TH, Sheron N, Zelber-Sagi S, Carrieri P, Dusheiko G, Bugianesi E, Pryke R, Hutchinson SJ, Sangro B, Martin NK, Cecchini M, Dirac MA, Belloni A, Serra-Burriel M, Ponsioen CY, Sheena B, Lerouge A, Devaux M, Scott N, Hellard M, Verkade HJ, Sturm E, Marchesini G, Yki-Järvinen H, Byrne CD, Targher G, Tur-Sinai A, Barrett D, Ninburg M, Reic T, Taylor A, Rhodes T, Treloar C, Petersen C, Schramm C, Flisiak R, Simonova MY, Pares A, Johnson P, Cucchetti A, Graupera I, Lionis C, Pose E, Fabrellas N, Ma AT, Mendive JM, Mazzaferro V, Rutter H, Cortez-Pinto H, Kelly D, Burton R, Lazarus JV, Ginès P, Buti M, Newsome PN, Burra P, Manns MP. The EASL-Lancet Liver Commission: protecting the next generation of Europeans against liver disease complications and premature mortality. Lancet. 2022;399:61–116. doi: 10.1016/S0140-6736(21)01701-3. [DOI] [PubMed] [Google Scholar]
- 23.Labenz C, Arslanow A, Nguyen-Tat M, Nagel M, Wörns MA, Reichert MC, Heil FJ, Mainz D, Zimper G, Römer B, Binder H, Farin-Glattacker E, Fichtner U, Graf E, Stelzer D, Van Ewijk R, Ortner J, Velthuis L, Lammert F, Galle PR. Structured Early detection of Asymptomatic Liver Cirrhosis: Results of the population-based liver screening program SEAL. J Hepatol . 2022;77:695–701. doi: 10.1016/j.jhep.2022.04.009. [DOI] [PubMed] [Google Scholar]
- 24.Dulai PS, Singh S, Patel J, Soni M, Prokop LJ, Younossi Z, Sebastiani G, Ekstedt M, Hagstrom H, Nasr P, Stal P, Wong VW, Kechagias S, Hultcrantz R, Loomba R. Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: Systematic review and meta-analysis. Hepatology. 2017;65:1557–1565. doi: 10.1002/hep.29085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dornquast C, Kroll LE, Neuhauser HK, Willich SN, Reinhold T, Busch MA. Regionale Unterschiede in der Prävalenz kardiovaskulärer Erkrankungen. Deutsches Ärzteblatt . 2016;42:704–11. doi: 10.3238/arztebl.2016.0704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bowlus CL, Willner I, Zern MA, Reuben A, Chen P, Holladay B, Xie L, Woolson RF, Strange C. Factors associated with advanced liver disease in adults with alpha1-antitrypsin deficiency. Clin Gastroenterol Hepatol. 2005;3:390–396. doi: 10.1016/s1542-3565(05)00082-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from AOK PLUS. Restrictions apply to the availability of these data, which were used under license for this study.