Abstract
Background
Low-intensity shockwave therapy for erectile dysfunction is emerging as a promising treatment option.
Aim
This randomized sham-controlled crossover trial assessed the efficacy of low-intensity shockwave therapy in the treatment of erectile dysfunction.
Methods
Thirty-three participants with organic erectile dysfunction were enrolled and randomized to shockwave therapy (n = 17) or sham (n = 16). The sham group was allowed to cross over to receive shockwave therapy after 1 month.
Outcomes
Primary outcomes were the changes in Sexual Health Inventory for Men (SHIM) score and Erection Hardness Score at 1 month following shockwave therapy vs sham, and secondary outcomes were erectile function measurements at 1, 3, and 6 months following shockwave therapy.
Results
At 1 month, mean SHIM scores were significantly increased in the shockwave therapy arm as compared with the sham arm (+3.0 vs −0.7, P = .024). Participants at 6 months posttreatment (n = 33) showed a mean increase of 5.5 points vs baseline (P < .001), with 20 (54.6%) having an increase ≥5. Of the 25 men with an initial Erection Hardness Score <3, 68% improved to a score ≥3 at 6 months. When compared with baseline, the entire cohort demonstrated significant increases in erectile function outcomes at 1, 3, and 6 months after treatment.
Clinical Implications
In this randomized sham-controlled crossover trial, we showed that 54.6% of participants with organic erectile dysfunction met the minimal clinically important difference in SHIM scores after treatment with low-intensity shockwave therapy.
Strengths and Limitations
Strengths of this study include a sham-controlled group that crossed over to treatment. Limitations include a modest sample size at a single institution.
Conclusions
Low-intensity shockwave therapy improves erectile function in men with erectile dysfunction as compared with sham treatment, which persists even 6 months after treatment.
Clinical Trial Registration
ClinicalTrials.gov NCT04434352.
Keywords: Keywords: extracorporeal shockwave therapy, erectile dysfunction, male sexual impotence, randomized controlled trial, sham treatment
Introduction
Erectile dysfunction (ED) is defined as the inability to achieve or maintain an erection sufficient for intercourse, with the mainstay of treatment being phosphodiesterase 5 inhibitors (PDE5is) followed by more invasive options.1 Low-intensity shockwave therapy (LiSWT) has emerged as a viable treatment option within the last decade,2,3 as many studies have reported improvements in erectile function.4-8
The exact mechanism of LiSWT on ED has yet to be elucidated; however, it has been proposed that the microtrauma caused by the process stimulates release of angiogenic growth factors through cellular signaling pathways.9,10 These angiogenic growth factors likely promote neovascularization and in turn increase blood flow to the corpora. Accordingly, multiple randomized controlled trials have demonstrated subjective and physiologic improvements in erectile function and penile hemodynamics, respectively.11,12
In our prospective randomized sham-controlled trial, we aim to expand on previous studies assessing the efficacy and durability of LiSWT in the treatment of ED. Furthermore, given the foundation of data on which this study is based, we elected to allow the sham arm to cross over 1 month following treatment. We hypothesized that LiSWT would be more efficacious than sham and that following crossover, the sham arm treated with LiSWT would see similar benefits.
Methods
Population
We implemented a 2-arm stratified single-blinded randomized controlled clinical trial to determine the impact of sham vs LiSWT on erectile function. Participants were included by baseline Sexual Health Inventory for Men (SHIM) scores (≥8 and ≤21), hemoglobin A1c (≤7.5% within 3 months), and testosterone levels (>300 ng/dL). Exclusion criteria were as follows: a history of extensive pelvic surgery, non–prostate-related cancer treatment within the previous 6 months, any past prostate cancer treatment, significant neurologic disease, and known penile malformation (eg, Peyronie’s disease). Participants who underwent randomization and analysis were those with organic ED, either PDE5i responsive or nonresponsive. For those taking PDE5is prior to the study, a washout period of 2 weeks was implemented before treatment initiation, and participants were instructed to refrain from use of any erectile aids during their treatment course up to their assessment 1 month following treatment completion.
LiSWT intervention
Participants were treated in clinic twice weekly for 3 consecutive weeks for 6 treatment visits. Treatments were performed with a handheld Duolith device (Storz). At each treatment visit, a urologist experienced in performing LiSWT delivered 1000 shocks to each corpus cavernosum along the penile shaft and 500 additional shocks to each proximal corpus at the level of the perineum, for a total of 3000 shocks at 0.1 mJ/mm2 and 5.0 Hz per treatment session. Shockwaves were prevented from penetrating tissue in the sham arm by an alternate probe tip that blocks any shockwave energy. Prior to each treatment, participants were asked if they experienced any adverse effects from previous treatments. Of note, while participants were blinded, all authors, providers, and statisticians were unblinded to grouping.
At 1 month after the last treatment, the sham arm was informed of its placement and given the opportunity to cross over to LiSWT. For the crossover group, randomized intervention scores at 1 month were used as the baseline.
Outcome measurement
We measured erectile function outcomes using 2 validated instruments: the abridged 5-item version of the International Index of Erectile Function (IIEF), also known as the SHIM, and the Erection Hardness Score (EHS).13,14 The SHIM has a maximum score of 25, with 8 to 11 defining moderate ED, 12 to 16 mild-moderate, and 17 to 21 mild. Our study used a SHIM change ≥5 points as the minimal clinically important difference (MCID) in accordance with Chung and Cartmill.15 Follow-up then continued with the SHIM and EHS at 1, 3, and 6 months for the combined arms. The EHS, ranging from 0 to 4, is a widely validated survey to assess strength of erection. A score ≥3 indicates ability to achieve successful penetration. Analyses were performed with an intention-to-treat methodology (randomized).
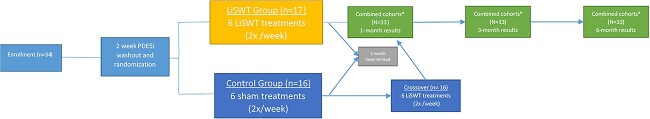
Primary outcomes were the change in SHIM score and EHS at 1 month following treatment with LiSWT or sham. Secondary outcomes included changes in SHIM score and EHS of the original LiSWT treatment group combined with the crossover group from baseline to 1, 3, and 6 months posttreatment. Of note, SHIM and EHS measurements at months 1, 3, and 6 in the crossover arm were compared with measurements immediately following sham treatment. Absolute change in scores from baseline was determined with the remaining patients at time intervals. A detailed study protocol is presented in Figure 1. Since there was an interim analysis, the nominal alpha for this final analysis was .049 (ie, P < .05) with 80% power.
Figure 1.
Study protocol. Of note, 1 participant randomized to sham was lost to follow-up before assessment of the primary outcome. *Participants who crossed over were measured at 1, 3, and 6 months after completion of their 3-week, 6-treatment course of low-intensity shockwave therapy.
Statistical analysis
Changes in SHIM scores were compared between the treatment arms with a Student t-test, while changes in EHS were compared by Wilcoxon rank sum test. Fisher exact tests were used to compare categorized scores with levels based on decrease, no change, or increase. Mixed-effects models were used to test for changes in outcome over time for all patients undergoing LiSWT. Models were adjusted for cohort (group) and smoking and underwent a Sidak adjustment for multiple comparisons. Data visualization and statistical analysis were performed with Microsoft Excel, Microsoft Word, and Stata version 17 (StataCorp). This study was performed per the CONSORT reporting guidelines.16 Randomization was performed by permutated block randomization; block sizes ranged from 2 to 8 via the blockrand package in R stratified by clinical group. Electronic randomization was generated by the study biostatistician. Clinical research coordinators enrolled patients, and all participants provided written consent. Only the clinician performing the treatment had access to the randomization module, with other study personnel blinded to the arm. Enrollment began in April 2020 and ended due to limits on clinical time constraints. Institutional review board approval was obtained (HSR 190082).
Results
Thirty-four participants enrolled in the trial and 33 completed treatment: 17 in the LiSWT arm and 16 in the sham arm. One in the sham arm was lost to follow-up before the primary outcome was assessed. Demographics and baseline clinical characteristics are shown in Table 1.
Table 1.
Demographic and baseline clinical characteristics.a
| Sham (n = 16) | LiSWT (n = 17) | |
|---|---|---|
| Age, y | 64.6 (52.3–70.2) | 67.0 (47.2–69.6) |
| History of | ||
| Diabetes mellitus | 3 (18.8) | 4 (23.5) |
| Coronary artery disease | 2 (12.5) | 1 (5.9) |
| Hypertension | 9 (56.3) | 5 (29.4) |
| Hyperlipidemia | 6 (37.5) | 6 (35.3) |
| Low testosterone | 4 (25.0) | 3 (17.6) |
| Smoking | 4 (25.0) | 5 (29.4) |
| Denies any medical history | 3 (18.8) | 5 (29.4) |
| PDE5i response prior to treatment | 6 (37.5) | 5 (29.4) |
Abbreviations: LiSWT, low-intensity shockwave therapy; PDE5i, phosphodiesterase 5 inhibitor.
aData are presented as median (IQR) or No. (%).
Regarding the primary outcome of the study (Table 2), participants had a 1-month change in mean SHIM score of +3.0 in the LiSWT arm and −0.7 in the sham-treated arm (P = .024). This corresponds to 38.1% improvement in the LiSWT arm and 0.1% decline in the sham arm (P = .026). Eight patients (47.1%) in the LiSWT arm and none in the sham arm reached a SHIM score change ≥5 points at 1 month posttreatment . No statistically significant differences were observed in EHS between the LiSWT and sham arms at 1 month.
Table 2.
LiSWT effect on SHIM score and EHS at 1 month.
| Sham (n = 16) | LiSWT (n = 17) | P value | |
|---|---|---|---|
| SHIM score, mean (SD) | |||
| Baseline | 12.1 (3.3) | 10.8 (3.6) | .31 |
| 1 mo | 11.4 (3.6) | 13.8 (4.7) | .10 |
| Change | |||
| Absolute | −0.7 (4.1) | +3.0 (4.8) | .024a |
| Relative, % | −0.1 (36.2) | +38.1 (55.2) | .026a |
| Change in EHS | |||
| Median (IQR) | |||
| Absolute | 0.0 (−1.0 to 0.0) | 0.0 (−1.0 to 1.0) | .98 |
| Relative, % | 0.0 (−50.0 to 0.0) | 0.0 (−50.0 to 33.3) | .92 |
| No. (%) | .06 | ||
| Decreased | 1 (6.3) | 5 (29.4) | |
| None | 10 (62.5) | 4 (23.5) | |
| Increased | 5 (31.3) | 8 (47.1) | .48 |
Abbreviations: EHS, Erection Hardness Score; LiSWT, low-intensity shockwave therapy; SHIM, Sexual Health Inventory for Men.
P < .05.
At 1 month, all 16 participants opted to cross over and receive LiSWT. Furthermore, 1 from the original treatment arm was lost to follow-up after receiving LiSWT.
Among the 33 participants (Figure 2), mean SHIM scores increased by 4.0, 4.4, and 5.5 at 1, 3, and 6 months following treatment (P = .001, P = .001, and P < .001), respectively, as compared with baseline. Additionally, at 1, 3, and 6 months, 8 (24.2%), 15 (45.4%), and 18 (54.6%) participants had SHIM scores increase by ≥5. Mean EHS vs baseline increased by 0.5 at 1 month, 0.8 at 3 months, and 1.0 at 6 months (P = .029, P = .001, and P < .001; Table 3). Of the 25 patients with an initial EHS <3, 17 (68%) improved to ≥3 at 6 months. No one reported adverse effects as a result of treatment.
Figure 2.
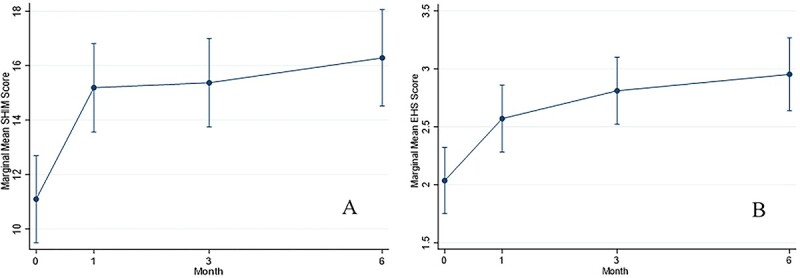
Longitudinal mean (A) SHIM score and (B) EHS for participants after LiSWT treatment. EHS, Erection Hardness Score; LiSWT, low-intensity shockwave therapy; SHIM, Sexual Health Inventory for Men.
Table 3.
Longitudinal mean SHIM score and EHS for participants after LiSWT treatment.a
| LiSWT (n = 33) | P value | |
|---|---|---|
| SHIM score | ||
| Baseline | 11.1 (3.5) | |
| 1 mo | 15.2 (4.7) | .001 |
| 3 mo | 15.4 (4.9) | .001 |
| 6 mo | 16.3 (5.9) | <.001 |
| EHS | ||
| Baseline | 2.0 (0.9) | |
| 1 mo | 2.6 (0.9) | .03 |
| 3 mo | 2.8 (0.8) | .001 |
| 6 mo | 3.0 (0.9) | <.001 |
Abbreviations: EHS, Erection Hardness Score; LiSWT, low-intensity shockwave therapy; SHIM, Sexual Health Inventory for Men.
aData are presented as mean (SD). Each P value reaches statistical significance (P < .05).
Discussion
This prospective sham-controlled crossover study composed of men with mild to moderate ED showed that 6 sessions of LiSWT over a 3-week period is effective at improving erectile function at 1 month posttreatment as compared with sham. Additionally, following crossover, our study found that LiSWT leads to significant improvements in SHIM score and EHS at all measured time points, with persistent improvements from baseline at 6 months following treatment. Furthermore, 54.6% of participants with organic ED met the MCID in SHIM scores.15,17 While there were no significant changes in EHS between the LiSWT and sham arms after treatment, among those with an initial EHS <3, 68% reached an EHS ≥3 at study completion, which correlates to an increased likelihood of successful penetrative sexual intercourse.18
Despite several first-line treatments according to the American Urological Association guidelines on ED—such as PDE5i, vacuum erectile device, and intracavernosal injections—patients may report dissatisfaction with these treatments, experience adverse effects, or have difficulty with treatment compliance.19-22 Additionally, these treatment modalities do not restore spontaneous erections. The development of a method that rehabilitates spontaneous erectile function without medication, injections, or surgery would be an advantageous and satisfying aid in restoring or maintaining erectile function. Furthermore, if men who undergo LiSWT have improved responsiveness to less invasive ED treatments, this may also positively affect quality of life and patient satisfaction.
Kalyvianakis et al performed a double-blind randomized sham-controlled trial on 70 men with moderate vasculogenic ED who responded to PDE5is.23 The authors saw a significant increase of 4.9 in mean IIEF–Erectile Function score at 1 month in the LiSWT arm relative to 0.9 in the sham arm. Of 34 participants undergoing LiSWT, 27 (79%) met the MCID at 3 months for the IIEF–Erectile Function score. This study included 2 arms of 35 participants who underwent 12 sessions of 5000 shocks at 0.096 mJ/mm2 and 5 Hz over 6 weeks with an ARIES 2 device. While our study had similar changes in SHIM score, the Kalyvianakis et al study had more participants who met the MCID. This may be explained by the study authors excluding mild ED and using a different treatment protocol than ours; furthermore, their study comprised participants with a lower median age, and it did not include PDE5i nonresponders. Chung et al also reported a double-blind randomized sham-controlled trial on men with mild to moderate vascular ED (SHIM ≥12) refractory to medical therapy, with 12 treatments of 3000 shocks at 0.25 mJ/mm2 and an emission frequency of 6 Hz over 6 weeks.24 The 30 participants who received LiSWT had SHIM increases of 4.4, 4.2, and 4.2 at 1, 3, and 6 months, respectively, vs baseline. Their results are comparable to ours. They also reported that 70% of their LiSWT arm met the MCID. There are notable differences that may explain the higher percentage who met the MCID—for instance, their study population had a lower median age and included participants with a higher median baseline SHIM score. In addition, their study excluded PDE5i-responding participants and had a different treatment protocol. While the energy density that we used for LiSWT was lower than that in these recently published studies, several meta-analyses have reported greater therapeutic benefit with low energy density.4-6
We believe that the strength of our study lies in the crossover of the sham arm. Given our hypothesis that after 1 month there would be significant erectile function improvements in the treatment arm, we designed our study to allow for the sham-treated group to cross over to receive LiSWT. When the arms were combined, the erectile function improvements persisted. There is no clear reason for the lack of statistical improvement in EHS at 1 month; however, we note continual improvement in both study metrics over the study period and believe that the full effect of the neoangiogenesis mechanism likely takes >1 month. This study contributes to a growing body of literature that LiSWT is a safe and effective method for improving baseline erectile function in men who have mild to moderate organic ED.
A limitation of this study is the lack of objective measurements of penile hemodynamics, although a recent study demonstrated through power Doppler measurements that LiSWT promotes neovascularization of the functional arteries in the penis.25 Other limitations include the small sample size and performance at a single institution. Additionally, the crossover at 1 month prevents a long-term comparison of LiSWT vs sham. Still, as mentioned earlier, we felt it appropriate to allow for crossover at this time point, given our expectation of improvement in erectile function. Another limitation is that the sham group, after crossover, was unblinded to active treatment and therefore this in troduced the potential for placebo effect that they know they are receiving active treatment. Unfortunately, this cannot be corrected for. Despite these limitations, our data contribute to the literature by assessing longitudinal LiSWT effectiveness in patients with organic ED and maintaining our significant positive results on erectile function.
Conclusion
Restorative therapies for the treatment of ED, such as LiSWT, have grown in popularity. The present analysis shows improvement in SHIM scores in men undergoing LiSWT for ED when compared with a sham arm at 1 month. Furthermore, after crossover of the sham arm to LiSWT, our cohort saw improvements in SHIM score and EHS, with 54.6% of participants meeting the MCID for the former. Last, the erectile function recovery resulting from LiSWT persisted even 6 months after treatment. Our study contributes to the ever-growing literature of the effectiveness and safety of LiSWT in the treatment of ED.
Author contributions
E.H.K., D.J.B., M.M.A.: manuscript drafting, manuscript reviewing, data interpretation, final approval. S.J.R., I.V.M.: statistics and data interpretation, manuscript reviewing, final approval. B.J.O.: data collection and data interpretation, manuscript reviewing, final approval. H.M.B., C.C.B., M.B.C.: data collection, project design, manuscript reviewing, final approval. M.L.G.: project design, manuscript reviewing, final approval. D.E.R., N.M.O.: project design, data interpretation, manuscript reviewing, final approval. R.P.S.: project design, data interpretation, manuscript reviewing, final approval, project supervision.
Funding
None declared.
Conflicts of interest
None declared.
Data availability
The data sets generated and/or analyzed during the current study are not publicly available due to patient-protected information status but are available from the corresponding author on reasonable request.
Contributor Information
Emmett H Kennady, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Darren J Bryk, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Marwan M Ali, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Sarah J Ratcliffe, Department of Public Health Sciences, School of Medicine, University of Virginia, Charlottesville, VA 22903, United States.
Indika V Mallawaarachchi, Department of Public Health Sciences, School of Medicine, University of Virginia, Charlottesville, VA 22903, United States.
Bahrom J Ostad, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Hamza M Beano, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Christopher C Ballantyne, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Sarah C Krzastek, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Matthew B Clements, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Mikel L Gray, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
David E Rapp, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Nicolas M Ortiz, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
Ryan P Smith, Department of Urology, University of Virginia, Charlottesville, VA 22903, United States.
References
- 1. Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013;381(9861):153–165. [DOI] [PubMed] [Google Scholar]
- 2. Lurz K, Dreher P, Levy J, et al. Low-intensity shockwave therapy in the treatment of erectile dysfunction. Cureus. 2020;12(11):e11286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vardi Y, Appel B, Jacob G, Massarwi O, Gruenwald I. Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. Eur Urol. 2010;58(2):243–248. [DOI] [PubMed] [Google Scholar]
- 4. Yao H, Wang X, Liu H, et al. Systematic review and meta-analysis of 16 randomized controlled trials of clinical outcomes of low-intensity extracorporeal shock wave therapy in treating erectile dysfunction. Am J Mens Health. 2022;16(2):155798832210875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zou ZJ, Tang LY, Liu ZH, et al. Short-term efficacy and safety of low-intensity extracorporeal shock wave therapy in erectile dysfunction: a systematic review and meta-analysis. Int Braz J Urol. 2017;43(5):805–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Man L, Li G. Low-intensity extracorporeal shock wave therapy for erectile dysfunction: a systematic review and meta-analysis. Urology. 2018;119:97–103. 10.1016/j.urology.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 7. Campbell JD, Trock BJ, Oppenheim AR, Anusionwu I, Gor RA, Burnett AL. Meta-analysis of randomized controlled trials that assess the efficacy of low-intensity shockwave therapy for the treatment of erectile dysfunction. Ther Adv Urol. 2019;11:175628721983836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dong L, Chang D, Zhang X, et al. Effect of low-intensity extracorporeal shock wave on the treatment of erectile dysfunction: a systematic review and meta-analysis. Am J Mens Health. 2019;13(2):155798831984674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gotte G, Amelio E, Russo S, Marlinghaus E, Musci G, Suzuki H. Short-time non-enzymatic nitric oxide synthesis from L-arginine and hydrogen peroxide induced by shock waves treatment. FEBS Lett. 2002;520(1-3):153–155. [DOI] [PubMed] [Google Scholar]
- 10. Xu L, Zhao Y, Wang M, et al. Defocused low-energy shock wave activates adipose tissue-derived stem cells in vitro via multiple signaling pathways. Cytotherapy. 2016;18(12):1503–1514. [DOI] [PubMed] [Google Scholar]
- 11. Gruenwald I, Appel B, Vardi Y. Low-intensity extracorporeal shock wave therapy—a novel effective treatment for erectile dysfunction in severe ED patients who respond poorly to PDE5 inhibitor therapy. J Sex Med. 2012;9(1):259–264. [DOI] [PubMed] [Google Scholar]
- 12. Clavijo RI, Kohn TP, Kohn JR, Ramasamy R. Effects of low-intensity extracorporeal shockwave therapy on erectile dysfunction: a systematic review and meta-analysis. J Sex Med. 2017;14(1):27–35. [DOI] [PubMed] [Google Scholar]
- 13. Mulhall JP, Goldstein I, Bushmakin AG, Cappelleri JC, Hvidsten K. Validation of the Erection Hardness Score. J Sex Med. 2007;4(6):1626–1634. [DOI] [PubMed] [Google Scholar]
- 14. Rosen R, Cappelleri J, Smith M, Lipsky J, Peña B. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11(6):319–326. [DOI] [PubMed] [Google Scholar]
- 15. Chung E, Cartmill R. Evaluation of long-term clinical outcomes and patient satisfaction rate following low intensity shock wave therapy in men with erectile dysfunction: a minimum 5-year follow-up on a prospective open-label single-arm clinical study. Sex Med. 2021;9(4):100384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rosen RC, Allen KR, Ni X, Araujo AB. Minimal clinically important differences in the erectile function domain of the International Index of Erectile Function scale. Eur Urol. 2011;60(5):1010–1016. [DOI] [PubMed] [Google Scholar]
- 18. Goldstein I, Mulhall JP, Bushmakin AG, Cappelleri JC, Hvidsten K, Symonds T. The Erection Hardness Score and its relationship to successful sexual intercourse. J Sex Med. 2008;5(10):2374–2380. [DOI] [PubMed] [Google Scholar]
- 19. Mykoniatis I, Pyrgidis N, Sokolakis I, et al. Assessment of combination therapies vs monotherapy for erectile dysfunction: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(2):e2036337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brison D, Seftel A, Sadeghi-Nejad H. The resurgence of the vacuum erection device (VED) for treatment of erectile dysfunction. J Sex Med. 2013;10(4):1124–1135. [DOI] [PubMed] [Google Scholar]
- 21. Hsiao W, Bennett N, Guhring P, Narus J, Mulhall JP. Satisfaction profiles in men using intracavernosal injection therapy. J Sex Med. 2011;8(2):512–517. [DOI] [PubMed] [Google Scholar]
- 22. Belew D, Klaassen Z, Lewis RW. Intracavernosal injection for the diagnosis, evaluation, and treatment of erectile dysfunction: a review. Sex Med Rev. 2015;3(1):11–23. [DOI] [PubMed] [Google Scholar]
- 23. Kalyvianakis D, Mykoniatis I, Pyrgidis N, et al. The effect of low-intensity shock wave therapy on moderate erectile dysfunction: a double-blind, randomized sham-controlled clinical trial. J Urol. 2022;208(2):388–395. [DOI] [PubMed] [Google Scholar]
- 24. Chung E, Bailey W, Wang J. A prospective, randomized, double-blinded, clinical trial using a second-generation Duolith SD1 low-intensity shockwave machine in males with vascular erectile dysfunction. World J Mens Health. 2022;41(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scroppo FI, Pezzoni F, Gaeta F, et al. LI-ESWT improves hemodynamic parameters thus suggesting neoangiogenesis in patients with vascular erectile dysfunction. Int J Impot Res. 2022;34(3):237–242. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets generated and/or analyzed during the current study are not publicly available due to patient-protected information status but are available from the corresponding author on reasonable request.