Supplemental Digital Content is Available in the Text.
Key Words: HIV care continuum, criminal justice, arrest, mental health, substance use, outpatient care utilization
Abstract
Objective:
Justice involvement and psychiatric comorbidities contribute to excess HIV morbidity, yet their interaction is poorly understood. We examined associations of this overlap with HIV outcomes among people living with HIV (PLWH).
Methods:
We conducted a retrospective cohort study of PLWH aged 13 years and older residing in Marion County (Indianapolis), IN, during 2018 (n = 5730) using linked HIV surveillance, arrest, and clinical data. We used univariable and multivariable regression to evaluate main and interaction effects of 2010–2017 arrest and mental health diagnosis on 2018 linkage to care (LTC), retention in care (RIC), and undetectable viral load (UVL).
Results:
LTC decreased among those with, versus without, an arrest (P = 0.02), although mental health diagnoses had no significant effect on LTC. When controlling for demographics and substance use disorder, analyses indicated a protective effect of arrest history on odds of RIC (adjusted odds ratio [aOR] = 1.54) and UVL (aOR = 1.26). Mental health diagnosis also increased odds of RIC (aOR = 2.02) and UVL (aOR = 1.95). Post hoc tests demonstrated that these results were mediated by outpatient care utilization, although an arrest or mental health diagnosis did increase odds of RIC among PLWH and a history of low outpatient utilization.
Conclusions:
Outpatient care utilization improves HIV outcomes, even among those with justice involvement and psychiatric comorbidities. Holistic approaches to care can increase utilization. Implementation of “no wrong door” approaches, such as integration of mental health care in the primary care setting, simplifies health care navigation and improves access. Among those arrested, access to a Behavioral Court program can improve, rather than disrupt, HIV care.
INTRODUCTION
Incarceration and mental health are inextricably linked. Deinstitutionalization of psychiatric care placed the burden of mental health treatment on the criminal justice system.1,2 Roughly half of police encounters have a psychiatric basis,3 and more people with mental health disorders are incarcerated than in hospitals.4 Worsening matters, criminal justice involvement may aggravate mental health disorders.5 Prevalence of serious mental illness is 3 to 5 times higher in the US criminal justice system than in the general population.6 Moreover, given a history of justice involvement, mental illness is more prevalent among those living with versus without HIV.7
Incarceration and mental health are independently associated with HIV outcomes. Jail is considered one of the strongest predictors of HIV care disruption.8 People living with HIV (PLWH) and released from incarceration face barriers, including unemployment, homelessness, substance use disorder (SUD), and access to HIV care.9 Although retention in care (RIC) can improve during incarceration, it diminishes postrelease.10 Access to antiretroviral treatment (ART) is also negatively affected. Incarceration, particularly at intake and release, is associated with lengthy delays in prescription refills.11
Mental health diagnoses can precede, or result from, HIV infection.12 Several mental health diagnoses are linked to HIV progression through poor medication adherence13,14 and risky behaviors.13,15 After controlling for adherence and clinical and demographic characteristics, depression is linked to a decline in CD4 count16–18 and increased viral load and mortality.16,18–21 Mental illnesses are often underreported, but national estimates indicate that up to half of PLWH may be affected.22 Mental health diagnoses are often comorbid with SUD. Nearly half of PLWH in the United States are thought to misuse at least 1 substance,23,24 and both mental health and SUD play important roles in HIV treatment compliance.25–27 SUD is associated with increased transmission risk behavior, delayed HIV diagnosis, delayed linkage to care (LTC), and poor RIC.24,27
The overlap between justice involvement, mental health diagnosis, and SUD has been shown to contribute to excess HIV mortality among PLWH postrelease.28 Still, the interaction between these issues is unclear. We aim to assess whether the following are associated with RIC and undetectable viral load (UVL): (1) arrest history overall and by charge; (2) mental health diagnosis overall and by category; and (3) interaction effects between arrest history, mental health diagnosis, and SUD. Our findings may be relevant for discharge planning and community reentry for justice-involved PLWH with a mental health diagnosis.
METHODS
Sample and Study Design
We performed a retrospective cohort study of PLWH ≥13 years of age residing in Marion County during 2018. We used archived HIV surveillance data from the Centers for Disease Control and Prevention's Enhanced HIV/AIDS Reporting System (eHARS). Demographics, HIV diagnosis date, and HIV laboratory dates and results are captured within eHARS. Of 5730 PLWH in eHARS at any point during 2018, 5283 (92%) were present during each of the 4 quarters (“continuously in eHARS”). The remaining 8% were not consistently present for 1 or more of the following reasons: (1) newly diagnosed, (2) in- or out-migration, or (3) death (see Results section).
Person-level data from the 2018 eHARS cohort were linked to arrest records from the Indianapolis Metropolitan Police Department and clinical data from the Indiana Network for Patient Care (INPC) for calendar years 2000–2018. INPC is one of the largest, longest-operating, and best-studied health information exchanges in the United States.29–31 Through a collaborative effort among all major hospital systems, INPC captures statewide encounter data to serve clinical, public health, and research needs. For validation purposes, we supplemented INPC data with raw electronic health record data from the 2 largest hospital systems in Marion County.
Data were stored and analyzed on a password-protected and encrypted server behind the university firewall. Only the core research team had access to identifiers, which were used solely to link records between the sources. The study was reviewed and approved by Indiana University's Institutional Review Board and Marion County Public Health Department's Research Review Committee.
Study Procedures
Record linkage was performed using individual identifiers, including first/middle/last name, gender, month/day/year of birth, and social security number. Twenty-four deterministic algorithms employed a conservative approach by matching exact combinations of identifier subsets. We then used RecMatch software and various combinations of blocking/matching schemes with 24 probabilistic algorithms to identify additional matches based on linkage score threshold.32,33 True matches from the remaining records were determined by manual review. Matched pairs were “daisy-chained” to identify an aggregation of records representing an individual, and each aggregation of records was assigned a unique identifier. In rare cases where demographic or clinical data elements differed between linked records for the same unique individual records, we used the most recent data elements.
Measures
Demographic characteristics, including age, gender (sex at birth), and race/ethnicity, originated from eHARS. Arrest history was defined as any 2010–2017 arrest, and categorized as violent, drug-related, prostitution, intoxication, and felony (any).
Three clinical measures (mental health diagnosis, SUD, and health care utilization) were assessed by ICD-9 or ICD-10 diagnosis codes during ≥1 encounters during 2010–2017. We chose a sufficient period to offset the possibility of infrequent care utilization and inconsistent coding practices. We defined having a mental health diagnosis as ≥1 encounters with a mental health ICD code. Mental health diagnosis was assessed overall and categorized as mood, anxiety, psychosis, attention deficit, and personality disorders. SUD was assessed overall and by substance, including alcohol, opioid, and nonopioid drug misuse. Health care utilization was defined as whether individuals had ≥1 clinical encounters and was categorized as inpatient, outpatient, routine, and emergency department (ED). Routine visits were defined using diagnosis codes consistent with annual well visits.
Outcomes of interest included LTC, RIC, and UVL. LTC was defined as receiving a HIV-related clinical encounter within 30 days of diagnosis.34 RIC was defined as ≥2 CD4 or viral load tests performed ≥90 days apart during 2018.34 UVL was defined as any viral load value of <50 copies per milliliter in 2018.34
Analysis
Descriptive analyses were performed overall, and by history of arrest and mental health diagnosis. We performed Bonferroni-corrected univariable analyses of descriptive and outcome measures using independent samples t tests. Multivariable regression analysis was used to evaluate main and interaction effects of 2010–2017 arrest and mental health diagnosis on odds of 2018 RIC and UVL. We performed marginal effects analysis to calculate predicted probabilities of RIC and UVL with and without an arrest and/or mental health diagnosis. Further analysis of LTC was omitted because the study period bridged a 2015 move in the goal from ≤90 to ≤30 days.22 Individuals with missing data were excluded from regression analyses, as were variables demonstrating collinearity. Our final model included arrest history and mental health diagnosis for the subset continuously in eHARS, while controlling for age, race, gender, and history of SUD (n = 5140). To prevent bias that might arise from missing data, descriptive and regression analyses were primarily restricted to PLWH who were continuously in eHARS during 2018.
We conducted post hoc analyses to explore counterintuitive findings of apparent protective associations with HIV care outcomes. Outcomes were stratified by outpatient care utilization, which was added to our final regression model.
All analyses were performed using Stata/MP 14.1 (College Station, TX). P values <0.05 were considered statistically significant.
RESULTS
There were 5730 PLWH ≥13 years old residing in Marion County in 2018. Of 447 not continuously in eHARS, 218 were newly diagnosed, 58 died, and 260 either in- or out-migrated during ≥1quarters (not mutually exclusive categories). Those continuously in eHARS, versus those who were not, were older (mean age 45 vs 38 years, P < 0.05) and more likely to have any clinical encounter (88% vs 60%, P < 0.05).
Those continuously in eHARS were predominately male (80%) and disproportionately black (50% versus 29% in Marion County)35 (Table 1). Mean age was 44.8 ± 12.7 years, with less than 6% <18 or >64. Nine of 10 (88%) had ≥1 clinical encounters, but only 34% had a routine visit. Two-thirds (68%) had ≥1 ED visits, and 43% had ≥1 inpatient stays.
TABLE 1.
Characteristics of PLWH in Marion County, IN, in 2018: Overall and by 2010–2017 Arrest History and Mental Health Diagnosis*
| Variable | All PLWH | Arrest History | Mental Health Diagnosis | ||||
| (n = 5283) | No (n = 4009) | Yes (n = 1274) | P | No (n = 3434) | Yes (n = 1849) | P | |
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |||
| Age (yrs) | <0.05 | 0.6 | |||||
| 13–17 | 22 (0.4) | 20 (0.5) | 2 (0.2) | 16 (0.5) | 6 (0.3) | ||
| 18–24 | 230 (4.4) | 140 (3.5) | 90 (7.1) | 131 (3.8) | 99 (5.4) | ||
| 25–34 | 1083 (20.5) | 662 (16.5) | 421 (33.0) | 715 (20.8) | 368 (19.9) | ||
| 35–44 | 1126 (21.3) | 829 (20.7) | 297 (23.3) | 740 (21.5) | 386 (20.9) | ||
| 45–54 | 1525 (28.9) | 1235 (30.8) | 290 (22.8) | 967 (28.2) | 558 (30.2) | ||
| 55–64 | 1015 (19.2) | 870 (21.7) | 145 (11.4) | 663 (19.3) | 352 (19.0) | ||
| 65+ | 282 (5.3) | 253 (6.3) | 29 (2.3) | 202 (5.9) | 80 (4.3) | ||
| Gender | >0.9 | <0.05 | |||||
| Male | 4224 (80.0) | 3185 (79.4) | 1039 (81.6) | 2835 (82.6) | 1389 (75.1) | ||
| Female | 1059 (20.0) | 824 (20.6) | 235 (18.4) | 599 (17.4) | 460 (24.9) | ||
| Race/ethnicity | <0.05 | <0.05 | |||||
| Black | 2566 (49.9) | 1723 (44.5) | 843 (66.7) | 1690 (51.1) | 876 (47.7) | ||
| Hispanic | 455 (8.9) | 375 (9.7) | 80 (6.3) | 343 (10.4) | 112 (6.1) | ||
| White | 1948 (37.9) | 1651 (42.6) | 297 (23.5) | 1162 (35.2) | 786 (42.8) | ||
| Other | 171 (3.3) | 127 (3.3) | 44 (3.5) | 110 (3.3) | 61 (3.3) | ||
| Mental health Dx | 1849 (35.0) | 1176 (29.3) | 673 (52.8) | <0.05 | NA | NA | |
| Mood | 1446 (27.4) | 906 (22.6) | 540 (42.4) | <0.05 | NA | 1446 (78.2) | |
| Anxiety | 896 (17.0) | 569 (14.2) | 327 (25.7) | <0.05 | NA | 896 (48.5) | |
| Psychosis | 415 (7.9) | 194 (4.8) | 221 (17.3) | <0.05 | NA | 415 (22.4) | |
| Attention deficit | 113 (2.1) | 59 (1.5) | 54 (4.2) | <0.05 | NA | 113 (6.1) | |
| Personality | 114 (2.2) | 45 (1.1) | 69 (5.4) | <0.05 | NA | 114 (6.2) | |
| Substance use | 983 (18.6) | 447 (11.1) | 536 (42.1) | <0.05 | 261 (7.6) | 722 (39.0) | <0.05 |
| Alcohol | 489 (9.3) | 208 (5.2) | 281 (22.1) | <0.05 | 123 (3.6) | 366 (19.8) | <0.05 |
| Opioid | 128 (2.4) | 54 (1.3) | 74 (5.8) | <0.05 | 19 (0.6) | 109 (5.9) | <0.05 |
| Other/unspec | 710 (13.4) | 306 (7.6) | 404 (31.7) | <0.05 | 157 (4.6) | 553 (29.9) | <0.05 |
| Clinical encounter | 4659 (88.2) | 3396 (84.7) | 1263 (99.1) | <0.05 | 2810 (81.8) | 1849 (100) | <0.05 |
| Outpatient | 4560 (86.3) | 3325 (82.9) | 1235 (96.9) | <0.05 | 2720 (79.2) | 1840 (99.5) | <0.05 |
| Routine visit | 1782 (33.7) | 1326 (33.1) | 456 (35.8) | >0.9 | 875 (25.5) | 907 (49.1) | <0.05 |
| Emergency department | 3613 (68.4) | 2419 (60.3) | 1194 (93.7) | <0.05 | 1948 (56.7) | 1665 (90.0) | <0.05 |
| Inpatient | 2243 (42.5) | 1526 (38.1) | 717 (56.3) | <0.05 | 1053 (30.7) | 1190 (64.4) | <0.05 |
| Arrest history | 2082 (39.4) | NA | NA | 1092 (31.8) | 990 (53.5) | <0.05 | |
| Violent | 304 (5.8) | NA | 304 (23.9) | 107 (3.1) | 197 (10.7) | <0.05 | |
| Prostitution | 48 (0.9) | NA | 48 (3.8) | 12 (0.3) | 36 (1.9) | <0.05 | |
| Drug related | 307 (5.8) | NA | 307 (24.1) | 134 (3.9) | 173 (9.4) | <0.05 | |
| Intoxication | 274 (5.2) | NA | 274 (21.5) | 111 (3.2) | 163 (8.8) | <0.05 | |
| Felony | 650 (12.3) | NA | 650 (51.0) | 279 (8.1) | 371 (20.1) | <0.05 | |
Bonferroni-corrected P values. Bolded P-values are significant at P < 0.05 or less.
Includes only PLWH with an eHARS record in Marion County during all 4 quarters of 2018.
Arrest History
One-fourth (24%) of PLWH were arrested during 2010–2017 (Table 1). Among these, half (51%) had ≥1 felony offenses, 24% had ≥1 violent offenses, 24% had ≥1 drug offenses, and 22% had ≥1 intoxication offenses. Four percent were charged with prostitution.
Mental Health Diagnosis
One-third (35%) of PLWH had a mental health diagnosis and two-thirds (64%) among those had ≥1 inpatient hospitalizations (Table 1). The most prevalent mental health diagnoses were mood (27%) and anxiety disorders (17%). More than half (53%) of those with an arrest had a mental health diagnosis (P < 0.05) and those with a mental health diagnosis were more likely to have been arrested for each arrest category, when compared with PLWH without a mental health diagnosis (all P < 0.05).
Substance Use Disorder
One in 5 PLWH (19%) had a SUD diagnosis. Nonopioid drug misuse (13%) was more prevalent than alcohol (9%) and opioid misuse (2%). PLWH and SUD were more likely to have an arrest (42% vs 11%, P < 0.05) or mental health diagnosis (39% vs 8%, P < 0.05; Table 1).
Health care Utilization
Among PLWH, 88% had ≥1 clinical encounters during 2010–2017. Outpatient visits accounted for most utilization, with 86% having ≥1 outpatient encounters (Table 1). Sixty-eight percent of PLWH had ≥1 ED visit; 43% had ≥1 inpatient hospitalizations, and 34% had ≥1 routine visits. Those with an arrest were more likely than those without to have any clinical encounter (99% vs 85%, P < 0.05). In fact, they were more likely than those without an arrest to have received inpatient, outpatient, or ED care (P < 0.05), although arrest history was unrelated to routine care. PLWH and a mental health diagnosis were more likely than those without a mental health diagnosis to have any type of clinical encounter (100% vs 82%, P < 0.05).
HIV Care Continuum
Individuals with an arrest were less likely than those without an arrest to have LTC regardless of whether they were diagnosed during (42% vs 63%, P = 0.02) or before (38% vs 43%, P = 0.012; Table 2) 2018. LTC did not differ by receipt of a mental health diagnosis regardless of when HIV diagnosis was received.
TABLE 2.
HIV Care Continuum Among PLWH in Marion County, IN, in 2018: Overall and by 2010–2017 Arrest History and Mental Health Diagnosis
| Independent Variable | All PLWH | Arrest History | Mental Health Diagnosis | ||||
| No | Yes | P | No | Yes | P | ||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |||
| Linked to care within 30 d | |||||||
| 2018 diagnosis (n = 215) | 122 (56.7) | 97 (62.6) | 25 (41.7) | 0.02 | 94 (55.0) | 28 (63.6) | >0.9 |
| Pre-2018 diagnosis* (n = 5245) | 2187 (41.7) | 1705 (42.8) | 482 (38.1) | 0.012 | 1413 (41.5) | 774 (42.1) | >0.9 |
| Retention in care* (n = 5283) | 2179 (41.2) | 1555 (38.8) | 624 (49.0) | 0.004 | 1216 (35.4) | 963 (52.1) | 0.004 |
| Undetectable viral load* (n = 5283) | 2296 (43.5) | 1743 (43.5) | 553 (43.4) | >0.9 | 1343 (39.1) | 953 (51.5) | 0.004 |
Bonferroni-corrected P values. Bolded P-values are significant at P < 0.05 or less.
Includes only PLWH with an eHARS record in Marion County during all 4 quarters of 2018.
RIC was improved among PLWH and an arrest history versus those with no arrest (49% vs 39%, P = 0.004), although an arrest had no significant association with UVL. Both RIC and UVL improved among those with versus without a mental health diagnosis (52% vs 35% RIC, P = 0.004; 52% vs 39% UVL, P = 0.004).
Multivariable Regression Analysis
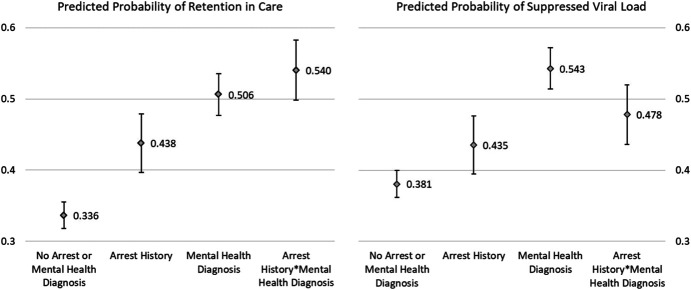
Of 5283 PLWH in our cohort, 143 were excluded from regression analyses because of missing values. Imputation was not performed because this accounted for <3% of the cohort, minimizing the risk of bias. PLWH with an arrest history or mental health diagnosis, versus those without, experienced increased odds of RIC and UVL (Table 3). Specifically, those with an arrest had 1.54 times the odds of those without an arrest to have RIC (95% CI: 1.27 to 1.86) and 1.26 times the odds of an UVL (95% CI: 1.04 to 1.52). There was significant interaction between arrest and mental health diagnosis. When either predictor was present, the protective effect on RIC was enhanced, increasing the predicted probability (PP) of RIC to 54% (Fig. 1). This interaction reduced the protective effect on UVL such that a mental health diagnosis without an arrest history led to the highest PP of UVL (54%; Fig. 1).
TABLE 3.
Adjusted Odds of Retention in Care and Undetectable Viral Load by Arrest History, Mental Health Diagnosis, and Outpatient Care Utilization for People Living With HIV in Marion County, IN, in 2018 (n = 5140)
| Outcome: Odds of Retention in Care | |||||
| Model | Controlling for Outpatient Care Utilization | ||||
| No | Yes | ||||
| aOR | 95% CI | aOR | 95% CI | ||
| Arrest history | 1.54 | 1.27 to 1.86 | 1.18 | 0.97 | 1.44 |
| Mental health diagnosis | 2.02 | 1.75 to 2.34 | 1.05 | 0.89 | 1.23 |
| Arrest history*mental health diagnosis | 0.75 | 0.57 to 0.97 | 1.05 | 0.80 | 1.38 |
| Outpatient care visits = 1–9 | — | 5.14 | 3.78 | 6.98 | |
| Outpatient care visits = 10–24 | — | — | 8.10 | 5.96 | 11.01 |
| Outpatient care visits = 25–49 | — | — | 13.58 | 10.01 | 18.43 |
| Outpatient care visits = 50–99 | — | — | 17.07 | 12.37 | 23.54 |
| Outpatient care visits = 100+ | — | — | 18.75 | 12.86 | 27.34 |
| Outcome: Odds of Undetectable Viral Load | |||||
| Model | Controlling for Outpatient Care Utilization | ||||
| No | Yes | ||||
| aOR | 95% CI | aOR | 95% CI | ||
| Arrest history | 1.26 | 1.04 to 1.52 | 0.91 | 0.74 | 1.11 |
| Mental health diagnosis | 1.95 | 1.68 to 2.25 | 0.90 | 0.77 | 1.07 |
| Arrest history*mental health diagnosis | 0.61 | 0.47 to 0.80 | 0.92 | 0.69 | 1.21 |
| Outpatient care visits = 1–9 | — | — | 5.55 | 4.12 | 7.47 |
| Outpatient care visits = 10–24 | — | — | 10.73 | 7.97 | 14.45 |
| Outpatient care visits = 25–49 | — | — | 16.74 | 12.43 | 22.55 |
| Outpatient care visits = 50–99 | — | — | 21.91 | 15.97 | 30.04 |
| Outpatient care visits = 100+ | — | — | 28.55 | 19.58 | 41.63 |
Exponentiated coefficients; multivariable logistic regression models adjusted for age, race/ethnicity, sex, and history of substance use; 143 observations were deleted because of missing values.
FIGURE 1.
Adjusted predictions of retention in care and suppressed viral load among people living with HIV in Marion County, IN, in 2018: By arrest history, mental health diagnosis, and arrest*mental health diagnosis. Average marginal effects, with 95% CIs, adjusted for age, race/ethnicity, gender, and substance use diagnosis.
Post Hoc Analysis
In post hoc analyses, when controlling for health care utilization, neither arrest nor mental health diagnosis was a significant predictor of RIC or UVL. We included only outpatient care utilization history in the final model because it was strongly associated (P < 0.05) with RIC and UVL with a clear dose response (Table 3). There were no clear patterns of association between ED or inpatient utilization and RIC or UVL (see Supplemental Digital Content 1, http://links.lww.com/QAI/C117). We stratified outcomes by annualized outpatient visits during 2010–2017. Categories were based on meaningful thresholds of <25 (∼3/year), 25–50 (3–6/year), or >50 (>6/year) visits. Minimal variability existed within strata, with 2018 RIC and UVL increasing as 2010–2017 outpatient visits increased. Importantly, we found that arrest (adjusted odds ratio [aOR]: 2.04) and mental health diagnosis (aOR: 1.71) provided protective effects for RIC only among those with the lowest utilization history (Table 4).
TABLE 4.
Adjusted Odds of Retention in Care and Undetectable Viral Load by Arrest History and Mental Health Diagnosis—Stratified by Outpatient Care Utilization—For People Living With HIV in Marion County, IN, in 2018 (n = 5140)
| Outcome: Odds of Retention in Care | |||||||||
| Model | Outpatient Care Utilization during 2010–2017 | ||||||||
| <25 Visits (Average ≈3 per year) | 25-50 Visits (Average 3–6 per year) | >50 Visits (Average >6 per year) | |||||||
| aOR | 95% CI | P | aOR | 95% CI | P | aOR | 95% CI | P | |
| Arrest history | 2.04 | 1.44 to 2.88 | <0.001 | 1.24 | 0.86 to 1.80 | 0.25 | 0.94 | 0.68 to 1.29 | 0.70 |
| Mental health diagnosis | 1.71 | 1.10 to 2.66 | 0.02 | 1.26 | 0.90 to 1.77 | 0.17 | 0.99 | 0.81 to 1.22 | 0.96 |
| Arrest history*mental health diagnosis | 0.72 | 0.34 to 1.54 | 0.40 | 0.93 | 0.53 to 1.63 | 0.81 | 1.24 | 0.84 to 1.83 | 0.28 |
| Outcome: Odds of Undetectable Viral Load | |||||||||
| Model | Outpatient Care Utilization during 2010–2017 | ||||||||
| <25 Visits (Average ≈3 per year) | 25-50 Visits (Average 3–6 per year) | >50 Visits (Average >6 per year) | |||||||
| aOR | 95% CI | P | aOR | 95% CI | P | aOR | 95% CI | P | |
| Arrest history | 1.22 | 0.86 to 1.75 | 0.27 | 0.76 | 0.52 to 1.10 | 0.15 | 0.95 | 0.69 to 1.32 | 0.77 |
| Mental health diagnosis | 1.24 | 0.79 to 1.93 | 0.35 | 0.85 | 0.61 to 1.19 | 0.35 | 1.04 | 0.85 to 1.28 | 0.68 |
| Arrest history*mental health diagnosis | 0.70 | 0.31 to 1.61 | 0.41 | 1.16 | 0.66 to 2.04 | 0.62 | 0.81 | 0.55 to 1.20 | 0.30 |
Exponentiated coefficients; multivariable logistic regression models adjusted for age, race/ethnicity, sex, and history of substance use; 143 observations were deleted because of missing values.
DISCUSSION
In this large retrospective cohort of PLWH, initial analyses identified patterns of HIV care outcomes among individuals with an arrest history and/or mental health diagnosis that diverged from previous studies. We found that (1) PLWH with an arrest in the preceding 8 years were less likely to have LTC within 30 days but to have increased odds of RIC and UVL and (2) mental health diagnosis was associated with increased odds of RIC and UVL, but its protective effect on UVL was reduced in the presence of an arrest history. Post hoc tests indicate that outpatient care utilization mediated these effects, although arrest and mental health diagnosis both increased odds of RIC among PLWH with low outpatient utilization.
Although few studies have evaluated the full HIV care continuum among PLWH and an arrest history, release from incarceration has been associated with an increased risk of falling out of care and losing viral suppression.8–11 Within the justice system, PLWH have reported treatment interruptions during intake and release, lack of HIV-specific staffing in institutional care settings, and long delays in prescription refills.11 By contrast, we found that PLWH with an arrest history and high outpatient care utilization were more likely to have RIC and an UVL, particularly if they had a mental health diagnosis.
Previous studies noted an association between mental health diagnosis and inadequate viral suppression,16,19 lower ART adherence,13,14 and increased mortality,18,20 although Yehia et al19 found no difference in RIC between those with or without a mental health diagnosis. We found that PLWH with a history of mental health diagnosis and higher outpatient care utilization were more likely to have RIC and UVL, although an arrest reduced the protective effect for UVL. We found that those diagnosed with mood or anxiety disorders were more likely to achieve RIC and UVL. In the Yehia et al19 study, people diagnosed with depression or anxiety were less likely to achieve viral suppression compared with those with no mental health diagnosis. Like Yehia et al,19 we found no significant difference among those with psychoses.
We do not know with certainty why a mental health diagnosis led to improved HIV outcomes among those with a history of outpatient care utilization, although depression treatment has been shown to increase the likelihood of ART adherence36 and viral load suppression.37 However, our initial findings were strong enough that we considered health care utilization as a mediator of this effect. We considered that because anxiety and depression are often embedded in outpatient medical systems, engagement in outpatient care may be associated with engagement and retention in HIV care. Indeed, our post hoc analyses did indicate outpatient utilization as a driver of positive health outcomes among PLWH and an arrest history or mental health diagnosis, demonstrating a clear dose response.
Another explanation could be that PLWH and a mental health diagnosis are diverted from incarceration directly to a health care facility. This was a consideration because, during 2011–2015, the Marion County criminal justice system implemented 3 distinct mental health programs for offenders, collectively referred to as Behavioral Court.38 Evidence indicates that these programs reduced emergency medical services utilization in the year following program participation,39 so it was reasonable to speculate that PLWH and incarcerated during 2010–2017 might have higher odds of RIC and UVL. In fact, RIC did increase among those in our cohort with an arrest during this period, particularly if they had a mental health diagnosis. However, an arrest weakened the protective effect of a mental health diagnosis on UVL. A larger study of behavioral health courts evaluated data from Marion County and 3 other jurisdictions, finding a significant increase in medication compliance and use of mental health services, as well as decreased risk of future arrest.40 Yet another study reported that only those behavioral court programs offering specific features such as access to housing, case management, and vocational services were effective,41 highlighting the need for further research into these interactions.
There were several limitations in this study. First, we likely did not identify all mental health and drug-related diagnoses for the following reasons: (1) individuals may not have presented for mental health care because of stigma, lack of mental health care access, or other reasons; (2) individuals may have presented for care at a location not reporting to the INPC; (3) providers may not have coded these diagnoses, particularly when mental health services were not offered; and (4) there is no consistent systematic screening for depression across medical systems, so undiagnosed illness is missed. Nevertheless, the INPC has good clinical data capture in Marion County, particularly for inpatient and ED care29–31; thus, we would expect to capture at least severe mental illness. Second, our findings represent a single large metropolitan area such as those in which the majority of PLWH reside in the United States.42 Although each jurisdiction may differ slightly in approaches to incarceration and mental illness, there is little reason to believe that differential associations and interactions between arrest and mental health diagnosis history, with regard to HIV outcomes, should vary regionally or between urban centers. Nevertheless, because of our strong partnerships with the Marion County Public Health Department and multiple Marion County justice agencies, we are aware of interventions our partners have initiated or in which they participated (eg, timing of Ryan White Part A mental health services expansion). This knowledge helped inform the period we selected for analysis, prompting us to use a 1-year period to minimize temporal effects. That said, we did not control for time between arrest or mental health diagnosis and the outcomes of interest, aside from confining that window to 2010–2017. Individuals met these definitions whether they experienced an event in 2010, in 2017, or at any time in between. That timing may be important. Another limitation we faced was legislatively sealed juvenile court records. We had to obtain Indiana Supreme Court permission to receive juvenile records and, even then, received limited identifiers. We matched juvenile records based on full name, mo/yr of birth, and last 4 of the Social Security number. Considering this reduced data availability, it is possible that linkages might be incorrect for juveniles; however, participants with a juvenile court record accounted for only 2 of the individuals in our cohort. Another limitation is that our UVL measure does not capture improvements in viral load that do not reach the point of UVL, meaning that PLWH with significant improvements not meeting our benchmark were not captured. Finally, we could not measure some key confounding factors such as other interactions with the justice system and personal factors that might have influenced care seeking behavior for mental health, SUD, ART adherence, or other HIV-related care. These and other factors may more generally reflect life chaos or stress, or there may be factors such as income, medication prices, burden of travel to the clinic, and safe stable housing that affect outcomes.
A strength of this study is the partnership with Marion County Public Health Department, which allowed us to clearly define our cohort and to obtain high-quality HIV outcomes data. Partnerships that allow for data sharing of surveillance, clinical, and justice data are possible to replicate and offer 1 approach to population surveillance and responding to and evaluating findings such as in this study.
The story behind mental health and arrest history among PLWH is complex. Although each is associated with HIV outcomes and they often co-occur, rarely are the 2 considered concurrently in research. It is of public health significance to study the interaction between these conditions among PLWH so that appropriate and effective action can be taken to reduce viral load and resistance and reduce the spread of HIV. Because as many as half of PLWH are thought to be have a mental health diagnosis,22 a holistic approach to health care is critical. Integration of mental health care into the primary care setting creates a “no wrong door” approach, simplifying health care navigation and increasing access to care—especially for vulnerable populations.43 Integrated care also helps to destigmatize mental illness.43 As previously noted, mental health treatment—particularly for depression—has been shown to improve HIV ART compliance and viral load suppression.36,37 In addition, mental health care utilization has been shown to decrease criminal justice involvement,44 further improving the likelihood of positive HIV outcomes. For individuals who do become involved in the criminal justice system, access to a Behavioral Court program can improve linkage to care among those living with a mental health diagnosis rather than detaining them in jail and possibly disrupting their HIV and/or mental health care.
Our study also has implications for population health by helping develop existing large data sets to measure disparities in HIV care among PLWH, with a particular focus on vulnerable populations who may neither present for recurring care nor participate in clinical trials and other prospective studies. Cross-sector collaborative data sharing and research will allow us to better recognize barriers and to intervene to achieve optimal care outcomes among PLWH.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the contributions from Regenstrief Institute and our other data-sharing partners, including the Indiana Network for Patient Care, Indianapolis Metropolitan Police Department, and the Marion County Public Health Department. The authors acknowledge our team member, Maguette Diop, from Marion County Public Health Department for her contributions.
Footnotes
Supported by grants from the National Institute of Health (R01AI114435; R01HD098013), the Agency for Healthcare Research and Quality (R01HS023318; R01HS024296), and the US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Research Program (R40MC08721).
The authors have no funding or conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
Contributor Information
Tammie L. Nelson, Email: talnelso@iu.edu.
Matthew C. Aalsma, Email: maalsma@iu.edu.
Marc B. Rosenman, Email: mrosenman@luriechildrens.org.
Sami Gharbi, Email: sagharbi@iu.edu.
J. Dennis Fortenberry, Email: jfortenb@iu.edu.
REFERENCES
- 1.Lamb HR, Bachrach LL. Some perspectives on deinstitutionalization. Psychiatr Serv. 2001;52:1039–1045. [DOI] [PubMed] [Google Scholar]
- 2.Lamb HR, Weinberger LE. The shift of psychiatric inpatient care from hospitals to jails and prisons. J Am Acad Psychiatry Law. 2005;33:529–534. [PubMed] [Google Scholar]
- 3.Clifford K. Mental health crisis and interventions and the politics of police use of deadly force. In: Chappell D, ed. Policing and the Mentally Ill: International Perspectives. Boca Raton, FL: CRC Press; 2013:171–195. [Google Scholar]
- 4.Torrey EF, Kennard AD, Eslinger D, et al. More Mentally IL Persons Are in Jails and Prisons than Hospitals: A Survey of the States. Washington, DC: U.S. Department of Justice; 2010. Available at: https://www.ojp.gov/ncjrs/virtual-library/abstracts/more-mentally-ill-persons-are-jails-and-prisons-hospitals-survey. Accessed August 13, 2018. [Google Scholar]
- 5.Haney C. Prison effects in the era of mass incarceration. Prison J. 2012. Available at: https://journals.sagepub.com/doi/10.1177/0032885512448604. Accessed August 7, 2018.
- 6.Bronson J, Berzofsky M. Indicators of Mental Health Problems Reported by Prisoners and Jail Inmates, 2011–12. Bureau of Justice Statistics Special Report, NCJ; 2017;250612.
- 7.Baillargeon J, Ducate S, Pulvino J, et al. The association of psychiatric disorders and HIV infection in the correctional setting. Ann Epidemiol. 2003;13:606–612. [DOI] [PubMed] [Google Scholar]
- 8.Spaulding AC, Messina LC, Kim BI, et al. Planning for success predicts virus suppressed: results of a non-controlled, observational study of factors associated with viral suppression among HIV-positive persons following jail release. AIDS Behav. 2013;17:S203–S211. [DOI] [PubMed] [Google Scholar]
- 9.Clements-Nolle K, Marx R, Pendo M, et al. Highly active antiretroviral therapy use and HIV transmission risk behaviors among individuals who are HIV infected and were recently released from jail. Am J Public Health. 2008;98:661–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loeliger KB, Meyer JP, Desai MM, et al. Retention in HIV care during the 3 years following release from incarceration: a cohort study. Plos Med. 2018;15:e1002667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Small W, Wood E, Betteridge G, et al. The impact of incarceration upon adherence to HIV treatment among HIV-positive injection drug users: a qualitative study. AIDS Care. 2009;21:708–714. [DOI] [PubMed] [Google Scholar]
- 12.Cournos F, McKinnon K, Sullivan G. Schizophrenia and comorbid human immunodeficiency virus or hepatitis C virus. J Clin Psychiatry. 2005;66(suppl 6):27–33. [PubMed] [Google Scholar]
- 13.Angelino AF, Treisman GJ. Issues in co-morbid severe mental illnesses in HIV infected individuals. Int Rev Psychiatry. 2008;20:95–101. [DOI] [PubMed] [Google Scholar]
- 14.Mugavero M, Ostermann J, Whetten K, et al. Barriers to antiretroviral adherence: the importance of depression, abuse, and other traumatic events. AIDS Patient Care STDs. 2006;20:418–428. [DOI] [PubMed] [Google Scholar]
- 15.Kelly JA, Murphy DA, Bahr GR, et al. Factors associated with severity of depression and high-risk sexual behavior among persons diagnosed with human immunodeficiency virus (HIV) infection. Health Psychol. 1993;12:215–219. [DOI] [PubMed] [Google Scholar]
- 16.Ironson G, O'Cleirigh C, Fletcher MA, et al. Psychosocial factors predict CD4 and viral load change in men and women with human immunodeficiency virus in the era of highly active antiretroviral treatment. Psychosom Med. 2005;67:1013–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ickovics JR, Hamburger ME, Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285:1466–1474. [DOI] [PubMed] [Google Scholar]
- 18.Mugavero MJ, Pence BW, Whetten K, et al. Predictors of AIDS-related morbidity and mortality in a southern U.S. Cohort. AIDS Patient Care STDs. 2007;21:681–690. [DOI] [PubMed] [Google Scholar]
- 19.Yehia BR, Stephens-Shield AJ, Momplaisir F, et al. Health outcomes of HIV-infected people with mental illness. AIDS Behav. 2015;19:1491–1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lima VD, Geller J, Bangsberg DR, et al. The effect of adherence on the association between depressive symptoms and mortality among HIV-infected individuals first initiating HAART. AIDS. 2007;21:1175–1183. [DOI] [PubMed] [Google Scholar]
- 21.Nurutdinova D, Chrusciel T, Zeringue A, et al. Mental health disorders and the risk of AIDS-defining illness and death in HIV-infected veterans. AIDS. 2012;26:229–234. [DOI] [PubMed] [Google Scholar]
- 22.White House Office of National AIDS Policy . National HIV/AIDS Strategy for the United States; 2010. Available at: https://www.hiv.gov/federal-response/national-hiv-aids-strategy. Accessed October 20, 2021. [Google Scholar]
- 23.Hartzler B, Dombrowski JC, Crane HM, et al. Prevalence and predictors of substance use disorders among HIV care enrollees in the United States. AIDS Behav. 2017;21:1138–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaswa R, De Villiers M. Prevalence of substance use amongst people living with human immunodeficiency virus who attend primary healthcare services in Mthatha, South Africa. South Afr Fam Pract. 2020;62:e1–e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chaudri NA. Adherence to long-term therapies: evidence for action. Ann Saudi Med. 2004;24:221–222. [Google Scholar]
- 26.Health Resources and Services Administration . Guide for HIV/AIDS Clinical Care – 2014 Edition. U.S. Department of Health and Human Services; 2014. Available at: https://ryanwhite.hrsa.gov/sites/default/files/ryanwhite/grants/2014-guide.pdf. Accessed July 12, 2018. [Google Scholar]
- 27.Idrisov B, Lunze K, Cheng DM, et al. Role of substance use in HIV care cascade outcomes among people who inject drugs in Russia. Addict Sci Clin Pract. 2017;12:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loeliger KB, Altice FL, Ciarleglio MM, et al. All-cause mortality among people with HIV released from an integrated system of jails and prisons in Connecticut, USA, 2007–14: a retrospective observational cohort study. Lancet HIV. 2018;5:e617–e628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McDonald CJ, Overhage JM, Barnes M, et al. The Indiana Network for patient care: a working local health information infrastructure. Health Aff. 2005;24:1214–1220. [DOI] [PubMed] [Google Scholar]
- 30.McDonald CJ, Overhage JM, Tierney WM, et al. The Regenstrief medical record system: a quarter century experience. Int J Med Inform. 1999;54:225–253. [DOI] [PubMed] [Google Scholar]
- 31.Regenstrief Institute. How we bring the data to you: data sources - Indiana Network for patient care. Availabe at: https://www.regenstrief.org/rds/data/. Accessed July 17, 2023.
- 32.Grannis S, Egg J, Ribeka N. RecMatch: Probabilistic Patient Record Matching (Version 1.0) [Software]. Indianapolis, IN: Regenstrief Institute; 2008. Available at: http://svn.openmrs.org/openmrs-modules/patientmatching/. [Google Scholar]
- 33.Dusetzina SB, Tyree S, Meyer A-M, et al. Linking Data for Health Services Research: A Framework and Instructional Guide. Agency for Healthcare Research and Quality; 2014. (Prepared by the University of North Carolina at Chapel Hill under Contract No. 290-2010-000141). [PubMed] [Google Scholar]
- 34.Kay ES, Batey DS, Mugavero MJ. The HIV treatment cascade and care continuum: updates, goals, and recommendations for the future. AIDS Res Ther. 2016;13:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.U.S. Census Bureau . Data from: 2018 American Community Survey 1-year Estimates: Table S0201 Selected Population Profile in the United States. Suitland-Silver Hill, MD: U.S. Census Bureau; 2018. [Google Scholar]
- 36.Springer SA, Dushaj A, Azar MM. The impact of DSM-IV mental disorders on adherence to combination antiretroviral therapy among adult persons living with HIV/AIDS: a systematic review. AIDS Behav. 2012;16:2119–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tsai AC, Weiser SD, Petersen ML, et al. A marginal structural model to estimate the causal effect of antidepressant medication treatment on viral suppression among homeless and marginally housed persons with HIV. Arch Gen Psychiatry. 2010;67:1282–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ray B, Sapp D, Thelin R. Behavioral health court impacts on mental health in the Marion County criminal justice system (Update to Previous Study Published in 2017, #16-C03). 2017. 17-C14; 2017. Available at: https://ppidb.iu.edu/Uploads/ProjectFiles/MentalHealthBrief_Final_040617.pdf. Accessed July 17, 2023. [Google Scholar]
- 39.Ray B, Bailey K, Huynh P, et al. Arrest and emergency medical services events among participants from one of the first mental health courts. Int J L Psychiatry. 2020;73:101644. [DOI] [PubMed] [Google Scholar]
- 40.Han W, Redlich AD. The impact of community treatment on recidivism among mental health court participants. Psychiatr Serv. 2016;67:384–390. [DOI] [PubMed] [Google Scholar]
- 41.Loong D, Bonato S, Barnsley J, et al. The effectiveness of mental health courts in reducing recidivism and police contact: a systematic review. Community Ment Health J. 2019;55:1073–1098. [DOI] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention Division of HIV/AIDS Prevention. HIV in the United States by geography. January 21, 2018. Updated January 11, 2018. Available at: https://www.cdc.gov/hiv/statistics/overview/geographicdistribution.html. Accessed January 21, 2018.
- 43.Kwarciany J. Why We Need Mental Health Care Integration. NAMI Blog. National Alliance on Mental Illness; 2022. Available at: https://www.nami.org/Blogs/NAMI-Blog/March-2022/Why-We-Need-Mental-Health-Care-Integration#:∼:The/Benefits/of/Integrated/Care=Integrated/care/also/helps/ensure,improve/outcomes/and/reduce/costs.Mental/health/integration/can/also,with/receiving/mental/health/care. Accessed July 17, 2023. [Google Scholar]
- 44.Jacome E. Policy Brief: How Better Access to Mental Health Care Can Reduce Crime. Stanford, CA: Stanford University; 2021. Available at: https://siepr.stanford.edu/publications/policy-brief/how-better-access-mental-health-care-can-reduce-crime#:∼:text=Within/two/years/of/losing,crime/and/criminal/justice/expenditures. Accessed July 17, 2023. [Google Scholar]