Women with intellectual and developmental disabilities enrolled in North Carolina Medicaid are less likely to be provided highly or moderately effective contraception.
Abstract
OBJECTIVE:
To compare contraceptive provision to women with and without intellectual and developmental disabilities enrolled in North Carolina Medicaid.
METHODS:
Our retrospective cohort study used 2019 North Carolina Medicaid claims to identify women aged 15–44 years with and without intellectual and developmental disabilities at risk for pregnancy who were continuously enrolled during 2019 or had Family Planning Medicaid with at least one claim. We calculated the proportion in each cohort who received 1) most or moderately effective contraception, 2) long-acting reversible contraception, 3) short-acting contraception, and 4) individual methods. We classified contraceptive receipt by procedure type and disaggregated across sociodemographic characteristics. Adjusting for age, race, ethnicity, and urban or rural setting, we constructed logistic regression models to estimate most or moderately effective contraceptive provision odds by intellectual and developmental disability status and by level or type of intellectual and developmental disability. We performed subanalyses to estimate co-occurrence of provision and menstrual disorders.
RESULTS:
Among 9,508 women with intellectual and developmental disabilities and 299,978 without, a significantly smaller proportion with intellectual and developmental disabilities received most or moderately effective contraception (30.1% vs 36.3%, P<.001). With the exception of injectable contraception, this trend was consistent across all measures and remained statistically significant after controlling for race, ethnicity, age, and urban or rural status (adjusted odds ratio 0.75, 95% CI 0.72–0.79; P<.001). Among those who received most or moderately effective contraception, a significantly greater proportion of women with intellectual and developmental disabilities had co-occurring menstrual disorders (31.3% vs 24.3%, P<.001).
CONCLUSION:
These findings suggest disparities in contraceptive provision and potential differences in clinical indication by intellectual and developmental disability status. Future studies should investigate reasons for and barriers to contraceptive use among women with intellectual and developmental disabilities.
Sexual and reproductive health needs of people with intellectual and developmental disabilities have historically been overlooked.1,2 People with intellectual and developmental disabilities face sexual and reproductive health barriers, including poor health care access, restricted decision-making ability, discrimination, and limited contraceptive knowledge.3–6 Contrary to misconceptions that people with intellectual and developmental disabilities are sexually inactive, young women with and without intellectual and developmental disabilities have similar age-specific fertility rates.7,8 Young people with mild or moderate intellectual disabilities are also more likely to engage in sex without precautions or contraception.9 Intellectual and developmental disability–related concerns exist around contraceptive use (eg, prescription adherence, consent); analysis of the 2012 Massachusetts All-Payer Claims Database identified provision disparities by intellectual and developmental disability status.10,11 However, contraceptive access varies across states as a result of differences in demographics, insurance legislation, and health care policy.12,13
Little is known about the contraceptive health care utilization patterns of people with intellectual and developmental disabilities in North Carolina, who constitute about 2.24% of the population.14 Existing studies use binary intellectual and developmental disability presence (ie, intellectual and developmental disabilities vs no intellectual and developmental disabilities); however, it remains poorly understood whether and how level and type of intellectual and developmental disabilities affect contraceptive receipt. Analyses should also consider racial, ethnic, and geographic differences along with intellectual and developmental disabilities, as these factors are understood to affect contraceptive use.15,16
To address these gaps, we analyzed 2019 North Carolina Medicaid claims data. Our objective was to characterize most or moderately effective contraceptive provision among women of reproductive age with intellectual and developmental disabilities. Specifically, we assessed service receipt differences by method and procedure type and explored the influence of sociodemographic factors. We hypothesized that women with intellectual and developmental disabilities would be less likely to receive contraception and that provision would vary by level and type of intellectual and developmental disability.
METHODS
We accessed North Carolina Medicaid claims data for the period of January 1, 2018, to December 31, 2019. This source contains individual-level medical, dental, and pharmacy claims data for about 2.18 million 2019 enrollees.17 Medicaid remains a predominant insurance payer for people with intellectual and developmental disabilities, capturing service data across a broad range of diagnoses, residential arrangements, and support needs.18 Therefore, this data set allows the establishment of baseline measures for contraceptive health care provision.
We selected the year 2019 for our retrospective cohort analysis because it was the most recent, complete data set unaffected by the coronavirus disease 2019 (COVID-19) pandemic. We based our approach on the U.S. Department of Health and Human Services (DHHS) Office of Population Affairs' Contraceptive Care–All Women methodology.19 This guidance has been formally adopted by the Centers for Medicare & Medicaid Services and endorsed by the National Quality Forum.20,21 Medicaid claims did not specify more detailed sexual orientation and gender identity data than binary designations of male and female. We therefore examined claims of enrollees identified as women in the data set and have used the term “women” throughout this article.
To identify eligible women and relevant contraceptive claims, we used International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) diagnosis and Procedure Coding System (ICD-10-PCS) codes, Current Procedural Terminology codes, Healthcare Common Procedure Coding System codes, and National Drug Codes. We referenced these codes in institutional, professional, and pharmacy claims files. All diagnoses on the claims were included.
Following DHHS Office of Population Affairs specifications, we included women aged 15–44 years who either were continuously enrolled throughout 2019 (ie, no more than one enrollment gap of up to 45 days) or had Family Planning Medicaid. We then excluded women who did not have at least one 2019 institutional or professional claim. The reason is that these files contain ICD-10-CM codes, which are necessary to determine the presence of intellectual and developmental disabilities. In addition, we excluded women who were medically or surgically infecund for noncontraceptive reasons (eg, natural menopause, oophorectomy), women who had a live birth in November or December because there was inadequate time to document postpartum contraceptive provision, and women who had an unknown pregnancy outcome at the end of 2019.19
Eligible women who had at least one ICD-10-CM code specifying an intellectual or developmental disability during 2019 were subsequently assigned to the “with intellectual and developmental disabilities” cohort. All remaining women were included in the “without intellectual and developmental disabilities” cohort. Codes used for intellectual and developmental disability identification were derived from previous studies (Appendix 1, available online at http://links.lww.com/AOG/D442).11,22,23
Our primary outcomes included the proportion of women in each cohort who received 1) most or moderately effective contraception (ie, sterilization, intrauterine device or system [IUD or IUS], implant, injection, oral pills, patch, ring, diaphragm), 2) long-acting reversible contraception (LARC) (ie, IUD or IUS, implant), 3) short-acting contraception (ie, injection, oral pills, patch, ring), and 4) individual contraceptive methods. For each measure of interest, contraceptive receipt was identified by the presence of at least one relevant ICD-10-CM code, ICD-10-PCS code, Current Procedural Terminology code, Healthcare Common Procedure Coding System code, or National Drug Code. We used 2019 code sets supplied by the DHHS Office of Population Affairs for the provision of most or moderately effective contraception, LARC, and individual contraceptive methods.19 Because provision of short-acting contraception was not a DHHS Office of Population Affairs–established measure, we created a code set to mirror the LARC indicator that included access-related codes for injection, oral pills, patch, and ring (Appendix 2, available online at http://links.lww.com/AOG/D442).
To further characterize service utilization, we developed code sets to examine the breakdown of encounters related to most or moderately effective contraception by procedure type (ie, initial provision, surveillance, removal) (Appendix 2, http://links.lww.com/AOG/D442). We also calculated the contraceptive method mix to evaluate method distribution among each cohort (ie, the number of women who received each method divided by the total number of women who received most or moderately effective contraception). We disaggregated most or moderately effective contraceptive receipt by sociodemographic factors, including age, race, ethnicity, level of intellectual disability, type of developmental disability, and urban or rural setting based on North Carolina's county-level classification.24 Race was included as a factor in our study because race and systemic racism may affect access to health care services. Missing data for sociodemographic characteristics were classified as a separate category, “unreported,” for race, ethnicity, and urban or rural setting variables.
We conducted a subanalysis to evaluate use of contraception for secondary benefits, specifically menstrual management, as a potential driver of differences in contraceptive provision between women with and without intellectual and developmental disabilities. To test the hypothesis that women with intellectual and developmental disabilities are more likely to receive contraception for menstrual management, we calculated the prevalence of common menstrual disorder codes (ie, abnormal uterine bleeding, dysmenorrhea, premenstrual syndrome) among women with and without intellectual and developmental disabilities (Appendix 3, available online at http://links.lww.com/AOG/D442). For each cohort, we examined the co-occurrence of menstrual disorder diagnoses and contraceptive provision, calculating the proportion of women with a menstrual disorder code among the total number of women who received most or moderately effective contraception. We repeated this analysis for each individual contraceptive method.
We used χ2 tests to compare the distribution of sociodemographic characteristics and the proportion of women who received contraception between our two cohorts. An unadjusted logistic regression model estimated odds of most or moderately effective contraceptive provision based on intellectual and developmental disability status. We also constructed a multivariable logistic regression model controlling for age, race, ethnicity, and urban or rural setting. In addition, we replaced the intellectual and developmental disability status predictor variable (ie, with intellectual and developmental disabilities vs without intellectual and developmental disabilities) with two alternative variables: level of intellectual disability and type of developmental disability (Appendix 1, http://links.lww.com/AOG/D442). Regression coefficients, P values, and 95% CIs were reported, and model diagnostics were performed. The residuals randomly scattered around zero with no obvious patterns, suggesting that the linearity assumption was satisfied. All analyses were conducted with SAS 9.4 and R 4.0.3 at the 0.05 significance level (α=0.05).
It was possible that some women without an intellectual and developmental disability ICD-10-CM code in 2019 may have received such a diagnosis in prior years and been incorrectly classified as “without intellectual and developmental disabilities.” To assess the robustness of our results, we performed a sensitivity analysis using a 1-year look-back period. We first selected women who were initially allocated to the 2019 “without intellectual and developmental disabilities” cohort and who also met 2018 enrollment criteria. If a woman received an intellectual and developmental disability ICD-10-CM code during 2018, we reassigned them to the 2019 “with intellectual and developmental disabilities” cohort. We repeated all analyses using the updated cohorts and compared the results with our original findings. Study approval was provided by the Duke University Health System IRB and the North Carolina Department of Health and Human Services Medicaid Review Committee.
RESULTS
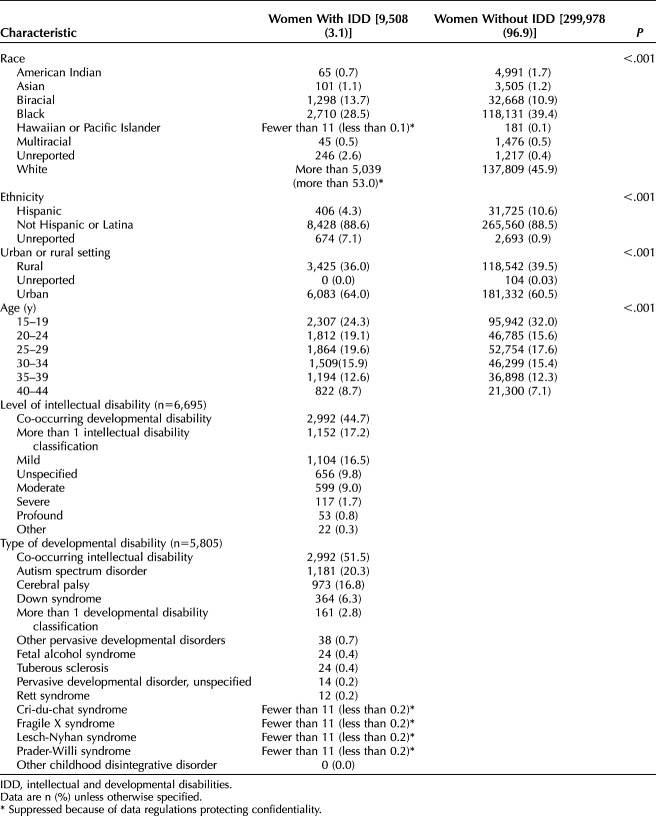
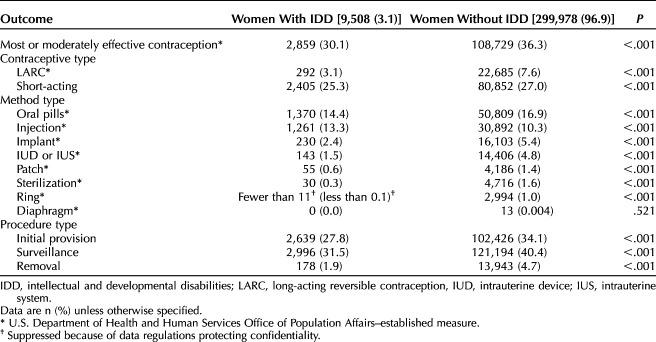
Of the 1,502,083 women enrolled in 2019 North Carolina Medicaid, 309,486 met the inclusion and exclusion criteria (Fig. 1). Among these women, 9,508 (3.1%) had intellectual and developmental disabilities, and 299,978 (96.9%) did not have intellectual and developmental disabilities. Our intellectual and developmental disabilities cohort was less diverse across racial, ethnic, and geographic characteristics and was significantly older than women without intellectual and developmental disabilities (P<.001) (Table 1). Of women with intellectual and developmental disabilities, 6,695 had an intellectual disability, 5,805 had a developmental disability, and 2,992 had both an intellectual and a developmental disability. A plurality of women with intellectual disabilities received ICD-10-CM codes for more than one level classification (17.2%). However, among those with only a single classification, mild intellectual disability (16.5%) was most common. The most prevalent developmental disabilities were autism spectrum disorder (20.3%) and cerebral palsy (16.8%) (Table 1).
Fig. 1. Cohort identification flow diagram. *There were 213 women who were excluded because of overlapping infertility and pregnancy criteria.
Mitchell. Contraceptive Provision by Intellectual and Developmental Disability Status. Obstet Gynecol 2023.
Table 1.
Cohort Demographics by Intellectual and Developmental Disability Status (N=309,486)
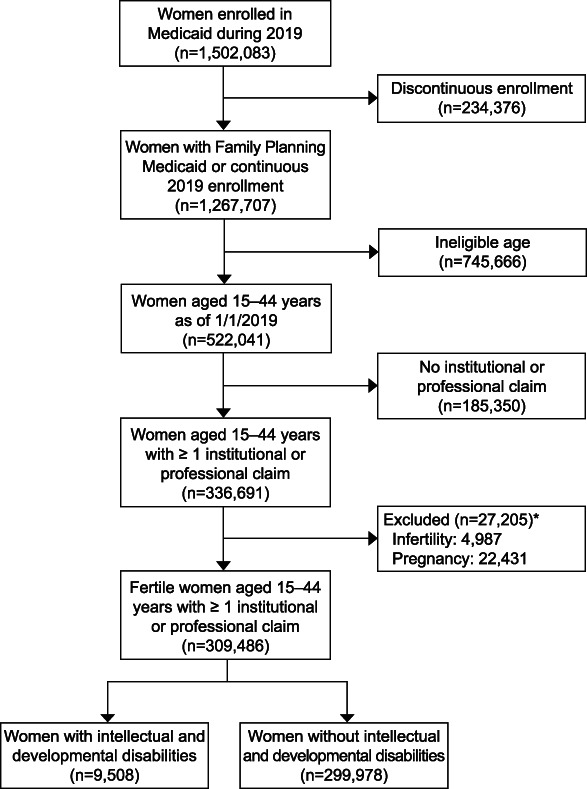
A significantly smaller proportion of women with intellectual and developmental disabilities were provided most or moderately effective contraception compared with women without intellectual and developmental disabilities (30.1% vs 36.3%, P<.001) (Table 2). This finding held true for both LARC (3.1% vs 7.6%; P<.001) and short-acting contraception (25.3% vs 27.0%, P<.001), as well as for all individual methods except diaphragm and injection. Diaphragm use was uncommon in both cohorts. However, compared with their counterparts, a significantly greater proportion of women with intellectual and developmental disabilities received injectable contraception (13.3% vs 10.3%, P<.001) (Table 2). Overall, oral contraceptives were the most commonly used contraceptive type among both cohorts. Women with intellectual and developmental disabilities were less likely than women without intellectual and developmental disabilities to use sterilization, IUD or IUS, implant, patch, and ring, although they were more likely to use injectable contraception (44.1% vs 28.4%; P<.001) (Appendix 4, available online at http://links.lww.com/AOG/D442).
Table 2.
Contraceptive Provision by Intellectual and Developmental Disability Status (N=309,486)
Among women with a single intellectual disability diagnosis, those with a mild disability were most frequently provided most or moderately effective contraception (16.5%), followed by those with moderate (7.7%), severe (1.5%), and profound (0.5%) disabilities (Appendix 5, available online at http://links.lww.com/AOG/D442). Similarly, among those with a single developmental disability diagnosis, women with autism spectrum disorder (21.8%), cerebral palsy (14.8%), and Down syndrome (3.8%) most commonly received most or moderately effective contraception (Appendix 5, http://links.lww.com/AOG/D442).
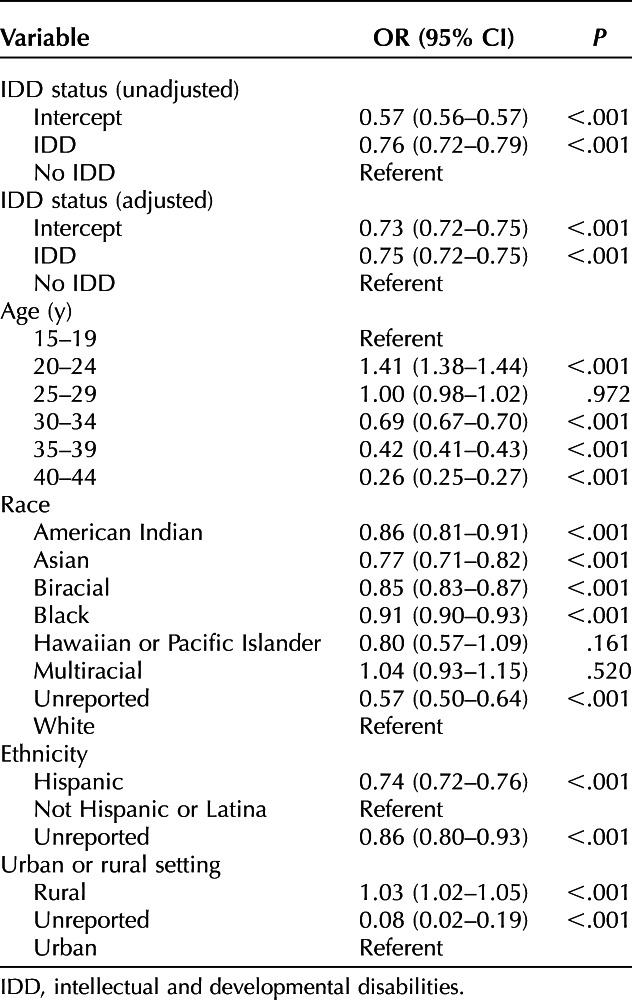
In logistic regression models controlling for sociodemographic factors, women with intellectual and developmental disabilities remained significantly less likely to receive most or moderately effective contraception (adjusted odds ratio 0.75, 95% CI 0.72–0.79, P<.001) (Table 3 and Appendix 6, available online at http://links.lww.com/AOG/D442). When stratified by level of intellectual disability, we observed that the odds of most or moderately effective contraceptive receipt decrease with increasing disability severity. The likelihood of most or moderately effective contraceptive receipt is 0.82 for women with a mild disability (95% CI 0.72–0.93, P=.002) and 0.68 for women with a moderate disability (95% CI 0.57–0.82, P<.001), compared with women without intellectual disabilities (Appendix 7, available online at http://links.lww.com/AOG/D442). Odds of most or moderately effective contraceptive receipt also varied significantly by type of developmental disability. Compared with women without developmental disabilities, odds of most or moderately effective contraceptive provision for women with autism spectrum disorder, cerebral palsy, and Down syndrome were 0.67 (95% CI 0.59–0.76, P<.001), 0.63 (95% CI 0.55–0.73, P<.001), and 0.39 (95% CI 0.30–0.51, P<.001), respectively (Appendix 8, available online at http://links.lww.com/AOG/D442). No statistically significant difference was observed for other individual developmental disorders. In addition, women with intellectual and developmental disabilities who were aged 20–24 years, White, non-Hispanic or Latina, and reported an urban ZIP code were more likely to receive most or moderately effective contraception (Table 3) (Appendices 7 and 8, http://links.lww.com/AOG/D442).
Table 3.
Odds of Most or Moderately Effective Contraceptive Receipt Among Eligible Women Aged 15–44 Years (N=309,486)
Subanalyses assessing the co-occurrence of contraceptive provision and menstrual disorder diagnosis suggested that menstrual disorders may be a mediator of contraceptive use among women with intellectual and developmental disabilities. Of women with intellectual and developmental disabilities, 18.1% received a diagnosis for a common menstrual disorder during 2019 compared with 16.6% of women without intellectual and developmental disabilities (P<.001) (Appendix 9, available online at http://links.lww.com/AOG/D442). Those with intellectual and developmental disabilities who received most or moderately effective contraception also had a higher prevalence of menstrual disorders than their counterparts (31.3% vs 24.3%, P<.001) (Appendices 9–11, available online at http://links.lww.com/AOG/D442).
In our sensitivity analysis using a 1-year look-back period, we identified 1,153 women who received an intellectual and developmental disability diagnosis in 2018 but not in 2019. Results yielded comparable estimates when we reclassified these additional individuals as having intellectual and developmental disabilities (Appendices 12–16, available online at http://links.lww.com/AOG/D442).
DISCUSSION
Findings in North Carolina suggest several disparities in contraceptive use among women with intellectual and developmental disabilities. Those with intellectual and developmental disabilities were more likely to use injectable contraception and less likely to use all other methods than women without intellectual and developmental disabilities. It is important to note that we found lower rates of most or moderately effective contraceptive provision to women with more severe intellectual disabilities or three of the most prevalent developmental disabilities (ie, autism spectrum disorder, cerebral palsy, Down syndrome). In addition, these findings suggest that need for menstrual regulation may be a major facilitator of contraceptive provision among women with intellectual and developmental disabilities.
Our findings align with an analysis of 2012 Massachusetts insurance claims, which demonstrated lower odds of receiving LARC and moderately effective contraception but higher odds of receiving injection among women with intellectual and developmental disabilities.11 The results are also consistent with 2011–2015 National Survey of Family Growth data, which demonstrated higher contraceptive nonuse among women self-reporting cognitive disabilities.25 A population-level study of postpartum contraceptive provision to individuals participating in a publicly funded Ontario drug plan similarly identified higher rates of injectable contraceptive receipt among women with intellectual and developmental disabilities.26 Potential explanations for this trend include the high rate of induced amenorrhea with injection compared with other methods,27 as well as its convenience and administrative ease.10 For this reason, it is also possible that physician bias or coercion toward injection occurs when caring for patients with intellectual and developmental disabilities. Overall, qualitative data suggest that women with intellectual and developmental disabilities face inaccessible clinical settings, physician bias, and low contraceptive knowledge, which may restrict health care access.28,29 Few women with intellectual and developmental disabilities in North Carolina received sterilization, but we do not have a measure of prevalence comparable with other studies.
Past studies have demonstrated why menstrual regulation may motivate contraceptive use among this population. A 2022 literature review concluded that women with intellectual disabilities experience menstrual hygiene challenges.29 In a cohort study of young women with physical or cognitive disabilities presenting for menstrual management (ie, irregular or heavy bleeding, dysmenorrhea, convenience or hygiene-related desires), nearly 80% sought hormonal suppression methods.27 Our study builds on these findings to suggest that physicians may be more likely to supply contraception for menstrual health among women with intellectual and developmental disabilities. However, the greater co-occurrence of menstrual disorders and contraceptive receipt among women with intellectual and developmental disabilities identified in our study should not be interpreted as a direct correlation. It is possible that other confounders or clinical decision-making processes influence this association.
Our study provides a more comprehensive view of contraceptive provision by intellectual and developmental disability status than previous population-level analyses by controlling for numerous sociodemographic characteristics, including race, ethnicity, and geography, and by exploring the influence of intellectual and developmental disability classification and menstrual disorder co-occurrence. In addition, the use of Medicaid claims offers insight into health care utilization patterns of large samples of women who may otherwise be excluded from national data sets and avoids self-reporting and selection bias, common in large-scale surveys. Our study also has several limitations. Administrative data sets lack clinical detail such as the primary motivation for contraceptive use and may have inaccuracies inherent in the translation of a clinical visit to billing and diagnosis codes.30 As stated, the data set does not identify noncisgender individuals, and we were unable to determine whether women were sexually active to characterize unmet need for family planning. Other characteristics relevant to contraceptive uptake such as marital status, parity, and pregnancy desire are also unavailable in Medicaid claims, which could potentially bias the presented estimates. Bias could arise if women with and without intellectual and developmental disabilities were not equally as likely to have a claim during the study period. Therefore, our results apply to women with claims rather than all women enrolled in Medicaid. Our data also may not be generalizable to patients with private insurance or other states. In addition, because we analyzed data preceding the COVID-19 pandemic, it is possible that contraceptive receipt has since changed as a result of telehealth expansion and altered prescribing patterns.
The noted disparities in contraceptive provision to women with intellectual and developmental disabilities merit further qualitative study assessing physician and patient motivations, perceptions, and preferences. North Carolina has a shameful history of eugenics-based, forced sterilization that included a focus on people with intellectual and developmental disabilities,31 which may continually affect clinician and patient interactions around contraceptive use. For example, medical mistrust among women with intellectual and developmental disabilities and their caretakers might prevent or delay sexual and reproductive health care, and physician hesitancy may stem from difficulty navigating patients' capacity to consent, guardianship status, or existing sexual and reproductive health knowledge levels. Future interventions such as physical and communication accommodations, antibias training, and physician education in care delivery for patients with intellectual and developmental disabilities3 may be important to help combat accessibility barriers and to ensure equity in access to care.
Footnotes
Duke University Bass Connections provided financial support for this work. Jonas J. Swartz is supported by award K12HD103083 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Financial Disclosure Jonas J. Swartz is a current NEXPLANON trainer for Organon. The other authors did not report any potential conflicts of interest.
This research was supported by a Student Research Award from Duke University Bass Connections. North Carolina Medicaid claims data were made available through partnership between the Duke Department of Population Health Sciences and the North Carolina Department of Health and Human Services. The authors thank Dr. Kelley Jones for methodologic assistance and data consultation.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/D443.
REFERENCES
- 1.Greenwood NW, Wilkinson J. Sexual and reproductive health care for women with intellectual disabilities: a primary care perspective. Int J Fam Med 2013;2013:1–8. doi: 10.1155/2013/642472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McCarthy M. Women with intellectual disability: their sexual lives in the 21st century. J Intellect Dev Disabil 2014;39:124–31. doi: 10.3109/13668250.2014.894963 [DOI] [Google Scholar]
- 3.Johnston KJ, Chin MH, Pollack HA. Health equity for individuals with intellectual and developmental disabilities. JAMA 2022;328:1587–8. doi: 10.1001/jama.2022.18500 [DOI] [PubMed] [Google Scholar]
- 4.Ledger S, Earle S, Tilley E, Walmsley J. Contraceptive decision-making and women with learning disabilities. Sexualities 2016;19:698–724. doi: 10.1177/1363460715620576 [DOI] [Google Scholar]
- 5.Ali A, Scior K, Ratti V, Strydom A, King M, Hassiotis A. Discrimination and other barriers to accessing health care: perspectives of patients with mild and moderate intellectual disability and their carers. PLoS One 2013;8:e70855. doi: 10.1371/journal.pone.0070855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brkić-Jovanović N, Runjo V, Tamaš D, Slavković S, Milankov V. Persons with intellectual disability: sexual behaviour, knowledge and assertiveness. Slovenian J Public Health 2021;60:82–9. doi: 10.2478/sjph-2021-0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Silvers A, Francis L, Badesch B. Reproductive rights and access to reproductive services for women with disabilities. AMA J Ethics 2016;18:430–7. doi: 10.1001/journalofethics.2016.18.4.msoc1-1604 [DOI] [PubMed] [Google Scholar]
- 8.Brown HK, Lunsky Y, Wilton AS, Cobigo V, Vigod SN. Pregnancy in women with intellectual and developmental disabilities. J Obstet Gynaecol Can 2016;38:9–16. doi: 10.1016/j.jogc.2015.10.004 [DOI] [PubMed] [Google Scholar]
- 9.Baines S, Emerson E, Robertson J, Hatton C. Sexual activity and sexual health among young adults with and without mild/moderate intellectual disability. BMC Public Health 2018;18:667–12. doi: 10.1186/s12889-018-5572-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verlenden JV, Bertolli J, Warner L. Contraceptive practices and reproductive health considerations for adolescent and adult women with intellectual and developmental disabilities: a review of the literature. Sex Disabil 2019;37:541–57. doi: 10.1007/s11195-019-09600-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu J, Zhang J, Mitra M, Parish SL, Minama Reddy GK, Kavya G. Provision of moderately and highly effective reversible contraception to insured women with intellectual and developmental disabilities. Obstet Gynecol 2018;132:565–74. doi: 10.1097/AOG.0000000000002777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Darney BG, Jacob RL, Hoopes M, Rodriguez MI, Hatch B, Marino M, et al. Evaluation of Medicaid expansion under the Affordable Care Act and contraceptive care in US community health centers. JAMA Netw Open 2020;3:e206874. doi: 10.1001/jamanetworkopen.2020.6874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rice WS, Redd SK, Luke AA, Komro K, Jacob Arriola K, Hall KS. Dispersion of contraceptive access policies across the United States from 2006 to 2021. Prev Med Rep 2022;27:101827. doi: 10.1016/j.pmedr.2022.101827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larson S, Eschenbacher H, Pettingell S, Anderson L, Taylor B, Sowers M, et al. In-home and residential long-term supports and services for persons with intellectual or developmental disabilities: status and trends through 2017. Accessed April 1, 2023. https://ici-s.umn.edu/files/aCHyYaFjMi?variant=&locale=&fileGroup=pdf
- 15.Jackson AV, Wang L, Morse J. Racial and ethnic differences in contraception use and obstetric outcomes: a review. Semin Perinatol 2017;41:273–7. doi: 10.1053/j.semperi.2017.04.003 [DOI] [PubMed] [Google Scholar]
- 16.Rodriguez MI, Meath T, Huang J, Darney BG, McConnell KJ. Association of rural location and long acting reversible contraceptive use among Oregon Medicaid recipients. Contraception 2021;104:571–6. doi: 10.1016/j.contraception.2021.06.019 [DOI] [PubMed] [Google Scholar]
- 17.North Carolina Department of Health and Human Services, Division of Health Benefits. North Carolina Medicaid enrollment overview. Accessed April 21, 2022. https://medicaid.ncdhhs.gov/reports/dashboards#enroll
- 18.Barth S, Lewis S, Simmons T. Medicaid services for people with intellectual or developmental disabilities–evolution of addressing service needs and preferences: report to the Medicaid and CHIP Payment and Access Commission. Accessed February 15, 2023. https://healthmanagement.com/wp-content/uploads/MedicaidIDDDevolution_FINAL-1.20.21.pdf
- 19.U.S. Department of Health and Human Services, Office of Population Affairs. Measure CCW: contraceptive care-all women ages 15-44. Accessed June 12, 2022. https://opa.hhs.gov/sites/default/files/2020-12/2019-measure-specifications-ccw-for-opa-website.pdf
- 20.Centers for Medicare & Medicaid Services. The Maternal and Infant Health Initiative grant to support development and testing of Medicaid contraceptive care measures. Accessed February 15, 2023. https://medicaid.gov/medicaid/quality-of-care/downloads/mihi-contraceptive-measures.pdf
- 21.National Quality Forum. NQF endorses perinatal and reproductive health measures. Accessed February 15, 2023. http://www.qualityforum.org/News_And_Resources/Press_Releases/2017/NQF_Endorses_Perinatal_and_Reproductive_Health_Measures.aspx
- 22.Bonine NG, Banks E, Harrington A, Vlahiotis A, Moore-Schiltz L, Gillard P. Contemporary treatment utilization among women diagnosed with symptomatic uterine fibroids in the United States. BMC Womens Health 2020;20:174. doi: 10.1186/s12905-020-01005-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitra M, Parish SL, Clements KM, Cui X, Diop H. Pregnancy outcomes among women with intellectual and developmental disabilities. Am J Prev Med 2015;48:300–8. doi: 10.1016/j.amepre.2014.09.032 [DOI] [PubMed] [Google Scholar]
- 24.North Carolina Department of Health and Human Services. North Carolina rural and urban counties. Accessed September 10, 2021. https://files.nc.gov/ncdhhs/RuralUrban_2019.pdf
- 25.Mosher W, Hughes RB, Bloom T, Horton L, Mojtabai R, Alhusen JL. Contraceptive use by disability status: new national estimates from the National Survey of Family Growth. Contraception 2018;97:552–8. doi: 10.1016/j.contraception.2018.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brown HK, Kirkham YA, Lunsky Y, Cobigo V, Vigod SN. Contraceptive provision to postpartum women with intellectual and developmental disabilities: a population-based cohort study. Perspect Sex Reprod Health 2018;50:93–9. doi: 10.1363/psrh.12060 [DOI] [PubMed] [Google Scholar]
- 27.Frances Fei Y, Ernst SD, Dendrinos ML, Quint EH. Satisfaction with hormonal treatment for menstrual suppression in adolescents and young women with disabilities. J Adolesc Health 2021;69:482–8. doi: 10.1016/j.jadohealth.2021.01.031 [DOI] [PubMed] [Google Scholar]
- 28.Horner-Johnson W, Klein KA, Campbell J, Guise JM. Experiences of women with disabilities in accessing and receiving contraceptive care. J Obstet Gynecol Neonatal Nurs 2021;50:732–41. doi: 10.1016/j.jogn.2021.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh Shrestha P, Ishak A, Maskey U, Neupane P, Sarwar S, Desai S, et al. Challenges in providing reproductive and gynecologic care to women with intellectual disabilities: a review of existing literature. J Fam Reprod Health 2022;16:9–15. doi: 10.18502/jfrh.v16i1.8589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stein JD, Lum F, Lee PP, Rich WL, Coleman AL. Use of health care claims data to study patients with ophthalmologic conditions. Ophthalmology 2014;121:1134–41. doi: 10.1016/j.ophtha.2013.11.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gartner DR, Krome-Lukens AL, Delamater PL. Implementation of eugenic sterilization in North Carolina: geographic proximity to Raleigh and its association with female sterilization during the mid-20th century. Southeast Geographer 2020;60:254–74. doi: 10.1353/sgo.2020.0020 [DOI] [Google Scholar]