Abstract
Introduction
The opportunity of using Endocrown-type restorations in the current prosthetic dentistry practice as an alternative to other, well-established methods of corono-radicular restorations and the evolving palette of adhesive materials has made these restorations more popular in the last few years.
Objective
The purpose is to review the available literature about Endocrown restorations regarding mechanical properties – fracture strength and resistance, survival rate, the preparation design – marginal and internal adaptation, and esthetics.
Method
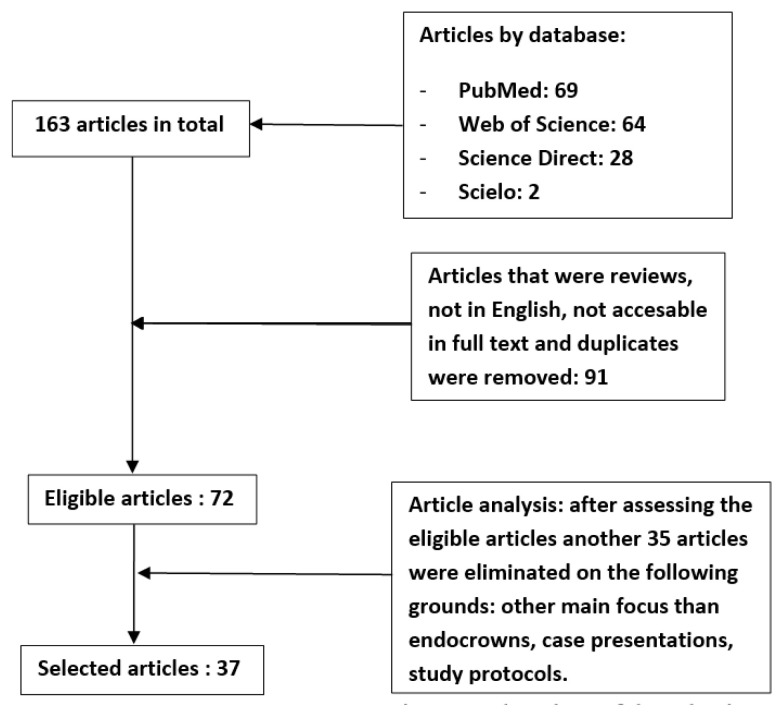
The search was carried out on four databases: PubMed, Scopus (ScienceDirect), Web of Science, and Scielo using the following terms: ”endocrowns”, ”endodontic crown”, and” no buildup crown”. Initially, a total of 163 articles published between 2015 and May 2021 were selected. After the duplicates, papers presented only as abstracts, articles in any other languages except English, and review articles were eliminated; a total of 72 articles remained to be considered for this review.
After assessing the 72 considered articles, 37 were chosen as fit for this review. The reasons for the elimination of the other 35 articles were: their main focus was other than endocrowns, e.g., direct restorations, indirect restorations of vital teeth; case reports; study protocols.
Results
From the 37 articles selected, 34 were focused on mechanical properties, including the influence of the preparation design, and three on survival rate, of which one also had a point of view regarding esthetics.
Conclusions
The literature included in this review shows that endocrowns perform similarly or even better in some cases than other coronal restorations. However, this statement must be interpreted cautiously, given that most articles were in vitro or finite element analysis studies. Given the high degree of conflicting results found in the articles included in this review, the authors consider as reasonable to conclude that further studies are needed to confirm the feasibility of endocrowns and the best choice of material.
Keywords: endocrowns, corono-radicular restorations, non-vital teeth, minimal invasive prosthodontics
Introduction
In everyday practice, clinicians often need to restore teeth with extensive destruction, either as a result of dental decays which have infiltrated a large portion of the tooth structure or due to macro- or microtraumatic events. Moreover, in these cases, additional endodontic treatment is frequently required. This situation leads to even more tooth structure needing to be excised [1]. Because of the considerable amount of hard tissue loss and complex microstructure modifications of dentine, the mechanical properties and longevity of the endodontically treated teeth may be severely compromised [2]. As a result, when considering prosthetic restoration, the rehabilitation of these teeth becomes problematic [3].
In the last years, different materials and innovative techniques were introduced to fabricate restorations that improve the function and esthetics of non-vital teeth [2].
Standard and well-established therapies, both the classical, cast metal dowel and the newer fiber-reinforced posts, have disadvantages. A significant problem is the supplementary removal of the dental structure, especially from the walls of the root canals, which causes a further decrease in mechanical resistance; in addition, the existence of multiple adhesion surfaces, acting as possible infiltration layers; differences between modulus of elasticity between tooth structure and restorative materials, which leads to uneven stress distribution, are reported [3–7].
Clinicians prefer prefabricated fiber posts due to their similar mechanical behavior and elasticity modulus to that of dentin and improved esthetics. However, the primary role of the fiber-reinforced posts and traditional metal posts was to ensure good mechanical retention of the core buildup, not to increase the fracture resistance of the endodontically treated roots [8].
The modern adhesive techniques offer new possibilities to fabricate less invasive restorations, which lead to the conservation of an increased amount of healthy dental structures; subsequently, the use of posts to provide mechanical retention for the full-coverage crowns was questioned.
Endocrowns represent monolithic conservative restorations introduced as an alternative to the conventional prosthodontic approach for severely compromised endodontically treated teeth. The anchorage of the endocrowns is into the pulp chamber or at the emergence of the root canal, without extending into it [9].
Lately, in the field of restorative dentistry, computer-aided design (CAD) and computer-aided manufacture (CAM) technology has developed tremendously, allowing to fabricate endocrown restorations. These variants have a precise internal and marginal adaptation, functional occlusal contacts, and pleasant esthetic appearance. The clinicians can choose from various dental materials, like feldspathic, lithium disilicate, leucite-reinforced, and lithium silicate glass ceramics, zirconia, hybrid ceramics, and composite resins, according to the particularities of the clinical case [10]. Thanks to these materials’ properties, endocrowns benefit from both macro and micro retention [11,12]. Other advantages of endocrowns are: the minimal amount of dental tissue required to be removed and the reduced working time by eliminating certain clinical and technical steps. Due to their configuration and pattern of contact with the remaining dental structures, after cementation, the endocrowns ensure the distribution of the occlusal forces that mimic the natural tooth [13,14].
However, there is extensive debate in the literature regarding the restorative options for the endodontically treated teeth with a decreased amount of healthy coronal structure.
Although there are other reviews available concerning endocrown restorations, they focus on specific issues: the influence of materials on their mechanical properties [15], survival and success rate [16], correlation with the type of tooth restored [17], comparison to other conventional treatments [18].
Therefore, this review aims to offer a more comprehensive image of endocrowns and assess the influence of different materials and preparation designs on the mechanical properties, survival, success rate and esthetics of endocrowns.
Methods
The online research was performed on PubMed, Scopus (ScienceDirect), Web of Science, and Scielo databases to identify the significant articles. The following keywords were selected for the search strategy:”endocrown”, ”endodontic crown”, ”no buildup crown”, as shown in table I. The publications written in English between 2015 and 2021, which referred to the mechanical properties, survival rate, influence of preparation design and esthetics of endocrowns, were included in the study.
Table I.
The strategy used for the online research.
| PubMed “Endocrown” OR “Endocrowns” OR “Endodontic crown” OR “Endodonticcrown” OR “no buildup crown” OR “no buildup crown” |
| Scopus(ScienceDirect) (Endocrown) OR (Endocrowns) OR (Endodontic crown) OR (Endodonticcrown) OR (no buildup crown) OR (no buildup crown) |
| Web of Science “Endocrown” OR “Endocrowns” OR “Endodontic crown” OR “Endodonticcrown” OR “no buildup crown” OR “no buildup crown” |
| Scielo (Endocrown) OR (Endocrowns) OR (Endodontic crown) OR (Endodonticcrown) OR (no buildup crown) OR (no buildup crown) |
A total of 163 articles published between 2015 and May 2021 were initially selected; in the next stage, 91 articles that were duplicates, reviews, or presented as abstracts were removed, as seen in table II, which resulted in a total of 72 titles; after a thorough examination of their content and the relevance to the aim of the present review, 37 titles have been selected. The flowchart of this research is presented in figure 1.
Table II.
Eligibility criteria for study selection.
| Inclusion criteria | Exclusion criteria |
|---|---|
| In-vitro and in-vivo studies published in English | Studies reported in languages other than English |
| Studies where experiments were conducted in endodontically treated human permanent teeth or on models of permanent teeth | Reviews and abstracts |
| Studies that followed the influence of different materials and preparation designs on the mechanical properties, survival and success rate, and esthetics of endocrowns. | Case reports |
| Studies that compare endocrowns to other conventional restorations | Duplicates |
Figure 1.
Flowchart of the selection.
Results
According to their topics, the selected articles were divided into several categories: the mechanical properties and the influence of preparation design on the fracture strength of the endocrowns (34 articles), the endocrowns’ survivability (3 articles), and the endocrown’s esthetic appearance (1 article – has the survival rate as the main subject, but also assesses the esthetic properties).
The mechanical properties were assessed from different perspectives: studies that compared different materials indicated to fabricate the endocrowns (10), various preparation designs for endocrowns (6), a combination of these two parameters (6), studies that compared the mechanical properties of endocrowns with other restorations (7), studies that compared different materials for endocrowns versus other types of restorations (5). The publications are included in table III [19–52].
Table III.
Studies regarding mechanical properties.
| Author (year) | Tested properties | Results |
|---|---|---|
|
RESTORATIVE MATERIALS Studies that compared different types of materials indicated to fabricate the endocrowns and their mechanical properties | ||
| Zirconia | ||
| Elashmawy (2021) [19] | Fracture strength Thermocycling + chewing simulation/fatigue strength |
Zirconia – highest/ Biohpp – lowest fracture strength; After thermocycling: Significant fracture strength reduction for zirconia and biohpp, Not significant for the Vita Enamic and IPS E.Max CAD |
| Kanat (2018) [20] | Fracture strength at 45 angle after thermocycling | Zirconia showed the best results but had the most non-repairable failures |
| Dartora (2020) [21] | Fracture strength after thermocycling and chewing simulation/ fatigue strength | Zirconia had the highest fracture strength |
| Skalskyi (2017) [22] | Fracture strength | Zirconia showed the highest fracture strength in the experimental group on materials samples, metal-ceramic in the teeth group |
| Resin nanoceramic | ||
| El-Damanhoury (2015) [23] | Fracture strength at 35 angle after thermocycling Microleakage – immersion in methylene-blue |
Resin nanoceramic showed the highest fracture resistance but also the highest degree of microleakage |
| Taha (2018) [24] | Marginal adaptation evaluated by stereomicroscope before and after cementation and after thermomechanical aging Fracture strength |
Marginal adaptation showed no significant differences between materials but significantly increased after both cementation and cycling Resin nanoceramics and lithium disilicate showed the highest fracture resistance |
| Lithium disilicate | ||
| Gresnigt (2016) [25] | Axial and lateral loading fracture strength after thermocycling | Axial loading showed no significant difference between the lithium disilicate, resin composite, and control group Under lateral loading, the lithium disilicate group showed significantly higher resistance |
| Saglam (2020) [26] | Marginal adaptation after thermocycling Fracture strength after thermocycling |
No significant differences were found concerning marginal adaptation Both lithium disilicate groups (CAD and press) showed a significantly higher fracture resistance |
| Other materials | ||
| Skalskyi (2017) [22] | Fracture strength | Zirconia showed the highest fracture strength in the experimental group on materials samples, metal-ceramic in the teeth group |
| Sedrez-Porto (2019) [27] | Fracture strength under axial loading after fatigue simulation | Bulk-Fill direct endocrowns exhibited the highest load-to-fracture values and were more significant than the controls and the Z350 and GFP_Z350 groups, while the E.max and sound tooth group presented the lowest mechanical behavior of the study |
| Zheng (2020) [28] | Stress distribution under axial and lateral loading Fracture strength under axial loading |
Composite resin endocrowns showed better stress distribution and a higher fracture strength |
|
DESIGN PREPARATION Studies that compared the influence of different designs on the mechanical properties of endocrowns | ||
| Turkistani (2020) [29] | Fracture strength for three different thicknesses (3, 4.5, 6 mm), all lithium disilicate | The highest fracture strength was found in the 3 mm group |
| Doaa Taha (2017) [30] | Fracture strength after thermal aging Shoulder/butt-joint with 2mm and 3.5mm thickness |
Both shoulder groups showed a higher fracture resistance |
| Shin (2017) [31] | Marginal and internal discrepancies for two different cavity depths of 2/4 mm | Before cementation, the 4 mm group showed higher discrepancies |
| Hayes (2017) [32] | Fracture strength under a 45-degree angle for three different measurements of cavity depth 2/3/4 mm | 2 and 4 mm groups had the highest fracture resistance |
| Zhu (2020) [33] | Stress distribution in dentin around endocrowns under oblique load | The central retainer shape should be designed based on the anatomical form of the pulp chamber |
| De Kuijper (2020) [34] | Thermomechanical aging and fracture strength under axial loading. | Extension in the pulp chamber has no significant effect |
|
ENDOCROWNS VS. CROWNS Studies that compared the mechanical properties of endocrowns with other restorations | ||
| Rocca (2016) [35] | Thermo-mechanical fatigue loading and stepwise fatigue loading | No differences between endocrowns and the respective crowns |
| Rocca (2018) [36] | Thermo-mechanical cyclic loading and cyclic isometric stepwise loading | No differences were found between endocrowns and crowns |
| Pedrollo (2017) [37] | Cyclic loading and fracture strength under a 45-degree compressive loading | Composite endocrowns performed better |
| Kassis (2021) [38] | Thermo cycling and fracture strength under compressive load at 30 degrees | Endocrowns showed the highest fracture resistance |
| Li (2020) [39] | Stress distribution under static loading force (100N at 45 degrees) | 3 mm endocore endocrowns showed the best results for the incomplete ferrule groups |
| de Kuijper (2019) [40] | Thermomechanical aging and fracture strength under axial loading. | Lithium disilicate endocrowns performed significantly better than composite post, core buildup, and full contour crowns. |
| Silva-Sousa (2020) [41] | Thermomechanical aging and fracture strength | The „crown associated with glass fiber post and ferrule” showed the highest fracture resistance |
|
MATERIALS FOR ENDOCROWNS AND FULL-COVERAGE CROWNS Studies that compared different types of materials for endocrowns versus other types of restorations | ||
| Gungor (2017) [42] | Fracture strength under 45 degrees | Lithium disilicate endocrowns had the highest fracture point |
| El Ghoul (2019) [43] | Cycle loading and fracture strength – axial and lateral loading | Lithium disilicate endocrowns showed the highest fracture resistance under axial and lateral loading. All endocrown groups showed higher fracture resistance than the full crowns but showed increased irreparable failures. |
| Dejak (2020) [44] | Finite element analysis of stresses (according to the modified von Mises criteria) | Highest stress – zirconia onlay group |
| Hasanzade (2020) [45] | Internal and marginal adaptation | Endocrowns showed lower discrepancies invariable of the material |
| Tribst (2020) [46] | Finite element analysis – stress distribution under axial and lateral load | Endocrowns show an advantageous stress distribution under axial load; however, they have a higher cement layer failure risk under oblique load |
|
PREPARATION DESIGN and RESTORATIVE MATERIALS Studies that compared the influence of preparation design on different materials indicated for endocrowns | ||
| Madruga (2018) [47] | Fatigue loading and fracture strength | Thickness did not influence the outcome; lithium disilicate showed higher mean values of load to failure |
| Tribst (2018) [48] | Non-linear finite element analysis – stress distribution | The presence of more dental crown residual structure leads to a higher stress concentration on the restoration and a lower one for the cement line. |
| Ghajghouj (2019) [49] | Fracture strength and microleakage | Cavity depth did not influence fracture resistance or microleakage. Poly-ether-ether-ketone (PEEK) had the highest fracture resistance |
| El Ghoul (2019) [50] | Marginal and internal adaptation | Ceramic groups showed lower discrepancies |
| Haralur (2020) [51] | Thermocycling and fracture strength under axial load | Lithium disilicate showed the highest fracture strength for the 4.5 mm occlusal thickness/ 2mm endocore. Zirconia for the 2 mm thickness groups |
| Lin (2020) [52] | Finite element analysis – stress distribution | Endocrowns showed a reduced stress concentration on the inner root canal wall, making the restored teeth less prone to fracture. |
Most of the articles regarding mechanical properties included in this review were centered on molar specimens (22 of the 34 articles). Three articles used frontal teeth (central incisors and canines), three used premolars, and eight were based on models (7 on molar models and one on central incisor models).
Our research showed that most of the studies mainly analyzed the endocrowns fracture strength, regardless of the restorations configuration or material type. The fatigue strength, stress distribution, microleakage, and marginal and internal adaptation were also assessed. For a more accessible overview, the 34 studies were divided into various categories, such as those which focused mainly on fracture strength (9), fatigue strength (2), microleakage and internal and marginal adaptation (4), stress distribution (2), finite element analysis for stress distribution (4), or those which analyzed the influence of fatigue and fracture strength (9), microleakage and internal and marginal adaptation and fracture strength (3) or fatigue, fracture strength, microleakage and internal and marginal adaptation (1) on the mechanical properties of endocrowns. These categories are shown in figure 1.
Discussion
Mechanical properties
The studies included in this category were divided into three main categories – studies that focused on the different materials used for endocrowns, studies that compared various types of restorations, and studies concerning the influence of the preparation design.
1. Mechanical properties of the endocrowns concerning the materials
From the eleven studies that focus on different materials for endocrowns, 8 used mandibular molars, two maxillary molars, one mixed molars, and one used central maxillary incisors. The results of these twelve studies are not in consensus.
The first group of studies showed that monolithic zirconia endocrowns have the highest fracture resistance. Zirconia was compared to other restorative materials such as feldspathic ceramic, lithium disilicate ceramic, resin nano ceramic, polymer infiltrated ceramic (Kanat et al.), leucite ceramic, lithium disilicate ceramic and zirconia reinforced lithium disilicate ceramic (Dartora et al.), polymer infiltrated ceramic, PEEK and lithium disilicate ceramic (Elashmawy et al.), lithium disilicate ceramic, metal reinforced glass ceramic, composite resin (Skalskyi et al.) [19–22]. Dejak et al. [44] reported zirconia endocrowns having the highest fracture strength in a finite element analysis of stress distribution. Also, zirconia was shown to have a higher stress concentration point than lithium disilicate regardless of the occlusal thickness of the endocrown in finite element analysis that analyzed stress distribution (Lin et al.) [52].
However, in their studies, Dartora et al. and Elashmawy et al., concluded that despite their increased fracture resistance, monolithic zirconia endocrowns also presented the highest non-restorable failure patterns [19,21].
Resin nanoceramic endocrowns were found to have higher fracture resistance in two studies. El-Damanhoury et al. usedfeldspathic and lithium disilicate ceramics compared to resin nanoceramic, on maxillary molars [23]. Taha et al. compared fracture strength for resin nanoceramic endocrowns to lithium disilicate, polymer-infiltrated ceramic, and zirconia-reinforced lithium disilicate endocrowns, on mandibular molars and found that the resin nanoceramic and lithium disilicate groups showed the highest fracture strength [24].
Lithium disilicate was also found to have the highest fracture resistance in two studies. Gresnigt et al. compared it to resin nanoceramic for endocrowns on mandibular molars [25]. Saglam et al. used the Press and CAD variations of lithium disilicate ceramic, comparing it to feldspathic ceramic, polymer infiltrated ceramic, and zirconia-reinforced glass ceramic [26]. In another study, El Ghoul et al. found lithium disilicate endocrowns to have a higher fracture strength when compared to zirconia-reinforced lithium disilicate and resin nanoceramic for both endocrowns and crowns [43].
Also, Güngör et al., in comparing resin nanoceramic and lithium disilicate endocrowns and crowns, found that lithium disilicate endocrowns had the highest fracture strength [42].
Madruga et al. showed that lithium disilicate endocrowns havehigher fracture strength than leucite endocrowns [47]. However, Tribst et al. concluded that leucite ceramic endocrowns presented a lower stress concentration than those milled from lithium disilicate, thus being in direct contradiction [46].
Other materials were also shown to have good results concerning their mechanical properties when used for endocrowns. Metal-ceramic endocrowns showed the highest fracture strength compared to monolithic zirconia, lithium disilicate, metal-reinforced ceramic, and composite resin (Skalskyi et al.) [22]. In another instance, bulk-fill composite endocrowns had the highest fracture resistance compared to two other variants: composite modeled with resin adhesives and lithium disilicate ceramic (Sedrez-Porto et al.) [27]. According to Zheng et al., resin composite could also be an effective option for endocrowns compared to lithium disilicate, polymer infiltrated ceramic, resin nanoceramic, zirconia-reinforced glass ceramic, and hybrid nanoceramic since it showed a more uniform stress distribution and a higher fracture resistance [28].
2. Mechanical properties of the endocrowns versus full coverage crowns / other types of restorations
Another important topic of this study was to assess the fracture strength of endocrowns when compared to other types of restorations with different designs. The full-coverage crowns were considered by most clinicians as the most suitable alternative to endocrowns. The results showed no significant differences between these two types of dental restorations, according to Rocca et al. [35,36]. Opposed to this, de Kuijper et al. found that lithium disilicate endocrowns performed significantly better than composite full contour crowns with post and core [40].
Pedrollo et al. found no significant differences between endocrowns and full crowns with post and core when both restorations had a 5 mm root canal extension. However, for the restorations inserted 2.5 mm in the root canal, their study showed that endocrowns had higher fracture strength under a 45-degree compressive loading [37].
The influence of the ferrule effect was demonstrated by Li et al. They showed that even if the ferrule is incomplete around the cervical margins of a central maxillary incisor, the endocrowns with a 3 mm endocore thickness presented higher mechanical properties than the restorations with fiber-post core and crown or cast post, core and crown [39]. However, these results did not agree with those obtained by Silva-Sousa et al., who concluded that fiber post, core and crown had higher fracture resistance when compared to endocrowns [41].
In comparing endocrowns with other types of restoration, overlays (Rocca et al.), inlays, and onlays (Kassis et al.), the conclusion is that endocrowns have higher fracture strength [35,36,38]. Other studies concluded that the endocrowns have a better performance regarding fracture resistance (Gungor et al., El Ghoul et al.), and stress distribution of the occlusal loads (Tribst et al., Dejak et al.) compared to inlays, onlays or overlays [42–44,46].
3. Mechanical properties of the endocrowns in relation to preparation design
Over the years, different configurations for endocrown preparations were introduced, each having certain particularities regarding the height of the axial walls, the intraradicular length of the endocore, and the marginal finish lines.
Dimensions
Endocrown thickness, measured as the vertical distance from the margins of the axial walls to the most occlusal limit of the restoration, as shown in figure 2, was addressed in three studies. Turkistani et al. compared three thickness values – 3, 4.5, and 6 mm – showing that the 3 mm group had the highest fracture resistance [29]. Doaa Taha et al. found no difference concerning fracture resistance between 2 and 3 mm thickness for endocrowns [30]. Hayes et al., in comparing 2, 3, and 4 mm occlusal thickness, found that the 2 and 4 mm groups had higher fracture resistance [32].
Figure 2.
Configuration of the endocrown cemented on a molar.
Concerning endocore length (Figure 2), given by the depth of the restoration into the pulp chamber), it was reported that it does not influence the fracture resistance (De Kuijper et al.). or the marginal or internal discrepancies of the restorations (Shin et al.); both studies had addressed the same two length values (2 vs. 4 mm) [31,34]. In another study carried out on maxillary incisors, Kanat et al. have found that a more extensive length leads to marginally better mechanical performance for all of the following materials – feldspathic, lithium disilicate, resin, and polymer infiltrated ceramics and zirconia [20].
However, there is a relation between the preparation design, material type, endocore length, and fracture strength. Haralur et al. compared restorations with endocore thickness of 2mm and 4.5 mm without intraradicular extension with endocrowns with 4.5 mm endocore thickness and 2 mm radicular extension milled from zirconia, lithium disilicate and infiltrated ceramics. The highest fracture strength was found for the zirconia 2 mm endocore thickness group. In contrast, for the other types of endocore design, the lithium disilicate endocrowns presented higher fracture resistance than zirconia [51].
Marginal preparation design
Comparing the butt joint and a 1 mm shoulder preparation, Doaa Taha et al. showed that the shoulder preparation significantly increases fracture resistance [30]. In two other studies (Zhu et al. and De Kuijper et al.), no significant differences were found between butt joint and shoulder marginal preparations regarding stress distribution, respectively fracture strength [33,34].
Microleakage and adaptation
Some studies that focused on different mechanical properties also addressed the subject of internal and external discrepancies and microleakage.
Taha et al. analyzed different endocrowns made from resin nanoceramic, lithium disilicate, polymer-infiltrated ceramic, and zirconia-reinforced lithium disilicate on mandibular molars regarding marginal adaptation evaluated by stereomicroscope before and after cementation and after thermomechanical aging. No significant differences between the study groups were found concerning marginal vertical gaps; however, they significantly increased after cementation and thermocycling in all groups [30]. In addition, Saglam et al. used both the Press and CAD variations of lithium disilicate ceramic, comparing it to feldspathic ceramic, polymer infiltrated ceramic, and zirconia-reinforced glass ceramic and showed that the lithium disilicate Press ceramic has a higher marginal gap, but with no statistical difference [26].
El Ghoul et al. compared hybrid ceramic, fiber composite, lithium disilicate, and zirconia-reinforced lithium disilicate endocrowns regarding internal and external discrepancies. They found that the resin groups had significantly larger discrepancies [43]. Hasanzade et al. showed that endocrowns have better marginal and internal adaptation than inlays, onlays, or overlays [45].
El-Damanhoury et al. analyzed microleakage in comparing feldspathic and lithium disilicate ceramic endocrowns to resin nanoceramic ones. They showed that the latter has the highest microleakage of all three variants [23].
Regarding the influence of cementation material, Ghajghouj et al. addressed both material resistance, comparing lithium disilicate ceramic, zirconia reinforced glass ceramic, and PEEK, and the degree of leakage for different types of cement - Panavia V5, RelyX, and Ultimate GC. The PEEK endocrowns had the highest fracture resistance, while lithium disilicate had the lowest. Their research also concluded that Panavia V5 showed the lowest leakage degree while Ultimate GC showed the highest [49].
Survivability
Of the 38 selected articles, three were clinical survival studies. They had different follow-up periods, as well as materials that were used.
In an article from 2017, Fages et al. assessed a total of 235 endocrowns and 212 all ceramic crowns for seven years. All restorations were made from Vita Mark II. Concerning preparation design for the endocrowns, the teeth were prepared with at least a 2 mm occlusal reduction and a butt joint. In contrast, the preparation for all the ceramic crowns was made with a 1.5 mm occlusal reduction and right shoulder marginal preparation. All restorations were cemented using the same resin cement (RelyX Unicem, 3M). At the seven-year evaluation, the authors recorded six failures, from which five involved crowns and only one involved an endocrown [53].
In a study from 2020, Munoz-Sanchez et al. studied a cohort of 30 molars restored after pulpotomy with CAD/CAM endocrowns made of IPS e.max CAD or Vita Enamic. The teeth were subjected to clinical and radiological examinations at 1, 6, and 12 months. The study showed no failures from the point of view of the coronal restorations, only regarding the success of the pulpotomy [54].
Tzimas et al. followed 3 cases restored with endocrowns on molars and premolars from resin composite, feldspathic ceramics, and hybrid ceramic The preparation was made using a 1 mm wide butt joint, a 1.2 mm ferrule, and 1–1.5 mm occlusal reduction. We have included this study since it was the only one we found to consider esthetic parameters. After five months, the hybrid resin composite ceramic endocrown suffered a fracture [55].
Esthetics
As mentioned in the previous section, the only study that tackled the esthetic aspect of endocrown restorations was the one carried out by Tzimas et al. They evaluated the color match between the tooth and the endocrown. From the four cases included in this study, two endocrowns made from composite resin were rated as having a “clinically acceptable restoration” at the 20-month recall, and the other two – made out of feldspathic ceramic and hybrid resin composite-ceramic - were rated as “clinically excellent restoration” at the ten months and12 months recalls, respectively [55].
Conclusions
The literature included in this review concludes that endocrowns perform in most cases similarly or even better than other restorations from a mechanical standpoint; they seem to be a promising alternative in restoring endodontically treated teeth with extensive coronal destruction. However, most research is based on in vitro or finite element analysis studies.
Lithium disilicate and resin nanoceramics have been proven as the most successful materials for endocrowns. Still, other options, such as zirconia, PEEK, and composite resins, also show good behavior in particular situations.
Concerning preparation design, there is no “Golden Standard” for endocrowns. The main conclusion is that different materials have different indications depending on a particular given situation when discussing endocrown thickness and endocore length. The same can be stated regarding the type of marginal preparation. The main goal of the clinical approach is to preserve as much sound dental tissue as possible. This approach is also encouraged by the fact that a lower thickness of the endocrowns leads to better mechanical performances. Concerning endocore length, a design that occupies only the pulp chamber has better stress distribution properties than the ones that extend into the root canals.
Thus, further studies should be carried out to confirm the feasibility of endocrowns and the best choice of materials in correlation to the preparation design.
References
- 1.Marchionatti AME, Wandscher VF, Rippe MP, Kaizer OB, Valandro LF. Clinical performance and failure modes of pulpless teeth restored with posts: a systematic review. Braz Oral Res. 2017;31:e64. doi: 10.1590/1807-3107BOR-2017.vol31.0064. [DOI] [PubMed] [Google Scholar]
- 2.Kinney JH, Balooch M, Marshall SJ, Marshall GW, Jr, Weihs TP. Atomic force microscope measurements of the hardness and elasticity of peritubular and intertubular human dentin. J Biomech Eng. 1996;118:133–135. doi: 10.1115/1.2795939. [DOI] [PubMed] [Google Scholar]
- 3.Pjetursson BE, Tan K, Lang NP, Brägger U, Egger M, Zwahlen M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004 Dec;15(6):667–676. doi: 10.1111/j.1600-0501.2004.01120.x. [DOI] [PubMed] [Google Scholar]
- 4.Al-Wahadni A, Gutteridge DL. An in vitro investigation into the effects of retained coronal dentine on the strength of a tooth restored with a cemented post and partial core restoration. Int Endod J. 2002;35:913–918. doi: 10.1046/j.1365-2591.2002.00596.x. [DOI] [PubMed] [Google Scholar]
- 5.Gómez-Polo M, Llidó B, Rivero A, Del Río J, Celemín A. A 10-year retrospective study of the survival rate of teeth restored with metal prefabricated posts versus cast metal posts and cores. J Dent. 2010;38:916–920. doi: 10.1016/j.jdent.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Sarkis-Onofre R, Jacinto RC, Boscato N, Cenci MS, Pereira-Cenci T. Cast metal vs. glass fibre posts: a randomized controlled trial with up to 3 years of follow up. J Dent. 2014;42:582–587. doi: 10.1016/j.jdent.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: a literature review. J Endod. 2004;30:289–301. doi: 10.1097/00004770-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies) Quintessence Int. 2008;39:117–129. [PubMed] [Google Scholar]
- 9.Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63:529–536. doi: 10.1016/0022-3913(90)90070-s. [DOI] [PubMed] [Google Scholar]
- 10.Carlos RB, Thomas Nainan M, Pradhan S, Sharma Roshni, Benjamin S, Rose R. Restoration of endodontically treated molars using all ceramic endocrowns. Case Rep Dent. 2013;2013:210763. doi: 10.1155/2013/210763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Biacchi GR, Mello B, Basting RT. The endocrown: an alternative approach for restoring extensively damaged molars. J Esthet Restor Dent. 2013;25:383–390. doi: 10.1111/jerd.12065. [DOI] [PubMed] [Google Scholar]
- 12.Fages M, Bennasar B. The endocrown: a different type of all-ceramic reconstruction for molars. J Can Dent Assoc. 2013;79:d140. [PubMed] [Google Scholar]
- 13.Zogheib LV, Saavedra Gde S, Cardoso PE, Valera MC, Araújo MA. Resistance to compression of weakened roots subjected to different root reconstruction protocols. J Appl Oral Sci. 2011;19:648–654. doi: 10.1590/S1678-77572011000600018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fernandes AS, Dessai GS. Factors affecting the fracture resistance of post-core reconstructed teeth: a review. Int J Prosthodont. 2001;14:355–363. [PubMed] [Google Scholar]
- 15.Beji Vijayakumar J, Varadan P, Balaji L, Rajan M, Kalaiselvam R, Saeralaathan S, et al. Fracture resistance of resin based and lithium disilicate endocrowns. Which is better? - A systematic review of in-vitro studies. Biomater Investig Dent. 2021;8:104–111. doi: 10.1080/26415275.2021.1932510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al-Dabbagh RA. Survival and success of endocrowns: A systematic review and meta-analysis. J Prosthet Dent. 2021;125:415e1–415.e9. doi: 10.1016/j.prosdent.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Thomas RM, Kelly A, Tagiyeva N, Kanagasingam S. Comparing endocrown restorations on permanent molars and premolars: a systematic review and meta-analysis. Br Dent J. 2020 Nov 12; doi: 10.1038/s41415-020-2279-y. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 18.Sedrez-Porto JA, Rosa WL, da Silva AF, Münchow EA, Pereira-Cenci T. Endocrown restorations: A systematic review and meta-analysis. J Dent. 2016;52:8–14. doi: 10.1016/j.jdent.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 19.Elashmawy Y, Elshahawy W, Seddik M, Aboushelib M. Influence of fatigue loading on fracture resistance of endodontically treated teeth restored with endocrowns. J Prosthodont Res. 2021;65:78–85. doi: 10.2186/jpr.JPOR_2019_485. [DOI] [PubMed] [Google Scholar]
- 20.Kanat-Ertürk B, Saridağ S, Köseler E, Helvacioğlu-Yiğit D, Avcu E, Yildiran-Avcu Y. Fracture strengths of endocrown restorations fabricated with different preparation depths and CAD/CAM materials. Dent Mater J. 2018;37:256–265. doi: 10.4012/dmj.2017-035. [DOI] [PubMed] [Google Scholar]
- 21.Dartora NR, Maurício Moris IC, Poole SF, Bacchi A, Sousa-Neto MD, Silva-Sousa YT, et al. Mechanical behavior of endocrowns fabricated with different CAD-CAM ceramic systems. J Prosthet Dent. 2021;125:117–125. doi: 10.1016/j.prosdent.2019.11.008. [DOI] [PubMed] [Google Scholar]
- 22.Skalskyi V, Makeev V, Stankevych O, Pavlychko R. Features of fracture of prosthetic tooth-endocrown constructions by means of acoustic emission analysis. Dent Mater. 2018;34:e46–e55. doi: 10.1016/j.dental.2018.01.023. [DOI] [PubMed] [Google Scholar]
- 23.El-Damanhoury HM, Haj-Ali RN, Platt JA. Fracture resistance and microleakage of endocrowns utilizing three CAD-CAM blocks. Oper Dent. 2015;40:201–210. doi: 10.2341/13-143-L. [DOI] [PubMed] [Google Scholar]
- 24.Taha D, Spintzyk S, Sabet A, Wahsh M, Salah T. Assessment of marginal adaptation and fracture resistance of endocrown restorations utilizing different machinable blocks subjected to thermomechanical aging. J Esthet Restor Dent. 2018;30:319–328. doi: 10.1111/jerd.12396. [DOI] [PubMed] [Google Scholar]
- 25.Gresnigt MM, Özcan M, van den Houten ML, Schipper L, Cune MS. Fracture strength, failure type and Weibull characteristics of lithium disilicate and multiphase resin composite endocrowns under axial and lateral forces. Dent Mater. 2016;32:607–614. doi: 10.1016/j.dental.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 26.Sağlam G, Cengiz S, Karacaer Ö. Marginal adaptation and fracture strength of endocrowns manufactured with different restorative materials: SEM and mechanical evaluation. Microsc Res Tech. 2021;84:284–290. doi: 10.1002/jemt.23586. [DOI] [PubMed] [Google Scholar]
- 27.Sedrez-Porto JA, Münchow EA, Cenci MS, Pereira-Cenci T. Which materials would account for a better mechanical behavior for direct endocrown restorations? J Mech Behav Biomed Mater. 2020;103:103592. doi: 10.1016/j.jmbbm.2019.103592. [DOI] [PubMed] [Google Scholar]
- 28.Zheng Z, He Y, Ruan W, Ling Z, Zheng C, Gai Y, Yan W. Biomechanical behavior of endocrown restorations with different CAD-CAM materials: A 3D finite element and in vitro analysis. J Prosthet Dent. 2021;125:890–899. doi: 10.1016/j.prosdent.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 29.Turkistani AA, Dimashkieh M, Rayyan M. Fracture resistance of teeth restored with endocrowns: An in vitro study. J Esthet Restor Dent. 2020;32:389–394. doi: 10.1111/jerd.12549. [DOI] [PubMed] [Google Scholar]
- 30.Taha D, Spintzyk S, Schille C, Sabet A, Wahsh M, Salah T, et al. Fracture resistance and failure modes of polymer infiltrated ceramic endocrown restorations with variations in margin design and occlusal thickness. J Prosthodont Res. 2018;62:293–297. doi: 10.1016/j.jpor.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 31.Shin Y, Park S, Park JW, Kim KM, Park YB, Roh BD. Evaluation of the marginal and internal discrepancies of CAD-CAM endocrowns with different cavity depths: An in vitro study. J Prosthet Dent. 2017;117:109–115. doi: 10.1016/j.prosdent.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 32.Hayes A, Duvall N, Wajdowicz M, Roberts H. Effect of Endocrown Pulp Chamber Extension Depth on Molar Fracture Resistance. Oper Dent. 2017;42:327–334. doi: 10.2341/16-097-L. [DOI] [PubMed] [Google Scholar]
- 33.Zhu J, Wang D, Rong Q, Qian J, Wang X. Effect of central retainer shape and abduction angle during preparation of teeth on dentin and cement layer stress distributions in endocrown-restored mandibular molars. Dent Mater J. 2020;39:464–470. doi: 10.4012/dmj.2019-050. [DOI] [PubMed] [Google Scholar]
- 34.de Kuijper MCFM, Cune MS, Tromp Y, Gresnigt MMM. Cyclic loading and loat to failure of lithium disilicate endocrowns: Influence of the restoration extension in the pulp chamber and the enamel outline. J Mech Behav Biomed Mater. 2020 May;105:103670. doi: 10.1016/j.jmbbm.2020.103670. [DOI] [PubMed] [Google Scholar]
- 35.Rocca GT, Sedlakova P, Saratti CM, Sedlacek R, Gregor L, Rizcalla N, et al. Fatigue behavior of resin-modified monolithic CAD-CAM RNC crowns and endocrowns. Dent Mater. 2016;32:e338–e350. doi: 10.1016/j.dental.2016.09.024. [DOI] [PubMed] [Google Scholar]
- 36.Rocca GT, Daher R, Saratti CM, Sedlacek R, Suchy T, Feilzer AJ, et al. Restoration of severely damaged endodontically treated premolars: The influence of the endo-core length on marginal integrity and fatigue resistance of lithium disilicate CAD-CAM ceramic endocrowns. J Dent. 2018;68:41–50. doi: 10.1016/j.jdent.2017.10.011. [DOI] [PubMed] [Google Scholar]
- 37.Pedrollo Lise D, Van Ende A, De Munck J, Umeda Suzuki TY, Cardoso Vieira LC, Van Meerbeek B. Biomechanical behavior of endodontically treated premolars using different preparation designs and CAD/CAM materials. J Dent. 2017;59:54–61. doi: 10.1016/j.jdent.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 38.Kassis C, Khoury P, Mehanna CZ, Baba NZ, Bou Chebel F, Daou M, et al. Effect of Inlays, Onlays and Endocrown Cavity Design Preparation on Fracture Resistance and Fracture Mode of Endodontically Treated Teeth: An In Vitro Study. J Prosthodont. 2021;30:625–631. doi: 10.1111/jopr.13294. [DOI] [PubMed] [Google Scholar]
- 39.Li X, Kang T, Zhan D, Xie J, Guo L. Biomechanical behavior of endocrowns vs fiber post-core-crown vs cast post-core-crown for the restoration of maxillary central incisors with 1 mm and 2 mm ferrule height: A 3D static linear finite element analysis. Medicine (Baltimore) 2020;99:e22648. doi: 10.1097/MD.0000000000022648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Kuijper M, Gresnigt M, van den Houten M, Haumahu D, Schepke U, Cune MS. Fracture Strength of Various Types of Large Direct Composite and Indirect Glass Ceramic Restorations. Oper Dent. 2019;44:433–442. doi: 10.2341/18-111-L. [DOI] [PubMed] [Google Scholar]
- 41.Silva-Sousa AC, Moris ICM, Barbosa AFS, Silva-Sousa YTC, Sousa-Neto MD, Pires CRF, et al. Effect of restorative treatment with endocrown and ferrule on the mechanical behavior of anterior endodontically treated teeth: An in vitro analysis. J Mech Behav Biomed Mater. 2020;112:104019. doi: 10.1016/j.jmbbm.2020.104019. [DOI] [PubMed] [Google Scholar]
- 42.Bankoğlu Güngör M, Turhan Bal B, Yilmaz H, Aydin C, Karakoca Nemli S. Fracture strength of CAD/CAM fabricated lithium disilicate and resin nano ceramic restorations used for endodontically treated teeth. Dent Mater J. 2017;36:135–141. doi: 10.4012/dmj.2016-017. [DOI] [PubMed] [Google Scholar]
- 43.El Ghoul W, Özcan M, Silwadi M, Salameh Z. Fracture resistance and failure modes of endocrowns manufactured with different CAD/CAM materials under axial and lateral loading. J Esthet Restor Dent. 2019;31:378–387. doi: 10.1111/jerd.12486. [DOI] [PubMed] [Google Scholar]
- 44.Dejak B, Młotkowski A. A comparison of mvM stress of inlays, onlays and endocrowns made from various materials and their bonding with molars in a computer simulation of mastication - FEA. Dent Mater. 2020;36:854–864. doi: 10.1016/j.dental.2020.04.007. [DOI] [PubMed] [Google Scholar]
- 45.Hasanzade M, Sahebi M, Zarrati S, Payaminia L, Alikhasi M. Comparative Evaluation of the Internal and Marginal Adaptations of CAD/CAM Endocrowns and Crowns Fabricated from Three Different Materials. Int J Prosthodont. 2021;34:341–347. doi: 10.11607/ijp.6389. [DOI] [PubMed] [Google Scholar]
- 46.Tribst JPM, Dal Piva AMO, de Jager N, Bottino MA, de Kok P, Kleverlaan CJ. Full-Crown Versus Endocrown Approach: A 3D-Analysis of Both Restorations and the Effect of Ferrule and Restoration Material. J Prosthodont. 2021;30:335–344. doi: 10.1111/jopr.13244. [DOI] [PubMed] [Google Scholar]
- 47.Madruga CFL, Tribs JPM, Dal Piva AMO, Bresciani E, Bottino MA, Melo RM. Failure load of fatigued CAD\CAM endocrowns: Material and thickness effect. Dental Materials. 2018;34(Suppl 1):e48. Available from: https://www.sciencedirect.com/science/article/pii/S010956411830856X. [Google Scholar]
- 48.Tribst JPM, Dal Piva AMO, Madruga CFL, Valera MC, Borges ALS, Bresciani E, et al. Endocrown restorations: Influence of dental remnant and restorative material on stress distribution. Dent Mater. 2018;34:1466–1473. doi: 10.1016/j.dental.2018.06.012. [DOI] [PubMed] [Google Scholar]
- 49.Ghajghouj O, Taşar-Faruk S. Evaluation of Fracture Resistance and Microleakage of Endocrowns with Different Intracoronal Depths and Restorative Materials Luted with Various Resin Cements. Materials (Basel) 2019;12:2528. doi: 10.3390/ma12162528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ghoul WE, Özcan M, Tribst JPM, Salameh Z. Fracture resistance, failure mode and stress concentration in a modified endocrown design. Biomater Investig Dent. 2020 Aug 7;7(1):110–119. doi: 10.1080/26415275.2020.1801348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Haralur SB, Alamrey AA, Alshehri SA, Alzahrani DS, Alfarsi M. Effect of different preparation designs and all ceramic materials on fracture strength of molar endocrowns. J Appl Biomater Funct Mater. 2020;18:2280800020947329. doi: 10.1177/2280800020947329. [DOI] [PubMed] [Google Scholar]
- 52.Lin J, Lin Z, Zheng Z. Effect of different restorative crown design and materials on stress distribution in endodontically treated molars: a finite element analysis study. BMC Oral Health. 2020;20:226. doi: 10.1186/s12903-020-01214-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fages M, Raynal J, Tramini P, Cuisinier FJ, Durand JC. Chairside Computer-Aided Design/Computer-Aided Manufacture All-Ceramic Crown and Endocrown Restorations: A 7-Year Survival Rate Study. Int J Prosthodont. 2017;30:556–560. doi: 10.11607/ijp.5132. [DOI] [PubMed] [Google Scholar]
- 54.Munoz-Sanchez ML, Linas N, Decerle N, Nicolas E, Hennequin M, Cousson PY. A Combination of Full Pulpotomy and Chairside CAD/CAM Endocrown to Treat Teeth with Deep Carious Lesions and Pulpitis in a Single Session: A Preliminary Study. Int J Environ Res Public Health. 2020;17:6340. doi: 10.3390/ijerph17176340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tzimas K, Tsiafitsa M, Gerasimou P, Tsitrou E. Endocrown restorations for extensively damaged posterior teeth: clinical performance of three cases. Restor Dent Endod. 2018;43:e38. doi: 10.5395/rde.2018.43.e38. [DOI] [PMC free article] [PubMed] [Google Scholar]