Abstract
BACKGROUND
A limited number of studies have demonstrated that sleeping in the left lateral decubitus (LLD) decreases nocturnal reflux in patients with gastroesophageal reflux disease (GERD) compared to right lateral decubitus (RLD) and supine.
AIM
This systematic review summarizes the association between sleeping in the LLD position and nocturnal reflux in patients with GERD.
METHODS
Studies published up to July 17, 2023, in MEDLINE, EMBASE, and CENTRAL were searched. Eligible studies were randomized and nonrandomized studies assessing the effect of sleeping in LLD compared to RLD and supine in reducing nocturnal reflux in GERD patients. Outcomes include the acid exposure time (AET) (% time in pH<4), acid clearance time (ACT) (in sec/episode), number of reflux episodes, and improvement in N-GSSIQ scores.
RESULTS
Two nonrandomized studies showed decreased AET and ACT in LLD sleep position in comparison to RLD (mean difference [MD] -2.03 [95%CI: -3.62 to -0.45]; -81.84 [95%CI: -127.48 to -36.20], respectively) and supine position (MD -2.71 [95%CI: -4.34 to -1.09]; -74.47 [95%CI: -116.26 to -32.69], respectively). There was no difference in AET and ACT between RLD sleep position and supine. Furthermore, one randomized controlled trial investigating the use of electronic sleep positional therapy, which increased the duration of LLD sleep and decreased the duration of RLD sleep compared to sham, showed nocturnal symptoms improvement (improved N-GSSIQ score, increased reflux-free nights, and resolution of nocturnal reflux symptoms).
CONCLUSION
Current evidence suggests that sleeping on the left side could reduce nocturnal reflux and improve GERD-related quality of life, therefore warranting interventions that promote LLD sleep position.
Keywords: Gastroesophageal reflux disease, Left lateral decubitus, Sleep position, Systematic review
Core Tip: This systematic review summarizes the association between left lateral decubitus (LLD) sleep position and nocturnal reflux in GERD patients. Overall, sleeping in the LLD position demonstrated significantly decreased acid exposure time and acid clearance time compared to right lateral decubitus (RLD) and supine. Furthermore, increased LLD sleep was shown to improve nocturnal symptoms, as evidenced by a randomized controlled trial using sleep positional therapy to promote LLD sleep and reduce RLD sleep. The above findings suggest that LLD sleep benefits GERD patients who experience nocturnal symptoms and warrants interventions that promote LLD sleep position.
INTRODUCTION
Gastroesophageal reflux disease (GERD) is a global medical condition characterized by the movement of gastric contents into the esophagus, thus causing multiple symptoms and sequelae[1]. GERD patients experience symptoms throughout the day; however, those who experience nocturnal GERD symptoms reported having sleep disturbances and impaired quality of life compared to subjects who only reported daytime symptoms[2]. Despite no clear consensus on the definition of nocturnal GERD, most GERD individuals report nocturnal GERD symptoms such as night-time reflux (52%-79%)[3]. Furthermore, GERD was associated with sleep disturbances (OR 1.48; 95%CI: 2.7-3.7), and those who suffer from nocturnal GERD reported decreased productivity in the subsequent day, ultimately affecting their quality of life[3,4].
With the advent of superior pharmacological treatment for managing GERD, lifestyle modifications, which are cheaper, become much more underemphasized. The 2022 American College of Gastroenterologists (ACG) guidelines recommended left lateral decubitus (LLD) sleeping position as one of the lifestyle modifications of GERD management with unequivocal evidence[5]. However, although it is common practice for physicians to educate GERD patients to sleep with the head elevated to prevent nocturnal acid reflux, there is a lack of interest in recommending that patients sleep on the left side. Recent evidence has shown that sleeping with the head elevated and lying to the left side reduced gastric acid exposure and improved nocturnal GERD symptoms and [6]. This improvement can be explained by the pathophysiology and anatomy of the faulty gastroesophageal junction in GERD patients. Lying on the right side would position the esophagus inferior to the gastroesophageal junction, further precipitating reflux and promoting longer acid clearance time[7,8]. This systematic review aims to evaluate and consolidate accumulating evidence regarding the effect of LLD sleep position on nocturnal symptoms in GERD patients.
MATERIALS AND METHODS
This systematic review and meta-analysis was written based on the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guideline (Supplementary Table 1). Before starting the review, the protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO CRD42022369609).
Search strategy
We searched three electronic literature databases: MEDLINE (Ovid interface), EMBASE (Ovid interface), and CENTRAL (Cochrane Library). Studies published from database conception until July 17, 2023, were retrieved and assessed for inclusion in this systematic review. Additional studies were also sought through hand-searching references and study citations from relevant studies. The search strategies were constructed uniquely for each database and were primarily based on the following key points: “Gastroesophageal Reflux Disease,” “Sleep Position,” and “Left Lateral Decubitus” (Supplementary Table 2).
Eligibility criteria
Randomized controlled trials (RCTs) and observational studies that include adult patients aged 18 years and older with GERD with data comparing the effect of Left Lateral Decubitus (LLD) to supine and/or Right Lateral Decubitus (RLD) sleeping position were eligible for inclusion.
Study selection and data extraction
Three independent reviewers (EL, MPW, and BRA), which were done in pairs, were responsible for the study selection, data extraction, and quality assessment of the included studies. All studies retrieved from the electronic databases were imported into Endnote X20. Duplicate studies were removed, and the unique studies were screened based on the titles and abstracts. Subsequently, full texts of the selected studies were reviewed for potential inclusion in this systematic review. Essential information was extracted using an Excel form, which included the study identification (comprised of first author and year of publication), inclusion and exclusion criteria for study subjects, methods for determining sleep positions, baseline characteristics of study participants, and outcomes of interest. The outcomes of interest were: Nocturnal GERD Symptom Severity and Impact Questionnaire (N-GSSIQ) scores, GERD Health-Related Quality of Life Questionnaire, Reflux Disease Questionnaire (RDQ), Pittsburgh Sleep Quality Index (PSQI), Work Productivity and Activity Impairment (WPAI), Position Change Reflux Event, Acid Exposure Time (AET), Acid Clearance Time (ACT), and Number of Reflux Episodes. For RCTs, only the intention-to-treat outcome data were used for comparative analysis. Any disagreements between the two reviewers were resolved through independent review from a third reviewer.
Quality assessment
The Newcastle-Ottawa Quality Assessment Scale for cross-sectional studies was used to assess the quality of included observational studies. Meanwhile, Cochrane’s Risk of Bias 2 (RoB2) tool was used to rate the risk of bias of the included RCTs. Any disagreements between the two reviewers were arbitrated by an independent review of the third reviewer.
Data synthesis
Results from the included studies were summarized in tabular format. Quantitative data were included in the meta-analysis if data were reported by at least two studies using the same study design (observational study or RCT). Meta-analysis was done using the “meta” package of the R software (Vienne, Austria). The fixed “common” effect model was used to pool the data to give more weight to studies with more sample sizes, considering the low number of studies included in the review. The overall mean difference (MD) and its 95% confidence interval were reported for studies that compared continuous outcomes. Between-study heterogeneity was assessed using the I2 and the Cochran-Q. A significant result was determined if P < 0.05. Publication bias was not considered due to the paucity of studies analyzed (k < 10).
RESULTS
Study selection and baseline characteristics
A total of 2815 records were identified from a database search, and after screening based on the title and abstract, 24 full-text articles were reviewed for eligibility (Figure 1). Three articles met the inclusion criteria[7-9], and the reasons for full-text article exclusion were generally abstract-only publications (n = 8), wrong study design (n = 4), and wrong PICO (n = 9). All studies have included only GERD patients as the study population; however, two studies were cross-sectional studies[7,8] which evaluated the impact of spontaneous sleep positions and nocturnal reflux symptoms, while the remaining one study was a randomized, sham-controlled trial[9] which assessed the effect of a sleep positional therapy device intervention used to promote LLD sleeping and nocturnal reflux symptoms (Supplementary Table 3). Two studies were conducted in the Netherlands[8,9], while only one was in the United States of America[7]. The baseline characteristics of study participants in each study were presented in Table 1. In brief, the majority of included GERD patients were female, overweight with a mean BMI range of 25.1-26.7 kg/m2, had hiatal hernia (mean % of 40.6-56.1), and used acid suppressive drugs (either PPI, H2RA, or antacids).
Figure 1.
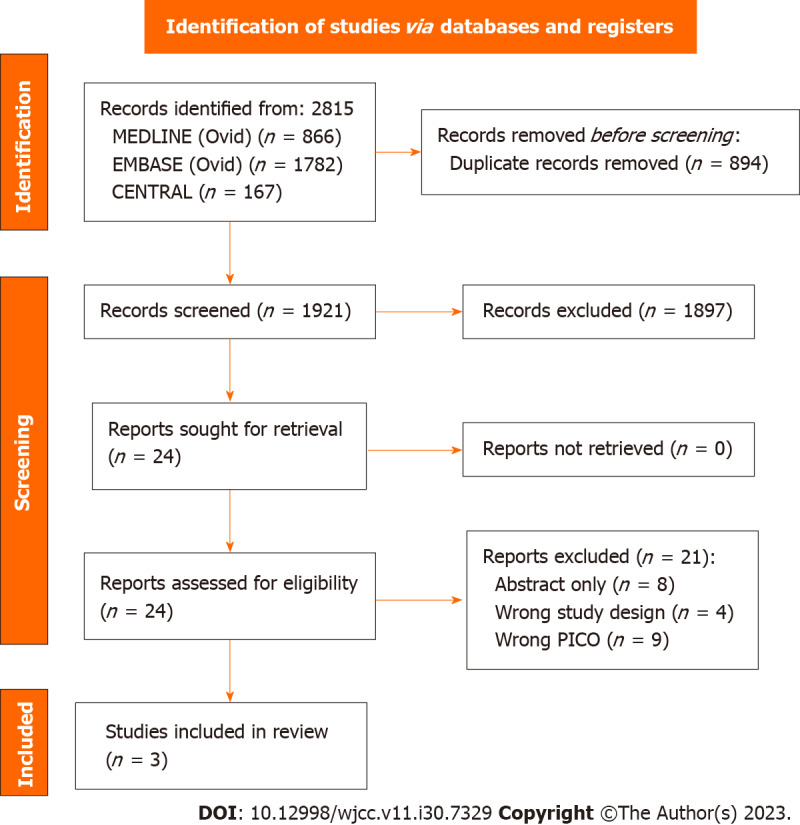
PRISMA 2020 flow diagram for study selection.
Table 1.
Baseline characteristics of patients included in the study
|
Study identifier
|
Khoury et al[7], 1999
|
Schuitenmaker et al[8], 2022
|
Schuitenmaker et al[9], 2022
|
|
| Study design | Cross-sectional | Cross-sectional | Randomized Controlled Trial | |
| Study location | United States of America | Netherlands | Netherlands | |
| Groups | N/A | N/A | Intervention | Sham |
| Number of subject | 10 | 57 | 50 | 50 |
| Age (yr) mean ± SD/(range) | 47.6 (30-67) | 48.9 ± 16.1 | 52.0 ± 12.0 | 52.5 ± 12.2 |
| Sex ratio (M/F) | 7/3 | 26/31 | 16/34 | 21/29 |
| BMI kg/m2, mean ± SD | NR | 26.7 ± 4.6 | 25.1 ± 4.3 | 26.3 ± 4.1 |
| Smoking N (%) | NR | NR | 4 (8) | 4 (8) |
| Disease severity, N (%) | NR | Grade A RE: 10 (17.5); Grade B RE: 11 (19.3); Grade C RE: 2 (3.5); NERD: 16 (29.1); Esophageal hypersensitivity: 9 (16.4); Functional heartburn: 7 (12.7); Unknown: 2 (3.5) | NR | NR |
| Diaphgramatic hernia, N (%) | NR | 32 (56.1) with mean size 3.0 ± 1.3 | Total: 32; Yes: 13 (40.6); No: 13 (40.6); Unknown: 6 (18.8) | Total 30; Yes: 13 (43.3); No: 15 (50.0); Unknown: 2 (6.7) |
| Medication use, N (%) | None | PPI and H2RA: 9 (15.8); PPI: 37 (64.9); H2RA: 1 (1.8); None: 10 (17.5) | PPI: 20 (40); H2RA: 2 (4); Antacids: 33 (66) | PPI: 27 (54); H2RA: 3 (6); Antacids: 27 (54) |
| GERDQ score, mean ± SD | NR | NR | 11.9 ± 2.0 | 12.2 ± 2.0 |
GERDQ: GERD questionnaire; H2RA: Histamine 2 receptor antagonist; GERD: Gastroesophageal reflux disease; M/F: Male/Female; N/A: Not applicable; NR: Not reported; PPI: Proton pump inhibitor; RE: Reflux esophagitis; SD: Standard deviation.
Quality assessment and risk of bias
The overall quality assessment and risk of bias of included studies are presented in Supplementary Tables 4 and 5. Overall, the quality assessment of cross-sectional studies was moderate-to-high quality (scores of 6 and 9), while the included randomized controlled trial had a low risk of bias.
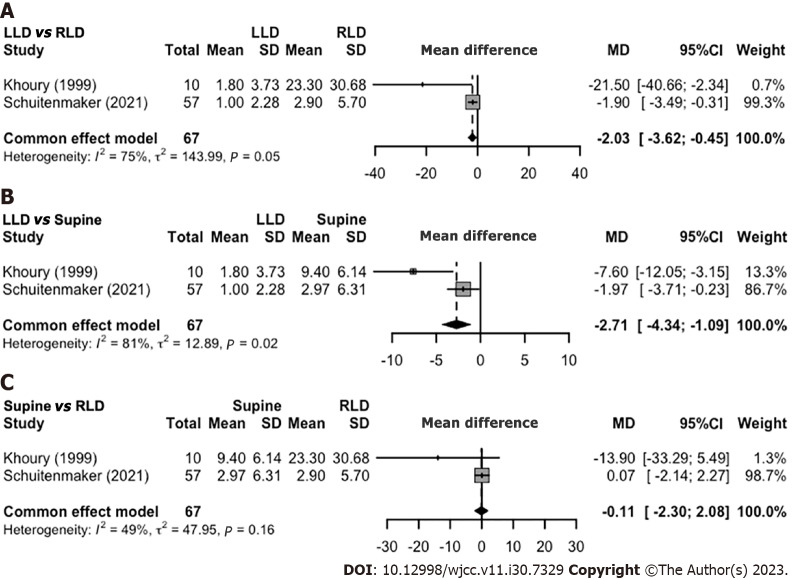
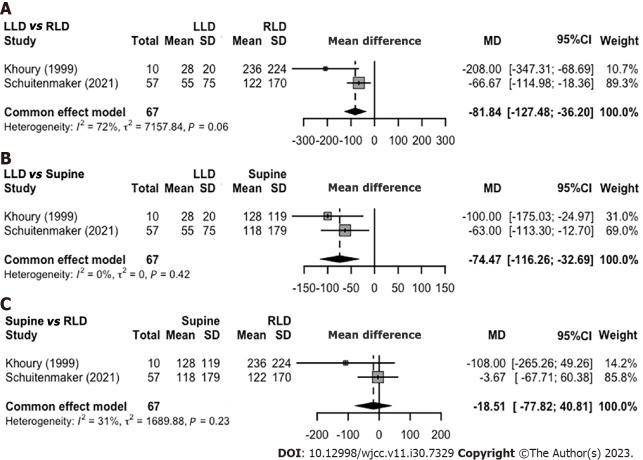
Spontaneous sleep position and nocturnal reflux symptoms
Two cross-sectional studies, comprising a total of 67 patients, assessed the effect of spontaneous sleep position and nocturnal reflux symptoms[7,8]. Three major sleeping positions measured were LLD, RLD, and supine (not in order of duration). Sleeping in LLD was shown to have significantly decreased AET when compared to sleeping in RLD (pooled MD -2.03% [95%CI: -3.62% to -0.45%]) and supine position (pooled MD -2.71 [95%CI: -4.34% to -1.09%]) (Figure 2). Meanwhile, no difference in AET was observed when comparing sleeping in supine and RLD (pooled MD -0.11 [95%CI: -2.30% to 2.08%]). As for the ACT, sleeping in LLD was shown to reduce the duration of ACT in sec/episode compared to sleeping in RLD (pooled MD -81.84 [95%CI: -127.48 to -36.20]) and supine position (pooled MD -74.47 [95%CI: -116.26 to -32.69]) (Figure 3). Similar to AET, no significant difference was observed in the ACT between supine and RLD (pooled MD -18.51 [95%CI: -77.82 to 40.81]).
Figure 2.
Spontaneous sleep position and nocturnal reflux symptoms. A: Acid exposure time (% time pH<4) in left lateral decubitus (LLD) vs right lateral decubitus (RLD); B: LLD vs supine; C: Supine vs RLD. LLD: Left lateral decubitus; MD: Mean difference; RLD: Right lateral decubitus; SD: Standard deviation; 95%-CI: 95% confidence interval.
Figure 3.
Spontaneous sleep position and nocturnal reflux symptoms. A: Acid clearance time (sec/episode) in left lateral decubitus (LLD) vs right lateral decubitus (RLD); B: LLD vs Supine; C: Supine vs RLD. LLD: Left lateral decubitus; MD: Mean difference; RLD: Right lateral decubitus; SD: Standard deviation; 95%-CI: 95% confidence interval.
Khoury et al[7] also demonstrated a decrease in position change reflux events and the number of reflux episodes per hour in the LLD group compared to the supine and RLD groups (60% vs 90% vs 100%, and 1.2 [0-3.0] vs 2.1 [1.6-3.0] vs 1.5 [0.9-2.4], respectively). Additionally, Schuitenmaker et al[8] showed a decreased total number of reflux episodes per sleep position in the LLD group compared to the supine and RLD groups (80 vs 102 vs 109).
Sleep positional therapy device and nocturnal reflux symptoms
Schuitenmaker et al[9] performed a randomized, sham-controlled trial comparing nocturnal reflux symptoms in patients randomized to an electronic sleep positional therapy device, which promotes sleeping in the LLD position and to the sham device. The study reported similar baseline characteristics and sleep positions between participants randomized to the intervention and sham groups and demonstrated significantly increased duration of LLD sleep position (60.9% ± 16.4% vs 38.5% ± 14.3%) and decreased time of RLD sleep position (2.2% ± 2.9% vs 23.5% ± 12.3%) in the intervention group compared to the sham group. Overall, those randomized in the intervention group had significantly greater proportions of participants with ≥ 50% reduction in the N-GSSIQ score, reflux-free nights, and resolution of nocturnal reflux complaints, and improved nocturnal symptoms as shown by a lower total number of reflux symptoms, total N-GSSIQ score, especially the nocturnal GERD symptom severity subscale, and RDQ score after two weeks of treatment. However, the two groups did not differ in the global score of the PSQI questionnaire and the WPAI-GERD-sleep components.
DISCUSSION
Our meta-analysis reported that the LLD sleep position significantly reduces acid exposure and clearance (AET and ACT) in patients with GERD compared to other sleeping positions, such as supine and RLD. Patients were also found to have fewer reflux events in the LLD position compared to supine and RLD. Meanwhile, an RCT evaluating a sleep therapy device that prompted patients to sleep more often in the LLD and less in the RLD position demonstrated superior effects in reducing N-GSSIQ score, nocturnal reflux symptoms, and RDQ score[9].
Anatomically, the relative position of the esophagus in relation to the stomach changes according to sleep position changes. Previous studies have shown that sleeping in the RLD position induced more heartburn and reflux episodes than in other positions, as the stomach becomes relatively superior to the esophagus[10-12]. In conditions of relaxation or weakening of the lower esophageal sphincter, the RLD position promotes more flow of stomach contents into the esophagus, thus causing reflux. On the contrary, sleeping in the LLD position will position the esophagus relatively superior to the stomach, lowering the likelihood of gastric content reflux back to the esophagus[8]. However, some reflux can still occur during the LLD sleep position, which is usually composed of gas-only or a mixture of gas and liquid reflux[13].
The two observational studies did not explore the effects of LLD sleep position on GERD-related quality of life (QoL) endpoints, such as any nocturnal GERD symptoms and their impact. However, it is understandable since discriminating nocturnal GERD symptoms based on specific sleeping positions from the overall sleep duration is difficult. Besides, maintaining a specific sleep position from the overall sleep duration is difficult due to the dynamic changes in position throughout sleep[14]. These hypothesis-generating studies suggested that decreased acid exposure and clearance in LLD sleep position compared to supine and/or RLD could be translated to less damage to the esophagus and fewer nocturnal symptoms of GERD. The RCT by Schuitenmaker et al[9] was able to confirm this hypothesis by reporting a significant increase in reflux-free nights and a significantly larger proportion of patients with lower post-intervention N-GSSIQ and RDQ scores.
However, interestingly, Schuitenmaker et al[9] reported no statistically significant difference in the PSQI score and WPAI-GERD questionnaires. A possible explanation would be that the duration of intervention used in the trial was only short-term (2 weeks). Thus, there is an excellent possibility that the short duration of the intervention is not adequate to influence those indicators, especially considering that the PSQI questionnaire was initially created to assess sleep quality in one month[15]. Meanwhile, the WPAI-GERD questionnaire was developed to measure a reduction in productivity caused by GERD, a distal endpoint to GERD-QoL[16]. Thus, the nature of the WPAI-GERD questionnaire could allow the outcome to be diluted by other extraneous factors aside from nocturnal symptoms, such as the effect of daytime GERD. In addition, symptoms are neither sensitive nor specific for quantifying GERD, and we acknowledge that pH-impedance monitoring would serve as an objective evaluation for evidence of GERD.
As of the writing of this systematic review and meta-analysis, this was the first study to summarize the results of published studies that explored the promising effect of LLD sleep position on improving nocturnal GERD symptoms. LLD sleep position not only alters the biological aspect of nocturnal GERD, such as acid exposure and clearance (AET and ACT), but was also reported to improve nocturnal GERD symptoms. However, we acknowledge the paucity of evidence exploring the benefits of LLD compared to supine and/or RLD sleep positions and that studies only enrolled a small number of patients. Furthermore, sleep positional therapy will likely be needed to promote LLD sleep, considering that relying solely on recommendations for patients to sleep in LLD may not produce any beneficial effect. Therefore, despite current evidence suggesting superior effects of sleeping in LLD compared to other sleep positions for GERD patients in reducing nocturnal GERD symptoms, more studies are needed to replicate and confirm the potentially beneficial effects of this lifestyle intervention to promote improved nocturnal symptoms and other GERD-related QoL in GERD patients. In addition, studies should try to define which GERD phenotypes will most benefit from LLD sleep position.
CONCLUSION
This systematic review with meta-analysis supported the hypothesis that LLD sleep positions were superior to other sleep positions in decreasing acid exposure, improving acid clearance, and subsequently improving nocturnal GERD symptoms. Ultimately, combining the LLD sleep position with head elevation could improve nocturnal reflux and improve patient QoL, though this needs further exploration. However, due to the very limited number of studies with limited subjects available in the literature, more studies should reassess and confirm this finding and its implementation in actual clinical practice.
ARTICLE HIGHLIGHTS
Research background
Sleeping in the left lateral decubitus (LLD) has been shown to decrease nocturnal reflux in patients with gastroesophageal reflux disease (GERD) compared to right lateral decubitus (RLD) sleep position and supine.
Research motivation
This is the first systematic review that summarizes the association between sleeping in the LLD position and nocturnal reflux in patients with GERD.
Research objectives
The study aimed to summarize the evidence on sleep position for treating nocturnal reflux and GERD symptoms in GERD patients.
Research methods
We searched for randomized and nonrandomized evidence assessing LLD sleep position in comparison to RLD and supine position in reducing nocturnal reflux in patients with GERD. A meta-analysis was done to pool outcomes such as acid exposure time (AET) and acid clearance time (ACT).
Research results
Two nonrandomized studies showed decreased AET and ACT in LLD sleep position in comparison to RLD and supine. There was no difference in AET and ACT between RLD sleep position and supine. A randomized controlled trial investigating the use of electronic sleep positional therapy, which increased the duration of LLD sleep and decreased the duration of RLD sleep compared to sham, showed nocturnal symptom improvements.
Research conclusions
Current evidence suggests that sleeping on the left side could reduce nocturnal reflux and improve GERD-related quality of life, therefore warranting interventions that promote LLD sleep position.
Research perspectives
LLD sleep should be recommended for GERD patients, especially those who experience nocturnal symptoms. Studies should look into the practicality and feasibility of using an electronic sleep positional therapy and whether patients can tolerate it in real life.
Footnotes
Conflict-of-interest statement: All authors have no conflict of interest to declare.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2020 Checklist, and the manuscript was prepared and revised according to the PRISMA 2020 Checklist.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: August 7, 2023
First decision: September 14, 2023
Article in press: October 8, 2023
Specialty type: Gastroenterology & hepatology
Country/Territory of origin: Indonesia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Contini S, Italy S-Editor: Liu JH L-Editor: A P-Editor: Yu HG
Contributor Information
Daniel Martin Simadibrata, Department of Internal Medicine, Faculty of Medicine Universitas Indonesia, Jakarta 10430, Indonesia; Nuffield Department of Population Health, University of Oxford, Oxford OX3 7LF, United Kingdom; Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, MN 55905, United States.
Elvira Lesmana, Department of Internal Medicine, Faculty of Medicine Universitas Indonesia, Jakarta 10430, Indonesia.
Bagus Ramasha Amangku, Department of Internal Medicine, Faculty of Medicine Universitas Indonesia, Jakarta 10430, Indonesia.
Muhammad Prasetio Wardoyo, Department of Internal Medicine, Faculty of Medicine Universitas Indonesia, Jakarta 10430, Indonesia.
Marcellus Simadibrata, Division of Gastroenterology, Department of Internal Medicine, Faculty of Medicine Universitas Indonesia, Jakarta 10430, Indonesia. prof.marcellus.s@gmail.com.
References
- 1.Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430–440. doi: 10.1136/gutjnl-2016-313589. [DOI] [PubMed] [Google Scholar]
- 2.Mody R, Bolge SC, Kannan H, Fass R. Effects of gastroesophageal reflux disease on sleep and outcomes. Clin Gastroenterol Hepatol. 2009;7:953–959. doi: 10.1016/j.cgh.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 3.Shibli F, Skeans J, Yamasaki T, Fass R. Nocturnal Gastroesophageal Reflux Disease (GERD) and Sleep: An Important Relationship That Is Commonly Overlooked. J Clin Gastroenterol. 2020;54:663–674. doi: 10.1097/MCG.0000000000001382. [DOI] [PubMed] [Google Scholar]
- 4.Hyun MK, Baek Y, Lee S. Association between digestive symptoms and sleep disturbance: a cross-sectional community-based study. BMC Gastroenterol. 2019;19:34. doi: 10.1186/s12876-019-0945-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2022;117:27–56. doi: 10.14309/ajg.0000000000001538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan BA, Sodhi JS, Zargar SA, Javid G, Yattoo GN, Shah A, Gulzar GM, Khan MA. Effect of bed head elevation during sleep in symptomatic patients of nocturnal gastroesophageal reflux. J Gastroenterol Hepatol. 2012;27:1078–1082. doi: 10.1111/j.1440-1746.2011.06968.x. [DOI] [PubMed] [Google Scholar]
- 7.Khoury RM, Camacho-Lobato L, Katz PO, Mohiuddin MA, Castell DO. Influence of spontaneous sleep positions on nighttime recumbent reflux in patients with gastroesophageal reflux disease. Am J Gastroenterol. 1999;94:2069–2073. doi: 10.1111/j.1572-0241.1999.01279.x. [DOI] [PubMed] [Google Scholar]
- 8.Schuitenmaker JM, van Dijk M, Oude Nijhuis RAB, Smout AJPM, Bredenoord AJ. Associations Between Sleep Position and Nocturnal Gastroesophageal Reflux: A Study Using Concurrent Monitoring of Sleep Position and Esophageal pH and Impedance. Am J Gastroenterol. 2022;117:346–351. doi: 10.14309/ajg.0000000000001588. [DOI] [PubMed] [Google Scholar]
- 9.Schuitenmaker JM, Kuipers T, Oude Nijhuis RAB, Schijven MP, Smout AJPM, Fockens P, Bredenoord AJ. Sleep Positional Therapy for Nocturnal Gastroesophageal Reflux: A Double-Blind, Randomized, Sham-Controlled Trial. Clin Gastroenterol Hepatol. 2022;20:2753–2762.e2. doi: 10.1016/j.cgh.2022.02.058. [DOI] [PubMed] [Google Scholar]
- 10.Loots C, Smits M, Omari T, Bennink R, Benninga M, van Wijk M. Effect of lateral positioning on gastroesophageal reflux (GER) and underlying mechanisms in GER disease (GERD) patients and healthy controls. Neurogastroenterol Motil. 2013;25:222–229, e161. doi: 10.1111/nmo.12042. [DOI] [PubMed] [Google Scholar]
- 11.Katz LC, Just R, Castell DO. Body position affects recumbent postprandial reflux. J Clin Gastroenterol. 1994;18:280–283. doi: 10.1097/00004836-199406000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Shay SS, Conwell DL, Mehindru V, Hertz B. The effect of posture on gastroesophageal reflux event frequency and composition during fasting. Am J Gastroenterol. 1996;91:54–60. [PubMed] [Google Scholar]
- 13.Shay SS, Lopez R. Impedance monitoring shows that posture and a meal influence gastro-oesophageal reflux composition and frequency. Neurogastroenterol Motil. 2007;19:94–102. doi: 10.1111/j.1365-2982.2006.00860.x. [DOI] [PubMed] [Google Scholar]
- 14.Zhang Y, Xiao A, Zheng T, Xiao H, Huang R. The Relationship between Sleeping Position and Sleep Quality: A Flexible Sensor-Based Study. Sensors (Basel) 2022;22 doi: 10.3390/s22166220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 16.Wahlqvist P, Carlsson J, Stålhammar NO, Wiklund I. Validity of a Work Productivity and Activity Impairment questionnaire for patients with symptoms of gastro-esophageal reflux disease (WPAI-GERD)--results from a cross-sectional study. Value Health. 2002;5:106–113. doi: 10.1046/j.1524-4733.2002.52101.x. [DOI] [PubMed] [Google Scholar]