Abstract
This integrative review assessed the factors influencing cancer patients' caregivers’ burden and quality of life (QoL). Relevant studies were retrieved from five electronic databases and screened. After systematic screening by title, abstract, and full text, the review included 15 studies published between 2000 and 2022 and used an interpretive thematic synthesis design for analysis. Age (older), sex (male), high work requirements, relationships with patients, low-income levels, high subjective stress, patient dependency level, and trait anxiety were significantly associated with higher caregiver burden. Factors associated with the low QoL of caregivers were age (less than 35 years), caregiving role (more responsibility), relationship with patients (first-degree relative), low income, living in the same home with the patient, and higher social and family responsibilities. A moderate negative correlation (n = 6) was identified between the sum of the QoL scores and the burden. Future research should be integrated into identifying appropriate means to support caregivers of patients with chronic diseases, including cancer by segregating interventions to target specific caregiver populations.
Keywords: Caregiver burden, Quality of life, Oncology, Review
1. Introduction
Cancer and its treatment adversely affect patients' physical and psychological well-being [1]. This is because cancer is responsible for one out of every six deaths globally and is the second most common cause after cardiovascular-related deaths [1,2]. The disease burden is not limited to patients alone but significant family members, especially the informal/family caregivers. Family caregivers support patients financially, physically, emotionally, and socially and take on many responsibilities to meet patients' needs [3,4]. The role of family caregivers in cancer management is, therefore, critical in the overall prognosis of the disease [[4], [5], [6]]. Cancer caregivers are prone to critical challenges in their personal life, and the role of caregiving may make these burdens worse [7]. The impact of cancer caregiving is even worse as some family caregivers lose their jobs and source of livelihood during the period of informal caregiving [8].
The caregiving role, especially to cancer patients, can be a source of worry and difficulty as it is speculated that they face an increased burden and have a lower quality of life (QoL) [7,9,10]. The caregiving burden among cancer patients is mostly related to uncertainty in diagnosis, longer duration of illness, repeated acute phases of the disease, doubtfulness of prognosis, longer duration of treatment requirement, repeated hospital admissions, and increasing experiences of side-effects of polyvalent treatment options [6,10,11]. In low and middle-income countries like Bangladesh informal caregivers regularly stay in hospitals with high responsibilities, especially during acute episodes of the disease [12]. The repeated and prolonged admission periods for cancer patients in developing countries may burden family caregivers more than in other patients or among patients from developed countries [12]. Caregivers of highly symptomatic cancer patients are more prone to psychological, physical, financial, and social burdens [2,13]. The influence of cancer patients’ caregiver burden can be devastating and sometimes increase the need for additional care and support for both the patient and the caregiver [14,15]. The burden of caregiving also could decrease caregivers' social relationships, and this change can lead to psychological problems, and its consequences result in a deterioration of QoL [7,10].
Although there are many indications that cancer patients' family caregivers can experience burden and even develop physical symptoms, little is known about the influencing factors [7,10,16]. Diverse reviews are concerned about the care burden among caregivers of patients with dementia [17,18], stroke [19], mental illness [20], epilepsy [21], older adults [15], pancreatic cancer [22], or the burden faced by breast cancer caregivers [23]. Other reviews focused on only the QoL of caregivers of cancer patients [22,[24], [25], [26]]. However, limited reviews have assessed the factors associated with the burden and the QoL among cancer patient caregivers. This paper assessed the factors influencing the burden and the QoL of caregivers of cancer patients. Identifying, outlining, and integrating the factors associated with cancer patients' caregivers’ burden and QoL will be critical for policy formulation to mitigate those factors and improve the lifes of both patients and caregivers.
2. Methods
2.1. Study design
This integrative review discovered critical concepts related to cancer patients' caregivers' burden and the QoL. Integrative reviews usually focus on sustaining a research area and providing more comprehensive coverage of a particular field [[27], [28], [29]] by identifying important factors that influence health. The proposed six stages of the integrative review process involve: preparing the guiding question, searching or sampling the literature, data collection, critical analysis of the studies including discussion of results, and presentation of the integrative review [27]. Therefore, we adopted this design to describe the factors associated with burden on the QoL of cancer patients’ caregivers using these proposed stages.
2.2. Search strategy
This study was performed and reported based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [30,31]. Relevant studies were retrieved from five electronic databases: Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, Medline Ovid, and Web of Science. The search in this integrative review adhered to the Population, Concept, and Context (PCC) framework. The search strategy integrated terminologies for population (caregiver), concept (Burden, quality of life), and context (cancer patients). The synonyms were obtained using MeSH-controlled vocabulary in Medline Ovid, CINAHL, and Emtree words in Embase. The primary search words were first created using scoping search techniques in Medline Ovid and subsequently transferred and adjusted based on the appropriate use of Boolean operators in each database. The search was performed from 2020 until July 21, 2022.
2.3. Study selection
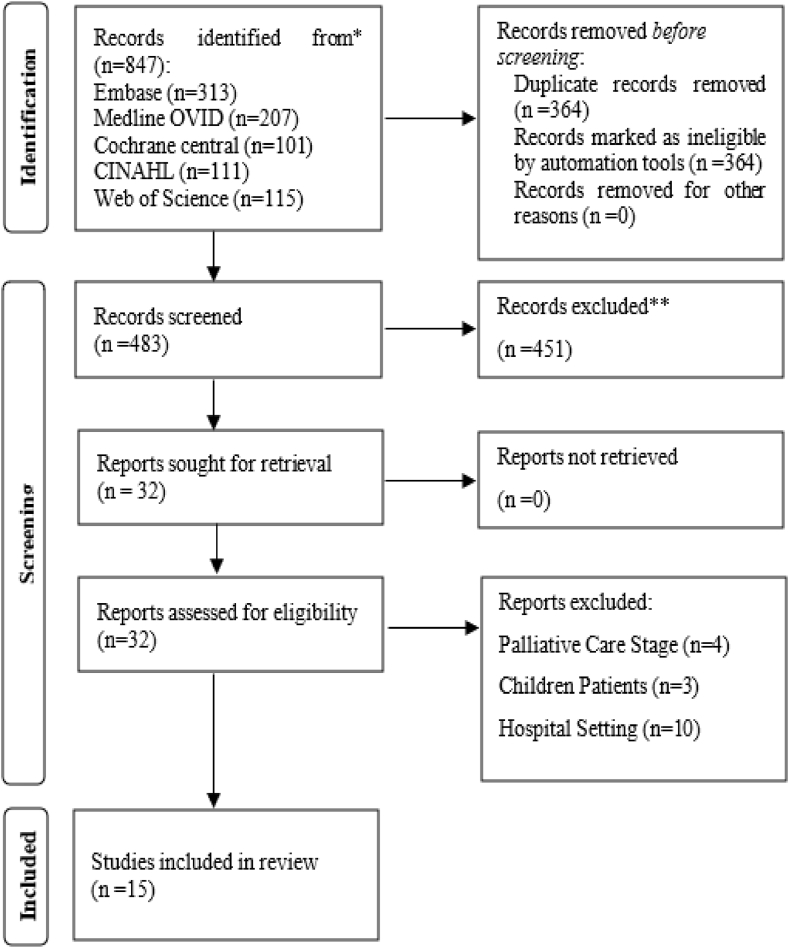
The findings from the database search (847 articles) were integrated through the EndNote 20 reference manager, and duplicates were deleted automatically and manually verified. Two authors (JA and MN) independently examined the retrieved search outcome (483 articles) by titles and abstracts. The selected abstracts (32) were retrieved as full articles for further screening based on predetermined criteria. The screening process was verified by one of the authors (KDK). The criteria included all types of designs involving experimental, observational, and qualitative studies. The population was caregivers of cancer patients. The exclusion criteria were studies describing the stages of palliative care, child patients involving parent-child caregiving relations, and those assessing the caregiver burden of the acute stages of cancer in the hospital setting. This exclusion criteria was used because this study sought to identify the factors that are associated with caregiver burden and its related influence on the QoL of informal caregivers of cancer patients. By consensus, the authors believed that the factors could be assessed through the stated inclusion and exclusion criteria. During the screening and selection, discrepancies were resolved by discussion until consensus in several meetings with the two other authors (KDK and AI). Finally, there were 15 articles selected as eligible for this study. The screening and selection process is shown in Fig. 1 in a PRISMA flow diagram.
Fig. 1.
Figure: PRISMA, flow chart for article selection.
2.4. Quality appraisal
We used the Mixed Methods Appraisal tool (MMAT) to assess each study. Two authors (KDK, and AI) evaluated the articles separately. In instances where the two authors disagreed on the point of assessment, it was discussed until a consensus. The MMAT tool can be used to assess qualitative, quantitative, and mixed methods designs. This made it suitable for this study because of its multifaceted ability to assess multiple designs concomitantly. In using the MMAT, there are two critical screening questions before the appraisal. The screening questions are (A) the presence of clear research questions and (B) collected data addressing the research question. In this review, all the studies met these fundamental criteria. The MMAT allows that when studies meet these fundamental criteria, the appraisal of such a study can progress with the specific designated design section [32].
In this study, one study was quantitative non-randomized, and fourteen studies were quantitative descriptive. The quantitative non-randomized section assessed 1) are the participants representative of the target population, 2) are the measurements appropriate regarding both the outcome and intervention or exposure, 3) are there complete outcome data, 4) are the confounders accounted for in the design analysis, and 5) during the study period, is the intervention administered as an intended. Only one study [33] was assessed under this category. The study met the criteria except for one portion concerned that the confounders were not accounted for in the designed analysis. In the quantitative descriptive segment, the criteria included 1) Is the sampling strategy relevant to address the research question? 2) Is the sample representative of the target population? 3) Are the measurements appropriate? 4) Is the risk of nonresponse bias low? and 5) Is statistical analysis appropriate to answer the research question? All the remaining (n = 14) studies were assessed under this category. The results showed an affirmative for all the evaluation criteria for this segment.
2.5. Data extraction and analysis
Two authors performed data extraction based on a predetermined developed matrix (JA and MN). Two other authors (KDK and AI) further verified the extracted data to ensure that relevant information regarding caregiver burden and QoL was extracted. The information extracted using the matrix includes study characteristics (country, design, samples, analysis), caregiver characteristics (relationship to patients, gender, age), factors associated with caregiver burden, and QoL. The two data extractors compared results, and when they disagreed, the other authors re-examined and resolved discrepancies through discussions until consensus.
The interpretative thematic synthesis design was used for analysis [34]. The key findings were first transformed into qualitative statements. This is because, in this integrative review, there was high heterogeneity in the various studies as they used varied sample sizes, intervention approaches, designs, and inconsistent measurement tools. Consequently, we chose to use the integrative interpretative thematic synthesis analysis method to describe the factors associated with caregiver burden and QoL. Through the use of this analysis process, related statements (codes) were merged to form sub-themes and then aggregated into main themes [35]. The themes that emerged from the analysis included 1) characteristics of caregivers of cancer patients, 2) caregivers' burden, 3) caregivers' QoL, and 4) the relationship between caregivers' burden and QoL.
3. Results
3.1. Characteristics of studies
This review included 15 studies published between 2000 and 2022. The studies were conducted in 8 countries, including Turkey (n = 6) [[36], [37], [38], [39], [40], [41]], USA (n = 3) [[42], [43], [44]], Brazil (n = 1) [45], Iran (n = 1) [46], South Africa (n = 1) [33], France (n = 1) [47], South Korea (n = 1) [48], and Italy (n = 1) [49]. The studies were cross-sectional design (n = 11) [[36], [37], [38], [39], [40], [41],[44], [45], [46],48,49], longitudinal (n = 3) [42,43,47] and quasi-experimental design (n = 1) [33]. The sample ranged from 34 to 224 [44,45]. Fifteenth studies reported the mean age of the caregiver to range from 39 to 57.2 years, while one did not report the mean age [46]. The details of the study characteristics are shown in Table 1.
Table 1.
Distribution of study characteristics.
| Reference | Country | Purpose | Design | Analysis | Caregiver's Characteristics |
|||
|---|---|---|---|---|---|---|---|---|
| Female (%) | Mean age | Sample | Spouse/(%) | |||||
| Akpinar & Yurtsever, 2018 [36] | Turkey | Determined the relationship between the caregiving burden and QOL of family caregivers | Cross-sectional | Kolmogorov-Smirnov test, Mann Whitney U test, ANOVA | 67 | 42 | 67 | 38.3 |
| Araújo et al., 2019 [45] | Brazil | Assessed the QoL and the burden of female caregivers | Cross-sectional | Kruskal-Wallis test, Mann-Whitney test, Spearman test | NP | 51.8 | 224 | NP |
| Deniz & Inci, 2015 [37] | Turkey | Identified the burden of care and QoL of caregivers | Cross-sectional | Spearman's correlation, Kruskal Wallis, Mann-Whitney U test | 69.9 | 42.2 | 123 | NP |
| Gabriel & Mayers, 2019 [33] | South Africa | Implemented and evaluated the effectiveness of a psychosocial intervention program on the QOL and caregiver burden | Quasi-experimental | Independent t-tests, Chi-square tests, ANOVA | 55.6 | NP | 108 | 30.6 |
| Gaston-Johansson et al., 2004 [42] | USA | Determined the effects of sociodemographic variables, psychological distress, fatigue, and QOL on Burden of care in caregivers | Longitudinal | Spearman's correlation | 25 | 47.6 | 102 | 87 |
| Germain et al., 2017 [47] | France | Evaluated the perceived burden and the QoL of primary caregiver of patients | Longitudinal | Multivariable analysis, Bonferroni correction | 55.2 | 64 | 96 | 35.4 |
| Grant et al., 2013 [43] | USA | Reduced caregiver burden, improved caregiving skills, and promoted self-care | Longitudinal | ANOVA | 64 | 57.2 | 163 | 68.1 |
| Gur & Ersin, 2021 [38] | Turkey | Determined the care load, quality of life of caregivers, and the influencing factors | Cross-sectional | Kruskal-Wallis Test, Mann Whitney U test | 47.5 | 34.8 | 160 | NP |
| Nightingale et al., 2016 [44] | USA | Determined the relationship between perceived social support, burden; and quality of life | Cross-sectional | Repeated measures ANOVA | 85 | 57 | 34 | 74 |
| Rha et al., 2015 [48] | Korea | Identified factors contributing the caregiving burden and QOL | Cross-sectional | t-test, ANOVA, correlation, Multiple linear regression | 79.2 | 46.2 | 212 | 48.6 |
| Serin et al., 2020 [39] | Turkey | Determined the relationship between care burden and QoL | Cross-sectional | Mann-Whitney U test, t-test, correlation, Linear regression | 75.3 | 39.6 | 89 | NP |
| Shahvand & Sarafraz, 2020 [46] | Iran | Identified patients who have cancer need to receive care from their family | Cross-sectional | Path regression analysis | NP | NP | 141 | NP |
| Spatuzzi et al., 2017 [49] | Italy | Evaluated caregiver burden and QoL in active treatment settings and hospice care | Cross-sectional | Chi-square test | 81.1 | 46.3 | 76 | NP |
| Turkoglu & kilic, 2012 [40] | Turkey | Examined the effects of caring burdens of family caregivers of cancer patients on QoL | Cross-sectional | Pearson Correlation, Linear and logistic regression | 58.9 | 42.3 | 190 | 59.3 |
| Uzar-Ozceti & Dursun, 2020 [41] | Turkey | Examined the relations between resilience, caregiver burden, and QoL | Cross-sectional | Independent t-test, Pearson's correlation | 52.4 | 39.6 | 210 | NP |
Legends: NP; Not reported.
3.2. Influence of caregiver burden on QoL
We used an integrative interpretative synthesis design to identify themes related to caregiver burden and QoL. In this integrative review, five key themes were identified. These five themes were 1) characteristics of caregivers of cancer patients, 2) caregivers' burden, 3) caregivers' QoL, and 4) the relationship between caregivers' burden and QoL.
3.2.1. CharacterisCtics of caregivers
Several caregiver characteristics were identified in this review (see Table 2). The parameters largely measured were age, sex, nature of the relationship with the patient, caregiver experience and duration of caregiving, and the need for help as a caregiver. The age distribution of caregivers considerably varied but mostly above 40 years [36,37,45]. The mean age of family caregivers was 42 ± 13 years [36], 51.8 ± 13.7 [45], 42.22 ± 11.68 years [37], and 35.01 ± 14.85 years [39]. We also identified that most (69.9 %) caregivers were female [37]. The nature of the relationship between caregivers and the patients indicated that diverse family members were involved in the informal caregiving. It was shown that 57.1 % of caregivers were first-degree relatives (father, mother, or children), 23.7 % were non-consanguineous, like the patients' parent-in-law, daughter-in-law, son-in-law, and wife/husband, and the others were second and third-degree relatives [44,45].
Table 2.
Distribution of the factors associated with caregiver burden and QoL.
| Ref | Caregiver Burden | Caregivers QoL | Factors Affecting QoL | Relationship of Burden to QoL |
|---|---|---|---|---|
| Akpinar & Yurtsever, 2018 [36] | Tool: Caregiver's Stress Scale (CSI) Family members tended to cry, had stress, unhappiness, and experienced despair |
Tool: Caregivers' quality of life of cancer (CQOLC) CQOLC scores were low |
Females, with formal education, a job, low incomes, caring for spouses, longer care duration have the worst QOL | Higher caregiver burden was related to poor quality of life. |
| Araújo et al., 2019 [45] |
Tool: Zarit Burden Interview (ZBI) Caregivers (46.4 %) had moderate burden, and 64.3 % had a significant level of burden |
Tool: World Health Organization Quality of Life Brief (WHOQOL-BREF) Mean QOL score was moderate to severe burden |
Income level, number of people living in the household, and duration of care | It was significant that the higher the QOL score, the lower the burden. |
| Deniz & Inci, 2015 [37] | Tool: ZBI Perceived burden of caregiving was high |
Tool: CQOLC Total mean quality of life score was higher |
Caregiver characteristics like gender-men, poor economic status, caregiving to a spouse | Increasing caregiver burden resulted in low QoL |
| Gabriel & Mayers, 2019 [33] | Tool: ZBI The intervention reduces the caregiver's burden decline |
Tool: CQOLC The intervention enhances the caregiver's QOL |
Not Reported (NR) | Psychosocial intervention reduced the caregiver burden at both T1 and T2 and improved the caregiver QOL |
| Gaston-Johansson et al., 2004 [42] | Tool: Measurement of Objective Burden (MOB) and the Measurement of Subjective Burden Burden means score was slightly higher than the mean subjective burden score; |
Tool: Quality of Life Index (QLI) Mean QOL scores were low |
Age and subjective burden, income level, caregiver fatigue, subjective burden, trait anxiety | Mean QOL scores were low and significantly intercorrelated, except for subjective burden and temporal and sensory fatigue |
| Germain et al., 2017 [47] | Tool: ZBI Primary caregivers felt a low burden, a mild burden, and a moderate to severe burden |
Tool: Short Form Health Survey (SF-12) QoL scores were significantly decreased by 5 points for the “emotional burden” and “physical pain” dimensions |
Age of caregiver, remote relationship with the patient, non-dependent, fewer comorbidities, and a greater life expectancy of patient were determined better QoL | Perceived burden was the main determinants of caregiver's QoL |
| Grant et al., 2013 [43] | Tool: Caregiver Burden Scale Caregivers experienced high levels of Subjective Stress; objective burden changed significantly across time, peaking at 12 weeks |
Tool: City of Hope-QOL Scale – Family Version At baseline, overall QOL was moderate and decreased significantly over time. |
Help from family and/or neighbours, cleaning services, spiritual counselling, home health services, support groups for caregivers, social work, and professional counselling. | Caregivers experience high levels of emotional stress related to the caregiving role and report deteriorations in psychological well-being and overall QOL over time. |
| Gur & Ersin, 2021 [38] | Tool: ZBI Caregivers had a low caregiving burden |
Tool: CQOLC Caregiver life quality was not at the desired level |
Income status of the caregivers affected their quality of life. | Care burden was affected by negative perceptions about health, while income status affected life quality |
| Nightingale et al., 2016 [44] | Tool: Caregiver Reaction Assessment (CRA) Caregivers showed a significant change in two of the burden subscales, including esteem and impact on health. |
Tool: CQOLC The QOL subscales showed a significant time effect on caregivers' disruption. |
Higher perceived social support was associated with higher overall QOL | Higher perceived social support is associated with a lower Burden and higher quality of life at T2. |
| Rha et al., 2015 [48] | Tool: ZBI Reported a moderate caregiving burden, although about one-quarter reported a high caregiving burden. |
Tool: K-WHOQOL-BREF QOL is moderate, with a mean score of 3.12 ± 0.50 (out of 5) |
Male caregivers with more education demonstrated higher QOL Hospitalized patients demonstrated lower QOL |
Caregiving burden explained the variance of the QOL Caregivers caring for patients with functional deterioration experienced a higher burden |
| Serin et al., 2020 [39] | Tool: ZBI Caregiver burden was high (43.82 ± 13.77) |
Tool: QoL-FV Negative relationship between the ZBI total score and the QoL-FV subscales |
Low income, divorce, and spouse, were predictors of quality of life | Care burden of caregivers increased, and QoL total scale and subscales mean scores decreased |
| Shahvand & Sarafraz, 2020 [46] |
Tool: ZBI Caregiver burden negatively correlated with hope. Hope and QOL both formed strong relations with the caregiver's burden |
Tool: QOL by the European Organization for Research of Cancer Mean QOL was −45.07 ± 16.13 |
Lower age, female gender, lower level of education, a mixed relation, and higher levels of anxiety and depression | A direct and negative relationship between caregiver burden and hope An indirect and positive relationship between caregiver burden and QOL |
| Spatuzzi et al., 2017 [49] |
Tool: Caregiver Burden Inventory (CBI) No significant difference in CBI scores between the palliative and the active group |
Tool: SF-36 Palliative group has a greater general health and physical component score but a lower mental component score |
NR | The hospice group reported significantly lower QoL scores in the mental component summary score and higher scores in the general health subscale |
| Turkoglu & kilic, 2012 [40] | Tool: ZBI Caregivers had a burden for disruptiveness, positive adaptation, and financial difficulties |
Tool: CQOLC Palliative group has a greater general health and physical component score but a lower mental component score |
Being under 35, having a low income, being the spouse and parent of the patient, and the patient has their room (p < 0.05) | There was a negative relationship between burdens and the quality of life |
| Uzar-Ozceti & Dursun, 2020 [41] | Tool: ZBI Resilience negatively mediated the caregiver's burden |
Tool: CQOLC Resilience positively predicted the QoL |
Caregiving process, family interdependence, social norm, and family resource | Low levels of resilience, which in turn was associated with greater caregiver burden and poorer QoL |
The ability of caregivers to keep to their previous work and contribute to the economic needs of the patients was also influenced by the nature of the strain required from the caregiving. This is because it was reported that 60.0 % of the caregivers had difficulties in their working life [38]. Caregivers also indicated their experience in providing caregiving services. The level of caregiving experiences varied, as 21.8 % of caregivers had previous experience providing care to another patient [38]. The strong family bonds necessitated the reasons for providing caregiving [38,44]. As part of the informal caregiving role, respondents were also engaged in diverse domestic chores and responsibilities. These caregiving functions included; participants being responsible for household chores and having paid jobs [45].
3.2.2. Caregiver burden
In this theme, two main sub-themes were identified. The level of burden and the factors that are associated with caregiver burden.
3.2.3. Caregivers' level of burden
The level of burden among caregivers was mostly measured using the Zarit caregiver burden scale [37,38,40,41,48]. The ZBI total scores range from 0 to 103 as a summed score. The average burden score was mostly reported to be very high (n = 4) among caregivers [37,38,40,41]. In other studies, the mean score of the burden interview of caregivers was 36.65 ± 11.21 [40], 32.65 ± 15.14 [38], 70.75 ± 17.09 [41]. However, other studies reported that most caregivers (46.4 %) had a moderate burden, while 64.3 % had a significant level of burden [45]. The average subscale of caregivers on the burden score average was 16.84 ± 11.58 [37]. The family caregivers of cancer patients reported experiencing a moderate caregiving burden, although about one-quarter reported a high burden [48]. The level of burden on the burden scale had an average of 14.96 ± 4.8 for disruptiveness, 12.31 ± 3.9 for positive adaptation, and 5.69 ± 3.0 for financial difficulties [40].
3.2.4. Factors associated with caregiver burden
Several factors were identified to directly influence caregivers' burden level [33,42,43]. Age (older), gender (male), subjective stress, and trait anxiety were significantly associated with higher caregiver burden [33,37,42,43]. Also, a weak positive correlation was found between the patient's age (younger) and their caregiver's emotional burden [42,48]. Other personal factors associated with the caregiver, like work, relationships with patients, and income levels, influence the caregiver's burden. The caregiving burden was significantly higher among caregivers who were employed or working [37]. The emotional burden was lower for currently working caregivers and was much influenced as the financial need for the family appeared to increase [37,48]. Caregiver burden scores were higher among caregivers who described their economic status as “poor” compared with economic status as “better” and “medium” [37].
The caregiver burden increased as the patient dependency level increased [37]. The disease level also predicted the caregiver burden as caregivers of patients with advanced-stage cancer experienced more burden [48]. Level of care also influenced other social activities of the caregiver as the higher burden was reported for time for self, personal privacy, time for recreation, the tension in life, vacation and trips, time for own work and chores, and time for friends/relatives [43]. The caregiver burden was increased if the patient was living with the caregiver in the same home [48]. Caregivers who provided care to their spouses reported greater burdens and lower QoL than caregivers who provided care to their mothers [37].
3.2.5. Caregivers' QoL
In this theme, two sub-themes were identified to be associated with the QoL of cancer caregivers. These two sub-themes are caregivers' QoL level and factors associated with the caregivers' QoL.
3.2.6. Caregivers' QoL level
The tool used to measure the QoL of caregivers was the caregiver QoL index scale [37,40,41]. The Caregiver Family Members' Life Quality Scale (CQOLC) average scores were 60.70 ± 25.89 and ranged from 0 to 175. The QoL was low (n = 4) among caregivers [37,38,41]. The average score of QoL on the scale for caregivers was 37.54 ± 7.68 [37], 78.75 ± 16.31 [38], and 21.18 ± 5.3 [40]. Caregivers of cancer patients rated their QOL as moderate, with a mean on the Korean version of World Health Organization QOL-BREF (K-WHOQOL-BREF) of 3.12 ± 0.50 [48]. The level of caregiver QoL was even worse when it was reported that 39.2 % of caregivers had a total score of <3 [48]. Also, the mean score of the caregiver QoL Index on cancer was 81.40 ± 17.3 [40].
3.2.7. Factors associated with caregiver QoL
Diverse factors were identified to influence the QoL of family caregivers. Factors associated with the QoL of caregivers were age (less than 35 years), caregiving role, relationship to patients (spouse or parent), having a low income, and living in the same home with the patient [36,40,45,47]. Other influencing factors to caregiver QoL included the caregiver's responsibility and other social and family responsibilities [36,40,45]. Family members who took care of a child (29.5 %), and two children (50 %), and were in charge of 3–5 children (20.6 %) had a considerably lower level of QoL [36]. Another important factor that influenced caregivers' QoL was the caregiving duration. The QOL average score of family members giving care between an hour to ten per day was high, but the average QoL score of those giving care 21 h and over per day was the lowest [36].
The resilience also positively predicted the QoL [41]. Caregivers with no disease scored higher on the Overall Quality of Life Index (OQOLI) [37,45]. CQOLC average scores of those facing financial problems and changes in family and social relations were found to be lower [36]. A remote relationship with the patient, a low perceived burden, being non-dependent, receiving help, being patient with fewer comorbidities, and patient having higher life expectancy were determinant factors for a better QoL [36,47]. Higher perceived social support was associated with higher overall QOL [36,39,44]. Primary caregivers who received a psychosocial intervention showed a significant improvement in burden [33,37].
3.2.8. Relationship between burden and QoL
Some studies assessed the relationship between caregiver burden and QoL [[40], [41], [42],44,45]. It was noted that as the caregiver burden increased, the QoL of caregivers decreased [[40], [41], [42],44,45]. A moderate negative correlation was identified between the sum of the QOL scores and the burden questions [40,45]. Burden substantially predicted patient-reported subjective QoL [42]. Caregivers whose family life were affected by their caregiving activities reported a higher total care burden and a lower QoL score on the discomfort dimension [37,42,47,48]. The results showed that there was a negative relationship between the ZBI total score and the QoL scale family version (QoL-FV) subscales of psychological and spiritual health conditions, physical health conditions, support, and economic effect conditions, and QoL-FV total score [39,46]. Also, the caregiver burden is negatively correlated with hope [46,49].
Several other critical factors are identified to influence the life of caregivers. These factors associated with caregivers' life were the level of discomfort, positive adaptation, financial challenges, and the relationship with the patient [36,37]. The average discomfort subscale score was 39.67 ± 13.33, the positive adaptation subscale score was 70.24 ± 13.81, and the financial problems subscale score was 20.48 ± 26.90 [37,38]. Also, informal caregivers reported that they have been experiencing psychological distress while looking after the patients [37,38]. Also, 34.5 % of the family members stated that they tended to cry, 32.8 % had stress, 26.6 % unhappiness, and 23.3 % experienced despair [36].
4. Discussion
This integrative review identified the factors associated with cancer patients' caregivers' burden and QoL. The assessment of the factors associated with caregivers' burden and QoL is critical because caregivers play an important role in the management of cancer including treatment acquisition and utilization, management of adverse events, and providing psychological support to the patient [50,51]. These caregivers' roles are critical in ensuring that a desirable disease prognosis is achieved [52]. Caregivers' burden may be so high that they subordinate the demands of everyday life to the treatment/workload required for the patient [53]. This is particularly the case when caregivers and patients are required to follow regimented structural treatment procedures [53,54]. Given the burden and the structural nature of cancer treatment, patients and caregivers must identify personal treatment pathways, navigating between institutions in healthcare systems to meet the needs of uncertain and often lengthy disease and treatment trajectories. The culminating effects of these demanding requirements result in a high burden and lower QoL for the informal caregiver. In this integrative review, we identified an inverse relationship between caregiver burden and QoL. Most of the studies reported that as the burden of caregiving increased, the QoL conversely deteriorated [55,56]. To improve caregivers' QoL, efforts must be channeled toward alleviating the burden. Caregivers are burdened in several and multiple dimensions. These dimensions ranged from physical, psychological, financial, and social, and the continuous emotional torture of seeing a loved one suffer the long-term consequence of cancer [56,57]. These consequences may be a product of the disease trajectory or a consequence of adverse effects of treatment. Therefore, there must be a concerted effort to alleviate the burden of caregivers of cancer patients and improve their QoL. This can be achieved if health service providers meticulously collaborate with patients and family members in providing care to patients with cancer at all stages [54,58]. The preference of patients and the benefits of the role of caregivers cannot be downplayed. Therefore, this essential care provider (informal caregiver) must be involved as an active participant in the care process.
We also identified that personal characteristics, including resilience, positively mediated the relationship between caregiver burden and QoL. As individual socioeconomic characteristics were reported to be improved, the burden level was minimal with improved QoL. Other studies reported that the QoL in caregivers depends on personal characteristics, including demographic factors [56,57]. Having patients with cancer in the family, receiving support, and conditions arising from the caregiving process, such as affected health, and marital difficulties, were found to affect the burden of caregiving [10]. Service providers and policymakers must focus on leveraging other social support services for patients and caregivers to improve their living conditions and the demands of caregiving [14,15,59]. This is important because a recent meta-analysis demonstrated a negative relationship between social support and caregiving burden [15,59]. Also, we identified that the financial burden of caregivers increased the overall burden and significantly reduced the QoL of cancer patients' caregivers. Finances are critical in supporting patients and relatives in mitigating medical bills, caring for everyday expenses, and promoting the use of related medical services [57,60]. The cost-to-income ratio for cancer treatment is consistent with perceived financial difficulty [60]. The related cost of cancer treatment can be mitigated if health insurance can cover the cost of therapy and related treatment. This will then minimize the burden patients may have to impose on informal caregivers [61,62]. The inability of health insurance to pay for the cost of cancer therapy is more of a concern in lower- and middle-income countries where health insurance services led by governments do not cover the cost of chronic diseases and income-intensive therapies [62]. Patients with a financial burden, especially those with extreme health spending and perceived severe financial difficulty, are likely to have poor HRQOL and symptom burden [60,61]. In this current review, we identified multiple and diverse factors including the socio-economic, cultural, physical, psychological, and health-illness status of the caregiver, and health service-related factors to influence the QoL of cancer patients’ caregivers. In a related review that considered the QoL of cancer patients' caregivers, similar factors were identified [59,63]. It is imperative to continue developing intervention programs that target informal caregivers of cancer patients. The imperative for these interventions is increased by the current impact of the coronavirus infection. The global pandemic has left in its trail deteriorating socioeconomic situations that caregivers and patients must mitigate for their treatments. This is because family caregivers' fears and concerns have been exacerbated by the current situation of the pandemic [63].
4.1. Strengths and limitations
In this review, we demonstrated the factors associated with cancer patients' caregivers' burden and how that influences their QoL. We identified multiple factors that influence or mitigate caregiver burden and the QoL by using qualitative data synthesis techniques. However, certain limitations are associated with this review. Firstly, the review was limited to only studies that were written and published in English. This might have left out essential literature written in other languages, even though we ensured the comprehensiveness of the search by using the PICO framework. We also noted that the studies were largely conducted in developed countries in the global west with limited numbers in Africa, Asia, and other developing countries. Therefore, the generalization of the study findings in resource-limited settings and diverse cultures may be done with caution. This is particularly important that cultural variations between continents may influence caregiving requirements and the resultant burden and QoL. Nonetheless, this integrative review may be a panacea for conducting studies to assess caregiver burden and QoL in resource-limited settings, especially in Africa and Asia. Secondly, in this integrative review, there was high heterogeneity in the various studies because they used varied sample sizes, intervention approaches, designs, and inconsistent tools to measure the outcome variables. This made it difficult to conduct a systematic meta-analysis of the results that could show a direct causal relationship. Therefore, future studies must use rigorous scientific RCT designs to test the efficacy of diverse interventions that target the burden and QoL of cancer patients' caregivers. This is particularly important that RCT studies that assess the influence of these factors are limited hence, the majority of the studies were mainly cross-sectional. It is critical to have intervention studies among caregivers of cancer patients to limit the caregiving burden and generally improve the QoL.
5. Conclusion
In this review, we identified varied and diverse factors that influence caregiver burden and QoL. Increasing caregiver burden was identified to be negatively associated with QoL. As a result, pragmatic strategies must be adopted to reduce caregiver burden and promote QoL. These can be achieved through technology and web-based interventions to reduce caregiver burden, improve the psychological situation, and promote QoL. Given the burden and the structural nature of the treatment, patients and caregivers must identify personal treatment pathways, navigating between institutions in healthcare systems to meet the needs of uncertain and often lengthy disease and treatment trajectories. Future research should identify appropriate means to support caregivers of patients with cancer by mitigating the burden and promoting effective QoL. Also, a lower socioeconomic level was associated with a higher burden and low QoL. Consequently, interventions to promote the QoL of caregivers must consider segregating the population to have tailor-made specific interventions to ensure maximum effect. The current world trends demand that investments be made to mitigate the caregiver burden's influence and improve their QoL by developing and testing internet and technology-based strategies.
Data availability
Data included in article/supp. material/referenced in article.
CRediT authorship contribution statement
Jotsna Akter: Writing – original draft, Methodology, Formal analysis, Conceptualization. Kennedy Diema Konlan: Writing – review & editing, Writing – original draft, Validation, Supervision, Resources, Project administration, Methodology, Formal analysis, Data curation, Conceptualization. Meherun Nesa: Writing – original draft, Methodology, Data curation, Conceptualization. Aloysia Ispriantari: Writing – review & editing, Writing – original draft, Validation, Methodology, Formal analysis, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e21243.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Sung H., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Chopra D., et al. Chemotherapy-induced adverse drug reactions in oncology patients: a prospective observational survey. Indian J. Med. Paediatr. Oncol. 2016;37(1):42–46. doi: 10.4103/0971-5851.177015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lapid M.I., et al. Cancer caregiver quality of life: need for targeted intervention. Psycho Oncol. 2016;25(12):1400–1407. doi: 10.1002/pon.3960. [DOI] [PubMed] [Google Scholar]
- 4.Pramanik P. Bangladesh Health Professions Institute, Faculty of Medicine, the University; 2018. Perceived Understanding of Barriers Related to Quality of Daily Life Among Cancer Caregivers. [Google Scholar]
- 5.Hu X., et al. Caregiver burden among Chinese family caregivers of patients with lung cancer: a cross-sectional survey. Eur. J. Oncol. Nurs. 2018;37:74–80. doi: 10.1016/j.ejon.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 6.Liu Z., Heffernan C., Tan J. Caregiver burden: a concept analysis. International journal of nursing sciences. 2020;7(4):438–445. doi: 10.1016/j.ijnss.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fumaneeshoat O., Ingviya T. Quality of life and burden of lung cancer patients' caregivers: a cross-sectional study from Southern Thailand. Journal of Health Science and Medical Research. 2020;38(3):177–192. [Google Scholar]
- 8.Nemati S., et al. Perceptions of family caregivers of cancer patients about the challenges of caregiving: a qualitative study. Scand. J. Caring Sci. 2018;32(1):309–316. doi: 10.1111/scs.12463. [DOI] [PubMed] [Google Scholar]
- 9.Borges E.L., et al. Family caregiver burden: the burden of caring for lung cancer patients according to the cancer stage and patient quality of life. J. Bras. Pneumol. 2017;43:18–23. doi: 10.1590/S1806-37562016000000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eskin S.G., Yuksel R., Bulut H. Investigation of the relationship between care giving burden and quality of life of caregivers of cancer patients. J. Evol. Med. Dent. Sci. 2021;10(9):567–573. [Google Scholar]
- 11.Tan J.Y., et al. Burden, emotional distress and quality of life among informal caregivers of lung cancer patients: an exploratory study. Eur. J. Cancer Care. 2018;27(1) doi: 10.1111/ecc.12691. [DOI] [PubMed] [Google Scholar]
- 12.Hogan U., et al. The experience of informal caregivers in providing patient care in hospitals in low-and middle-income countries: a qualitative meta-synthesis. J. Health Serv. Res. Policy. 2022 doi: 10.1177/13558196221101968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mishra S., et al. Caregiver burden and quality of life among family caregivers of cancer patients on chemotherapy: a prospective observational study. Indian J. Palliat. Care. 2021;27(1):109. doi: 10.4103/IJPC.IJPC_180_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leung D.Y., et al. Source of social support and caregiving self-efficacy on caregiver burden and patient's quality of life: a path analysis on patients with palliative care needs and their caregivers. Int. J. Environ. Res. Publ. Health. 2020;17(15):5457. doi: 10.3390/ijerph17155457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.del-Pino-Casado R., et al. Social support and subjective burden in caregivers of adults and older adults: a meta-analysis. PLoS One. 2018;13(1) doi: 10.1371/journal.pone.0189874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johansen S., Cvancarova M., Ruland C. The effect of cancer patients' and their family caregivers' physical and emotional symptoms on caregiver burden. Cancer Nurs. 2018;41(2):91–99. doi: 10.1097/NCC.0000000000000493. [DOI] [PubMed] [Google Scholar]
- 17.Etters L., Goodall D., Harrison B.E. Caregiver burden among dementia patient caregivers: a review of the literature. J. Am. Acad. Nurse Pract. 2008;20(8):423–428. doi: 10.1111/j.1745-7599.2008.00342.x. [DOI] [PubMed] [Google Scholar]
- 18.Egan K.J., et al. Online training and support programs designed to improve mental health and reduce burden among caregivers of people with dementia: a systematic review. J. Am. Med. Dir. Assoc. 2018;19(3):200–206. doi: 10.1016/j.jamda.2017.10.023. e1. [DOI] [PubMed] [Google Scholar]
- 19.Visser-Meily J.A., et al. Measures used to assess burden among caregivers of stroke patients: a review. Clin. Rehabil. 2004;18(6):601–623. doi: 10.1191/0269215504cr776oa. [DOI] [PubMed] [Google Scholar]
- 20.Addo R., et al. Economic burden of caregiving for persons with severe mental illness in sub-Saharan Africa: a systematic review. PLoS One. 2018;13(8) doi: 10.1371/journal.pone.0199830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lai S.-T., et al. Burden in caregivers of adults with epilepsy in Asian families. Seizure. 2019;71:132–139. doi: 10.1016/j.seizure.2019.07.008. [DOI] [PubMed] [Google Scholar]
- 22.Bauer M.R., et al. Quality of life in patients with pancreatic cancer and their caregivers: a systematic review. Pancreas. 2018;47(4):368–375. doi: 10.1097/MPA.0000000000001025. [DOI] [PubMed] [Google Scholar]
- 23.Kusi G., et al. The experiences of family caregivers living with breast cancer patients in low-and middle-income countries: a systematic review. Syst. Rev. 2020;9(1):1–18. doi: 10.1186/s13643-020-01408-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hsu T., et al. Understanding caregiver quality of life in caregivers of hospitalized older adults with cancer. J. Am. Geriatr. Soc. 2019;67(5):978–986. doi: 10.1111/jgs.15841. [DOI] [PubMed] [Google Scholar]
- 25.Kehoe L.A., et al. Quality of life of caregivers of older patients with advanced cancer. J. Am. Geriatr. Soc. 2019;67(5):969–977. doi: 10.1111/jgs.15862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ochoa C.Y., Lunsford N.B., Smith J.L. Impact of informal cancer caregiving across the cancer experience: a systematic literature review of quality of life. Palliat. Support Care. 2020;18(2):220–240. doi: 10.1017/S1478951519000622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Souza M.T.d., Silva M.D.d., Carvalho R.d. Integrative review: what is it? How to do it? Einstein (São Paulo) 2010;8:102–106. doi: 10.1590/S1679-45082010RW1134. [DOI] [PubMed] [Google Scholar]
- 28.Hopia H., Latvala E., Liimatainen L. Reviewing the methodology of an integrative review. Scand. J. Caring Sci. 2016;30(4):662–669. doi: 10.1111/scs.12327. [DOI] [PubMed] [Google Scholar]
- 29.Munn Z., et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018;18(1):1–7. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Toronto C.E., Remington R. Springer; 2020. A Step-by-step Guide to Conducting an Integrative Review. [Google Scholar]
- 31.Sarkis-Onofre R., et al. How to properly use the PRISMA Statement. Syst. Rev. 2021;10(1):1–3. doi: 10.1186/s13643-021-01671-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hong Q.N., Gonzalez‐Reyes A., Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT) J. Eval. Clin. Pract. 2018;24(3):459–467. doi: 10.1111/jep.12884. [DOI] [PubMed] [Google Scholar]
- 33.Gabriel I.O., Mayers P.M. Effects of a psychosocial intervention on the quality of life of primary caregivers of women with breast cancer. Eur. J. Oncol. Nurs. 2019;38:85–91. doi: 10.1016/j.ejon.2018.12.003. [DOI] [PubMed] [Google Scholar]
- 34.Braun V., Clarke V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006;3(2):77–101. [Google Scholar]
- 35.Braun V., Clarke V. Can I use TA? Should I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern-based qualitative analytic approaches. Counsell. Psychother. Res. J. 2021;21(1):37–47. [Google Scholar]
- 36.Akpinar N.B., Yurtsever S. Care burden and quality of life of family members caring for cancer outpatients. Int. J. Caring Sci. 2018;11(3) [Google Scholar]
- 37.Deniz H., Inci F. The burden of care and quality of life of caregivers of leukemia and lymphoma patients following Peripheric stem cell transplantation. J. Psychosoc. Oncol. 2015;33(3):250–262. doi: 10.1080/07347332.2015.1019660. [DOI] [PubMed] [Google Scholar]
- 38.Gür S.C., ErsİN F. The investigation of caregiving burden and life quality of caregivers who care for cancered patients. Kanserli Hastalara Bakım Veren Bireylerin Bakım Yükü, Yaşam Kalitesi ve Etkileyen Faktörlerin İncelenmesi. 2021;18(1):88–94. [Google Scholar]
- 39.Serin E.K., et al. Care burden and quality of life of caregivers of cancer patients with stem cell transplantation. Int. J. Caring Sci. 2020;13(3):1826–1834. [Google Scholar]
- 40.Turkoglu N., Kilic D. Effects of care burdens of caregivers of cancer patients on their quality of life. Asian Pac. J. Cancer Prev. APJCP : Asian Pac. J. Cancer Prev. APJCP. 2012;13(8):4141–4145. doi: 10.7314/apjcp.2012.13.8.4141. [DOI] [PubMed] [Google Scholar]
- 41.Uzar-Ozcetin Y.S., Dursun S.I. Quality of life, caregiver burden, and resilience among the family caregivers of cancer survivors. Eur. J. Oncol. Nurs. 2020;48 doi: 10.1016/j.ejon.2020.101832. [DOI] [PubMed] [Google Scholar]
- 42.Gaston-Johansson F., et al. Psychological distress, fatigue, burden of care, and quality of life in primary caregivers of patients with breast cancer undergoing autologous bone marrow transplantation. Oncol. Nurs. Forum. 2004;31(6):1161–1169. doi: 10.1188/04.ONF.1161-1169. [DOI] [PubMed] [Google Scholar]
- 43.Grant M., et al. Family caregiver burden, skills Preparedness, and quality of life in non-small cell lung cancer. Oncol. Nurs. Forum. 2013;40(4):337–346. doi: 10.1188/13.ONF.337-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nightingale C.L., et al. Burden, quality of life, and social support in caregivers of patients undergoing radiotherapy for head and neck cancer: a pilot study. Chron. Illness. 2016;12(3):236–245. doi: 10.1177/1742395316644305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Araújo M.G.d.O., et al. Cuidando de quem cuida: qualidade de vida e sobrecarga de mulheres cuidadoras. Rev. Bras. Enferm. 2019;72:728–736. [Google Scholar]
- 46.Shahvand T., Sarafraz M.R. Investigating the mediatory role of hope and shame in the relationship between caregiver burden and quality of life of patients with cancer. South Asian journal of cancer. 2020;9(3):174–179. doi: 10.1055/s-0041-1723109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Germain V., et al. Management of elderly patients suffering from cancer: assessment of perceived burden and of quality of life of primary caregivers. Journal of Geriatric Oncology. 2017;8(3):220–228. doi: 10.1016/j.jgo.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 48.Rha S.Y., et al. Caregiving burden and the quality of life of family caregivers of cancer patients: the relationship and correlates. Eur. J. Oncol. Nurs. 2015;19(4):376–382. doi: 10.1016/j.ejon.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 49.Spatuzzi R., et al. Quality of life and burden in family caregivers of patients with advanced cancer in active treatment settings and hospice care: a comparative study. Death Stud. 2017;41(5):276–283. doi: 10.1080/07481187.2016.1273277. [DOI] [PubMed] [Google Scholar]
- 50.Kang A., et al. Evaluating burden and quality of life among caregivers of patients receiving Peritoneal dialysis. Perit. Dial. Int. 2019;39(2):176–180. doi: 10.3747/pdi.2018.00049. [DOI] [PubMed] [Google Scholar]
- 51.Wood R., et al. The humanistic burden of advanced non-small cell lung cancer (NSCLC) in Europe: a real-world survey linking patient clinical factors to patient and caregiver burden. Qual. Life Res. 2019;28(7):1849–1861. doi: 10.1007/s11136-019-02152-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vashistha V., et al. Quality of life among caregivers of lower-income cancer patients: a Single-Institutional Experience in India and Comprehensive Literature Review. Asian Pacific Journal of Cancer Care. 2019;4(3):87–93. [Google Scholar]
- 53.Lippiett K.A., et al. Patients and informal caregivers' experiences of burden of treatment in lung cancer and chronic obstructive pulmonary disease (COPD): a systematic review and synthesis of qualitative research. BMJ Open. 2019;9(2) doi: 10.1136/bmjopen-2017-020515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bain K.T., et al. Discontinuing medications: a novel approach for revising the prescribing stage of the medication‐use process. J. Am. Geriatr. Soc. 2008;56(10):1946–1952. doi: 10.1111/j.1532-5415.2008.01916.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abbasi A., et al. Relationship between caring burden and quality of life in caregivers of cancer patients in Iran. Support. Care Cancer. 2020;28(9):4123–4129. doi: 10.1007/s00520-019-05240-y. [DOI] [PubMed] [Google Scholar]
- 56.Cengiz Z., et al. Care burden and quality of life in family caregivers of palliative care patients. J. Soc. Work End-of-Life Palliat. Care. 2021;17(1):50–63. doi: 10.1080/15524256.2021.1888844. [DOI] [PubMed] [Google Scholar]
- 57.Xia B.T., et al. Patient-caregiver dyads in pancreatic cancer: identification of patient and caregiver factors associated with caregiver well-being. J. Behav. Med. 2022;45(6):935–946. doi: 10.1007/s10865-022-00354-x. [DOI] [PubMed] [Google Scholar]
- 58.Bártolo A., et al. Effectiveness of psychosocial interventions on the burden and quality of life of informal caregivers of hemodialysis patients: a systematic review. Disabil. Rehabil. 2021:1–12. doi: 10.1080/09638288.2021.2013961. [DOI] [PubMed] [Google Scholar]
- 59.Guerra-Martín M.D., et al. Quality of life in caregivers of cancer patients: a literature review. Int. J. Environ. Res. Publ. Health. 2023;20(2):1570. doi: 10.3390/ijerph20021570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen J.E., et al. Objective and subjective financial burden and its associations with health-related quality of life among lung cancer patients. Support. Care Cancer. 2018;26(4):1265–1272. doi: 10.1007/s00520-017-3949-4. [DOI] [PubMed] [Google Scholar]
- 61.Dieleman J.L., et al. Trends in future health financing and coverage: future health spending and universal health coverage in 188 countries, 2016–40. Lancet. 2018;391(10132):1783–1798. doi: 10.1016/S0140-6736(18)30697-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.El-Sayed A.M., Vail D., Kruk M.E. Ineffective insurance in lower and middle income countries is an obstacle to universal health coverage. Journal of global health. 2018;8(2) doi: 10.7189/jogh.08.020402. 020402-020402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sousa H., et al. Caring for patients with end-stage renal disease during COVID-19 lockdown: what (additional) challenges to family caregivers? Scand. J. Caring Sci. 2022;36(1):215–224. doi: 10.1111/scs.12980. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data included in article/supp. material/referenced in article.