Abstract
Alkaline phosphatase (ALP) is a group of enzymes that catalyze hydrolysis of phosphate esters at an alkaline pH, resulting in the generation of inorganic phosphate. These enzymes are widely distributed, and their activity is found in various tissues including bone, liver, intestine, and placenta. However, abnormalities in ALP expression and activity have been observed in certain types of cancer. In some cases, elevated serum levels of ALP are observed in patients with liver and bone metastasis. In other cases, increased levels of ALP have been observed in patients with pancreatic and lung cancer. On the other hand, low expression of ALP has also been associated with poor prognosis in patients with certain types of tumors, including colorectal cancer (CRC), breast cancer, and non-small cell lung cancer (NSCLC). In these cases, low ALP activity may be associated with decreased differentiation of cancer cells and increased cancer cell proliferation. Overall, the role of ALP in cancer is complex and context-dependent. This article reviews application progress of ALP in cancer, and we hypothesize that ALP might be a potential tumor biomarker, combined detection of aspartate aminotransferase (AST)/alanine aminotransferase (ALT), bone-specific alkaline phosphatase (BSAP), carbohydrate antigen 19-9 (CA 19-9), lactate dehydrogenase (LDH) and ALP isozymes levels can be used for more accurate diagnosis of a particular tumor. Further research is needed to better understand the mechanisms underlying ALP dysregulation in cancer and to identify potential therapeutic targets.
Keywords: Alkaline phosphatase (ALP), cancer, biomarker, bone metastasis
Introduction
Alkaline phosphatase (ALP) is a crucial group of enzymes that play an essential role in the human body (1). These enzymes catalyze the hydrolysis of phosphate esters at an alkaline pH level, which results in the generation of inorganic phosphate (2). ALP is widely distributed throughout various tissues within the body, including bone, liver, intestine, and placenta. Their activity is critical for proper bone development and growth during childhood and adolescence (3). Additionally, they aid in digestion by breaking down complex molecules into simpler ones that can be absorbed by the body (3). However, abnormalities in ALP expression and activity have been observed in certain types of cancer.
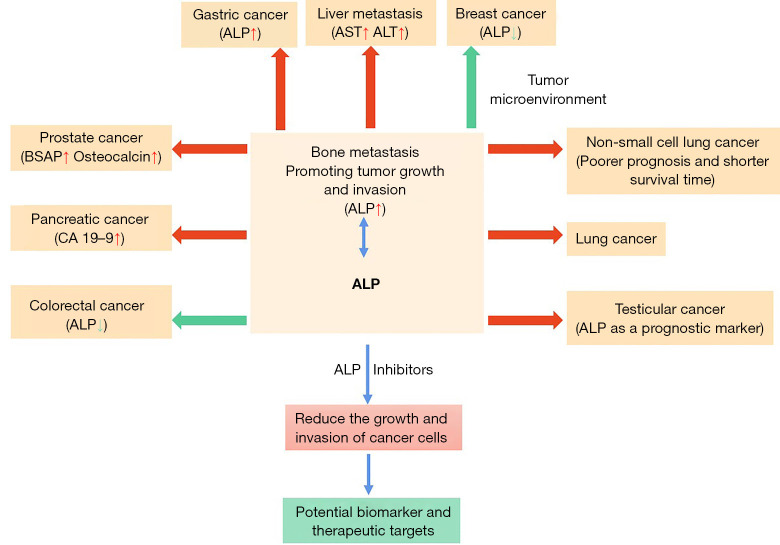
ALP plays a crucial role in various physiological processes such as bone formation and liver function (4,5). However, when there are abnormal growths or tumors present in these areas of the body, it can cause an overproduction of ALP which then leak into the bloodstream. This phenomenon is especially prevalent among those suffering from prostate cancer since this type of malignancy tends to spread to bones more frequently than other types (6). Therefore, monitoring ALP levels through regular blood tests can help doctors detect any potential bone metastases early on and provide appropriate treatment options accordingly. In conclusion, while elevated serum levels of ALP may not always indicate the presence of cancerous growths or tumors within the body; they do serve as valuable indicators for physicians to monitor closely when assessing patients’ overall health status (Figure 1).
Figure 1.
Abnormalities in ALP expression and activity have been observed in certain types of cancer. In some cases, including prostate cancer, liver metastasis, pancreatic cancer, lung cancer, non-small cell lung cancer, testicular cancer, elevated serum levels of ALP are observed in patients with bone metastasis. While, low ALP activity is associated with breast cancer and colorectal cancer. ALP inhibitors can reduce the growth and invasion of cancer cells. In all, ALP might be a potential tumor biomarker, and a potential therapeutic target. Red arrows indicate upregulated expression levels and green arrows indicate downregulated expression levels. ALP, alkaline phosphatase; AST, aspartate aminotransferase; ALT, alanine aminotransferase; BSAP, bone-specific alkaline phosphatase; CA 19-9, carbohydrate antigen 19-9.
In the realm of medical diagnosis, serum levels of ALP have been proven to be a valuable indicator for various conditions (7). One such condition is liver metastasis, where an increase in ALP levels can signify damage to the liver caused by invasive tumor cells (8). This finding has been observed in numerous studies and serves as a crucial diagnostic tool for physicians (9-11). However, it is not just liver metastasis that can cause elevated ALP levels. In fact, patients with pancreatic and lung cancer have also shown increased ALP levels, although the exact mechanism behind this phenomenon remains unclear (12,13). Nonetheless, these findings highlight the importance of monitoring ALP levels in cancer patients as they may provide early indications of disease progression or treatment efficacy. Overall, while there is still much to learn about how ALP function within the body and its relationship with various diseases, it is clear that this enzyme plays a significant role in diagnosing and treating certain conditions, particularly those related to cancer (Table 1). As research continues to shed light on this topic, we can hope for even more effective methods for detecting and managing illnesses moving forward.
Table 1. The level of alkaline phosphatase in human cancers.
| Cancer type | Levels | Functions | Combined diagnosis | References |
|---|---|---|---|---|
| Prostate cancer | Up | Promoting cell growth, metastasis and invasion | Osteocalcin/BSAP | (14-19) |
| Liver metastasis | Up | Promoting liver damage, cell invasion | AST/ALT/CT/MRI | (20-26) |
| Pancreatic cancer | Up | Promoting tumor growth and invasion | CA 19-9 | (27-34) |
| Lung cancer | Up | Promoting tumor proliferation, invasion, bone metastases | N/A | (13,35-41) |
| Breast cancer | Down | Modulating the tumor micro-environment, cytokine expression, cell proliferation and migration | N/A | (42-47) |
| Colorectal cancer | Down | Promotion of cell proliferation, colony formation, and decreased tumor suppressor gene expression | N/A | (48-52) |
| NSCLC | Up | Promoting tumor growth and invasion | ALK/EGFR | (53-55) |
| NSGCT | Up | Promoting tumor growth and invasion | N/A | (56-60) |
| GC | Up | Increased metastasis | LDH | (19,61,62) |
NSCLC, non-small cell lung cancer; NSGCT, non-seminoma germ cell tumor; GC, gastric cancer; BSAP, bone-specific alkaline phosphatase; AST, aspartate aminotransferase; ALT, alanine aminotransferase; CT, computed tomography; MRI, magnetic resonance imaging; CA 19-9, carbohydrate antigen 19-9; N/A, not available; ALK, anaplastic lymphoma kinase; EGFR, epidermal growth factor receptor; LDH, lactate dehydrogenase.
ALP isozymes
ALP isozymes are a family of enzymes that catalyze the hydrolysis of phosphate esters at an alkaline pH. ALPs are found in different tissues and organs in the body, and different tissues express different ALP isozymes. There are four major ALP isozymes: placental, intestinal, liver/bone/kidney (tissue-nonspecific), and germ cell (63). Placental and intestinal isozymes are present in fetal and adult tissues, respectively, while the liver/bone/kidney isozyme is found in the liver, bone, and kidney (Table 2). The different ALP isozymes differ in their enzymatic properties, tissue distribution, and regulation. For example, germ cell ALP is only found in some stages of germ cell development in males (64,65). Placental ALP isozyme is produced exclusively during pregnancy, and its levels in maternal serum serve as a marker for placental health (66,67). Intestinal ALP is expressed in the brush border of intestinal cells and is involved in the absorption of dietary phosphates (68,69). Intestinal and placental ALP isoenzymes are not usually associated with tumor metastasis diagnosis, but their measurement can help exclude non-tumor-related causes of elevated ALP levels (70-72). Liver/bone/kidney ALP is the most widely expressed isozyme and is involved in bone metabolism and mineralization. By assessing the levels and ratios of ALP isoenzymes, along with total ALP, healthcare professionals can obtain valuable information regarding the potential presence and source of tumor metastasis. The combination of ALP isoenzyme analysis with other clinical and imaging investigations can aid in the diagnosis, staging, and monitoring of tumor metastasis, particularly in cases where bone or liver involvement is suspected (73-75). The measurement of ALP isozymes in blood serum or tissue has diagnostic and prognostic value in different diseases. In some diseases, specific ALP isozymes can be used as biomarkers to differentiate between normal and pathological conditions (73-75).
Table 2. Classification and function of alkaline phosphatase isozymes in human.
| Classes | Locations/stages | Protein/gene | Functions | References |
|---|---|---|---|---|
| Germ cell | Male germ cells | GCAP/ALPG | Up-regulation in primary seminoma of the prostate | (64,65) |
| Placental | Cervix, uterine, pregnancy | PLALP/ALPP | Biomarker for placental health, biomarker for pancreatic cancer | (66,67) |
| Intestinal | Brush border of intestinal cells | IAP/ALPI | Absorption of dietary phosphates | (68,69) |
| Liver/bone/kidney (tissue-nonspecific) | Liver, bone, kidney | TNAP/ALPL | Bone metabolism and mineralization | (70-72) |
Overall, the study of ALP isozymes is important in understanding their different roles in the body, their regulation, and their potential use as diagnostic and prognostic markers in cancers. By studying the function of each ALP isozyme in specific tissues and organs, the non-specific ALP can be used as a molecular marker for specific tumor diseases.
ALPs in advanced prostate cancer
In advanced prostate cancer, the level of tissue-nonspecific alkaline phosphatase (TNAP), an enzyme involved in bone formation, is often elevated (14). This is because prostate cancer cells can grow in the bones, leading to an increase in ALP activity, indicating the presence of bone metastases (15). Bone metastases in prostate cancer patients cause bone pain and increase the risk of fracture, leading to a decreased quality of life (16). The increased ALP levels, therefore, serve as an important biomarker to monitor prostate cancer progression and assess the effectiveness of treatment. ALP has also been studied as a potential target for treatment in advanced prostate cancer (17). Studies have shown that targeting ALP with ALP inhibitors can reduce the growth and invasion of prostate cancer cells in vitro and in vivo (15-18). In bone metastatic castration-resistant prostate cancer, ALP-bouncing and lactate dehydrogenase (LDH)-normalization may be a good prognostic marker (19). However, more clinical trials are needed to evaluate the safety and efficacy of ALP inhibitors in prostate cancer patients. In addition to ALP, other bone-related markers such as osteocalcin and bone-specific alkaline phosphatase (BSAP) have also been found to be useful in monitoring the progression of bone metastases in prostate cancer patients (20).
The combination of ALP with other bone markers may provide a more comprehensive understanding of bone metastasis in advanced prostate cancer and assist in personalized treatment decision-making. We believe that we can explore the specific targets of ALP in prostate tissue, and further determine the association between ALP and prostate cancer through the targets of ALP.
ALPs in liver metastasis
In liver metastasis, ALP levels can be elevated in serum and signify liver damage due to the invasion of tumor cells (21). The liver is a common site for the metastasis of tumors originating from other organs including the colon, stomach, pancreas, and breast (22). The presence of liver metastasis may be associated with a worse prognosis, as it often indicates advanced disease. In cases of liver metastasis, ALP can serve as a useful biomarker to monitor the progression of the disease and assess the effectiveness of treatment (23). In addition to ALP, other liver enzymes such as aspartate aminotransferase (AST) and alanine aminotransferase (ALT) may also be elevated with liver metastasis (24). These liver enzymes are released into the bloodstream when liver cells are damaged. In addition to monitoring the levels of ALP and other liver enzymes, diagnostic imaging modalities like computed tomography (CT) scans and magnetic resonance imaging (MRI) can also detect the presence and location of liver metastasis. Treatment options for liver metastasis depend on the type and stage of cancer, and may include surgery, radiation therapy, chemotherapy, and targeted therapy (25,26).
Although AST and ALT are classic indicators of abnormal liver function, the abnormality of ALP is also closely related to liver metastasis. Therefore, exploring the regulatory relationship between ALP and AST will greatly improve the accuracy of ALP as a marker of liver cancer. In short, monitoring ALP levels along with other liver enzymes and diagnostic imaging is an important part of managing liver metastasis in cancer patients.
ALPs in pancreatic cancer
ALPs have been found to be elevated in some cases of pancreatic cancer, though the exact mechanism is not well understood (27). In one study, elevated levels of ALP were observed in approximately 30% of patients with pancreatic cancer (28). However, in combination with other tumor markers like carbohydrate antigen 19-9 (CA 19-9), elevated ALP levels may be used to aid in diagnosing pancreatic cancer (29,30). While the exact role of ALPs in pancreatic cancer is still unknown, some studies have suggested that ALP may be involved in promoting tumor growth and invasion (31-33). In animal studies, inhibiting ALP has been found to reduce the progression and metastasis of pancreatic cancer (34).
ALP is not specific to pancreatic cancer and can also be elevated in other conditions such as liver and bone disease, making it an unspecific marker of pancreatic cancer. While placental isozymes, PLALP, is localized in the pancreas, so we can study the specific mechanism of PLALP in the pancreas, and this isozyme can be further used as a marker of pancreatic cancer. Overall, while elevated ALP levels may be a potential marker for pancreatic cancer, more research is needed to fully understand the role of ALPs in pancreatic cancer progression and to identify the potential therapeutic benefit of targeting ALP in the treatment of pancreatic cancer.
ALPs in lung cancer
ALP has been found to be elevated in some cases of lung cancer, though the exact mechanism is not well understood (35). In one study, elevated levels of ALP were observed in approximately 10% of patients with lung cancer (36). In some cases, high levels of ALP in patients with lung cancer may indicate the presence of bone metastases (37). Bone metastases are a common complication of lung cancer and result in the release of ALP into the bloodstream due to the breakdown of bone tissue (38). In addition to being a potential marker of bone metastases, ALP may also be involved in promoting tumor growth and invasion in lung cancer (39). In animal studies, inhibiting ALP has been found to reduce lung cancer cell proliferation and migration (13,40,41).
In sum, while elevated ALP levels may be a potential marker of bone metastases in lung cancer patients, the clinical significance of ALP as a biomarker and its role in lung cancer progression is still unclear, and more research is needed to better understand the mechanisms underlying ALP. We know ALP dysregulation in lung cancer and accompanied by bone metastases. While tissue-nonspecific isozymes are involved in bone metabolism and mineralization, so we could detect the level of TNAP in lung cancer, to investigate the mechanism of TNAP in the proliferation and migration of lung cancer cells.
ALPs in breast cancer
ALPs have been studied in breast cancer as potential biomarkers for diagnosis, prognosis, and treatment (42). ALP has been found to be low in breast cancer, and researchers have reported a correlation between low ALP levels and a more aggressive cancer subtype, higher tumor stage, and poorer outcomes (43). Low ALP activity is associated with a higher probability of recurrence and metastasis, as well as a reduced overall survival rate in breast cancer patients (44). However, the exact mechanisms underlying the association between ALP and breast cancer progression remain unclear. In breast cancer cell lines, studies have shown that ALP may be involved in modulating the tumor microenvironment by regulating extracellular matrix (ECM) and cytokine expression, as well as cell proliferation and migration (33,40,41). Additionally, ALP may play a role in bone homeostasis and remodeling, which are important processes in the metastasis of breast cancer to the bone (45). ALP has also been studied as a potential target for breast cancer treatment (46). In vitro, high ALP-expressing breast cancer cell lines were shown to be more sensitive to treatment with some chemotherapeutic agents (47).
However, more studies are needed to explore the therapeutic potential of targeting ALP in breast cancer treatment. ALP levels in breast cancer and other cancers are diametrically opposite, suggesting that ALP functions differently in different tissues. Breast tissue is mainly tissue-nonspecific isoenzymes, future studies can explore the expression level of TNAP in different tumors and study how TNAP regulates the occurrence and development of breast cancer. In summary, low ALP activity may serve as a potential biomarker for breast cancer diagnosis and prognosis. Further research is needed to fully understand the underlying mechanisms linking ALP with breast cancer progression and to determine its therapeutic potential.
ALPs in colorectal cancer (CRC)
CRC is one of the most common malignancies worldwide, and several studies have reported that ALP levels are decreased in patients with newly diagnosed, untreated CRC (48-50). Low ALP activity has been associated with a poor prognosis in patients with advanced or metastatic CRC, indicating a correlation between low ALP expression and more aggressive tumor behaviour (49). However, the specific mechanism for this relationship is not yet well understood. In colon cancer cell lines, inhibiting ALP activity has been found to result in the promotion of cell proliferation, colony formation, and decreased tumor suppressor gene expression (50). These findings suggest that ALP modulates the growth and progression of colon cancer cells, though more research is needed to investigate the role of ALP in human CRC. Additionally, ALP has been used as a marker to monitor the effectiveness of chemotherapy in CRC patients (51). Studies have shown that elevated serum ALP levels can be reduced after chemotherapy regimens and that this reduction is associated with a better clinical outcome (51,52).
In a word, the role of ALP in the development and progression of CRC is complex and context-dependent. While low ALP activity may indicate a poor prognosis in advanced or metastatic CRC, is similar to that in breast cancer, but opposite to that in other cancers, indicating that the mechanism of ALP action in cancer is a double-edged sword. Further investigations are required to fully elucidate the underlying mechanisms and determine if it could serve as a therapeutic target.
ALPs in non-small cell lung cancer (NSCLC)
ALPs have been found to be elevated in NSCLC patients, though the exact mechanism is not well understood (53). In some cases, elevated levels of ALP in NSCLC patients may indicate the presence of bone metastases. Bone metastases are a common complication of NSCLC and result in the release of ALP into the bloodstream due to the breakdown of bone tissue (54). ALP has also been studied as a potential biomarker in NSCLC patients, though the results of studies have been inconsistent (38). Some studies have reported that high levels of ALP are associated with a poorer prognosis and shorter survival time in NSCLC patients, while others have found no significant correlation between ALP levels and prognosis in NSCLC (38,54,55). In addition to being a potential marker of bone metastases, ALP may also be involved in promoting tumor growth and invasion in NSCLC. In animal studies, inhibiting ALP has been found to reduce lung cancer cell proliferation and migration (40,41).
All in all, elevated ALP levels may be a potential marker of bone metastases in NSCLC patients, the role of ALP as a prognostic or therapeutic biomarker in NSCLC is still unclear and requires further research. ALP is not strongly correlated with the diagnosis of NSCLC, so it is necessary to identify the regulatory targets of ALP in NSCLC. While ALK fusion oncogene, EGFR mutations are served as predictive biomarkers in NSCLC, to explore the effect of ALP on ALK fusion oncogene and EGFR mutations and to use ALK and EGFR together as a diagnostic marker for NSCLC.
ALPs in testicular cancer
ALPs have been studied in testicular cancer, specifically in non-seminoma germ cell tumors (NSGCTs), and have shown potential as a diagnostic and prognostic marker (56). In NSGCT, elevations in serum ALP levels are commonly seen when there is a presence of metastases in the body, primarily bone metastases (57). Elevated ALP levels can aid in the diagnosis of NSGCT and in monitoring the treatment response of the tumor. Studies have suggested that high ALP levels in NSGCT patients are associated with an increased risk of disease recurrence and a decreased overall survival rate, indicating a potential role for ALP as a prognostic marker (57-59). ALP can also help identify chemotherapy-resistant or metastatic NSGCT, which can guide personalized treatment decisions (59). ALP has also been studied as a potential therapeutic target in NSGCT (59). In preclinical studies, inhibiting ALP activity has been found to reduce the growth and invasion of testicular cancer cells (60).
In a nutshell, the study of ALP in testicular cancer has potential in the detection, prognosis, and treatment of NSGCT. Further research is necessary to confirm the clinical significance of ALP in testicular cancer treatment. It is known that germ cell ALP isoenzyme is found in the testes, so GCAP protein is enriched in the testis tissue. Next, we can study the specific mechanism of GCAP in NSGCT, and this ALP isozyme can be further used as a marker of pancreatic cancer.
ALPs in gastric cancer (GC)
Elevated levels of ALP can be observed in the blood of some GC patients, particularly in cases with liver metastasis. High levels of ALP have been associated with poorer prognosis and shorter survival rates in GC patients (61). Elevated levels of ALP and LDH have been associated with poorer prognosis in various types of cancers, including GC (62). Studies have shown that high levels of ALP and LDH are associated with advanced tumor stage, increased metastasis, and worse overall survival in patients with unresectable advanced GC. Higher levels of ALP and LDH are indicative of greater tumor volume and aggressiveness. They are associated with larger tumor size, lymph node involvement, and the presence of distant metastases, all of which contribute to a poor prognosis (62).
Higher baseline levels of ALP and LDH have been associated with poorer response to chemotherapy and targeted therapies in GC (19). Monitoring ALP and LDH during treatment can help assess treatment efficacy and identify patients who may benefit from alternative therapies. it is important to note that the prognostic value of ALP and LDH, along with host-related factors, may vary depending on other tumor characteristics, patient demographics, and the specific treatment regimen. Assessing these factors in combination with ALP and LDH can provide a more comprehensive prognostic evaluation for patients with unresectable advanced GC (19).
ALPs in chemotherapy and radiation therapy
ALPs have been investigated as potential biomarkers for assessing the effectiveness of chemotherapy and radiation therapy in cancer treatment (25,26,51,52,59). In some types of cancer, such as testicular cancer, elevation of ALP levels in the blood can indicate the presence of chemotherapy-resistant or metastatic disease (59). In these cases, monitoring of ALP levels can be an important tool in the management of cancer treatment. ALP levels have also been studied as potential prognostic biomarkers in chemotherapy-treated cancer patients (57,58). In some studies, a reduction in ALP levels after chemotherapy has been associated with improved outcomes in certain types of cancer, including CRC and pancreatic cancer (28,29,52). This suggests that changes in ALP levels can serve as a marker for treatment response and guide personalized treatment decisions. In radiation therapy, ALP activity has been found to be increased in normal tissue after radiation-induced injury (76). This elevation in ALP levels is thought to reflect the changes in the cellular environment of the injured tissue. Studies have shown that measuring ALP levels before and after radiation therapy can provide insights into the effectiveness of the treatment and the level of tissue toxicity (76,77). To sum up, the role of ALP in assessing the effectiveness of chemotherapy and radiation therapy in cancer treatment is promising. Further research is needed to fully understand the use of ALP as a prognostic biomarker and to explore the therapeutic potential of targeting ALP in combination with chemotherapy and radiation therapy.
Challenges of ALPs in tumor diagnosis
There are several methods available for analyzing ALP activity in clinical samples. Such as enzyme assays, which measure the enzymatic activity of ALP by monitoring the conversion of substrate to product. Different substrates can be used, such as p-nitrophenyl phosphate (p-NPP) or 5-bromo-4-chloro-3-indolyl phosphate (BCIP) (78,79). If we want to improve the sensitivity and specificity of detecting and quantifying ALP activity, enzyme-linked immunosorbent assay (ELISA) or chemiluminescent immunoassay (CLIA) can be used (80,81). While ALP isoenzymes can be separated and analyzed using methods like electrophoresis or high-performance liquid chromatography (HPLC). This helps to identify different forms of ALP and distinguish them from other isoenzymes (82).
Although there are so many methods to analyze ALP activity. The biggest problem often faced in ALP analysis is the interference from other enzymes or compounds present in clinical samples. Some compounds can lead to false-positive or false-negative results, affecting the accuracy of ALP activity measurements. To overcome this problem, various measures can be taken: (I) selective inhibitors: addition of specific inhibitors can help suppress interfering enzymes while measuring ALP activity. For example, levamisole is commonly used to inhibit interference from intestinal ALP (83). (II) Sample preparation: proper sample preparation techniques, such as sample dilution or filtration, can help remove interfering substances and improve the accuracy of ALP activity measurements. (III) Validation and quality control: regular validation and quality control should be performed to monitor the accuracy and precision of the analytical methods used for ALP analysis. This ensures reliable and consistent results.
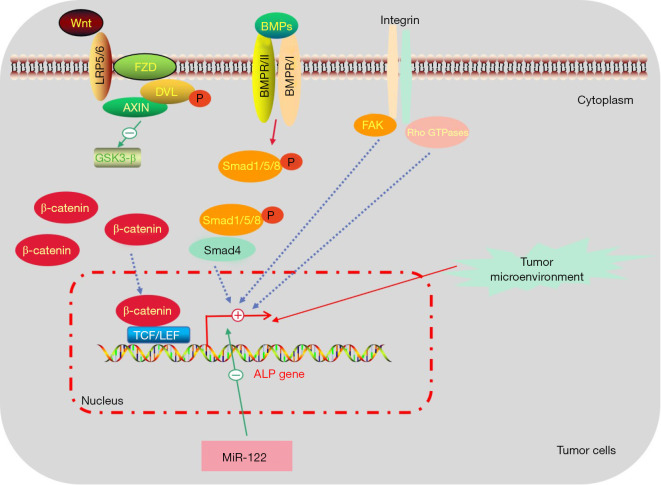
Regulation pathways of ALP in cancer
The expression of ALPs in cancer is complex and context-dependent. Its abnormal expression is associated with multiple molecular pathways (Figure 2). Activation of the Wnt/β-catenin pathway is associated with increased ALP expression in multiple cancer types, including colon, liver, and bone cancers. β-catenin translocates to the nucleus and promotes the transcription of ALP gene, leading to increased ALP production (84). Activation of bone morphogenetic protein (BMP) pathway leads to increased ALP expression in cancer cells, particularly in bone metastases of solid tumors, where tumor cells acquire osteoblastic features (85). In the tumor microenvironment, changes in ECM composition and stiffness can modulate ALP expression in cancer cells (86). Activation of integrin-mediated signaling pathways, such as focal adhesion kinase (FAK) or Rho GTPases, can upregulate ALP expression and promote cancer cell invasion and metastasis (87). MiR-122 targets ALP in hepatocellular carcinoma (liver cancer) and is associated with reduced ALP activity (88).
Figure 2.
The mechanisms underlying ALP dysregulation in tumor cells. Wnt/β-catenin pathway, BMP pathway, integrin-mediated signaling pathways, and tumor microenvironment lead to increased ALP expression in tumor cells. While MiR-122 is associated with reduced ALP activity. Wnt, Wingless-Type MMTV Integration Site Family; LRP5/6, lipoprotein receptor-associated protein 5/6; FZD, frizzled; DVL, dishevelled; GSK3-β, glycogen synthase kinase 3 beta; BMP, bone morphogenetic protein; BMPR-I/II, BMP receptor I/II; FAK, focal adhesin kinase; TCF, T-cell factor; LEF, lymphoid enhance factor; ALP, alkaline phosphatase.
More and more studies are exploring how ALP affects the occurrence and development of tumors. Therefore, we can detect the abnormal expression of upstream regulatory molecules in specific tumors, and then design targets in the upstream molecular pathways to control ALP expression.
Conclusions
ALPs have been studied extensively in various types of tumors and have shown potential as diagnostic, prognostic, and therapeutic markers. One of the key applications of ALPs in tumor diagnosis is as a marker for bone metastases (15,19,37,54,57). Elevated levels of ALPs in the blood have been shown to be associated with bone metastases in prostate cancer, breast cancer, and other types of cancer (34,36). ALP levels can be measured to determine the presence of bone metastases, which can help guide treatment decisions.
In addition to diagnosis, ALPs have also shown potential as prognostic markers in tumors (56,58,73-75). In some cancers, such as CRC, breast cancer, and NSCLC, low levels of ALP have been associated with a worse prognosis (43,44,49). This suggests that ALP activity may play a role in tumor growth and proliferation.
ALPs have also been investigated as therapeutic targets in tumors. In preclinical studies, ALP inhibitors were shown to reduce the growth and invasion of tumor cells, indicating that ALPs may play a role in tumor progression (18,76). Other studies have shown that ALP can modulate the tumor microenvironment, and that targeting ALP may be an effective strategy to treat certain tumors (33,40,41,77,86).
Furthermore, ALP levels have been used to monitor the effectiveness of cancer treatments, including chemotherapy and radiation therapy. Decreased ALP levels after treatment have been associated with improved clinical outcomes in some types of cancer, suggesting that ALP monitoring may be a useful tool in assessing treatment response (61,62).
Low ALP activity was found in CRC, and breast cancer, but opposite to that in prostate cancer, liver metastasis, pancreatic cancer, lung cancer, NSCLC and NSGCT, indicating that the mechanism of ALP action in cancer is a double-edged sword. We should analyze the regulatory mechanism of ALP in different tumors, explore the functions of different ALP isoenzymes in various tumors, and combine variety of molecular markers on cancer diagnosis.
The ALP gene overexpression and gene amplification by polyploidy of chromosomes 1 and 2 may be related in certain lesions, although it is important to note that the specific relationship can vary depending on the context and specific biological system (89). In certain lesions or diseases, such as certain types of cancer, genetic alterations can occur, leading to the overexpression of specific genes and the amplification of certain chromosomal regions. In this context, it is possible that ALP gene overexpression and gene amplification by polyploidy of chromosomes 1 and 2 are associated in these lesions. The increased number of chromosomes 1 and 2 due to polyploidy could contribute to the amplified copy number of the ALP gene, leading to its overexpression (89,90). Therefore, we need to further distinguish between these two conditions in clinical research, such as DNA copy number analysis, DNA sequencing and other methods.
In the context of ALP, there are genetic polymorphisms that can affect its expression, activity, or other characteristics. These polymorphisms can have implications for various biological processes and disease conditions (91). ALP isozyme polymorphisms, the ALPL gene encodes TNAP (Table 2), mutations or single nucleotide polymorphisms in the ALPL gene can lead to different forms of TNAP with varying enzymatic activity and stability (92). Vitamin D plays a role in the regulation of ALP expression. Polymorphisms in the vitamin D receptor (VDR) gene can affect ALP levels (92). For example, the FokI and BsmI polymorphisms in the VDR gene have been associated with ALP activity variations in different populations (93).
On the other hand, it is worth noting that a deficiency in ALP can also have negative implications for cancer patients. Studies have shown that low levels of ALPs are linked to poorer outcomes in individuals with specific types of tumors, such as CRC, breast cancer, and NSCLC (44,47-52,54,55). This is because reduced ALP activity may be indicative of decreased differentiation among cancer cells, meaning they are less specialized and more likely to grow uncontrollably. Additionally, low ALP levels could contribute to increased proliferation of malignant cells within the body (43,44,49). Therefore, it is crucial for healthcare professionals to monitor ALP levels in cancer patients and take appropriate action if deficiencies are detected. By doing so, we can help improve prognosis and ultimately save lives.
The intricate relationship between ALPs and cancer is a multifaceted one, with various factors influencing their role in the disease. To fully comprehend the mechanisms underlying ALP dysregulation in cancer, further research is imperative. Only then can we identify potential therapeutic targets that could revolutionize cancer treatment. It is important to note that the context of each individual case plays a significant role in determining how ALPs function within it. This means that there are no universal rules when it comes to understanding ALPs’ impact on cancer development and progression. Despite this complexity, researchers remain optimistic about uncovering new insights into this critical area of study. With continued investigation and collaboration across disciplines, we may be able to unlock novel approaches for treating even the most challenging forms of cancer. In conclusion, while much remains unknown about the precise nature of ALP involvement in cancer, ongoing research offers hope for future breakthroughs. By working together towards a better understanding of these complex interactions, we can pave the way for more effective treatments and ultimately improve outcomes for patients worldwide.
Overall, ALPs have shown great potential in the diagnosis, prognosis, and treatment of tumors. Further research and clinical trials are necessary to fully understand the clinical significance of ALPs in tumor management and develop effective therapeutic strategies targeting these enzymes.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: This work was supported by the Scientific Research Project of Hunan Provincial Health Committee (No. 20201915); the Emergency Special Project of Epidemic Prevention and Control of COVID-19 Pneumonia in the University of South China (No. 12); the Hengyang Science and Technology Planning Project (No. 202250045307); the Natural Science Foundation of Hunan Province (No. 2022JJ40406); and the Excellent Youth Project of Hunan Provincial Education Department (No. 22B0411).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Peer Review File: Available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-1190/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tcr.amegroups.com/article/view/10.21037/tcr-23-1190/coif). The authors have no conflicts of interest to declare.
References
- 1.Haarhaus M, Cianciolo G, Barbuto S, et al. Alkaline Phosphatase: An Old Friend as Treatment Target for Cardiovascular and Mineral Bone Disorders in Chronic Kidney Disease. Nutrients 2022;14:2124. 10.3390/nu14102124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grote-Koska D, Klauke R, Brand K, et al. Alkaline phosphatase activity - pH impact on the measurement result. Clin Chem Lab Med 2017;55:e146-9. 10.1515/cclm-2016-0771 [DOI] [PubMed] [Google Scholar]
- 3.Green MR, Sambrook J. Alkaline Phosphatase. Cold Spring Harb Protoc 2020;2020:100768. 10.1101/pdb.top100768 [DOI] [PubMed] [Google Scholar]
- 4.Zaher DM, El-Gamal MI, Omar HA, et al. Recent advances with alkaline phosphatase isoenzymes and their inhibitors. Arch Pharm (Weinheim) 2020;353:e2000011. 10.1002/ardp.202000011 [DOI] [PubMed] [Google Scholar]
- 5.Jiang Y, Li X, Walt DR. Single-Molecule Analysis Determines Isozymes of Human Alkaline Phosphatase in Serum. Angew Chem Int Ed Engl 2020;59:18010-5. 10.1002/anie.202007477 [DOI] [PubMed] [Google Scholar]
- 6.Mori K, Janisch F, Parizi MK, et al. Prognostic value of alkaline phosphatase in hormone-sensitive prostate cancer: a systematic review and meta-analysis. Int J Clin Oncol 2020;25:247-57. 10.1007/s10147-019-01578-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brichacek AL, Brown CM. Alkaline phosphatase: a potential biomarker for stroke and implications for treatment. Metab Brain Dis 2019;34:3-19. 10.1007/s11011-018-0322-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ma X, Fan Y, Chen Z, et al. Blood biomarkers of bone metastasis in digestive tract malignant tumors. Future Oncol 2021;17:1507-18. 10.2217/fon-2020-0509 [DOI] [PubMed] [Google Scholar]
- 9.Jiang C, Hu F, Xia X, et al. Prognostic value of alkaline phosphatase and bone-specific alkaline phosphatase in breast cancer: A systematic review and meta-analysis. Int J Biol Markers 2023;38:25-36. 10.1177/03936155231154662 [DOI] [PubMed] [Google Scholar]
- 10.Titaux C, Ternynck C, Pauchet M, et al. Total alkaline phosphatase levels by gestational age in a large sample of pregnant women. Placenta 2023;132:32-7. 10.1016/j.placenta.2022.12.005 [DOI] [PubMed] [Google Scholar]
- 11.Shu J, Tan A, Li Y, et al. The correlation between serum total alkaline phosphatase and bone mineral density in young adults. BMC Musculoskelet Disord 2022;23:467. 10.1186/s12891-022-05438-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xiao Y, Lu J, Chang W, et al. Dynamic serum alkaline phosphatase is an indicator of overall survival in pancreatic cancer. BMC Cancer 2019;19:785. 10.1186/s12885-019-6004-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martínez VR, Aguirre MV, Todaro JS, et al. Interaction of Zn with Losartan. Activation of Intrinsic Apoptotic Signaling Pathway in Lung Cancer Cells and Effects on Alkaline and Acid Phosphatases. Biol Trace Elem Res 2018;186:413-29. 10.1007/s12011-018-1334-x [DOI] [PubMed] [Google Scholar]
- 14.Has Simsek D, Kuyumcu S, Karadogan S, et al. Outcome of 177 Lu-PSMA Radionuclide Treatment in Advanced Prostate Cancer and Its Association With Clinical Parameters: A Single-Center Experience. Clin Nucl Med 2022;47:e521-8. 10.1097/RLU.0000000000004222 [DOI] [PubMed] [Google Scholar]
- 15.Gardani CFF, Cappellari AR, de Souza JB, et al. Hydrolysis of ATP, ADP, and AMP is increased in blood plasma of prostate cancer patients. Purinergic Signal 2019;15:95-105. 10.1007/s11302-018-9642-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmed ME, Joshi VB, Badawy M, et al. Radium-223 in the Third-Line Setting in Metastatic Castration-Resistant Prostate Cancer: Impact of Concomitant Use of Enzalutamide on Overall Survival (OS) and Predictors of Improved OS. Clin Genitourin Cancer 2021;19:223-9. 10.1016/j.clgc.2020.12.009 [DOI] [PubMed] [Google Scholar]
- 17.Yordanova A, Linden P, Hauser S, et al. The value of tumor markers in men with metastatic prostate cancer undergoing [177Lu]Lu-PSMA therapy. Prostate 2020;80:17-27. 10.1002/pros.23912 [DOI] [PubMed] [Google Scholar]
- 18.Yao D, Yang S, Wang Y, et al. An ALP-activatable and mitochondria-targeted probe for prostate cancer-specific bimodal imaging and aggregation-enhanced photothermal therapy. Nanoscale 2019;11:6307-14. 10.1039/C9NR00913B [DOI] [PubMed] [Google Scholar]
- 19.Schlack K, Krabbe LM, Rahbar K, et al. ALP bouncing and LDH normalization in bone metastatic castration-resistant prostate cancer patients under therapy with Enzalutamide: an exploratory analysis. Transl Androl Urol 2021;10:3986-99. 10.21037/tau-20-1117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tripathi T, Gupta P, Sharma J, et al. Bone-specific alkaline phosphatase - a potential biomarker for skeletal growth assessment. J Orthod 2018;45:4-10. 10.1080/14653125.2017.1416571 [DOI] [PubMed] [Google Scholar]
- 21.Zhan J, Wang Y, Ma S, et al. Organelle-inspired supramolecular nanomedicine to precisely abolish liver tumor growth and metastasis. Bioact Mater 2021;9:120-33. 10.1016/j.bioactmat.2021.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suzuki K, Masuike Y, Mizuno R, et al. LIN28B induces a differentiation program through CDX2 in colon cancer. JCI Insight 2021;6:e140382. 10.1172/jci.insight.140382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cotogno PM, Ranasinghe LK, Ledet EM, et al. Laboratory-Based Biomarkers and Liver Metastases in Metastatic Castration-Resistant Prostate Cancer. Oncologist 2018;23:791-7. 10.1634/theoncologist.2017-0564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colomba E, Marret G, Baciarello G, et al. Liver tests increase on abiraterone acetate in men with metastatic prostate cancer: Natural history, management and outcome. Eur J Cancer 2020;129:117-22. 10.1016/j.ejca.2020.01.017 [DOI] [PubMed] [Google Scholar]
- 25.Cho MJ, An C, Aljoqiman KS, et al. Diagnostic performance of Liver Imaging Reporting and Data System in patients at risk of both hepatocellular carcinoma and metastasis. Abdom Radiol (NY) 2020;45:3789-99. 10.1007/s00261-020-02581-9 [DOI] [PubMed] [Google Scholar]
- 26.Laun FB, Führes T, Seuss H, et al. Flow-compensated diffusion encoding in MRI for improved liver metastasis detection. PLoS One 2022;17:e0268843. 10.1371/journal.pone.0268843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qiu G, Zhang L, Gu Z, et al. Preoperative Alkaline Phosphatase-to-Cholesterol Ratio as a Predictor of Overall Survival in Pancreatic Ductal Adenocarcinoma Patients Undergoing Radical Pancreaticoduodenectomy. Med Sci Monit 2021;27:e931868. 10.12659/MSM.931868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang K, Dong S, Jing YH, et al. Albumin-to-alkaline phosphatase ratio serves as a prognostic indicator in unresectable pancreatic ductal adenocarcinoma: a propensity score matching analysis. BMC Cancer 2020;20:541. 10.1186/s12885-020-07023-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Engle DD, Tiriac H, Rivera KD, et al. The glycan CA19-9 promotes pancreatitis and pancreatic cancer in mice. Science 2019;364:1156-62. 10.1126/science.aaw3145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fahrmann JF, Schmidt CM, Mao X, et al. Lead-Time Trajectory of CA19-9 as an Anchor Marker for Pancreatic Cancer Early Detection. Gastroenterology 2021;160:1373-83.e6. 10.1053/j.gastro.2020.11.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zi X, Zhang G, Qiu S. Up-regulation of LINC00619 promotes apoptosis and inhibits proliferation, migration and invasion while promoting apoptosis of osteosarcoma cells through inactivation of the HGF-mediated PI3K-Akt signalling pathway. Epigenetics 2022;17:147-60. 10.1080/15592294.2021.1890873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wessely A, Waltera A, Reichert TE, et al. Induction of ALP and MMP9 activity facilitates invasive behavior in heterogeneous human BMSC and HNSCC 3D spheroids. FASEB J 2019;33:11884-93. 10.1096/fj.201900925R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang F, Liu R, Zhang H, et al. Suppressing Dazl modulates tumorigenicity and stemness in human glioblastoma cells. BMC Cancer 2020;20:673. 10.1186/s12885-020-07155-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fu H, Tang B, Lang J, et al. High-Fat Diet Promotes Macrophage-Mediated Hepatic Inflammation and Aggravates Diethylnitrosamine-Induced Hepatocarcinogenesis in Mice. Front Nutr 2020;7:585306. 10.3389/fnut.2020.585306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Siva S, Bressel M, Wood ST, et al. Stereotactic Radiotherapy and Short-course Pembrolizumab for Oligometastatic Renal Cell Carcinoma-The RAPPORT Trial. Eur Urol 2022;81:364-72. 10.1016/j.eururo.2021.12.006 [DOI] [PubMed] [Google Scholar]
- 36.Katzke V, Johnson T, Sookthai D, et al. Circulating liver enzymes and risks of chronic diseases and mortality in the prospective EPIC-Heidelberg case-cohort study. BMJ Open 2020;10:e033532. 10.1136/bmjopen-2019-033532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sandfeld-Paulsen B, Aggerholm-Pedersen N, Winther-Larsen A. Pretreatment Albumin-to-Alkaline Phosphatase Ratio Is a Prognostic Marker in Lung Cancer Patients: A Registry-Based Study of 7077 Lung Cancer Patients. Cancers (Basel) 2021;13:6133. 10.3390/cancers13236133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu X, Li Y, Zhao Q, et al. Albumin-to-alkaline phosphatase ratio: A novel prognostic index for patients with driver mutation-negative advanced non-small cell lung cancer. Clin Respir J 2021;15:540-9. 10.1111/crj.13339 [DOI] [PubMed] [Google Scholar]
- 39.Zheng D, Chen Y, Ai S, et al. Tandem Molecular Self-Assembly Selectively Inhibits Lung Cancer Cells by Inducing Endoplasmic Reticulum Stress. Research (Wash D C) 2019;2019:4803624. 10.34133/2019/4803624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhou S, Wang H, Jiang W, et al. Prognostic Value of Pretreatment Albumin-to-Alkaline Phosphatase Ratio in Extensive-Disease Small-Cell Lung Cancer: A Retrospective Cohort Study. Cancer Manag Res 2020;12:2015-24. 10.2147/CMAR.S247967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lou Z, Lin W, Zhao H, et al. Alkaline phosphatase downregulation promotes lung adenocarcinoma metastasis via the c-Myc/RhoA axis. Cancer Cell Int 2021;21:217. 10.1186/s12935-021-01919-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moura SL, Pallarès-Rusiñol A, Sappia L, et al. The activity of alkaline phosphatase in breast cancer exosomes simplifies the biosensing design. Biosens Bioelectron 2022;198:113826. 10.1016/j.bios.2021.113826 [DOI] [PubMed] [Google Scholar]
- 43.Aqeel Rashid F, Mahdi S, Abd-Alkader Mahdy S, et al. Effect of Obesity on Plasma Alkaline Phosphatase Activity in Breast Cancer. Rep Biochem Mol Biol 2021;10:307-13. 10.52547/rbmb.10.2.307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yazdani A, Dorri S, Atashi A, et al. Bone Metastasis Prognostic Factors in Breast Cancer. Breast Cancer (Auckl) 2019;13:1178223419830978. 10.1177/1178223419830978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gentile M, Centonza A, Lovero D, et al. Application of "omics" sciences to the prediction of bone metastases from breast cancer: State of the art. J Bone Oncol 2020;26:100337. 10.1016/j.jbo.2020.100337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tayubi IA, Madar IH. Biomineralization associated alkaline phosphatase as a potential marker of bone metastasis in the patients with invasive breast cancer. Saudi J Biol Sci 2022;29:103340. 10.1016/j.sjbs.2022.103340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fushimi A, Takeyama H, Tachibana T, et al. Osteogenic cocktail induces calcifications in human breast cancer cell line via placental alkaline phosphatase expression. Sci Rep 2020;10:12669. 10.1038/s41598-020-69622-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Park HS, Chun YJ, Kim HS, et al. Clinical features and KRAS mutation in colorectal cancer with bone metastasis. Sci Rep 2020;10:21180. 10.1038/s41598-020-78253-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Qader G, Aali M, Smail SW, et al. Cardiac, Hepatic and Renal Dysfunction and IL-18 Polymorphism in Breast, Colorectal, and Prostate Cancer Patients. Asian Pac J Cancer Prev 2021;22:131-7. 10.31557/APJCP.2021.22.1.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li AA, Cao ZY, Liu JM, et al. The risk factors for bone metastases in patients with colorectal cancer. Medicine (Baltimore) 2018;97:e12694. 10.1097/MD.0000000000012694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nemoto T, Endo S, Isohata N, et al. Change in the neutrophil-to-lymphocyte ratio during chemotherapy may predict prognosis in patients with advanced or metastatic colorectal cancer. Mol Clin Oncol 2021;14:107. 10.3892/mco.2021.2269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kachur O, Fira L, Lykhatskyi P, et al. Evaluation of membrane-destructive processes in rats with induced carcinogenesis of the colon using the cytostatic vincristine. Rocz Panstw Zakl Hig 2022;73:215-20. [DOI] [PubMed] [Google Scholar]
- 53.Li D, Yu H, Li W. Albumin-to-alkaline phosphatase ratio at diagnosis predicts survival in patients with metastatic non-small-cell lung cancer. Onco Targets Ther 2019;12:5241-9. 10.2147/OTT.S203321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wu XT, Zhou JW, Pan LC, et al. Clinical features and prognostic factors in patients with bone metastases from non-small cell lung cancer. J Int Med Res 2020;48:300060520925644. 10.1177/0300060520925644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang T, Cheng J, Fu S, et al. Pretreatment levels of serum alkaline phosphatase are associated with the prognosis of patients with non-small cell lung cancer receiving immune checkpoint inhibitors. Oncol Lett 2023;25:154. 10.3892/ol.2023.13740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Barrachina F, de la Iglesia A, Jodar M, et al. Histone H4 acetylation is dysregulated in active seminiferous tubules adjacent to testicular tumours. Hum Reprod 2022;37:1712-26. 10.1093/humrep/deac130 [DOI] [PubMed] [Google Scholar]
- 57.Takasawa T, Minagawa T, Domen T, et al. Successful management of testicular primitive neuroectodermal tumor with multiple bone metastases. IJU Case Rep 2022;5:179-82. 10.1002/iju5.12431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Basiri M, Pahlavanneshan S. Evaluation of Placental Alkaline Phosphatase Expression as A Potential Target of Solid Tumors Immunotherapy by Using Gene and Protein Expression Repositories. Cell J 2021;23:717-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smith ZL, Werntz RP, Eggener SE. Testicular Cancer: Epidemiology, Diagnosis, and Management. Med Clin North Am 2018;102:251-64. 10.1016/j.mcna.2017.10.003 [DOI] [PubMed] [Google Scholar]
- 60.Mohammadzadeh S, Kiani A, Amiri M. Lycopene modulates hepatic toxicity and testicular injury induced by etoposide in male rats. F S Sci 2023;4:30-5. 10.1016/j.xfss.2022.07.005 [DOI] [PubMed] [Google Scholar]
- 61.Slagter AE, Vollebergh MA, Caspers IA, et al. Prognostic value of tumor markers and ctDNA in patients with resectable gastric cancer receiving perioperative treatment: results from the CRITICS trial. Gastric Cancer 2022;25:401-10. 10.1007/s10120-021-01258-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Namikawa T, Ishida N, Tsuda S, et al. Prognostic significance of serum alkaline phosphatase and lactate dehydrogenase levels in patients with unresectable advanced gastric cancer. Gastric Cancer 2019;22:684-91. 10.1007/s10120-018-0897-8 [DOI] [PubMed] [Google Scholar]
- 63.Makris K, Mousa C, Cavalier E. Alkaline Phosphatases: Biochemistry, Functions, and Measurement. Calcif Tissue Int 2023;112:233-42. 10.1007/s00223-022-01048-x [DOI] [PubMed] [Google Scholar]
- 64.Okamoto M, Yamaguchi S, Ishi Y, et al. Diagnostic Capability of Cerebrospinal Fluid-Placental Alkaline Phosphatase Value in Intracranial Germ Cell Tumor. Oncology 2021;99:23-31. 10.1159/000509395 [DOI] [PubMed] [Google Scholar]
- 65.Chiba K, Aihara Y, Kawamata T. Precise detection of the germinomatous component of intracranial germ cell tumors of the basal ganglia and thalamus using placental alkaline phosphatase in cerebrospinal fluid. J Neurooncol 2021;152:405-13. 10.1007/s11060-021-03715-9 [DOI] [PubMed] [Google Scholar]
- 66.Hirschmugl B, Crozier S, Matthews N, et al. Relation of placental alkaline phosphatase expression in human term placenta with maternal and offspring fat mass. Int J Obes (Lond) 2018;42:1202-10. 10.1038/s41366-018-0136-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chiba K, Aihara Y, Komori T, et al. Placental alkaline phosphatase in cerebrospinal fluid as a biomarker for optimizing surgical treatment strategies for pineal region germ cell tumors. Brain Tumor Pathol 2020;37:60-8. 10.1007/s10014-020-00364-0 [DOI] [PubMed] [Google Scholar]
- 68.Alvarenga L, Cardozo LFMF, Lindholm B, et al. Intestinal alkaline phosphatase modulation by food components: predictive, preventive, and personalized strategies for novel treatment options in chronic kidney disease. EPMA J 2020;11:565-79. 10.1007/s13167-020-00228-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nakaoka K, Yamada A, Noda S, et al. Vitamin D-restricted high-fat diet down-regulates expression of intestinal alkaline phosphatase isozymes in ovariectomized rats. Nutr Res 2018;53:23-31. 10.1016/j.nutres.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 70.Soma K, Izumi M, Yamamoto Y, et al. In Vitro and In Vivo Pharmacological Profiles of DS-1211, a Novel Potent, Selective, and Orally Bioavailable Tissue-Nonspecific Alkaline Phosphatase Inhibitor. J Bone Miner Res 2022;37:2033-43. 10.1002/jbmr.4680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sato M, Saitoh I, Kiyokawa Y, et al. Tissue-Nonspecific Alkaline Phosphatase, a Possible Mediator of Cell Maturation: Towards a New Paradigm. Cells 2021;10:3338. 10.3390/cells10123338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pan WJ, Pradhan R, Pelto R, et al. Pharmacokinetics of Asfotase Alfa in Adult Patients With Pediatric-Onset Hypophosphatasia. J Clin Pharmacol 2021;61:1334-43. 10.1002/jcph.1870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nizet A, Cavalier E, Stenvinkel P, et al. Bone alkaline phosphatase: An important biomarker in chronic kidney disease - mineral and bone disorder. Clin Chim Acta 2020;501:198-206. 10.1016/j.cca.2019.11.012 [DOI] [PubMed] [Google Scholar]
- 74.Kalahasthi R, Barman T, Bagepally BS. Assessment of Bone Turnover Biomarkers in Lead-Battery Workers with Long-Term Exposure to Lead. Int J Occup Environ Med 2020;11:140-7. 10.34172/ijoem.2020.1951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Reiswich V, Gorbokon N, Luebke AM, et al. Pattern of placental alkaline phosphatase (PLAP) expression in human tumors: a tissue microarray study on 12,381 tumors. J Pathol Clin Res 2021;7:577-89. 10.1002/cjp2.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Movahedi MM, Karimaghaei GR, Noori A, et al. Changes in Serum Alkaline Phosphatase, Calcium, and Parathyroid Hormone with Different Doses of Iodine Therapy: Galen Med J 2022;11:e2397. 10.31661/gmj.v11i.2397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim E, Sher A, Abboud G, et al. Radiation segmentectomy for curative intent of unresectable very early to early stage hepatocellular carcinoma (RASER): a single-centre, single-arm study. Lancet Gastroenterol Hepatol 2022;7:843-50. 10.1016/S2468-1253(22)00091-7 [DOI] [PubMed] [Google Scholar]
- 78.Wang HB, Tao BB, Wu NN, et al. Glutathione-stabilized copper nanoclusters mediated-inner filter effect for sensitive and selective determination of p-nitrophenol and alkaline phosphatase activity. Spectrochim Acta A Mol Biomol Spectrosc 2022;271:120948. 10.1016/j.saa.2022.120948 [DOI] [PubMed] [Google Scholar]
- 79.Sun D, Cao F, Cong L, et al. Cellular heterogeneity identified by single-cell alkaline phosphatase (ALP) via a SERRS-microfluidic droplet platform. Lab Chip 2019;19:335-42. 10.1039/C8LC01006D [DOI] [PubMed] [Google Scholar]
- 80.Zheng S, Zhou C, Yang H, et al. Melatonin Accelerates Osteoporotic Bone Defect Repair by Promoting Osteogenesis-Angiogenesis Coupling. Front Endocrinol (Lausanne) 2022;13:826660. 10.3389/fendo.2022.826660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Karadeniz B, Gur C, Cakir D, et al. The relationship between glycemic control and osteocalcin, type 1 collagen C-terminal telopeptide, bone-specific alkaline phosphatase and the effects of anti-diabetic regimens on circulating markers of bone turnover in newly diagnosed diabetic patients: Bone health in diabetics. Clin Nephrol 2021;96:96-104. 10.5414/CN110394 [DOI] [PubMed] [Google Scholar]
- 82.Rao H, Ahmad S, Madni A, et al. Single-step extraction for simultaneous quantification of desvenlafaxine and alprazolam in human spiked plasma by RP-HPLC. PLoS One 2020;15:e0238954. 10.1371/journal.pone.0238954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hatayama K, Nishihara Y, Kimura S, et al. Alkaline phosphatase isoenzymes in mouse plasma detected by polyacrylamide-gel disk electrophoresis. J Toxicol Sci 2011;36:211-9. 10.2131/jts.36.211 [DOI] [PubMed] [Google Scholar]
- 84.Shen J, Sun Y, Liu X, et al. EGFL6 regulates angiogenesis and osteogenesis in distraction osteogenesis via Wnt/β-catenin signaling. Stem Cell Res Ther 2021;12:415. 10.1186/s13287-021-02487-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ishida M, Kawao N, Mizukami Y, et al. Serpinb1a suppresses osteoclast formation. Biochem Biophys Rep 2021;26:101004. 10.1016/j.bbrep.2021.101004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shen Y, Jing D, Zhao Z. The effect of AKT in extracellular matrix stiffness induced osteogenic differentiation of hBMSCs. Cell Signal 2022;99:110404. 10.1016/j.cellsig.2022.110404 [DOI] [PubMed] [Google Scholar]
- 87.Chen NX, Chen X, O'Neill KD, et al. RhoA/Rho kinase (ROCK) alters fetuin-A uptake and regulates calcification in bovine vascular smooth muscle cells (BVSMC). Am J Physiol Renal Physiol 2010;299:F674-80. 10.1152/ajprenal.00730.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shao D, Wang C, Sun Y, et al. Effects of oral implants with miR-122-modified cell sheets on rat bone marrow mesenchymal stem cells. Mol Med Rep 2018;17:1537-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hofmann MC, Jeltsch W, Brecher J, et al. Alkaline phosphatase isozymes in human testicular germ cell tumors, their precancerous stage, and three related cell lines. Cancer Res 1989;49:4696-700. [PubMed] [Google Scholar]
- 90.Almstrup K, Hoei-Hansen CE, Nielsen JE, et al. Genome-wide gene expression profiling of testicular carcinoma in situ progression into overt tumours. Br J Cancer 2005;92:1934-41. 10.1038/sj.bjc.6602560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.İbrahim A, Esra GT, Burcu GY, et al. The effect of ALPL gene polymorphism on the development of urolithiasis in the Turkish population. Urolithiasis 2022;51:23. 10.1007/s00240-022-01396-1 [DOI] [PubMed] [Google Scholar]
- 92.Guarnieri V, Sileri F, Indirli R, et al. Clinical, biochemical and genetic findings in adult patients with chronic hypophosphatasemia. J Endocrinol Invest 2022;45:125-37. 10.1007/s40618-021-01625-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shahmoradi A, Aghaei A, Ghaderi K, et al. A meta-analysis of the association of ApaI, BsmI, FokI, and TaqI polymorphisms in the vitamin D receptor gene with the risk of polycystic ovary syndrome in the Eastern Mediterranean Regional Office population. Int J Reprod Biomed 2022;20:433-46. 10.18502/ijrm.v20i6.11439 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as