Abstract
Purpose:
Chemoimmunotherapy (chemoIO) is a prevalent first-line treatment for advanced driver-negative non–small cell lung cancer (NSCLC), with maintenance therapy given after induction. However, there is significant clinical variability in the duration, dosing, and timing of maintenance therapy after induction chemoIO. We used circulating tumor DNA (ctDNA) monitoring to inform outcomes in patients with advanced NSCLC receiving chemoIO.
Experimental Design:
This retrospective study included 221 patients from a phase III trial of atezolizumab+carboplatin+nab-paclitaxel versus carboplatin+nab-paclitaxel in squamous NSCLC (IMpower131). ctDNA monitoring used the FoundationOne Tracker involving comprehensive genomic profiling of pretreatment tumor tissue, variant selection using an algorithm to exclude nontumor variants, and multiplex PCR of up to 16 variants to detect and quantify ctDNA.
Results:
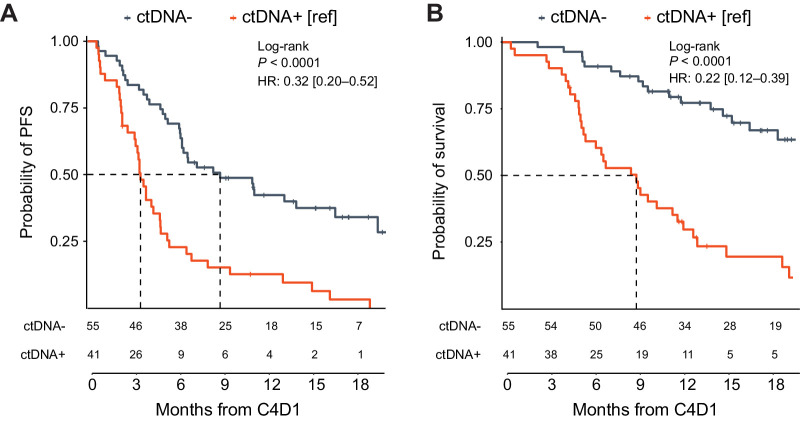
ctDNA was detected (ctDNA+) in 96% of pretreatment samples (median, 93 mean tumor molecules/mL), and similar ctDNA dynamics were noted across treatment arms during chemoIO. ctDNA decrease from baseline to C4D1 was associated with improved outcomes across multiple cutoffs for patients treated with chemoIO. When including patients with missing plasma or ctDNA- at baseline, patients with ctDNA- at C4D1 (clearance), had more favorable progression-free survival (median 8.8 vs. 3.5 months; HR, 0.32;0.20–0.52) and OS (median not reached vs. 8.9 months; HR, 0.22; 0.12–0.39) from C4D1 than ctDNA+ patients.
Conclusions:
ctDNA monitoring during induction chemoIO can inform treatment outcomes in patients with advanced NSCLC. Importantly, monitoring remains feasible and informative for patients missing baseline ctDNA. ctDNA testing during induction chemoIO identifies patients at higher risk for disease progression and may inform patient selection for novel personalized maintenance or second-line treatment strategies.
Translational Relevance.
Monitoring of circulating tumor DNA (ctDNA) has emerged as a potentially powerful tool for understanding therapeutic benefit in patients with advanced cancer. Here, we investigate a novel method for personalized ctDNA tracking leveraging historical tissue comprehensive genomic profiling results with algorithmic identification of tumor variants for highly sensitive monitoring. We found that ctDNA changes (decrease or complete clearance) prior to maintenance therapy can distinguish patients that achieve a durable benefit from those at risk for early disease progression. Notably, this insight can be gained without pretreatment ctDNA testing, as ctDNA detection following induction chemoimmunotherapy was highly prognostic. Moreover, longitudinal monitoring throughout induction provided additional prognostic insight, offering the possibility to continually tailor therapy strategies. These data point to tumor-informed ctDNA monitoring as a powerful tool for understanding the effect of investigational therapies, identifying patients at higher risk for disease progression, and informing patient selection for novel personalized maintenance treatment strategies.
Introduction
Immune checkpoint inhibitors (ICI) have revolutionized the treatment of advanced non–small cell lung cancer (NSCLC) due to the potential for durable clinical benefit, contributing to measurable improvements in patient survival (1–3). While ICI can be very active as single agents (4–7), particularly in patients with high tumoral programmed death-ligand 1 (PD-L1) expression or high tumor mutational burden (TMB), chemotherapy is often added to ICI to reduce the risk of early progression (8). Per clinical guidelines (9), the addition of chemotherapy to ICI can be considered for driver-negative NSCLC in the absence of a positive-selection biomarker (e.g., PD-L1 IHC), in patients with a high tumor burden, or when molecular profiling for negative selection biomarkers (e.g., EGFR, ALK) is incomplete.
The variable benefit seen across patients treated with ICI, and occasional equivocal response patterns on imaging (10–12), showcase the need for novel biomarkers for risk and response stratification. This clinical uncertainty persists in patients receiving ICI plus chemotherapy [chemo-immunotherapy (chemoIO)]. The landmark clinical trials of chemoIO were designed with four to six cycles of induction chemoIO followed by platinum-free maintenance therapy for up to 2 years (1, 13–15). However, the real-world adoption of maintenance therapy is variable in terms of timing, duration, and dosing (16). Moreover, the duration of response during maintenance therapy is unpredictable with a subset of patients achieving durable response and others developing rapid disease progression (1, 17–20). Currently, there are no biomarkers established to inform maintenance treatment strategies. In this setting, biomarkers like circulating tumor DNA (ctDNA) may offer an opportunity to risk stratify patients and identify those who will most likely achieve durable benefit (21–24). Early response biomarkers predicting downstream survival could also be beneficial for analysis of ICI clinical trials, given imaging endpoints do not always correlate with overall survival (OS; refs. 25–27).
Here, we aimed to determine whether ctDNA monitoring during chemoIO induction using FoundationOne Tracker, an emerging ctDNA methodology, which enables personalized ctDNA monitoring by leveraging a patient's historical tissue comprehensive genomic profiling (CGP) results, could reliably identify patients responding to treatment and predict the durability of immunotherapy benefit. We hypothesized that ctDNA analysis during induction treatment can inform patient outcomes and provide data to potentially personalize induction therapy duration and maintenance treatment strategies. To study this, we leveraged the IMpower131 study, a completed phase III trial evaluating chemotherapy versus chemoIO in patients with advanced squamous NSCLC with historical tissue CGP available as well as plasma specimens banked for ctDNA monitoring (13).
Materials and Methods
Patients and study design
Patients prospectively treated as part of the completed phase III IMpower131 trial (NCT02367794) were retrospectively selected for inclusion based on the availability of tissue CGP results (as reported previously; ref. 28) and baseline/on-treatment plasma samples. Briefly, this trial enrolled patients with stage IV squamous NSCLC and randomized them to receive atezolizumab+carboplatin+nab-paclitaxel (A+CnP) or carboplatin+nab-paclitaxel (CnP) for the primary outcome analysis; a third arm received atezolizumab+carboplatin+paclitaxel (A+CP) and was analyzed secondarily. Patients were treated with four or six cycles of induction therapy, and patients treated with atezolizumab continued receiving it as maintenance therapy until disease progression. Baseline PD-L1 tumor expression was evaluated in archival tissue or tissue obtained from a biopsy at screening using the SP142 PD-L1 IHC assay (Ventana Medical Systems, Inc., Tucson, AZ) and was scored by a central laboratory, as previously described (29). Expression from tumor cells (TC) and tumor-infiltrating immune cells (IC) was considered for stratifying patients into 3 groups based off PD-L1 expression: TC3 or IC3 (high expression: PD-L1 expression on ≥ 50% of TC or ≥ 10% of IC), TC1/2 or IC1/2 (low expression: PD-L1 expression on ≥ 1% of TC or IC and < 50% of TC and < 10% of IC), and TC0 and IC0 (negative: PD-L1 expression on < 1% of TC and IC). Tissue and plasma collection for research was not a requirement for trial enrollment; rather, written informed consent from the patients was obtained separately for the collection and use of their samples for future research. These studies were conducted in accordance with the Declaration of Helsinki and approved by an institutional review board.
Tissue CGP to enable patient-specific monitoring
Tissue CGP was performed using a clinical trial assay version of Foundation Medicine tissue testing (>300-gene panel, as described previously; ref. 28) to identify patient-specific alterations, which informed the design for the FoundationOne Tracker (ctDNA) assay, a tissue-informed personalized assay for ctDNA monitoring, as described previously (30). Tissue CGP results were only available for the A+CnP and CnP arms (133 and 120 patients respectively), which constituted the primary analysis population of the IMpower131 trial (13). For CGP results that passed quality control metrics, a novel, proprietary algorithm was used to select up to 16 alterations (substitutions and short indels) from both exonic and intronic regions in the CGP results while excluding non-tumor–derived variants (germline, clonal hematopoiesis (CH)-derived, sequencing artifacts). Alterations include likely or known pathogenic variants, variants of unknown significance in coding regions, variants in noncoding regions, and synonymous variants. To move forward with ctDNA analysis, a minimum of two patient-specific variants must have been identified for monitoring. The selected alterations were used to design PCR amplicons with optimized design parameters, ensuring robust specificity and sensitivity (30).
Plasma ctDNA monitoring analysis
Blood was collected in cell-free DNA (cfDNA) BCT tubes (Streck, La Vista, NE) at the beginning of treatment cycles 1, 2, 3, 4, and 8. ctDNA testing was performed retrospectively on cfDNA extracted from 2 to 5 mL of plasma, as previously described (31). Using the proprietary algorithm, a confidence score was calculated for each target variant detected, as previously described (30). Tumor DNA detection in the plasma was determined on the basis of a validated combined confidence level that considers all patient-specific variants of the assay. A ctDNA-positive call required the detection of at least two patient-specific variants above the selected confidence threshold (30). ctDNA levels were reported in mean tumor molecules per mL of plasma (MTM/mL). The A+CP arm was excluded from analysis due to lack of tissue, baseline plasma, or patient consent.
Statistical analysis
To minimize bias, ctDNA measurements were conducted with blinding to clinical data and patient treatment. Clinical data collection was conducted without the knowledge of ctDNA measurements. For the primary analyses, ctDNA results at cycle 4, day 1 (C4D1) were classified as a binary variable (detected/not detected) to determine the association between investigator-assessed progression-free survival (PFS), OS, and best overall response/objective response rate (ORR) with the detection of ctDNA at the start of cycle 4 (C4D1). Secondary analyses investigated quantitative changes in ctDNA (MTM/mL; ΔctDNA) from baseline to C4D1 during chemoIO treatment. Patients who had negative ctDNA levels (ctDNA-) at baseline were excluded from these analyses. On the basis of prior studies, prespecified cutoffs of any decrease (30), ≥50% (22), and 100% decrease (full clearance; ref. 32) were used to stratify patients. PFS and OS analyses were landmarked from C4D1 unless otherwise stated; patients with progression/death before the landmark date were excluded. Kaplan–Meier curves were used to estimate and visualize the survival distributions in ctDNA increasing and decreasing groups. Log-rank test was used to evaluate the significance of the effect of ΔctDNA on PFS and OS. Both univariate Cox proportional hazards regression model and multivariate models adjusting for prognostic and predictive covariates were used to estimate the hazard ratios. r version 4.2.1 (www.r-project.org/) software was used for all statistical analyses and ggplot2 and survminer for visualization. Additional exploratory analyses were performed using a 90% decrease cutoff, ctDNA detection in plasma samples from the start of cycle 2 (C2D1), start of cycle 3 (C3D1), and start of cycle 8 (C8D1), and PFS/OS differences between four and six cycles of induction in ctDNA+ patients at C4D1, which were landmarked from the relevant treatment timepoint.
Data availability statement
All relevant data are provided within the article and its accompanying Supplementary Data. Because of Health Insurance Portability and Accountability Act requirements, we are not consented to share individualized patient genomic data, which contains potentially identifying or sensitive patient information. Foundation Medicine is committed to collaborative data analysis, and we have well-established and widely used mechanisms by which investigators can query our core genomic database of >600,000 deidentified sequenced cancers to obtain aggregated datasets. More information and mechanisms for data access can be obtained by contacting the corresponding authors or the Foundation Medicine Data Governance Council at data.governance.council@foundationmedicine.com. For IMpower131, qualified researchers may request access to individual patient-level data through the clinical study data request platform (https://vivli.org/members/enquiries-about-studies-not-listed-on-the-vivli-platform [vivli.org]/).
Results
Study cohort
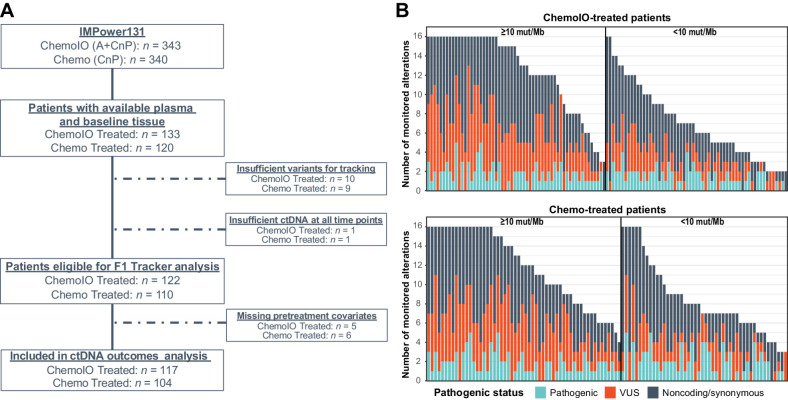
Both historical tissue CGP results and baseline/on-treatment plasma samples were available for research from a total of 253 patients treated with either A+CnP (chemoIO) or CnP (chemo). Nineteen patients (8%) were excluded across both treatment arms due to insufficient variants (<2 variants per sample) detected by tissue CGP to enable analysis with the ctDNA assay. Two additional patients (0.7%) had insufficient cfDNA extracted across all plasma samples and were excluded. Therefore, 232 of 253 patients (92%) with historical tissue profiling and plasma samples available were eligible for ctDNA analysis. For survival analysis, 11 patients were excluded due to missing baseline clinical characteristics, leaving a total of 221 patients for ctDNA outcomes analysis (Fig. 1A). Across the 221 patients included in the survival analyses, a median of 10 variants (range, 2–16) from baseline tissue CGP were selected for tracking, and no differences in the number of detected variants were seen in patients across the two treatment arms (chemoIO: 10 vs. chemo: 9.5). For patients with high TMB (≥10 mut/Mb) detected in tissue CGP, a median of 13 variants (range, 3–16) were tracked per patient, compared with a median of 7 (range, 2–16) for patients with low TMB (<10 mut/Mb) tumors (Fig. 1B).
Figure 1.
Patient cohort for analysis. Per the CONSORT diagram (A), of 253 patients with tissue NGS results and plasma available, 232 (92%) were eligible for analysis using FoundationOne Tracker and 221 (87%) were included in ctDNA outcomes analysis. B, Distribution and number of monitorable variants per patient according to pathogenic status and TMB. Across the 221 patients with sufficient variants for FoundationOne Tracker, the median number of trackable variants was 13 in those with TMB ≥ 10 and 7 in those with TMB < 10. Chemo, chemotherapy; ChemoIO, chemotherapy plus immunotherapy; NGS, next-generation sequencing; VUS, variant of unknown significance.
Clinical and demographic characteristics of patients in this study were largely similar to the intention-to-treat population from the IMpower131 trial (8). The median age was 64 years (range, 23–81), and 85% of patients were male. Ninety-five percent of patients were previous or current smokers. High PD-L1 expression was detected in 15%, low expression in 48%, and negative expression in 37% of the patients (Supplementary Table S1). Genomic alterations detected by CGP were similar to those previously described in squamous cell NSCLC (33). TP53 (90%), CDKN2A (23%), KMT2D (19%), and PIK3CA (12%) alterations were the most frequently detected, and CDKN2A homozygous deletions (26%) and amplifications of genes on chromosome 3q26, such as SOX2 (28%) and PRKCI (19%), as well as PIK3CA amplifications (22%) were also frequently observed. No ALK fusions were detected, and three patients had EGFR mutations (two concurrent G719S/S768I; one L858R; Supplementary Fig. S1A). Median TMB was 10.5 mut/Mb (range, 0.9–91.3), and high TMB was observed in 114 tissue samples (52%; Supplementary Fig. S1B; refs. 33–35).
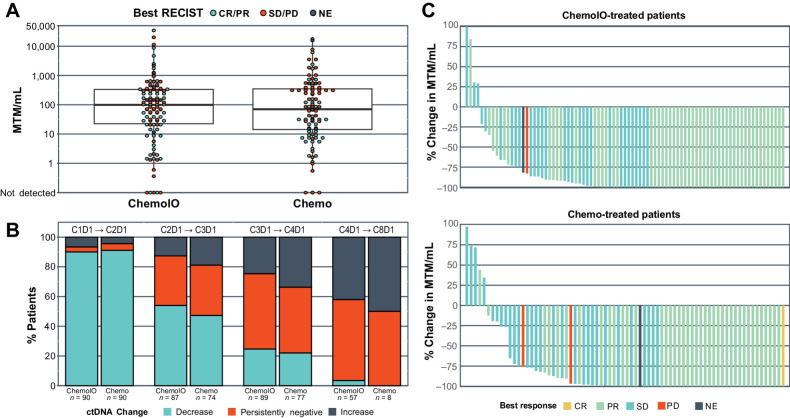
ctDNA detection and dynamics on chemoIO
Of the 221 patients with available baseline clinical characteristics, 210 patients had evaluable pretreatment baseline plasma samples across both treatment arms. ctDNA was detected in 201 patients (96%) across a wide range of MTM/mL (Fig. 2A). When dichotomizing patients using the patient cohort median ctDNA level (93 MTM/mL), there was a trend toward lower overall response rate in patients with baseline ctDNA levels above the median (47% vs. 60%). The difference in overall response rate was more pronounced in patients treated with chemotherapy alone (36% vs. 58%) than in patients treated with chemoIO (56% vs. 62%). Extending these analyses to PFS and OS in patients treated with chemoIO, we observed shorter PFS and OS in overall patients with baseline ctDNA levels above versus below the median (PFS: 6.0 vs. 8.5 months; OS: 11.1 vs. 20.7 months). In multivariate analyses, baseline ctDNA levels remained independently prognostic (PFS: HR, 2.28; 1.43–3.64; OS: HR, 2.23; 1.29–3.85). To understand how ctDNA changes may differ between treatment arms, ctDNA increase vs. decrease was assessed across all longitudinal timepoints. Most patients experienced ctDNA decrease from baseline to C2D1 (chemo: 91%; chemoIO: 90%), with 81% of patients having ≥ 50% decrease and 25% having full clearance, regardless of treatment arm. Increasing ctDNA from C2D1 to C3D1 (19% vs. 13%), as well as from C3D1 to C4D1 (34% vs. 25%), was more common in patients treated with chemo alone compared with those treated with chemoIO (Fig. 2B). Yet, by C4D1 94% of patients still had an overall decrease in ctDNA from baseline regardless of treatment arm (Fig. 2C).
Figure 2.
ctDNA is prevalent at baseline and highly dynamic on therapy. A, Baseline ctDNA detected per therapy arm reported as MTM/mL. B, The percentage of patients for each therapy arm with an increase, decrease, or no change in ctDNA between sequential cycles. Included any patients with available plasma at specified timepoints. C, Waterfall plot depicting the percent change in ctDNA between C1D1 and C4D1, measured in MTM/mL. Patients’ best objective response is represented by the color of the bar. Chemo, chemotherapy; ChemoIO, chemotherapy plus immunotherapy; CR, complete response; MTM/mL, mean tumor molecules per mL of plasma; NE, not evaluable; PR, partial response; SD, stable disease; PD, progressive disease.
ctDNA monitoring and outcomes on ChemoIO
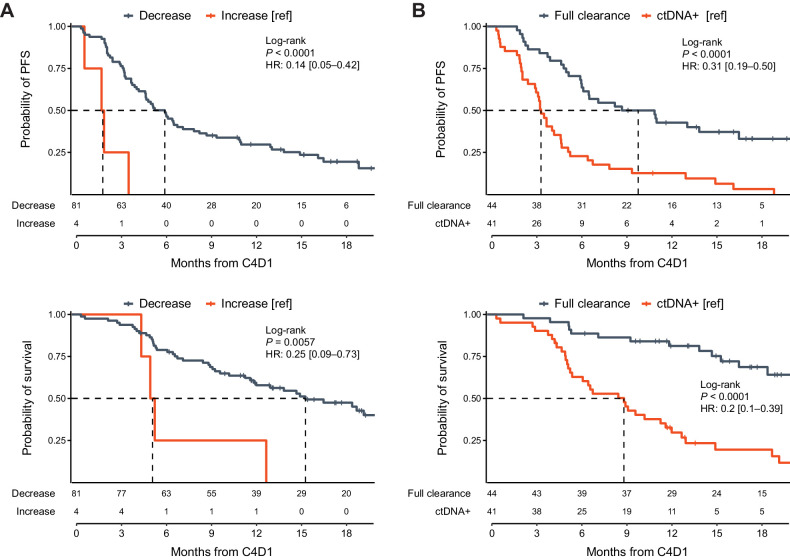
Given the variable outcomes on chemoIO, we investigated whether ctDNA monitoring can reliably identify patients responding to chemoIO that will achieve a more durable benefit. We focused on the C4D1 timepoint for testing because obtaining results at this stage allows for timely information to guide the planning of maintenance therapy at C5D1. Limiting the analysis to 85 patients treated with chemoIO with detectable ctDNA pretreatment, we found that most patients exhibited a decrease in ctDNA levels from baseline to C4D1 (81/85, 95.3%) and that these patients had significantly longer median PFS (6.1 vs. 2.0 months; HR, 0.14; 0.05–0.42; Fig. 3A) and median OS (15.3 vs. 5.3 months; HR, 0.25; 0.09–0.73; Fig. 3A) compared with those with a ctDNA increase. Similar results were seen for both PFS (6.1 vs. 1.9 months; HR, 0.24; 0.11–0.53) and OS (15.3 vs. 5.1 months; HR, 0.32; 0.14–0.77) when stratifying patients based on ≥50% ctDNA decrease (78/85; Supplementary Fig. S2A). Patients with complete ctDNA clearance (full clearance) at C4D1 (100% ctDNA decrease; 44/85, 52%) had significantly improved PFS (9.9 vs. 3.5 months; HR, 0.31; 0.19–0.50) and OS (NR vs. 8.9 months; HR, 0.20; 0.10–0.39) compared with patients with ctDNA+ at C4D1 (Fig. 3B). Other studies have additionally used 90% decrease as a cutoff (36). As an exploratory analysis, we stratified patients based on ≥ 90% decrease in ctDNA (64/85) and saw comparable results to full clearance (Supplementary Fig. S2B). When adjusting for covariates, including PD-L1, any ctDNA decrease and full ctDNA clearance at C4D1 from baseline remained statistically significant as independent prognostic factors for clinical outcomes (Supplementary Figs. S3 and S4). Improved ORR was associated with decrease from baseline for all assessed cutoffs (Supplementary Table S2). The same analysis was performed for patients treated in the chemo arm, but only 90% and full clearance was associated with favorable PFS (90%: 4.9 vs. 3.3 months; HR, 0.43; 0.25–0.75; full clearance: 6.3 vs. 3.4 months; HR, 0.42; 0.25–0.69), and only full clearance was associated with improved OS (10.3 vs. 5.3 months; HR, 0.41; 0.23–0.75); the other ctDNA cutoffs were unable to identify patients with durable benefit (Supplementary Fig. S5).
Figure 3.
ctDNA monitoring on chemoIO identifies patients with poorer outcomes on IO maintenance. Comparing C4 to C1 ctDNA levels, Kaplan–Meier analysis demonstrates favorable outcomes in patients with (A) any decrease and (B) full ctDNA clearance. In multivariate analysis using a Cox model adjusting for clinical and genomic features, ctDNA change remains a statistically significant prognostic factor (Supplementary Fig. S3).
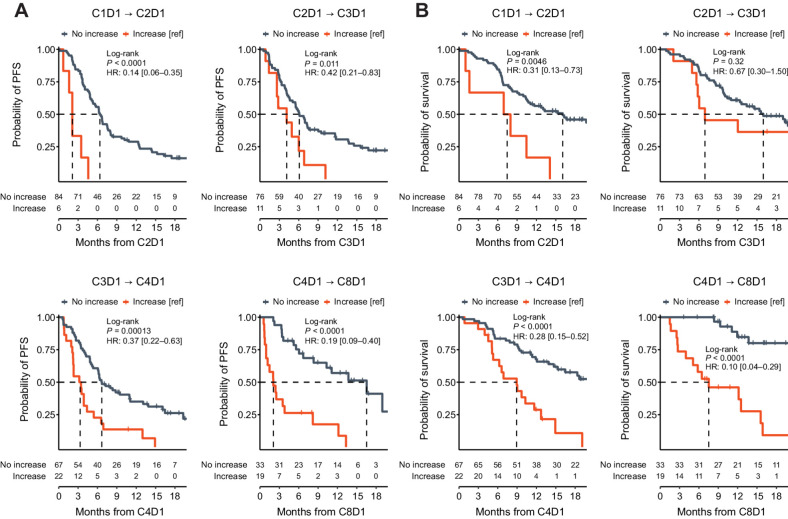
We further investigated whether serial monitoring on chemoIO could offer insight into clinical outcomes. Regardless of which interval was analyzed (C1→C2, C2→C3, C3→C4, or C4→C8), any increase in MTM/mL from the prior cycle was associated with shorter median PFS and OS from the landmark time (Fig. 4A and B) and lower ORRs (Supplementary Table S3). Importantly, of 38 chemoIO patients with ctDNA clearance at C4D1, only 21 (55%) had early clearance at C2D1; and of the 23 patients with early clearance at C2D1, two developed detectable ctDNA by C4D1.
Figure 4.
Across serial timepoints, ctDNA increase between any sequential cycles is associated with poorer outcomes. Kaplan–Meier analysis depicting (A) PFS and (B) OS for patients with ctDNA increase versus decrease between C1D1 and C2D1, C2D1 and C3D1, C3D1 and C4D1, and C4D1 and C8D1. PFS and OS analyses were landmarked from C2D1, C3D1, C4D1, or C8D1 respectively; patients with progression/death before the landmark date were excluded. OS, overall survival; PFS, progression-free survival.
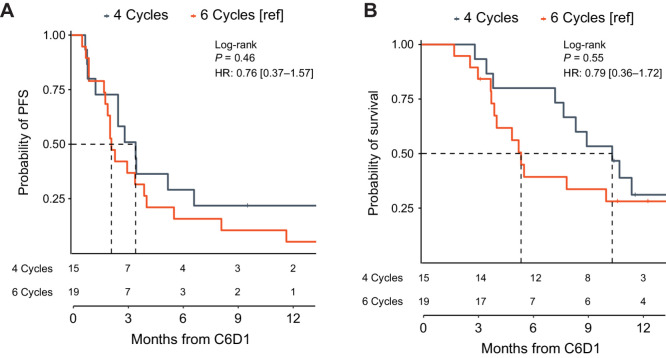
In clinical practice, many patients may not have baseline ctDNA analysis performed. Therefore, we investigated the prognostic value of ctDNA+ at C4D1 in all patients with available samples at this timepoint (n = 96), even when baseline testing was missing or baseline ctDNA levels were negative. Among the 96 analyzed samples, 43% were ctDNA+ (median, 14.6 MTM/mL; range, 0.3–787.3), and ctDNA positivity at C4D1 was associated with a lower ORR (43%) compared with those with undetectable ctDNA at the same timepoint (ctDNA-, 78%; P < 0.001). Patients with ctDNA- at C4D1 (55/96) had a higher PFS than their ctDNA+ counterparts (median PFS from C4D1: 8.8 vs. 3.5 months, respectively; HR, 0.32; 0.20–0.52; Fig. 5A). Median OS from C4D1 was not reached for ctDNA- patients and was 8.9 months for ctDNA+ patients (HR, 0.22; 0.12–0.39; Fig. 5B). Adjustments for clinical and genomic characteristics did not diminish the independent prognostic value of ctDNA detection at C4D1 (Supplementary Fig. S6). Results were similar when assessing ctDNA detection at other time points (Supplementary Fig. S7). We then hypothesized that in patients with ctDNA+ at C4D1, additional induction therapy (up to cycle 6) may provide benefit over four cycles. However, in an exploratory C6D1 landmark analysis of 34 patients who were ctDNA+ at C4D1, prolonged induction (six cycles vs. four cycles) was not associated with any improvement in PFS (2.1 vs. 3.5 months; HR, 0.76; 0.37–1.57) or OS (5.4 vs. 10.3 months; HR, 0.79; 0.36–1.72; Fig. 6A and B).
Figure 5.
In the absence of a baseline monitoring timepoint, ctDNA detection on chemoIO can inform subsequent outcomes on IO maintenance. Kaplan–Meier analysis depicting (A) PFS and (B) OS for all patients with an available C4 sample (including those with no baseline sample or negative baseline ctDNA levels). In multivariate analysis using a Cox model adjusting for clinical and genomic features, ctDNA positivity remains a statistically significant prognostic factor (Supplementary Fig. S6). IO, immunotherapy; OS, overall survival; PFS, progression-free survival.
Figure 6.
Additional cycles of induction therapy are not associated with improved outcomes in patients with ctDNA detection at C4D1. Kaplan–Meier analysis depicting (A) PFS and (B) OS for patients treated with chemoIO receiving four vs. six cycles of chemo induction therapy. ChemoIO, chemotherapy plus immunotherapy; OS, overall survival; PFS, progression-free survival.
Discussion
ChemoIO is an increasingly common first-line treatment for advanced driver-negative NSCLC, with platinum-free maintenance therapy recommended after induction. However, key questions remain regarding the optimal time to start ICI maintenance after chemoIO induction as well as the intensity and duration of maintenance. In current guidelines and clinical trials, ICI maintenance therapy is recommended after four or six cycles of chemoIO; however, there is lack of affirmative data to more precisely guide decisions related to subsequent maintenance therapy. Some regimens are exploring as few as two cycles of induction chemotherapy (37). Furthermore, while chemoIO with continued ICI maintenance is effective in a portion of patients, there are still those who do not exhibit durable benefit. Early determination of response or risk of progression on chemoIO induction could enable a more personalized approach—those with favorable response and low risk can more confidently advance to ICI maintenance, and patients with poor response and high risk can consider alternative and potentially more intensified maintenance therapies (13, 36–38).
Here, we demonstrate that ctDNA monitoring using a tissue CGP-informed, personalized monitoring assay can identify patients with advanced NSCLC gaining benefit from chemoIO. In a prespecified analysis, we find that ctDNA changes (decrease or complete clearance) prior to initiating the maintenance phase of treatment can distinguish between patients expected to have durable benefit and those at risk of rapid progression (ctDNA decrease HR, 0.14; ctDNA clearance HR, 0.31). Notably, this insight can also be gained regardless of whether a patient had pretreatment ctDNA testing—the detection of ctDNA following induction chemoIO had significant prognostic implications for maintenance therapy (OS HR, 0.22). Moreover, ongoing monitoring at subsequent timepoints provided additional prognostic insight, offering the possibility to continually tailor therapy for such patients. These findings are overall consistent with prior work demonstrating the potential for ctDNA monitoring to inform outcomes on immunotherapy in advanced solid tumors (21–24, 30).
Previous ctDNA monitoring studies in advanced solid tumors treated with IO (monotherapy or dual) have shown that ctDNA decrease after 6 to 9 weeks strongly predicts response and improved PFS and OS (32, 38). These studies dichotomize change in ctDNA as an increase or decrease from baseline, or evaluated 50% decrease or full clearance of ctDNA. While that analytic approach was informative, in the patients treated with chemoIO in our study, we did observe rapid and significant decreases in ctDNA across most patients at C2D1, which continued through C4D1 in both treatment arms (Fig. 2). For patients treated with chemoIO, we observed only four patients with an increase in ctDNA from baseline at C4D1 and only three patients with a <50% decrease by C4D1. The dramatic decrease in ctDNA levels seen in most patients is likely explained by the addition of chemotherapy to IO and highlights an important distinction in the interpretation of ctDNA monitoring results between IO therapy versus chemoIO. Since most patients exhibit considerable ctDNA decrease on chemoIO, an increased threshold for response (90%–100%) may be needed at C4D1 to discern a prevalent population with more or less favorable outcomes. Furthermore, it is important to consider the durability of benefit while on chemoIO. Our serial monitoring analyses showed that an increase in ctDNA levels between any subsequent on-treatment timepoints (C2D1 to C3D1 or C3D1 to C4D1) was associated with poorer clinical outcomes (Fig. 4; Supplementary Table S2). Decreasing ctDNA levels from pretreatment to C4D1 was informative using all evaluated cutoffs, with greater reductions of ctDNA providing more confidence in durable benefit. On the basis of this study, for chemoIO, on-treatment serial monitoring up to C4D1 and assessment at C4D1 as a single timepoint can both be informative for response assessment and risk stratification, but interpreting the magnitude of change in ctDNA is different than with ICI therapy alone. Further cohort analyses could be beneficial in further characterizing the optimal timing for ctDNA response analysis on chemoIO, such as the ongoing efforts by Friends of Cancer Research (22).
ChemoIO induction is effective in advanced NSCLC, with the majority of patients achieving response. There is greater uncertainty in the duration of benefit on IO maintenance. However, ctDNA monitoring may still have additional utility by allowing for early detection of nonresponders to chemoIO induction. Our serial monitoring analyses showed that an increase in ctDNA levels between any subsequent on-treatment timepoints (baseline to C2D1, C2D1 to C3D1, or C3D1 to C4D1) was associated with poorer response and long-term clinical outcomes (Fig. 4; Supplementary Table S2). In fact, an increase/decrease in ctDNA at C2D1 relative to baseline was associated with similar ORR as increase/decrease in ctDNA at C4D1 relative to baseline. Importantly, ctDNA remained dynamic across induction timepoints for some patients, with some having ctDNA increase after full clearance at C2D1 and others experiencing slower reductions of ctDNA, not obtaining clearance until C4D1. Taken together, this highlights the potential utility and significance of having multiple timepoints, specifically for assessing benefit of IO maintenance.
For patients with an inadequate ctDNA response after chemoIO, it remains uncertain what the best management approach is. In an exploratory analysis, we investigated whether, in these high-risk molecular nonresponder patients, additional cycles of induction chemotherapy resulted in prolonged PFS. Yet, additional chemotherapy cycles did not confer improved outcomes for these patients in our study. These results may not be surprising given the historical literature finding that additional platinum-based chemotherapy beyond the first four cycles resulted in no survival benefit in advanced NSCLC (39). Instead, such patients may require early access to emerging salvage therapies including targeted agents, (40, 41) antibody–drug conjugates, (42, 43) or new immunotherapies to alter their treatment outcomes.
While here we study a tissue-informed ctDNA monitoring approach, we and others have reported on tissue-naïve approaches for ctDNA monitoring as well. In a recent analysis of the IMpower150 trial of chemoIO in advanced NSCLC (44), a ctDNA panel covering >300 genes was used to test for somatic alterations at baseline and on-treatment. Despite avoidance of common germline and CH variants, the study team found that paired analysis of white blood cells was needed to further filter germline and CH variants. This and other tissue-naïve approaches have been able to provide prognostic insight from ctDNA monitoring in advanced NSCLC, (45) yet the risk of false-positive test results from CH remains a persistent concern (46), particularly at lower tumor fraction. Use of a tumor-informed approach offers an opportunity to reduce the risk of mistakenly tracking germline and CH signal, and the potential for increased sensitivity by tracking multiple patient-specific variants. Further development work would be needed to establish scalable tissue-naïve monitoring tools that can offer reliable sensitivity while avoiding confusing CH signal.
The algorithmic approach for selection of tumor variants used here is pragmatically designed for clinical care, allowing generation of a personalized ctDNA assay using a tumor tissue CGP result without the need of paired germline sequencing. To minimize risk of analytic false-positives, a sample is only identified as ctDNA-positive if two or more variants are detected. However, on occasion, a non-tumor variant (e.g., germline, CH, or other nontumor somatic) may be tracked along with the other tumor-derived variants. Of note, the cohort studied here had greater prevalence of elevated TMB (52%) than we saw in our recent analysis of real-world NSCLC outcomes on immunotherapy (40%; ref. 7), potentially increasing the feasibility of the monitoring approach studied. The impact of TMB and the number of variants tracked on immunotherapy monitoring deserves further investigation, though in this study, sensitivity analysis found no obvious impact of the number of tracked variants on monitoring and associated outcomes (Supplementary Fig. S8).
In conclusion, here we quantify the potential clinical insights from ctDNA monitoring on patients with advanced NSCLC receiving chemoIO. Importantly, ctDNA monitoring is not a replacement for baseline predictive biomarkers but may be able to complement these. ctDNA monitoring was prognostic across a range of cutoffs and a range of timepoints. Our data suggest that CGP-informed ctDNA monitoring can distinguish patients with favorable versus poor outcomes on immunotherapy maintenance, potentially allowing the development of precision maintenance treatment strategies. Future utility studies should investigate specific management approaches for patients undergoing ctDNA monitoring on chemoIO.
Supplementary Material
Supplementary Figure S1: Genomic landscape and tumor mutational burden (TMB) from 221 baseline tissue NGS for patients included in the outcomes analysis
Supplementary Figure S2: ctDNA decrease ≥ 50% or ≥ 90% at C4D1 on chemoIO identifies patients with poorer outcomes on IO maintenance
Supplementary Figure S3: Any ctDNA decrease or full clearance at C4D1 on chemoIO identifies patients with poorer outcomes on IO maintenance
Supplementary Figure S4: Full clearance of ctDNA at C4D1 on chemoIO identifies patients with poorer outcomes on IO maintenance, independent of PD-L1 status
Supplementary Figure S5: ctDNA monitoring on chemo requires greater levels of ctDNA clearance to effectively predict patient outcomes.
Supplementary Figure S6: In the absence of a baseline monitoring timepoint, ctDNA detection at C4D1 on chemoIO can inform subsequent outcomes on IO maintenance
Supplementary Figure S7: ctDNA detection was associated with worse outcomes across all monitoring timepoints
Supplementary Figure S8: Number of variants tracked per patient did not impact prognostic outcomes of ctDNA monitoring
Biomarker analysis patient cohort characteristics and ITT patient characteristics. Clinical and biomarker characteristics are similar between treatment arms of the biomarker analysis patient cohort evaluated in this study. Clinical and biomarker characteristics are similar between the ITT population in IMpower131 and the biomarker analysis patient cohort evaluated in this study.
ctDNA decrease from C1 to C4 was associated with greater objective response in patients treated with chemoIO at all cutoffs. Number of patients per best objective response with associated increase or decreases in ctDNA between C1 and C4. *Progression-free rate was calculated from the start of therapy rather than the start of C4D1.
ctDNA decrease from any subsequent cycle was associated with greater objective response in patients treated with chemoIO. Number of patients per best objective response with associated increase or decreases in ctDNA levels between subsequent cycles.
Acknowledgments
This study was supported by Foundation Medicine, Inc. (R.W. Madison, M.A. Childress, S.T. Miller, O. Gjoerup, R.S.P. Huang, A. Young, G.R. Oxnard).
The publication costs of this article were defrayed in part by the payment of publication fees. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
This article is featured in Selected Articles from This Issue, p. 4519
Footnotes
Note: Supplementary data for this article are available at Clinical Cancer Research Online (http://clincancerres.aacrjournals.org/).
Authors' Disclosures
B. Pellini reports grants from BMS Foundation and BMS and personal fees from Merck, BMS, AH Merus, AstraZeneca, Regeneron, Illumina, Guardant Health, Foundation Medicine, Guidepoint, MJH Life Sciences, MLI, Bio Ascend, Grupo Pardini, GBOT, Play to Know AG and Doctaforum outside the submitted work. R.W. Madison reports personal fees from Foundation Medicine Inc. and Roche Holding AG during the conduct of the study. M.A. Childress reports employment by Foundation Medicine and stock ownership with Roche. S.T. Miller reports personal fees from Foundation Medicine Inc. and Roche Holding AG during the conduct of the study. O. Gjoerup reports other support from Roche outside the submitted work. J. Cheng reports employment by Genentech, Inc. and hold shares of Roche stock. R.S.P. Huang reports other support from Foundation Medicine during the conduct of the study and other support from Foundation Medicine outside the submitted work. M. Krainock reports other support from Natera during the conduct of the study. P. Gupta reports employment by Genentech/Roche. W. Zou reports other support from Roche outside the submitted work. D.S. Shames reports employment by Genentech Inc. and stock ownership in Roche Holdings. S. Moshkevich reports other support from Natera, Inc. outside the submitted work. M. Ballinger reports other support from Genentech, Inc. during the conduct of the study; other support from Genentech Inc. outside the submitted work; employment at Genentech, Inc., and Roche stock ownership. M.C. Liu reports other support from Natera during the conduct of the study and funding to Mayo Clinic from Eisai, Exact Sciences, Genentech, Genomic Health, GRAIL, Menarini Silicon Biosystems, Merck, Novartis, Seattle Genetics, and Tesaro; and ad hoc advisory board meetings with financial compensation deferred to Mayo Clinic from AstraZeneca, Celgene, Roche/Genentech, Genomic Health, GRAIL, Ionis, Merck, Pfizer, Seattle Genetics, and Syndax. A. Young reports personal fees from Foundation Medicine during the conduct of the study. G.R. Oxnard reports personal fees from Foundation Medicine and Roche during the conduct of the study. M.A. Socinski reports grants and personal fees from Genentech and AZ; grants and other support from Spectrum and Beigene; grants from Novartis, Cullinan, Pfizer, and Daiichi Sankyo; personal fees and other support from Lilly; grants, personal fees, and other support from Mirati; other support from BMS; and personal fees from Regeneron, G1 Therapuetics, Jazz, and Janssen outside the submitted work. No disclosures were reported by the other authors.
Authors' Contributions
B. Pellini: Conceptualization, supervision, writing–review and editing. R.W. Madison: Conceptualization, software, formal analysis, investigation, visualization, writing-original draft, writing–review and editing. M.A. Childress: Conceptualization, formal analysis, visualization, writing-original draft, writing–review and editing. S.T. Miller: Resources, project administration, writing–review and editing. O. Gjoerup: Conceptualization, project administration, writing–review and editing. J. Cheng: Resources, writing–review and editing. R.S.P. Huang: Conceptualization, supervision, writing–review and editing. M. Krainock: Resources, writing–review and editing. P. Gupta: Resources, writing–review and editing. W. Zou: Resources, writing–review and editing. D.S. Shames: Resources, writing–review and editing. S. Moshkevich: Resources, supervision, writing–review and editing. M. Ballinger: Resources, writing–review and editing. M.C. Liu: Resources, Supervision, writing–review and editing. A. Young: Conceptualization, writing–review and editing. M.K. Srivastava: Resources, writing–review and editing. G.R. Oxnard: Conceptualization, supervision, writing-original draft, writing–review and editing. M.A. Socinski: Conceptualization, writing–review and editing.
References
- 1. Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al. Pembrolizumab versus chemotherapy for PD-L1–positive non–small cell lung cancer. N Engl J Med 2016;375:1823–33. [DOI] [PubMed] [Google Scholar]
- 2. Hellmann MD, Paz-Ares L, Bernabe Caro R, Zurawski B, Kim S-W, Carcereny Costa E, et al. Nivolumab plus ipilimumab in advanced non–small cell lung cancer. N Engl J Med 2019;381:2020–31. [DOI] [PubMed] [Google Scholar]
- 3. Reck M, Rodríguez–Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al. Updated analysis of KEYNOTE-024: pembrolizumab versus platinum-based chemotherapy for advanced non–small cell lung cancer with PD-L1 tumor proportion score of 50% or greater. JCO 2019;37:537–46. [DOI] [PubMed] [Google Scholar]
- 4. Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, et al. Pembrolizumab for the treatment of non–small cell lung cancer. N Engl J Med 2015;372:2018–28. [DOI] [PubMed] [Google Scholar]
- 5. Herbst RS, Baas P, Kim D-W, Felip E, Pérez-Gracia JL, Han J-Y, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non–small cell lung cancer (KEYNOTE-010): a randomized controlled trial. Lancet North Am Ed 2016;387:1540–50. [DOI] [PubMed] [Google Scholar]
- 6. Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus docetaxel in advanced nonsquamous non–small cell lung cancer. N Engl J Med 2015;373:1627–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Huang RSP, Carbone DP, Li G, Schrock A, Graf RP, Zhang L, et al. Durable responders in advanced NSCLC with elevated TMB and treated with 1L immune checkpoint inhibitor: a real-world outcomes analysis. J Immunother Cancer 2023;11:e005801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shields MD, Marin-Acevedo JA, Pellini B. Immunotherapy for advanced non–small cell lung cancer: a decade of progress. Am Soc Clin Oncol Educ Book 2021;41:1–23. [DOI] [PubMed] [Google Scholar]
- 9. Non–small cell lung cancer version 2.2023. National Comprehensive Cancer Network 2023 Feb. Available from: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf [DOI] [PubMed]
- 10. Ribas A, Chmielowski B, Glaspy JA. Do we need a different set of response assessment criteria for tumor immunotherapy? Clin Cancer Res 2009;15:7116–8. [DOI] [PubMed] [Google Scholar]
- 11. Wolchok JD, Hoos A, O'Day S, Weber JS, Hamid O, Lebbé C, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res 2009;15:7412–20. [DOI] [PubMed] [Google Scholar]
- 12. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumors: Revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. [DOI] [PubMed] [Google Scholar]
- 13. Jotte R, Cappuzzo F, Vynnychenko I, Stroyakovskiy D, Rodríguez-Abreu D, Hussein M, et al. Atezolizumab in combination with carboplatin and nab-paclitaxel in advanced squamous NSCLC (IMpower131): results from a randomized phase III trial. J Thorac Oncol 2020;15:1351–60. [DOI] [PubMed] [Google Scholar]
- 14. Wakelee HA, Stephenson P, Keller SM, Wagner H, Herskovic A, Komaki R, et al. Post-operative radiotherapy (PORT) or chemoradiotherapy (CPORT) following resection of stages II and IIIA non–small cell lung cancer (NSCLC) does not increase the expected risk of death from intercurrent disease (DID) in Eastern Cooperative Oncology Group (ECOG) trial E3590. Lung Cancer 2005;48:389–97. [DOI] [PubMed] [Google Scholar]
- 15. Scagliotti GV, Parikh P, von Pawel J, Biesma B, Vansteenkiste J, Manegold C, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non–small cell lung cancer. JCO 2008;26:3543–51. [DOI] [PubMed] [Google Scholar]
- 16. Aggarwal H, Bayo K, Han Y, Muehlenbein CE, Zhu YE, Kim JS. Real-world maintenance therapy and survival outcomes for pembrolizumab plus pemetrexed and platinum for non–small cell lung cancer in USA. Immunotherapy 2023;15:267–81. [DOI] [PubMed] [Google Scholar]
- 17. Leighl NB, Hellmann MD, Hui R, Carcereny E, Felip E, Ahn M-J, et al. Pembrolizumab in patients with advanced non–small cell lung cancer (KEYNOTE-001): 3-year results from an open-label, phase I study. Lancet Respir Med 2019;7:347–57. [DOI] [PubMed] [Google Scholar]
- 18. Borghaei H, Gettinger S, Vokes EE, Chow LQM, Burgio MA, de Castro Carpeno J, et al. Five-year outcomes from the randomized, phase III trials CheckMate 017 and 057: nivolumab versus docetaxel in previously treated non–small cell lung cancer. JCO 2021;39:723–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Herbst RS, Garon EB, Kim D-W, Cho BC, Gervais R, Perez-Gracia JL, et al. Five year survival update from KEYNOTE-010: pembrolizumab versus docetaxel for previously treated, programmed death-ligand 1–positive advanced NSCLC. J Thorac Oncol 2021;16:1718–32. [DOI] [PubMed] [Google Scholar]
- 20. Shukla N, Hanna N, Durm G. Optimal duration of maintenance checkpoint inhibitor therapy in patients with advanced NSCLC. JCO Oncol Pract 2021;17:472–4. [DOI] [PubMed] [Google Scholar]
- 21.Cindy Yang SY, Lien SC, Wang BX, Clouthier DL, Hanna Y, Cirlan I, et al. Pan-cancer analysis of longitudinal metastatic tumors reveals genomic alterations and immune landscape dynamics associated with pembrolizumab sensitivity. Nat Commun 2021;12:5137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vega DM, Nishimura KK, Zariffa N, Thompson JC, Hoering A, Cilento V, et al. Changes in circulating tumor DNA reflect clinical benefit across multiple studies of patients with non–small cell lung cancer treated with immune checkpoint inhibitors. JCO Precis Oncol 2022;6:e2100372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Anagnostou V, Forde PM, White JR, Niknafs N, Hruban C, Naidoo J, et al. Dynamics of tumor and immune responses during immune checkpoint blockade in non–small cell lung cancer. Cancer Res 2019;79:1214–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Moding EJ, Liu Y, Nabet BY, Chabon JJ, Chaudhuri AA, Hui AB, et al. Circulating tumor DNA dynamics predict benefit from consolidation immunotherapy in locally advanced non–small cell lung cancer. Nat Cancer 2020;1:176–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ferrara R, Pilotto S, Caccese M, Grizzi G, Sperduti I, Giannarelli D, et al. Do immune checkpoint inhibitors need new studies methodology? J Thorac Dis 2018;10:S1564–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chen T-T. Statistical issues and challenges in immuno-oncology. J Immunother Cancer 2013;1:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shukuya T, Mori K, Amann JM, Bertino EM, Otterson GA, Shields PG, et al. Relationship between overall survival and response or progression-free survival in advanced non–small cell lung cancer patients treated with anti–PD-1/PD-L1 antibodies. J Thorac Oncol 2016;11:1927–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Singh A, Daemen A, Nickles D, Jeon S-M, Foreman O, Sudini K, et al. NRF2 activation promotes aggressive lung cancer and associates with poor clinical outcomes. Clin Cancer Res 2021;27:877–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F., von Pawel J, et al. Atezolizumab versus docetaxel in patients with previously treated non–small cell lung cancer (OAK): a phase III, open-label, multicenter, randomized controlled trial. Lancet North Am Ed 2017;389:255–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kansara M, Bhardwaj N, Thavaneswaran S, Xu C, Lee JK, Chang L, et al. Early circulating tumor DNA dynamics as a pan-tumor biomarker for long-term clinical outcome in patients treated with durvalumab and tremelimumab. Molecular Oncology 2023;17:298–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Reinert T, Henriksen TV, Christensen E, Sharma S, Salari R, Sethi H, et al. Analysis of plasma cell-free DNA by ultradeep sequencing in patients with stages I to III colorectal cancer. JAMA Oncol 2019;5:1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bratman SV, Yang SYC, Iafolla MAJ, Liu Z, Hansen AR, Bedard PL, et al. Personalized circulating tumor DNA analysis as a predictive biomarker in solid tumor patients treated with pembrolizumab. Nat Cancer 2020;1:873–81. [DOI] [PubMed] [Google Scholar]
- 33. The Cancer Genome Atlas Research Network. Comprehensive genomic characterization of squamous cell lung cancers. Nature 2012;489:519–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hendriks LE, Rouleau E, Besse B. Clinical utility of tumor mutational burden in patients with non–small cell lung cancer treated with immunotherapy. Transl Lung Cancer Res 2018;7:647–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ricciuti B, Wang X, Alessi JV, Rizvi H, Mahadevan NR, Li YY, et al. Association of high tumor mutation burden in non–small cell lung cancers with increased immune infiltration and improved clinical outcomes of PD-L1 blockade across PD-L1 expression levels. JAMA Oncol 2022;8:1160–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Davis AA, Iams WT, Chan D, Oh MS, Lentz RW, Peterman N, et al. Early assessment of molecular progression and response by whole-genome circulating tumor DNA in advanced solid tumors. Mol Cancer Ther 2020;19:1486–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Paz-Ares L, Ciuleanu T-E, Cobo M, Schenker M, Zurawski B, Menezes J, et al. First-line nivolumab plus ipilimumab combined with two cycles of chemotherapy in patients with non–small cell lung cancer (CheckMate 9LA): an international, randomized, open-label, phase III trial. Lancet Oncol 2021;22:198–211. [DOI] [PubMed] [Google Scholar]
- 38. Thompson JC, Carpenter EL, Silva BA, Rosenstein J, Chien AL, Quinn K, et al. Serial monitoring of circulating tumor DNA by next-generation gene sequencing as a biomarker of response and survival in patients with advanced NSCLC receiving pembrolizumab-based therapy. JCO Precis Oncol 2021;510–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Socinski MA, Schell MJ, Peterman A, Bakri K, Yates S, Gitten R, et al. Phase III trial comparing a defined duration of therapy versus continuous therapy followed by second-line therapy in advanced-stage IIIB/IV non–small cell lung cancer. J Clin Oncol 2002;20:1335–43. [DOI] [PubMed] [Google Scholar]
- 40. Nakajima EC, Drezner N, Li X, Mishra-Kalyani PS, Liu Y, Zhao H, et al. FDA approval summary: sotorasib for KRAS G12C-mutated metastatic NSCLC. Clin Cancer Res 2022;28:1482–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Jänne PA, Riely GJ, Gadgeel SM, Heist RS, Ou S-HI, Pacheco JM, et al. Adagrasib in non–small cell lung cancer harboring a KRASG12C mutation. N Engl J Med 2022;387:120–31. [DOI] [PubMed] [Google Scholar]
- 42. Levy B, Leventakos K, Lou Y, Savvides P, Rixe O, Tolcher A, et al. P47.04 TROPION-Lung02: datopotamab deruxtecan (Dato-DXd) plus pembrolizumab and platinum-based chemotherapy in advanced NSCLC. J Thorac Oncol 2021;16:S1097–8. [Google Scholar]
- 43. Levy BP, Reck M, Yang JC-H, Cappuzzo F, Rawat S, Xie J, et al. Datopotamab deruxtecan (Dato-DXd) plus pembrolizumab in treatment-naive advanced/metastatic (adv/met) non–small cell lung cancer (NSCLC) with PD-L1 ≥ 50% and without actionable genomic alterations. J Clin Oncol 2022;40:TPS3162. [Google Scholar]
- 44. Assaf ZJF, Zou W, Fine AD, Socinski MA, Young A, Lipson D, et al. A longitudinal circulating tumor DNA-based model associated with survival in metastatic non–small cell lung cancer. Nat Med 2023;29:859–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhang Q, Luo J, Wu S, Si H, Gao C, Xu W, et al. Prognostic and predictive impact of circulating tumor DNA in patients with advanced cancers treated with immune checkpoint blockade. Cancer Discov 2020;10:1842–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hu Y, Ulrich BC, Supplee J, Kuang Y, Lizotte PH, Feeney NB, et al. False-positive plasma genotyping due to clonal hematopoiesis. Clin Cancer Res 2018;24:4437–43. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure S1: Genomic landscape and tumor mutational burden (TMB) from 221 baseline tissue NGS for patients included in the outcomes analysis
Supplementary Figure S2: ctDNA decrease ≥ 50% or ≥ 90% at C4D1 on chemoIO identifies patients with poorer outcomes on IO maintenance
Supplementary Figure S3: Any ctDNA decrease or full clearance at C4D1 on chemoIO identifies patients with poorer outcomes on IO maintenance
Supplementary Figure S4: Full clearance of ctDNA at C4D1 on chemoIO identifies patients with poorer outcomes on IO maintenance, independent of PD-L1 status
Supplementary Figure S5: ctDNA monitoring on chemo requires greater levels of ctDNA clearance to effectively predict patient outcomes.
Supplementary Figure S6: In the absence of a baseline monitoring timepoint, ctDNA detection at C4D1 on chemoIO can inform subsequent outcomes on IO maintenance
Supplementary Figure S7: ctDNA detection was associated with worse outcomes across all monitoring timepoints
Supplementary Figure S8: Number of variants tracked per patient did not impact prognostic outcomes of ctDNA monitoring
Biomarker analysis patient cohort characteristics and ITT patient characteristics. Clinical and biomarker characteristics are similar between treatment arms of the biomarker analysis patient cohort evaluated in this study. Clinical and biomarker characteristics are similar between the ITT population in IMpower131 and the biomarker analysis patient cohort evaluated in this study.
ctDNA decrease from C1 to C4 was associated with greater objective response in patients treated with chemoIO at all cutoffs. Number of patients per best objective response with associated increase or decreases in ctDNA between C1 and C4. *Progression-free rate was calculated from the start of therapy rather than the start of C4D1.
ctDNA decrease from any subsequent cycle was associated with greater objective response in patients treated with chemoIO. Number of patients per best objective response with associated increase or decreases in ctDNA levels between subsequent cycles.
Data Availability Statement
All relevant data are provided within the article and its accompanying Supplementary Data. Because of Health Insurance Portability and Accountability Act requirements, we are not consented to share individualized patient genomic data, which contains potentially identifying or sensitive patient information. Foundation Medicine is committed to collaborative data analysis, and we have well-established and widely used mechanisms by which investigators can query our core genomic database of >600,000 deidentified sequenced cancers to obtain aggregated datasets. More information and mechanisms for data access can be obtained by contacting the corresponding authors or the Foundation Medicine Data Governance Council at data.governance.council@foundationmedicine.com. For IMpower131, qualified researchers may request access to individual patient-level data through the clinical study data request platform (https://vivli.org/members/enquiries-about-studies-not-listed-on-the-vivli-platform [vivli.org]/).