Abstract
Background
Infants born very and extremely premature (V/EPT) are at a significantly elevated risk for neurodevelopmental disorders and delays even in the absence of structural brain injuries. These risks may be due to earlier-than-typical exposure to the extrauterine environment, and its bright lights, loud noises, and exposures to painful procedures. Given the relative underdeveloped pain modulatory responses in these infants, frequent pain exposures may confer risk for later deficits.
Methods
Resting-state fMRI scans were collected at term equivalent age from 148 (45% male) infants born V/EPT and 99 infants (56% male) born at term age. Functional connectivity analyses were performed between functional regions correlating connectivity to the number of painful skin break procedures in the NICU, including heel lances, venipunctures, and IV placements. Subsequently, preterm infants returned at 18 months, for neurodevelopmental follow-up and completed assessments for autism risk and general neurodevelopment.
Results
We observed that V/EPT infants exhibit pronounced hyperconnectivity within the cerebellum and between the cerebellum and both limbic and paralimbic regions correlating with the number of skin break procedures. Moreover, skin breaks were strongly associated with autism risk, motor, and language scores at 18 months. Subsample analyses revealed that the same cerebellar connections strongly correlating with breaks at term age were associated with language dysfunction at 18 months.
Conclusions
These results have significant implications for the clinical care of preterm infants undergoing painful exposures during routine NICU care, which typically occurs without anesthesia. Repeated pain exposures appear to have an increasingly detrimental effect on brain development during a critical period, and effects continue to be seen even 18 months later.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-023-03141-w.
Keywords: Early-life pain, fMRI, Brain development, Cerebellum, Prematurity, Neonatal intensive care unit, Neurodevelopment, Autism spectrum disorder, Language development, Motor development
Background
Nearly 1 out of 10 babies worldwide are born premature, with minimal change over the past decade [1–4], although survival rates have increased significantly [5, 6]. Despite increasing survival, infants born very preterm (VPT) < 32 weeks postmenstrual age (PMA) and extremely preterm (EPT) < 28 weeks PMA [7] remain at heightened risk for developmental deficits even in the absence of any detectable brain injury, especially sensorimotor [8–10], language [11, 12], and cognitive [10, 12, 13] impairments. Moreover, they experience higher rates of neurodevelopmental disorders such as autism spectrum disorder (ASD) [14–17].
While the association between prematurity and developmental outcomes is well established, mechanisms driving the association remain unclear. One possibility is alterations in brain development arising from earlier-than-typical exposure to the extrauterine environment. The late second through third trimester is a critical period for brain development, seeing rapid increases in global and regional brain volumes [18–22], strengthening of white matter tracts [23, 24], and organizing of functional brain networks [25, 26]. While V/EPT infant’s brains exhibit volumetric increases [27], it is less than term-born infants, especially in the cerebellum and brainstem [22, 28–30]. Furthermore, functional network development in preterm infants is disrupted compared to term-born infants [31, 32].
Importantly, not all infants born V/EPT will experience neurodevelopmental impairments. It is likely the qualities of experiences during this critical period play a role in modifying trajectories. Neonatal intensive care units (NICU) are significantly more sensorially intense relative to the intrauterine environment, with bright lights and loud noises that reach as high as 85 decibels [33, 34]. Exposure to these intense sensory experiences have been linked to altered development (for review see Ream & Lehwald (2018)) [35]. In fact, one study found that the rates of neurodevelopmental disorders such as ASD are higher following a NICU stay even in term-born infants, suggesting NICU exposure itself may play a role [36].
Lengthy NICU stays for V/EPT infants include exposures to various noxious stimuli, especially repeated painful exposures. These infants are regularly exposed to painful procedures over the course of their clinical care, including heel sticks, venipunctures, and catheterizations. Infants born VPT experience an average of 115 painful procedures during their NICU stay, with some reporting over 600 [37] and most occur in the absence of any analgesia [38–40]. Pain pathways are vulnerable to perturbations in V/EPT infants, because of asynchronicity in the earlier developing afferent nociceptive pathways and later maturating efferent modulatory responses [41], suggesting the development of pain sensations precedes the ability to moderate the experience of pain. Research into the effects of painful exposures in the NICU on functional brain development is relatively limited; however, greater NICU pain exposures have been associated with other health and neurodevelopmental alterations including decreased infant weight [42], lower white matter fractional anisotropy, and lower IQ at school age [43], as well as decreased cerebellar volume at school age [44]. Moreover, animal models have linked early pain exposures to increased neuroinflammation and hippocampal development [45], as well as greater neural sensitivity to future noxious exposures in the somatosensory and prefrontal cortex [46]. Most of this research focuses on differences later into childhood and emphasizes structural abnormalities. This results in a significant gap in our understanding of how these experiences change the functional organization of the brain and how early in development these differences can be detected—an essential step in identifying periods of early intervention.
This study aims to examine the association between early pain exposures in both near-term development of functional connections and later neurodevelopment. Using a cohort of V/EPT infants who underwent resting state fMRI at term-equivalent age (TEA), we examined differences in early functional connectivity from term-born infants. We then assessed whether NICU skin break procedures prior to TEA were associated with changes in inter-regional functional brain connectivity. Thereafter, we evaluated whether breaks were associated with risk for neurodevelopmental difficulties at 18 months, and whether the connectivity in regions sensitive to pain were associated with deficits at 18 months.
Methods
Participants
A total of 293 V/EPT infants were recruited between 2016 and 2022 for ongoing prospective cohort studies at Children’s National Hospital on the impact of preterm birth on the developing brain and subsequent neurodevelopment. Infants were excluded if they lacked a TEA scan (n = 17), the fMRI scan had excessive motion artifacts (n = 81), or the infant rated above “mild brain injury” on the Kidokoro scale [47] as determined by an experienced pediatric neuroradiologist (J.M.) (n = 47). Follow-up data at 18 months corrected age was only available for a subsample of the total cohort. The final sample consisted of 148 participants possessing both acceptable fMRI scan and procedure data with an average of 6:40 ± 1:45 min of viable resting state data. Importantly, while those not meeting inclusion criteria were slightly younger than included infants (26.85 vs 27.94 weeks, t(291) = 3.178, p = 0.002), there was no difference in the total number of skin breaks prior to term age (98 vs 112, p = 0.208). Based on the initial sample, multiple subsamples were utilized for follow-up analyses. Namely, a subset of possessing both procedures and follow-up data (n = 47) and a second subset possessing MRI scan and follow-up data (n = 41) (Fig. 1). Finally, an additional 99 term-born infants were recruited as controls (Table 1). The study was approved by the Children’s National Hospital Institutional Review Board (IRB) and performed within regulations and guidelines of the IRB.
Fig. 1.
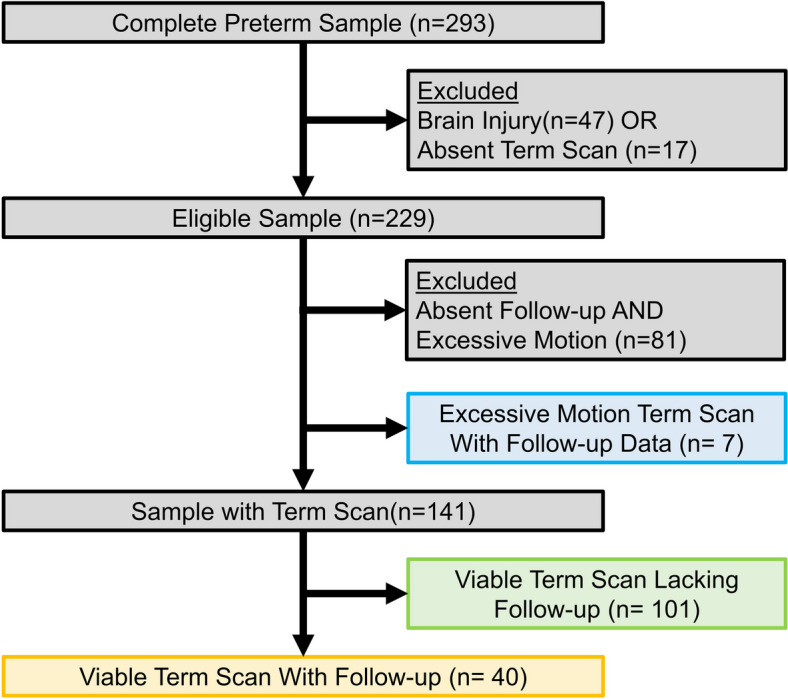
Participant flowsheet. Participant exclusion for the final sample, including all participants with viable term age scans (n = 141, green + yellow), participants with follow-up data (n = 47, yellow and blue), and participants with both a viable term age scan and follow-up data (n = 40, yellow)
Table 1.
Demographics and clinical characteristics
| Term (n = 99) |
Preterm (n = 148) |
P value | |
|---|---|---|---|
| Gestational at birth (weeks) | 39.2 (1.3) | 28.02 (2.8) | < .001 |
| Postmenstrual age at scan (weeks) | 40.9 (1.3) | 40.1 (2.0) | < .001 |
| Age at scan (weeks) | 1.6 (0.9) | 12.0 (3.3) | < .001 |
| Sex (% male) | 55.6 | 45.4 | .117 |
| Maternal characteristics | |||
| Maternal age (years) | 34.1 (5.8) | 28.0 (5.6) | < .001 |
| Gravida | 2 [1, 9] | 2 [1, 8] | .058 |
| Primipara (% yes) | 55.6 | 77.2 | .001 |
| Education level (%) | < .001 | ||
| < HS | 6.6 | 9.8 | |
| HS | 12.1 | 32.6 | |
| Some college | 19.8 | 27.2 | |
| College degree | 18.7 | 19.6 | |
| Graduate degree | 42.9 | 10.9 | |
| Employment (%) | .087 | ||
| Professional | 61.5 | 41.3 | |
| Skilled/clerical/sales | 13.2 | 18.5 | |
| Unemployed/homemaker | 25.3 | 40.2 | |
| Race and Ethnicity (%) | < .001 | ||
| American/Alaskan Indian | 2.0 | 1.3 | |
| Asian/Pacific Islander | 4.0 | 16.5 | |
| Non-Hispanic Black | 39.4 | 27.8 | |
| Hispanic | 11.1 | 1.3 | |
| Non-Hispanic White | 40.4 | 53.2 | |
| Other | 3.0 | 0 | |
| APGAR at 1 min | 8 [6, 9] | 4 [0,9] | < .001 |
| APGAR at 5 min | 9 [8, 10] | 7 [0,9] | < .001 |
| NICU care clinical care | |||
| Number of NICU procedures | - | 111 (93.2) | |
| Length of NICU stay (days) | - | 67.7 (34.9) | |
| Opioid pain medication in NICU (%) | - | 79.7 | |
| Fentanyl exposure (%) | - | 54.0 | |
| Morphine exposure (%) | - | 41.6 | |
| Benzodiazepine medication in NICU (%) | - | 27.9 | |
| Dexmedetomidine in NICU (%) | - | 15.0 | |
| Underwent surgery prior to TEA (%) | - | 30.7 | |
| Ventilated in NICU (%) | - | 12.1 | |
| Rates of necrotizing enterocolitis (%) | - | 11.4 | |
| Rates of patent ductus arteriosus (%) | - | 29.2 | |
| Rates of bronchopulmonary dysplasia (%) | - | 21.4 | |
Numerical data presented as mean (sd) or median [range]
Reported p values are from independent t-tests for continuous variables and χ2 for categorical
HS High school, NICU Neonatal intensive care unit
Measures and behavioral assessments
A retrospective chart review was performed to catalogue painful procedures experienced during their NICU stay. Consistent with prior literature, we utilized the total number of skin break procedures which included the number of heel sticks, venipunctures, and IV placements [48–50].
Caregivers and infants returned at approximately 18 months postnatal for developmental testing. They completed the Modified Checklist for Autism in Toddlers-Revised (MCHAT), a 20-item assessment utilized as an early screen for autism [51]. The MCHAT score was categorized into levels of autism risk: “not at risk” (< 3) and “at risk” (≥ 3). Caregivers also complete the Mullen Scales of Early Learning (MSEL). The MSEL assesses neurodevelopment from infancy through toddlerhood with scales for gross and fine motor, visual, and receptive and expressive language development [52] and is significantly associated of ASD risk at 18–36 months [53]. While the MCHAT is a clinical screener resulting in difficulty capturing variations in typically developing children who score 0–1, the MSEL is normed using the general population and thus captures typical variability in neurodevelopment.
MRI acquisition and preprocessing
All MRI images were acquired using a 3 T GE scanner (Discovery MR750, GE Healthcare, Milwaukee, WI) using an 8-channel infant head coil as part of the research protocol. To minimize motion, infants were fed, swaddled in a warm blanket, secured using an infant vacuum pillow, and provided with ear protection consisting of silicone ear plugs and adhesive earmuffs. Infants were not otherwise sedated. All infants were unventilated at time of TEA scan. Anatomical T2 weighted 3D fast-spin echo structural images were collected with the following parameters: 2502 ms TR, 84.37 ms TE, 0.5 × 1.0 × 0.5 mm voxel size, 90° flip angle. Resting state scans were collected with 2000 ms TR, 25 ms TE, 2.5 × 2.5 × 3.2 mm voxel size, 60° flip angle, 100 cm field of view, anterior-to-posterior phase encoding, and 10 min scan duration (300 volumes).
Resting state data were preprocessed using a modified previously published pipelines [54] using Analysis of Functional NeuroImages (AFNI) [55]. In brief, scans underwent within-volume motion correction, slice-time correction, dropping the first four volumes. Following, images were despiked, bias-field corrected, and outliers were censored. Functional images were then aligned to their anatomical and normalized to a PMA 40 template [56]. Signal was intensity scaled to a global mode of 1000 and smoothed using a 5 mm full-width half-maximum blur. Demeaned motion was calculated and volumes exceeding 0.2 mm were excluded. Motion, CSF, and white matter signal were regressed out, and the image underwent 0.009–0.08 bandpass filtering. Throughout the processes, visual inspections of the data were performed for noticeable distortions and drop-off including the raw resting state data, following processing, and again to the parcellation template. After preprocessing, only images with at least 4 min of available data were included in the analyses. Prior work has suggested that 4 min of rest is sufficient to elicit functional proto-networks [25, 32] and been used to successfully track changes of functional connectivity from infancy into early childhood [57].
Experimental design and statistical analysis
Infants were recruited from Children’s National for a prospective cohort study which included MRI scans during the preterm period and at TEA. Infants were then followed longitudinally to evaluate neurodevelopment, which included a battery of caregiver reports and questionnaires at 18 months of age. Utilizing this cohort, based on infants possessing a high-quality TEA scan as described above, a retrospective chart review was performed to summarize the number of skin break procedures experienced prior to TEA.
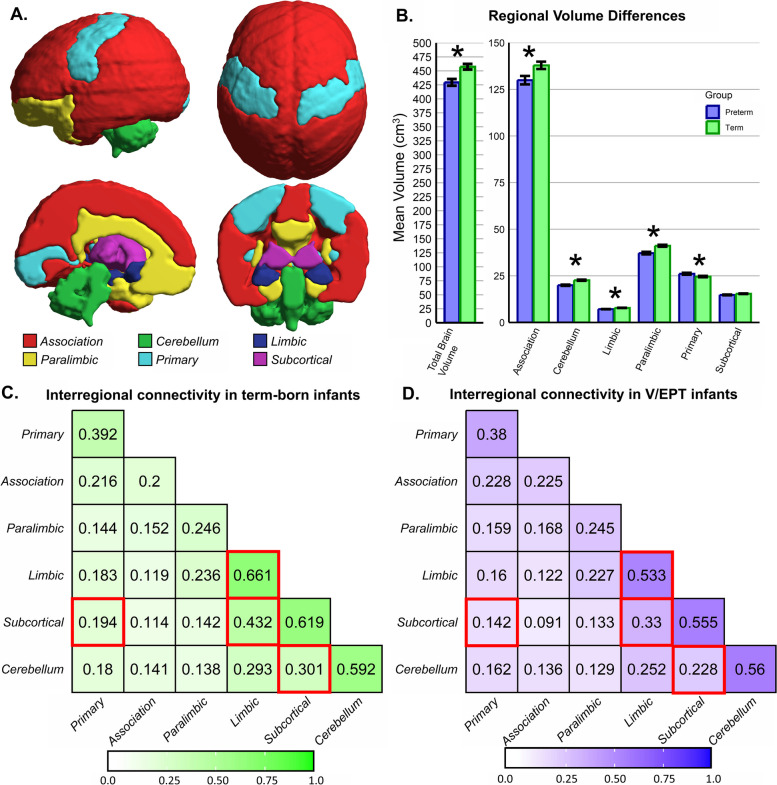
The mean BOLD time series were extracted from the neonatal aal atlas [56] with the inclusion of additional ROIs comprising the brainstem and cerebellum. Importantly, despite evidence of some functional distinctions across cerebellar lobules [57], given the size of infant cerebellums and our smoothing parameters, we have elected to collapse lobules into cerebellar lobes to minimize signal bleed across ROIS, resulting in a total of 96 ROIs (Additional file 1: Supplemental Information (SI) 1). Pearson correlations were computed between all ROIs and z-transformed using a Fischer transformation (Additional file 1: SI 2) [25, 58, 59]. ROIs were grouped into functional regions defined by Mesulam (2000) into primary, association, paralimbic, limbic, subcortical, and cerebellum [60] (Fig. 2A; Additional file 1: SI 3). For structural analyses, the six functional regions were warped into subject space with tissue masking to only include gray matter for cortical ROI. Total parenchymal volume was calculated for the entire brain, followed by volume for each functional region.
Fig. 2.
Interregional connectivity differences by birth. A Regional parcellation into red-association, green-cerebellum, dark blue-limbic, yellow-paralimbic, light blue-primary, and purple-subcortical. B Differences in volume for all regions with all differences significant at p < .05. Term-born infants exhibit greater volume in all regions except primary sensorimotor regions which are larger in very and extremely preterm (V/EPT) infants. C,D Differences in connectivity for all regional connections, with term-born infants exhibiting greater connectivity for four connection highlighted in red: cerebellum-subcortical, limbic-limbic, subcortical-limbic, and subcortical-primary
First, case–control analyses were performed between the term-born and preterm infants to assess differences in brain volume and connectivity. Group difference ANCOVAs for regional volumes were performed including total brain volume as a covariate to correct for differences across individuals and postmenstrual age to account for the small group difference. The results were then subjected to multiple comparisons correction via false discovery rate (FDR) [61]. Mean interregional connectivity was then compared using multiple independent t-tests.
Second, to assess the effect of painful procedures on developing connections, connectivity was correlated with number of skin breaks in V/EPT infants, including intraregional connectivity by assessing connectivity between all ROIs within a region. Then, individual ROI-to-ROI connections exhibiting a significant relationship were identified.
Third, analyses were performed with assessments collected at 18 months of age. Initially, t-tests were performed to evaluate differences in skin breaks between ASD risk groups. Due to a purported relationship between autism and prematurity [10, 62] and to assess a dose–response relationship, a regression analysis was then performed examining painful procedures, GA at birth, and the interaction of the two on autism risk, using the MCHAT total score. Following significant interactions, marginal effects for breaks at each week of birth GA were calculated. Next, MSEL subscales were examined in the same manner to assess variation in neurodevelopment.
Finally, analyses were conducted to assess the relationship between connectivity and neurodevelopmental scores. Connections sensitive to breaks at TEA were correlated with neurodevelopmental scores sensitive to breaks at 18 months to assess connectivity-neurodevelopmental overlaps.
Results
Study population
The study population includes 247 subjects: 148 infants born V/EPT with mean birth GA of 28.02 ± 2.80 weeks and scanned at 40.10 ± 2.01 weeks PMA and 99 healthy term-born infants from uncomplicated pregnancies with a mean birth GA of 39.15 ± 1.25 weeks and scanned at 40.90 ± 1.31 weeks PMA (Table 1).
Differences in term and V/EPT infant brain volume and connectivity
Compared to term-born infants, V/EPT infants exhibit significant differences in brain volume and connectivity. Term-born infants display significantly larger brain volumes overall (457.30cm3 vs 430.62cm3, t(238) = 3.485, p < 0.001), including larger association, cerebellar, limbic, and paralimbic volumes (pcorr < 0.001). Convesely, preterm infants exhibit larger primary sensorimotor regions (pcorr < 0.001) (Fig. 2B, Table 2). Term-born infants exhibit differences in connectivity relative to V/EPT infants, with greater cerebellum-subcortical, limbic-limbic, subcortical-limbic, and subcortical-primary connectivity (pcorr < 0.037) compared to V/EPT infants (Fig. 2C,D; Additional file 1: SI 4).
Table 2.
Volumetric group differences
| Region | Term | Preterm | Group F | Group p | Group pcorr | TBV F | TBV p | TBV pcorr | Age F | Age p | Age pcorr |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Association | 137,851.8 | 129,913.5 | 138.2 | < .001 | < .001 | 4669.1 | < .001 | < .001 | 70.17 | < .001 | < .001 |
| Cerebellum | 22,626.67 | 19,954.29 | 108.5 | < .001 | < .001 | 529.8 | < .001 | < .001 | 17.62 | < .001 | < .001 |
| Limbic | 7809.824 | 7134.252 | 79.2 | < .001 | < .001 | 409.5 | < .001 | < .001 | 0.2 | .656 | .727 |
| Paralimbic | 41,120.24 | 37,188.5 | 129.9 | < .001 | < .001 | 1419.3 | < .001 | < .001 | 6.6 | .011 | .162 |
| Primary | 24,625.42 | 26,126.44 | 30.0 | < .001 | < .001 | 1267.8 | < .001 | < .001 | 7.5 | .007 | < .001 |
| Subcortical | 15,394.36 | 14,775.56 | 19.9 | < .001 | < .001 | 825.0 | < .001 | < .001 | .1 | .727 | .727 |
Volumes presented in mm3, with corrected p values based on FDR correction
Skin break procedures and brain measures in V/EPT infants
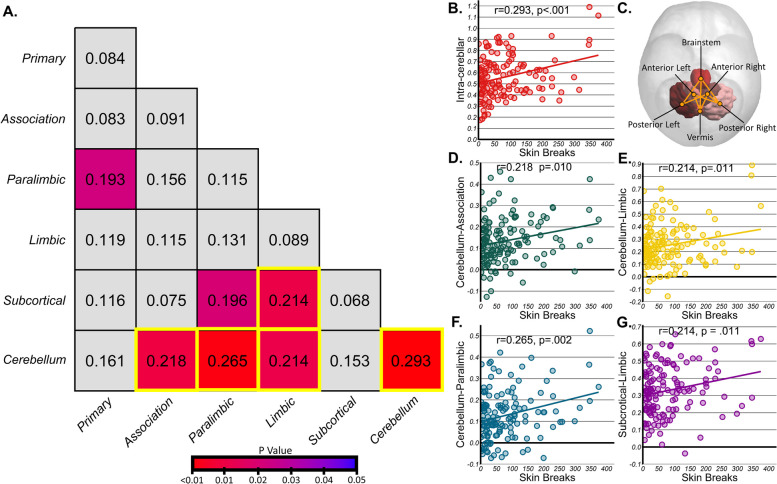
First, no significant relationships were observed between painful procedures and regional volume (pcorr ≥ 0.341); however, significant relationships were observed with functional connectivity. Following multiple comparison correction, intra-cerebellar connectivity (r(138) = 0.293, p < 0.001, pcorr = 0.009), as well as cerebellum connectivity with association (r(138) = 0.218, p = 0.002, pcorr = 0.047), paralimbic (r(138) = 0.265, p < 0.001, pcorr = 0.016) and limbic (r(138) = 0.214, p = 0.001, pcorr = 0.047) regions and subcortical-limbic connectivity (r(138) = 0.214, p = 0.011, pcorr = 0.047) exhibited a clear, positive relationship with the number of skin breaks (Fig. 3A). Subsequent control analyses for sociodemographic variables found no relationship between connectivity at term age between regions and maternal race (ps > 0.314), education (ps > 0.150), or employment status (ps > 0.125).
Fig. 3.
Interregional correlations for connectivity and painful procedures. A Interregional correlation r-values for each comparison, colored by p-value. Following false discovery rate (FDR) correction, cerebellum to association, paralimbic, limbic, and cerebellum as well as subcortical to limbic remained significant and are highlighted in yellow. B,C Significant relationship for inter-cerebellar connectivity with skin breaks, alongside ROI-to-ROI connections sensitive to pain. D–G Significant relationship for other regional connections and breaks. No significant ROI-to-ROI connections survived multiple comparison corrections across these regions
Subsequently, individual ROI-to-ROI comparisons revealed individual connections sensitive to skin breaks. Following correction, 8 intra-cerebellar connections exhibited significant positive relationships (pcorr < 0.024) with skin breaks (range = 0.210–0.287) (Table 3 and Fig. 3, see Additional file 1: SI 5–9 for the full tables). For the interregional connections, 44 of 264 cerebellum-association, 38 of 144 cerebellum-paralimbic connections, 9 of 36 cerebellum-limbic connections, and 10 of 48 subcortical-limbic connections were exhibited significant positive relationships between breaks and connectivity but none survived multiple comparison correction.
Table 3.
Significant ROI-to-ROI connections correlated with skin breaks by region
| Regions | ROI 1 | ROI2 | r | p | pcorr |
|---|---|---|---|---|---|
| Intra-cerebellar | Anterior left | Posterior right | 0.323 | < .001 | .001* |
| Posterior left | Brainstem | 0.319 | < .001 | .001* | |
| Posterior right | Brainstem | 0.319 | < .001 | .001* | |
| Anterior right | Posterior right | 0.297 | < .001 | .002* | |
| Anterior left | Vermis | 0.250 | .003 | .010* | |
| Vermis | Brainstem | 0.221 | .010 | .022* | |
| Anterior left | Anterior right | 0.220 | .010 | .022* | |
| Anterior right | Vermis | 0.208 | .016 | .029* | |
| Cerebellum-limbic | Posterior left | Rectus left | 0.330 | < .001 | .013* |
| Vermis | Parahippocampal gyrus right | 0.300 | < .001 | .027* | |
| Posterior left | Rectus right | 0.292 | < .001 | .027* | |
| Posterior left | Orbital (superior) left | 0.281 | < .001 | .027* | |
| Brainstem | Anterior cingulate left | 0.275 | .001 | .027* | |
| Posterior left | Orbital (superior) right | 0.275 | .001 | .027* | |
| Posterior right | Parahippocampal gyrus right | 0.273 | .001 | .027* | |
| Cerebellum-paralimbic | Posterior right | Olfactory right | 0.267 | .002 | .036* |
| Vermis | Olfactory right | 0.257 | .003 | .036* | |
| Posterior left | Olfactory left | 0.445 | .004 | .036* | |
| Anterior right | Olfactory right | 0.241 | .004 | .036* | |
| Posterior left | Amygdala left | 0.241 | .005 | .036* | |
| Vermis | Olfactory left | 0.226 | .009 | .044* | |
| Posterior left | Olfactory right | 0.225 | .009 | .044* |
* Significant at p < .05 corrected
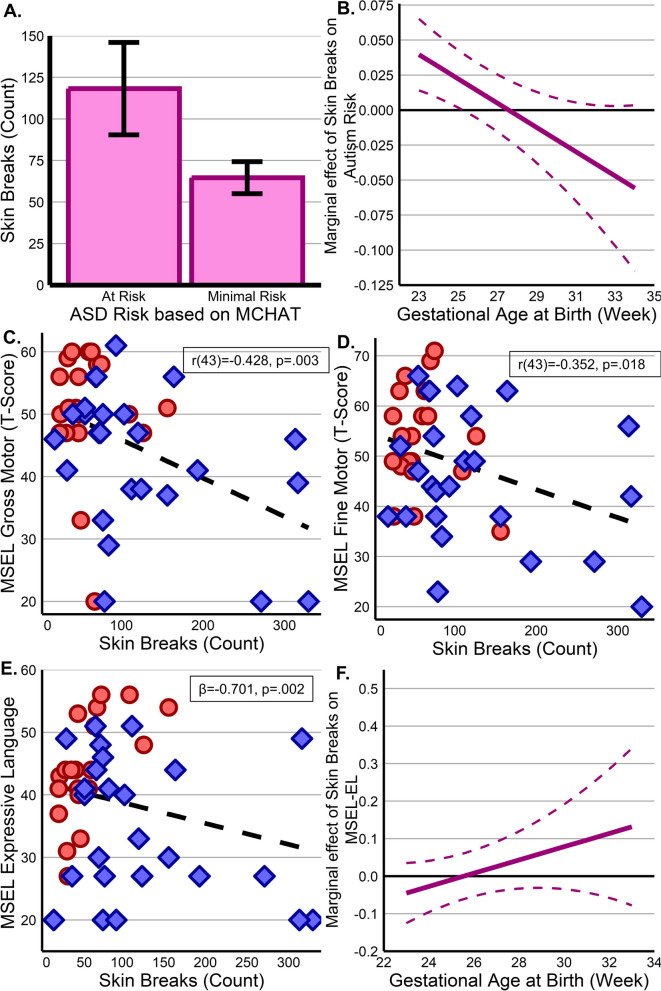
Skin break procedures and neurodevelopmental outcomes
At 18 months of age, toddlers identified as at risk for autism based on the MCHAT experienced significantly more breaks (mean = 118.27 ± 92.26), than those not at risk (mean = 64.65 ± 56.31, t(43) = 2.327, p = 0.024) (Fig. 4A). A subsequent regression model was significant (R2adj=0.329, F(3,41) = 6.701, p < 0.001). The model found that there is both a significant main effect for skin breaks (β = 0.175, p = 0.023) and an interaction between skin breaks and GA at birth (β = − 0.006, p = 0.035), but GA alone was not significant (p = 0.833). Evaluating marginal effects of skin breaks at each week of birth GA, skin breaks are positively associated with MCHAT score at younger birth ages, suggesting the most prematurely born infants are more vulnerable (Fig. 4B). Subsequent follow-up analyses controlling for sociodemographic variables found these results were present when controlling for the impact of maternal race, education, and employment status (Additional file 1: SI 10).
Fig. 4.
Impact of skin break procedures on neurodevelopment. A Infants at risk for autism spectrum disorder (ASD) experienced significantly more procedures than those not as risk with an apparently age effect (B) where earlier birth GA is positive associated between skin breaks and ASD risk score. C,D MSEL Gross and Fine motor scales exhibit a clear relationship of increasing deficits with greater pain exposures, showing EPT infants with blue diamonds and VPT infants with red circles. E A similar effect is observable in the expressive language scale which also shows a prominent age effect (F) with earlier birth GA showing a relationship between painful procedures and greater impairment (lower scores) which lessens over time
Consistent with prior literature [53], all MSEL subscales were strongly correlated with the MCHAT (range = − 0.548 to − 0.677, ps < 0.001) with higher MCHAT scores associated with greater impairment on MSEL subscales. While there were no relationships between breaks and visual reception or receptive language (ps > 0.261), simple relationships were observed with gross (r(43) = − 0.428, p = 0.003) and fine (r(43) = − 0.352, p = 0.018) motor scales (Fig. 4C,D), with no birth GA or interaction effects observable. Alternatively, expressive language exhibited the same complex relationship as the MCHAT (R2adj=0.402, F(3,41) = 9.191, p < 0.001), with a main effect for exposures (β = − 0.701, p = 0.002) (Fig. 4E) and interaction (β = 0.027, p = 0.001), but no effect for GA alone (p = 0.471). Marginal effects suggest that pain exposure early in life is negatively associated with expressive language—an effect that is minimized with increasing age (Fig. 4F). Follow-up analyses found these relationships to be durable even when accounting for maternal race, education, and employment status (Additional file 1: SI 9).
Connectivity and longitudinal neurodevelopment
Finally, analyses were performed to assess associations between TEA brain connectivity and 18-month neurodevelopment. Both MCHAT and Mullens scores were then compared to the 8 cerebellar ROI-to-ROI pairs associated with skin breaks. MCHAT scores were not associated with term age connectivity of any of the cerebellar connections (ps > 0.248). Similarly, no relationship was observed between cerebellar connectivity and either gross motor (ps > 0.228) or fine motor (ps > 0.528) scores at 18 months. Conversely, expressive language was associated with connectivity strength at term equivalent age between the anterior left and posterior left (r(38) = − 0.388, p = 0.016, pcorr = 0.048) anterior left and vermis (r(38) = − 0.447, p = 0.005, pcorr = 0.040), and anterior right and vermis (r(38) = − 0.381, p = 0.018, pcorr = 0.48) (Table 4). Negative relationships for each connection suggest that greater connectivity is associated with lower expressive language skills at 18 months.
Table 4.
Associations between connectivity and 18-month follow-up
| Cerebellar ROI 1 | Cerebellar ROI 2 | r | p | pcorr | |
|---|---|---|---|---|---|
| MCHAT | Anterior left | Posterior left | 0.173 | .313 | .453 |
| Anterior left | Vermis | 0.146 | .396 | .453 | |
| Anterior left | Posterior right | 0.197 | .248 | .453 | |
| Anterior right | Posterior left | 0.018 | .919 | .919 | |
| Anterior right | Vermis | 0.158 | .356 | .453 | |
| Posterior left | Brainstem | 0.173 | .313 | .453 | |
| Vermis | Brainstem | 0.146 | .396 | .453 | |
| Posterior right | Brainstem | 0.197 | .248 | .453 | |
| MSEL Gross Motor | Anterior left | Posterior left | 0.035 | .836 | .836 |
| Anterior left | Vermis | − 0.071 | .676 | .836 | |
| Anterior left | Posterior right | 0.105 | .538 | .836 | |
| Anterior right | Posterior left | 0.042 | .805 | .836 | |
| Anterior right | Vermis | − 0.203 | .228 | .836 | |
| Posterior left | Brainstem | 0.057 | .738 | .836 | |
| Vermis | Brainstem | − 0.085 | .618 | .836 | |
| Posterior right | Brainstem | 0.047 | .781 | .836 | |
| MSEL Fine Motor | Anterior left | Posterior left | − 0.071 | .677 | .864 |
| Anterior left | Vermis | 0.033 | .847 | .864 | |
| Anterior left | Posterior right | 0.107 | .528 | .864 | |
| Anterior right | Posterior left | 0.067 | .695 | .864 | |
| Anterior right | Vermis | − 0.029 | .864 | .864 | |
| Posterior left | Brainstem | − 0.043 | .801 | .864 | |
| Vermis | Brainstem | − 0.083 | .623 | .864 | |
| Posterior right | Brainstem | 0.044 | .798 | .864 | |
| MSEL Expressive Language | Anterior left | Posterior left | − 0.388 | .016 | .048* |
| Anterior left | Vermis | − 0.447 | .005 | .040* | |
| Anterior left | Posterior right | − 0.247 | .135 | .221 | |
| Anterior right | Posterior left | − 0.245 | .138 | .221 | |
| Anterior right | Vermis | − 0.381 | .018 | .048* | |
| Posterior left | Brainstem | − 0.074 | .659 | .720 | |
| Vermis | Brainstem | − 0.214 | .197 | .263 | |
| Posterior right | Brainstem | − 0.060 | .720 | .720 |
Correlation table for the Modified Checklist for Autism in Toddlers (MCHAT) and Mullens Scales of Early Learning (MSEL) scores at 18 months with ROI-to-ROI connectivity sensitive to pain at term equivalent age. *Significant at p < .05 corrected
Discussion
Our findings provide four major advances in the understanding of early-life painful exposures in preterm infants. First, exposures are associated with alterations in functional connectivity as early as TEA. Second, exposures are associated with worse neurodevelopmental outcomes including motor and language deficits and autism risk. Third, there may be an early critical period of vulnerability to pain. And fourth, connectivity within pain-sensitive connections may be predictive of future neurodevelopmental impairments.
Our cerebellar results harmonize with previous research showing atypical development in V/EPT infants, with smaller cerebellar volumes at TEA [22, 28–30]. This may be due to relative early cerebellar development, which experiences rapid growth in the second trimester [63] and can quadruple in volume prior to birth [30]. Between rapid structural growth and acting as an early functional hub [58], the cerebellum is a logical focus for understanding early disruptions in brain development.
The differences in cerebellum connectivity may stem from its role in the brain’s pain matrix. The cerebellum, together with the primary somatosensory cortex, limbic and paralimbic regions, including the amygdala, ventral striatum, and insula [64–67] make up the backbone of the mature, adult pain system [68]. While this network is fully intact in childhood, most functional networks are just beginning to organize during late gestation [26, 69–71]. While not directly causative, we may be observing early disruptions in this network’s formation with co-activations through repeated painful exposures. This interpretation would strongly comport with findings in adults, where chronic pain is associated with hyper-connectivity between pain regions, including the cerebellum, brainstem, and prefrontal regions [72, 73] (for review see Mayer et al. [74]). Our findings mirror chronic pain in adults, where repeated experiences of pain are associated with increases in connectivity. It should be noted, however, that other reports emphasize changes in the medial and inferior frontal lobes in both humans [72, 73] and rodents [46]. Conversely, our results largely implicate only the inferior frontal lobe. While not clear, this may be due to the relative underdevelopment of the region at later gestational ages (GA), making these more immature connections easier to influence than more established regions. Although more work is required to directly assess causal mechanisms between painful experiences and alterations in connectivity, greater connectivity is believed to be a proxy for the degree of synchronicity between two regions, derived from consistent and repeated coactivation. Therefore, functional connections are generally thought to form and strengthen in an experience-driven manner [75]. Importantly, the observed differences are not simply brain-wide increases in connectivity, but instead appear to be heavily localized within pain regions, further suggesting the changes are likely associated the repeated coactivation of the pain matrix when exposed to painful experiences. Importantly, this pattern extends beyond the broad, functional dysmaturation often observed in premature infants compared to term born both prior to TEA [22, 76] as well as at and beyond TEA [77], and instead suggest that pain exposures are associated with greater connectivity between selective regions that far outpaces the deficits seen between term and preterm born infants across other regions.
In our study cerebellar alterations at TEA were associated with development at 18 months. Altered cerebellar volume and connectivity are a consistently reported feature in ASD [78–80], including hyperconnectivity between the cerebellum and inferior frontal regions [81–83]. In addition, disrupted limbic connectivity has been associated with deficits in ASD including social and executive function [84, 85]. Therefore, pronounced alterations in the connections of these regions may be mimicking autistic-like differences. Additionally, our findings in expressive language are bolstered by growing evidence in the importance of the cerebellum in language, especially language production [86] and has similarly been linked to ASD [87]. While this cohort will continue to be assessed throughout toddlerhood and early childhood, these findings represent important associations to be followed as more infants reach assessment ages to validate the significance of these findings in the larger cohort.
Finally, there may be a particularly vulnerable period for EPT infants during which pain exposure may elevate the risk of neurodevelopmental deficits. Our findings corroborate prior work on the worsening impacts of prematurity on structural brain development [88]. The most likely reason being the lagging development of pain modulation pathways relative to afferent nociceptive pathways. Additionally, due to the rostral to caudal development of the brain in third trimester [89, 90], the most rostral frontal regions may be the most vulnerable to insult as they are still more actively developing than more posterior regions.
Despite the strengths of this study, there are some limitations. First, there is no standard way to measure NICU pain, with highly variable ratings across raters and between subjective, physiological, and behavioral measures [91–93]. Skin breaks serve as a common procedure that is widely accepted to cause pain/discomfort that occur frequently as part of routine care and have been linked with development of pain pathways in both human and animal studies [49, 88, 94]. Given the known discomfort associated with skin breaks, routine care often employees nonpharmacological interventions such as kangaroo care [95] swaddling or pacifier use to temper discomfort [96, 97]. Such interventions are difficult to quantify and are unaccounted for in this work. Furthermore, pharmacologic interventions, such as morphine, are also known to adversely influence brain development, and as such seldom employed as routine interventions prior to common skin break procedures. Similarly, we utilized caregiver report and questionnaires at 18 months rather than clinician-driven neurodevelopmental assessments. Future prospective studies should collect and control for both forms of pain management [95] as well as utilize clinical neurodevelopmental assessments. Second, in some cases multiple skin breaks may be required to successfully complete a single procedure, such as requiring a second heel stick to successfully draw blood. Multiple attempts for skin break procedures are variably recorded (routine for central line and intravenous placement, but not for heel lance) and, as such, could not be fully accounted for in our analyses. Third, the neurodevelopmental outcomes reported likely reflect both the effects of skin break procedures, as well as illness severity. Infants with higher disease burden require more consistent monitoring including more heel sticks and receive more interventions. This significant collinearity cannot be adequately controlled in the presented study design due to the tight coupling between the variables. As a result, we are unable to fully disentangle the impact of disease burden and the frequent experience of invasive skin break procedures. However, there is evidence that painful experiences are associated with alterations in brain connectivity [72, 73]. As a result, it is likely a contributor to altered neurodevelopmental trajectories that, unlike disease severity, is a more easily modifiable experience that can be targeted by interventions to optimally support neurodevelopment even in cases of significant illness. Fourth, pain is only one of several sensory experiences that are heightened in the extrauterine versus intrauterine environment. While pain is an intuitive mechanism driving these changes, extreme auditory and visual stimuli likely also impact development but were not accounted for here. Future studies should explore their impact on development. Finally, our subsample analyses linking connectivity to neurodevelopment are likely underpowered to detect more subtle relationships, especially as many of our observed correlations are between 0.2 and 0.4. Brain-behavior connections are often complex even when not assessed with 18-month lag and report correlation values within the observed range [98–100]. More work is required, however, to properly assess the longitudinal effects of painful exposures and interventions at all stages of development. Finally, social and societal risk factors are thought to play a significant role in neurodevelopment. While our findings remain durable when controlling for a subset of sociodemographic, a more robust collection of a wide range of socioeconomic data should be collected in the future to assess its interaction with pain and long-term development.
Conclusions
These findings provide an important step in understanding the impacts of earlier-than-typical exposure to the extrauterine environment. Our results suggest that early, repeated exposures to pain have a significant impact on the developing functional connectome and neurodevelopmental outcomes. These observed differences have important implications for our wider understanding of the effect of painful NICU procedures, which are often performed in the absence of analgesia, and how we conceptualize the long-term risks of these procedures. Finally, these findings emphasize the need to anticipate and develop novel strategies to treat pain given the known adverse effects of traditional, opioid-based pharmacotherapies.
Supplementary Information
Additional file 1: Supplemental Information 1. Full Brain Parcellation. Supplemental Information 2. Z-score Transformation. Supplemental Information 3. ROI and regional classifications. Supplemental Information 4. All Regional Connections.
Acknowledgements
We thank the participants and their families for their invaluable contributions.
Abbreviations
- V/EPT
Very and extremely premature
- VPT
Very preterm
- EPT
Extremely preterm
- PMA
Postmenstrual age
- ASD
Autism spectrum disorder
- NICU
Neonatal intensive care units
- TEA
Term-equivalent age
- MCHAT
Modified checklist for autism in toddlers-revised
- MSEL
Mullen scales of early learning
- AFNI
Analysis of functional neuroImages
- FDR
False discovery rate
- GA
Gestational age
Authors’ contributions
KMC contributed to the conception and design of the work, the analysis and interpretation of data, and drafted the manuscript. JDC contributed to the conception and design of the work, analysis and interpretation of data, and substantively revised the manuscript. JHK contributed to the design of the work and interpretation of data. SKB contributed to the interpretation of data, and substantively revised the manuscript. NA contributed to the conception of the work, interpretation of data, and substantively revised the manuscript. JM contributed to the acquisition and interpretation of data. ES contributed to the acquisition and interpretation of data. ML contributed to the acquisition and interpretation of data. AJP contributed to the conception of the work, interpretation of data, and substantively revised the manuscript. CL contributed to the conception and design of the work, interpretation of data, and substantively revised the manuscript. All authors read and approved the final manuscript.
Authors’ Twitter handles
Twitter handles: @KevinCookPhD (KMC).
Twitter handles: @DevBrainLab (CL).
Funding
This work is supported by the NIH National Heart, Lung, and Blood Institute at the National Institutes of Health (R01-HL116585 to CL); Eunice Kennedy Shriver National Institute of Child Health and Human Development at the National Institutes of Health (T32-HD098066 to KMC., U54-HD090257 & R01-HD099393 to CL); and the Canadian Institutes of Health Research (MOP-81116 to CL).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Children’s National Hospital Institutional Review Board (IRB) under approval ID #2391. Written consent was obtained from the parents of each infant.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller A-B, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 2.Gyamfi-Bannerman C, Ananth CV. Trends in spontaneous and indicated preterm delivery among singleton gestations in the United States, 2005–2012. Obstet Gynecol. 2014;124:1069–1074. doi: 10.1097/AOG.0000000000000546. [DOI] [PubMed] [Google Scholar]
- 3.Chawanpaiboon S, Vogel JP, Moller A-B, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7:e37–46. doi: 10.1016/S2214-109X(18)30451-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vogel JP, Chawanpaiboon S, Moller A-B, Watananirun K, Bonet M, Lumbiganon P. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018;52:3–12. doi: 10.1016/j.bpobgyn.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Younge N, Goldstein RF, Bann CM, Hintz SR, Patel RM, Smith PB, et al. Survival and Neurodevelopmental Outcomes among Periviable Infants. N Engl J Med. 2017;376:617–628. doi: 10.1056/NEJMoa1605566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993–2012. JAMA. 2015;314:1039–1051. doi: 10.1001/jama.2015.10244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Who: Recommended definitions, terminology and format for statistical tables related to the perinatal period and use of A new certificate for cause of perinatal deaths. Acta Obstet Gynecol Scand. 1977;56:247–53. [PubMed]
- 8.Cabral TI, da Silva LGP, Martinez CMS, Tudella E. Analysis of sensory processing in preterm infants. Early Hum Dev. 2016;103:77–81. doi: 10.1016/j.earlhumdev.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Bröring T, Oostrom KJ, Lafeber HN, Jansma EP, Oosterlaan J. Sensory modulation in preterm children: Theoretical perspective and systematic review. PLoS ONE. 2017;12:e0170828. doi: 10.1371/journal.pone.0170828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hee Chung E, Chou J, Brown KA. Neurodevelopmental outcomes of preterm infants: a recent literature review. Transl Pediatr. 2020;9(Suppl 1):S3–8. doi: 10.21037/tp.2019.09.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barre N, Morgan A, Doyle LW, Anderson PJ. Language abilities in children who were very preterm and/or very low birth weight: a meta-analysis. J Pediatr. 2011;158:766–774.e1. doi: 10.1016/j.jpeds.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 12.Woodward LJ, Moor S, Hood KM, Champion PR, Foster-Cohen S, Inder TE, et al. Very preterm children show impairments across multiple neurodevelopmental domains by age 4 years. Arch Dis Child Fetal Neonatal Ed. 2009;94:F339–F344. doi: 10.1136/adc.2008.146282. [DOI] [PubMed] [Google Scholar]
- 13.Kerr-Wilson CO, Mackay DF, Smith GCS, Pell JP. Meta-analysis of the association between preterm delivery and intelligence. J Public Health. 2012;34:209–216. doi: 10.1093/pubmed/fdr024. [DOI] [PubMed] [Google Scholar]
- 14.Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJS. Cognitive and Behavioral Outcomes of School-Aged Children Who Were Born Preterm: A Meta-analysis. JAMA. 2002;288:728–737. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]
- 15.Sucksdorff M, Lehtonen L, Chudal R, Suominen A, Joelsson P, Gissler M, et al. Preterm birth and poor fetal growth as risk factors of attention-deficit/ hyperactivity disorder. Pediatrics. 2015;136:e599–608. doi: 10.1542/peds.2015-1043. [DOI] [PubMed] [Google Scholar]
- 16.Kuzniewicz MW, Wi S, Qian Y, Walsh EM, Armstrong MA, Croen LA. Prevalence and neonatal factors associated with autism spectrum disorders in preterm infants. J Pediatr. 2014;164:20–25. doi: 10.1016/j.jpeds.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 17.Joseph RM, Korzeniewski SJ, Allred EN, O’Shea TM, Heeren T, Frazier JA, et al. Extremely low gestational age and very low birthweight for gestational age are risk factors for autism spectrum disorder in a large cohort study of 10-year-old children born at 23–27 weeks’ gestation. Am J Obstet Gynecol. 2017;216:304.e1–304.e16. doi: 10.1016/j.ajog.2016.11.1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gong QY, Roberts N, Garden AS, Whitehouse GH. Fetal and fetal brain volume estimation in the third trimester of human pregnancy using gradient echo MR imaging. Magn Reson Imaging. 1998;16:235–240. doi: 10.1016/S0730-725X(97)00281-6. [DOI] [PubMed] [Google Scholar]
- 19.Ge X, Shi Y, Li J, Zhang Z, Lin X, Zhan J, et al. Development of the human fetal hippocampal formation during early second trimester. Neuroimage. 2015;119:33–43. doi: 10.1016/j.neuroimage.2015.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andescavage NN, DuPlessis A, McCarter R, Vezina G, Robertson R, Limperopoulos C. Cerebrospinal Fluid and Parenchymal Brain Development and Growth in the Healthy Fetus. Dev Neurosci. 2016;38:420–429. doi: 10.1159/000456711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krsnik Ž, Majić V, Vasung L, Huang H, Kostović I. Growth of Thalamocortical Fibers to the Somatosensory Cortex in the Human Fetal Brain. Front Neurosci. 2017;11:233. doi: 10.3389/fnins.2017.00233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu Y, Stoodley C, Brossard-Racine M, Kapse K, Vezina G, Murnick J, et al. Altered local cerebellar and brainstem development in preterm infants. Neuroimage. 2020;213:116702. doi: 10.1016/j.neuroimage.2020.116702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilson S, Pietsch M, Cordero-Grande L, et al. Development of human white matter pathways in utero over the second and third trimester. Proc Natl Acad Sci U S A. 2021;118(20):e2023598118. 10.1073/pnas.2023598118 [DOI] [PMC free article] [PubMed]
- 24.Jaimes C, Machado-Rivas F, Afacan O, Khan S, Marami B, Ortinau CM, et al. In vivo characterization of emerging white matter microstructure in the fetal brain in the third trimester. Hum Brain Mapp. 2020;41:3177–3185. doi: 10.1002/hbm.25006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turk E, van den Heuvel MI, Benders MJ, de Heus R, Franx A, Manning JH, et al. Functional Connectome of the Fetal Brain. J Neurosci. 2019;39:9716–9724. doi: 10.1523/JNEUROSCI.2891-18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Asis-Cruz J, Andersen N, Kapse K, Khrisnamurthy D, Quistorff J, Lopez C, et al. Global Network Organization of the Fetal Functional Connectome. Cereb Cortex. 2021;31:3034–3046. doi: 10.1093/cercor/bhaa410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matthews LG, Walsh BH, Knutsen C, Neil JJ, Smyser CD, Rogers CE, et al. Brain growth in the NICU: critical periods of tissue-specific expansion. Pediatr Res. 2018;83:976–981. doi: 10.1038/pr.2018.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Limperopoulos C, Soul JS, Gauvreau K, Huppi PS, Warfield SK, Bassan H, et al. Late gestation cerebellar growth is rapid and impeded by premature birth. Pediatrics. 2005;115:688–695. doi: 10.1542/peds.2004-1169. [DOI] [PubMed] [Google Scholar]
- 29.Lee W, Al-Dossary H, Raybaud C, Young JM, Morgan BR, Whyte HEA, et al. Longitudinal cerebellar growth following very preterm birth. J Magn Reson Imaging. 2016;43:1462–1473. doi: 10.1002/jmri.25098. [DOI] [PubMed] [Google Scholar]
- 30.Bouyssi-Kobar M, du Plessis AJ, McCarter R, et al. Third Trimester Brain Growth in Preterm Infants Compared With In Utero Healthy Fetuses. Pediatrics. 2016;138(5):e20161640. 10.1542/peds.2016-1640. [DOI] [PMC free article] [PubMed]
- 31.Sa de Almeida J, Meskaldji D-E, Loukas S, Lordier L, Gui L, Lazeyras F, et al. Preterm birth leads to impaired rich-club organization and fronto-paralimbic/limbic structural connectivity in newborns. Neuroimage. 2021;225:117440. [DOI] [PubMed]
- 32.Bouyssi-Kobar M, De Asis-Cruz J, Murnick J, Chang T, Limperopoulos C. Altered functional brain network integration, segregation, and modularity in infants born very preterm at term-equivalent age. J Pediatr. 2019;213:13–21.e1. doi: 10.1016/j.jpeds.2019.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Slevin M, Farrington N, Duffy G, Daly L, Murphy JF. Altering the NICU and measuring infants’ responses. Acta Paediatr. 2000;89:577–581. doi: 10.1111/j.1651-2227.2000.tb00342.x. [DOI] [PubMed] [Google Scholar]
- 34.Williams AL, van Drongelen W, Lasky RE. Noise in contemporary neonatal intensive care. J Acoust Soc Am. 2007;121 5 Pt1:2681–90. [DOI] [PubMed]
- 35.Ream MA, Lehwald L. Neurologic consequences of preterm birth. Curr Neurol Neurosci Rep. 2018;18:48. doi: 10.1007/s11910-018-0862-2. [DOI] [PubMed] [Google Scholar]
- 36.Winkler-Schwartz A, Garfinkle J, Shevell MI. Autism spectrum disorder in a term birth neonatal intensive care unit population. Pediatr Neurol. 2014;51:776–780. doi: 10.1016/j.pediatrneurol.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 37.Carbajal R, Rousset A, Danan C, Coquery S, Nolent P, Ducrocq S, et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA. 2008;300:60–70. doi: 10.1001/jama.300.1.60. [DOI] [PubMed] [Google Scholar]
- 38.Cignacco E, Hamers J, van Lingen RA, Stoffel L, Büchi S, Müller R, et al. Neonatal procedural pain exposure and pain management in ventilated preterm infants during the first 14 days of life. Swiss Med Wkly. 2009;139:226–232. doi: 10.4414/smw.2009.12545. [DOI] [PubMed] [Google Scholar]
- 39.Cong X, Wu J, Vittner D, Xu W, Hussain N, Galvin S, et al. The impact of cumulative pain/stress on neurobehavioral development of preterm infants in the NICU. Early Hum Dev. 2017;108:9–16. doi: 10.1016/j.earlhumdev.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Britto CD, Rao Pn S, Nesargi S, Nair S, Rao S, Thilagavathy T, et al. PAIN–perception and assessment of painful procedures in the NICU. J Trop Pediatr. 2014;60:422–427. doi: 10.1093/tropej/fmu039. [DOI] [PubMed] [Google Scholar]
- 41.Fitzgerald M. The development of nociceptive circuits. Nat Rev Neurosci. 2005;6:507–520. doi: 10.1038/nrn1701. [DOI] [PubMed] [Google Scholar]
- 42.Vinall J, Miller SP, Chau V, Brummelte S, Synnes AR, Grunau RE. Neonatal pain in relation to postnatal growth in infants born very preterm. Pain. 2012;153:1374–1381. doi: 10.1016/j.pain.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 43.Vinall J, Miller SP, Bjornson BH, Fitzpatrick KPV, Poskitt KJ, Brant R, et al. Invasive procedures in preterm children: brain and cognitive development at school age. Pediatrics. 2014;133:412–421. doi: 10.1542/peds.2013-1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ranger M, Zwicker JG, Chau CMY, Park MTM, Chakravarthy MM, Poskitt K, et al. Neonatal pain and infection relate to smaller cerebellum in very preterm children at school age. J Pediatr. 2015;167:292–8.e1. doi: 10.1016/j.jpeds.2015.04.055. [DOI] [PubMed] [Google Scholar]
- 45.Leslie ATFS, Akers KG, Martinez-Canabal A, Mello LE de A, Covolan L, Guinsburg R. Neonatal inflammatory pain increases hippocampal neurogenesis in rat pups. Neurosci Lett. 2011;501:78–82. [DOI] [PubMed]
- 46.Chang P, Fabrizi L, Fitzgerald M. Early life pain experience changes adult functional pain connectivity in the rat somatosensory and the medial prefrontal cortex. J Neurosci. 2022;42:8284–8296. doi: 10.1523/JNEUROSCI.0416-22.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kidokoro H, Neil JJ, Inder TE. New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. AJNR Am J Neuroradiol. 2013;34:2208–2214. doi: 10.3174/ajnr.A3521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Valeri BO, Holsti L, Linhares MBM. Neonatal pain and developmental outcomes in children born preterm: a systematic review. Clin J Pain. 2015;31:355–362. doi: 10.1097/AJP.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 49.Duerden EG, Grunau RE, Chau V, Groenendaal F, Guo T, Chakravarty MM, et al. Association of early skin breaks and neonatal thalamic maturation: A modifiable risk? Neurology. 2020;95:e3420–e3427. doi: 10.1212/WNL.0000000000010953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nunes AS, Kozhemiako N, Hutcheon E, Chau C, Ribary U, Grunau RE, et al. Atypical neuromagnetic resting activity associated with thalamic volume and cognitive outcome in very preterm children. Neuroimage Clin. 2020;27:102275. doi: 10.1016/j.nicl.2020.102275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Robins DL, Fein D, Barton ML, Green JA. The Modified Checklist for Autism in Toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord. 2001;31:131–144. doi: 10.1023/A:1010738829569. [DOI] [PubMed] [Google Scholar]
- 52.Mullen EM. Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service Inc; 1995. [Google Scholar]
- 53.Harel-Gadassi A, Friedlander E, Yaari M, Bar-Oz B, Eventov-Friedman S, Mankuta D, et al. Risk for ASD in Preterm Infants: A Three-Year Follow-Up Study. Autism Res Treat. 2018;2018:8316212. doi: 10.1155/2018/8316212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.De Asis-Cruz J, Donofrio MT, Vezina G, Limperopoulos C. Aberrant brain functional connectivity in newborns with congenital heart disease before cardiac surgery. Neuroimage Clin. 2018;17:31–42. doi: 10.1016/j.nicl.2017.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comput Biomed Res. 1996;29:162–173. doi: 10.1006/cbmr.1996.0014. [DOI] [PubMed] [Google Scholar]
- 56.Shi F, Yap P-T, Wu G, Jia H, Gilmore JH, Lin W, et al. Infant brain atlases from neonates to 1- and 2-year-olds. PLoS ONE. 2011;6:e18746. doi: 10.1371/journal.pone.0018746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stoodley CJ, Schmahmann JD. Functional topography of the human cerebellum. Handb Clin Neurol. 2018;154:59–70. doi: 10.1016/B978-0-444-63956-1.00004-7. [DOI] [PubMed] [Google Scholar]
- 58.van den Heuvel MI, Turk E, Manning JH, Hect J, Hernandez-Andrade E, Hassan SS, et al. Hubs in the human fetal brain network. Dev Cogn Neurosci. 2018;30:108–115. doi: 10.1016/j.dcn.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cook KM, De Asis-Cruz J, Lopez C, Quistorff J, Kapse K, Andersen N, et al. Robust sex differences in functional brain connectivity are present in utero. Cereb Cortex. 2023;33:2441–2454. doi: 10.1093/cercor/bhac218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mesulam M. Principles of behavioral and cognitive neurology. Oxford UK: Oxford University Press; 2000. [Google Scholar]
- 61.Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J R Stat Soc. 1995;57:289–300. [Google Scholar]
- 62.Wang C, Geng H, Liu W, Zhang G. Prenatal, perinatal, and postnatal factors associated with autism: A meta-analysis. Medicine. 2017;96:e6696. doi: 10.1097/MD.0000000000006696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dovjak GO, Schmidbauer V, Brugger PC, Gruber GM, Diogo M, Glatter S, et al. Normal human brainstem development in vivo: a quantitative fetal MRI study. Ultrasound Obstet Gynecol. 2021;58:254–263. doi: 10.1002/uog.22162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Coombes SA, Misra G. Pain and motor processing in the human cerebellum. Pain. 2016;157:117–127. doi: 10.1097/j.pain.0000000000000337. [DOI] [PubMed] [Google Scholar]
- 65.Damascelli M, Woodward TS, Sanford N, Zahid HB, Lim R, Scott A, et al. Multiple Functional Brain Networks Related to Pain Perception Revealed by fMRI. Neuroinformatics. 2022;20:155–172. doi: 10.1007/s12021-021-09527-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Michelle Welman FHS, Smit AE, Jongen JLM, Tibboel D, van der Geest JN, Holstege JC. Pain Experience is Somatotopically Organized and Overlaps with Pain Anticipation in the Human Cerebellum. Cerebellum. 2018;17:447–460. doi: 10.1007/s12311-018-0930-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zheng W, Woo C-W, Yao Z, Goldstein P, Atlas LY, Roy M, et al. Pain-Evoked Reorganization in Functional Brain Networks. Cereb Cortex. 2020;30:2804–2822. doi: 10.1093/cercor/bhz276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jensen KB, Regenbogen C, Ohse MC, Frasnelli J, Freiherr J, Lundström JN. Brain activations during pain: a neuroimaging meta-analysis of patients with pain and healthy controls. Pain. 2016;157:1279–1286. doi: 10.1097/j.pain.0000000000000517. [DOI] [PubMed] [Google Scholar]
- 69.Keunen K, Counsell SJ, Benders MJNL. The emergence of functional architecture during early brain development. Neuroimage. 2017;160:2–14. doi: 10.1016/j.neuroimage.2017.01.047. [DOI] [PubMed] [Google Scholar]
- 70.Fransson P, Skiöld B, Horsch S, Nordell A, Blennow M, Lagercrantz H, et al. Resting-state networks in the infant brain. Proc Natl Acad Sci U S A. 2007;104:15531–15536. doi: 10.1073/pnas.0704380104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.van den Heuvel MI, Thomason ME. Functional Connectivity of the Human Brain in Utero. Trends Cogn Sci. 2016;20:931–939. doi: 10.1016/j.tics.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jones SA, Morales AM, Holley AL, Wilson AC, Nagel BJ. Default mode network connectivity is related to pain frequency and intensity in adolescents. Neuroimage Clin. 2020;27:102326. doi: 10.1016/j.nicl.2020.102326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Li T, Zhang S, Kurata J. Suppressed descending pain modulatory and enhanced sensorimotor networks in patients with chronic low back pain. J Anesth. 2018;32:831–843. doi: 10.1007/s00540-018-2561-1. [DOI] [PubMed] [Google Scholar]
- 74.Mayer EA, Gupta A, Kilpatrick LA, Hong J-Y. Imaging brain mechanisms in chronic visceral pain. Pain. 2015;156(Suppl 1):S50–63. doi: 10.1097/j.pain.0000000000000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kelly C, Castellanos FX. Strengthening connections: functional connectivity and brain plasticity. Neuropsychol Rev. 2014;24:63–76. doi: 10.1007/s11065-014-9252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.De Asis-Cruz J, Kapse K, Basu SK, Said M, Scheinost D, Murnick J, et al. Functional brain connectivity in ex utero premature infants compared to in utero fetuses. Neuroimage. 2020;219:117043. doi: 10.1016/j.neuroimage.2020.117043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Volpe JJ. Dysmaturation of Premature Brain: Importance, Cellular Mechanisms, and Potential Interventions. Pediatr Neurol. 2019;95:42–66. doi: 10.1016/j.pediatrneurol.2019.02.016. [DOI] [PubMed] [Google Scholar]
- 78.Wang SS-H, Kloth AD, Badura A. The cerebellum, sensitive periods, and autism. Neuron. 2014;83:518–32. [DOI] [PMC free article] [PubMed]
- 79.Beckinghausen J, Sillitoe RV. Insights into cerebellar development and connectivity. Neurosci Lett. 2019;688:2–13. doi: 10.1016/j.neulet.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Stoodley CJ. The Cerebellum and Neurodevelopmental Disorders. Cerebellum. 2016;15:34–37. doi: 10.1007/s12311-015-0715-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Oldehinkel M, Mennes M, Marquand A, Charman T, Tillmann J, Ecker C, et al. Altered Connectivity Between Cerebellum, Visual, and Sensory-Motor Networks in Autism Spectrum Disorder: Results from the EU-AIMS Longitudinal European Autism Project. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4:260–270. doi: 10.1016/j.bpsc.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 82.Van Overwalle F, Mariën P. Functional connectivity between the cerebrum and cerebellum in social cognition: A multi-study analysis. Neuroimage. 2016;124 Pt A:248–55. [DOI] [PubMed]
- 83.Long Z, Duan X, Mantini D, Chen H. Alteration of functional connectivity in autism spectrum disorder: effect of age and anatomical distance. Sci Rep. 2016;6:26527. doi: 10.1038/srep26527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tuchman R. Autism. Neurol Clin. 2003;21:915–932. doi: 10.1016/S0733-8619(03)00011-2. [DOI] [PubMed] [Google Scholar]
- 85.Cook KM, You X, Cherry JB, Merchant JS, Skapek M, Powers MD, et al. Neural correlates of schema-dependent episodic memory and association with behavioral flexibility in autism spectrum disorders and typical development. J Neurodev Disord. 2021;13:35. doi: 10.1186/s11689-021-09388-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mariën P, Borgatti R. Language and the cerebellum. Handb Clin Neurol. 2018;154:181–202. doi: 10.1016/B978-0-444-63956-1.00011-4. [DOI] [PubMed] [Google Scholar]
- 87.Belteki Z, Lumbreras R, Fico K, Haman E, Junge C. The Vocabulary of Infants with an Elevated Likelihood and Diagnosis of Autism Spectrum Disorder: A Systematic Review and Meta-Analysis of Infant Language Studies Using the CDI and MSEL. Int J Environ Res Public Health. 2022;19(3):1469. 10.3390/ijerph19031469. [DOI] [PMC free article] [PubMed]
- 88.Brummelte S, Grunau RE, Chau V, Poskitt KJ, Brant R, Vinall J, et al. Procedural pain and brain development in premature newborns. Ann Neurol. 2012;71:385–396. doi: 10.1002/ana.22267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rakic P. Specification of cerebral cortical areas. Science. 1988;241:170–176. doi: 10.1126/science.3291116. [DOI] [PubMed] [Google Scholar]
- 90.Huttenlocher PR, Dabholkar AS. Regional differences in synaptogenesis in human cerebral cortex. J Comp Neurol. 1997;387:167–178. doi: 10.1002/(SICI)1096-9861(19971020)387:2<167::AID-CNE1>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 91.Stevens B, McGrath P, Dupuis A, Gibbins S, Beyene J, Breau L, et al. Indicators of pain in neonates at risk for neurological impairment. J Adv Nurs. 2009;65:285–296. doi: 10.1111/j.1365-2648.2008.04854.x. [DOI] [PubMed] [Google Scholar]
- 92.Shapiro CR. Nurses’ judgments of pain in term and preterm newborns. J Obstet Gynecol Neonatal Nurs. 1993;22:41–47. doi: 10.1111/j.1552-6909.1993.tb01781.x. [DOI] [PubMed] [Google Scholar]
- 93.Cignacco E, Hamers JPH, Stoffel L, van Lingen RA, Schütz N, Müller R, et al. Routine procedures in NICUs: factors influencing pain assessment and ranking by pain intensity. Swiss Med Wkly. 2008;138:484–491. doi: 10.4414/smw.2008.12147. [DOI] [PubMed] [Google Scholar]
- 94.Vinall J, Grunau RE. Impact of repeated procedural pain-related stress in infants born very preterm. Pediatr Res. 2014;75:584–587. doi: 10.1038/pr.2014.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hall RW, Anand KJS. Pain management in newborns. Clin Perinatol. 2014;41:895–924. doi: 10.1016/j.clp.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.McNair C, Campbell-Yeo M, Johnston C, Taddio A. Nonpharmacologic management of pain during common needle puncture procedures in infants: current research evidence and practical considerations: An update. Clin Perinatol. 2019;46:709–730. doi: 10.1016/j.clp.2019.08.006. [DOI] [PubMed] [Google Scholar]
- 97.van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, Kuis W, Schulpen TWJ, L’Hoir MP. Swaddling: a systematic review. Pediatrics. 2007;120:e1097–e1106. doi: 10.1542/peds.2006-2083. [DOI] [PubMed] [Google Scholar]
- 98.Wang K, Xu M, Ji Y, Zhang L, Du X, Li J, et al. Altered social cognition and connectivity of default mode networks in the co-occurrence of autistic spectrum disorder and attention deficit hyperactivity disorder. Aust N Z J Psychiatry. 2019;53:760–771. doi: 10.1177/0004867419836031. [DOI] [PubMed] [Google Scholar]
- 99.Yang S, Liu Z, Xiong X, et al. Effects of Mini-Basketball Training Program on Social Communication Impairment and Executive Control Network in Preschool Children with Autism Spectrum Disorder. Int J Environ Res Public Health. 2021;18(10):5132. 10.3390/ijerph18105132. [DOI] [PMC free article] [PubMed]
- 100.Vandewouw MM, Safar K, Mossad SI, Lu J, Lerch JP, Anagnostou E, et al. Do shapes have feelings? Social attribution in children with autism spectrum disorder and attention-deficit/hyperactivity disorder. Transl Psychiatry. 2021;11:493. doi: 10.1038/s41398-021-01625-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Supplemental Information 1. Full Brain Parcellation. Supplemental Information 2. Z-score Transformation. Supplemental Information 3. ROI and regional classifications. Supplemental Information 4. All Regional Connections.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.