Abstract
Introduction
Authentic leadership has been identified as a style needed to promote quality patient care and nurses’ retention.
Objective
The objective of this study was to investigate the correlation between the authentic leadership exhibited by nurse managers and the levels of resilience and self-efficacy among nurses.
Methods
A descriptive correlational study was conducted in an Egyptian hospital. A sample of convenience nurses (N = 285) completed the Authentic Leadership Inventory, the Connor-Davidson Resilience Scale, and the General Self-Efficacy Scale. The data were analyzed with correlation and structural equation modeling.
Results
The highest percentages of nurses (53.33% and 45.96%) perceived their nurse managers as having either moderate or high levels of authentic leadership. The majority of nurses rated themselves as moderately resilient (63.98%, 25.59 ± 6.56) and highly efficacious (76.70%, 30.68 ± 4.95). Furthermore, the analysis conducted using SPSS-AMOS reveals a significant positive association between the variables. Specifically, authentic leadership, along with its constituent components, accounts for approximately 22% of the overall variance observed in nurses’ resilience. Additionally, it is shown that these same factors explain approximately 34% of the variance in nurses’ self-efficacy. Moreover, the mediating role of self-efficacy was found to explain 49.3% of the variability in nurses’ resilience.
Conclusion
Nurse leaders should be aware of and implement effective and authentic leadership behaviors and apply tailored strategies for fostering nurses’ resilience and self-efficacy to deal with the challenging healthcare environment.
Keywords: authentic leadership, nurses, resilience, self-efficacy, structural equation model
1. Introduction
One theory of leadership that has been found to improve nurses’ outcomes is authentic leadership (AL). An authentic leader was identified as an effective leadership style needed in the healthcare sector to build positive work environments that promote quality patient care and the retention of nurses (Malik & Dhar, 2017; Alilyyani, 2022). The fundamental aspect of a leader's authenticity is in their capacity to cultivate self-awareness, appreciate and acknowledge others, and maintain unwavering commitment to their own identity. This entails comprehending the characteristics and principles of their followers, understanding their beliefs and values, and effectively incorporating these values and beliefs into their interactions with transparency (Avolio et al., 2004; Anwar et al., 2019).
Additionally, authentic leaders establish conducive conditions that cultivate employees’ autonomy and excitement for their work. Employees who perceive this support are more likely to demonstrate proactive behaviors. Additionally, Hu et al. (2018) assert that followers’ self-efficacy can be enhanced by the demonstration of confidence and trust in their talents, as well as by facilitating their awareness and acknowledgement of their own potential. Since nurses are responsible for making crucial decisions in a wide variety of patient care and work settings, it is crucial that the healthcare industry recognize the benefits that AL styles can bring to the healthcare sector and how they can improve nurses’ work effectiveness (Anwar et al., 2019). Exploring the relationship between AL and its influence on nurses’ resilience and self-efficacy is thus a study topic that requires further investigation in various health contexts, and our research aim extends to this purpose.
2. Review of Literature
2.1. Conceptual and Theoretical Framework
Our study is based on the conceptualization of three variables, namely AL, nurses’ resilience, and self-efficacy:
2.1.1. Authentic Leadership
Our research was guided by the AL theory developed by Avolio et al. (2004). AL is one of the relational or people-oriented styles of leadership. AL is a concept that encompasses a leader's behavioral pattern aimed at enhancing positive psychological capacities and cultivating a favorable ethical climate. The objective is to facilitate the development of self-awareness, internalized moral values, unbiased information processing, and transparent relationships between leaders and followers, thereby promoting positive personal development. Through personal and social identification, hope, positive emotions, optimism, and trust, this theory describes how AL and its elements and core behaviors affect the attitudes and behaviors of followers (Avolio et al., 2004; Walumbwa et al., 2008).
Within the hospital setting, the concept of AL has emerged as a prominent factor in fostering a positive work environment thorough understanding of team members’ roles within the institution, hence creating a conducive atmosphere for both leaders and team members (Maziero et al., 2020). In the same way, the leadership approach nurse managers demonstrate could be a key factor in boosting nurses’ confidence, which could make them more involved and committed to their jobs (Malik & Dhar, 2017; Alilyyani, 2022). Based on that, we hypothesized that AL and its four elements have a positive and significant effect on nurses’ resilience and self-efficacy.
2.1.2. Resilience
Resilience is an essential determinant in the realm of effective nursing leadership, denoting the capacity of individuals to adeptly adjust to the challenges they encounter and maintain an optimistic attitude towards forthcoming circumstances (Dzau et al., 2018). On the individual level, resilience is a process in which one leverages coping tools or mechanisms to respond positively to stress, resulting in a positive outcome (Braun et al., 2017). To remain resilient, an individual first encounters a stressor or hardship and then leverages the correct coping skills, resilience mechanisms, or tools that will result in a positive outcome for the specific situation. While in the workplace, resilience is effectively operationalized through relevant behavioral strategies associated with facilitating emotional and psychological change in the face of a challenge. This includes adapting to new ways of doing things, changing activities easily, or experimenting with new ideas (Braun et al., 2017).
Nursing is a profession that tests one's capacity for resilience because of the negative effects that long hours and a heavy workload have on nurses’ physical and mental health and the numerous stressful work situations (Abou Hashish & Ghanem Atalla, 2023). This highlights the significance of having resilience skills and the ability to adapt to and face the different challenges of the workplace (Erdogan et al., 2018; Abou Hashish & Ghanem Atalla, 2023). Nurse managers at the first level of hospital management are acknowledged as crucial professionals who establish a necessary link between the organization's strategic vision and the nurses operating at the forefront. They also directly affect the nursing workforce by their leadership and capacity to influence behaviors (Abd-El Aliem & Abou Hashish, 2021; Abou Hashish et al., 2023). The leaders’ creation and promotion of a culture of resilience are catalysts for nurses’ involvement in their jobs. However, nurses’ resilience could be affected by the degree of their confidence and self-efficacy (Abd-El Aliem & Abou Hashish, 2021).
2.1.3. Self-Efficacy
Another individual aspect that may be influenced by the leadership practices of nurse managers and hence affect nurses’ resilience is nurses’ sense of self-efficacy. According to Bandura's social cognitive theory (Bandura et al., 1997), self-efficacy is conceptualized as an individual's self-perception of their ability to effectively navigate various situations. It is closely associated with the conviction that one possesses the capability to successfully execute the anticipated actions. An individual's perception of their ability to engage in specific behaviors is shaped by cognitive, motivational, emotional, and selection processes (Bandura et al., 1997; Shorey & Lopez, 2021). There is a relationship that could exist between the nurses’ cognitive assessment of self-efficacy and their level of goal-setting and commitment towards attaining such goals. Nurses engage in cognitive evaluations to assess their own standards and understanding of their performance level, enabling them to make informed decisions regarding the issues they must confront and the level of effort required to address them (Shorey & Lopez, 2021).
2.2. Research Hypotheses
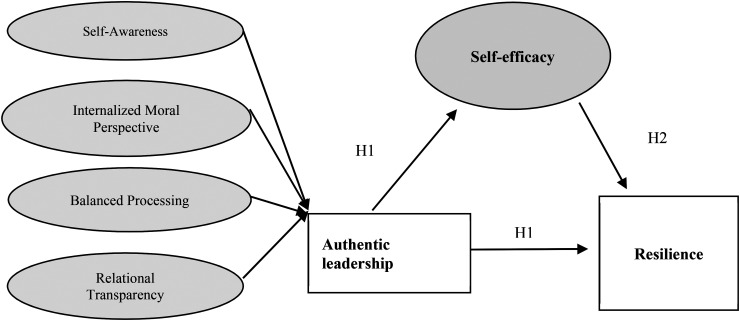
The current study's interest in AL stems from prior conceptualizations that suggested an association between AL and nurses’ positive outcomes in the workplace. The assumption of structural equation modeling (SEM) for this study was that the resilience and self-efficacy of nurses would improve if their managers modeled AL. See Figure 1. Based on this model, the following hypotheses were postulated:
H (1): There is a significant relationship between nurse managers’ AL (overall and components) and each of the nurses’ resilience and self-efficacy. AL has predictive power in this relationship.
H (2): Self-efficacy acts as a mediating factor in the relationship between AL and nurses’ resilience.
Figure 1.
Proposed Conceptual Model of the Study.
2.3. Significance of the Study
In comparison to other healthcare professionals, nurses frequently occupy a prominent position in patient care, where they regularly encounter the physical and emotional distress experienced by patients as part of their routine duties. Additionally, nurses contend with a demanding workload, rotating shifts, and the challenging work environment (Abou Hashish & Ghanem Atalla, 2023). Nurses require a leader that possesses the ability to provide support, empower individuals, and foster the development of their confidence and resilience. This study places emphasis on the AL leadership style, as it is recognized for its efficacy in promoting pleasant employee behaviors and generating advantages for both specific workgroups and entire organizations (Lee et al., 2019). Previous studies were conducted on AL and found that an authentic leader encourages followers to learn, discloses their values, engage in creative activities (Ahmad et al., 2015), build nurses’ self-efficacy (Laschinger et al., 2015), and promotes nurses’ creativity and team performance (Alilyyani, 2022). According to Alilyyani et al. (2018), authentic leaders possess the ability to inspire and encourage their employees, foster a sense of confidence and trust among them. Additionally, they are capable of creating ethical work environments, promoting organizational commitment, and maximizing employee involvement in their respective tasks (Ausar et al., 2016).
Limited studies have been conducted to investigate the relationship between nurse leaders’ successful behaviors and the resilience of nurses (Abd-El Aliem & Abou Hashish, 2021) as well as their self-efficacy (Laschinger et al., 2015), despite the existing theoretical connection between these variables. To our knowledge, there have been no studies that link AL, resilience, and self-efficacy as mediating factor in the nursing or management literature, especially among Egyptian nurses. The act of building upon prior research is crucial in order to address the existing void in knowledge. This study is hypothesized to yield valuable insights for the development of managerial and leadership approaches that are designed to foster favorable work attitudes among nurses, as well as improve results for both staff nurses and patients.
2.4. Aim of the Study
This research aimed to determine the relationship between the AL of nurse managers and nurses’ resilience and self-efficacy through SEM.
3. Methods
3.1. Research Design and Setting
A descriptive-correlational study was conducted in all inpatient care units at an Egyptian hospital in Alexandria governorate.
3.2. Sample and Inclusion /Exclusion Criteria
The total number of nurses employed in the hospital was 650. The inclusion criteria included registered nurses who had work experience of 6 months or more, were in full-time employment as hospital nurses, were willing to partake in the study, and could provide written informed consent as eligible participants. The exclusion criteria were student nurses, intern nurses, and nurses who were on leave during the data collection and who were unwilling to participate in the study. Hence, the final possible population size was 600. The determination of the sample size was conducted utilizing the Raosoft sample size calculator, employing the subsequent parameters: a population size of 600, a margin error of 5, a 95% confidence interval (CI), and a significance level set at P ≤ 0.05. Therefore, it is advised that a minimum sample size of 235 be used. In order to achieve the intended sample size, a total of 400 questionnaires were distributed among nurses. Out of this, 40 nurses participated in the pilot study, while the final questionnaires were completed and returned by 285 nurses. This number surpassed the predetermined sample size.
3.3. Research Instruments
This empirical study utilized three standardized questionnaires, which are outlined as follows:
3.3.1. Authentic Leadership Inventory
Authentic leadership inventory (ALI) was developed by Neider and Schriesheim (2011) to measure the level of AL as perceived by the study participants. ALI is a modified version of the Authentic Leadership Questionnaire developed by Avolio et al. (2007). The tool consisted of 16 items that assessed four subscales: self-awareness (four items), internalized moral perspective (five items), balanced processing (three items), and relational transparency (four items). Responses were measured with a five-point Likert-type scale ranging from (1) “strongly disagree” to (5) “strongly agree.” The total score ranged between 16 and 80, with a higher score indicating a high level of AL.
3.3.2. Connor-Davidson Resilience Scale
The Connor-Davidson Resilience Scale (CD-RISC-10) was developed by Connor and Davidson (2003) and validated by Nartova-Bochaver et al. (2021) to assess psychological resilience in the workplace. It is a single dimensional tool with 10 items rated on a four-point Likert scale, where the respondents are asked to rate the extent to which the items describe the resilient person, ranging from (1) Not at all true to (4) Exactly true, with a score ranging from 10 to 40. High scores represent greater adherence to the resilience criteria.
3.3.3. General Self-Efficacy Scale
Schwarzer and Jerusalem (1995) developed the General Self-Efficacy Scale (GSE) to assess a general sense of perceived self-efficacy, with 10 items rated on a four-point Likert scale ranging from (1) Not at all true to (4) Exactly true. For the GSE, the total score ranged between 10 and 40, with a higher score indicating more self-confidence.
Demographic form: In addition, the researchers developed a demographic information form for nurses. This form encompasses questions about their age, gender, years of work experience, and weekly working hours. Responses on this form are represented by frequency and percentage.
3.4. Validity and Reliability
A panel of experts in the related field tested the three questionnaires for content validity, and the results showed that they were valid, with content validity indices of 0.90, 0.87, and 0.83 for ALI, CD-RISC-10, and GSE, respectively. Also, the reliability was determined using Cronbach's alpha coefficient, which proved them reliable, with coefficient values of 0.716, 0.816, and 0.795 for ALI, CD-RISC-10, and GSE, respectively. In addition, a pilot study was carried out on 40 nurses with no change in the final tool.
3.5. Approvals, Ethical Considerations, and Data Collection
The Ethics Committee of the Faculty of Nursing at Alexandria University approved the study (April 2022). All ethical considerations related to written informed consent, confidentiality of the obtained data, securing anonymity, and respecting privacy were maintained. Prior to data collection, signed informed consent was collected from the participants after receiving approval from the hospital's administration. The participants were provided with information regarding the study's objectives and their ethical rights. It was made clear to the participants that they could withdraw from the study at any moment. The researchers distributed the questionnaires in paper form to nurses who agreed to participate in the study. The data were collected during nurses’ convenient times in the morning and evening shifts. Subsequently, the researchers proceeded to the units in order to retrieve the filled questionnaires, which were frequently entrusted to the nurse managers. The data were collected throughout a 4-month duration spanning from July to October 2022.
3.6. Data Analysis
The data that were gathered underwent a process of revision, coding, and entry into the statistical software program SPSS, version 25. The descriptive statistics employed to summarize the scaled data were the mean score and standard deviation, while the categorical data was summarized using frequencies and percentages. The study employed Pearson correlation coefficient analysis (r) to examine the association among AL, nurses’ resilience, and self-efficacy. The adequacy of the measurement model's fit was confirmed by the utilization of SPSS Amos for SEM. The statistical analyses were conducted using two-tailed tests and a significance level (α-error) of P ≤ 0.05.
Results
4.1. Nurses’ Characteristics
The majority of the participants (75.8%) were female, in the age group above 30 years old (79.6%) and had more than 5 years of experience (75.4%). About half of them worked between 48 and 55 hours per week. See Table 1.
Table 1.
Nurses’ Demographic Characteristics (N = 285).
| Demographic characteristics | No. (285) | % |
|---|---|---|
| Gender | ||
| Male | 69 | 24.2 |
| Female | 216 | 75.8 |
| Age | ||
| -≥30 | 58 | 20.4 |
| 31- | 227 | 79.6 |
| Years of experience | ||
| -≥5 | 70 | 24.6 |
| 6- | 215 | 75.4 |
| Number of working hours / weeks | ||
| 40h | 117 | 41.1 |
| 48h | 143 | 50.2 |
| 56 h | 25 | 8.7 |
4.2. Perceived AL, Nurses’ Resilience, and Self-Efficacy
Table 2 reveals that the highest percentage of nurses (53.33% and 45.96%) perceived moderate and high levels of their nurse managers’ AL, respectively, where the mean percent score was 57.87 ± 6.51. For AL dimensions, balanced processing showed the greatest mean value and high level of authenticity (75.65%, 11.35 ± 1.68), while the lowest mean percent score was related to relational transparency (70.91%, 14.18 ± 2.35). In addition, the mean percent score of nurses’ resilience showed a moderate level (63.98%, 25.59 ± 6.56), and about half of nurses (51.58%) showed a high self-efficacy score (76.70%, 30.68 ± 4.95). See supplementary Tables A1 and A2 for the detailed values of the resilience and self-efficacy items’ scores.
Table 2.
The Overall Mean Score of Perceived Authentic Leadership, Nurses’ Resilience, and Self-Efficacy (N = 285).
| Variables | Levels | No. | % | Min- Max | Mean ± SD | Mean% score |
|---|---|---|---|---|---|---|
| Self-awareness | Low | 6 | 2.11 | 6-20 | 14.31 ± 2.28 | 71.56% |
| Medium | 147 | 51.58 | ||||
| High | 132 | 46.32 | ||||
| Internalized moral perspective | Low | 3 | 1.05 | 8-25 | 18.03 ± 2.63 | 72.13% |
| Medium | 153 | 53.68 | ||||
| High | 129 | 45.26 | ||||
| Balanced processing | Low | 3 | 1.05 | 3-15 | 11.35 ± 1.68 | 75.65% |
| Medium | 72 | 25.26 | ||||
| High | 210 | 73.68 | ||||
| Relational transparency | Low | 3 | 1.05 | 5-20 | 14.18 ± 2.35 | 70.91% |
| Medium | 155 | 54.39 | ||||
| High | 127 | 44.56 | ||||
| Overall Authentic Leadership | Low | 2 | 0.70 | 22-76 | 57.87 ± 6.51 | 72.34% |
| Medium | 152 | 53.33 | ||||
| High | 131 | 45.96 | ||||
| Resilience | Low | 11 | 3.86 | 11-40 | 25.59 ± 6.56 | 63.98% |
| Medium | 139 | 48.77 | ||||
| High | 135 | 47.37 | ||||
| Self-efficacy | Low | 6 | 2.11 | 14-40 | 30.68 ± 4.95 | 76.70% |
| Medium | 132 | 46.32 | ||||
| High | 147 | 51.58 |
Note. SD = standard deviation.
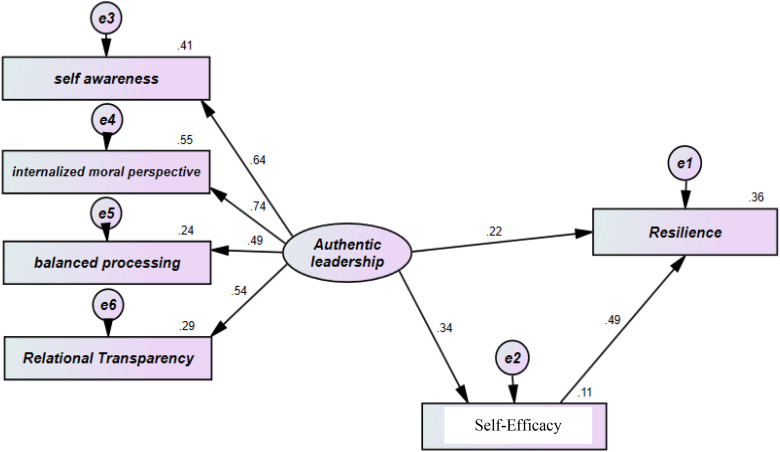
4.3. Correlation Among AL Practices, Nurses’ Resilience, and Self-Efficacy
The findings demonstrated a statistically significant and moderate correlation between the AL practices and both the resilience (r = 0.319, P < .001) and self-efficacy (r = 0.287, P < .001) of nurses. Additionally, a strong and significant correlation was observed between the nurses’ resilience and their self-efficacy (r = 0.567, P < .001). For more correlation values, see supplementary Table A3. Furthermore, the results presented in Table 3 and Figure 2 illustrate the structural equation model that was constructed using SPSS-AMOS. These findings provide a clear depiction of the standardized regression weights associated with the structured equation modeling, together with the model fit parameters (GFI = .986; RMSEA = .045; RMR = -.240, P < .001). The study found that AL, along with its components, explained approximately 22% and 34% of the variance in nurses’ resilience and self-efficacy. Furthermore, self-efficacy, serving as a mediating factor, was responsible for explaining 49.3% of the variability observed in the resilience levels of nurses. All variables that were observed in the model under examination exhibited a high level of significance (P < .001), and demonstrated robust estimates for the variables being studied.
Table 3.
Mediating Role of Self-Efficacy to the Relationship Between Authentic Leadership and Resilience.
| Variables | Estimate | R 2 | S.E. | C.R. | P | ||
|---|---|---|---|---|---|---|---|
| Resiliencea | <— | Authentic leadership | .987 | .219 | .288 | 3.429 | *** |
| Self-efficacyb | <— | Authentic leadership | 1.151 | .338 | .249 | 4.618 | *** |
| Resiliencec | <— | Self-efficacy | .653 | .493 | .069 | 9.435 | *** |
| Self-awareness | <— | Authentic leadership | 1.000 | .639 | |||
| Internalized moral perspective | <— | Authentic leadership | 1.334 | .739 | .171 | 7.797 | *** |
| Balanced processing | <— | Authentic leadership | .568 | .493 | .089 | 6.373 | *** |
| Relational transparency | <— | Authentic leadership | .868 | .538 | .127 | 6.811 | *** |
Note. Model fit parameters GFI = .986; RMSEA = .045; RMR=-.240. r = Pearson correlation; R2 = regression coefficient; CFI = comparative fit index; and RMSEA = root mean square error of approximation.
(r = 0.319, P < .001), b(r = 0.287, P < .001), c(r = 0.567, P < .001).
Figure 2.
Standardized coefficients for the effect of authentic leadership on nurses’ resilience mediated by self-efficacy.
4. Discussion
Our study expands the empirical research on the effect of AL among nurses. The findings revealed a moderate and statistically significant relationship between the perceived AL practices of nurse managers and the levels of resilience and self-efficacy reported by the nurses. The SEM outcome confirmed this correlation and revealed that AL and its components have a predictive power of 22% of the variance in nurses’ resilience and 34% of the variance in self-efficacy. Also, self-efficacy plays a mediating role and accounted for 49.3% of the variance in nurses’ resilience. In other words, our result demonstrated a significant effect of AL as an independent variable on nurses’ resilience as a dependent variable through the mediating effect of self-efficacy. These findings supported our hypotheses 1 and 2. The observed result can be attributed to the assertion that authentic leaders enhance the resilience of nurses. This is accomplished through the provision of timely support, fostering nurses’ autonomy, promoting self-efficacy, facilitating recovery from adversity, demonstrating heightened awareness of potential challenges, and developing contingency plans that help nurses in managing such challenges (Malik & Dhar, 2017).
Similarly, Sihvola et al. (2022) delineated that AL, as a famous leadership style, can foster a healthy work environment and positively impact nurses’ job satisfaction, recruitment, retention, and productivity through motivating and inspiring the employees towards mutual goals, as well as mentoring and guiding their performance. Concur with our research, Rego et al. (2016) documented that the primary responsibility of an authentic leader is to cultivate the self-efficacy of their followers through the demonstration of confidence and trust, fostering their awareness of their own potential, and enhancing their capacity to confront obstacles. Also, Laschinger et al. (2015) and Labrague et al. (2021) reported that AL correlated positively and moderately with self-efficacy. Moreover, Mao et al. (2023) found that AL positively predicted employee resilience, especially in the COVID-19 pandemic, and Abd-El Aliem and Abou Hashish (2021) indicated that the empowering leadership practices of nurse managers have a positive relationship with nurses’ resilience and work involvement. In this regard, Shaughnessy et al. (2018) and Abou Hashish et al. (2023) affirmed the need for continued professional development of effective leadership practices in nursing.
As we move to the descriptive level of the studied variables, the current findings reveal that the studied nurses perceived their nurse managers as having either moderate or high levels of AL, with higher authenticity associated with balanced processing and an internalized moral perspective. The result might be explained by considering the perceived role of nurse managers as role models for nurses through their leadership behaviors. This perspective aligns with prior studies that substantiate the necessity of authentic leaders in the workplace. Such leaders are inclined to cultivate trust and instill confidence in their subordinates by exemplifying honesty and truthfulness. Furthermore, they actively promote the cultivation of organizational norms and values among nurses. Consequently, these practices engender favorable outcomes within the nursing profession (Laschinger et al., 2015; Malik & Dhar, 2017; Lee et al., 2019; Alilyyani, 2022). In this regard, Hussein and Abou Hashish (2023) emphasized the role of nurse leaders in promoting an ethical work climate that fosters professional value and work accountability among nurses. This finding is consistent with Mrayyan et al. (2022), who reported average level of AL, but the highest dimension was the self-awareness. While Laschinger et al. (2015) and Wong et al. (2020) reported lower mean scores for AL and its subscales.
Moreover, the current study revealed that nurses had a moderate level of self-reported resilience. This level could be satisfactory and may be related to many factors, such as reported AL, supportive work environment, and the perceived role of nurses as frontline providers. In a similar vein, the study conducted by Chesak et al. (2020) established a correlation between authentic behaviors and the resilience of nurses. The researchers concluded that resilience can be ascribed to a nurturing work environment and supportive networks among colleagues, both of which play a vital role in enhancing employee morale, promoting unity, and facilitating the sharing of responsibilities. Results of the current study are in keeping with several studies that reported moderate to high resilience among nurses (Kannappan & Veigas, 2022; Jose et al., 2020). However, nurses still need to improve their resilience. According to Abou Hashish and Ghanem Atalla (2023), nurses are expected to demonstrate resilience, trust in their own capabilities, and adopt a proactive approach to effectively address and overcome various work-related issues through collaborative efforts. It is crucial for nursing leaders to recognize and comprehend the strategies by which nurses’ resilience can be cultivated.
Likewise, the present study showed that nurses had a high level of self-efficacy, which might be related to the perceived importance of self-efficacy as one of the indicators of resilience behavior (Kalandyk et al., 2016) and a good indicator of nurses performance (Abou Hashish & Bajbeir, 2022). According to the findings of Mróz (2015), individuals who exhibited a greater degree of generalized self-efficacy demonstrated better levels of mental resilience and greater capacity to effectively navigate challenging circumstances. These findings are consistent with the results reported by Handiyani et al. (2019), which revealed that more than 50% of the participants fell into the “high self-efficacy” category. On the other hand, Tong et al. (2021) mentioned that most nurses had a below-moderate level of perceived self-efficacy. They found different factors that could influence nurses’ self-efficacy, such as demographic characteristics, experiences, cultural background, and the degree of their nurse managers’ support. In this respect, Abou Hashish and Bajbeir (2022) emphasized that self-efficacy is a learned behavior and that different measures should be taken to develop self-efficacy beliefs and increase self-confidence among nurses. For instance, Dadipoor et al. (2021) proposed that nurse managers and supervisors should establish a congenial, supporting, and cooperative atmosphere to bolster the nursing personnel within the work environment. Additionally, it was suggested that further interventional research be conducted in order to enhance the self-efficacy of nurses. Tong et al. (2021) suggested that nursing managers should tailor continuing education programs to align with nurses’ characteristics.
5. Strengths and Limitations
There are certain limitations inherent to this study. The research employed a descriptive design, so precluding the establishment of causal relationships among the variables under investigation. Additional research utilizing experimental or longitudinal methodologies is necessary to validate our findings. Furthermore, it is worth noting that this research was carried out within the context of an Egyptian governorate, hence potentially limiting the applicability of the findings to broader contexts. Another limitation pertained to the utilization of self-reported data, which may possess an inherent bias. Notwithstanding these limitations, the present study contributes to the existing body of knowledge regarding the impact of AL on the outcomes of nurses, hence warranting further investigation in future study endeavors.
6. Conclusion
The findings of this study emphasize the significance of AL within the context of nursing practice. The results showed that nurses perceived their nurse managers as authentic leaders. Authentic leaders act as role models by balancing their roles, having self-awareness and open-mindedness, possessing self-regulation guided by a moral perspective, and creating a supportive and ethical work environment that allows for nurses’ autonomy and development. Through correlation and SEM, the current study shows that authentic leaders can create a healthy work environment and improve nurses’ self-efficacy and resilience. The majority of nurses rated themselves as moderately resilient and highly efficacious. Thus, nurse leaders should be aware of and implement effective and AL behaviors in their work environment and apply tailored strategies to foster nurses’ resilience and self-efficacy in the challenging healthcare environment.
7. Implications of the Study
The following implications are recommended:
7.1. Implications for Nursing Practice
Applying AL strategies that promote nurses’ wellbeing and quality of life, especially during challenging situations like the COVID-19 epidemic, is essential. Hence, advancing ongoing leadership training programs is inevitable.
Nurse managers should plan for learning opportunities and strive to inspire confident, efficacious, resilient, and assertive nurses. Participative decision-making and shared governance are essential strategies to promote nurse autonomy and self-efficacy. Equally, maintaining an ethical work climate can support AL and empower both leaders and nurses. The implementation of a self-efficacy and resilience training program has the potential to enhance individuals’ ability to effectively manage workplace challenges, bolster personal resilience, and impact the retention of nurses in the workplace.
7.2. Future Research Implications
Future research is recommended to explore the influence of AL on different nurses’ outcomes, such as job performance and deviance behaviors, as well as organizational variables such as ethical work climate, organizational justice, and support. Applying a qualitative study with an interview-based approach may allow for a better understanding of the effect of AL from nurses’ perspectives. It would be interesting to conduct a follow-up qualitative case study to determine how nurses define AL, resiliency, and self-efficacy in depth. Also, future interventional studies could examine the effect of AL, resilience-building, and succession planning on managers, nurses, and patient outcomes.
Supplemental Material
Supplemental material, sj-docx-1-son-10.1177_23779608231214213 for The Relationship Between Authentic Leadership and Nurses’ Resilience: A Mediating Role of Self-Efficacy by Heba Farouk Mohammad, Ebtsam Aly Abou Hashish and Nancy Sabry Elliethey in SAGE Open Nursing
Acknowledgments
The authors would like to extend their gratitude to all the nurses who have graciously consented to partake in this research.
Footnotes
Author Contributions: All authors have substantial contributions to Conceptualization, Methodology, Software, Data curation, Writing- Original draft preparation Abou Hashish E: final manuscript draft and correspondence.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval and Considerations: The study was authorized by the Ethics Committee of the Alexandria University Faculty of Nursing (April 2022). All ethical considerations related to informed written consent, confidentiality of the obtained data, securing anonymity, and respecting privacy were maintained. Participants were informed that they could opt out of the study at any time.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ebtsam Aly Abou Hashish https://orcid.org/0000-0003-0492-7615
Supplemental Material: Supplemental material for this article is available online.
References
- Abd-El Aliem S. M. F., Abou Hashish E. A. (2021). The relationship between transformational leadership practices of first-line nurse managers and Nurses’ organizational resilience and job involvement: A structural equation model. Worldviews on Evidence-Based Nursing, 18(5), 273–282. 10.1111/wvn.12535 [DOI] [PubMed] [Google Scholar]
- Abou Hashish E., Alnajjar H., Al Saddon A. (2023). Managerial power bases and its relationship to influence tactics and conflict management styles: Bedside nurses’ perspective. Worldviews on Evidence-Based Nursing, 20, 442–450. 10.1111/wvn.12670 [DOI] [PubMed] [Google Scholar]
- Abou Hashish E. A., Bajbeir E. F. (2022). The effect of managerial and leadership training and simulation on senior nursing Students’ career planning and self-efficacy. SAGE open Nursing, 8, 23779608221127952. 10.1177/23779608221127952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abou Hashish E. A., Ghanem Atalla A. D. (2023). The relationship between coping strategies, compassion satisfaction, and compassion fatigue during the COVID-19 pandemic. SAGE open Nursing, 9, 1–10. 10.1177/23779608231160463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad I., Zafar M. A., Shahzad K. (2015). Authentic leadership style and academia’s creativity in higher education institutions: Intrinsic motivation and mood as mediators. Transylvanian Review of Administrative Sciences, 11(46), 5–19. [Google Scholar]
- Alilyyani B. (2022). The effect of authentic leadership on Nurses’ trust in managers and job performance: A cross-sectional study. Nursing Reports (Pavia, Italy), 12(4), 993–1003. 10.3390/nursrep12040095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alilyyani B., Wong C. A., Cummings G. (2018). Antecedents, mediators, and outcomes of authentic leadership in healthcare: A systematic review. International Journal of Nursing Studies, 83(Jul 2018), 34–64. 10.1016/j.ijnurstu.2018.04.001 [DOI] [PubMed] [Google Scholar]
- Anwar A., Abid G., Waqas A. (2019). Authentic leadership and creativity: Moderated meditation model of resilience and hope in the health sector. European Journal of Investigation in Health, Psychology and Education, 10(1), 18–29. 10.3390/ejihpe10010003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ausar K., Kang H. J. A., Kim J. S. (2016). The effects of authentic leadership and organizational commitment on turnover intention. Leadership & Organization Development Journal, 37(2), 181–199. 10.1108/LODJ-05-2014-0090 [DOI] [Google Scholar]
- Avolio B. J., Gardner W., Walumbwa F. O. (2007). Authentic leadership questionnaire (ALQ). Default journal. https://www.mindgarden.com/69-authentic-leadership-questionnaire [Google Scholar]
- Avolio B. J., Gardner W. L., Walumbwa F. O., Luthans F., May D. R. (2004). Unlocking the mask: A look at the process by which authentic leaders impact follower attitudes and behaviors. The Leadership Quarterly, 15(6), 801–823. 10.1016/j.leaqua.2004.09.003 [DOI] [Google Scholar]
- Bandura A., Freeman W. H., Lightsey R. (1997). Self-Efficacy: The exercise of control. Journal of Cognitive Psychotherapy, 13, 158–166. 10.1891/0889-8391.13.2.158 [DOI] [Google Scholar]
- Braun T. J., Hayes B. C., DeMuth R. L. F., Taran O. A. (2017). The development, validation, and practical application of an employee agility and resilience measure to facilitate organizational change. Industrial and Organizational Psychology, 10(4), 703–723. 10.1017/iop.2017.79 [DOI] [Google Scholar]
- Chesak S. S., Bhagra A., Cutshall S., Ingram A., Benoit R., Medina-Inojosa J. R., Hayes S. N., Carolan B. J., Luthar S. (2020). Authentic connections groups: A pilot test of an intervention aimed at enhancing resilience among nurse leader mothers. Worldviews on Evidence-Based Nursing, 17(1), 39–48. 10.1111/wvn.12420 [DOI] [PubMed] [Google Scholar]
- Connor K. M., Davidson J. R. (2003). Development of a new resilience scale: The connor-davidson resilience scale (CD-RISC). Depression and Anxiety, 18(2), 76–82. 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Dadipoor S., Alavi A., Ghaffari M., Safari-Moradabadi A. (2021). Association between self-efficacy and general health: A cross-sectional study of the nursing population. BMC nursing, 20(1), 49. 10.1186/s12912-021-00568-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzau V. J., Kirch D. G., Nasca T. J. (2018). To Care Is Human - Collectively Confronting the Clinician-Burnout Crisis. The New England journal of medicine, 378(4), 312–314. 10.1056/NEJMp1715127 [DOI] [PubMed] [Google Scholar]
- Erdogan T. K., Sener A., Masat S., Kaya G., Palazoglu C. A., Koc Z. (2018). The factors affecting the resilience levels of the nurses working in a public hospital. New Trends and Issues Proceedings on Advances in Pure and Applied Sciences, 10, 01–10. 10.18844/gjpaas.v0i10.3739 [DOI] [Google Scholar]
- Handiyani H., Kusumawati A. S., Karmila R., Wagiono A., Silowati T., Lusiyana A., Widyana R. (2019). Nurses’ self-efficacy in Indonesia. Enfermeria Clinica, 29(52), 252–256. 10.1016/j.enfcli.2019.04.030 [DOI] [Google Scholar]
- Hu Y., Wu X., Zong Z., Xiao Y., Maguire P., Qu F., Wei J., Wang D. (2018). Authentic leadership and proactive behavior: The role of psychological capital and compassion at work. Frontiers in Psychology, 9(December 2018), 2470. 10.3389/fpsyg.2018.02470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussein A., Abou Hashish E. (2023). Relationship between nurses’ ethical ideology, professional values, and clinical accountability. Nursing Ethics., 096973302311722. 10.1177/09697330231172282 [DOI] [PubMed] [Google Scholar]
- Jose S., Dhandapani M., Cyriac M. C. (2020). Burnout and resilience among frontline nurses during COVID-19 pandemic: A cross-sectional study in the emergency department of a tertiary care center, north India. Indian Journal of Critical Care Medicine : Peer-Reviewed, Official Publication of Indian Society of Critical Care Medicine, 24(11), 1081–1088. 10.5005/jp-journals-10071-23667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalandyk H., Penar-Zadarko B., Krajewska-Kułak E. (2016). Nurses’ generalized self-efficacy in relation to their workplace. Progress in Health Sciences, 6(2), 92–99. 10.5604/01.3001.0009.5055 [DOI] [Google Scholar]
- Kannappan S. R., Veigas J. (2022). Perceived stress and resilience among nurses working in a selected hospital at mangalore. Journal of Health and Allied Sciences NU, 12(03)(3), 247–252. 10.1055/s-0041-1736455 [DOI] [Google Scholar]
- Labrague L. J., Al Sabei S., Al Rawajfah O., AbuAlRub R., Burney I. (2021). Authentic leadership and nurses’ motivation to engage in leadership roles: The mediating effects of nurse work environment and leadership self-efficacy. Journal of Nursing Management, 29(8), 2444–2452. 10.1111/jonm.13448 [DOI] [PubMed] [Google Scholar]
- Laschinger H. K., Borgogni L., Consiglio C., Read E. (2015). The effects of authentic leadership, six areas of worklife, and occupational coping self-efficacy on new graduate nurses’ burnout and mental health: A cross-sectional study. International Journal of Nursing Studies, 52(6), 1080–1089. 10.1016/j.ijnurstu.2015.03.002 [DOI] [PubMed] [Google Scholar]
- Lee H. F., Chiang H. Y., Kuo H. T. (2019). Relationship between authentic leadership and nurses’ intent to leave: The mediating role of work environment and burnout. Journal of Nursing Management, 27(1), 52–65. 10.1111/jonm.12648 [DOI] [PubMed] [Google Scholar]
- Malik N., Dhar R. L. (2017). Authentic leadership and its impact on extra role behaviour of nurses: The mediating role of psychological capital and the moderating role of autonomy. Personnel Review, 46(2), 277–296. 10.1108/PR-05-2015-0140 [DOI] [Google Scholar]
- Mao Y., Kang X., Lai Y., Yu J., Deng X., Zhai Y., Kong F., Ma J., Bonaiuto F. (2023). Authentic leadership and employee resilience during the COVID-19: The role of flow, organizational identification, and trust. Current Psychology (New Brunswick, N.J.), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziero V. G., Bernardes A., Righetti E. A. V., Spiri W. C., Gabriel C. S. (2020). Positive aspects of authentic leadership in nursing work: Integrative review. Revista Brasileira de Enfermagem, 73(6), e20190118. 10.1590/0034-7167-2019-0118 [DOI] [PubMed] [Google Scholar]
- Mrayyan M. T., Al-Atiyyat N., Al-Rawashdeh S., Algunmeeyn A., Abunab H. Y. (2022). Nurses’ authentic leadership and their perceptions of safety climate: Differences across areas of work and hospitals. Leadership in Health Services (Bradford, England), 35(3), 372–389. 10.1108/LHS-05-2021-0040 [DOI] [PubMed] [Google Scholar]
- Mróz J. (2015). Predictive roles of coping and resilience for the perceived stress in nurses. Progress in Health Sciences, 5(2), 77–83. 10.1007/s12144-022-04148-x [DOI] [Google Scholar]
- Nartova-Bochaver S., Korneev A., Bochaver K. (2021). Validation of the 10-item connor-davidson resilience scale: The case of Russian youth. Frontiers in Psychiatry, 12, 611026. 10.3389/fpsyt.2021.611026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neider L. L., Schriesheim C. A. (2011). The authentic leadership inventory (ALI): Development and empirical tests. The Leadership Quarterly, 22(6), 1146–1164. 10.1016/j.leaqua.2011.09.008 [DOI] [Google Scholar]
- Rego P., Lopes M. P., Nascimento J. L. (2016). Authentic leadership and organizational commitment: The mediating role of positive psychological capital. Journal of Industrial Engineering and Management (JIEM), 9(1), 129–151. 10.3926/jiem.1540 [DOI] [Google Scholar]
- Schwarzer R., Jerusalem M. (1995). Generalized self-efficacy scale. In Weinman J., Wright S.,, & Johnston M. (Eds.), Measures in health psychology: A user’s portfolio. Causal and control beliefs (pp. 35–37). NFER-NELSON. [Google Scholar]
- Shaughnessy M. K., Quinn Griffin M. T., Bhattacharya A., Fitzpatrick J. J. (2018). Transformational leadership practices and work engagement among nurse leaders. The Journal of Nursing Administration, 48(11), 574–579. 10.1097/NNA.0000000000000682 [DOI] [PubMed] [Google Scholar]
- Shorey S., Lopez V. (2021). Self-Efficacy in a nursing context. In Haugan G. (Ed.), Health promotion in health care – vital theories and research (pp. 145–158). Springer. [Google Scholar]
- Sihvola S., Kvist T., Nurmeksela A. (2022). Nurse leaders’ resilience and their role in supporting nurses’ resilience during the COVID-19 pandemic: A scoping review. Journal of Nursing Management, 30(6), 1869–1880. 10.1111/jonm.13640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong L., Tong T., Wang J., Li Y., Noji A. (2021). Determinants of transcultural self-efficacy among nurses in China: A cross-sectional study. Nursing & Health Sciences, 23(4), 880–887. 10.1111/nhs.12876 [DOI] [PubMed] [Google Scholar]
- Walumbwa F. O., Avolio B. J., Gardner W. L., Wernsing T. S., Peterson S. J. (2008). Authentic leadership: Development and validation of a theory-based measure. Journal of Management, 34(1), 89–126. 10.1177/0149206307308913 [DOI] [Google Scholar]
- Wong C., Walsh E. J., Basacco K. N., Mendes Domingues M. C., Pye D. R. (2020). Authentic leadership and job satisfaction among long-term care nurses. Leadership in Health Services, 33(3), 247–263. 10.1108/LHS-09-2019-0056 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-son-10.1177_23779608231214213 for The Relationship Between Authentic Leadership and Nurses’ Resilience: A Mediating Role of Self-Efficacy by Heba Farouk Mohammad, Ebtsam Aly Abou Hashish and Nancy Sabry Elliethey in SAGE Open Nursing