Abstract
Background and aim:
The pre-hospital management of a possible stroke is fundamental for the transport of patients to the correct HUB facility; thus, they must be transported to the Emergency Department (ED) by EMS vehicles. Our study aims to analyze the factors correlated with a higher probability of accessing the ED through the EMS in this event.
Methods:
This is a retrospective observational study. All accesses in the 120 EDs of the Lombardy region, with a diagnosis of discharge whose symptoms could resemble CPSS, were analyzed between 1 January 2019 and 31 December 2019.
Results:
We identified an increased probability of using the EMS vehicles of 0,05% (I.C. 95%: 0.04% - 0.06%; p<0.0001) for each additional year of age, considering patients aged 20 to 100 years and the percentage was significantly higher in the female population (58% vs 49%; p<0.001). Moreover, we calculated that the incidence of stroke was approximately 140 cases per 100,000 inhabitants.
Conclusions:
Only half of the citizens in the Lombardy region use the EMS in case of suspicion of stroke; further information campaigns are essential to educate citizens. Information strategies should be directed especially at men between 30 and 59 years old. (www.actabiomedica.it)
Keywords: emergency care pre-hospital, emergency medical services, Italy, stroke, training
Background
During the Covid-19 pandemic (1) the EMS (Emergency Medical System) and hospitals (2–5) have undergone significant changes in their organizational structure and in patients’ management (6,7). The time-dependent stroke network also underwent this major reorganization (8,9).
In the pre-hospital setting, only a clinical finding can lead to the suspicion of a stroke (10); in fact, the diagnosis of certainty is possible only after accessing the ED (Emergency Department) with second-level diagnostic tests. Nonetheless, it is important to recognize a possible stroke right from the call to the EMS, because the centralization time to the hospital, meaning the transport of the patient to the correct HUB facility, and the early warning to the admission hospital are essential to improve the outcome (11,12). Different scales have been developed to increase stroke recognition (13,14), to speed up the possible diagnosis by the EMS, which can then activate specific protocols in a short interval of time(15,16).
Patients’ management by the EMS improves the outcome (12,17) and guarantees treatment within the necessary time (18,19). For this reason, the laymen, who either face the symptoms of a possible stroke or of another time-dependent pathology as patients or witness them as bystanders, must activate the EMS and must not use their own means for accessing the ED independently. To improve the management of a possible stroke, the EMS has activated different projects (21,22) and they also studied the position of the hospitals, to ensure travel times are in line with the indications (23).
Nonetheless, the chain of survival must begin with the call to 118, the number of the Emergency Urgency Health Service (Servizio Sanitario Emergenza Urgenza), from either patients or bystanders (24), but adherence to this indication does not reach satisfactory values (25), despite the numerous information campaigns (26) that have shown a partial result in increasing adherence to call 118 (27).
The barriers that prevent the access of patients to the 118 system are many and varied (28); in fact, factors such as sex, age, or the presence of cohabitants (29) can influence the choice to call 118. For this reason, the formation of laymen is an important issue and must be implemented for the recognition of a possible stroke (30, 31).
Lombardy is the most populated Italian region with about ten million inhabitants; the whole Emergency Urgency system is managed by a single Agency, AREU (Agenzia Regionale Emergenza Urgenza – Emergency Urgency Regional Agency). Each call to the 118 system is handled by a professional operator present in the operations center, who, based on the type of patient and his characteristics, defines the vehicle to be sent to the scene. Vehicles are divided into basic life-support medical vehicles (BMV) with crews trained in Basic Life Support (BLS) maneuvers, Intermediate Life Support (ILS) medical vehicles with nurses (IMV), and Advanced Life Support (ALS) medical vehicles with both doctors and nurses; all IMV and AMV crews are trained in ALS (32).
Based on the clinical feedback of the patient at the scene, evaluated by either the doctor or the nurse according to the vehicle sent, the central office defines the hospital of destination. For AREU doctors and nurses, a possible stroke is defined as a patient with a positive Cincinnati Prehospital Stroke Scale (CPSS) (17), and the patient is centralized in one of the 38 regional HUB structures.
All patients who access an ED in the Lombardy region are registered in a single portal, called EUOL (Emergency and Urgency Online). Within the portal, 120 EDs of the region are present and both walk-in patients and those who access through the 118 system are registered (2).
Our study aims to define the factors correlated with a higher probability of accessing the ED through the 118 system in the event of a possible stroke.
Methods
This is a retrospective observational study. The study was conducted in accordance with the principles of the Helsinki Declaration.
All accesses in the 120 EDs of the Lombardy region which presented a diagnosis at discharge whose symptoms could resemble CPSS were analyzed in the period between 1 January 2019 and 31 December 2019.
We considered the ICD9 CM code for stroke (430.X, 431.X, 432.X, 433.X, 434.X, 435.X, 436.X, 437.X, 443.X).
The categorical variables are presented as absolute values and percentages, while the continuous variables are presented as mean and standard deviation. The categorical variables were analyzed using the χ2 test, and a linear regression has been implemented to correlate the age of the groups and the possibility to access the ED using the 118 system.
Differences were considered significant when p<0.05, otherwise they were considered non-significant (NS). The CI was defined at 95%. The Prism 8.0.1 statistical software (GraphPad Software LLC, San Diego, CA, USA) was used for this aim.
Results
In 2019, 25113 diagnoses of stroke-like syndromes were registered in Lombardy, according to the EDs portals; of these, 13436 (53%) had access with transport performed by the 118 system, while 11677 (47%) were walk-in patients. The mean age of the patients was 74 (15) and 12722 (51%) were females. 5598 (22%) patients have been registered as red codes, while 13466 (54%) as yellow.
221 (129 F and 92 M) died in the ED, of which 92% (203) were over 70 years old. Of these, 73% (161) had intracerebral hemorrhage (ICD 9-CM: 431) as a discharge diagnosis, and 8% (18) had subarachnoid hemorrhage (ICD 9-CM: 430).
In Figure 1, we performed a linear regression between the age of the subjects and the percentage of subjects who accessed the ED via the 118 system. We identified a coefficient equal to Y= 0.005*X+0,175, with a 95% CI range of 0.004 a 0.006; p<0.0001, meaning that there is an increased probability of using EMS vehicles of 0,05% for each additional year of age. The analysis was carried out taking into consideration patients aged 20 to 100 years.
Figure 1.
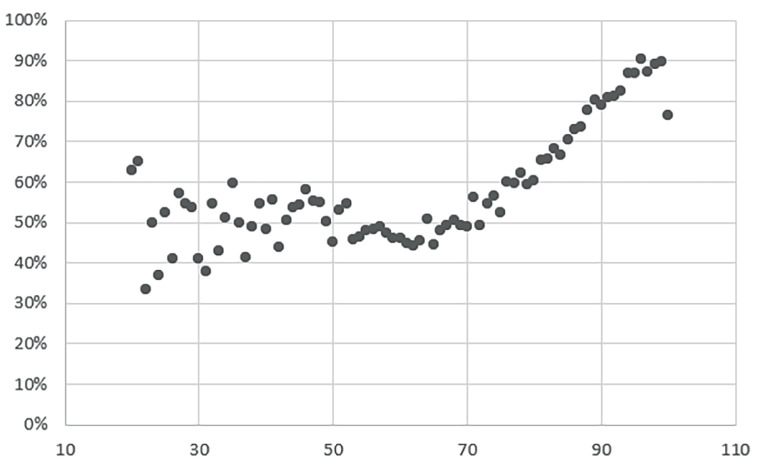
Percentage of patients (y-axis) with possible stroke admitted to the ED transported by the 118 system, grouped by age (x-axis).
The number of females with a diagnosis was 12730 (51%) and 7357 (58%) of them were transported by the EMS; 6079 (42%) were walk-in patients. The number of men was 12383 (49%) and 6079 (49%) of them were transported by the EMS; 6304 (51%) were walk-in patients.
The percentage of patients transported by the 118 system was significantly high in the female population (58% vs 49%).
In Table 1, we calculated the incidence of stroke-like syndromes per 100,000 inhabitants per year divided by age group. The demographic data was calculated taking into consideration the ISTAT (Istituto Nazionale di Statistica – National Statistical Institute) 2019 population data, using the reference population of 2019. The incidence was calculated by including the diagnosis of stroke (ischemic and hemorrhagic – about 14000), transient total amnesia (1922), and transient acute ischemia (7346); the diagnosis codes are shown in the Supplementary materials (Table S1).
Table 1.
Distribution of patients by age group and incidence of stroke-like syndromes per 100,000 inhabitants per year.
| Men | Females | Total | |
|---|---|---|---|
| 0-9 | 2,9 | 6,6 | 4,7 |
| 10-19 | 10,7 | 9,1 | 10,0 |
| 20-29 | 20,9 | 23,5 | 22,2 |
| 30-39 | 31,9 | 35,3 | 33,6 |
| 40-49 | 49,5 | 75,7 | 62,4 |
| 50-59 | 114,4 | 178,1 | 146,3 |
| 60-69 | 254,4 | 374,0 | 316,5 |
| 70-79 | 647,6 | 632,8 | 639,6 |
| 80-89 | 2035,8 | 962,5 | 1377,2 |
| 90 + | 6689,1 | 802,5 | 2228,5 |
| Total± | 258,8 | 241,6 | 250,0 |
±19 patients missing, missing data on sex
Table S1.
| ICD 9 CM | CODING | F | M | Tot |
|---|---|---|---|---|
| 4359 | UNSPECIFIED TRANSIENT CEREBRAL ISCHEMIA | 2379 | 2189 | 4568 |
| 431 | INTRACEREBRAL HEMORRHAGE | 1983 | 2126 | 4109 |
| 4358 | OTHER SPECIFIED TRANSIENT CEREBRAL ISCHEMIAS | 1437 | 1341 | 2778 |
| 43401 | CEREBRAL THROMBOSIS WITH CEREBRAL INFARCTION | 990 | 970 | 1960 |
| 4377 | TRANSIENT GLOBAL AMNESIA | 1027 | 895 | 1922 |
| 4371 | OTHER GENERALIZED ISCHEMIC CEREBROVASCULAR DISEASE | 898 | 837 | 1735 |
| 43400 | CEREBRAL THROMBOSIS WITHOUT MENTION OF CEREBRAL INFARCTION | 764 | 749 | 1513 |
| 436 | ACUTE, BUT ILL-DEFINED, CEREBROVASCULAR DISEASE | 707 | 653 | 1360 |
| 43491 | CEREBRAL ARTERY OCCLUSION, UNSPECIFIED WITH CEREBRAL INFARCTION | 502 | 500 | 1002 |
| 4321 | SUBDURAL HEMORRHAGE | 282 | 472 | 754 |
| 430 | SUBARACHNOID HEMORRHAGE | 348 | 289 | 637 |
| 43490 | CEREBRAL ARTERY OCCLUSION, UNSPECIFIED WITHOUT MENTION OF CEREBRAL INFARCTION | 244 | 240 | 484 |
| 4379 | UNSPECIFIED CEREBROVASCULAR DISEASE | 185 | 170 | 355 |
| 43411 | CEREBRAL EMBOLISM WITH CEREBRAL INFARCTION | 200 | 153 | 353 |
| 4378 | OTHER ILL-DEFINED CEREBROVASCULAR DISEASE | 173 | 171 | 344 |
| 43410 | CEREBRAL EMBOLISM WITHOUT MENTION OF CEREBRAL INFARCTION | 158 | 142 | 300 |
| 4370 | CEREBRAL ATHEROSCLEROSIS | 92 | 104 | 196 |
| 4329 | UNSPECIFIED INTRACRANIAL HEMORRHAGE | 84 | 104 | 188 |
| 43310 | OCCLUSION AND STENOSIS OF CAROTID ARTERY WITHOUT MENTION OF CEREBRAL INFARCTION | 41 | 67 | 108 |
| 4430 | RAYNAUD’S SYNDROME | 48 | 21 | 69 |
| 4373 | CEREBRAL ANEURYSM, NONRUPTURED | 33 | 28 | 61 |
| 4350 | BASILAR ARTERY SYNDROME | 30 | 20 | 50 |
| 43311 | OCCLUSION AND STENOSIS OF CAROTID ARTERY WITH CEREBRAL INFARCTION | 14 | 23 | 37 |
| 4372 | HYPERTENSIVE ENCEPHALOPATHY | 16 | 16 | 32 |
| 43301 | OCCLUSION AND STENOSIS OF BASILAR ARTERY WITH CEREBRAL INFARCTION | 11 | 13 | 24 |
| 43320 | OCCLUSION AND STENOSIS OF VERTEBRAL ARTERY WITHOUT MENTION OF CEREBRAL INFARCTION | 8 | 13 | 21 |
| 43390 | OCCLUSION AND STENOSIS OF UNSPECIFIED PRECEREBRAL ARTERY WITHOUT MENTION OF CEREBRAL INFARCTION | 9 | 9 | 18 |
| 43300 | OCCLUSION AND STENOSIS OF BASILAR ARTERY WITHOUT MENTION OF CEREBRAL INFARCTION | 6 | 12 | 18 |
| 4353 | VERTEBROBASILAR ARTERY SYNDROME | 6 | 11 | 17 |
| 4320 | NONTRAUMATIC EXTRADURAL HEMORRHAGE | 9 | 8 | 17 |
| 43391 | OCCLUSION AND STENOSIS OF UNSPECIFIED PRECEREBRAL ARTERY WITH CEREBRAL INFARCTION | 8 | 8 | 16 |
| 43321 | OCCLUSION AND STENOSIS OF VERTEBRAL ARTERY WITH CEREBRAL INFARCTION | 8 | 7 | 15 |
| 43380 | OCCLUSION AND STENOSIS OF OTHER SPECIFIED PRECEREBRAL ARTERY WITHOUT MENTION OF CEREBRAL INFARCTION | 6 | 7 | 13 |
| 4376 | NONPYOGENIC THROMBOSIS OF INTRACRANIAL VENOUS SINUS | 10 | 1 | 11 |
| 43330 | OCCLUSION AND STENOSIS OF MULTIPLE AND BILATERAL PRECEREBRAL ARTERIES WITHOUT MENTION OF CEREBRAL INFARCTION | 4 | 2 | 6 |
| 43381 | OCCLUSION AND STENOSIS OF OTHER SPECIFIED PRECEREBRAL ARTERY WITH CEREBRAL INFARCTION | 1 | 4 | 5 |
| 4374 | CEREBRAL ARTERITIS | 2 | 3 | 5 |
| 4352 | SUBCLAVIAN STEAL SYNDROME | 3 | 2 | 5 |
| 43331 | OCCLUSION AND STENOSIS OF MULTIPLE AND BILATERAL PRECEREBRAL ARTERIES WITH CEREBRAL INFARCTION | 2 | 1 | 3 |
| 4375 | MOYAMOYA DISEASE | 1 | 1 | 2 |
| 4351 | VERTEBRAL ARTERY SYNDROME | 1 | 1 | 2 |
Using the data in the Supplementary materials, we can define that the incidence of stroke in the Lombardy region is approximately 140 cases per 100,000 inhabitants per year.
In Table 2 we divided walk-in patients and patients transported by 118 vehicles stratified according to the triage code at arrival to the ED, whereas in Table 3 we distributed the two categories of patients according to the outcome.
Table 2.
Triage code and arrival mode.
| Triage | 118 vehicle | Walk-in patients |
|---|---|---|
| White | 31 (0.2%) | 85 (0.9%) |
| Green | 2094 (15.4%) | 3159 (32.8%) |
| Yellow | 7044 (51.8%) | 5552 (57.6%) |
| Red | 4427 (32.6%) | 848 (8.8%) |
| Black | 1 (0,01%) | 0 |
| Not performed | 11 (0.08%) | 75 (0.80%) |
| Total± | 13608 (58.4%) | 9719 (41.6%) |
±1786 data are missing; χ2 test p-value < 0.001
Table 3.
Arrival mode and outcome.
| Arrival mode | Deceased | Discharged | Abandoned the ED | Hospitalized |
|---|---|---|---|---|
| 118 vehicle | 206 (0.9%) | 2633 (11.3%) | 154 (0.7%) | 10615(45.5%) |
| Walk-in patients | 11 (0.1%) | 3636 (15.6%) | 335 (1.4%) | 5737 (24.6%) |
| Total± | 217 | 6269 | 489 | 16352 |
±1786 data are missing; χ2 test p-value < 0.001
Out of 489 subjects who either abandoned the ED or refused hospitalization, 137 (28%) have a diagnosis of unspecified transient cerebral ischemia (ICD9 4359), 78 (16%) have a diagnosis of other specified transient cerebral ischemias (ICD9 4358), 45 (9%) have a diagnosis of intracerebral hemorrhage (ICD9 431) and 43 (9%) cerebral thrombosis with cerebral infarction (ICD9 43401).
In addition, Table 3 underlines that 217 patients died after entering the ED. Of these, 206 accessed the EDs using EMS vehicles, and 11 self-presented.
Patients that have been hospitalized after accessing the ED on their own amount to 24.6% of the total of cases taken into consideration.
Discussion
Following the purpose of the study, we highlighted the demographic factors that characterize the population that uses the 118 system in case of stroke-like symptoms. We report that only 53% of patients with stroke or stroke-like syndromes access the ED by transport with the 118 system; among the factors considered, the age of the subject is positively correlated with the use of the EMS. In fact, the percentage of subjects that use this system increases by about 0.5% for each additional year of age. This phenomenon could be linked to the greater fragility of elderly subjects, who often have more comorbidities and for which a lower degree of autonomy could explain the use of the EMS. Furthermore, stroke is perceived as a rare pathology in young subjects, who may therefore not think of a stroke and go to the ED by their own means, thinking about a different cause of the symptoms.
The link between the symptoms under study and the age of the patient is highlighted in Table 1, which shows the incidence per 100,000 inhabitants of stroke-like pathologies in the Lombardy region. The incidence increases markedly beyond the 50-59 range. The total incidence is equal to 250.00 cases per 100,000 inhabitants, with a greater impact on the men population than on the female population (258.8 vs 241.6).
Regarding Table 1, it is important to point out that the incidence in the subjects aged over 90 years in the men population has little relevance because the resident population is small and is less than a third of the female population.
In our analysis, we found that the female population is more predisposed to use the 118 system than the men population (58% vs 49%, p <0.001). The reason could be linked to greater sensitivity during an emergency.
We recorded a significant difference between the triage code at arrival in the ED and transport mode. In fact, in case of patients with a red access code, 32.6% accessed the ED via EMS while 8.8% with their own vehicle. This trend is reversed in green code patients, where only 15.4% accessed the ED on a 118 vehicle compared to 32.8% who self-presented. Greater use of the 118 system in case of clinical instability or higher triage code is foreseeable; in fact, an autonomous transport may not be practicable, though the number of subjects in red code transported autonomously remains very high; these patients are exposed to an important risk. In fact, they could go into shock during the transfer and not be attended to by properly trained staff.
As presented in Table 3, there are also significant differences regarding the outcome; in fact, the percentage of patients admitted after access to the emergency room is equal to 45.51% in subjects who have access employing the 118 system and 24.59% in subjects who have autonomous access. It is very relevant to report that 489 subjects leave the ED before having a destination or before the diagnostic-therapeutic workup is completed. Furthermore, we point out that the number of deaths is higher in the population transported by EMS (0.9% vs 0.1%); this shows how the 118 system is used only in cases where the patient has greater instability.
The management of a possible stroke must begin as soon as possible, from the moment that either the patient or a bystander recognizes symptoms that hint at it. The transportation of these patients to the correct HUB facility is essential to correctly identify and diagnose the stroke with specific tests and treat the patients according to the protocols to improve their outcomes. Thus, the management of the possible stroke begins on the scene of the onset of symptoms and the EMS must be alerted.
The barriers preventing the access of patients to the EMS are known to be mainly sex, age, and the presence of cohabitants.
This study analyzed the behavior of the population of the Lombardy region when facing or witnessing the symptoms of a possible stroke, to identify specific sub-populations that are less likely to alert the EMS in case of a possible stroke. This will help design specific informative campaigns targeted specifically to those sub-populations so that more and more citizens will be aware of the importance of the use of the EMS. Moreover, we calculated the incidence of stroke-like syndromes and stroke in the Lombardy population.
Our study has some limitations; in fact, a series of clinical diagnoses made in the ED that are attributable to stroke are examined, such as amnesia, TIA (Unspecified Transient Cerebral Ischemia) and stroke, but we must point out that other conditions, such as facial paralysis, can give a similar picture but have not been examined within our population. Furthermore, following the pandemic, the habits of the population might have changed, and patients might therefore make greater use of the 118 system. A reason that could explain why few patients use the EMS might be the proximity of residential areas to large hubs, and for this reason, they might access the ED autonomously within short intervals of time; it becomes difficult to act on this population also because they see a great opportunity in autonomous access to the ED.
Conclusion
Our study shows that only half of the citizens use the 118 system, thus for this reason it is necessary to implement further information campaigns. Information strategies should be aimed at men subjects aged between 30 and 59, to identify and train the most refractory population.
A further study might have the purpose of defining only the patients diagnosed with stroke to understand if indeed in the case of the specific pathology, the attitudes and behavior of the subjects remain unchanged.
Ethics Committee:
The study was conducted in accordance with the Declaration of Helsinki and approved by AREU data protection officer 7.2022
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement, etc.) that might pose a conflict of interest in connection with the submitted article.
Authors Contribution:
GS and CS conceived and designed the study; GS, GR, AA and EK collected and analyzed the data; GS, AA, EK, and AC interpreted the results of the experiments; EK prepared figures; GS, AA, GMS, MM, drafted the first version of the manuscript. All authors edited and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
References
- Signorelli C, Odone A, Stirparo G, et al. SARS-CoV-2 transmission in the Lombardy Region: the increase of household contagion and its implication for containment measures. Acta Biomed. 2020 Nov 20;91(4):e2020195. doi: 10.23750/abm.v91i4.10994. doi: 10.23750/abm.v91i4.10994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirparo G, Oradini-Alacreu A, et al. Public health impact of the COVID-19 pandemic on the emergency healthcare system. J Public Health (Oxf) 2022 Mar 7;44(1):e149–e152. doi: 10.1093/pubmed/fdab212. doi: 10.1093/pubmed/fdab212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirparo G, Oradini-Alacreu A, Signorelli C, et al. Smart-working policies during COVID-19 pandemic: a way to reduce work-related traumas? Intern Emerg Med 17. 2022:2427–2430. doi: 10.1007/s11739-022-03076-9. doi: 10.1007/s11739-022-03076-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirparo G, Fagoni N, Bellini L, et al. Cardiopulmonary resuscitation missed by bystanders: Collateral damage of coronavirus disease 2019. Acta Anaesthesiol Scand. 2022 Oct;66(9):1124–1129. doi: 10.1111/aas.14117. doi: 10.1111/aas.14117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirparo G, Bellini L, Ristagno G, et al. The Impact of COVID-19 on Lombardy Region ST-Elevation Myocardial Infarction Emergency Medical System Network-A Three-Year Study. J Clin Med. 2022 Sep 27;11(19):5718. doi: 10.3390/jcm11195718. doi: 10.3390/jcm11195718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagoni N, Perone G, Villa GF, et al. The Lombardy emergency medical system faced with COVID-19: the impact of out-of-hospital outbreak. Prehosp Emerg Care. 2021 Jan-Feb;25(1):1–7. doi: 10.1080/10903127.2020.1824051. doi: 10.1080/10903127.2020.1824051. [DOI] [PubMed] [Google Scholar]
- Stirparo G, Ristagno G, Bellini L, et al. Changes to the major trauma pre-hospital emergency medical system network before and during the 2019 COVID-19 pandemic. J Clin Med. 2022;11:6748. doi: 10.3390/jcm11226748. doi: 10.3390/jcm11226748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pezzini A, Grassi M, Silvestrelli G, et al. Impact of SARS-CoV-2 on reperfusion therapies for acute ischemic stroke in Lombardy, Italy: the STROKOVID network. J Neurol. 2021 Oct;268(10):3561–3568. doi: 10.1007/s00415-021-10497-7. doi: 10.1007/s00415-021-10497-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asteggiano F, Divenuto I, Ajello D, et al. Stroke management during the COVID-19 outbreak: challenges and results of a hub-center in Lombardy, Italy. Neuroradiology. 2021 Jul;63(7):1087–1091. doi: 10.1007/s00234-020-02617-3. doi: 10.1007/s00234-020-02617-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worster A, Chan T. Evidence-based emergency medicine. Does this patient have a hemorrhagic stroke? Ann Emerg Med. 2011 May;57(5):535–6. doi: 10.1016/j.annemergmed.2010.08.023. doi: 10.1016/j.annemergmed.2010.08.023. [DOI] [PubMed] [Google Scholar]
- Heemskerk JL, Domingo RA, Tawk RG, et al. Time is brain: prehospital emergency medical services response times for suspected stroke and effects of prehospital interventions. Mayo Clin Proc. 2021 Jun;96(6):1446–1457. doi: 10.1016/j.mayocp.2020.08.050. doi: 10.1016/j.mayocp.2020.08.050. [DOI] [PubMed] [Google Scholar]
- Viereck S, M⊘ller TP, Iversen HK, Christensen H, Lippert F. Medical dispatchers recognise substantial amount of acute stroke during emergency calls. Scand J Trauma Resusc Emerg Med. 2016 Jul 7;24:89. doi: 10.1186/s13049-016-0277-5. doi: 10.1186/s13049-016-0277-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidale S, Agostoni E. Prehospital stroke scales and large vessel occlusion: A systematic review. Acta Neurol Scand. 2018 Jul;138(1):24–31. doi: 10.1111/ane.12908. doi: 10.1111/ane.12908. [DOI] [PubMed] [Google Scholar]
- Vidale S, Arnaboldi M, Frangi L, Longoni M, Monza G, Agostoni E. The Large ARtery Intracranial Occlusion Stroke Scale: A New Tool With High Accuracy in Predicting Large Vessel Occlusion. Front Neurol. 2019 Feb 19;10:130. doi: 10.3389/fneur.2019.00130. doi: 10.3389/fneur.2019.00130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuberg S, Song S, Saver JL, Mack WJ, Cen SY, Sanossian N. Impact of emergency medical services stroke routing protocols on Primary Stroke Center certification in California. Stroke. 2013 Dec;44(12):3584–6. doi: 10.1161/STROKEAHA.113.000940. doi: 10.1161/STROKEAHA.113.000940. [DOI] [PubMed] [Google Scholar]
- Katz BS, McMullan JT, Sucharew H, Adeoye O, Broderick JP. Design and validation of a prehospital scale to predict stroke severity. Stroke. 2015 Jun 4;46(6):1508–12. doi: 10.1161/STROKEAHA.115.008804. doi:10.1161/STROKEAHA.115.008804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Luca A, Giorgi Rossi P, Villa GF. Stroke group Italian Society pre hospital emergency Services. The use of Cincinnati Prehospital Stroke Scale during telephone dispatch interview increases the accuracy in identifying stroke and transient ischemic attack symptoms. BMC Health Serv Res. 2013 Dec 11;13:513. doi: 10.1186/1472-6963-13-513. doi: 10.1186/1472-6963-13-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alper BS, Foster G, Thabane L, Rae-Grant A, Malone-Moses M, Manheimer E. Thrombolysis with alteplase 3-4.5 hours after acute ischaemic stroke: trial reanalysis adjusted for baseline imbalances. BMJ Evid Based Med. 2020 Oct;25(5):168–171. doi: 10.1136/bmjebm-2020-111386. doi: 10.1136/bmjebm-2020-111386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturla MI, Kacerik E, Andreassi A, et al. Out of hospital cardiac arrest in sporting facilities: an overview of rescue for sideline doctors. Med Sport. 2023;76:70–8. doi: 10.23736/ S0025-7826.23.04231-X. [Google Scholar]
- Stirparo G, Andreassi A, Sechi GM, Signorelli C. Spring, it’s time to ROSC. J Prev Med Hyg. 2023;64:E87, E91. doi: 10.15167/2421-4248/jpmh2023.64.1.2782. doi: 10.15167/2421-4248/jpmh2023.64.1.2782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis NW, Bailey M, Buchwald N, Farooqui A, Khanna A. Factors that influence door-to-needle administration for acute stroke patients in the emergency department. J Neurosci Nurs. 2021 Jun 1;53(3):134–139. doi: 10.1097/JNN.0000000000000590. doi: 10.1097/JNN.0000000000000590. [DOI] [PubMed] [Google Scholar]
- Jauch EC, Huang DY, Gardner AJ, Blum JL. Strategies for improving outcomes in the acute management of ischemic stroke in rural emergency departments: a quality improvement initiative in the Stroke Belt. Open Access Emerg Med. 2018;10:53–9. doi: 10.2147/OAEM.S160269. doi: 10.2147/OAEM.S160269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eswaradass PV, Swartz RH, Rosen J, Hill MD, Lindsay MP. Access to hyperacute stroke services across Canadian provinces: a geospatial analysis. CMAJ Open. 2017 Jun 14;5(2):E454–E459. doi: 10.9778/cmajo.20160166. doi: 10.9778/cmajo.20160166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018 Mar 1;49(3):e46–110. doi: 10.1161/STR.0000000000000158. doi: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- Fussman C, Rafferty AP, Lyon-Callo S, Morgenstern LB, Reeves MJ. Lack of association between stroke symptoms knowledge and intent to call 911. Stroke. 2010 Jul;41(7):1501–7. doi: 10.1161/STROKEAHA.110.578195. doi: 10.1161/STROKEAHA.110.578195. [DOI] [PubMed] [Google Scholar]
- Silver FL, Rubini F, Black D, Hodgson CS. Advertising strategies to increase public awareness of the warning signs of stroke. Stroke. 2003 Aug 1;34(8):1965–8. doi: 10.1161/01.STR.0000083175.01126.62. doi: 10.1161/01.STR.0000083175.01126.62. [DOI] [PubMed] [Google Scholar]
- Mellon L, Hickey A, Doyle F, Dolan E, Williams D. Can a media campaign change health service use in a population with stroke symptoms? Examination of the first Irish stroke awareness campaign. Emerg Med J. 2014 Jul;31(7):536–540. doi: 10.1136/emermed-2012-202280. doi: 10.1136/emermed-2012-202280. [DOI] [PubMed] [Google Scholar]
- Kwan J, Hand P, Sandercock P. A systematic review of barriers to delivery of thrombolysis for acute stroke. Age Ageing. 2004 Mar;33(2):116–21. doi: 10.1093/ageing/afh064. doi: 10.1093/ageing/afh064. [DOI] [PubMed] [Google Scholar]
- Meurer WJ, Levine DA, Kerber KA, et al. Neighborhood influences on emergency medical services use for acute stroke: a population-based cross-sectional study. Ann Emerg Med. 2016 Mar 1;67(3):341–348.e4. doi: 10.1016/j.annemergmed.2015.07.524. doi: 10.1016/j.annemergmed.2015.07.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirparo G, Gambolò L, Bellini L, et al. Satisfaction evaluation for ACLS training. Acta Biomed. 2022 Jul 1;93(3):e2022260. doi: 10.23750/abm.v93i3.13337. doi: 10.23750/abm.v93i3.13337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuseppe S, Bellini L, Fagoni N, et al. Missed training, collateral damage from COVID 19? Disaster Med Public Health Prep. 2022 Jan 10:1–8. doi: 10.1017/dmp.2022.14. doi: 10.1017/dmp.2022.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stirparo G, Pireddu R, Kacerik E, et al. Stroke and the need for immediate assistance at the place of onset: the future of mandatory training for lay people in Italy. Ann Ig. 2022 Dec 15 doi: 10.7416/ai.2022.2553. doi: 10.7416/ai.2022.2553. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


