Abstract
Objectives:
Benign paroxysmal positional vertigo (BPPV) is a condition in which a patient gets severe vertigo on moving his head from one position to another. This study aims at comparing the traditional maneuver-Epley repositioning maneuver (ERM) and the newly emerged maneuver-Gans Repositioning maneuver (GRM).
Design:
A randomized controlled trial.
Settings:
Tertiary care teaching University Hospital.
Participants:
Posterior canal BPPV.
Intervention:
Two hundred and thirty-four patients with BPPV (PC-BPPV) of the posterior canal, diagnosed using the Dix-hallpike test (DH test), were recruited for the study as per random allocation. Two groups were divided by the random allocation method. One group was treated with the Epley maneuver and the other with Gans maneuver by two separate physiotherapists.
Main Outcome Measures:
DH test negativity (absence of vertigo and nystagmus), Vertigo Analogue Scale (VAS), and Dizziness Handicap Inventory (DHI). Twenty-four hours post-treatment assessments and data analysis were conducted by another (third) therapist. A one month follow-up subjective assessment was performed.
Results:
Results of one-variable Chi-square tests revealed significant improvement (P < .0001) in maximum (95%) patients of both groups whether subjects were given GRM or ERM. Also, objective improvement (DH test) was found in the Epley group (n = 118, 82.20%) and the Gans group (n = 116, 78.44%). Patients in both groups improved significantly with no dizziness on the VVAS scale (n = 118, 82.20%) in the Epley group and (n = 116, 78.44%) in the Gans group.
Conclusion:
GRM is as easy, effective, and safe maneuver as the ERM with the absence of recurrence for the treatment of posterior canal BPPV.
Trial Registration:
Clinical Trials Registry (CTRI/2019/10/021681).
Keywords: Positional vertigo, randomized controlled trial, vestibular
INTRODUCTION
Benign paroxysmal positional vertigo (BPPV) is one of the commonly occurring causes of vertigo. BPPV can be categorized into three types according to the involvement of semicircular canals in the inner ear: posterior, anterior, and lateral/horizontal canal BPPV. The posterior canal is the most commonly affected semicircular canal; thence posterior canal BPPV is the commonest among other types. Approximately 90% of the cases of BPPV are posterior canal BPPV (PC-BPPV).[1] Patient has short and severe episodes of vertigo that occur only when the patient changes his/her position.[2,3] Dix-Hallpike test (DH) is the diagnostic maneuver for assessing posterior canal BPPV, which aggravates vertigo and the up-beating torsional nystagmus toward the involved ear. This test involves turning the patient’s head to one side and then lying straight in the supine position with the neck extended at 20 degrees. If the patient complains of vertigo with a few seconds delay and there is nystagmus too, it indicates a positive test and the involvement of the side of the head turned in the initial position.[4,5,6,7] In patients with comorbid variables like cervical-related disorders, the side-lying test can also be used as an analytic tool for surveying BPPV.[8]
Many treatment methods are being used in clinical practice by medical as well as physiotherapy practitioners. Recent guidelines for BPPV also recommend repositioning as the best treatment option rather than medicines or rehabilitation, unless there is any medical reason for not giving the repositioning maneuvers.[9] Medical intervention can control the symptoms but cannot reposition the crystals in their original place.[10,11] Vestibular habituation and rehabilitation therapy are also effective.[12] In this interim, many repositioning maneuvers, like Semont[13] and Epley,[14] maneuver are surprisingly beneficial for the complete resolution of the condition with less recurrence. Epley repositioning maneuver (ERM) is one of the mostly applied and effective traditional maneuvers for the treatment of posterior canal BPPV. By performing these maneuvers in a step-wise positioning order, the dislodged otoconia move toward the utricle in a single shot. However, other treatments for BPPV have been developed to expand the variety of therapeutic methods accessible and boost success rates.[4] By far, no study has been conducted on the subject with such a large sample size. The goal of this study was to see how effective this new repositioning maneuver called, Gans repositioning maneuver (GRM),[15] is for treating PC-BPPV, which is a hybrid approach of Epley and Semont maneuvers. This maneuver does not include the attempt of a straight supine position with the neck in an extended position, which can be a difficult positioning movement for the elderly and patients with cervical spine disorders. This approach was developed considering the complications of the Epley maneuver in conditions like vertebrobasilar insufficiency, cervical degenerative changes, etc., and the Semont maneuver in neck and back mobility disorders.[3] Absence of vertigo, negative D-H test, and absence of recurrence on one-month follow-up were the important factors to determine the efficacy of the maneuver.
MATERIALS AND METHODS
Study design
This randomized controlled trial was conducted in a tertiary care teaching and research institute/hospital from March 2020 to March 2022. The study was approved by the Ethical committee of the institution with code Dean/2020/EC/2156 and registered in the Clinical Trial Registry of India (http://ctri.nic.in/Clinicaltrials/login.php) by the numberCTRI/2019/10/021681 on October 16, 2019.
Subjects
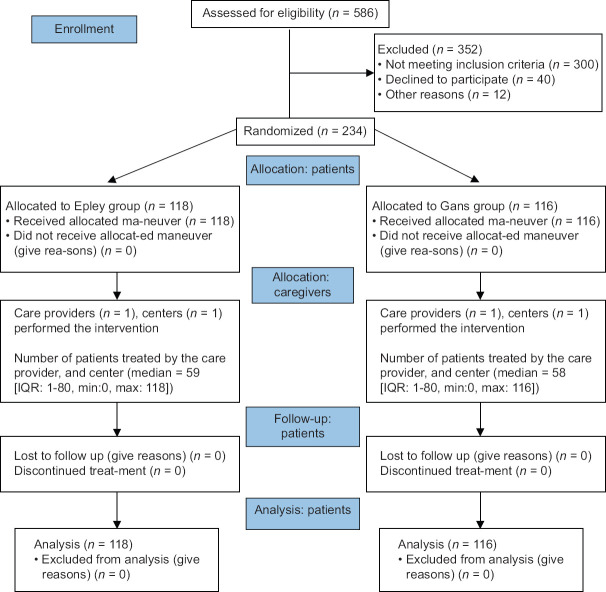
The Consort patient flow chart describes the assessment of eligibility in Figure 1. Two hundred and thirty-four subjects diagnosed with PC-BPPV were involved in the study according to the eligibility criteria age group above 18 years, diagnosed unilateral PC-BPPV confirmed by the presence of vertigo, and a positive DH test. The DH test was considered positive or negative as per the presence or absence of vertigo and visible nystagmus, respectively. Patients having normal central nervous system and Ear, Nose and Throat (ENT) examinations. Participants must be able to understand and follow spoken instructions. Patients taking medicines for dizziness, drowsiness, or lightheadedness, as well as anti-vertigo medications, were excluded.
Figure 1.
Consort patient flow chart
Twenty PC-BPPV patients were included in one pilot study to estimate the sample size. There were 10 participants in each group, and according to the results, the calculated sample size was 60 patients for one group. For the accuracy of the results and also taking the loss to follow-up into consideration, we included 234 participants: 118 in the Epley group and 116 in the Gans group. Groups were divided by the random allocation method. Patients in both groups were examined to be similar in various parameters like age, gender, and duration of symptoms for the accuracy of the results. All patients gave their informed permission.
Procedure
After initial assessment and getting informed consent, a blinded investigator used a computer to generate a basic randomization sequence that was placed in sealed, opaque, and sequentially numbered envelopes and then assigned individuals to one of two groups, making patients blind to the treatment procedure. Two separate therapists performed the assessment and repositioning for both groups individually. The data analysts and the intervention outcome assessors were blinded to the allocation of participants and treatment maneuvers. One group was treated with the Epley maneuver (Epley group) and the other with the Gans maneuver (Gans group) by individual physiotherapists, specialized in the Neurology division and had 2 years of experience in the same field. Maneuvers were repeated by the time the DH test became negative, which took a maximum of 2–3 repetitions. Treatment maneuvers explanation: ERM,[2,3,14]: Patient sitting on the couch with legs unfolded, turning the head 45 degrees to the involved side, lying on the bed in supine/straight position with turned and 20 degrees extended head, then turning 90 degrees to uninvolved side, turning completely to normal side with head to another 90 degrees on same side (face is downward now), and finally, sitting on the edge with head straight. The patient holds each position for 30 s to 1 min. [Figure 2] GRM:[14] [Figure 3] The patient sits on the edge of the bed, turns his head 45 degrees to the uninvolved side, lies down sideways on the involved side, and then totally rotates to the other side into the bed. Face down, he turns his head side to side two or three times, then sits up straight with his head straight. Post maneuver instructions were not given to the patients.
Figure 2.

The Epley maneuver for an imaginary individual of right-sided posterior canal BPPV. Positions starting from 1 to 4
Figure 3.

The Gans maneuver for an imaginary individual of right-sided posterior canal BPPV. Positions starting from 1 to 4
Post-treatment DH test and VAS assessments were performed, after 24 h (the next day) of application of the maneuver. Patients were told to inform the researchers immediately if they observe vertigo once they leave and taught vestibular rehabilitation exercises if did not respond to repositioning at all. Patients were left to go home and called for follow-up subjective assessment (presence/absence of vertigo, VAS, and DHI) after 1 month. Recurrence was also noted, which was characterized by the return of symptoms.
Outcome measures
Epley and Gans Maneuvers’ success was investigated by the resolution of vertigo and nystagmus on the D-H test and Visual Analog Scale (VAS) score. The presence and absence of vertigo were the two probable dichotomous outcomes asked by the patient himself. The VAS scale ranges from 0 to 10, with 0 indicating no subjective vertigo and 10 indicating severe vertigo with a cut-off score: Of 0–3 mild; 4–6 moderate; >7 severe. The VAS is a good way to gauge the severity of vertigo.[16] Nystagmus was analyzed visually and recorded as a video on mobile phone. Dix Hallpike Inventory questionnaire (DHI) was determined in recovered patients only pre- and one-month post-maneuver. The DHI is a 25-item scale with a 0 to 100 score that assesses the functional, emotional, and physical implications of dizziness and imbalance (cut-off: 16–34 = mild handicap; 36–52 = moderate handicap; 54+ = severe handicap).[17,18] There is no evidence of the side effects of these movements other than persistent vertigo. Nonetheless, on the next day, when the patient came for evaluation following the procedure, we monitored the adverse effects, if any.
Data analysis
The participants’ demographic features were obtained using means and standard deviations for descriptive data analysis. A two-tailed analysis with a 0.05 significance level and 95 percent confidence intervals was utilized in the study. The Chi-square test was applied to compare the categorical variables. The effect size was calculated using Statical evaluation (SPSS 22) with 0.05 as the P value for significance.
RESULTS
A total of 234 patients were enrolled for the study procedure: 118 in the Epley group and 116 in the Gans group. Epley group and Gans group age range from 21 to 84 with mean ± SD of 43.99 ± 12.68 and 48.43 ± 14.09 respectively. Epley group had 74 (62.7%) female and 44 (37.28%) male patients, while the Gans group had 68 (58.6%) female and 48 (41.37%) male patients [Table 1]. A total of 11 (4.70%) patients had mild, 107 (45.7%) had moderate, and 116 (49.57%) had severe handicap according to the VVAS categorization of vertigo intensity. A total of 59 (25.21%) patients had mild, 116 (49.57%) had moderate, and 59 (25.21%) had severe handicaps according to DHI subdivisions of vertigo intensity and its interference with daily activities. There was a similarity in both groups regarding age and gender. Only a few patients reported any history of trauma before the onset of vertigo. Patients in both groups were matched concerning onset, involved ear, and family history of vertigo.
Table 1.
Demographic data of BPPV patients
| Variable | Gans Group | Epley Group |
|---|---|---|
| Age (mean±SD) | 48.4±14.0 | 43.9±12.6 |
| Gender | ||
| Male | 48 (41.3%) | 44 (37.2%) |
| Female | 68 (58.6%) | 74 (62.7%) |
| Side of ear | ||
| Right | 65 (56.0%) | 60 (50.8%) |
| Left | 51 (43.9%) | 58 (49.1%) |
With this baseline data, we have found that the older age population is affected less than the young, and females are affected more than males. About the side of involvement, the right-side posterior canal BPPV is more common than the left side. Results of one-variable Chi-square tests revealed significant improvement (P < .0001) in maximum (95%) patients of both groups whether subjects were given GRM or the Epley maneuver [Table 2]. Also, objective improvement (DH test) was found in the Epley group (n = 97 out of 118, 82.20%) and the Gans group (n = 91 out of 116, 78.44%). The effect size (Cohen’s h) of both maneuvers was 0.094. Patients in both groups improved significantly with no dizziness on the VVAS scale (n = 97, 82.20%) in the Epley group and (n = 91, 78.44%) in the Gans group. From 21 patients with a positive DH test even after giving the maneuver in the Epley group, 52.38% had mild dizziness and 47.61% had severe dizziness. From 25 patients with positive DH test after giving maneuver in the Gans group, 52% had mild dizziness and 48% had severe dizziness.
Table 2.
Comparison between treatment groups:
| Variable | Maneuver | P-value | |
|---|---|---|---|
|
| |||
| EM (118) | GM (116) | ||
| Immediate Improvement (D-H test) N=234 | |||
| Present (negative) | 97 | 91 | |
| Absent (positive) | 21 | 25 | P=0.470 |
| P<0.0001 | P<0.0001 | ||
| 24 hours-Post maneuver VVAS (Mild/moderate/severe dizziness) N=234 | |||
| No dizziness | 97 | 91 | |
| Mild dizziness | 11 | 13 | P=0.769 |
| Severe dizziness | 10 | 12 | |
| P<0.0001 | P<0.0001 | ||
|
| |||
| Post-one-month Follow-up call-subjective assessment | EM (97) | GM (91) | |
|
| |||
| only for patients who improved at 24-hour assessment N=188 | |||
| No vertigo | 93/97 | 89/91 | P=0.452 |
| Recurred | 4/97 | 2/91 | |
| P<0.0001 | P<0.0001 | ||
|
| |||
| Post one-month Call-DHI assessment | |||
|
| |||
| only for patients who improved at 24-hour assessment N=188 | |||
| No handicap | 93/97 | 89/91 | |
| Mild handicap | 4/97 | 2/91 | P=0.442 |
| Severe handicap | 0/97 | 0/91 | |
| P<0.0001 | P<0.0001 | ||
No missing data
Post-one-month follow-up subjective assessment showed significant (P < 0.0001) sustained improvement in 93 (95.87%) subjects and recurrence in 4 (4.12%) subjects in the Epley group. Almost similar sustained improvement was noticed in 89 (97.80%) subjects and recurrence in 2 (2.19%) subjects in the Gans group. No adverse effect was noted in any patient from both group.
Post-24-hour subjective as well as objective assessment indicated insignificant differences in both groups with a P value of 0.470. Post one-month comparative assessment also determined insignificant (P = 0.452) differences in both groups.
DISCUSSION
This study compared the effectiveness of two repositioning treatment maneuvers, the Gans maneuver and the Epley maneuver, in resolving vertigo in PC-BPPV patients. We observed improvement in maximum patients of both groups statistically but no difference in both maneuvers concerning the superiority of one treatment maneuver over another. This proves that Gans, the new hybrid maneuver, is similar to the Epley maneuver, which is the established traditional maneuver, for the posterior canal BPPV treatment, with no adverse effects or complications. And this is especially beneficial for BPPV patients who have cervical-related illnesses such as stenosis, scoliosis, limited mobility, radiculopathy, postural dysfunction, osteoporosis, and spinal cord injuries, as they are unable to undertake activities like suddenly lying down on their back with neck hyperextension position, the starting component of the Epley treatment maneuver. The DHI and the VVAS are two measures that can assist to evaluate the disability and impairments caused by dizziness in a person’s everyday life. When used together, they can aid with patient management and therapy. Because there is no association between the two instruments due to a lack of study, using one instead of the other is not suggested. Because the VVAS is a more basic and subjective assessment than the DHI total score, it may give a lower score for determining the severity of vertigo. The Dizziness Handicap Inventory has 25 questions that cover the patient’s physical, emotional, and functional elements, allowing for a more thorough assessment of the dizziness, and answers to many of them depend upon individual personality. Moreover, VVAS is a parametric interval measurement while the DHI is an ordinal measurement. That’s why it is difficult to make associations about the severity of symptoms in both tests.
Six studies have been conducted on this hybrid approach till now. Richards A. Roberts et al.[15] and his team conducted a single group study to reveal the efficacy of GRM and found it as a useful treatment for PC-BPPV. Francesco Dispenza et al.[19] described the effectiveness of GRM as the most comfortable maneuver against Semont and Epley repositioning maneuvers. Badawy WM et al.[20] investigated the effect of the GRM with and without post-maneuver instructions and found no difference; they had a very small sample size. This indicates that GRM itself is an effective maneuver therapy, and there is no need for post-maneuver instructions to be given. Alia Saberi et al.[21] conducted the study to find out the difference between GRM and ERM in 73 patients with a 1-week follow-up. As they mentioned in their result that longer time follow-ups can be done in the future to examine the reversibility of symptoms or recurrence of vertigo, and in our study, we followed the patients after one month. Their sample size was also smaller. Abir Omara et al.[22] investigated the comparison between GRM and EM for postural stability and vertigo and found both equally effective. Last study is a systematic review, published recently also indicated the effectiveness of the Gans maneuver.[23] The results obtained from the study have great clinical significance in the field of medical research. Patients with vertigo can obtain instant relief without any supporting therapy after performing the technique, which will contribute not only scientific but also economic, social, and individual value to this endeavor. In addition, GRM is shown to be equal to the Epley maneuver in elderly and postural compromised BPPV patients with cervical-associated neck stiffness and discomfort or any other condition, so it might be used instead of the Epley maneuver as this includes neck extension and rotation. This will help raise awareness of this innovative BPPV treatment procedure among the general public and practitioners.
CONCLUSION
Through this study, we conclude that GRM is as easy, effective, and safe maneuver as the Epley maneuver for the treatment of patients with posterior canal BPPV. Considering the similarity of patients in both groups on age, gender, side of the involved ear, and duration, this treatment maneuver can be chosen.
Ethical approval
Clinical Trials Registration (CTRI/2019/10/021681) on October 16, 2019 and Institutional ethical committee approval of Institute of Medical Sciences, Banaras Hindu University, Varanasi-UP, India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Indian Council of Medical Research, New Delhi.
REFERENCES
- 1.Baloh RW, Honrubia V. Clinical Neurophysiology of the Vestibular System. Oxford: University Press; 2001. Benign positional vertigo; pp. 239–51. [Google Scholar]
- 2.Mandala M. Bedside examination of the vestibular and ocular motor system-Level 2: How to diagnose and treat BPPV. 3rd Congress of the European Academy of Neurology 2017; June 24-27 [Google Scholar]
- 3.Argaet EC, Bradshaw AP, Welgampola MS. Benign positional vertigo, its diagnosis, treatment, and mimics. Clin Neurophysiol Pract. 2019;4:97–111. doi: 10.1016/j.cnp.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vital V, Pillas G, Printza A, Vital I, Triaridis S, Konstantinidis I, et al. An alternative maneuver for posterior canal BPPV treatment. B-ENT. 2010;6:9–13. [PubMed] [Google Scholar]
- 5.Dix MR, Hallpike CS. Pathology, symptomatology, and diagnosis of certain disorders of the vestibular system. Proc R Soc Med. 1952;45:341–54. doi: 10.1177/003591575204500604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zainun Z, Zakaria MN, Sidex D, Ismail Z. Determination of sensitivity and specificity of Dix Hallpike test (DHT) in peripheral vestibular disordered subjects. Int Med J. 2013;20:1–2. [Google Scholar]
- 7.Schuknecht HF. Positional vertigo: Clinical and experimental observations. Trans Am Acad Opthalmol Otolaryngol. 1962;66:319–32. [PubMed] [Google Scholar]
- 8.Cohen HS. Side-Lying as an alternative to the Dix-Hallpike Test of the posterior canal. Otol Neurotol. 2004;25:130–4. doi: 10.1097/00129492-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, et al. Clinical practice guideline: Benign paroxysmal positional vertigo (update) executive summary. Otolaryngol Head Neck Surg. 2017;156:403–16. doi: 10.1177/0194599816689660. [DOI] [PubMed] [Google Scholar]
- 10.McClure JA, Willett JM. Lorazepam and diazepam in the treatment of benign paroxysmal vertigo. J Otolaryngol. 1980;9:472–7. [PubMed] [Google Scholar]
- 11.Yimtae K, Srirompotong S, Srirompotong S, Sae-seaw P. A randomized trial of the canalith repositioning procedure. Laryngoscope. 2003;113:828–32. doi: 10.1097/00005537-200305000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Banfield GK, Wood C, Knight J. Does vestibular habituation still have a place in the treatment of benign paroxysmal positional vertigo? J Laryngol Otol. 2000;114:501–5. doi: 10.1258/0022215001906237. [DOI] [PubMed] [Google Scholar]
- 13.Semont A, Freyss G, Vitte E. Curing the BPPV with a liberatory maneuver. Adv Otorhinolaryngol. 1988;42:290–3. doi: 10.1159/000416126. [DOI] [PubMed] [Google Scholar]
- 14.Epley JM. The canalith repositioning procedure: For treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107:399–404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 15.Roberts RA, Gans RE, Montaudo RL. Efficacy of a new treatment maneuver for posterior canal benign paroxysmal positional vertigo. J Am Acad Audiol. 2006;17:598–604. doi: 10.3766/jaaa.17.8.6. [DOI] [PubMed] [Google Scholar]
- 16.Dannenbaum E, Chilingaryan G, Fung J. Visual vertigo analogue scale: An assessment questionnaire for visual vertigo. J Vestib Res. 2011;21:153–9. doi: 10.3233/VES-2011-0412. [DOI] [PubMed] [Google Scholar]
- 17.Jacobson GP, Newman CW. The development of the dizziness handicap inventory. Arch Otolaryngol Head Neck Surg. 1990;116:424–7. doi: 10.1001/archotol.1990.01870040046011. [DOI] [PubMed] [Google Scholar]
- 18.Yorke A, Ward I, Vora S, Combs S, Johnson TK. Measurement characteristics and clinical utility of the dizziness handicap inventory among individuals with vestibular disorders. Arch Phys Med Rehabil. 2013;94:2313–4. [Google Scholar]
- 19.Dispenza F, Kulamarva G, Stefano AD. Comparison of repositioning maneuvers for benign paroxysmal positional vertigo of posterior semicircular canal: Advantages of hybrid maneuver. Am J Otolaryngol. 2012;33:528–32. doi: 10.1016/j.amjoto.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 20.Badawy WM, Gad El-Mawla EK, Chedid AE, Mustafa AH. Effect of a hybrid maneuver in treating posterior canal benign paroxysmal positional vertigo. J Am Acad Audiol. 2015;26:138–44. doi: 10.3766/jaaa.26.2.4. [DOI] [PubMed] [Google Scholar]
- 21.Saberi A, Nemati S, Sabnan S, Mollahoseini F, Kazemnejad E. A safe-repositioning maneuver for the management of benign paroxysmal positional vertigo: Gans vs. Epley maneuver;a randomized comparative clinical trial. Eur Arch Otorhinolaryngol. 2017;274:2973–9. doi: 10.1007/s00405-016-4235-7. [DOI] [PubMed] [Google Scholar]
- 22.Omara A, Mosaad DM, Mohamed AS, Raoof NAE. Epley repositioning maneuver versus Gans repositioning maneuver on postural instability in elderly patients with benign paroxysmal positional vertigo. Egypt J Otolaryngol. 2017;33:518–22. [Google Scholar]
- 23.Joshi D, Gyanpuri V, Pathak A, Chaurasia RN, Mishra VN, Kumar A, et al. Gans repositioning maneuver for the posterior canal BPPV patients: Systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2022;279:4241–6. doi: 10.1007/s00405-022-07396-6. [DOI] [PubMed] [Google Scholar]