Abstract
PURPOSE
Despite the disproportionately high risk of breast cancer among women of African heritage, little is known about the facilitators and barriers to implementing germline genetic testing and counseling (GT/C).
METHODS
This scoping review followed guidelines recommended by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews. Published manuscripts from database inception through 2021 were sourced from PubMed, Cumulative Index to Nursing and Allied Health Literature via EBSCO, Embase, Cochrane Library, and Scopus. Search terms were used to retrieve articles addressing (1) African heritage, (2) breast cancer, and (3) GT or GC. The screening involved abstract and title review and full-text review. Data were extracted for all articles meeting the inclusion criteria.
RESULTS
A total of 154 studies were included. Most studies that took place were conducted in the United States (71.4%), and most first authors (76.9%) were from the United States. GT was conducted in 73 (49.7%) studies. BRCA1/BRCA2 were the most commonly studied genes for germline mutations. GC was conducted in 49 studies (33.3%), and perspectives on GC were evaluated in 43 (29.3%). The use of racial/ethnic categories varied broadly, although African American was most common (40.1%). Racism was mentioned in three studies (2.0%).
CONCLUSION
There is a growing body of literature on GT/C for breast cancer in women of African heritage. Future studies on GT/C of African populations should consider increased clarity around racial/ethnic categorizations, continued community engagement, and intentional processes for informed consent.
A scoping review on germline genetic testing for breast cancer among women of African heritage identifies a growing body of literature and key bioethical considerations for genetic testing/counseling.
INTRODUCTION
Breast cancer mortality rates in the United States have decreased since 1989.1 However, these reductions in mortality are not appreciated across patient groups equally. Black women have death rates that are 40% higher than White women and have the lowest 5-year survival of any racial/ethnic group across tumor subtype, hormone receptor status, and disease stage.1
Poor outcomes in patients who are racialized as Black are seen across geographies. Breast cancer is the second leading cancer among women of African heritage,2 and breast cancer–associated mortality ranks the highest in the world, with a disproportionately low 5-year survival of 66% in contrast to high-income countries where survival approaches 90%.3,4 Country-specific survival estimates are as low as 12% in Uganda and neighboring countries.5
One area of research that seeks to explain these disparities is through the lens of genetics. Genetic testing (GT) is part of standard of care, but uptake has been relatively low.6 Some studies have reported genetic differences among racial/ethnic groups that may be partially attributable to population-level disparities. For example, women of African heritage are more likely to present with triple-negative breast tumors (TNBC), which are less responsive to standard treatment.7,8 Geographic subsets of TNBC prevalence have been reported at higher frequencies in West African regions than in African American or White American populations.9 Yet, studies have also noted that patients of African heritage are often not included in genetic studies.10-13
Globally, there is limited literature on genetic testing and counseling (GT/C) that considers how racial groups are constructed in different time periods and geographies. Furthermore, racism and its impacts on inclusion and access to GT/C at a global scale are underexplored. GT/C has been used as a standard model in high-income countries,14 and is suggested to increase cancer-related knowledge, perceived personal control, and risk perception accuracy, and decrease cancer-related anxiety and decisional conflict among patients.15 Further, GT can affect surgical planning and play an essential role in the treatment course.16-18 In TNBC, deleterious mutations have been reported at higher rates, and GT/C for BRCA1 and BRCA2 has been recommended regardless of age or family history.19
Despite the disproportionate disease burden and potential benefits for improving screening and treatment, GT/C does not appear to be widely incorporated into breast cancer care for women of African heritage. GT must be delivered with rigorous consideration of sociocultural, economic, and ethical contexts,20-22 and guidelines for GT/C implementation in populations of African heritage have yet to be standardized. The purpose of this scoping review23 was to evaluate the literature on germline GT/C for breast cancer in women of African heritage. We aimed to assess previous germline breast cancer GT/C applications, identify barriers and facilitators for implementation, and identify gaps in the present literature.
METHODS
This scoping review was conducted with the guidelines recommended by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for a scoping review.24
A trained clinical health sciences librarian (S.T.W.) performed our comprehensive electronic search of publications using the following databases: PubMed, Cumulative Index to Nursing and Allied Health Literature via EBSCO, Embase, Cochrane Library, and Scopus. Our search was not restricted by language. All results were collected from the database's inception through July 4, 2021. Search terms were used to retrieve articles addressing the three main concepts of the search strategy: (1) African heritage, (2) breast cancer, and (3) GT or genetic counseling (GC; Appendix 1). The search strategy was conducted in PubMed using keyword and MeSH combinations. Other database search strategies included text word searching and database-specific thesaurus terms, if available. Results were downloaded to EndNote, and duplicates were removed. All references were uploaded to Covidence Systematic Review software (Covidence, Melbourne, Australia), a web-based tool designed to track each step of the abstraction and review process.
To evaluate germline GT/C in women of African descent, the decision was made to broadly include racial/ethnic categories that could consist of individuals of African heritage and relate to the overlapping but distinct exposures of inheritance and global anti-Black racism. Studies with African American, Black, or Black American participants were included. Of note, the term sub-Saharan Africa was used throughout the search process. Still, the authors have moved away from this terminology for a more accurate and equitable representation of the study focus.25,26 The authors also use the term heritage to acknowledge the broad scope of genetic, sociocultural, and historical contexts that are passed down to individuals and holistically capture how communities may choose to define themselves. The term ancestry was generally avoided as identifying biological correlates of race was not the primary goal of this study.
Inclusion criteria were studies published before July 4, 2021; involving GT/C of human participants for breast cancer; including participants of African heritage by ancestry informative markers or self-report; and quantitative, qualitative, or mixed-methods studies. Exclusion criteria were incorrect study type, focus, intervention, population, cancer type, or article type (eg, commentaries). All articles were screened by title and abstract by two reviewers (Y.I., K.T., J.S.M., or S.N.C.E.). A third reviewer resolved conflicts (J.S.M. or S.N.C.E.). Selected articles underwent full-text review, where inclusion was determined based on the manuscript's contents. Two independent reviewers conducted this step (Y.I., K.T., J.S.M., or S.N.C.E.), with a third reviewer for conflict resolution (J.S.M. or S.N.C.E.).
Data extraction was conducted in an online form (Appendix 2) developed by the research team (Qualtrics XM, Provo, UT). A single reviewer extracted each article, and a second reviewer was consulted as needed. After data extraction, thematic content analysis was conducted. One reviewer (Y.I.) completed a line-by-line analysis and assigned preliminary themes. These themes were assessed by a second reviewer (S.N.C.E.), and conflicts were resolved through discussion.
Reflexivity was addressed throughout the analysis by including a diverse research team.27 The authors involved were cognizant of their own experiences with GT/C, racism, and cancer care. The team was composed of individuals who self-identified as Black/African American, Asian, and White.
Ethics Approval Statement
This is a literature review and did not require ethics approval.
RESULTS
Study Location and Authorship
The initial search yielded 2,890 articles. The distribution of articles per database is summarized in Figure 1. There were 1,820 articles remaining after duplicates were removed. After title and abstract screening, 503 articles were eligible for full-text review. A total of 154 studies met the inclusion criteria and were ultimately included.
FIG 1.
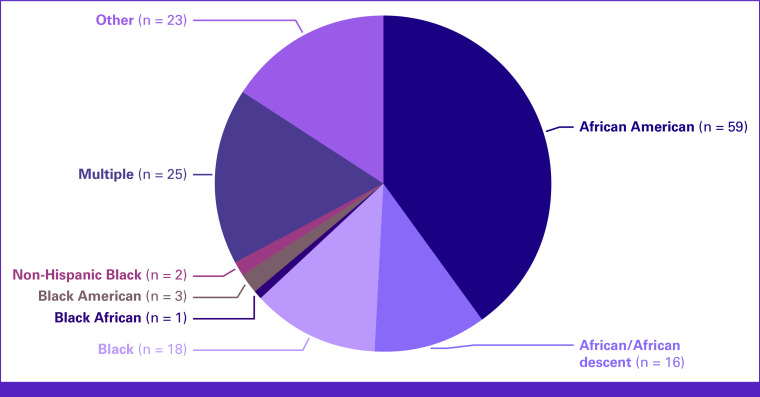
Map of countries included in scoping review. Geographic representation of studies on germline genetic testing/counseling for breast cancer.
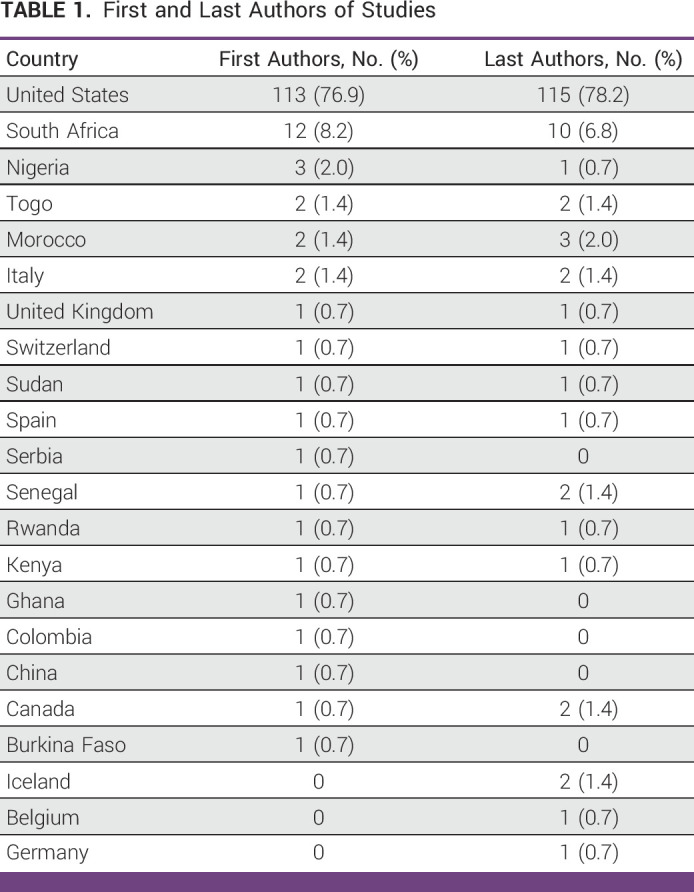
The countries where the studies took place are represented in Figure 2. Most studies were conducted in the United States (71.4%), followed by South Africa (8.4%), Nigeria (5.2%), Rwanda (1.9%), Sudan (1.9%), Ghana (1.3%), Kenya (1.3%), Senegal (1.3%), and Togo (1.3%). Five studies were conducted in multiple countries. The geographic spread of the first and last authors is summarized in Table 1, with most first authors (76.9%) and last authors (78.2%) being from the United States
FIG 2.
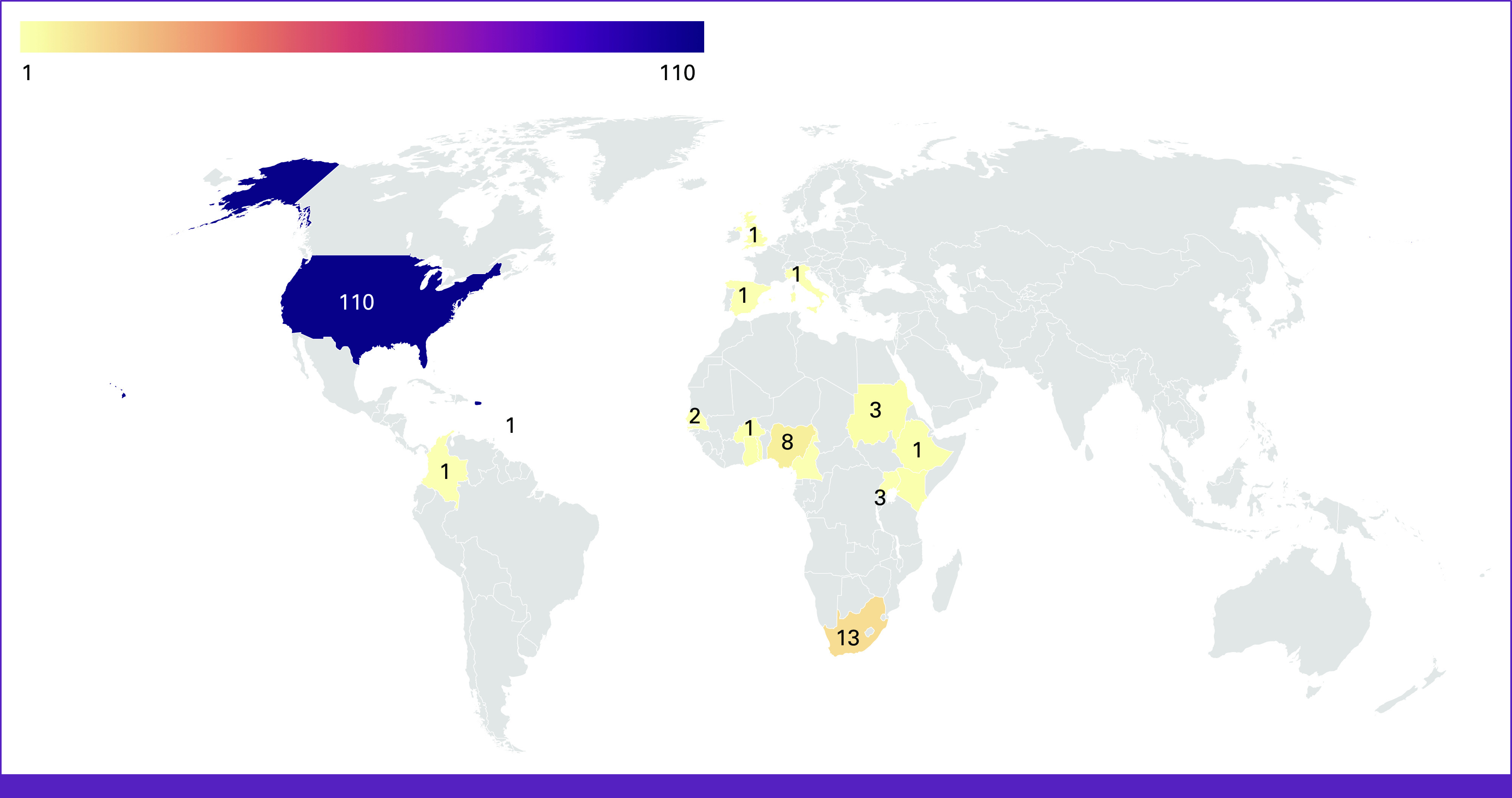
Pie chart of racial categories used by included studies.
TABLE 1.
First and Last Authors of Studies
Study Design, Data Sources, and Informed Consent
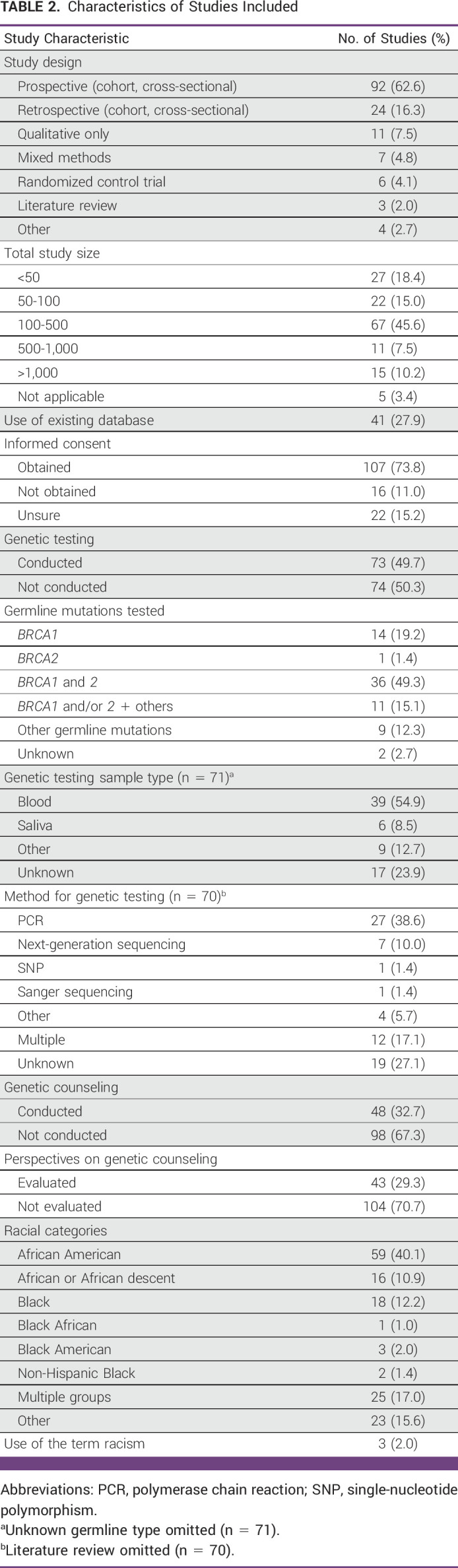
The characteristics of the studies that were included are summarized in Table 2. Most studies (65.3%) were prospective, including cohort and cross-sectional studies. Total population sizes varied, with approximately half of the studies (45.6%) having 100-500 participants. There were 41 studies (27.9%) that used an existing database, including state cancer registries or the SEER Program. Informed consent was obtained in 73.8% of studies and not obtained in 11.0%. There were 22 (15.3%) studies where informed consent status was unclear.
TABLE 2.
Characteristics of Studies Included
GT: Target Genes, Methods, and Variants of Uncertain Significance
Seventy-three (49.7%) studies conducted GT (Table 2). BRCA1 and BRCA2 were tested in 49.3% of studies, followed by studies that only tested BRCA1 mutations (19.2%) and for BRCA1 and/or BRCA2 mutations with other germline mutations (15.1%). Non-BRCA germline mutations were assessed in 12.3% of studies, including TP53,28-30 ATM,31 CHEK2,32 PALB2,33-35 and DARC/ACKR1.9 GT was done using peripheral blood most commonly (54.9%) and saliva (8.5%). GT was conducted using polymerase chain reaction (38.6%), next-generation sequencing (10.0%), single-nucleotide polymorphism (1.4%), and Sanger sequencing (1.4%). Many studies reported on variants of uncertain significance (VUS).28,30,33-61
Most studies (60.3%) that reported on GT were conducted in the United States. Ten (13.7%) GT studies were conducted in South Africa, three (4.1%) were conducted in Nigeria and Rwanda, and less than two studies were conducted in other non-US countries including Sudan and Cameroon. Non-US studies had relatively smaller sample sizes (studies with <100 subjects seen in 48.3% of non-US studies v 31.2% of US studies). Three non-US studies focused on participants at high risk of breast cancer (eg, patients with Li Fraumeni syndrome).29,45,58 Non-US studies varied in their recommendations for GT, with several recommending GT for breast cancer screening because of higher rates and/or risk of germline mutations,40,45,56,62,63 and others explicitly arguing against GT because of lower prevalence and/or risk of germline mutations related to breast cancer.28,30,32,64,65
Genetic Counseling
GC was conducted in 48 studies (32.7%), and perspectives on GC were evaluated in 43 (29.3%; Table 2). The majority (95.8%) of these studies were conducted in the United States, with two non-US studies from Kenya and South Africa.41,66 Of the studies that assessed perspectives on GC, 37.2% used surveys, 28.0% used individual interviews, 18.6% used multiple assessment methods, and 9.3% used focus groups.
Three studies assessed factors associated with the likelihood of receiving GT/C,67-69 and one explored eligibility for GT/C.70 Several studies reported rates of GT/C were lower among Black/African American women compared with White women, with rates of GT/C as low as 16 times less likely in Black women.42,44,45,71 Notably, three studies reported no differences in GT/C receipt by race.72-74 Several studies evaluated acceptance or satisfaction of BRCA testing; GT/C participation and recruitment was generally high (60%-80%) with rates >80% for participant satisfaction with their decision to undergo GT/C.75-79 Multiple studies explored other elements of GT/C, such as negative emotional reactions and rates of depression.74,80-84 Study findings varied from no baseline differences in GT/C-related distress to higher rates among women of African heritage.
Six studies implemented strategies for improving GT/C rates, including culturally competent genetic counselors and community-based GC practices.85-90 Knowledge around GT/C was assessed,68,76,91-93 with some studies reporting lower GT/C knowledge among Black or African American participants compared with White participants.68,91 Sociocultural beliefs were explored by multiple research groups, including medical mistrust.81,94-96
Definitions of Race, Ethnicity, and Racism
The use of racial/ethnic categories varied. The breakdown of the racial categories is visualized in Figure 2. The most common racial category was African American (40.1%). Other categories included African or African descent (10.9%), Black (12.2%), and Black American (2.0%). Multiple groups were used to describe individuals of African ancestry in 17.0% of studies, and 15.6% used other racial/ethnic groups (eg, Black African, Black British, and Black Caribbean97). Racial/ethnic categories were clearly defined in 15 studies (10.2%). For example, Friebel et al98 indicated participants were inferred to have African ancestry based on self-report or inference based on place of birth or residence. Some studies included single racial/ethnic groups but clearly stated these categories, for example, “Our sample consisted of 63 individuals from a single African American (Creole) kindred.”99 Approximately 75% of studies had no definition of race/ethnicity in their research methods.
The word “racism” was included in three studies (2.0%) conducted in 2006, 2008, and 2020.76,100,101 No other studies included the term racism in any part of their manuscript. Kinney et al76 assessed perspectives of racism in general and in the health care setting using a validated Perceptions of Prejudice scale. Edwards et al100 included the potential role of racism in introducing and discussing their study on attitudes toward BRCA1/2 testing among women of African heritage. Peterson et al101 contextualized their findings of hereditary breast cancer assessment disparities by discussing institutional racism and the historical context of the US Public Health Service Syphilis Study at Tuskegee.
DISCUSSION
In this study, we sought to explore germline GT/C for breast cancer in women of African heritage. Studies were heterogeneous in size, geographic spread, study goals, and findings. Key themes from this scoping review may serve further research and help shape how we consider the intersections of race, heritage, genetics, and the overarching frame of systemic racism in germline GT/C.
Although disparities in outcomes or access were a focus of many studies, reported findings ranged from no racial/ethnic differences74 in GT receipt to up to 16-fold differences between populations of African heritage versus White populations.42,44,45 Similarly, GT/C recommendations ranged from testing according to patient autonomy (even against physician recommendations)102 to GT in all young Black women.103 GT/C disparities varied across studies, likely because of differences in study size, location, sociocultural differences in African or African American subgroups, and differences in chosen comparators. Populations of African heritage were the primary focus of this study, but most studies were physically conducted in the United States
We also identified a high volume of studies that reported VUS among populations of African heritage. As suggested by some studies, these findings are likely a result of less-accessible GT data in specific populations.104 This may be due to limited GT/C access and the sociocultural and historical contexts of GT/C rather than lack of interest as demonstrated by the high rates of GT/C acceptance, adherence, and satisfaction reported among African and African American populations.75-79
Few studies (25%) provided definitions of race/ethnicity, and there was broad heterogeneity in the categories used to describe groups. These findings are consistent with bioethics scholarship, which report unclear racial/ethnic categorizations across genetics literature and concern for insufficient rigor because of inconsistencies.105-107
Furthermore, US studies often compared White versus African American populations without clear rationale for their limited comparison groups.42,52,74,91,101,102,108 Non-US studies were under-represented in this review; however, some non-US studies included broader racial categories.9,55 Given the general under-representation of individuals of African heritage in genetic and cancer registries, the genes that are tested in these studies may not be capturing the appropriate genes for the specific populations of interest.109 More robust inclusion of individuals of African heritage is essential for understanding which genes to test and develop study designs with purposeful comparisons.
Within genetics literature, some researchers argue for the continued use of historic racial/ethnic categories because they are thought to provide crude but meaningful information about disease states.11,12,106 Others have embraced race as a social construct, given the greater genetic diversity observed within groups than between them and the mutability of racial categorizations across time and place.105,110,111 Some genetics research has transitioned from typological categories to terms like ancestral group and geographic population. Still, the arbitrary categories continue to risk perpetuating racist typological notions.112
Empirical studies on racial/ethnic categories and their impact on clinical outcomes are sparse. Yet, small-scale analyses of genetics researchers reveal an absence of systematic mechanisms for racial grouping and instead reliance on typological beliefs that are scientifically unexamined implying tenuous scientific merit.105 Despite including contemporary studies, our findings show ongoing inconsistencies in racial groupings. Determining which categories were most clinically valuable was outside this study's scope; however, our findings underscore the importance of clearly defining racial/ethnic categories and documenting the intent for which they are meant to serve.
Genetics research is fraught with historic and present racism, yet only three studies explicitly discussed racism.11,113 Racial disparities were a common focus, and the dearth of explicit mentioning of, or grappling with, the context in which GT/C research takes place is another concern for ethicality and intent behind large-scale germline testing. Further reckoning with racism is warranted to develop a meaningfully race-conscious approach to GT/C.
Another theme that emerged was the investigator's relation to the local community. There were several studies where first or last author affiliations differed from the patient population or the study's geographic region. This is consistent with studies that report high rates of genetics research about African-descendant populations coming from Europe and the United States and the risks of authorship parasitism.114-116 Community engagement is a critical investment for conducting ethical research and improving patient outcomes.117,118 Involvement of the local community and key stakeholders is even more pressing when the research focuses on ethnic minorities or a global context where resource accessibility varies by geography.119,120
For studies where the investigator's affiliation differed from the country where the research was conducted, it was often unclear how the local community was involved; this was also true for studies conducted within the United States. These discrepancies may be partially addressed by standardized inclusion of the local community by institutional review boards and upholding rigorous publication criteria by academic outlets.27
Despite the high volume of research conducted outside the researcher's institution, the role of informed consent was difficult to discern in nearly 15% of studies. Such studies would benefit from clarifying consent processes, and publication outlets may benefit from ensuring sufficient verbiage to uphold appropriate ethical standards.
Contrary to our expectations, few studies discussed the role of data ownership in GT/C research. Disclosure of personal data regarding GT/C results was explored by one study,121 but larger-scale studies on data privacy, storage, and usage were sparse. Further studies are warranted to understand the ethics of GT/C data ownership, security, privacy, and patients' perspectives regarding these issues.
The scoping review was selected as a review strategy because of the unknown quantity and quality of literature on GT/C in women of African heritage.23 Quality assessment was not conducted because of heterogeneity of article types. This study was primarily conducted at a US academic center. Although the focus was on individuals of African heritage and members of the team were affiliated with a hospital in Malawi, the review methodology may be biased toward high-income countries. We attempted to address this by including all languages; however, no non-English studies were ultimately included.
In conclusion, in this scoping review of GT/C for breast cancer in women of African heritage, we identified a growing body of literature that was conducted predominantly in the United States by researchers in the United States Approximately half of the studies carried out GT, most commonly of BRCA1 and BRCA2, while one third conducted GC. Racial categories varied broadly, with insufficient definitions in most studies. Future research on GT/C for African heritage populations should consider increased clarity around racial/ethnic categorizations, more robust local community engagement, and intentional processes for informed consent and data ownership.
APPENDIX 1. DATABASE SEARCH STRATEGIES
PubMed
Searched February 7, 2021
1,056 results
("African descent" OR "African ancestry" OR "African Europeans*" OR "African Asians*" OR "African Americans*" OR "African migrants" OR "Southern African Development Community" OR "SADC" OR "African Caribbeans*" OR african continental ancestry group[mesh] OR “African continental ancestry” OR "Africa South of the Sahara"[Mesh] OR sub-sahara* OR subsahara* OR Angola OR Luanda OR Luanda OR Benin OR Porto-Novo OR Botswana OR Gaborone OR Burkina Faso OR Ouagadougou OR Burundi OR Gitega OR Cameroon OR Yaounde OR "Central African Republic" OR Bangui OR Chad OR N'Djamena OR Comoros OR Moroni OR "Democratic Republic of the Congo" OR Kinshasa OR "Republic of the Congo" OR Brazzaville OR "Cote d'Ivoire" OR Yamoussoukro OR Djibouti OR "Equatorial Guinea" OR Malabo OR Eritrea OR Asmara OR Eswatini OR Mbabane OR Ethiopia OR "Addis Ababa" OR Gabon OR Libreville OR Gambia OR Banjul OR Ghana OR Accra OR Guinea OR Conakry OR Guinea-Bissau OR Bissau OR Kenya OR Nairobi OR Lesotho OR Maseru OR Liberia OR Monrovia OR Madagascar OR Antananarivo OR Malawi OR Lilongwe OR Mali OR Bamako OR Mauritania OR Nouakchott OR Mauritius OR Port Louis OR Mozambique OR Maputo OR Namibia OR Windhoek OR Niger OR Niamey OR Nigeria OR Abuja OR Rwanda OR Kigali OR "Sao Tome and Principe" OR "Sao Tome" OR Senegal OR Dakar OR Seychelles OR "Sierra Leone" OR Freetown OR Somalia OR Mogadishu OR "South Africa" OR Pretoria OR South Sudan OR Juba OR Sudan OR Khartoum OR Tanzania OR Dodoma OR Togo OR Lomé OR Uganda OR Kampala OR Zambia OR Lusaka OR Zimbabwe OR Harare OR "west-africa*" OR "west africa*" OR "south african*" OR "east-africa*" OR "east africa*") AND (Breast Neoplasms[mesh] OR “breast neoplasm*” OR “breast cancer*” OR “breast neoplasm*” OR “cancer of the breast” OR “neoplasm of the breast” OR “neoplasms of the breast” OR “ductal breast carcinoma*” OR “mammary cancer*” OR “mammary neoplasm*” OR “breast malignant neoplasm*” OR “breast malignant tumor*” OR “breast malignant tumour*” OR “breast tumor*” OR “breast tumour*”) AND (((germline AND (breast[tiab] OR brca[tiab])) OR breast neoplasms/genetics[mesh] OR brca*[tiab] OR brca1 protein/genetics[mesh] OR brca2 protein/genetics[mesh] OR genes, brca1[mesh] OR genes, brca2[mesh]) OR brca1 protein, human[mesh] OR brca2 protein, human[mesh] OR Carcinoma, Ductal, Breast / genetics* OR Germ-Line Mutation[mesh] OR “germline mutation*” OR “germ-line mutation*” OR genes, p53[mesh] OR “p53 gene*” OR "TP53TG1 protein, human" [Supplementary Concept] OR "Tumor Suppressor Protein p53"[Mesh] OR "TP53 protein, human" [Supplementary Concept] OR "TP53TG5 protein, human" [Supplementary Concept] OR tp53[tiab] OR tp53tg1[tiab] OR tp53tg5[tiab] OR “TP53TG1 protein, human" [Supplementary Concept] OR "Tumor Suppressor Protein p53"[Mesh] OR "TP53 protein, human" [Supplementary Concept] OR "TP53TG5 protein, human" [Supplementary Concept] OR "TP53TG1 protein, human" [Supplementary Concept] OR "Tumor Suppressor Protein p53"[Mesh] OR "TP53 protein, human" [Supplementary Concept] OR "TP53TG5 protein, human" [Supplementary Concept] OR Tumor Suppressor p53-Binding Protein 1[mesh] OR "Rad52 DNA Repair and Recombination Protein"[Mesh] OR rad52[tiab] OR "Mutation"[Mesh] OR "Sequence Analysis, DNA"[Mesh] OR “dna sequence analysis” OR "Nanopore Sequencing"[Mesh] OR “nanopore sequenc*” OR
"High-Throughput Nucleotide Sequencing"[Mesh] OR “nucleotide sequenc*” OR "Sequence Analysis, DNA"[Mesh] OR “sequence analysis” OR "Nanopore Sequencing"[Mesh] OR “nanopore sequenc*” OR "High-Throughput Nucleotide Sequencing"[Mesh] OR “Nucleotide sequen*” OR "DNA Repair-Deficiency Disorders"[Mesh] OR “dna repair” OR "Li-Fraumeni Syndrome"[Mesh] OR “li-fraumeni” OR DNA, Neoplasm / genetics[mesh] OR DNA Mismatch Repair / genetics[mesh] OR CHEK2 protein, human[mesh] OR Chek2[tiab] OR
"Genetic Testing"[Mesh] OR “genetic test*” OR "Genetic Carrier Screening"[Mesh] OR “genetic carrier screen*” OR “genetic screen*” OR "Genetic Services"[Mesh] OR “Genetic service*” OR "Genetics, Medical"[Mesh] OR Genetic Variation[mesh] OR “Genetic variation*” OR Genetic Predisposition to Disease[mesh] OR “genetic predisposition to disease” OR DNA Mismatch Repair/genetics[mesh] OR “dna mismatch repair” OR Ethnic Groups / genetics[mesh])
Scopus
Searched April 7, 2021
648 results
TITLE-ABS-KEY (brca OR brca1 OR brca2 OR "germline mutation*" OR "germ-line mutation*" OR TP53TG1 OR TP53 OR TP53TG5 OR p53 OR "rad52" OR "gene mutat*" OR "nucleotide sequenc*" OR "dna sequence analysis" OR "nanopore sequenc*" OR "Nucleotide sequen*" OR "dna repair" OR "li-fraumeni" OR "neoplasm dna" OR "Chek2" OR "genetic test*" OR "genetic carrier screen*" OR "genetic screen*" OR "Genetic service*" OR "medical genetics" OR "Genetic variation*" OR "genetic predisposition to disease" OR "dna mismatch repair") AND ("African descent" OR "African ancestry" OR "African Europeans*" OR "African Asians*" OR "African Americans*" OR "African migrants" OR "Southern African Development Community" OR "SADC" OR "African Caribbeans*" OR "African continental ancestry" OR "Africa South of the Sahara" OR "sub-sahara*" OR "subsahara*" OR "Angola" OR "Luanda" OR "Luanda" OR "Benin" OR "Porto-Novo" OR "Botswana" OR "Gaborone" OR "Burkina Faso" OR "Ouagadougou" OR "Burundi" OR "Gitega" OR "Cameroon" OR "Yaounde" OR "Central African Republic" OR "Bangui" OR "Chad" OR "N'Djamena" OR "Comoros" OR "Moroni" OR "Democratic Republic of the Congo" OR "Kinshasa" OR "Republic of the Congo" OR "Brazzaville" OR "Cote d'Ivoire" OR "Yamoussoukro" OR "Djibouti" OR "Equatorial Guinea" OR "Malabo" OR "Eritrea" OR "Asmara" OR "Eswatini" OR "Mbabane" OR "Ethiopia" OR "Addis Ababa" OR "Gabon" OR "Libreville" OR "Gambia" OR "Banjul" OR "Ghana" OR "Accra" OR "Guinea" OR "Conakry" OR "Guinea-Bissau" OR "Bissau" OR "Kenya" OR "Nairobi" OR "Lesotho" OR "Maseru" OR "Liberia" OR "Monrovia" OR "Madagascar" OR "Antananarivo" OR "Malawi" OR "Lilongwe" OR "Mali" OR "Bamako" OR "Mauritania" OR "Nouakchott" OR "Mauritius" OR "Port Louis" OR "Mozambique" OR "Maputo" OR "Namibia" OR "Windhoek" OR "Niger" OR "Niamey" OR "Nigeria" OR "Abuja" OR "Rwanda" OR "Kigali" OR "Sao Tome and Principe" OR "Sao Tome" OR "Senegal" OR "Dakar" OR "Seychelles" OR "Sierra Leone" OR "Freetown" OR "Somalia" OR "Mogadishu" OR "South Africa" OR "Pretoria" OR "South Sudan" OR "Juba" OR "Sudan" OR "Khartoum" OR "Tanzania" OR "Dodoma" OR "Togo" OR "Lomé" OR "Uganda" OR "Kampala" OR "Zambia" OR "Lusaka" OR "Zimbabwe" OR "Harare" OR "west-africa*" OR "west africa*" OR
"south african*" OR "east-africa*" OR "east africa*") AND ("breast neoplasm*" OR "breast cancer*" OR "breast neoplasm*" OR "cancer of the breast" OR "neoplasm of the breast" OR "neoplasms of the breast" OR "ductal breast carcinoma*" OR "mammary cancer*" OR "mammary neoplasm*" OR "breast malignant neoplasm*" OR "breast malignant tumor*" OR "breast malignant tumour*" OR "breast tumor*" OR "breast tumour*")
CINAHL
Searched April 7, 2021
137 results
((MH "Africa, Southern+") OR (MH "Africa, Western+") OR (MH "Africa South of the Sahara+") OR (MH "Africa, Eastern") OR (MH "Africa, Central+") OR ("African descent" OR "African ancestry" OR "African Europeans*" OR "African Asians*" OR "African Americans*" OR "African migrants" OR "Southern African Development Community" OR "SADC" OR "African Caribbeans*" OR african continental ancestry group[mesh] OR “African continental ancestry” OR "Africa South of the Sahara"[Mesh] OR sub-sahara* OR subsahara* OR Angola OR Luanda OR Luanda OR Benin OR Porto-Novo OR Botswana OR Gaborone OR Burkina Faso OR Ouagadougou OR Burundi OR Gitega OR Cameroon OR Yaounde OR "Central African Republic" OR Bangui OR Chad OR N'Djamena OR Comoros OR Moroni OR "Democratic Republic of the Congo" OR Kinshasa OR "Republic of the Congo" OR Brazzaville OR "Cote d'Ivoire" OR Yamoussoukro OR Djibouti OR "Equatorial Guinea" OR Malabo OR Eritrea OR Asmara OR Eswatini OR Mbabane OR Ethiopia OR "Addis Ababa" OR Gabon OR Libreville OR Gambia OR Banjul OR Ghana OR Accra OR Guinea OR Conakry OR Guinea- Bissau OR Bissau OR Kenya OR Nairobi OR Lesotho OR Maseru OR Liberia OR Monrovia OR Madagascar OR Antananarivo OR Malawi OR Lilongwe OR Mali OR Bamako OR Mauritania OR Nouakchott OR Mauritius OR Port Louis OR Mozambique OR Maputo OR Namibia OR Windhoek OR Niger OR Niamey OR Nigeria OR Abuja OR Rwanda OR Kigali OR "Sao Tome and Principe" OR "Sao Tome" OR Senegal OR Dakar OR Seychelles OR "Sierra Leone" OR Freetown OR Somalia OR Mogadishu OR "South Africa" OR Pretoria OR South Sudan OR Juba OR Sudan OR Khartoum OR Tanzania OR Dodoma OR Togo OR Lomé OR Uganda OR Kampala OR Zambia OR Lusaka OR Zimbabwe OR Harare OR "west-africa*" OR "west africa*" OR "south african*" OR "east-africa*" OR "east africa*") AND (brca OR brca1 OR brca2 OR "germline mutation*" OR "germ-line mutation*" OR TP53TG1 OR TP53 OR TP53TG5 OR p53 OR "rad52" OR "gene mutat*" OR "nucleotide sequenc*" OR "dna sequence analysis" OR "nanopore sequenc*" OR "Nucleotide sequen*" OR "dna repair" OR "li-fraumeni" OR "neoplasm dna" OR "Chek2" OR "genetic test*" OR "genetic carrier screen*" OR "genetic screen*" OR "Genetic service*" OR "medical genetics" OR genetic* OR "Genetic variation*" OR "genetic predisposition to disease" OR "dna mismatch repair" OR (MH "Rapid Sequence Induction and Intubation") OR (MH "Sequence Analysis+") OR (MH "Genes, BRCA") OR (MH "Genetic Screening") OR (MH "Genetic Techniques+") OR (MH "Genetic Research+") OR (MH "Genetic Variation+") OR (MH "Genetic Markers")) AND ("breast neoplasm*" OR "breast cancer*" OR "breast neoplasm*" OR "cancer of the breast" OR "neoplasm of the breast" OR "neoplasms of the breast" OR "ductal breast carcinoma*" OR "mammary cancer*" OR "mammary neoplasm*" OR "breast malignant neoplasm*" OR "breast malignant tumor*" OR "breast malignant tumour*" OR "breast tumor*" OR "breast tumour*") OR (MH "Breast Neoplasms+") )
Cochrane Database
Searched April 7, 2021
47 results
(brca OR brca1 OR brca2 OR "germline mutation*" OR "germ-line mutation*" OR TP53TG1 OR TP53 OR TP53TG5 OR p53 OR "rad52" OR "gene mutat*" OR "nucleotide sequenc*" OR "dna sequence analysis" OR "nanopore sequenc*" OR "Nucleotide sequen*" OR "dna repair" OR "li-fraumeni" OR "neoplasm dna" OR "Chek2" OR "genetic test*" OR "genetic carrier screen*" OR "genetic screen*" OR "Genetic service*" OR "medical genetics" OR "Genetic variation*" OR "genetic predisposition to disease" OR "dna mismatch repair") AND ("African descent" OR "African ancestry" OR "African Europeans*" OR "African Asians*" OR "African Americans*" OR "African migrants" OR "Southern African Development Community" OR "SADC" OR "African Caribbeans*" OR "African continental ancestry" OR "Africa South of the Sahara" OR "sub-sahara*" OR "subsahara*" OR "Angola" OR "Luanda" OR "Luanda" OR "Benin" OR "Porto-Novo" OR "Botswana" OR "Gaborone" OR "Burkina Faso" OR "Ouagadougou" OR "Burundi" OR "Gitega" OR "Cameroon" OR "Yaounde" OR "Central African Republic" OR "Bangui" OR "Chad" OR "N'Djamena" OR "Comoros" OR "Moroni" OR "Democratic Republic of the Congo" OR "Kinshasa" OR "Republic of the Congo" OR "Brazzaville" OR "Cote d'Ivoire" OR "Yamoussoukro" OR "Djibouti" OR "Equatorial Guinea" OR "Malabo" OR "Eritrea" OR "Asmara" OR "Eswatini" OR "Mbabane" OR "Ethiopia" OR "Addis Ababa" OR "Gabon" OR "Libreville" OR "Gambia" OR "Banjul" OR "Ghana" OR "Accra" OR "Guinea" OR "Conakry" OR "Guinea-Bissau" OR "Bissau" OR "Kenya" OR "Nairobi" OR "Lesotho" OR "Maseru" OR "Liberia" OR "Monrovia" OR "Madagascar" OR "Antananarivo" OR "Malawi" OR "Lilongwe" OR "Mali" OR "Bamako" OR "Mauritania" OR "Nouakchott" OR "Mauritius" OR "Port Louis" OR "Mozambique" OR "Maputo" OR "Namibia" OR "Windhoek" OR "Niger" OR "Niamey" OR "Nigeria" OR "Abuja" OR "Rwanda" OR "Kigali" OR "Sao Tome and Principe" OR "Sao Tome" OR "Senegal" OR "Dakar" OR "Seychelles" OR "Sierra Leone" OR "Freetown" OR "Somalia" OR "Mogadishu" OR "South Africa" OR "Pretoria" OR "South Sudan" OR "Juba" OR "Sudan" OR "Khartoum" OR "Tanzania" OR "Dodoma" OR "Togo" OR "Lomé" OR "Uganda" OR "Kampala" OR "Zambia" OR "Lusaka" OR "Zimbabwe" OR "Harare" OR "west-africa*" OR "west africa*" OR "south african*" OR "east-africa*" OR "east africa*") AND ("breast neoplasm*" OR "breast cancer*" OR "breast neoplasm*" OR "cancer of the breast" OR "neoplasm of the breast" OR "neoplasms of the breast" OR "ductal breast carcinoma*" OR "mammary cancer*" OR "mammary neoplasm*" OR "breast malignant neoplasm*" OR "breast malignant tumor*" OR "breast malignant tumour*" OR "breast tumor*" OR "breast tumour*")
EMBASE
Searched April 7, 2021
1,002 results
(brca OR brca1 OR brca2 OR 'germline mutation*' OR 'germ-line mutation*' OR tp53tg1 OR tp53 OR tp53tg5 OR p53 OR 'rad52' OR 'gene mutat*' OR 'nucleotide sequenc*' OR 'dna sequence analysis' OR 'nanopore sequenc*' OR 'nucleotide sequen*' OR 'dna repair' OR 'li- fraumeni' OR 'neoplasm dna' OR 'chek2' OR 'genetic test*' OR 'genetic carrier screen*' OR 'genetic screen*' OR 'genetic service*' OR 'medical genetic*' OR 'genetic variation*' OR 'genetic predisposition to disease' OR 'dna mismatch repair' OR 'brca1 protein'/exp OR 'brca2 protein'/exp OR 'genetic screening'/exp OR 'protein p53'/exp OR 'gene sequence'/exp OR 'nanopore sequencing'/exp OR 'li-fraumeni syndrome'/exp OR 'dna repair'/exp OR 'heterozygote detection'/exp OR 'genetic predisposition'/exp) AND ('breast tumor'/exp OR 'breast cancer*' OR 'breast neoplasm*' OR 'cancer of the breast' OR 'neoplasm of the breast' OR 'neoplasms of the breast' OR 'ductal breast carcinoma*' OR 'mammary cancer*' OR 'mammary neoplasm*' OR 'breast malignant neoplasm*' OR 'breast malignant tumor*' OR 'breast malignant tumour*' OR 'breast tumor*' OR 'breast tumour*') AND ('african descent' OR 'african ancestry' OR 'african europeans*' OR 'african asians*' OR 'african americans*' OR 'african migrants' OR 'southern african development community' OR 'sadc' OR 'african caribbeans*' OR 'african continental ancestry' OR 'africa south of the sahara' OR 'sub-sahara*' OR 'subsahara*' OR 'angola'/exp OR 'angola' OR 'luanda' OR 'benin'/exp OR 'benin' OR 'porto-novo' OR 'botswana'/exp OR 'botswana' OR 'gaborone' OR 'burkina faso'/exp OR 'burkina faso' OR 'ouagadougou' OR 'burundi'/exp OR 'burundi' OR 'gitega' OR 'cameroon'/exp OR 'cameroon' OR 'yaounde' OR 'central african republic'/exp OR 'central african republic' OR 'bangui' OR 'chad'/exp OR 'chad' OR 'n djamena' OR 'comoros'/exp OR 'comoros' OR 'moroni' OR 'democratic republic of the congo'/exp OR 'democratic republic of the congo' OR 'kinshasa' OR 'republic of the congo' OR 'brazzaville' OR 'cote d ivoire'/exp OR 'cote d ivoire' OR 'yamoussoukro' OR 'djibouti'/exp OR 'djibouti' OR 'equatorial guinea'/exp OR 'equatorial guinea' OR 'malabo' OR 'eritrea'/exp OR 'eritrea' OR 'asmara' OR 'eswatini'/exp OR 'eswatini' OR 'mbabane' OR 'ethiopia'/exp OR 'ethiopia' OR 'addis ababa' OR 'gabon'/exp OR 'gabon' OR 'libreville' OR 'gambia'/exp OR 'gambia' OR 'banjul' OR 'ghana'/exp OR 'ghana' OR 'accra' OR 'guinea'/exp OR 'guinea' OR 'conakry' OR 'guinea-bissau'/exp OR 'guinea-bissau' OR 'bissau' OR 'kenya'/exp OR 'kenya' OR 'nairobi' OR 'lesotho'/exp OR 'lesotho' OR 'maseru' OR 'liberia'/exp OR 'liberia' OR 'monrovia' OR 'madagascar'/exp OR 'madagascar' OR 'antananarivo' OR 'malawi'/exp OR 'malawi' OR 'lilongwe' OR 'mali'/exp OR 'mali' OR 'bamako' OR 'mauritania'/exp OR 'mauritania' OR 'nouakchott' OR 'mauritius'/exp OR 'mauritius' OR 'port louis' OR 'mozambique'/exp OR 'mozambique' OR 'maputo' OR 'namibia'/exp OR 'namibia' OR 'windhoek' OR 'niger'/exp OR 'niger' OR 'niamey' OR 'nigeria'/exp OR 'nigeria' OR 'abuja' OR 'rwanda'/exp OR 'rwanda' OR 'kigali' OR 'sao tome and principe'/exp OR 'sao tome and principe' OR 'sao tome' OR 'senegal'/exp OR 'senegal' OR 'dakar' OR 'seychelles'/exp OR 'seychelles' OR 'sierra leone'/exp OR 'sierra leone' OR 'freetown' OR 'somalia'/exp OR 'somalia' OR 'mogadishu' OR 'south africa'/exp OR 'south africa' OR 'pretoria' OR 'south sudan'/exp OR 'south sudan' OR 'juba' OR 'sudan'/exp OR 'sudan' OR 'khartoum' OR 'tanzania'/exp OR 'tanzania' OR 'dodoma' OR 'togo'/exp OR 'togo' OR 'lomé' OR 'uganda'/exp OR 'uganda' OR 'kampala' OR 'zambia'/exp OR 'zambia' OR 'lusaka' OR 'zimbabwe'/exp OR 'zimbabwe' OR 'harare' OR 'west-africa*' OR 'west africa*' OR 'south african*' OR 'east-africa*' OR 'east africa*' OR 'africa south of the sahara'/exp)
APPENDIX 2. SCOPING REVIEW DATA EXTRACTION FORM
1. Manuscript title
2. Country of institutional affiliation for first author:
United States of America (187) … Zimbabwe (1357)
3. Record first-author institutional affiliation:
4. Country of institutional affiliation for last author:
United States of America (187) … Zimbabwe (1357)
5. Record last-author institutional affiliation:
6. Where was the research conducted?
-
7. Record study type:
a. Literature review (meta-analysis, systematic, scoping)
b. Randomized controlled trial (RCT)
c. Retrospective analysis (cross-sectional, cohort)
d. Prospective (cross-sectional, cohort)
e. Mixed methods
f. Qualitative study
g. Other
-
8. Was informed consent obtained in this study?
a. Yes
b. No
c. Unsure
9. Please elaborate on the informed consent process:
-
10. What germline mutation was studied?
a. None
b. BRCA1
c. BRCA2
d. TP53
e. RADS1
f. CDH1
g. NDN
h. CHEK2
i. FANCA
j. MRE11A
k. SPINK1
l. MLH1
m. ATM
n. Other (specify)
-
11. Was germline genetic testing conducted as part of this study?
a. Yes
b. No
-
12. What samples were used for genetic testing, if conducted?
a. Blood
b. Saliva
c. Unknown
d. Other (specify)
-
13. How were germline mutations tested?
a. SNPs
b. PCR
c. Next-generation sequencing
d. Sanger sequencing
e. Unsure
f. Other (specify)
14. Record specific testing platform or sequencing model if applicable:
-
15. Did they use an existing database?
a. No
b. Yes
c. Unsure
-
16. Record database
a. SEER
b. Cancer Genome Atlas
c. Breast Cancer Association Consortium
d. Consortium of Investigators of Modifiers of BRCA1/2 (CIMBA)
e. Women's Circle of Health Study
f. Breast Cancer Family Registry and the University of Chicago
g. Other State Cancer Registry (indicate state)
h. Other (specify)
-
17. Which racial/ethnic categories were used?
a. African American (AA)
b. African ancestry
c. Black African
d. African or African descent
e. Black American
f. Non-Hispanic Black
g. Black
h. Other (specify)
-
18. Was “race,” “ethnicity,” or other element describing these variable defined in the article?
a. Yes
b. No
c. Unsure
19. How was it defined?
-
20. Was “racism” ever mentioned in the manuscript
a. Yes
b. No
21. How was “racism” mentioned? Copy and paste the sentence or paragraph for context.
-
22. Record population size (No.):
Total study population:
African American population:
White population:
Other race/ethnicity or subpopulation:
Other race/ethnicity or subpopulation:
Other race/ethnicity or subpopulation:
Other race/ethnicity or subpopulation:
Other race/ethnicity or subpopulation:
-
23. Was genetic counseling implemented or evaluated?
a. Yes
b. No
-
24. Did this study evaluate perspectives on genetic testing?
a. Yes
b. No
-
25. Method for evaluation:
a. Interviews
b. Phone survey
c. Survey
d. Focus groups
e. Electronic medical record
f. Other (specify)
26. What were the outcomes/findings of the paper?
-
27. Was there a bioethical component to the manuscript?
a. Yes
b. Maybe
c. No
-
28. What ethical elements were raised?
a. Equity
b. Autonomy
c. Cost
d. Data ownership
e. Hesitance
f. Unintentional harm
g. Social or cultural norms
h. Religion
i. Other
29. Any additional comments about the manuscript:
Yuri Fedoriw
Honoraria: Alexion Pharmaceuticals
Oluwadamilola T. Oladeru
Employment: Mayo Clinic Cancer Center, HCA Healthcare, University of Florida
Research Funding: Bristol Myers Squibb Foundation, ASC/Pfizer, NRG Oncology, Radiation Oncology Institute (ROI)
Onyinye D. Balogun
Employment: Mission-Driven Tech
Stock and Other Ownership Interests: Mission-Driven Tech
Honoraria: New Century Health
Patents, Royalties, Other Intellectual Property: Mission-Driven Tech
Mya L. Roberson
Consulting or Advisory Role: Concert Genetics
Olufunmilayo I. Olopade
Employment: CancerIQ
Leadership: CancerIQ
Stock and Other Ownership Interests: CancerIQ, Tempus, 54gene, HealthWell Solutions
Consulting or Advisory Role: Tempus
Research Funding: Roche/Genentech (Inst), Color Genomics (Inst)
Uncompensated Relationships: ACS, Susan G. Komen for the Cure
Open Payments Link: https://openpaymentsdata.cms.gov/physician/olopade
No other potential conflicts of interest were reported.
SUPPORT
Supported by the Office of Global Health Education at the University of North Carolina at Chapel Hill School of Medicine.
DATA SHARING STATEMENT
All data can be made available upon reasonable request.
AUTHOR CONTRIBUTIONS
Conception and design: Yoshiko Iwai, Yuri Fedoriw, Tamiwe Tomoka, Shekinah N.C. Elmore
Financial support: Yoshiko Iwai
Collection and assembly of data: Yoshiko Iwai, Kadiata Toumbou, Takondwa Zuze, Jenny S. Morgan, Sarah T. Wright, Yuri Fedoriw, Shekinah N.C. Elmore
Data analysis and interpretation: Yoshiko Iwai, Kadiata Toumbou, Lusayo Simwinga, Oluwadamilola T. Oladeru, Onyinye D. Balogun, Mya L. Roberson, Tamiwe Tomoka, Shekinah N.C. Elmore
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Yuri Fedoriw
Honoraria: Alexion Pharmaceuticals
Oluwadamilola T. Oladeru
Employment: Mayo Clinic Cancer Center, HCA Healthcare, University of Florida
Research Funding: Bristol Myers Squibb Foundation, ASC/Pfizer, NRG Oncology, Radiation Oncology Institute (ROI)
Onyinye D. Balogun
Employment: Mission-Driven Tech
Stock and Other Ownership Interests: Mission-Driven Tech
Honoraria: New Century Health
Patents, Royalties, Other Intellectual Property: Mission-Driven Tech
Mya L. Roberson
Consulting or Advisory Role: Concert Genetics
Olufunmilayo I. Olopade
Employment: CancerIQ
Leadership: CancerIQ
Stock and Other Ownership Interests: CancerIQ, Tempus, 54gene, HealthWell Solutions
Consulting or Advisory Role: Tempus
Research Funding: Roche/Genentech (Inst), Color Genomics (Inst)
Uncompensated Relationships: ACS, Susan G. Komen for the Cure
Open Payments Link: https://openpaymentsdata.cms.gov/physician/olopade
No other potential conflicts of interest were reported.
REFERENCES
- 1.Giaquinto AN, Sung H, Miller KD, et al. : Breast cancer statistics, 2022. CA Cancer J Clin 72:524-541, 2022 [DOI] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, et al. : Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209-249, 2021 [DOI] [PubMed] [Google Scholar]
- 3.Allemani C, Matsuda T, Di Carlo V, et al. : Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 391:1023-1075, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCormack V, McKenzie F, Foerster M, et al. : Breast cancer survival and survival gap apportionment in sub-Saharan Africa (ABC-DO): A prospective cohort study. Lancet Glob Health 8:e1203-e1212, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Joko-Fru WY, Miranda-Filho A, Soerjomataram I, et al. : Breast cancer survival in sub-Saharan Africa by age, stage at diagnosis and human development index: A population-based registry study. Int J Cancer 146:1208-1218, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodriguez P, Yurgelun MB: How the USPSTF genetic testing update for BRCA-related cancers impacts care, 2020. https://dailynews.ascopubs.org/do/uspstf-genetic-testing-update-brca-related-cancers-impacts-care
- 7.Eng A, McCormack V, dos-Santos-Silva I: Receptor-defined subtypes of breast cancer in indigenous populations in Africa: A systematic review and meta-analysis. PLoS Med 11:e1001720, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sung H, DeSantis CE, Fedewa SA, et al. : Breast cancer subtypes among Eastern-African–born Black women and other Black women in the United States. Cancer 125:3401-3411, 2019 [DOI] [PubMed] [Google Scholar]
- 9.Newman LA, Jenkins B, Chen Y, et al. : Hereditary susceptibility for triple negative breast cancer associated with western sub-Saharan African ancestry: Results from an International Surgical Breast Cancer Collaborative. Ann Surg 270:484-492, 2019 [DOI] [PubMed] [Google Scholar]
- 10.Sirugo G, Williams SM, Tishkoff SA: The missing diversity in human genetic studies. Cell 177:26-31, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Borrell LN, Elhawary JR, Fuentes-Afflick E, et al. : Race and genetic ancestry in medicine—A time for reckoning with racism. N Engl J Med 384:474-480, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byeon YJJ, Islamaj R, Yeganova L, et al. : Evolving use of ancestry, ethnicity, and race in genetics research—A survey spanning seven decades. Am J Hum Genet 108:2215-2223, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flanagin A, Frey T, Christiansen SL, et al. : Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA 326:621, 2021 [DOI] [PubMed] [Google Scholar]
- 14.National Academies of Sciences, Engineering, and Medicine (U.S.) : An Evidence Framework for Genetic Testing. Washington, D.C., The National Academies Press, 2017 [PubMed] [Google Scholar]
- 15.Madlensky L, Trepanier AM, Cragun D, et al. : A rapid systematic review of outcomes studies in genetic counseling. J Genet Couns 26:361-378, 2017 [DOI] [PubMed] [Google Scholar]
- 16.Chiba A, Hoskin TL, Hallberg EJ, et al. : Impact that timing of genetic mutation diagnosis has on surgical decision making and outcome for BRCA1/BRCA2 mutation carriers with breast cancer. Ann Surg Oncol 23:3232-3238, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwartz MD, Lerman C, Brogan B, et al. : Impact of BRCA1/BRCA2 counseling and testing on newly diagnosed breast cancer patients. J Clin Oncol 22:1823-1829, 2004 [DOI] [PubMed] [Google Scholar]
- 18.Pederson HJ, Hussain N, Noss R, et al. : Impact of an embedded genetic counselor on breast cancer treatment. Breast Cancer Res Treat 169:43-46, 2018 [DOI] [PubMed] [Google Scholar]
- 19.Couch FJ, Hart SN, Sharma P, et al. : Inherited mutations in 17 breast cancer susceptibility genes among a large triple-negative breast cancer cohort unselected for family history of breast cancer. J Clin Oncol 33:304-311, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khabele D, Runowicz CD: Genetic counseling, testing, and screening for breast and ovarian cancer: Practical and social considerations. Curr Womens Health Rep 2:163-169, 2002 [PubMed] [Google Scholar]
- 21.Shah PD, Domchek SM: The contemporary landscape of genetic testing and breast cancer: Emerging issues. Breast J 26:1549-1555, 2020 [DOI] [PubMed] [Google Scholar]
- 22.Petrova D, Cruz M, Sánchez MJ: BRCA1/2 testing for genetic susceptibility to cancer after 25 years: A scoping review and a primer on ethical implications. Breast 61:66-76, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Munn Z, Peters MDJ, Stern C, et al. : Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 18:143, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tricco AC, Lillie E, Zarin W, et al. : PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med 169:467-473, 2018 [DOI] [PubMed] [Google Scholar]
- 25.Zeleza PT: The inventions of African identities and languages: The discursive and developmental implications, in Arasanyin OF and Pemberton MA (eds.): Selected Proceedings of the 36th Annual Conference on African Linguistics. Somerville, MA, Cascadilla Proceedings Project, 2006, pp 14-26
- 26.Tatenda Chinondidyachii Mashanda : Rethinking the term “sub Saharan Africa.” The African Exponent. https://www.africanexponent.com/bpost/rethinking-the-term-sub-saharan-africa-36
- 27.Saleh S, Masekela R, Heinz E, et al. : Equity in global health research: A proposal to adopt author reflexivity statements. PLoS Glob Public Health 2:e0000160, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aceto GM, Awadelkarim KD, Di Nicola M, et al. : Germline TP53 mutation spectrum in Sudanese premenopausal breast cancer patients: Correlations with reproductive factors. Breast Cancer Res Treat 175:479-485, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Macaulay S, Goodyear QC, Kruger M, et al. : The first two confirmed sub-Saharan African families with germline TP53 mutations causing Li-Fraumeni syndrome. Fam Cancer 17:607-613, 2018 [DOI] [PubMed] [Google Scholar]
- 30.Habyarimana T, Attaleb M, Mugenzi P, et al. : Association of p53 codon 72 polymorphism with breast cancer in a Rwandese population. Pathobiology 85:186-191, 2018 [DOI] [PubMed] [Google Scholar]
- 31.Hirsch AE, Atencio DP, Rosenstein BS: Screening for ATM sequence alterations in African-American women diagnosed with breast cancer. Breast Cancer Res Treat 107:139-144, 2007 [DOI] [PubMed] [Google Scholar]
- 32.Habyarimana T, Attaleb M, Mugenzi P, et al. : CHEK2 germ line mutations are lacking among familial and sporadic breast cancer patients in Rwanda. Asian Pac J Cancer Prev 19:375-379, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ding YC, Steele L, Chu LH, et al. : Germline mutations in PALB2 in African-American breast cancer cases. Breast Cancer Res Treat 126:227-230, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sluiter M, Mew S, van Rensburg EJ: PALB2 sequence variants in young South African breast cancer patients. Fam Cancer 8:347-353, 2009 [DOI] [PubMed] [Google Scholar]
- 35.Ding YC, Adamson AW, Steele L, et al. : Discovery of mutations in homologous recombination genes in African-American women with breast cancer. Fam Cancer 17:187-195, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McKean-Cowdin R, Spencer Feigelson H, Xia LY, et al. : BRCA1 variants in a family study of African-American and Latina women. Hum Genet 116:497-506, 2005 [DOI] [PubMed] [Google Scholar]
- 37.Pal T, Vadaparampil S, Betts J, et al. : BRCA1/2 in high-risk African American women with breast cancer: Providing genetic testing through various recruitment strategies. Genet Test 12:401-407, 2008 [DOI] [PubMed] [Google Scholar]
- 38.Conley CC, Kasting ML, Augusto BM, et al. : Impact of genetic testing on risk-management behavior of Black breast cancer survivors: A longitudinal, observational study. Ann Surg Oncol 27:1659-1670, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pal T, Bonner D, Kim J, et al. : Early onset breast cancer in a registry-based sample of African-American women: BRCA mutation prevalence, and other personal and system-level clinical characteristics. Breast J 19:189-192, 2013 [DOI] [PubMed] [Google Scholar]
- 40.Francies FZ, Wainstein T, De Leeneer K, et al. : BRCA1, BRCA2 and PALB2 mutations and CHEK2 c.1100delC in different South African ethnic groups diagnosed with premenopausal and/or triple negative breast cancer. BMC Cancer 15:912, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Torrorey-Sawe R, van der Merwe N, Mining SK, et al. : Pioneering informed consent for return of research results to breast cancer patients facing barriers to implementation of genomic medicine: The Kenyan BRCA1/2 testing experience using whole exome sequencing. Front Genet 11:170, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bishop MR, Omeler-Fenaud SM, Huskey ALW, et al. : Gene panel screening for insight towards breast cancer susceptibility in different ethnicities. PLoS One 15:e0238295, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Biunno I, Aceto G, Awadelkarim KD, et al. : BRCA1 point mutations in premenopausal breast cancer patients from Central Sudan. Fam Cancer 13:437-444, 2014 [DOI] [PubMed] [Google Scholar]
- 44.Olopade OI, Fackenthal JD, Dunston G, et al. : Breast cancer genetics in African Americans. Cancer 97:236-245, 2003 [DOI] [PubMed] [Google Scholar]
- 45.Zoure AA, Slaoui M, Bambara HA, et al. : BRCA1 c.68_69delAG (exon2), c.181T>G (exon5), c.798_799delTT and 943ins10 (exon11) mutations in Burkina Faso. J Public Health Afr 9:663, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Churpek JE, Walsh T, Zheng Y, et al. : Inherited predisposition to breast cancer among African American women. Breast Cancer Res Treat 149:31-39, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gao Q, Neuhausen S, Cummings S, et al. : Recurrent germ-line BRCA1 mutations in extended African American families with early-onset breast cancer. Am J Hum Genet 60:1233-1236, 1997 [PMC free article] [PubMed] [Google Scholar]
- 48.van der Merwe NC, Oosthuizen J, Theron M, et al. : The contribution of large genomic rearrangements in BRCA1 and BRCA2 to South African familial breast cancer. BMC Cancer 20:391, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fackenthal JD: Complete allelic analysis of BRCA1 and BRCA2 variants in young Nigerian breast cancer patients. J Med Genet 42:276-281, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Uyisenga JP, Segers K, Lumaka AZ, et al. : Screening of germline mutations in young Rwandan patients with breast cancers. Mol Genet Genomic Med 8:e1500, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zheng Y, Zhang J, Niu Q, et al. : Novel germline PALB2 truncating mutations in African American breast cancer patients. Cancer 118:1362-1370, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haffty BG: Racial differences in the incidence of BRCA1 and BRCA2 mutations in a cohort of early onset breast cancer patients: African American compared to White women. J Med Genet 43:133-137, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gao Q, Tomlinson G, Das S, et al. : Prevalence of BRCA1 and BRCA2 mutations among clinic-based African American families with breast cancer. Hum Genet 107:186-191, 2000 [DOI] [PubMed] [Google Scholar]
- 54.Diez O, Pelegrí A, Gadea N, et al. : Novel BRCA1 deleterious mutation (c.1949_1950delTA) in a woman of Senegalese descent with triple-negative early-onset breast cancer. Oncol Lett 2:1287-1289, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Adedokun B, Zheng Y, Ndom P, et al. : Prevalence of inherited mutations in breast cancer predisposition genes among women in Uganda and Cameroon. Cancer Epidemiol Biomarkers Prev 29:359-367, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gardiner SA, Smith D, Loubser F, et al. : New recurring BRCA1 variant: An additional South African founder mutation? S Afr Med J 109:544, 2019 [DOI] [PubMed] [Google Scholar]
- 57.Ricks-Santi L, McDonald JT, Gold B, et al. : Next generation sequencing reveals high prevalence of BRCA1 and BRCA2 variants of unknown significance in early-onset breast cancer in African American women. Ethn Dis 27:169, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Diop JPD, Diallo RN, Bourdon-Huguenin V, et al. : Novel BRCA2 pathogenic variant c.5219 T > G; p.(Leu1740Ter) in a consanguineous Senegalese family with hereditary breast cancer. BMC Med Genet 20:73, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ndugga-Kabuye MK, Issaka RB: Inequities in multi-gene hereditary cancer testing: Lower diagnostic yield and higher VUS rate in individuals who identify as Hispanic, African or Asian and Pacific Islander as compared to European. Fam Cancer 18:465-469, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reeves MD, Yawitch TM, van der Merwe NC, et al. : BRCA1 mutations in South African breast and/or ovarian cancer families: Evidence of a novel founder mutation in Afrikaner families. Int J Cancer 110:677-682, 2004 [DOI] [PubMed] [Google Scholar]
- 61.Palmer JR, Polley EC, Hu C, et al. : Contribution of germline predisposition gene mutations to breast cancer risk in African American women. JNCI J Natl Cancer Inst 112:1213-1221, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Amankwaa-Frempong E, Yeboah FA, Nguah SB, et al. : Breast cancer genetic testing among African patients with breast cancer: Deoxyribonucleic acid extraction from tumor tissue and international multidisciplinary partnerships. JAMA Surg 152:800, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zheng Y, Walsh T, Gulsuner S, et al. : Inherited breast cancer in Nigerian women. J Clin Oncol 36:2820-2825, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vargas E, Torres Lopez DM, Deugd R, et al. : Low prevalence of the four common Colombian founder mutations in BRCA1 and BRCA2 in early-onset and familial Afro-Colombian patients with breast cancer. Oncologist 24:e475-e479, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yawitch TM, van Rensburg EJ, Mertz M, et al. : Absence of commonly recurring BRCA1 mutations in Black South African women with breast cancer. S Afr Med J 90:788, 2000 [PubMed] [Google Scholar]
- 66.Oosthuizen J, Kotze MJ, Van Der Merwe N, et al. : Globally rare BRCA2 variants with founder haplotypes in the South African population: Implications for point-of-care testing based on a single-institution BRCA1/2 next-generation sequencing study. Front Oncol 10:619469, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Thompson HS, Sussner K, Schwartz MD, et al. : Receipt of genetic counseling recommendations among Black women at high risk for BRCA mutations. Genet Test Mol Biomark 16:1257-1262, 2012 [DOI] [PubMed] [Google Scholar]
- 68.Nikolaidis C, Duquette D, Mendelsohn-Victor KE, et al. : Disparities in genetic services utilization in a random sample of young breast cancer survivors. Genet Med 21:1363-1370, 2019 [DOI] [PubMed] [Google Scholar]
- 69.Doe S, Petersen S, Swain M: Utilization of genetic testing in breast cancer treatment after implementation of comprehensive multi-disciplinary care. Breast J 26:911-916, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Purrington KS, Schwartz AG, Ruterbusch JJ, et al. : Patterns of cancer family history and genetic counseling eligibility among African Americans with breast, prostate, lung, and colorectal cancers: A Detroit Research on Cancer Survivors cohort study. Cancer 126:4744-4752, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cragun D, Weidner A, Lewis C, et al. : Racial disparities in BRCA testing and cancer risk management across a population-based sample of young breast cancer survivors: Disparities in BRCA Testing and Care. Cancer 123:2497-2505, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pasick RJ, Joseph G, Stewart S, et al. : Effective referral of low-income women at risk for hereditary breast and ovarian cancer to genetic counseling: A randomized delayed intervention control trial. Am J Public Health 106:1842-1848, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sutton AL, Hurtado-de-Mendoza A, Quillin J, et al. : Reducing disparities in receipt of genetic counseling for underserved women at risk of hereditary breast and ovarian cancer. J Womens Health 29:1131-1135, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lerman C, Hughes C, Benkendorf JL, et al. : Racial differences in testing motivation and psychological distress following pretest education for BRCA1 gene testing. Cancer Epidemiol Biomarkers Prev 8:361-367, 1999 [PubMed] [Google Scholar]
- 75.Halbert CH, Kessler L, Stopfer JE, et al. : Low rates of acceptance of BRCA1 and BRCA2 test results among African American women at increased risk for hereditary breast-ovarian cancer. Genet Med 8:576-582, 2006 [DOI] [PubMed] [Google Scholar]
- 76.Kinney AY, Simonsen SE, Baty BJ, et al. : Acceptance of genetic testing for hereditary breast ovarian cancer among study enrollees from an African American kindred. Am J Med Genet A 140A:813-826, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Halbert CH, Kessler L, Collier A, et al. : Low rates of African American participation in genetic counseling and testing for BRCA1/2 mutations: Racial disparities or just a difference? J Genet Couns 21:676-683, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pal T, Rocchio E, Garcia A, et al. : Recruitment of Black women for a study of inherited breast cancer using a cancer registry–based approach. Genet Test Mol Biomark 15:69-77, 2011 [DOI] [PubMed] [Google Scholar]
- 79.Halbert CH, Love D, Mayes T, et al. : Retention of African American women in cancer genetics research. Am J Med Genet A 146A:166-173, 2008 [DOI] [PubMed] [Google Scholar]
- 80.Kodl MM, Lee JW, Matthews AK, et al. : Correlates of depressive symptoms among women seeking cancer genetic counseling and risk assessment at a high-risk cancer clinic. J Genet Couns 15:267-276, 2006 [DOI] [PubMed] [Google Scholar]
- 81.Sussner KM, Thompson HS, Jandorf L, et al. : The influence of acculturation and breast cancer-specific distress on perceived barriers to genetic testing for breast cancer among women of African descent: Genetic testing among women of African descent. Psychooncology 18:945-955, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Halbert C, Kessler L, Collier A, et al. : Psychological functioning in African American women at an increased risk of hereditary breast and ovarian cancer: Cancer distress in African Americans. Clin Genet 68:222-227, 2005 [DOI] [PubMed] [Google Scholar]
- 83.Thompson HS, Valdimarsdottir HB, Duteau-Buck C, et al. : Psychosocial predictors of BRCA counseling and testing decisions among urban African-American women. Cancer Epidemiol Biomarkers Prev 11:1579-1585, 2002 [PubMed] [Google Scholar]
- 84.Gonzalez BD, Hoogland AI, Kasting ML, et al. : Psychosocial impact of BRCA testing in young Black breast cancer survivors. Psychooncology 27:2778-2785, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ewing A, Thompson N, Ricks-Santi L: Strategies for enrollment of African Americans into cancer genetic studies. J Cancer Educ 30:108-115, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Charles S, Kessler L, Stopfer JE, et al. : Satisfaction with genetic counseling for BRCA1 and BRCA2 mutations among African American women. Patient Educ Couns 63:196-204, 2006 [DOI] [PubMed] [Google Scholar]
- 87.Pal T, Stowe C, Cole A, et al. : Evaluation of phone-based genetic counselling in African American women using culturally tailored visual aids. Clin Genet 78:124-131, 2010 [DOI] [PubMed] [Google Scholar]
- 88.Mays D, Sharff ME, DeMarco TA, et al. : Outcomes of a systems-level intervention offering breast cancer risk assessments to low-income underserved women. Fam Cancer 11:493-502, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Halbert CH, Kessler L, Troxel AB, et al. : Effect of genetic counseling and testing for BRCA1 and BRCA2 mutations in African American women: A randomized trial. Public Health Genomics 13:440-448, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Smith A, Vidal G, Pritchard E, et al. : Sistas taking a stand for breast cancer research (STAR) study: A community-based participatory genetic research study to enhance participation and breast cancer equity among African American women in Memphis, TN. Int J Environ Res Public Health 15:2899, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Donovan KA, Tucker DC: Knowledge about genetic risk for breast cancer and perceptions of genetic testing in a sociodemographically diverse sample. J Behav Med 23:15-36, 2000 [DOI] [PubMed] [Google Scholar]
- 92.Glenn BA, Chawla N, Bastani R: Barriers to genetic testing for breast cancer risk among ethnic minority women: An exploratory study. Ethn Dis 22:267-273, 2012 [PubMed] [Google Scholar]
- 93.Ford ME, Alford SH, Britton D, et al. : Factors influencing perceptions of breast cancer genetic counseling among women in an urban health care system. J Genet Couns 16:735-753, 2007 [DOI] [PubMed] [Google Scholar]
- 94.Sheppard VB, Mays D, Tercyak KP, et al. : Medical mistrust influences Black women’s level of engagement in BRCA1/2 genetic counseling and testing. J Natl Med Assoc 105:17-22, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hughes C, Fasaye GA, LaSalle VH, et al. : Sociocultural influences on participation in genetic risk assessment and testing among African American women. Patient Educ Couns 51:107-114, 2003 [DOI] [PubMed] [Google Scholar]
- 96.Conley CC, Ketcher D, Reblin M, et al. : The big reveal: Family disclosure patterns of BRCA genetic test results among young Black women with invasive breast cancer. J Genet Couns 29:410-422, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Machirori M, Patch C, Metcalfe A: Black and Minority Ethnic women’s decision-making for risk reduction strategies after BRCA testing: Use of context and knowledge. Eur J Med Genet 62:376-384, 2019 [DOI] [PubMed] [Google Scholar]
- 98.Friebel TM, Andrulis IL, Balmaña J, et al. : BRCA1 and BRCA2 pathogenic sequence variants in women of African origin or ancestry. Hum Mutat 40:1781-1796, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Baty BJ, Dudley WN, Musters A, et al. : Uncertainty in BRCA1 cancer susceptibility testing. Am J Med Genet C Semin Med Genet 142C:241-250, 2006 [DOI] [PubMed] [Google Scholar]
- 100.Edwards TA, Thompson HS, Kwate NOA, et al. : Association between temporal orientation and attitudes about BRCA1/2 testing among women of African descent with family histories of breast cancer. Patient Educ Couns 72:276-282, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Peterson JM, Pepin A, Thomas R, et al. : Racial disparities in breast cancer hereditary risk assessment referrals. J Genet Couns 29:587-593, 2020 [DOI] [PubMed] [Google Scholar]
- 102.Benkendorf JL, Reutenauer JE, Hughes CA, et al. : Patients’ attitudes about autonomy and confidentiality in genetic testing for breast-ovarian cancer susceptibility. Am J Med Genet 73:296-303, 1997 [DOI] [PubMed] [Google Scholar]
- 103.Pal T, Bonner D, Cragun D, et al. : A high frequency of BRCA mutations in young Black women with breast cancer residing in Florida: BRCA mutations in Black women. Cancer 121:4173-4180, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ademuyiwa FO, Salyer P, Ma Y, et al. : Assessing the effectiveness of the National Comprehensive Cancer Network genetic testing guidelines in identifying African American breast cancer patients with deleterious genetic mutations. Breast Cancer Res Treat 178:151-159, 2019 [DOI] [PubMed] [Google Scholar]
- 105.Hunt LM, Megyesi MS: The ambiguous meanings of the racial/ethnic categories routinely used in human genetics research. Soc Sci Med 66:349-361, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hunt LM, Megyesi MS: Genes, race and research ethics: Who’s minding the store? J Med Ethics 34:495-500, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mauro M, Allen DS, Dauda B, et al. : A scoping review of guidelines for the use of race, ethnicity, and ancestry reveals widespread consensus but also points of ongoing disagreement. Am J Hum Genet 109:2110-2125, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Susswein LR, Skrzynia C, Lange LA, et al. : Increased uptake of BRCA1/2 genetic testing among African American women with a recent diagnosis of breast cancer. J Clin Oncol 26:32-36, 2008 [DOI] [PubMed] [Google Scholar]
- 109.Moorman PG, Skinner CS, Evans JP, et al. : Racial differences in enrolment in a cancer genetics registry. Cancer Epidemiol Biomarkers Prev 13:1349-1354, 2004 [PubMed] [Google Scholar]
- 110.Race, Ethnicity, and Genetics Working Group : The use of racial, ethnic, and ancestral categories in human genetics research. Am J Hum Genet 77:519-532, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Callier S: The use of racial categories in precision medicine research. Ethn Dis 29:651-658, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gannett L: Racism and human genome diversity research: The ethical limits of “population thinking”. Philos Sci 68:S479-S492, 2001 [DOI] [PubMed] [Google Scholar]
- 113.Mohsen H: Race and genetics: Somber history, troubled present. Yale J Biol Med 93:215-219, 2020 [PMC free article] [PubMed] [Google Scholar]
- 114.Adedokun BO, Olopade CO, Olopade OI: Building local capacity for genomics research in Africa: Recommendations from analysis of publications in sub-Saharan Africa from 2004 to 2013. Glob Health Action 9:31026, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rees CA, Ali M, Kisenge R, et al. : Where there is no local author: A network bibliometric analysis of authorship parasitism among research conducted in sub-Saharan Africa. BMJ Glob Health 6:e006982, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lett E, Adekunle D, McMurray P, et al. : Health equity tourism: Ravaging the justice landscape. J Med Syst 46:17, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ekezie W, Routen A, Denegri S, et al. : Patient and public involvement for ethnic minority research: An urgent need for improvement. J R Soc Med 114:347-350, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Domecq JP, Prutsky G, Elraiyah T, et al. : Patient engagement in research: A systematic review. BMC Health Serv Res 14:89, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Dawson S, Campbell SM, Giles SJ, et al. : Black and minority ethnic group involvement in health and social care research: A systematic review. Health Expect 21:3-22, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.King KF, Kolopack P, Merritt MW, et al. : Community engagement and the human infrastructure of global health research. BMC Med Ethics 15:84, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Staunton C, Tindana P, Hendricks M, et al. : Rules of engagement: Perspectives on stakeholder engagement for genomic biobanking research in South Africa. BMC Med Ethics 19:13, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data can be made available upon reasonable request.