Abstract
Objective
To investigate changes in FPs’ self-reported clinical practices after participation in a comprehensive 1-year cognitive behavioural therapy (CBT) training course.
Design
Cross-sectional study.
Setting
Norway.
Participants
Family physicians.
Main outcome measures
Impact of the CBT training course on FPs’ delivery of CBT to patients and their use of referral to specialized mental health care providers.
Results
Of the 217 FPs who had participated in the training course between 2009 and 2016, 124 completed the survey (response rate=57.1%); 99.2% of participating FPs reported using CBT tools daily in patient consultations, more than three-quarters reported changing the way they organized their workdays to accommodate CBT, and 75.0% reported using structured CBT consultations at least monthly after completing the course. The most common patient groups receiving structured CBT were those experiencing mild or moderate depression (22.8%), anxiety disorders (30.4%), or a combination of an anxiety disorder and depression (43.5%). The odds of making fewer referrals to specialized mental health care providers were 5.4 times higher among FPs who used Socratic questioning (P=.02), 4.7 times higher among those who provided consultation summaries (P=.01), and 3.3 times higher among those who had participated in a refresher course (P=.05).
Conclusion
Comprehensive training in CBT promotes the use of CBT tools and strategies in family practice. Further longitudinal research (ideally randomized controlled studies) on patient outcomes related to CBT provided in family practices is required.
Résumé
Objectif
Examiner les changements dans les pratiques cliniques tels que signalés par les MF après leur participation à un cours complet de formation d’une durée de 1 an en thérapie cognitivo-comportementale (TCC).
Type d’étude
Une étude transversale.
Contexte
La Norvège.
Participants
Des médecins de famille.
Principaux paramètres à l’étude
Les impacts d’un cours de formation en TCC sur l’offre par les MF d’une TCC à leurs patients et leur recours aux demandes de consultations spécialisées en santé mentale.
Résultats
Parmi les 217 MF qui ont participé au cours de formation entre 2009 et 2016, 124 ont répondu au sondage (taux de réponse=57,1 %); 99,2 % des MF répondants ont signalé utiliser des outils de la TCC tous les jours durant les consultations avec leurs patients, plus des 3 quarts ont dit avoir changé la façon dont ils organisent leur emploi du temps pour accommoder la prestation de la TCC et 75,0 % ont rapporté utiliser des consultations structurées en TCC au moins chaque mois après avoir terminé le cours. Les groupes de patients qui suivaient le plus souvent une TCC structurée éprouvaient une dépression de légère à modérée (22,8 %), des troubles d’anxiété (30,4 %) ou une combinaison d’anxiété et de dépression (43,5 %). La probabilité que les demandes de consultations en soins spécialisés en santé mentale soient moins nombreuses était 5,4 fois plus élevée chez les MF qui utilisaient le questionnement socratique (p=,02), 4,7 fois plus élevée chez ceux qui fournissaient des résumés de consultation (p=,01) et 3,3 fois plus élevée chez ceux qui avaient participé à un cours de rafraîchissement (p=,05).
Conclusion
Une formation complète en TCC favorise l’utilisation des outils et des stratégies de la TCC en pratique familiale. D’autres études longitudinales (idéalement des essais randomisés contrôlés) sur les issues, chez les patients, liées à la TCC offerte dans les pratiques familiales sont nécessaires.
There were approximately 5400 family physicians in Norway in 2021,1 and the average panel size of Norwegian FPs in 2016 was 1120 patients.2 A study published in 2015 found 12.2% of appointments with FPs in Norway had mental health problems cited as the main reason for the encounters, and 26.4% of appointments included a presentation of a mental health problem, mostly mild or moderate depression or anxiety disorders.3 This is consistent with data from other countries.4
Primary care physicians are well positioned to be able to intervene early in the course of mental health disorders and are gatekeepers to specialist services.5 Yet only a small fraction of patients with mental health disorders are offered adequate treatment,5,6 and FPs may lack the skills needed to treat patients with mental health problems.7 National Institute for Health and Care Excellence guidelines recommend cognitive behavioural therapy (CBT) for the most common mental health disorders.8 Cognitive behavioural therapy strategies and skills9-20 have been shown to be helpful in treating and managing patients with mental health disorders in primary care,8,21-23 and seems to be effective in treating patients with medically unexplained symptoms such as non-chronic low back pain and some somatic disorders (eg, irritable bowel syndrome).24-27 By employing CBT strategies and skills, FPs can help patients cultivate healthier and more realistic thinking and behaviour.28
While some Norwegian FPs have participated in brief (usually 2-day) CBT courses, these programs may not provide them with sufficient knowledge to deliver effective treatment.6,29,30 A Canadian study demonstrated that a 10-session course delivered as 2 hours per week showed promise in teaching complex CBT skills to mental health care providers.31 To provide more comprehensive training, in 2009 the Norwegian Medical Association and the Norwegian Association for Cognitive Behavioral Therapy introduced a 1-year CBT course, which more than 200 FPs have now completed.26
The course is structured around two 2-day and three 1-day workshops, totalling 7 full days over a year. The workshops include lectures, group work, and role play and cover an introduction to CBT, treatment of mild or moderate depression (as well as the most common anxiety disorders and medically unexplained physical symptoms), and special challenges encountered when using CBT. The content was designed to be of maximum relevance to FPs. Between workshops, physicians receive a reading list of relevant articles and participate in smaller evening counselling groups led by a trained peer supervisor using videos of consultations conducted by participating FPs. The course ends with a 2-hour written examination.
Participating FPs have stated 2 main reasons for participating in the course. The first reason is to treat their patients more effectively themselves, as supportive talk and medication alone do not appear to be sufficient, and specialized mental health care is not easily accessed.26 The second reason is to do something more active for patients than just “containing“ their problems, or serving in an unsatisfying “container” function, where FPs merely listen to their patients’ complaints without being able to develop an active treatment plan.9 Participants want to use CBT techniques to take a more active role in their patients’ treatment and create shared responsibilities for their recovery.
All FPs who complete the 1-year course are offered an annual 2-day follow-up course that addresses specific, more advanced CBT skills.
The purpose of this study was to understand family physicians’ experiences with a comprehensive 1-year CBT training course and how it affected their use of CBT, the kinds of consultations in which they used CBT, and their referral patterns to psychiatric specialist services. In addition, we wanted to learn about the types of patients being treated, the CBT strategies and skills used, the impact of CBT on FPs’ satisfaction, whether it changed their containing role, and their perspectives on whether this benefited their patients.
METHODS
Study design
The target group for the study was all FPs who had attended 1 of the 8 annual 1-year CBT courses between 2009 and 2016. In 2017 we sent them an introductory email inviting them to participate in our study. Those who agreed to participate received a second email with a link to the questionnaire, which was sent using the Questback program. Two additional email invitations were sent to those who had not responded to the first.
The questionnaire was based on a previous qualitative study26 and had been evaluated in a pilot study with 5 FPs with CBT training and adapted based on their feedback. It included questions about practice characteristics: sex, number of patients on their panel, number of FPs in the practice, type of practice funding, and whether the physician was a specialist in family medicine.
The CBT-related questions included the number of monthly structured CBT consultations FPs provided and their use of CBT strategies and skills, such as setting an agenda, using problem lists (ie, the patient makes a prioritized list of problems), using Socratic questioning (open neutral questioning), using the ABC (Activating event, Belief, Consequence) model,32 assigning a daily activity log, discussing the panic cycle (which describes the connection between triggers, emotions, bodily reactions, and catastrophic thinking), discussing the anxiety curve (the effect of trigger on anxiety), using case formulation (exploring the relationship between life experiences and anxiety development), providing psychoeducation, providing a summary at the end of the consultation, and assigning and reviewing homework.
Participants
A total of 217 FPs were contacted through the introductory email and follow-ups, yielding 124 participants (response rate=57.1%).
Outcome and statistical analysis
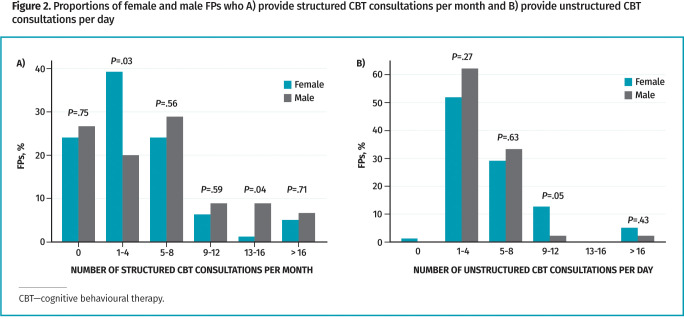
We used descriptive statistics to calculate frequencies and percentages. Chi-square tests were used to investigate associations among dichotomous variables. Binary responses were analyzed using logistic regression. Two steps preceded the modelling of these data. Univariate (unadjusted) logistic regression models were first fitted to the data. All covariates with P≤.20 and P≤.05 in the univariate analysis were then used to fit 2 separate adjusted logistic regression models. The models were compared using the Bayesian information criterion, which states that among nested models, the model with the smallest Bayesian information criterion is the better fit. To assess the accuracy of the final fitted logistic regression model, we plotted the sensitivity of the test against specificity (the false-positive rate) to produce the receiver operating characteristic curve (Figure 1), which had an area under the curve of 0.80. All analyses were performed using Stata SE 15, and the statistical significance level was set at P≤.05.
Figure 1.
Receiver operating characteristic curve for CBT referrals: The area under the curve suggests an 80% chance of correctly distinguishing FPs who made few referrals from those who made many (N=124).
RESULTS
Of the 124 participating FPs, 63.7% were female, compared with 42.3% in Norway’s overall FP population (Statistics Norway data, 2017), and 78.2% were family medicine specialists. Among the respondents, 22.6% had finished the course within the previous year, 32.3% within the previous 2 years, and 45.2% within 3 or more years prior to the survey.
Practice size and organization
Among participants, 55.6% had between 700 and 1199 patients, 42.7% had between 1200 and 1699 patients, and 1.6% had between 1700 and 2199 patients (Table 1). In terms of funding models, 92.7% of participants were self-employed and publicly funded (paid by per capita grant), 5.6% had fixed salaries from their municipalities, and 1.6% obtained their income from patient payments only (Table 1). This is similar to data for all Norwegian FPs (Statistics Norway data, 2017).
Table 1.
Characteristics of FPs who participated in the CBT training program and of their practices
| CHARACTERISTIC | FEMALE FPs (n=79) | MALE FPs (n=45) | TOTAL (N=124) |
|---|---|---|---|
| Percentage of respondents, % | 63.7 | 36.3 | 100.0 |
| Panel size, n (%) | |||
| • 700-1199 | 42 (53.2) | 27 (60.0) | 69 (55.6) |
| • 1200-1699 | 35 (44.3) | 18 (40.0) | 53 (42.7) |
| • 1700-2199 | 2 (2.5) | 0 (0.0) | 2 (1.6) |
| FPs in practice, n (%) | |||
| • 1 | 3 (3.8) | 1 (2.2) | 4 (3.2) |
| • 2-3 | 27 (34.2) | 6 (13.3) | 33 (26.6) |
| • 4-5 | 35 (44.3) | 21 (46.7) | 56 (45.2) |
| • 6-7 | 11 (13.9) | 11 (24.4) | 22 (17.7) |
| • >7 | 3 (3.8) | 6 (13.3) | 9 (7.3) |
| Funding of practice, n (%) | |||
| • Fixed salary | 4 (5.1) | 3 (6.7) | 7 (5.6) |
| • Per capita grant | 74 (93.7) | 41 (91.1) | 115 (92.7) |
| • Patient payment | 1 (1.3) | 1 (2.2) | 2 (1.6) |
| Family medicine specialization, n (%) | |||
| • Specialist | 61 (77.2) | 36 (80.0) | 97 (78.2) |
| • Non-specialist | 18 (22.8) | 9 (20.0) | 27 (21.8) |
| Recertifications, n (%) | |||
| • 0 | 10 (12.7) | 3 (6.7) | 13 (10.5) |
| • 1-3 | 34 (43.0) | 15 (33.3) | 49 (39.5) |
| • >3 | 35 (44.3) | 27 (60.0) | 62 (50.0) |
| Years since CBT course, n (%) | |||
| • 0-1 | 22 (27.8) | 6 (13.3) | 28 (22.6) |
| • 2-3 | 25 (31.6) | 15 (33.3) | 40 (32.3) |
| • >3 | 32 (40.5) | 24 (53.3) | 56 (45.2) |
CBT—cognitive behavioural therapy.
Patients
Participating FPs reported that the most common patient groups receiving structured CBT were those experiencing mild or moderate depression (22.8%), anxiety disorders (30.4%), or a combination of an anxiety disorder and depression (43.5%).
Structured and unstructured CBT consultations
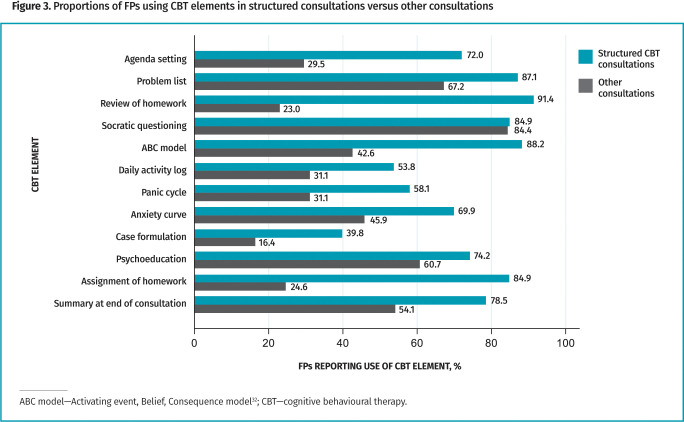
Among FP participants, 75.0% reported using structured CBT consultations at least monthly and 99.2% reported using CBT skills during regular patient visits daily. While the numbers of CBT consultations provided per month and per day did not show consistent differences based on FP sex, female FPs were more likely to provide only 1 to 4 structured CBT consultations per month (P=.03), male FPs were more likely to provide 13 to 16 structured CBT consultations per month (P=.04), and female FPs were more likely to provide 9 to 12 unstructured CBT consultations per day (P=.05). Male FPs were generally more likely than female FPs to provide higher numbers of structured CBT consultations (Figure 2).
Figure 2.
Proportions of female and male FPs who A) provide structured CBT consultations per month and B) provide unstructured CBT consultations per day
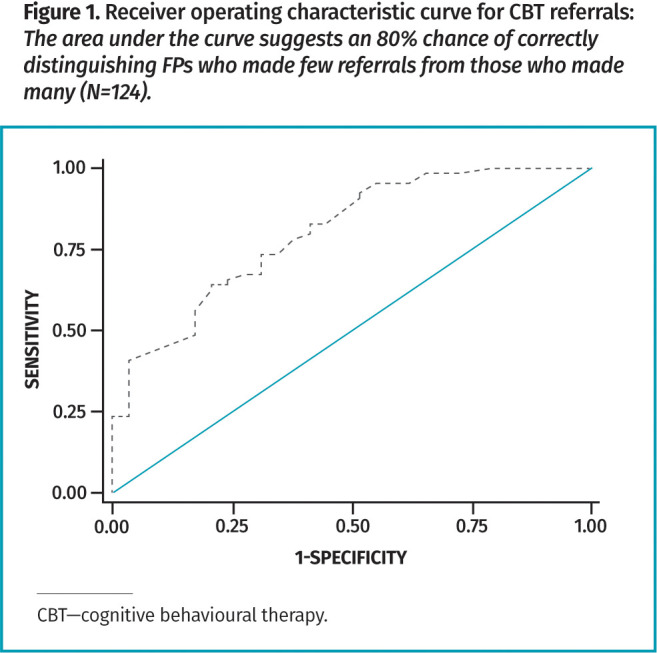
All the elements of CBT taught in the course were used in structured CBT consultations and in other types of visits (Figure 3).32 More than half of the FPs used problem lists, Socratic questioning, psychoeducation, and consultation summaries in all types of clinical consultations.
Figure 3.
Proportions of FPs using CBT elements in structured consultations versus other consultations
Changes in family physicians’ practices
Respondents described 3 important changes in the way they practised after having completed the course. Two-thirds of respondents said they tended to make fewer referrals to specialized mental health care, two-thirds said they were much less likely to take a passive “containing” role with patients, and three-quarters said they had changed their workweeks to include more dedicated time for CBT.
Factors associated with fewer referrals. Data from model 2 (Table 2)32 show factors significantly associated with fewer referrals to mental health professionals. The odds of making fewer referrals were 5.4 times higher among FPs who used Socratic questioning (P=.02), 4.7 times higher among those who made consultation summaries (P=.01), and 3.3 times higher among those who had participated in a CBT refresher course (P=.05).
Table 2.
Factors associated with fewer patient referrals to mental health professionals
| FACTOR | UNIVARIATE ANALYSIS OR (95% CI), P VALUE |
MODEL 1* (BIC=133.09) OR (95% CI), P VALUE |
MODEL 2* (BIC=124.32) OR (95% CI), P VALUE |
|---|---|---|---|
| Asking Socratic questions | 5.31 (1.59-17.72), P=.01 | 5.89 (1.32-26.25), P=.02 | 5.39 (1.27-22.84), P=.02 |
| Providing summaries at consultation end | 4.94 (1.74-14.07), P<.01 | 5.30 (1.40-20.08), P=.01 | 4.72 (1.37-16.32), P=.01 |
| Participating in a supervised education group | 2.60 (1.22-5.56), P=.01 | 1.09 (0.35-3.35), P=.88 | 1.06 (0.34-3.25), P=.92 |
| Having fixed time for CBT | 2.78 (1.21-6.37), P=.02 | 1.44 (0.45-4.58), P=.54 | 1.44 (0.46-4.47), P=.53 |
| Participating in a refresher course | 2.90 (1.34-6.26), P=.01 | 3.52 (1.04-11.86), P=.04 | 3.32 (1.01-10.95), P=.05 |
| Having an office colleague who uses CBT | 4.02 (1.42-11.35), P=.01 | 1.99 (0.50-7.89), P=.33 | 2.09 (0.56-7.89), P=.28 |
| Having economic incentives | 2.60 (1.10-6.13), P=.03 | 1.89 (0.54-6.67), P=.32 | 1.82 (0.53-6.30), P=.34 |
| Providing psychoeducation | 1.88 (0.71-4.95), P=.20 | 0.76 (0.21-2.81), P=.68 | NA |
| Assigning homework | 2.59 (0.81-8.24), P=.11 | 0.86 (0.16-4.49), P=.86 | NA |
| Setting an agenda | 0.75 (0.28-2.06), P=.58 | NA | NA |
| Using problem lists | 1.12 (0.31-4.07), P=.86 | NA | NA |
| Reviewing homework | 1.36 (0.30-6.13), P=.69 | NA | NA |
| Using the ABC model | 1.30 (0.35-4.85), P=.69 | NA | NA |
| Assigning a daily activity log | 1.33 (0.55-3.20), P=.52 | NA | NA |
| Discussing the panic cycle | 0.97 (0.40-2.36), P=.94 | NA | NA |
| Using the anxiety curve | 1.69 (0.66-4.29), P=.27 | NA | NA |
| Using a case formulation approach | 0.60 (0.25-1.46), P=.26 | NA | NA |
| Evaluation | 1.11 (0.46-2.70), P=.81 | NA | NA |
| Cooperating with local specialists | 1.32 (0.54-3.21), P=.54 | NA | NA |
| Having patients experience positive effects | 2.03 (0.61-6.72), P=.25 | NA | NA |
ABC—Activating event, Belief, Consequence32; BIC—Bayesian information criteria; CBT—cognitive behavioural therapy; NA—not applicable; OR—odds ratio.
Models 1 and 2 are based on variables with P≤.20 and P≤.05, respectively, from the univariate analysis. Model 2 was chosen for the analysis because of its smaller BIC estimate.
Factors associated with avoidance of “containing” role. We found no factors significantly associated with reducing the container function feeling among FPs in adjusted model 2 (Table 3).32 In the unadjusted univariate analysis, the use of Socratic questioning, psychoeducation, assignment of homework, participation in supervised education groups, having patients experience a positive effect, participation in a refresher course, and having an office colleague using CBT were statistically significantly associated with a higher probability of avoiding the containing role with patients.
Table 3.
Factors associated with FPs being less likely to occupy a container role (ie, listening to patients’ complaints without developing an active treatment plan)
| FACTOR | UNIVARIATE ANALYSIS OR (95% CI), P VALUE |
MODEL 1* (BIC=138.35) OR (95% CI), P VALUE |
MODEL 2* (BIC=125.49) OR (95% CI), P VALUE |
|---|---|---|---|
| Asking Socratic questions | 4.21 (1.30-13.67), P=.02 | 3.28 (0.74-14.47), P=.12 | 3.09 (0.79-12.10), P=.11 |
| Providing psychoeducation | 3.60 (1.35-9.63), P=.01 | 1.89 (0.57-6.29), P=.30 | 2.10 (0.66-6.75), P=.21 |
| Assigning homework | 4.21 (1.30-13.67), P=.02 | 2.16 (0.44-10.76), P=.35 | 2.58 (0.56-11.81), P=.22 |
| Participating in a supervised education group | 2.25 (1.05-4.82), P=.04 | 1.03 (0.32-3.28), P=.96 | 1.00 (0.32-3.09), P=.99 |
| Having patients experience positive effects | 7.50 (1.91-29.50), P<.01 | 2.23 (0.12-40.73), P=.59 | 2.44 (0.12-48.02), P=.56 |
| Participating in a refresher course | 2.44 (1.13-5.27), P=.02 | 2.85 (0.84-9.66), P=.09 | 2.62 (0.83-8.23), P=.10 |
| Having an office colleague who uses CBT | 2.81 (1.06-7.50), P=.04 | 3.64 (0.79-16.72), P=.10 | 4.11 (0.91-18.47), P=.07 |
| Assigning a daily activity log | 2.03 (0.82-5.02), P=.13 | 0.87 (0.27-2.76), P=.81 | NA |
| Using the anxiety curve | 1.98 (0.77-5.10), P=.16 | 1.29 (0.40-4.24), P=.67 | NA |
| Evaluation | 2.05 (0.83-5.08), P=.12 | 1.62 (0.51-5.16), P=.41 | NA |
| Setting an agenda | 1.44 (0.55-3.81), P=.46 | NA | NA |
| Using problem lists | 0.79 (0.20-3.18), P=.74 | NA | NA |
| Reviewing homework | 1.53 (0.34-6.88), P=.58 | NA | NA |
| Using the ABC model | 0.51 (0.10-2.52), P=.41 | NA | NA |
| Discussing the panic cycle | 1.43 (0.58-3.52), P=.44 | NA | NA |
| Using a case formulation approach | 1.18 (0.47-2.96), P=.73 | NA | NA |
| Providing summaries at the end of consultations | 1.06 (0.36-3.13), P=.91 | NA | NA |
| Cooperating with local specialists | 1.49 (0.60-3.71), P=.39 | NA | NA |
| Having fixed time for CBT | 1.49 (0.68-3.29), P=.32 | NA | NA |
| Having economic incentives | 1.63 (0.71-3.70), P=.25 | NA | NA |
ABC—Activating event, Belief, Consequence32; BIC—Bayesian information criteria; CBT—cognitive behavioural therapy; NA—not applicable; OR—odds ratio.
Models 1 and 2 are based on variables with P≤.20 and P≤.05, respectively, from the univariate analysis. Model 2 was chosen for the analysis because of its smaller BIC estimate.
Changes in workday organization. Most participants (75.5%) reported changing the way they organized their workdays in order to accommodate CBT. These changes included 12.9% reserving 1 day a week for CBT, 37.1% setting aside specific time for CBT consultations, and 58.4% doubling the time they allotted for CBT sessions.
DISCUSSION
Our findings indicate that following participation in a 1-year CBT course, FPs changed how they managed patients with mental and somatic health problems, and at least some participants were able to maintain this for more than 3 years after completion of the course. Family physicians in this study reported making fewer referrals to psychiatric specialist services and were less likely to serve in a containing role. Almost all FPs reported using CBT strategies and skills on a daily basis.
Although many FPs complete CBT courses of varying duration and teaching methods, the usefulness of these courses is seldom evaluated. A study by King et al from London, England, is one of the few that has addressed FPs’ experiences with CBT training in shorter courses.29 The researchers conducted a parallel group, cluster randomized controlled trial of a package of 4 half-days of brief CBT training and concluded that FPs need more training to acquire sufficient skills to help patients with depression. Our training is provided over 12 months and is more comprehensive than the course for FPs in London,29 which may explain the differences in our findings.
More than three-quarters of our respondents reported changing the organization of their workdays to accommodate CBT, suggesting they perceived CBT to be useful.
Although mild or moderate depression and anxiety disorders were the most common disorders treated with CBT, all respondents reported using CBT skills when treating other diagnoses such as pain, psychosomatic disorders, and medically unexplained symptoms.
Participants used most of the CBT skills taught in the courses, which they found easy to integrate within a primary care visit. The 4 most popular, used in more than 50% of all consultations, were problem lists, Socratic questioning, psychoeducation, and consultation summaries. These were also associated with reductions in the number of patient referrals and in family physicians’ reported feelings of “helplessness” when treating these patients.
It is also worth noting that FPs who participated in small follow-up group meetings with colleagues after the course to maintain their skills anecdotally reported making fewer referrals to specialist services, and they reported feeling more effective in managing patients’ problems.
Strengths and limitations
A 57.1% response rate after 2 reminders is considered acceptable for a Questback survey.33 The respondents’ population profile largely corresponded to the profile of FPs in Norway. New survey responses after each reminder round did not change the results and supported the notion that the selection of respondents was reasonably representative. It is possible, however, that respondents with more positive experiences of the CBT courses were overrepresented in our study.
Implications for clinical practice and for future research
Comprehensive CBT training promotes the use of CBT skills and strategies in primary care, and appears to facilitate change in the way physicians practice. The use of CBT may contribute to earlier interventions with people experiencing mental distress, reducing the burden of a person’s illness and fewer pressures on the second-line services. Our findings may also be helpful in planning family medicine residency training and continuing professional development offerings.
Conclusion
As a result of CBT training, referrals to specialized mental health services decreased and FPs were more satisfied and less frustrated in being able to provide more active and planned care for patients.
Acknowledgment
This article is dedicated to Dr Egil W. Martinsen, who passed away in 2023. The Norwegian Committee on Research in General Practice and the Norwegian Association of CBT funded the data collection for this research. Tor Carlsen, Senior Adviser in the Norwegian Medical Association, conducted the Questback survey.
Editor’s key points
▸ Cognitive behavioural therapy (CBT) strategies have been shown to be effective in treating and managing patients with mental health disorders in primary care, but brief training programs, such as 2-day courses, may not provide FPs with sufficient knowledge to deliver effective treatment.
▸ Following a year-long CBT training program in Norway that also provides annual refresher courses, 75.0% of participants reported providing structured CBT consultations at least monthly and 99.2% reported using CBT skills daily for regular patient visits. Mild or moderate depression and anxiety disorders were the most common disorders treated with CBT.
▸ The 4 most popular CBT tools, used in more than half of all consultations, were problem lists, Socratic questioning, psychoeducation, and consultation summaries. The CBT tools and strategies associated with FPs referring fewer patients to specialized mental health care providers were the use of Socratic questioning, the provision of consultation summaries, and participation in a refresher course on CBT.
Points de repère du rédacteur
▸ Il a été démontré que les stratégies de thérapie cognitivo-comportementale (TCC) sont efficaces dans le traitement et la prise en charge en soins primaires des patients atteints de troubles de santé mentale, mais des programmes de formation courts, comme d’une durée de 2 jours, pourraient ne pas fournir aux MF assez de connaissances pour offrir un traitement efficace.
▸ En Norvège, après un programme de formation en TCC d’une durée d’un an, qui offre aussi des cours de rafraîchissement annuels, 75,0 % des participants ont signalé offrir des consultations en TCC structurées au moins chaque mois, et 99,2 % ont dit se servir de leurs compétences en TCC chaque jour au cours des visites régulières de leurs patients. La dépression de légère à modérée et les troubles d’anxiété étaient les problèmes les plus souvent traités par la TCC.
▸ Les 4 outils de la TCC les plus populaires, utilisés dans plus de la moitié de toutes les consultations, étaient les listes de problèmes, le questionnement socratique, la psychoéducation et les résumés de consultation. Parmi les outils et les stratégies de la TCC qui sont associés à la réduction du nombre de demandes de consultations spécialisées en santé mentale figuraient le questionnement socratique, la fourniture de résumés de consultation et la participation à des cours de rafraîchissement sur la TCC.
Footnotes
Contributors
All authors of this paper have directly participated in the planning, execution, or analysis of the study; all have read and approved the final submitted version.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Physicians by specialty, 2021. Luxembourg: Eurostat; 2023. Available from: https://ec.europa.eu/eurostat/statistics-explained/indexphp?title=File:Physicians,_by_speciality,_2021_Health2023.png. Accessed 2023 Oct 7. [Google Scholar]
- 2.Sperre Saunes I, Tikkanen R, Osborn R, Mossialos E, Djordjevic A, Wharton GA. International health care system profiles: Norway. New York, NY: Commonwealth Fund; 2020. Available from: https://www.commonwealthfund.org/international-health-policy-center/countries/norway. Accessed 2023 Oct 7. [Google Scholar]
- 3.Bjørland E, Brekke M. What do patients bring up in consultations? An observational study in general practice. Scand J Prim Health Care 2015;33(3):206-11. Epub 2015 Jul 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finley CR, Chan DS, Garrison S, Korownyk C, Kolber MR, Campbell S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician 2018;64:832-40. [PMC free article] [PubMed] [Google Scholar]
- 5.Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 2007;370(9590):841-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Høifødt RS, Strøm C, Kolstrup N, Eisemann M, Waterloo K. Effectiveness of cognitive behavioural therapy in primary health care: a review. Fam Pract 2011;28(5):489-504. Epub 2011 May 9. [DOI] [PubMed] [Google Scholar]
- 7.Wittchen HU, Beesdo K, Bittner A, Goodwin RD. Depressive episodes—evidence for a causal role of primary anxiety disorders? Eur Psychiatry 2003;18(8):384-93. [DOI] [PubMed] [Google Scholar]
- 8.Depression in adults: treatment and management. London, UK: National Institute for Health and Care Excellence; 2022. Available from: https://www.nice.org.uk/guidance/ng222. Accessed 2023 Oct 8. [PubMed] [Google Scholar]
- 9.Dubord G. Part 1. Goalification. Can Fam Physician 2010;56:1312. [PMC free article] [PubMed] [Google Scholar]
- 10.Dubord G. Part 2. Scalification. Can Fam Physician 2011;57:54. [PMC free article] [PubMed] [Google Scholar]
- 11.Dubord G. Part 3. The reward chart. Can Fam Physician 2011;57:201. [PMC free article] [PubMed] [Google Scholar]
- 12.Dubord G. Part 4. Maturity coaching. Can Fam Physician 2011;57:323. [PMC free article] [PubMed] [Google Scholar]
- 13.Dubord G. Part 5. The mood pie. Can Fam Physician 2011;57:449. [PMC free article] [PubMed] [Google Scholar]
- 14.Dubord G. Part 6. The CUE question. Can Fam Physician 2011;57:573. [PMC free article] [PubMed] [Google Scholar]
- 15.Dubord G. Part 7. Pathogenic beliefs. Can Fam Physician 2011;57:689. [PMC free article] [PubMed] [Google Scholar]
- 16.Dubord G. Part 8. Cognitive illusions. Can Fam Physician 2011;57:799-800. [PMC free article] [PubMed] [Google Scholar]
- 17.Dubord G. Part 9. Thought records. Can Fam Physician 2011;57:913-4. [PMC free article] [PubMed] [Google Scholar]
- 18.Dubord G. Part 10. Persuasion. Can Fam Physician 2011;57:1027-9. [PMC free article] [PubMed] [Google Scholar]
- 19.Dubord G. Part 11. Viewpointing. Can Fam Physician 2011;57:1163. [PMC free article] [PubMed] [Google Scholar]
- 20.Dubord G. Part 12. Systematic desensitization. Can Fam Physician 2011;57:1299. [PMC free article] [PubMed] [Google Scholar]
- 21.Malins S, Kai J, Atha C, Avery A, Guo B, James M, et al. Cognitive behaviour therapy for long-term frequent attenders in primary care: a feasibility case series and treatment development study. Br J Gen Pract 2016;66(651):e729-36. Epub 2016 Jul 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ejeby K, Savitskij R, Ost LG, Ekbom A, Brandt L, Ramnerö J, et al. Randomized controlled trial of transdiagnostic group treatments for primary care patients with common mental disorders. Fam Pract 2014;31(3):273-80. Epub 2014 Mar 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wiebe E, Greiver M. Using cognitive behavioural therapy in practice. Qualitative study of family physicians’ experiences. Can Fam Physician 2005;51:992-3.e8. [PMC free article] [PubMed] [Google Scholar]
- 24.Everitt HA, Moss-Morris RE, Sibelli A, Tapp L, Coleman NS, Yardley L, et al. Management of irritable bowel syndrome in primary care: feasibility randomised controlled trial of mebeverine, methylcellulose, placebo and a patient self-management cognitive behavioural therapy website. (MIBS trial). BMC Gastroenterol 2010;10:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramond-Roquin A, Bouton C, Gobin-Tempereau AS, Airagnes G, Richard I, Roquelaure Y, et al. Interventions focusing on psychosocial risk factors for patients with non-chronic low back pain in primary care—a systematic review. Fam Pract 2014;31(4):379-88. Epub 2014 Mar 15. [DOI] [PubMed] [Google Scholar]
- 26.Aschim B, Lundevall S, Martinsen EW, Frich JC. General practitioners’ experiences using cognitive behavioural therapy in general practice: a qualitative study. Scand J Prim Health Care 2011;29(3):176-80. Epub 2011 Aug 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buffone A, Goldman RD. Cognitive-behavioural therapy for children with irritable bowel syndrome. Can Fam Physician 2021;67:905-7 (Eng), e323-5 (Fr). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beck JS. Cognitive behavior therapy: basics and beyond. 2nd ed. New York, NY: Guilford Press; 2011. [Google Scholar]
- 29.King M, Davidson O, Taylor F, Haines A, Sharp D, Turner R. Effectiveness of teaching general practitioners skills in brief cognitive behaviour therapy to treat patients with depression: randomised controlled trial. BMJ 2002;324(7343):947-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Twomey C, O’Reilly G, Byrne M. Effectiveness of cognitive behavioural therapy for anxiety and depression in primary care: a meta-analysis. Fam Pract 2015;32(1):3-15. Epub 2014 Sep 22. [DOI] [PubMed] [Google Scholar]
- 31.Lau MA, Dubord GM, Parikh SV. Design and feasibility of a new cognitive-behavioural therapy course using a longitudinal interactive format. Can J Psychiatry 2004;49(10):696-700. [DOI] [PubMed] [Google Scholar]
- 32.Ellis A. The revised ABC’s of rational-emotive therapy (RET). J Ration Emot Cogn Behav Ther 1991;9(3):139-72. [Google Scholar]
- 33.Fan W, Yan Z. Factors affecting response rates of the web survey: a systematic review. Comput Human Behav 2010;26(2):132-9. [Google Scholar]