Abstract
Solitary extramedullary plasmacytoma (SEP) of the nasal cavity is a rare neoplastic condition characterized by the localized proliferation of abnormal plasma cells. We present a case of SEP involving the nasal cavity in a 40-year-old male patient who presented with nasal obstruction and recurrent epistaxis. The diagnosis was confirmed through clinical evaluation, imaging studies, and histopathological examination of excised specimen. The patient underwent trans-nasal endoscopic excision of nasal mass without any adjuvant therapy, which resulted in successful local control. This case report highlights the clinical presentation, diagnostic approach, treatment modalities, and favourable prognosis associated with solitary extramedullary plasmacytoma of the nasal cavity.
Keywords: Plasmacytoma, Nasal mass, Epistaxis, Multiple myeloma, Angiofibroma
Introduction
Plasmacytoma is a rare tumour characterized by abnormal monoclonal proliferation of plasma cells. These can either be single or multiple and medullary or extra- medullary neoplasms. Solitary extra medullary plasmacytoma (EMP) constitutes 3% of all plasma cell tumours, most of which occur in the head and neck region, especially in the submucosal tissue of upper aerodigestive tract [1]. However, isolated plasmacytomas, especially those occurring in the nasal cavity, are extremely uncommon. We report a case of 40-year-old male presenting with progressive left sided nasal obstruction and spontaneous nasal bleeding. The mass was completely excised via trans-nasal endoscopic approach. Histopathological features were consistent with extramedullary plasmacytoma. Serum and urine electrophoresis and skeletal survey was performed to rule out multiple myeloma. Patient was relieved from symptoms with no evidence of recurrence till 6 months of follow-up. This report describes the diagnostic challenges and management of a rare tumour of nasal cavity.
Case Report
A 40-year-old male presented with one year history of recurrent epistaxis and nasal obstruction in the left nasal cavity. He reported no significant medical history or family history of haematological disorders. Diagnostic nasal endoscopy revealed a reddish smooth mass in the left nasal cavity arising from the lateral wall and extending posteriorly into the nasopharynx. [Fig. 1] On probing, the mass was firm with surface vascularity and bleeds on touch. A contrast-enhanced computed tomography (CT) scan of the paranasal sinuses demonstrated a well-defined soft tissue lesion of size 6.2 × 2.7 × 3 cm in left nasal cavity with no areas of internal calcifications or necrosis. The lesion was seen epicentered in posterior half of left nasal cavity in the region of middle turbinate extending posteriorly into nasopharynx and causing narrowing of the nasopharyngeal air passage. Superiorly, the lesion caused mild scalloping of the floor of ethmoids while abutting the palate inferiorly. No evidence of bony erosion or destruction was noted. The sphenopalatine foramen, pterygopalatine fossa and infratemporal fossa were found to be within normal limits. [Fig. 2] Based on above clinical findings, a working diagnosis of nasal angiofibroma was made and endoscopic excision of nasal mass was planned under general anaesthesia. Intra operatively the tumour was seen arising from free edge of middle turbinate with a broad vascular pedicle. Pedicle was cauterized with radiofrequency bipolar cautery forceps and mass was removed in toto. [Fig. 3] To prevent recurrence, partial middle turbinectomy was done. Keeping the possibility of diagnosis of angiofibroma in mind, further exploration of pterygopalatine fossa was done which was found to be uninvolved. Total duration of surgery was around 90 min with less than 30 ml blood loss. In post operative period, he recovered well and discharged on third post operative day. Histopathological examination revealed sheets of proliferation of plasma cells ranging from mature and immature morphology to plasma blasts pointing out to be plasma cell neoplasm favoring plasmacytoma. [Fig. 4] A comprehensive diagnostic workup was initiated to exclude systemic involvement. Renal and liver function tests were normal. Measurements of hematocrit, white blood cells, blood urea, serum creatinine, serum electrolytes, serum calcium, serum protein electrophoresis and immune electrophoresis were within normal limits. Urine analysis revealed absence of Bence Jones protein. Since the possibility of multiple myeloma was excluded, the diagnosis of solitary extramedullary plasmacytoma of the nasal cavity, was established. The case was discussed in multidisciplinary tumor clinic. Considering the patient’s localized disease and complete surgical excision, a decision of close follow up was made. Patient was followed up for 6 months postoperatively and no recurrence was detected in endoscopic examination.
Fig. 1.
Endoscopic image of left nasal cavity showing vascular mass (black asterix)
Fig. 2.
Contrast enhanced CT showing hyperintense mass in left nasal nasal cavity (denoted with red arrow)
Fig. 3.

Image showing excised nasal mass
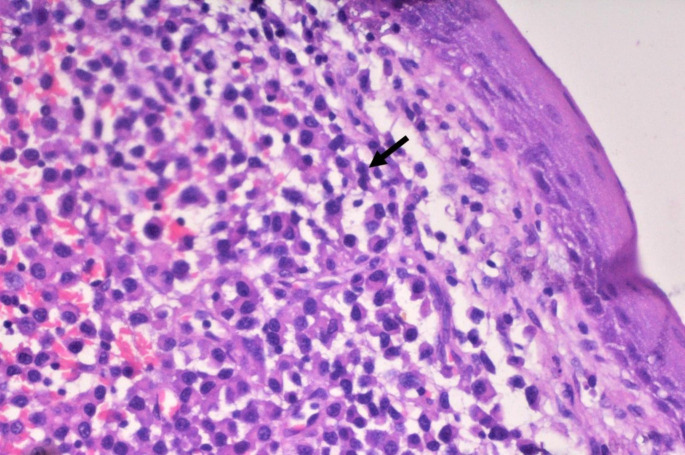
Fig. 4.
Histopathological section showing mucosa and sub epithelium with proliferation of plasma cells with round to oval eccentric nuclei and eosinophilic cytoplasm. (H&E; 40X). (black arrow)
Discussion
Plasmacytomas are rare tumours. They can present as solitary osteolytic lesion of bone or extramedullary plasmacytomas arising from lymph nodes, skin or mucosa. Extra medullary plasmacytoma of the soft tissues that could be either primary (without evidence of disease in other foci) or a part of a systemic manifestation of multiple myeloma [2]. Acquiring knowledge of extramedullary plasmacytoma is crucial for otolaryngologists, as the majority (80–90%) of cases are located in the head and neck [3].
Extramedullary plasmacytoma was first described by Schridde in 1905. The disease is estimated to have a global incidence of 1 case per 500,000 individuals [3]. The disease primarily affects individuals aged 40 and above, with over 95% of cases occurring in this age group. Typically, it manifests between the sixth and seventh decades of life and demonstrates a male predominance with 4:1 male to female ratio, particularly among Caucasians. Additionally, the disease is characterized by a gradual and slow progression.
Extramedullary plasmacytoma affecting head and neck are primarily confined to the mucosa of aerodigestive tract affecting mainly nasal cavity or paranasal sinuses (43.8%), followed by nasopharynx (18.3%), oropharynx (17.8%), and larynx (11.1%) [4]. When these tumours occupy nasal cavity, it needs to be differentiated from other commoner bleeding tumours like angiofibroma or haemangioma. Biopsy should not be the first choice for diagnosis in view of bleeding nature of these tumours.
Imaging modalities play a crucial role in the diagnosis, staging, and monitoring of extramedullary plasmacytoma (EMP). Contrast enhanced computed tomography and contrast enhanced magnetic resonance imaging are imaging modalities of choice for assessing bone and soft tissue involvement respectively.
The histopathological characteristics of extramedullary plasmacytoma are connective tissue extensively infiltrated by plasma cells, presenting as focal sheets, small islands, or plasmacytoid nodules. Immunohistochemical analysis differentiates monoclonal from polyclonal plasma cell groups with phenotyping the monoclonal plasma cell groups [5].
A negative bone marrow biopsy, the absence of lytic lesion in bone, and normal serum electrophoresis of immunoglobulins allows the possibility of a multiple myeloma to be excluded.
There is controversy in the published data regarding the treatment of extramedullary plasmacytoma in the head and neck [6, 7]. The choice between radiotherapy and surgery as standalone treatments is a matter of debate. Complete surgical resection of plasmacytoma, particularly in the upper respiratory tract is often challenging. As a result, radiotherapy is frequently the preferred initial treatment choice. Currently, there is no observed dose-response relationship, but the optimal radiation dose typically falls within the range of 40 to 50 Gy. However, if the tumor measures over 5 cm in diameter, a higher radiation dose might be necessary to ensure effective treatment [8]. Patients who undergo radiotherapy generally experience a low local recurrence rate of the tumour, typically less than 5%. Solitary plasmacytoma of the nasal cavity has a favourable prognosis with ten years survival rate of 70% [9].
Conclusion
Extramedullary plasmacytoma of the nasal cavity is a rare, aggressive tumour that should be considered in the differential diagnosis of nasal masses. Complete surgical excision with or without any adjuvant therapy remains the mainstay of management. However, long-term follow-up and monitoring are crucial, as they can potentially progress to multiple myeloma or recur locally.
Funding
None.
Disclaimer
Authors declare that the views expressed in this report are their own.
Disclosure of Potential Conflicts of Interest
The authors declare that they have no conflict of interest.
Research Involving Human Participants and/or Animals
Not applicable.
Informed Consent
Written Informed consent has been obtained from patient.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Belić B, Mitrović S, Arsenijević S, Erdevicki L, Stojanović J, Stojanović S, Stolić R (2013) Feb;70(2):221-4 Nasal septum extramedullary plasmacytoma. Vojnosanit Pregl. doi: 10.2298/vsp1302221b. PMID: 23607192 [DOI] [PubMed]
- 2.Shreif JA, Goumas PD, Mastronikolis N, Naxakis SS (2001) Jan;124(1):119 – 20 Extramedullary plasmacytoma of the nasal cavity. Otolaryngol Head Neck Surg. doi: 10.1067/mhn.2001.112480. PMID: 11228468 [DOI] [PubMed]
- 3.Corvo MA, Granato L, Ikeda F, de Próspero JD (2013 Apr) Extramedullary nasal plasmacytoma: literature review and a rare case report. Int Arch Otorhinolaryngol 17(2):213–217. 10.7162/S1809-97772013000200016PMID: 25992016; PMCID: PMC4423260 [DOI] [PMC free article] [PubMed]
- 4.Uppal HS, Harrison P (2001) Sep;115(9):745-6 Extramedullary plasmacytoma of the larynx presenting with upper airway obstruction in a patient with long-standing IgD myeloma. J Laryngol Otol. doi: 10.1258/0022215011908829. PMID: 11564308 [DOI] [PubMed]
- 5.Hu H, Hu X, Hu G, Li D, Cai J (2023) Diagnosis and management of extramedullary plasmacytoma in nasal cavity: Clinical experience and literature review. Medicine (Baltimore). Jan 13;102(2):e32647. doi: 10.1097/MD.0000000000032647. PMID: 36637932; PMCID: PMC9839280 [DOI] [PMC free article] [PubMed]
- 6.Wax MK, Yun KJ, Omar RA (1993) Nov;109(5):877 – 85 Extramedullary plasmacytomas of the head and neck. Otolaryngol Head Neck Surg. doi: 10.1177/019459989310900517. PMID: 8247569 [DOI] [PubMed]
- 7.Majumdar S, Raghavan U, Jones NS (2002) Nov;116(11):962-5 Solitary plasmacytoma and extramedullary plasmacytoma of the paranasal sinuses and soft palate. J Laryngol Otol. doi: 10.1258/00222150260369561. PMID: 12487681 [DOI] [PubMed]
- 8.Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, Samson D, Guidelines Working Group of the UK Myeloma Forum (2004) Mar;124(6):717 – 26 ; ; British Committee for Standards in Haematology; British Society for Haematology. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Br J Haematol. doi: 10.1111/j.1365-2141.2004.04834.x. PMID: 15009059 [DOI] [PubMed]
- 9.Sabattini E, Bacci F, Sagramoso C, Pileri SA (2010 Jun) WHO classification of tumours of haematopoietic and lymphoid tissues in 2008: an overview. Pathologica 102(3):83–87 PMID: 21171509 [PubMed]