Abstract
The use of cochlear implants (CI) may be associated with different complications, being extrusion of the device one of the most common. Reconstruction of the defect with a healthy and vascularized tissue is often required. We present two patients with a CI extrusion treated with a temporoparietal fascia flap.
Keywords: Temporoparietal fascia flap, Cochlear implants extrusion, Device extrusion, Management
Introduction
Cochlear implants (CI) are one of the latest treatments for sensorineural hearing loss [1]. Implantation surgery is generally safe and associated with different complications, being one of the most common implant extrusion [2, 3]. Reconstruction of the resulting defect with a healthy and vascularized tissue is often required [1, 4]. Among the reconstruction techniques we may find primary closure, local flaps as the temporoparietal fascia flap (TPFF) and free flaps [1, 4].
The TPFF is a versatile tool in head and neck reconstruction, being the thinnest and only fascial flap available in this area [1]. Its rich vascularity makes it an important tool for coverage of devitalized and chronically infected wounds [5]. Literature review shows few cases of the TPFF for this purpose. We present two cases in which a TPFF was raised to provide soft tissue coverage for the implants.
Case 1
A 44-year-old female carrier of a CI for 20 years with two episodes of device extrusion. The first extrusion was treated with a rotation flap that failed during the first year after surgery. Afterwards, a TPFF was used to cover the defect. As shown in Fig. 1, insetting of the TPFF ensured the implant´s coverage.
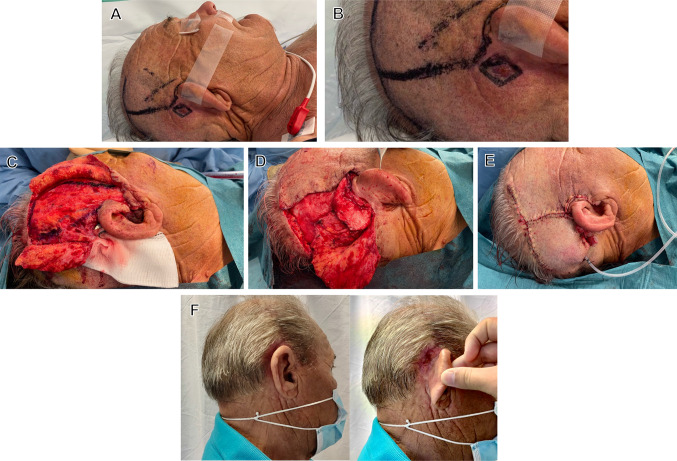
Fig. 1.
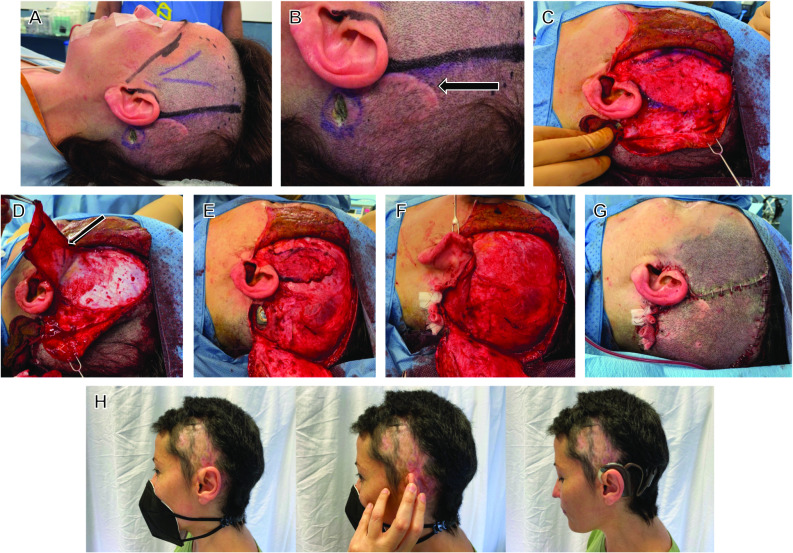
Cochlear implant extrusion and coverage surgery with a temporoparietal fascia flap. a Design of the skin incisions around the superficial temporal artery. b Zoom of the defect and scar of the previous rotation flap (arrow), c, d, e design of the thin TPFF and elevation with preservation of the vascular pedicle (arrow). f Insetting of the TPFF over the cochlear implant to prevent extrusion. g Skin closure and vacuum drain in place. h Three months post-operative result with external device in place and cochlear implant fully functional
During her 5 admission days after surgery, a hematoma was formed beneath the skin flaps. It was drained with no need of surgical reintervention. Superficial epidermolysis took place in the following weeks, we managed it with topical silver sulfadiazine. Complete wound healing was achieved 1 month after surgery, after which the patient was able to use the external device. Post-operative alopecia improved three months after surgery without specific treatment.
Case 2
A 74-year-old-male with a CI extrusion. Carrier of the implant for 4 years. A first extrusion, that happened 3 years after the implantation of the device, was treated with direct closure of the skin. A second extrusion, a month after the last surgery, was covered with a TPFF as shown in Fig. 2. After surgery, the patient had a hospital stay of one night with no immediate surgical complications.
Fig. 2.
Cochlear implant extrusion and coverage surgery with a temporoparietal fascia flap. a Design of the skin incisions around the superficial temporal artery. b Close look of the defect c, d design of the thin TPFF, elevation and insetting of the TPFF over the cochlear implant. e Skin closure and vacuum drain in place. f 3 month post-operative result
Discussion
Even though complications after CI implantation are infrequent (up to 10% cases), and some may be easily managed, they require immediate attention [6]. Implant extrusion, infection and skin flap necrosis are within the most common complications [2, 3]. While prevention of extrusion remains the best approach, when present, soft tissue coverage should be rapidly planned [4].
Despite the relative lack of reports in the literature about CI extrusion and infection, an aggressive treatment involving removal of the implant has been previously recommended [4, 7]. Current advice involves conservative measures including culture directed intravenous antibiotics and revision surgery of the scalp flap [7], basing the decision of device salvage on the infectious agent, the response to antibiotic treatment or the presence of biofilm [8].
Different techniques are available for treating CI extrusion. The most common methods include the use of well vascularized flaps to cover the defect. The TPFF is a great reconstruction method mainly because of its vascularity and flexibility. Other advantages include minimal site morbidity, high reliability, wide rotational arc, constant anatomy and versatility [4, 5]. Moreover, TPFF is a thin flap, and its use does not result in an excessive increment in the thickness of the scalp (which should not exceed 6 mm, in order to maintain the external device in place by magnetic attraction).
The temporoparietal fascia (TPF) lies immediately deep to the hair follicles being continuous with the galea superiorly and to the superficial musculoaponeurotic system inferiorly.It is mainly irrigated by the superficial temporal artery (STA), which will be the vessel that supplies irrigation to the flap and the pivot point for the rotation of the elevated fascia.
The first incision extends from the root of the helix to the superior temporal line [5]. Beforehand, the site is infiltrated with a lidocaine—epinephrine solution (dilution 1:1.000.000) for vasoconstriction and easier dissection. Anterior and posterior scalp flaps are carefully raised in the subdermal plane to avoid hair follicle damage.
Design of the fascia flap is based on the trajectory of the parietal branch of the STA. The flap is raised following the plane that separates the superficial and deep temporal fascia until the root of the helix is reached. The proximal region of the flap may be narrowed to approximately two centimeters, permitting pedicle preservation and a good rotation arc [5].
Before advancing the flap, thorough cleaning and careful debridement of the devitalized tissue surrounding the implant should take place. Once transposed, rotation of the scalp flaps allows complete closure of the defect. A suction drain is advised over the donor site.
Evolution of both cases was favorable, after surgery both were able to use the sound processing unit and the magnet on top of the flaps with the CI fully functional.
Conclusion
Many options are available for the reconstruction of wounds caused by CI extrusion. The anatomical proximity, pliable contour, reliability, rotational arc, minimal donor morbidity and high vascularization make the TPFF an excellent reconstruction choice for covering CI extrusion defects.
Author Contributions
All authors contributed to the manuscript conception and design. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
This is an observational study. The CEIm SESCAM ethics committee has confirmed that no ethical approval is required.
Informed Consent
Written informed consent was obtained from all individual participants included in this paper. The authors affirm that participants provided informed consent for the publication of the images in Fig. 1 and Fig. 2.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kang JK, Lee JS, Suh M, Lim GC, Shin MS, Yun BM. Reconstruction of a scalp defect due to cochlear implant device extrusion using a temporoparietal fascia flap and a split-thickness skin graft from the scalp. Arch Craniofacial Surg. 2019;20(5):319–323. doi: 10.7181/acfs.2019.00353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gatto A, Tofanelli M, Piccinato A, Antonio JK, Zucchini S, Achilli VP, et al. Cochlear implant surgery: How to fix receiver/stimulator avoiding extrusion. Ear Nose Throat J. 2019;9:014556131988062. doi: 10.1177/0145561319880625. [DOI] [PubMed] [Google Scholar]
- 3.Cohen NL, Hoffman RA. Complications of cochlear implant surgery in adults and children. Ann Otol Rhinol Laryngol. 1991;100(9 Pt 1):708–711. doi: 10.1177/000348949110000903. [DOI] [PubMed] [Google Scholar]
- 4.Karimnejad K, Akhter AS, Walen SG, Mikulec AA. The temporoparietal fascia flap for coverage of cochlear reimplantation following extrusion. Int J Pediatr Otorhinolaryngol. 2017;94:64–67. doi: 10.1016/j.ijporl.2017.01.020. [DOI] [PubMed] [Google Scholar]
- 5.Collar RM, Zopf D, Brown D, Fung K, Kim J. The versatility of the temporoparietal fascia flap in head and neck reconstruction. J Plast Reconstr Aesthet Surg JPRAS. 2012;65(2):141–148. doi: 10.1016/j.bjps.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 6.Lima Sánchez J, Berenguer B, Aránguez G, González Meli B, Marín Molina C, de Tomás P E. Extruded cochlear implant magnet covered with a temporoparietal fascial flap. A case report. Cirugia Pediatr Organo Of Soc Espanola Cirugia Pediatr. 2013;26(1):48–51. [PubMed] [Google Scholar]
- 7.Cunningham CD, Slattery WH, Luxford WM. Postoperative infection in cochlear implant patients. Otolaryngol Neck Surg. 2004;131(1):109–114. doi: 10.1016/j.otohns.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Geraghty M, Fagan P, Moisidis E. Management of cochlear implant device extrusion: case series and literature review. J Laryngol Otol. 2014;128(S2):S55–S58. doi: 10.1017/S002221511300323X. [DOI] [PubMed] [Google Scholar]