Abstract
Aim
This study aimed to assess the awareness and acceptance of COVID-19 vaccines and associated factors among pharmacy students in Zambia.
Materials and Methods
We conducted a cross-sectional study among 326 undergraduate pharmacy students in Lusaka, Zambia, from February to April 2021. Data were analysed using Stata version 16.1. Multivariable logistic regression was used to determine key factors influencing vaccine acceptance.
Results
Of the 326 participants, 98.8% were aware of the COVID-19 vaccines, but only 24.5% would accept vaccination. Compared to other religions, being of Christian faith was associated with reduced odds of awareness of the COVID-19 vaccine (aOR=0.01, 95% CI: 0.01–0.20). Conversely, factors associated with vaccine acceptance were being male, single and unemployed. Compared to females, male respondents were 86% more likely to accept the vaccine if it was made available (aOR=1.86, 95% CI: 1.10–3.14). In addition, unmarried respondents were 2.65 times as likely to accept vaccination than married respondents (aOR=2.65, 95% CI: 1.06–6.63). Conversely, unemployed respondents were less likely to accept vaccination than their employed counterparts (aOR=0.32, 95% CI: 0.16–0.46). Barriers to the acceptability of the vaccine were possible side effects (78.5%) and scepticism about its effectiveness (10.2%).
Conclusion
There was significant vaccine hesitancy toward COVID-19 vaccines among Zambian pharmacy students despite their awareness of the vaccines. Health authorities must work collaboratively with training institutions to mitigate vaccine hesitancy, especially with healthcare students being a key part of the future healthcare workforce overseeing disease prevention strategies.
Keywords: acceptance, acceptability, awareness, COVID-19 vaccines, pharmacy students
Background
The novel coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in late 2019 in Wuhan City, China1. Subsequently, COVID-19 was declared a pandemic by the World Health Organization (WHO) on 11 March 20202 and spread rapidly across the globe. COVID-19 combined with the introduction of lockdown and other measures brought appreciable socioeconomic disruption and associated costs alongside increasing morbidity and mortality3–5.
Despite the initial containment of the pandemic in several countries through lockdown and other measures including social distancing, the mandatory wearing of personal protective equipment (PPE), promoting regular hand hygiene, closure of borders and mass testing6–9, infection rates continued to increase10. We have also seen a rise in morbidity and mortality from other diseases, including non-communicable diseases (NCDs), due to lockdown and other measures11–13. There has also been an appreciable increase in antibiotic prescribing and dispensing for patients with COVID-19 despite only a limited number of patients having underlying bacterial infections driving up antimicrobial resistance (AMR) rates14–17. However, this is not universal, with limited increases in the self-purchasing of antibiotics to treat COVID 19 among African countries with trained pharmacists14,18.
The concerns with the unintended consequences of COVID-19, coupled with the socioeconomic consequences of COVID 19 along with growing morbidity and mortality rates, have resulted in pharmaceutical companies, governments and funding agencies worldwide investing considerable efforts and resources in accelerating the research and development of vaccines as a viable future prevention measure once the gene sequence became known19–22. As of 16 June 2021, there were 287 vaccine candidates, 185 in the pre-clinical phase and 102 in the clinical phase23. In addition, 22 candidates had been submitted to the WHO for emergency use validation, of which seven (7) had been approved by 16 June 202124. This builds on 291 candidates being available as of 26 January 2021 in the tracker organised by the London School of Hygiene and Tropical Medicine25. However, despite appreciable progress with vaccination programmes, there are still significant challenges, especially in high-income countries. A key challenge is the uncertainty regarding the acceptance of COVID-19 vaccination among healthcare workers and the public across countries certainly during the early stages of the vaccine roll-out26–28, with vaccine hesitancy fuelled by social media activities29–32. For any immunisation program to be successful, acceptance of the vaccine is critical and mirrors the general awareness of disease risk, vaccine attitudes and demand for vaccination within the general population14,33,34.
Vaccine hesitancy is principally defined as a delay in acceptance or refusal of vaccination despite the availability of vaccination services35–38. To date, variable vaccine hesitancy rates have been reported regarding the acceptance of the COVID-19 vaccine across countries and populations38–41. In a systematic review, Sallam (2021) found low acceptance rates in Kuwait (23.6%) and Jordan (28.4%) versus appreciably higher acceptance rates in China (91.3%), Indonesia (93.3%) and Malaysia (94.3%)41. Lazarus et al (2021) also found variable acceptance rates40. Other authors have also documented low acceptance rates in Egypt (21%)42, the Democratic Republic of Congo (27.7%)26, Uganda (37.3%)43 and Jordan (37.4%)44. This is likely linked to considerable misinformation regarding the vaccine, including data on its effectiveness and safety fuelled, as mentioned, via social media and other activities, including conspiracy theories27,29–31. This is similar to the misinformation about potential treatments for COVID-19, such as hydroxychloroquine, ivermectin and remdesivir, with robust trials showing limited benefit in reality alongside potentially increased morbidity and mortality8,45–49.
The morbidity and mortality from COVID-19 appear lower among African countries than in higher-income countries certainly initially with proactive measures introduced across Africa6. In April 2021, the authorities in Zambia administered the first doses of the Oxford-AstraZeneca® COVID-19 vaccine. As of 21 December 2021, there had been 219,023 confirmed cases of COVID-19 with 3,685 deaths and at least 1,469,501 vaccine doses had been administered50. It is hoped that the nationwide programme would accelerate with the approval of at least five vaccines (AstraZeneca Covishield, AZD 12225-Korea AstraZeneca, Johnson & Johnson, Pfizer/BioNTech, and Sinopharm) in Zambia, building on the WHO's Emergency Use listing of the vaccines51. However, given the concerns with hesitancy surrounding the COVID-19 vaccine across countries, including African countries32,41, we believed there was an urgent need to describe and understand vaccine awareness and acceptance levels as well as associated factors in a key African country such as Zambia.
Consequently, this study aimed to assess the awareness and acceptance of COVID-19 vaccines and associated factors among pharmacy students in Zambia. We started with undergraduate pharmacy students as they are the future pharmacists and custodians of medicines and vaccines. As future pharmacists, they will be involved in disease prevention, provision of potential treatments as well as increasing vaccine uptake52–54. In addition, we were aware that there had been concerns with COVID-19 vaccines among University personnel in Africa as well as in other low- and middle-income countries (LMICs)28,39,43,55,56. The findings can help develop a working hypothesis for more extensive interventions to improve future vaccination rates in Zambia, building on experiences across countries.
Materials and Methods
Study design, setting and population
We conducted an online cross-sectional study using a self-administered questionnaire to ensure compliance with current public health guidelines such as social distancing and minimal person-to-person interactions. We invited 632 undergraduate pharmacy students enrolled in the pharmacy degree programme from the University of Zambia (UNZA), Lusaka Apex Medical University (LAMU) and Mulungushi University (MU) to participate.
Many students were invited via social media profiles (Facebook) and messaging applications (WhatsApp). Consequently, the online questionnaire was made available on Google Forms from early February through to 25 April 2021 when Zambia just started the administration of the Oxford/AstraZeneca vaccine. Questionnaires were sent to eligible students identified by university registers and student associations. To increase participation, reminders were sent twice a week for those who did not respond for three consecutive weeks.
Sample size calculation
A representative sample size of the population was calculated using Yamane's formula similar to another study involving pharmacy students in Zambia57. After extrapolating to a finite population of 632 undergraduate pharmacy students, a margin of error of 5% and an anticipated 10% loss or non-response, a minimum sample size of 259 was obtained. This resulted in a minimum of 259 study participants.
Data Collection Tool
A validated questionnaire was adapted from recent studies regarding COVID-19 vaccine acceptability across countries26,42,58. The questionnaire was first circulated to experts from the University of Zambia and Copperbelt University to allow for content and face validation.
The modified questionnaire was subsequently pre-tested on 20 pharmacy students at UNZA, who were later excluded from the principal study. We subsequently added questions on awareness and removed the questions on attitude and perceptions as our study did not focus on these two aspects.
The adapted questionnaire was used to collect data on socio-demographic characteristics (Section A), awareness (Section B) and acceptability (Section C) of COVID-19 vaccines among pharmacy students in Zambia. Demographic variables included: religion measured as Christian, Islam and others (minor religions in Zambia such as Hinduism and Buddhism), and employment status as pharmacy students in Zambia comprise those in employment as pharmacy technologists (holders of a diploma) and those that come directly into the degree programmes from high school. In addition, data on gender, residential area (rural-urban, rural and urban), heard of the COVID-19 vaccine (yes/no), source of information (Friends/Family, Health workers, Internet, Radio and Television), year of study (second, third, fourth and fifth) and age (number of years from the date of last birthday) were also collected. In sections A and B, the primary and secondary variables of interest were related to the statements, “If the COVID-19 vaccine was made available, would you accept to be vaccinated.” And “Have you heard of the COVID-19 vaccine?”, respectively.
Data Analysis
Stata/IC version 16.1 (Stata Corp., College Station, Texas, USA) was used for statistical analysis. Descriptive analysis was done on the socio-demographic characteristics of participants. Categorical variables were expressed as frequencies and percentages. The association between demographic variables and outcomes of interest was done using the Pearson Chi-square test or Fisher's exact test.
The logistic regression model was used to estimate the odds ratios with respective 95% confidence intervals (95% CI) for the predictor variables. Bivariate logistic regression was fitted to obtain crude estimates for the two outcomes, awareness (yes=1, no=0) and acceptability (yes=1, no=0). Subsequently, separate multivariable logistic regression models were fitted for the two outcomes, including only variables with a p<0.20 from the bivariate analysis to adjust for confounders. The multivariable regression models were fitted using stepwise regression and backward elimination algorithms with a liberal p-value for exclusion (p=0.10). Interactions were investigated and none was found to approach statistical significance. Hosmer-Lemeshow goodness-of-fit test was used to assess the predictive ability of the model. All statistical tests were undertaken at a 5% significance level and 95% confidence level.
Results
Socio-demographic characteristics of participants
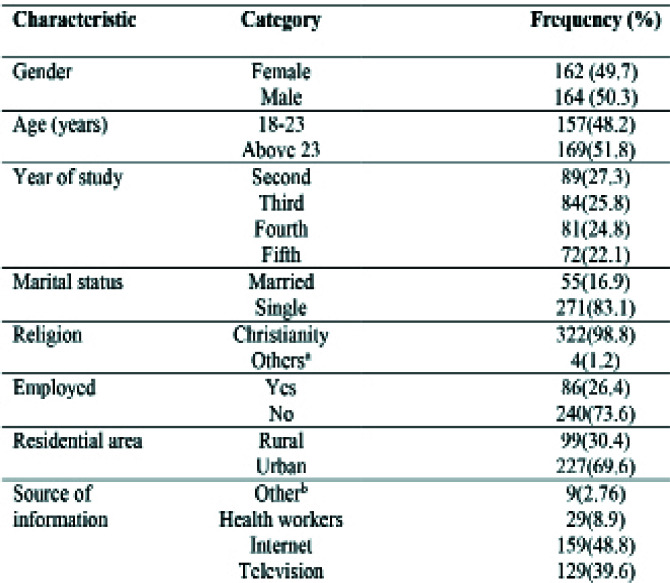
Three hundred and twenty-six (326) undergraduate pharmacy students participated and completed the questionnaire, including 164 (50.3%) males. The majority, 169 (51.8%), were older than 23 years, 89 (27.3%) were in their second year of study, and 271(83.1%) were single. Nearly everyone, i.e. 98.8% was of Christian faith. Approximately 73.6% of the participants were not employed, and 69.6% resided in urban areas. The socio-demographic characteristics of respondents are shown in Table 1.
Table 1.
Socio-demographic characteristics, N=326
aIncludes Islam, Hindu and minor religions in Zambia; bIncludes friends/family and radio
Key: a= Fisher's exact test, b=Pearson Chi-square test
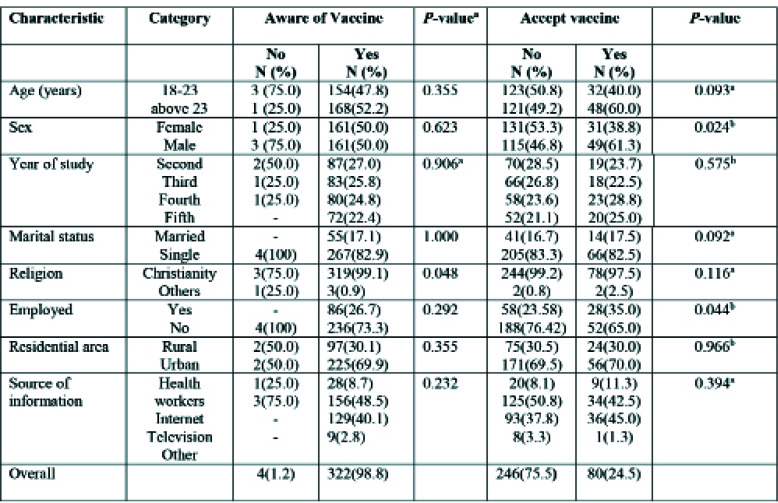
Results of the univariable analysis of factors associated with awareness and acceptability of the COVID-19 vaccine are shown in Table 2. Overall, awareness of vaccines was reported in nearly all respondents (98.8%); however, only approximately a quarter of participants (24.5%) would accept the vaccine if it was made available. Of those aware of the vaccine, slightly above half, i.e., 52.2%, were 23 years of age or older, and 69.9% resided in urban areas. In addition, over two-thirds (82.9%) were single and 73.3% were unemployed. The majority, 27.0% and 25.8% respectively were in the second and third year of study, and nearly half (48.5%) of surveyed students sourced information regarding the COVID-19 vaccines from the internet.
Table 2.
Socio-demographic characteristics of the participants according to their awareness and acceptance of COVID-19 vaccines
Key: a= Fisher's exact test, b=Pearson Chi-square test
Conversely, among the respondents who would accept vaccines if it was made available, approximately three-in-five (61.3%) were males, 60.0% older than 23 years, 28.8% were in the fourth year of study, 82.5% were single, 70.0% resided in urban areas and 45.0% sourced information about COVID-19 vaccines from the television. The gender of the respondents and employment were significantly associated with acceptance of the vaccine (p=0.024) and (p=0.044), respectively.
On the other hand, religion was associated with awareness of the vaccine (p=0.048).
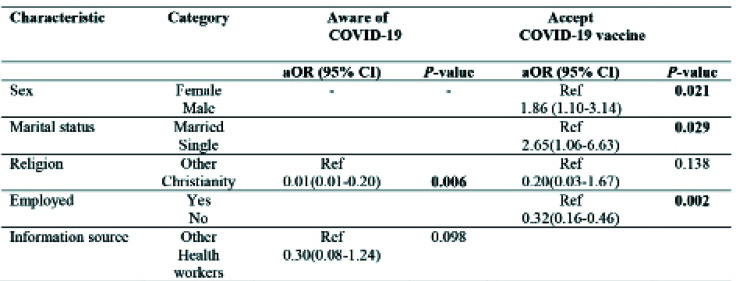
Factors influencing awareness and acceptability of COVID-19 vaccines
Factors associated with the awareness and acceptability of the COVID-19 vaccine are shown in Table 3. Compared to other religions, being of Christian faith was associated with reduced odds of awareness of the COVID-19 vaccination (aOR=0.01, 95% CI: 0.01–0.20), adjusting for the source of information. Conversely, factors associated with vaccine acceptance were male sex, being single and unemployed. Compared to females, male respondents were 86% more likely to accept the COVID-19 vaccine if it was made available (aOR=1.86, 95% CI: 1.10–3.14).
Table 3.
Adjusted Multivariable logistic regression of factors associated with awareness and acceptability of COVID-19 vaccines
Key: aOR-adjusted odds ratios, 95% CI-95% confidence intervals, Students of pharmacy with a diploma are in employment except for direct entrants into the degree program. In category others, we included all minor religions in Zambia (i.e., Islam, Hinduism, Buddhism etc). We measured acceptability by asking respondents to indicate whether they would accept the COVID-19 vaccine if it was made available (yes/no), awareness was measured by asking respondents if they were aware of the COVID-19 vaccine (yes/no)
In addition, unmarried respondents were 2.65 times as likely to accept vaccination than married respondents (aOR=2.65, 95% CI: 1.06–6.63). Conversely, unemployed respondents were less likely to accept vaccination than their employed counterparts (aOR=0.32, 95% CI: 0.16–0.46).
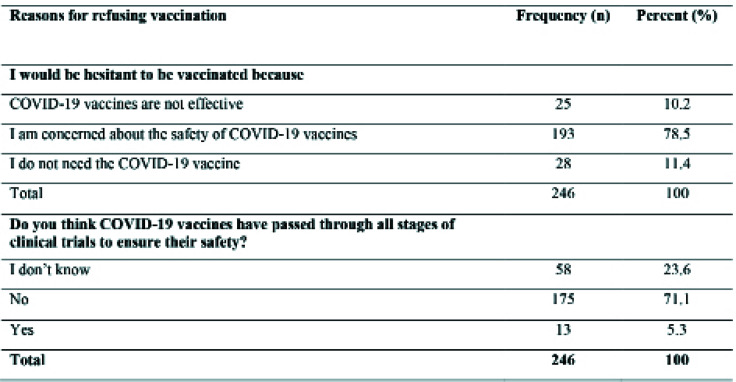
Reasons for student's refusal to be vaccinated against COVID-19
Out of the 246 participants who were hesitant to receive the COVID-19 vaccine, the majority (78.5%) were concerned about the possible adverse effects of COVID-19 vaccines (Table 4). Similarly, 71.1% felt that the COVID-19 vaccines did not pass through all the stages of the clinical trial process, which led to concerns about their safety.
Table 4.
Hesitancy against COVID-19 vaccination among pharmacy students
Discussion
To the best of our knowledge, we believe this is the first study conducted in Zambia to assess the awareness and acceptance of COVID-19 vaccines and associated factors among pharmacy students in Zambia. Despite 98.8% of the respondents being aware of the COVID-19 vaccine, only 24.5% were likely to accept the vaccine if it was made available. Factors associated with vaccine acceptability included being male, employed and unmarried whereas being of the Christian faith was associated with reduced awareness of the vaccine.
Encouragingly, we found a high awareness rate of 98.8% for COVID-19 vaccines, similar to medical students in Uganda (98.3%)43 and the Democratic Republic of Congo (99.3%)26. This could be attributed to awareness campaigns and information available on news and social media, with the students reporting the internet (48.8%), television (39.6%) and healthcare workers HCWs (8.9%) as their main sources of information about COVID-19 vaccines. This is different though from a study that was undertaken in the United States (US) where the main sources of information leading to increased awareness of the COVID-19 vaccines were the health agencies in addition to mass media59.
However, the low acceptance rate for the COVID-19 vaccine at 24.5% among our pharmacy undergraduates is a concern. The current acceptance rate is less but still comparable to low rates seen among the general population (33.4%)60 and caregivers (47%)61 in Zambia. These low rates require urgent attention if Zambia is to immunise the majority of its population to reduce the impact of future waves62. The misinformation and beliefs about the COVID-19 vaccine have contributed to increased vaccine hesitancy among the Zambian population60,62 similar to other populations31. The findings of the current study are similar to low acceptance rates of 29.4% reported among the public in Jordan, Kuwait and Saudi Arabia27, 34.9% among university students in Jordan28 and 37.3% among medical students in Uganda43. This compares with appreciably higher rates of 73% to 77% among medical students in the US63,64, 76.3% among college students in China58, 86.1% among university students in Italy65, and 91.99% among medical students in Poland66. Poland's high acceptability may well be because the medical students in the study were fearful of contracting the virus and spreading it to their family and friends66. We have also seen variable vaccine acceptance rates among HCWs and others across countries. These range from low acceptance rates of 21% in Egypt42, 23.4% in Taiwan67, and 27.7% in the Democratic Republic of Congo26, similar to the students in our study, up to 55% in Russia40, 71% in South Africa40, 78.1% in Israel41, 78.5% in Greece68 and nearly 90% in China40.
The current study found that religion was associated with vaccine awareness and hesitancy. This is similar to other published studies that have reported vaccine awareness and acceptance is influenced by religious beliefs69,70. A study among US medical students reported good attitudes and awareness but low vaccine acceptance in which the participants felt that prayers were more beneficial in preventing COVID-19 than vaccines63. Similar to our findings, a study conducted in Zimbabwe also reported low vaccine awareness and acceptance among Christians of the Apostolic church because they believed in the powers of prayers to protect them from the disease71. Consequently, it is imperative to address spiritual and religious beliefs when developing interventions that promote vaccine awareness, acceptance and uptake. This should include close working with religious leaders as well as physicians and other healthcare workers with considerable influence within religious organisations.
In our study, those who were married and not in employment were less likely to accept the COVID-19 vaccine, while male students were more likely to accept the vaccine. Other studies have also reported similar gender differences in hesitancy rates regarding the COVID-19 vaccine and other vaccines26,40,41,72,73. This may be due to male participants having a high-risk perception of diseases than females; consequently, a greater willingness to be vaccinated. In addition, the higher vaccine acceptance rate among employed personnel may be due to their employers' recommendation to be vaccinated.
Vaccine safety and effectiveness were the main reasons for vaccine hesitancy among our students, similar to students and HCWs in other countries39,42,43,74. This includes concerns that the COVID-19 vaccines have not passed through all key clinical trial stages to assure safety and effectiveness. The higher rate of vaccine hesitancy seen in our study could also potentially be attributed to adverse reports on social media, conspiracy beliefs and a lack of awareness campaigns generally concerning the effectiveness and safety of the different COVID-19 vaccines29,31,43,63,66. Interestingly, our recent findings in Zambia are similar to an earlier study in Zambia, which documented fear of adverse effects, lack of information on the benefits of vaccines, and other beliefs, including traditional beliefs, as barriers to accessing vaccines75. Consequently, there is a need for health authorities to provide adequate information on the safety and effectiveness of vaccines, which can be taken forward by community pharmacists and others when discussing prevention with patients including administering vaccines when available18,53,76. Besides, increased health education must be provided through government agencies and HCWs to address misinformation and myths regarding COVID-19 vaccines. The low vaccine acceptance among pharmacy students, the future HCWs, is very worrying and requires urgent attention. Because of this, we recommend that senior academics should urgently provide adequate sensitisation and educational programs to university students on COVID-19 vaccines. These programs should also be implemented among HCWs and the general population.
Strengths of the study
This is the first study to assess the awareness and acceptance of COVID-19 vaccines and associated factors among pharmacy students in Zambia and it has highlighted the need to improve information on the benefits of vaccines among university students. Further, the study explored the factors that influence vaccination against COVID-19 and the reasons for vaccine hesitancy. This is important as it can help the government, the Ministry of Health and other stakeholders on the cardinal information to focus on when implementing vaccination programs.
Limitations of the study
We are aware this study has some limitations. Since the study was limited to pharmacy undergraduate students in Zambia, its results cannot be generalised to students of other healthcare and non-healthcare programmes. In addition, concerns about high numbers of Christians and minority unmarried participants could have affected our findings. Despite this, we believe the findings are robust providing direction for the future.
Conclusion
This study showed a high level of awareness about COVID-19 vaccines among Zambian pharmacy students. In contrast, their acceptability of receiving the vaccine if made available was lower than regional estimates. Consequently, stakeholders in the healthcare sector need to develop strategies to reassure the populace of the safety and efficacy as well as the success story of COVID-19 vaccination. We also believe there is a critical role for the educators in Pharmacy and Medical schools in Zambia and across Africa to reduce the level of misinformation regarding COVID-19 vaccines, similar to general myths surrounding COVID-19 and its treatment. We will be following this up especially given the pivotal role of community pharmacists during current and future pandemics.
Acknowledgements
The authors are grateful to the University of Zambia for providing access to many articles used in this pilot study. We would like to acknowledge the pharmacy students in Zambia for taking part in this study. SM would like to acknowledge that some of his time dedicated to conducting research is supported by the University of Zambia in collaboration with the Africa Centre of Excellence for Infectious Diseases of Humans and Animals (ACEIDHA). MM would like to acknowledge that some of his time is supported by the UNC-UNZA-Wits Partnership for HIV and Women's Reproductive Health which is funded by the U.S. National Institute's Health (grant number: D43 TW010558).
Author contributions
SM conceptualised and designed the study. SM (Stewart Mudenda), MK, WM, VD, MCH, RLM and CNH participated in the acquisition of data. SM (Stewart Mudenda), MM, MK, VD, MC and RNO conducted data analysis and interpretation. All authors (SM (Stewart Mudenda), MM, CNH, JCM, JF, MK, ACK, SM (Sody Musaka), RNO, VD, MC, RLM, WM, BAW and BG) participated in the draft of the initial manuscript. All authors participated in reviewing the intellectual content of the manuscript. All authors approved the final version of the manuscript. All authors are accountable for any questions regarding the integrity and accuracy of this work.
Financial & conflict of interest disclosures
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. All the authors declare no competing interests. This study did not receive any medical writing or editorial support.
Ethical conduct of research
The study protocol was approved by the University of Zambia Health Sciences Research Ethics Committee (UNZAHSREC) and the Zambia National Health Research Authority (NHRA). The study was approved under the protocol ID: 20190217024, IORG no: 0009227, IRB no: 00011000. All participants were aware of the objectives of the study and provided informed consent by reading and responding to the online survey.
Data availability
The data that support the findings of this study are available from the corresponding authors, upon reasonable request.
References
- 1.Morens DM, Breman JG, Calisher CH, Doherty PC, Hahn BH, Keusch GT, et al. The Origin of COVID-19 and Why It Matters. Am J Trop Med Hyg. 2020;103(3):955–959. doi: 10.4269/ajtmh.20-0849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta bio-medica: Atenei Parmensis. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rasul G, Nepal AK, Hussain A, Maharjan A, Joshi S, Lama A, et al. Socioeconomic Implications of COVID-19 Pandemic in South Asia: Emerging Risks and Growing Challenges. Frontiers in sociology. 2021;6:629693. doi: 10.3389/fsoc.2021.629693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socioeconomic implications of the coronavirus pandemic (COVID-19): A review. International journal of surgery. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonotti M, Zech ST. The Human, Economic, Social, and Political Costs of COVID-19. Recovering Civility during COVID-19. 2021:1–36. [Google Scholar]
- 6.Ogunleye OO, Basu D, Mueller D, Sneddon J, Seaton RA, Yinka-Ogunleye AF, et al. Response to the Novel Corona Virus (COVID-19) Pandemic Across Africa: Successes, Challenges, and Implications for the Future. Frontiers in pharmacology. 2020;11:1205. doi: 10.3389/fphar.2020.01205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talic S, Shah S, Wild H, Gasevic D, Maharaj A, Ademi Z, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis. BMJ. 2021;17(375):e068302. doi: 10.1136/bmj-2021-068302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sefah I, Ogunleye O, Essah D, Opanga S, Rizvi N, Wamaitha A, et al. Rapid assessment of the potential paucity and price increases for suggested medicines and protection equipment for COVID-19 across developing countries with a particular focus on Africa and the implications. Frontiers in pharmacology. 2021;11:2055. doi: 10.3389/fphar.2020.588106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Afriyie DK, Asare GA, Amponsah SK, Godman B. COVID-19 pandemic in resource-poor countries: challenges, experiences and opportunities in Ghana. Journal of infection in developing countries. 2020;14(8):838–843. doi: 10.3855/jidc.12909. [DOI] [PubMed] [Google Scholar]
- 10.WHO, author. Weekly epidemiological update on COVID-19 - 8 June 2021. Available at URL: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---8-june-2021.
- 11.Kluge HHP, Wickramasinghe K, Rippin HL, Mendes R, Peters DH, Kontsevaya A, et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020;395(10238):1678–1680. doi: 10.1016/S0140-6736(20)31067-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Azarpazhooh MR, Morovatdar N, Avan A, Phan TG, Divani AA, Yassi N, et al. COVID-19 Pandemic and Burden of Non-Communicable Diseases: An Ecological Study on Data of 185 Countries. Journal of stroke and cerebrovascular diseases: the official journal of the National Stroke Association. 2020;29(9):105089. doi: 10.1016/j.jstrokecerebrovasdis.2020.105089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim MA, Huang I, Yonas E, Vania R, Pranata R. A wave of non-communicable diseases following the COVID-19 pandemic. Diabetes & metabolic syndrome. 2020;14(5):979–980. doi: 10.1016/j.dsx.2020.06.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Godman B, Egwuenu A, Haque M, Malande OO, Schellack N, Kumar S, et al. Strategies to Improve Antimicrobial Utilisation with a Special Focus on Developing Countries. Life. 2021;11(6):528. doi: 10.3390/life11060528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodríguez-Álvarez M, López-Vidal Y, Soto-Hernández JL, Miranda-Novales MG, Flores-Moreno K, Ponce de León-Rosales S. COVID-19: Clouds Over the Antimicrobial Resistance Landscape. Archives of medical research. 2021;52(1):123–126. doi: 10.1016/j.arcmed.2020.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Langford BJ, So M, Raybardhan S, Leung V, Soucy JR, Westwood D, et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin Microbiol Infect. 2021;27(4):520–531. doi: 10.1016/j.cmi.2020.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chowdhury K, Haque M, Nusrat N, Adnan N, Islam S, Lutfor AB, et al. Management of Children Admitted to Hospitals across Bangladesh with Suspected or Confirmed COVID-19 and the Implications for the Future: A Nationwide Cross-Sectional Study. Antibiotics. 2022;11(1):105. doi: 10.3390/antibiotics11010105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Opanga SA, Rizvi N, Wamaitha A, Sefah IA, Godman B. Availability of Medicines in Community Pharmacy to Manage Patients with COVID-19 in Kenya; Pilot Study and Implications. Sch Acad J Pharm. 2021;10(3):36–42. [Google Scholar]
- 19.Lurie N, Saville M, Hatchett R, Halton J. Developing Covid-19 Vaccines at Pandemic Speed. N Engl J Med. 2020;382(21):1969–1973. doi: 10.1056/NEJMp2005630. [DOI] [PubMed] [Google Scholar]
- 20.Graham BS. Rapid COVID-19 vaccine development. Science. 2020;368(6494):945–946. doi: 10.1126/science.abb8923. [DOI] [PubMed] [Google Scholar]
- 21.Haque A, Pant AB. Efforts at COVID-19 Vaccine Development: Challenges and Successes. Vaccines. 2020;8(4):739. doi: 10.3390/vaccines8040739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khandker SS, Godman B, Jawad MI, Meghla BA, Tisha TA, Khondoker MU, et al. A Systematic Review on COVID-19 Vaccine Strategies, Their Effectiveness, and Issues. Vaccines. 2021;9(12):1387. doi: 10.3390/vaccines9121387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO, author. COVID-19 vaccine tracker and landscape. 2021. Jun 16, Available at URL: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines.
- 24.WHO, author. Status of COVID-19 Vaccines within WHO EUL-PQ evaluation process. Available at URL: https://extranet.who.int/pqweb/sites/default/files/documents/Status_of_COVID-19_Vaccines_within_ WHO_EUL-PQ_evaluation_process-16June2021_Final.pdf.
- 25.Shrotri M, Swinnen T, Kampmann B, Parker EPK. An interactive website tracking COVID-19 vaccine development. The Lancet Global health. 2021;9(5):e590–e592. doi: 10.1016/S2214-109X(21)00043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, Banza Ndala DB, Mbidi Miema J, Luhata Lungoyo C, et al. Acceptability of Vaccination Against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. Pragmatic and observational research. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, et al. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines. 2021;9(1):42. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sallam M, Dababseh D, Eid H, Hasan H, Taim D, Al-Mahzoum K, et al. Low COVID-19 Vaccine Acceptance Is Correlated with Conspiracy Beliefs among University Students in Jordan. Int J Environ Res Public Health. 2021;18(5):2407. doi: 10.3390/ijerph18052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalised infectious diseases. Human vaccines & immunotherapeutics. 2020;16(11):2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ global health. 2020;5(10):e004206. doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muric G, Wu Y, Ferrara E. COVID-19 Vaccine Hesitancy on Social Media: Building a Public Twitter Data Set of Antivaccine Content, Vaccine Misinformation, and Conspiracies. JMIR Public Health Surveill. 2021;7(11):e30642. doi: 10.2196/30642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mutombo PN, Fallah MP, Munodawafa D, Kabel A, Houeto D, Goronga T, et al. COVID-19 vaccine hesitancy in Africa: a call to action. Lancet Glob Health. 2022;10(3):e320–e321. doi: 10.1016/S2214-109X(21)00563-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nguyen T, Henningsen KH, Brehaut JC, Hoe E, Wilson K. Acceptance of a pandemic influenza vaccine: a systematic review of surveys of the general public. Infection and drug resistance. 2011;4:197–207. doi: 10.2147/IDR.S23174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salmon DA, Dudley MZ. It is time to get serious about vaccine confidence. Lancet. 2020;396(10255):870–871. doi: 10.1016/S0140-6736(20)31603-2. [DOI] [PubMed] [Google Scholar]
- 35.Shen SC, Dubey V. Addressing vaccine hesitancy: Clinical guidance for primary care physicians working with parents. Canadian family physician Medecin de Famille canadien. 2019;65(3):175–181. [PMC free article] [PubMed] [Google Scholar]
- 36.MacDonald NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 37.Seale H, Kaur R, Wang Q, Yang P, Zhang Y, Wang X, et al. Acceptance of a vaccine against pandemic influenza A (H1N1) virus amongst healthcare workers in Beijing, China. Vaccine. 2011;29(8):1605–1610. doi: 10.1016/j.vaccine.2010.12.077. [DOI] [PubMed] [Google Scholar]
- 38.Wiysonge CS, Ndwandwe D, Ryan J, Jaca A, Batouré O, Anya BM, et al. Vaccine hesitancy in the era of COVID-19: could lessons from the past help in divining the future? Human vaccines & immunotherapeutics. 2021;18(1):1–3. doi: 10.1080/21645515.2021.1893062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saied SM, Saied EM, Kabbash IA, Abdo SAE. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. Journal of medical virology. 2021;93(7):4280–4291. doi: 10.1002/jmv.26910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nature medicine. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines. 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fares S, Elmnyer MM, Mohamed SS, Elsayed R. COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. Journal of primary care & community health. 2021;12:21501327211013303. doi: 10.1177/21501327211013303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kanyike AM, Olum R, Kajjimu J, Ojilong D, Akech GM, Nassozi DR, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Tropical medicine and health. 2021;49(1):37. doi: 10.1186/s41182-021-00331-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.El-Elimat T, AbuAlSamen MM, Almomani BA, Al-Sawalha NA, Alali FQ. Acceptance and attitudes toward COVID-19 vaccines: A cross-sectional study from Jordan. PloS one. 2021;16(4):e0250555. doi: 10.1371/journal.pone.0250555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abena PM, Decloedt EH, Bottieau E, Suleman F, Adejumo P, Sam-Agudu NA, et al. Chloroquine and Hydroxychloroquine for the Prevention or Treatment of COVID-19 in Africa: Caution for Inappropriate Off-label Use in Healthcare Settings. Am J Trop Med Hyg. 202;102(6):1184–1188. doi: 10.4269/ajtmh.20-0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haque M, Abubakar A, Ogunleye O, Sani I, Sefah I, Kurdi A, et al. Changes in the availability, utilisation, and prices of medicines and protection equipment for COVID-19 in an Urban population of Northern Nigeria. Journal of Research in Pharmacy Practice. 2021;10(1):17–22. doi: 10.4103/jrpp.JRPP_20_92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Godman B. Combating COVID-19: Lessons learnt particularly among developing countries and the implications. Bangladesh Journal of Medical Science. 2020;19:S103–S108. [Google Scholar]
- 48.Abubakar AR, Sani IH, Godman B, Kumar S, Islam S, Jahan I, et al. Systematic Review on the Therapeutic Options for COVID-19: Clinical Evidence of Drug Efficacy and Implications. Infection and drug resistance. 2020;13:4673–4695. doi: 10.2147/IDR.S289037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schellack N, Strydom M, Pepper MS, Herd CL, Hendricks CL, Bronkhorst E, et al. Social Media and COVID-19 - Perceptions and Public Deceptions of Ivermectin, Colchicine and Hydroxychloroquine: Lessons for Future Pandemics. Antibiotics. 2022;11(4):445. doi: 10.3390/antibiotics11040445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.WHO, author. COVID 19 Zambia. 2021. Aug 1, Available at URL: https://covid19.who.int/region/afro/country/zm.
- 51.Chabusha B. ZAMRA APPROVES 5 COVID-19 VACCINES FOR ZAMBIA. 2021. Jun, Available at URL: https://zambiareports.com/2021/06/01/zamra-approves-5-covid-19-vaccines-zambia/
- 52.Aruru M, Truong HA, Clark S. Pharmacy Emergency Preparedness and Response (PEPR): a proposed framework for expanding pharmacy professionals' roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Research in social & administrative pharmacy. 2021;17(1):1967–1977. doi: 10.1016/j.sapharm.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hedima EW, Adeyemi MS, Ikunaiye NY. Community Pharmacists: On the frontline of health service against COVID-19 in LMICs. Research in social & administrative pharmacy. 2021;17(1):1964–1966. doi: 10.1016/j.sapharm.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kayode OR, Babatunde OA, Adekunle O, Igbalajobi M, Abiodun AK. COVID-19 Vaccine Hesitancy: Maximising the Extending Roles of Community Pharmacists in Nigeria in Driving Behavioural Changes in Public Health Interventions. J Infect Dis Epidemiol. 2021;7:205. [Google Scholar]
- 55.Bolatov AK, Seisembekov TZ, Askarova AZ, Pavalkis D. Barriers to COVID-19 vaccination among medical students in Kazakhstan: development, validation, and use of a new COVID-19 Vaccine Hesitancy Scale. Hum Vaccin Immunother. 2021;17(12):4982–4992. doi: 10.1080/21645515.2021.1982280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Uzochukwu IC, Eleje GU, Nwankwo CH, Chukwuma GO, Uzuke CA, Uzochukwu CE, et al. COVID-19 vaccine hesitancy among staff and students in a Nigerian tertiary educational institution. Ther Adv Infect Dis. 2021;8:20499361211054923. doi: 10.1177/20499361211054923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mudenda S, Mukosha M, Mwila C, Saleem Z, Kalungia AC, Munkombwe D, et al. Impact of the coronavirus disease on the mental health and physical activity of pharmacy students at the University of Zambia: a cross-sectional study. International journal of basic and clinical pharmacology. 2021;10:324. [Google Scholar]
- 58.Bai W, Cai H, Liu S, Liu H, Qi H, Chen X, et al. Attitudes toward COVID-19 vaccines in Chinese college students. International journal of biological sciences. 2021;17(6):1469–1475. doi: 10.7150/ijbs.58835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Qiao S, Friedman DB, Tam CC, Zeng C, Li X. Vaccine acceptance among college students in South Carolina: Do information sources and trust in information make a difference? medRxiv. 2020 doi: 10.1080/07448481.2022.2059375. [DOI] [PubMed] [Google Scholar]
- 60.Mudenda S, Hikaambo CN, Daka V, Chileshe M, Mfune RL, Kampamba M, et al. Prevalence and factors associated with COVID-19 vaccine acceptance in Zambia: a web-based cross-sectional study. PAMJ. 2022;41:112. doi: 10.11604/pamj.2022.41.112.31219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Carcelen AC, Prosperi C, Mutembo S, Chongwe G, Mwansa FD, Ndubani P, et al. COVID-19 vaccine hesitancy in Zambia: a glimpse at the possible challenges ahead for COVID-19 vaccination rollout in sub- Saharan Africa. Hum Vaccines Immunother. 2021;18(1):1–6. doi: 10.1080/21645515.2021.1948784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mudenda S, Chileshe M, Mukosha M, Hikaambo CN, Banda M, Kampamba M, et al. Zambia's Response to the COVID-19 Pandemic: Exploring Lessons, Challenges and Implications for Future Policies and Strategies. Pharmacol Pharm. 2022;13(01):11–33. [Google Scholar]
- 63.Lucia VC, Kelekar A, Afonso NM. COVID-19 vaccine hesitancy among medical students. J Public Health (Oxf) 2021;43(3):445–449. doi: 10.1093/pubmed/fdaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kelekar AK, Lucia VC, Afonso NM, Mascarenhas AK. COVID-19 vaccine acceptance and hesitancy among dental and medical students. J Am Dent Assoc. 2021;152(8):596–603. doi: 10.1016/j.adaj.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. European journal of epidemiology. 2020;35(8):781–783. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Szmyd B, Bartoszek A, Karuga FF, Staniecka K, Błaszczyk M, Radek M. Medical Students and SARS-CoV-2 Vaccination: Attitude and Behaviors. Vaccines. 2021;9(2):128. doi: 10.3390/vaccines9020128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kukreti S, Lu MY, Lin YH, Strong C, Lin CY, Ko NY, et al. Willingness of Taiwan's Healthcare Workers and Outpatients to Vaccinate against COVID-19 during a Period without Community Outbreaks. Vaccines. 2021;9(3):246. doi: 10.3390/vaccines9030246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Papagiannis D, Rachiotis G, Malli F, Papathanasiou IV, Kotsiou O, Fradelos EC, et al. Acceptability of COVID-19 Vaccination among Greek Health Professionals. Vaccines. 2021;9(3):200. doi: 10.3390/vaccines9030200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Garcia LL, Yap JFC. The role of religiosity in COVID-19 vaccine hesitancy. J Public Health (Oxf) 2021;43(3):e529–e530. doi: 10.1093/pubmed/fdab192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kibongani Volet A, Scavone C, Catalán-Matamoros D, Capuano A. Vaccine Hesitancy Among Religious Groups: Reasons Underlying This Phenomenon and Communication Strategies to Rebuild Trust. Frontiers in public health. 2022;10:824560. doi: 10.3389/fpubh.2022.824560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Machekanyanga Z, Ndiaye S, Gerede R, Chindedza K, Chigodo C, Shibeshi ME, Goodson J, Daniel F, Zimmerman L, Kaiser R. Qualitative Assessment of Vaccination Hesitancy Among Members of the Apostolic Church of Zimbabwe: A Case Study. J Relig Health. 2017;56(5):1683–1691. doi: 10.1007/s10943-017-0428-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Detoc M, Bruel S, Frappe P, Tardy B, Botelho-Nevers E, Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020;38(45):7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Patelarou E, Galanis P, Mechili EA, Argyriadi A, Argyriadis A, Asimakopoulou E, et al. Factors influencing nursing students' intention to accept COVID-19 vaccination: A pooled analysis of seven European countries. Nurse education today. 2021;104:105010. doi: 10.1016/j.nedt.2021.105010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pugliese-Garcia M, Heyerdahl LW, Mwamba C, Nkwemu S, Chilengi R, Demolis R, et al. Factors influencing vaccine acceptance and hesitancy in three informal settlements in Lusaka, Zambia. Vaccine. 2018;36(37):5617–5624. doi: 10.1016/j.vaccine.2018.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cadogan CA, Hughes CM. On the frontline against COVID-19: Community pharmacists' contribution during a public health crisis. Res Social Adm Pharm. 2021;17(1):2032–2035. doi: 10.1016/j.sapharm.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding authors, upon reasonable request.