Abstract
Extracorporeal life support (ECLS) for acute respiratory failure encompasses veno-venous extracorporeal membrane oxygenation (V-V ECMO) and extracorporeal carbon dioxide removal (ECCO2R). V-V ECMO is primarily used to treat severe acute respiratory distress syndrome (ARDS), characterized by life-threatening hypoxemia or ventilatory insufficiency with conventional protective settings. It employs an artificial lung with high blood flows, and allows improvement in gas exchange, correction of hypoxemia, and reduction of the workload on the native lung. On the other hand, ECCO2R focuses on carbon dioxide removal and ventilatory load reduction (“ultra-protective ventilation”) in moderate ARDS, or in avoiding pump failure in acute exacerbated chronic obstructive pulmonary disease. Clinical indications for V-V ECLS are tailored to individual patients, as there are no absolute contraindications. However, determining the ideal timing for initiating extracorporeal respiratory support remains uncertain. Current ECLS equipment faces issues like size and durability. Innovations include intravascular lung assist devices (ILADs) and pumpless devices, though they come with their own challenges. Efficient gas exchange relies on modern oxygenators using hollow fiber designs, but research is exploring microfluidic technology to improve oxygenator size, thrombogenicity, and blood flow capacity. Coagulation management during V-V ECLS is crucial due to common bleeding and thrombosis complications; indeed, anticoagulation strategies and monitoring systems require improvement, while surface coatings and new materials show promise. Moreover, pharmacokinetics during ECLS significantly impact antibiotic therapy, necessitating therapeutic drug monitoring for precise dosing. Managing native lung ventilation during V-V ECMO remains complex, requiring a careful balance between benefits and potential risks for spontaneously breathing patients. Moreover, weaning from V-V ECMO is recognized as an area of relevant uncertainty, requiring further research. In the last decade, the concept of Extracorporeal Organ Support (ECOS) for patients with multiple organ dysfunction has emerged, combining ECLS with other organ support therapies to provide a more holistic approach for critically ill patients. In this review, we aim at providing an in-depth overview of V-V ECMO and ECCO2R, addressing various aspects of their use, challenges, and potential future directions in research and development.
Keywords: V-V ECMO, Acute respiratory failure, Gas exchange, Lung protective ventilation
Introduction: current available techniques and indications
Veno-venous extracorporeal membrane oxygenation (V-V ECMO) and extracorporeal carbon dioxide removal (ECCO2R) are extracorporeal life support (ECLS) systems, indicated in different severity degrees of acute respiratory failure [1].
The current main indication for V-V ECMO is severe acute respiratory distress syndrome (ARDS) with either life-threatening hypoxemia or inability to ventilate with protective settings [2].
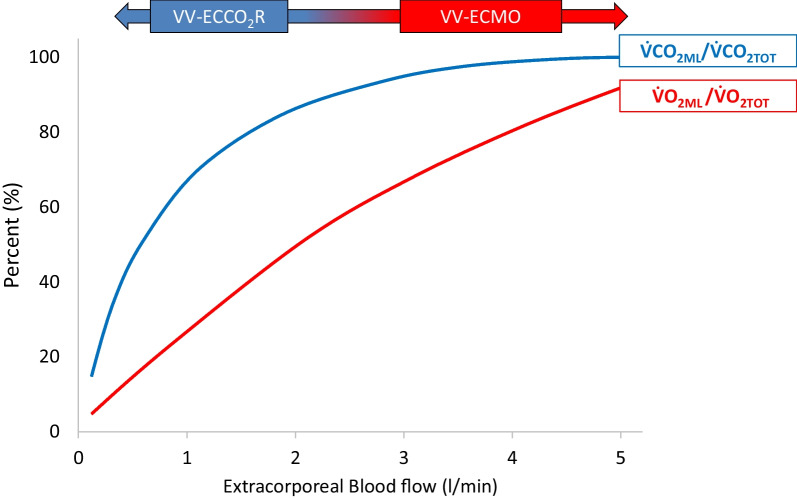
Under V-V ECMO, highly protective mechanical ventilation is obtained by reducing the ventilatory load (pressures, volumes and rate) on the native lung, whose gas exchange function is undertaken by an artificial (membrane) lung. The membrane is perfused by high blood flows (normally 4–6 L/min), and the “sweep gas” (with a variable concentration of oxygen) is forced through the membrane’s fibers, with efficient oxygen and carbon dioxide exchange [3]. The resulting oxygenated and de-carboxylated blood is then mixed in the right atrium with the venous return not passing the membrane lung, and finally flows through the patient’s native lung, which contributes (at a variable degree) to the final PaO2 and SaO2. However, the two most important determinants of oxygenation under V-V ECMO are the extracorporeal blood flow (Fig. 1) and the fraction of oxygen in the sweep gas (FmO2).
Fig. 1.
Extracorporeal oxygen delivery ( O2ML)/total oxygen consumption ( O2TOT) and extracorporeal carbon dioxide removal ( CO2ML)/total carbon dioxide production ( CO2TOT) as a function of extracorporeal blood flow (BF) at steady state in an adult patient. O2TOT = 250 mL/min and CO2TOT 200 mL/min. Veno-venous extracorporeal oxygenation support (V-V ECMO), veno-venous extracorporeal CO2 removal (V-V ECCO2R)
Differently from ECMO, ECCO2R uses lower blood flows, smaller circuits, membranes, and cannulas. As such, the main effect of this technique is to lower carbon dioxide, without any relevant effect on oxygenation (see Fig. 1). Indeed, the principal determinant of carbon dioxide removal is the amount of sweep gas flow. Accordingly, ECCO2R uses blood flows in the range of 300–1500 mL/min and sweep gas flows up to 8–10 L/min. Clinical indications for ECCO2R are still debated, but it is presently applied in severe exacerbations of chronic obstructive pulmonary disease (COPD) (with the aim of reducing the rate of intubation and duration of mechanical ventilation) and in moderate ARDS (to reduce the ventilatory load to allow “ultra-protective” ventilatory settings) [4, 5]. Combinations of ECCO2R with continuous renal replacement therapy (CRRT) have been recently described in patients with ARDS and acute kidney injury [6, 7].
In each section of this review, we will describe the current state of the art and, thereafter, the gaps in knowledge and potential research directions in the field of VV-ECLS.
Clinical indications and contraindications for V-V ECMO
Current indications for V-V ECLS are summarized in Table 1. The two main “classical” indications for V-V ECMO are life-threatening hypoxemia and/or the inability to ventilate with protective ventilatory settings in patients with potentially reversible severe ARDS [8] or other forms of acute hypoxemic respiratory failure such as interstitial lung disease [9] and as a bridge to lung transplant [10]. Several prediction scores have been proposed to assist clinicians in properly evaluating candidates [11–13].
Table 1.
Current indications for V-V ECLS
| Technique | Indications |
|---|---|
| V-V ECMO |
Severe ARDS with one of following, after optimization of MV [18]: • PaO2/FiO2 < 50 mmHg with FiO2 ≥ 0.8 for > 3 h • PaO2/FiO2 < 80 mmHg with FiO2 ≥ 0.8 for > 6 h • pH < 7.25 (with PaCO2 ≥ 60 mmHg) for > 6 h (with RR increased to 35 bpm) |
| V-V ECCO2R |
• Moderate ARDS with Pplat > 30 cmH2O after optimization of MV [19] • Acute hypercapnic exacerbation of COPD, with two of following, after 2 h of NIV [20]: – arterial pH ≤ 7.25 – RR ≥ 30 bpm – use of accessory muscles or paradoxical abdominal movements |
| Combined CRRT-ECCO2R | Mild or moderate ARDS with AKI needing CRRT [21] |
ARDS acute respiratory distress syndrome; bpm, breaths per minute; FiO2 inspiratory fraction of oxygen; NIV, non-invasive ventilation; PaCO2 arterial partial pressure of carbon dioxide; PaO2 arterial partial pressure of oxygen; Pplat airway plateau pressure; RR respiratory rate; COPD chronic obstructive pulmonary disease; CRRT continuous renal replacement therapy; AKI acute kidney injury
Besides this oversimplified view, there are still many “gray areas” of possible use of ECMO. Indeed, the ELSO guidelines state no absolute contraindications for V-V ECMO, since each patient is considered as a candidate individually with regard to potential risks and benefits. Careful consideration is warranted in patients with severe comorbidities, older age [14, 15], multiorgan failure, intracranial bleeding, mechanical ventilation for > 7 days at high settings (FiO2 > 0.9, plateau pressure > 30 cmH2O), or major pharmacological immunosuppression (absolute neutrophil count < 400/mm3) [16]; indeed, these patients could probably have a poor prognosis despite successful V-V ECMO treatment. Moreover, the ideal timing to consider extracorporeal respiratory support after the initiation of mechanical ventilation remains unclear. Patients on mechanical ventilation for 7 days or longer were excluded in all recent trials, with prolonged mechanical ventilation being an independent predictor of in-hospital mortality [17].
As for V-V ECCO2R, relevant clinical indications could be moderate ARDS with low static compliance and acute hypercapnic exacerbations of COPD. These are both covered in depth in another section of this review entitled ‘Low/medium-flow ECLS for protective lung ventilation’.
Equipment and new technology
Modern equipment for V-V ECLS typically includes many different components [22]: (a) large-bore cannulas for drainage and return of the patient’s blood; (b) specialized tubing and connectors to conduct the blood; (c) a centrifugal pump that provides a continuous and consistent blood flow; (d) a membrane oxygenator; (e) a gas blender; (f) a heat exchanger; (g) sensors ensuring precise measurement of blood flow, pressures and oxygen levels; (h) a control and monitoring console, with a graphic display and human interface devices (usually knobs and buttons); and (i) alarm systems. The problems and shortcomings of current ECLS equipment may be summarized as follows: (a) excessive size; (b) lack of portability and mobility limitations; (c) external pump dependence; (d) lack of durability; and (e) lack of metabolic functions. Accordingly, research in the field is focusing on finding smaller and longer-running alternatives to present ECLS devices [23].
To address the problems related to excessive size and lack of portability, intravascular lungs assist devices (ILADs) have been developed since the late 1980s [24]. They are basically small implantable intravascular membrane oxygenators; both static and dynamic (i.e., impeller-driven) configurations have been developed and tested preclinically [25], with the aim of providing partial lung support. However, to date, its translation into the clinical world has proven impossible because of the lack of adequate blood and gas flows, pressure gradients and biocompatibility [23].
To address excessive dependence on external pumps, pumpless devices have been developed; they are based on an arterio-venous shunt and use the patient’s cardiac output as a prime mover. The most famous pumpless device, the interventional lung assist (iLA, NovaLung, Germany), has proven to be effective in removing CO2, with a limited effect on oxygenation [26]. Accordingly, the technique has been proposed both for allowing “ultra-protective” ventilation in ARDS [26] and as a bridge to lung transplantation in patients with ventilator-refractory hypercapnia [27]. However, pumpless systems have shown low oxygenation efficacy, difficult applicability (especially in patients with hemodynamic instability), risk of complications (especially limb ischemia), and low durability and have therefore been progressively abandoned [23].
The issue of circuits and oxygenators durability is deeply intertwined with that of coagulation management and surface coating; this topic will be more extensively discussed in the section ‘Coagulation management during V-V ECMO’.
Gas exchange
As for other parts of equipment described above, presently used oxygenators are also very far from perfect. We will start by describing their structure and functioning and then move on to their shortcomings and possible future solutions.
Current oxygenators are based on the juxtaposition of multiple hollow fibers creating channels, with the most commonly used material being polymethylpentene (PMP). Compared to older materials, these fibers have better durability, cause less hemolysis, and cause less plasma leakage. In the oxygenator, O2 transfer is dependent on: (a) surface area and diffusion characteristics of the membrane; (b) O2 partial pressure (PO2) gradient between blood and sweep gas; and (c) blood flow. The surface area has been substantially increased by using hollow fibers and should not be a limiting factor in current adult oxygenators [28]. Increasing blood flow increases the number of fibers used and maximizes contact. However, increased blood flow can decrease transit time and reduce oxygenation. When 100% oxygen is used as sweep gas, the blood downstream the membrane lung has a PO2 up to 300–500 mmHg, with a maximized O2 content [29]. Further, the extracorporeal oxygen delivery at a given blood flow is highly dependent on the oxygen content of the blood entering the membrane lung. Almost 5 L/min of blood flow are required to provide an oxygen transfer comparable to the total body oxygen consumption of an adult patient (Fig. 1), assuming a hemoglobin saturation of 70% of the blood entering the membrane lung. Meanwhile, carbon dioxide is quickly transferred from the blood to the sweep gas according to the partial pressure gradient across the membrane. High sweep gas flows allow clearing an amount of CO2 comparable to 60% of the total CO2 production, while blood flows above 2–3 L/min may be required to remove an amount of CO2 comparable to the total CO2 production of an adult.
The shortcomings of presently used oxygenators fall into different domains: first, they are still voluminous and require relatively high priming volumes; second, they frequently induce blood cell trauma and hemolysis; and third, they tend to progressively lose efficiency over time due to coagulation and deposition of cells and fibers.
To address the shortcomings of currently available oxygenators, a significant amount of research is focused on microfluidic technology [23]. Systems utilizing this technology closely resemble the gas exchange interface of the native lung. They feature extremely thin channels, known as “microchannels”, that efficiently transport blood through the oxygenator’s gas-exchanging sections, while minimizing or even completely avoiding excessive shear stress, disturbed flow, and stasis [30]. Many different designs are presently under development and pre-clinical testing [30–37], but to date none of them have undergone clinical testing. One of the most relevant problems that needs to be solved prior to their clinical application is the relatively low blood flow that these oxygenators are presently able to sustain (i.e., 40–150 mL/min) [30]. Nevertheless, the technology is promising because it provides good gas exchange performance with lower thrombogenicity in a more compact size [23].
Coagulation management during V-V ECMO
Bleeding and thrombosis are among the most common and dangerous complications during ECMO [38]. Although critical illness per se puts the patient into an altered coagulative state (sepsis, liver dysfunction, and disseminated intravascular coagulopathy being the main drivers), the most important causes of coagulopathy during ECMO are shear stress, turbulent flow, and exposure of blood to synthetic surfaces in the circuit [39]. Precise mechanisms have been described elsewhere and include on the one side activation of platelets and coagulation factors due to direct mechanical forces (promoting thrombosis), and on the other side configuration changes in von Willebrand factor and consumption of other factors due to high shear stress (promoting bleeding) [40].
A further challenge is represented by the partially inadequate diagnostic tests that are commonly used in patients on V-V ECMO. Activated clotting time (ACT) continues to be used for monitoring unfractionated heparin or direct thrombin inhibitors (DTIs), but concordance with other tests is often limited [41–43]. Activated partial thromboplastin time (aPTT) evaluates intrinsic and common pathways and is therefore used to monitor heparin and DTIs. Even so, aPTT is affected by levels of some endogenous factors (among others, fibrinogen and antithrombin), and therapeutic ranges can widely differ between different laboratories; thus, clinicians must individualize the approach [43]. Anti-factor Xa activity levels (anti-Xa) are increasingly used, as their correlation with heparin levels is higher than with aPTT. However, clot formation and firmness are not tested with this approach, and using it as a therapeutic target does not seem to improve outcomes [41, 44]. Viscoelastic tests (thromboelastography or rotational thromboelastometry) are based on the use of specific activators to evaluate the formation of clots in whole blood samples. While there is some evidence supporting their use for bleeding assessment and management, the use of viscoelastic tests for anticoagulation monitoring in ECLS is still a subject of debate [43].
As for the therapeutic regimens, unfractionated heparin (UFH) continues to be widely used in ECLS due to its short duration of effect, ease of use and monitoring, and possibility of reversal [38]. Nevertheless, some patients may develop dangerous complications, such as heparin-induced thrombocytopenia (HIT) and “heparin resistance”. The latter should be sought when ACT or aPTT targets cannot be reached with UFH infusion > 35,000 units/day [45]. Anti-Xa levels may be useful for diagnostic purposes in the setting of high heparin requirements to achieve the desired aPTT or ACT values [43]. Heparin effectiveness is also deeply influenced by antithrombin-III (AT-III) levels, and this factor is frequently supplemented during ECLS; however, despite its widespread use, only one RCT has been published to date, showing no effect of AT-III supplementation on heparin requirements or on the incidence of bleeding [46]. Some authors suggest that the use of low-molecular-weight heparins for anticoagulation in patients undergoing ECLS could be beneficial in terms of reduced thromboembolic and hemorrhagic events [47]. However, the evidence on survival benefits is still scarce and, more importantly, no RCTs have compared different anticoagulation strategies on ECLS to date [48]. Direct thrombin inhibitors (DTIs) are possible alternatives to UFH in cases of heparin resistance or HIT. Argatroban reversibly binds to and inhibits thrombin; having eminent hepatic elimination (a half-life of 40–50 min), its use should be preferred in cases of renal failure [49]. Bivalirudin reversibly inhibits thrombin, with an elimination half-life of 20–30 min, which can be variably prolonged in renal failure; it is widely used as a heparin alternative during intravascular interventions, but its use has occasionally been reported also during ECMO [49, 50].
Optimizing anticoagulation practices still appears to be a work-in-progress. To date, there is not any wide consensus among experts on the best therapeutic regimen, the most appropriate monitoring, or the management of thrombotic or bleeding complications. Accordingly, future research should focus on finding the best anticoagulation regimen, the best coagulation monitoring systems, and developing less thrombogenic materials [51, 52]. The most intuitive solution in this regard is to coat the contact surfaces with antithrombotic material [23]. Currently, the most commonly used coating is heparin, which has indeed led to a decrease in systemic anticoagulation needs [53]. However, more advanced coatings, such as nitric oxide-generating surfaces (for example, S-nitroso-N-acetyl-penicillamine and poly-carboxybetaine) are currently under investigation. Although promising in terms of thrombosis reduction, these approaches still need refinement before being applied in clinical trials [54, 55].
Native lung ventilation during V-V ECMO
Mechanical ventilation can cause ventilator-induced lung injury (VILI) [56]. The classically recognized mechanisms of VILI include alveolar overdistension (barotrauma and volutrauma), cyclic alveolar collapse and reopening (atelectrauma), and consequent secondary inflammation (biotrauma). More recently, the unifying theory of ergotrauma has been proposed: the mechanical power (composed by pressures, volumes, respiratory rate, and flow) delivered to the lung should be the ‘primum movens’ of VILI [57]. Accordingly, “low power” ventilation (i.e., low tidal volume, low plateau pressure, and low respiratory rate) should reduce VILI but can possibly cause carbon dioxide retention and hypoxemia due to reduced ventilation [58].
V-V ECMO (and possibly ECCO2R) thus grants viable gas exchange while allowing protective (or even ultra-protective) settings. However, it should be noted that Gattinoni and Quintel recently proposed that the correct balance between lung rest and lung movement is difficult (if not impossible) to achieve [59, 60]. Indeed, during V-V ECMO, mechanical ventilation can often be required for two main reasons: (1) ECMO blood flow is not always sufficient to match the patient’s cardiac output (especially in hyperdynamic states), resulting in a substantial proportion of blood still passing exclusively through the native lung; (2) complete lung collapse due to hypoventilation may be detrimental for recovery from the underlying pathological mechanism [61].
Despite the lack of randomized controlled trials, there is a large body of observational evidence supporting the notion that protective ventilation during ECMO is generally associated with better outcomes. The reduction of plateau pressure seems to be particularly beneficial. In a retrospective series of more than sixty V-V ECMO patients, each cmH2O increase in plateau pressure was associated with a 14.4% decrease in the odds of achieving hospital survival [62]. On the contrary, the effect of positive end-expiratory pressure (PEEP) is more controversial. In a recent retrospective observational study, higher PEEP levels during the first 3 days of ECMO support were associated with lower mortality [63]. However, in another retrospective study considering PEEP values during the entire course of ECMO, every increase in PEEP (by 1 cmH2O) was associated with a 36.2% decrease in the odds of 30-day survival in multivariate analysis [64, 65].
In patients with severe ARDS, prone positioning has been associated with improved patient survival [66]. Prone positioning during ECMO is feasible, and it is possibly indicated in cases of severe hypoxemia (i.e., PaO2/FiO2 ratio < 70 mmHg), high plateau pressures (> 30 cmH2O despite protective settings), and difficulties in weaning from ECMO [61]. Although prone positioning may be safe if performed by properly trained personnel, there is evidence that it may entail significant risks to ECMO patients. Many severe adverse events have been reported, including cannula malfunction or malposition, accidental decannulation, unplanned extubation, bed sores, and dislodged arterial and central venous lines [67, 68].
Spontaneous breathing is usually not allowed during the early phases of severe ARDS: deep sedation and muscle relaxation are often needed to remove potentially injurious spontaneous effort and to allow protective mechanical ventilation [69]. Although early evidence showed a survival benefit with the use of cisatracurium in severe ARDS patients [70], these results were not confirmed in a later trial [71]. It is possible that adverse effects of paralysis, including respiratory muscle atrophy, which occurs as few as 18 h after the start of mechanical ventilation, may explain these results. The present vision is that restoration of respiratory muscle activity could possibly be helpful in decreasing or preventing such disuse myopathy [71].
However, it is not easy to find a satisfactory balance between the adverse effects of muscle relaxation and those of potentially injurious spontaneous breathing with effort, which warrants careful evaluation and continuous assessment. The removal of CO2 with an extracorporeal circuit can potentially control spontaneous breathing effort. Indeed, both in experimental settings and in observational clinical studies, an increase in CO2 removal by increasing gas and blood flow can modulate minute ventilation up to a condition of apnea [72]. Moreover, in a group of patients with chronic lung disease treated with ECMO as a bridge for lung transplantation, those spontaneously breathing demonstrated improved survival when compared to other bridging strategies [73].
Although allowing spontaneous breathing during ECMO seems physiological and could be tempting, especially because it may allow early mobilization and rehabilitation [74], there are still many uncertainties on indications and contraindications.
In an animal model of severe ARDS, Güldner and colleagues found that spontaneous breathing during V-V ECMO on the one side improved oxygenation and intrapulmonary shunt and redistributed ventilation towards dorsal areas, but on the other hand, ventilator-supported spontaneous breathing widely increased lung inflammation [75]. Moreover, in the early phases of severe ARDS, many patients show very high inspiratory efforts that are not adequately controlled even if PaCO2 is normalized by V-V ECMO [73]. Thus, allowing these patients to breathe spontaneously may be deleterious and less protective than controlled ventilation. Further studies in the field of neural control of ventilation are needed to fully understand and characterize this issue.
Low/medium-flow ECLS for protective lung ventilation
As previously stated, ECCO2R is the designation for lower blood flow (usually less than 1000 mL/min) veno-venous ECLS devices. ECCO2R was initially proposed for the treatment of acute hypoxemic respiratory failure, but it was soon replaced by high-blood flow devices that allowed more effective oxygenation. Therefore, ECCO2R was “re-discovered” in more recent years for the treatment of hypercapnic respiratory insufficiency or for facilitating protective ventilation in ARDS patients when permissive hypercapnia was not tolerable [76, 77].
Hypercapnic exacerbations have a significant impact on survival (hospital mortality ~ 10%) and the quality of life of patients with COPD [78, 79]; moreover, they play a major role in increasing healthcare costs [80]. The standard of care remains non-invasive ventilation (NIV), which, however, is burdened by a high rate of failure, the need for intubation and a subsequent higher risk of death [78]. ECCO2R, even with very low blood flows (300–500 mL/min), has the potential to prevent NIV failure and therefore reduce intubation and mortality rates [81]. However, available evidence is limited to case series and matched cohort studies. Several randomized trials are planned [20], and they will hopefully provide more robust evidence on the use of ECCO2R in acute decompensations of COPD [82].
In ARDS, ECCO2R allows to dissociate oxygenation (managed by the native lung) from the removal of carbon dioxide, thus allowing ultra-protective ventilation strategies (VT as low as 3–4 mL/Kg of PBW, plateau pressure < 30 cmH2O, reduction of respiratory rate, and minimization of mechanical power of ventilation). In observational studies, ultra-low VT ventilation (3–4 mL/Kg of PBW) was associated with a significant decrease in inflammatory markers compared to standard low volume, low pressure ventilation [76, 83]. A preliminary RCT showed that VT of 3 mL/Kg of PBW was easy and safe to implement with extracorporeal CO2 removal; when analyzing patients with PaO2/FiO2 < 150 mmHg, clinical outcome significantly improved in ECCO2R patients compared to controls [84]. A multicenter study showed that more than 80% of patients with moderate ARDS could achieve ultra-protective ventilation goals by using ECCO2R, and the incidence of severe adverse events was low (~ 2%) [19]. Interestingly, the efficacy and safety of ECCO2R were higher for devices that used blood flow in the range of 1000–1500 mL/min [85]. A more recent RCT, using lower-blood flow devices (up to 450 mL/min) in patients with acute hypoxemic respiratory failure, showed no difference in terms of mortality between ultra-protective ventilation with ECCO2R and standard protective ventilation, although ECCO2R patients had significantly lower ventilation-free days [86]. Other trials using higher blood flow devices are ongoing (clinicatrials.gov NCT04903262) and could possibly provide more definite answers on the use of ECCO2R in ARDS [87].
Pharmacokinetics and antibiotic therapy during VV ECMO
When patients receive ECMO support, important changes in drug pharmacokinetics can occur depending on interactions with the ECMO device, drug characteristics, and the patient’s clinical status [88].
The ECMO circuit itself may behave as an additional compartment by sequestering drugs, increasing volume of distribution (Vd), and changing drug clearance (CL) and elimination; moreover, the circuit may continuously release sequestered drugs even after their administration has stopped [89]. The extent of binding is influenced by drug properties such as molecular weight, plasma protein binding, degree of ionization, and lipophilicity. For instance, drugs with high lipophilicity (such as fentanyl, propofol and voriconazole) [90, 91] and/or high protein binding (such as vancomycin and ceftriaxone) [92] are more likely to be sequestered in ECMO circuits, resulting in a higher loss of the drugs [89]. Materials obviously influence the degree of drug binding, and higher drug concentrations were reported in silicone membrane oxygenators than in hollow-fiber microporous membrane oxygenators; however, there is still disagreement regarding whether the age of a circuit alters drug sequestration [91, 93].
Capillary penetration, fluid shifts and retention, pH, and plasma protein binding of drugs are all mechanisms that may lead to an increased Vd [89]. Besides, renal dysfunction, often present in ECMO patients, causes increased exposure to drugs excreted by the kidney, and continuous renal replacement therapy (CRRT) variably influences drug pharmacokinetics; however, limited data regarding the impact of the combination ECMO-CRRT on the pharmacokinetics of drugs are available [94].
Relevant variability in the pharmacodynamics and kinetics of antibiotics during ECMO has been shown in numerous studies [88, 93]; these differences may be associated with either underdosing (risk of treatment failure) or overdosing (risk of adverse events). Empirical dose adjustment is substantially impossible due to a lack of predictability. Consequently, the best approach towards personalized dosing of antibiotics is the use of therapeutic drug monitoring (TDM) [95]. Although the implementation of a TDM-based antibiotic stewardship program poses clinical, educational, and logistical challenges [96], it has been shown to be clinically beneficial and is recommended by scientific societies [97].
Weaning from V-V ECMO
The choice of the moment to start the weaning from the extracorporeal support and how to proceed is probably one of the most neglected research areas on ECMO.
The trigger for an ECMO weaning trial usually includes resolution of the underlying disease and patient tolerance of the target ventilator support criteria while maintaining adequate oxygenation and normocarbia [98]. Some experts proposed a multi-step, physiology-based algorithm comprising a reduction in membrane lung FiO2 (“ECMO Deoxy Challenge Test”), followed by a progressive reduction of sweep gas flow (“ECMO CO2 Challenge Test”), combined with continuous evaluation of gas exchange and inspiratory effort variables [99].
Some observational studies have described the most common reasons for weaning failure from ECMO. Almost invariably, they all showed that the respiratory system and/or lung mechanics are among the most important factors influencing the possibility of weaning. Moreover, markers of increased effort (such as P0.1 or esophageal pressure swings) nicely correlated with weaning failure [100]. More importantly, oxygenation variables usually have no correlation with weaning failure, thus underscoring the higher importance of respiratory variables other than gas exchange [101].
From respiratory support to extracorporeal organ support (ECOS)
In the course of a critical illness, it is common for multiple organ systems to be affected, with the initial impairment of one organ function frequently leading to damage to other organs. Although the etiology, primary affected organ, and underlying mechanisms may differ, the presence of crosstalk between organs ultimately leads to a progressive dysfunction of all organs involved and a significant deterioration in the clinical condition [1, 102].
A standard clinical and pharmacological approach may not provide adequate support for critically ill patients who develop multiple organ dysfunction. Combined lung and kidney failure [103] or liver and kidney failure (hepatorenal syndrome) [104] are typical examples of multiple organ dysfunction in the course of a critical illness, and much of the current knowledge in multiorgan support has been gained from the connection of CRRT to other organ support therapies, such as V-V ECMO [105–107].
Due to the crosstalk between native (and possibly artificial) organs, the effects of multiple extracorporeal techniques may enhance each other (as in kidney support leading to better hemodynamics and circulatory support leading to improved renal function), finally improving patient outcomes [106].
However, as for other very complex treatment options, current knowledge on ECOS is still lacking, especially in terms of precise indications, modes, timing, and duration [105]. The other critical point is the definition of adequate organizational models to deliver ECOS in a safe, appropriate, and cost-efficient manner [1].
Conclusions and future directions
V-V ECLS techniques have proven to be valuable tools in the management of acute respiratory failure and other critical conditions.
As we look to the future, several areas of research and development stand out.
The indications for V-V ECMO have been established primarily in the context of severe acute respiratory distress syndrome (ARDS) and other forms of acute hypoxemic respiratory failure. However, the gray areas in its use and the absence of absolute contraindications underline the need for careful patient selection and evaluation. On the other hand, ECCO2R is still waiting for a definite place in the management of moderate ARDS and acute exacerbations of COPD, and its use should be kept limited to the ongoing research protocols until safety and efficacy are better elucidated.
The quest for smaller, more portable, and more durable ECLS equipment is ongoing, with the goal of increasing patient mobility and reducing the limitations of current systems. Improving oxygenators remains a priority, and microfluidic technology shows promise in providing more efficient and compact oxygenators with lower thrombogenicity.
Coagulation management during V-V ECMO is a critical aspect of patient care, and finding the best anticoagulation regimen and coagulation monitoring systems is essential. However, research and development of less thrombogenic materials and advanced coatings for circuit surfaces may be key to revolutionizing the field and should be prioritized.
The use of protective ventilation during ECMO and how to wean a patient from extracorporeal support, especially in those cases where high inspiratory efforts are recorded, are still matters of debate and should also be placed high on the list of research priorities in the field.
Finally, an integrated approach to multiple organ support is on the rise, with the hope that the synergistic effects of different techniques may further improve the outcomes of critically ill patients and help shape the future of extracorporeal life support.
Acknowledgements
None.
Abbreviations
- ACT
Activated clotting time
- AKI
Acute kidney injury
- anti-Xa
Anti-factor Xa activity
- aPTT
Activated partial thromboplastin time
- ARDS
Acute respiratory distress syndrome
- AT-III
Antithrombin III
- bpm
Breaths per minute
- CL
Clearance
- CO2
Carbon dioxide
- COPD
Chronic obstructive pulmonary disease
- CRRT
Continuous renal replacement therapy
- DTI
Direct thrombin inhibitor
- ECCO2R
Extracorporeal removal of carbon dioxide
- ECLS
Extracorporeal life support
- ECMO
Extracorporeal membrane oxygenation
- ECOS
Extracorporeal organ support
- FiO2
Inspiratory fraction of oxygen
- FmO2
Membrane fraction of oxygen
- HIT
Heparin-induced thrombocytopenia
- ILAD
Intravascular lung assist device
- ML
Membrane lung
- NIV
Non-invasive ventilation
- PaCO2
Arterial partial pressure of carbon dioxide
- PaO2
Arterial partial pressure of oxygen
- PBW
Predicted body weight
- PEEP
Positive end-expiratory pressure
- PMP
Polymethylpentene
- Pplat
Airway plateau pressure
- RCT
Randomized controlled trial
- RR
Respiratory rate
- TDM
Therapeutic drug monitoring
- UFH
Unfractioned heparin
- V-V
Veno-venous
- VCO2
Production of carbon dioxide
- Vd
Dead space
- VILI
Ventilator-induced lung injury
- VO2
Oxygen uptake
Funding
The study was funded by Italian Ministry of Health – Current research.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
GG received personal fees from Getinge, Drager Medical and Fisher & Paykel. All other authors declare no conflict of interest related to this manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ranieri VM, Brodie D, Vincent JL. Extracorporeal organ support: from technological tool to clinical strategy supporting severe organ failure. JAMA. 2017;318(12):1105–1106. doi: 10.1001/jama.2017.10108. [DOI] [PubMed] [Google Scholar]
- 2.Brodie D, Slutsky AS, Combes A. Extracorporeal life support for adults with respiratory failure and related indications: a review. JAMA. 2019;322(6):557–568. doi: 10.1001/jama.2019.9302. [DOI] [PubMed] [Google Scholar]
- 3.Brodie D, Bacchetta M. Extracorporeal membrane oxygenation for ARDS in adults. N Engl J Med. 2011;365(20):1905–1914. doi: 10.1056/NEJMct1103720. [DOI] [PubMed] [Google Scholar]
- 4.Pham T, Combes A, Roze H, Chevret S, Mercat A, Roch A, et al. Extracorporeal membrane oxygenation for pandemic influenza A(H1N1)-induced acute respiratory distress syndrome: a cohort study and propensity-matched analysis. Am J Respir Crit Care Med. 2013;187(3):276–282. doi: 10.1164/rccm.201205-0815OC. [DOI] [PubMed] [Google Scholar]
- 5.Supady A, Combes A, Barbaro RP, Camporota L, Diaz R, Fan E, et al. Respiratory indications for ECMO: focus on COVID-19. Intensive Care Med. 2022;48(10):1326–1337. doi: 10.1007/s00134-022-06815-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartlett RH. ECMO: The next ten years. Egypt J Crit Care Med. 2016;4(1):7–10. doi: 10.1016/j.ejccm.2016.01.003. [DOI] [Google Scholar]
- 7.Fanelli V, Cantaluppi V, Alessandri F, Costamagna A, Cappello P, Brazzi L, et al. Extracorporeal CO2 removal may improve renal function of patients with acute respiratory distress syndrome and acute kidney injury: an open-label, interventional clinical trial. Am J Respir Crit Care Med. 2018;198(5):687–690. doi: 10.1164/rccm.201712-2575LE. [DOI] [PubMed] [Google Scholar]
- 8.Zapol W, Snider M, Hill J, Fallat R, et al. Extracorporeal membrane oxygenation in severe acute respiratory failure A randomized prospective study. JAMA. 1979;242(20):2193–2196. doi: 10.1001/jama.1979.03300200023016. [DOI] [PubMed] [Google Scholar]
- 9.Trudzinski FC, Kaestner F, Schäfers HJ, Fähndrich S, Seiler F, Böhmer P, et al. Outcome of patients with interstitial lung disease treated with extracorporeal membrane oxygenation for acute respiratory failure. Am J Respir Crit Care Med. 2016;193(5):527–533. doi: 10.1164/rccm.201508-1701OC. [DOI] [PubMed] [Google Scholar]
- 10.Tipograf Y, Salna M, Minko E, Grogan EL, Agerstrand C, Sonett J, et al. Outcomes of extracorporeal membrane oxygenation as a bridge to lung transplantation. Ann Thorac Surg. 2019;107(5):1456–1463. doi: 10.1016/j.athoracsur.2019.01.032. [DOI] [PubMed] [Google Scholar]
- 11.Shah N, Said A (2022) ECMO Predictive Scores, Past, Present, and Future. In: Laforte A (ed) Extracorporeal Membrane Oxygenation Support Therapy [Working Title]. IntechOpen, London
- 12.Maca J, Matousek V, Bursa F, Klementova O, Hanak R, Burda M, et al. Extracorporeal membrane oxygenation survival: external validation of current predictive scoring systems focusing on influenza A etiology. Artif Organs. 2021;45(8):881–892. doi: 10.1111/aor.13932. [DOI] [PubMed] [Google Scholar]
- 13.Enger TB, Philipp A, Videm V, Lubnow M, Wahba A, Fischer M, et al. Prediction of mortality in adult patients with severe acute lung failure receiving veno-venous extracorporeal membrane oxygenation: a prospective observational study. Crit Care. 2014;18(2):R67. doi: 10.1186/cc13824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deatrick KB, Mazzeffi MA, Galvagno SM, Tesoriero RB, Kaczoroswki DJ, Herr DL, et al. Outcomes of venovenous extracorporeal membrane oxygenation when stratified by age: how old is too old? ASAIO J. 2020;66(8):946–951. doi: 10.1097/MAT.0000000000001076. [DOI] [PubMed] [Google Scholar]
- 15.Giani M, Forlini C, Fumagalli B, Rona R, Pesenti A, Foti G. Indication for venovenous extracorporeal membrane oxygenation: is 65 years old, too old? ASAIO J. 2021;67(1):e55. doi: 10.1097/MAT.0000000000001273. [DOI] [PubMed] [Google Scholar]
- 16.Harnisch LO, Moerer O. Contraindications to the initiation of veno-venous ECMO for severe acute respiratory failure in adults: a systematic review and practical approach based on the current literature. Membranes (Basel) 2021;11(8):584. doi: 10.3390/membranes11080584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cui XQ, Tian JK, Zhang M, Tian ZW, Gu M, Zhang JX, et al. Timing of starting veno-venous extracorporeal membrane oxygenation. Zhonghua Yi Xue Za Zhi. 2022;102(25):1887–1890. doi: 10.3760/cma.j.cn112137-20220311-00502. [DOI] [PubMed] [Google Scholar]
- 18.Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–1975. doi: 10.1056/NEJMoa1800385. [DOI] [PubMed] [Google Scholar]
- 19.Combes A, Fanelli V, Pham T, Ranieri VM, Goligher EC, Brodie D, et al. Feasibility and safety of extracorporeal CO2 removal to enhance protective ventilation in acute respiratory distress syndrome: the SUPERNOVA study. Intensive Care Med. 2019;45(5):592–600. doi: 10.1007/s00134-019-05567-4. [DOI] [PubMed] [Google Scholar]
- 20.Tonetti T, Pisani L, Cavalli I, Vega ML, Maietti E, Filippini C, et al. Extracorporeal carbon dioxide removal for treatment of exacerbated chronic obstructive pulmonary disease (ORION): study protocol for a randomised controlled trial. Trials. 2021;22(1):718. doi: 10.1186/s13063-021-05692-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alessandri F, Tonetti T, Pistidda L, Busani S, Borrazzo C, Fanelli V, et al. Extracorporeal CO2 removal during renal replacement therapy to allow lung-protective ventilation in patients with COVID-19-associated acute respiratory distress syndrome. ASAIO J. 2023;69(1):36–42. doi: 10.1097/MAT.0000000000001803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fan E, Gattinoni L, Combes A, Schmidt M, Peek G, Brodie D, et al. Venovenous extracorporeal membrane oxygenation for acute respiratory failure: a clinical review from an international group of experts. Intensive Care Med. 2016;42(5):712–724. doi: 10.1007/s00134-016-4314-7. [DOI] [PubMed] [Google Scholar]
- 23.Syed A, Kerdi S, Qamar A. Bioengineering progress in lung assist devices. Bioeng (Basel, Switzerland) 2021;8(7):89. doi: 10.3390/bioengineering8070089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mortensen J, Berry G. Conceptual and design features of a practical, clinically effective intravenous mechanical blood oxygen/carbon dioxide exchange device (IVOX) Int J Artif Organs. 1989;12(6):384–389. doi: 10.1177/039139888901200607. [DOI] [PubMed] [Google Scholar]
- 25.Cattaneo GFM, Reul H, Schmitz-Rode T, Steinseifer U. Intravascular blood oxygenation using hollow fibers in a disk-shaped configuration: experimental evaluation of the relationship between porosity and performance. ASAIO J. 2006;52(2):180–185. doi: 10.1097/01.mat.0000204151.56591.28. [DOI] [PubMed] [Google Scholar]
- 26.Moerer O, Quintel M. Protective and ultra-protective ventilation: using pumpless interventional lung assist (iLA) Minerva Anestesiol. 2011;77(5):537–544. [PubMed] [Google Scholar]
- 27.Fischer S, Simon AR, Welte T, Hoeper MM, Meyer A, Tessmann R, et al. Bridge to lung transplantation with the novel pumpless interventional lung assist device NovaLung. J Thorac Cardiovasc Surg. 2006;131(3):719–723. doi: 10.1016/j.jtcvs.2005.10.050. [DOI] [PubMed] [Google Scholar]
- 28.Bartlett RH. Physiology of gas exchange during ECMO for respiratory failure. J Intensive Care Med. 2017;32(4):243–248. doi: 10.1177/0885066616641383. [DOI] [PubMed] [Google Scholar]
- 29.Badulak JH. Venovenous extracorporeal membrane oxygenation. Gas exchange, the membrane lung, and the ventilator. ATS Sch. 2020;2(1):136–137. doi: 10.34197/ats-scholar.2020-0077VO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gimbel AA, Hsiao JC, Kim ES, Lewis DJ, Risoleo TF, Urban JN, et al. A high gas transfer efficiency microfluidic oxygenator for extracorporeal respiratory assist applications in critical care medicine. Artif Organs. 2021;45(8):E247–E264. doi: 10.1111/aor.13935. [DOI] [PubMed] [Google Scholar]
- 31.Lee JK, Kung HH, Mockros LF. Microchannel technologies for artificial lungs: (1) theory. ASAIO J. 2008;54(4):372–382. doi: 10.1097/MAT.0b013e31817ed9e1. [DOI] [PubMed] [Google Scholar]
- 32.Hoganson DM, Pryor HI, Bassett EK, Spool ID, Vacanti JP. Lung assist device technology with physiologic blood flow developed on a tissue engineered scaffold platform. Lab Chip. 2011;11(4):700–707. doi: 10.1039/C0LC00158A. [DOI] [PubMed] [Google Scholar]
- 33.Potkay JA. The promise of microfluidic artificial lungs. Lab Chip. 2014;14(21):4122–4138. doi: 10.1039/C4LC00828F. [DOI] [PubMed] [Google Scholar]
- 34.Abada EN, Feinberg BJ, Roy S. Evaluation of silicon membranes for extracorporeal membrane oxygenation (ECMO) Biomed Microdevices. 2018;20(4):86. doi: 10.1007/s10544-018-0335-z. [DOI] [PubMed] [Google Scholar]
- 35.Dabaghi M, Saraei N, Fusch G, Rochow N, Brash JL, Fusch C, et al. An ultra-thin highly flexible microfluidic device for blood oxygenation. Lab Chip. 2018;18(24):3780–3789. doi: 10.1039/C8LC01083H. [DOI] [PubMed] [Google Scholar]
- 36.Ukita R, Potkay JA, Khanafer K, Cook KE. Advancing front oxygen transfer model for the design of microchannel artificial lungs. ASAIO J. 2020;66(9):1054–1062. doi: 10.1097/MAT.0000000000001129. [DOI] [PubMed] [Google Scholar]
- 37.Thompson AJ, Ma LJ, Major T, Jeakle M, Lautner-Csorba O, Goudie MJ, et al. Assessing and improving the biocompatibility of microfluidic artificial lungs. Acta Biomater. 2020;112:190–201. doi: 10.1016/j.actbio.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Combes A, Schmidt M, Hodgson CL, Fan E, Ferguson ND, Fraser JF, et al. Extracorporeal life support for adults with acute respiratory distress syndrome. Intensive Care Med. 2020;46(12):2464–2476. doi: 10.1007/s00134-020-06290-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parker RI. Anticoagulation monitoring during extracorporeal membrane oxygenation: continuing progress. Crit Care Med. 2020;48(12):1920–1921. doi: 10.1097/CCM.0000000000004635. [DOI] [PubMed] [Google Scholar]
- 40.ZeibiShirejini S, Carberry J, McQuilten ZK, Burrell AJC, Gregory SD, Hagemeyer CE. Current and future strategies to monitor and manage coagulation in ECMO patients. Thromb J. 2023;21(1):11. doi: 10.1186/s12959-023-00452-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Price EA, Jin J, Nguyen HM, Krishnan G, Bowen R, Zehnder JL. Discordant aPTT and anti-Xa values and outcomes in hospitalized patients treated with intravenous unfractionated heparin. Ann Pharmacother. 2013;47(2):151–158. doi: 10.1345/aph.1R635. [DOI] [PubMed] [Google Scholar]
- 42.Atallah S, Liebl M, Fitousis K, Bostan F, Masud F. Evaluation of the activated clotting time and activated partial thromboplastin time for the monitoring of heparin in adult extracorporeal membrane oxygenation patients. Perfusion. 2014;29(5):456–461. doi: 10.1177/0267659114524264. [DOI] [PubMed] [Google Scholar]
- 43.Levy JH, Staudinger T, Steiner ME. How to manage anticoagulation during extracorporeal membrane oxygenation. Intensive Care Med. 2022;48(8):1076–1079. doi: 10.1007/s00134-022-06723-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fina D, Matteucci M, Jiritano F, Meani P, Lo Coco V, Kowalewski M, et al. Extracorporeal membrane oxygenation without therapeutic anticoagulation in adults: a systematic review of the current literature. Int J Artif Organs. 2020;43(9):570–578. doi: 10.1177/0391398820904372. [DOI] [PubMed] [Google Scholar]
- 45.Chlebowski MM, Baltagi S, Carlson M, Levy JH, Spinella PC. Clinical controversies in anticoagulation monitoring and antithrombin supplementation for ECMO. Crit Care. 2020;24(1):19. doi: 10.1186/s13054-020-2726-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Panigada M, Cucino A, Spinelli E, Occhipinti G, Panarello G, Novembrino C, et al. A randomized controlled trial of antithrombin supplementation during extracorporeal membrane oxygenation. Crit Care Med. 2020;48(11):1636–1644. doi: 10.1097/CCM.0000000000004590. [DOI] [PubMed] [Google Scholar]
- 47.Gratz J, Pausch A, Schaden E, Baierl A, Jaksch P, Erhart F, et al. Low molecular weight heparin versus unfractioned heparin for anticoagulation during perioperative extracorporeal membrane oxygenation: A single center experience in 102 lung transplant patients. Artif Organs. 2020;44(6):638–646. doi: 10.1111/aor.13642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Quintel M, Bartlett RH, Grocott MPW, Combes A, Ranieri MV, Baiocchi M, et al. Extracorporeal membrane oxygenation for respiratory failure. Anesthesiology. 2020;132(5):1257–1276. doi: 10.1097/ALN.0000000000003221. [DOI] [PubMed] [Google Scholar]
- 49.Koster A, Faraoni D, Levy JH. Argatroban and bivalirudin for perioperative anticoagulation in cardiac surgery. Anesthesiology. 2018;128(2):390–400. doi: 10.1097/ALN.0000000000001976. [DOI] [PubMed] [Google Scholar]
- 50.Kaseer H, Soto-Arenall M, Sanghavi D, Moss J, Ratzlaff R, Pham S, et al. Heparin vs bivalirudin anticoagulation for extracorporeal membrane oxygenation. J Card Surg. 2020;35(4):779–786. doi: 10.1111/jocs.14458. [DOI] [PubMed] [Google Scholar]
- 51.Carter KT, Kutcher ME, Shake JG, Panos AL, Cochran RP, Creswell LL, et al. Heparin-sparing anticoagulation strategies are viable options for patients on veno-venous ECMO. J Surg Res. 2019;243:399–409. doi: 10.1016/j.jss.2019.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roberts TR, Garren MRS, Handa H, Batchinsky AI. Toward an artificial endothelium: development of blood-compatible surfaces for extracorporeal life support. J Trauma Acute Care Surg. 2020;89(Suppl 2):S59–S68. doi: 10.1097/TA.0000000000002700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aubron C, McQuilten Z, Bailey M, Board J, Buhr H, Cartwright B, et al. Low-dose versus therapeutic anticoagulation in patients on extracorporeal membrane oxygenation: a pilot randomized trial. Crit Care Med. 2019;47(7):e563–e571. doi: 10.1097/CCM.0000000000003780. [DOI] [PubMed] [Google Scholar]
- 54.Brisbois EJ, Major TC, Goudie MJ, Bartlett RH, Meyerhoff ME, Handa H. Improved hemocompatibility of silicone rubber extracorporeal tubing via solvent swelling-impregnation of S-nitroso-N-acetylpenicillamine (SNAP) and evaluation in rabbit thrombogenicity model. Acta Biomater. 2016;37:111–119. doi: 10.1016/j.actbio.2016.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ukita R, Wu K, Lin X, Carleton NM, Naito N, Lai A, et al. Zwitterionic poly-carboxybetaine coating reduces artificial lung thrombosis in sheep and rabbits. Acta Biomater. 2019;92:71–81. doi: 10.1016/j.actbio.2019.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hashemian SM, Mohajerani SA, Jamaati HR. Ventilator-induced lung injury. N Engl J Med. 2014;370(10):979–980. doi: 10.1056/NEJMc1400293. [DOI] [PubMed] [Google Scholar]
- 57.Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567–1575. doi: 10.1007/s00134-016-4505-2. [DOI] [PubMed] [Google Scholar]
- 58.López Sanchez M. Mechanical ventilation in patients subjected to extracorporeal membrane oxygenation (ECMO) Med intensiva. 2017;41(8):491–496. doi: 10.1016/j.medin.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 59.Gattinoni L, Tonetti T, Quintel M. How best to set the ventilator on extracorporeal membrane lung oxygenation. Curr Opin Crit Care. 2017;23(1):66–72. doi: 10.1097/MCC.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 60.Quintel M, Busana M, Gattinoni L. Breathing and ventilation during extracorporeal membrane oxygenation: how to find the balance between rest and load. Am J Respir Crit Care Med. 2019;200(8):954–956. doi: 10.1164/rccm.201906-1164ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Patroniti N, Bonatti G, Senussi T, Robba C. Mechanical ventilation and respiratory monitoring during extracorporeal membrane oxygenation for respiratory support. Ann Transl Med. 2018;6(19):386–386. doi: 10.21037/atm.2018.10.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Modrykamien AM, Hernandez OO, Im Y, Walters RW, Schrader CL, Smith LE, et al. Mechanical ventilation in patients with the acute respiratory distress syndrome and treated with extracorporeal membrane oxygenation: impact on hospital and 30 day postdischarge survival. ASAIO J. 2016;62(5):607–612. doi: 10.1097/MAT.0000000000000406. [DOI] [PubMed] [Google Scholar]
- 63.Schmidt M, Stewart C, Bailey M, Nieszkowska A, Kelly J, Murphy L, et al. Mechanical ventilation management during extracorporeal membrane oxygenation for acute respiratory distress syndrome: a retrospective international multicenter study. Crit Care Med. 2015;43(3):654–664. doi: 10.1097/CCM.0000000000000753. [DOI] [PubMed] [Google Scholar]
- 64.Abrams D, Schmidt M, Pham T, Beitler JR, Fan E, Goligher EC, et al. Mechanical ventilation for acute respiratory distress syndrome during extracorporeal life support. Research and practice. Am J Respir Crit Care Med. 2020;201(5):514–525. doi: 10.1164/rccm.201907-1283CI. [DOI] [PubMed] [Google Scholar]
- 65.Richard JC, Sigaud F, Gaillet M, Orkisz M, Bayat S, Roux E, et al. Response to PEEP in COVID-19 ARDS patients with and without extracorporeal membrane oxygenation. A multicenter case-control computed tomography study. Crit Care. 2022;26(1):195. doi: 10.1186/s13054-022-04076-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Guérin C, Reignier J, Richard J-C, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 67.Culbreth RE, Goodfellow LT. Complications of prone positioning during extracorporeal membrane oxygenation for respiratory failure: a systematic review. Respir Care. 2016;61(2):249–254. doi: 10.4187/respcare.03882. [DOI] [PubMed] [Google Scholar]
- 68.Giani M, Martucci G, Madotto F, Belliato M, Fanelli V, Garofalo E, et al. Prone positioning during venovenous extracorporeal membrane oxygenation in acute respiratory distress syndrome. A multicenter cohort study and propensity-matched analysis. Ann Am Thorac Soc. 2021;18(3):495–501. doi: 10.1513/AnnalsATS.202006-625OC. [DOI] [PubMed] [Google Scholar]
- 69.Crotti S, Bottino N, Ruggeri GM, Spinelli E, Tubiolo D, Lissoni A, et al. Spontaneous breathing during extracorporeal membrane oxygenation in acute respiratory failure. Anesthesiology. 2017;126(4):678–687. doi: 10.1097/ALN.0000000000001546. [DOI] [PubMed] [Google Scholar]
- 70.Papazian L, Forel J-M, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363(12):1107–1116. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 71.Moss M, Huang D, Brower R, Ferguson N, et al. Early neuromuscular blockade in the acute respiratory distress syndrome. N Engl J Med. 2019;380(21):1997–2008. doi: 10.1056/NEJMoa1901686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gattinoni L, Coppola S, Camporota L. Physiology of extracorporeal CO2 removal. Intensive Care Med. 2022;48(10):1322–1325. doi: 10.1007/s00134-022-06827-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Crotti S, Bottino N, Spinelli E. Spontaneous breathing during veno-venous extracorporeal membrane oxygenation. J Thorac Dis. 2018;10(Suppl 5):S661–S669. doi: 10.21037/jtd.2017.10.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhang Z, Gu WJ, Chen K, Ni H. Mechanical Ventilation during Extracorporeal Membrane Oxygenation in Patients with Acute Severe Respiratory Failure. Can Respir J. 2017;2017:1783857. doi: 10.1155/2017/1783857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Güldner A, Kiss T, Bluth T, Uhlig C, Braune A, Carvalho N, et al. Effects of ultraprotective ventilation, extracorporeal carbon dioxide removal, and spontaneous breathing on lung morphofunction and inflammation in experimental severe acute respiratory distress syndrome. Anesthesiology. 2015;122(3):631–646. doi: 10.1097/ALN.0000000000000504. [DOI] [PubMed] [Google Scholar]
- 76.Schmidt M, Jaber S, Zogheib E, Godet T, Capellier G, Combes A. Feasibility and safety of low-flow extracorporeal CO2 removal managed with a renal replacement platform to enhance lung-protective ventilation of patients with mild-to-moderate ARDS. Crit Care. 2018;22(1):122. doi: 10.1186/s13054-018-2038-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Morelli A, Del Sorbo L, Pesenti A, Ranieri VM, Fan E. Extracorporeal carbon dioxide removal (ECCO2R) in patients with acute respiratory failure. Intensive Care Med. 2017;43(4):519–530. doi: 10.1007/s00134-016-4673-0. [DOI] [PubMed] [Google Scholar]
- 78.Chandra D, Stamm JA, Taylor B, Ramos RM, Satterwhite L, Krishnan JA, et al. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998–2008. Am J Respir Crit Care Med. 2012;185(2):152–159. doi: 10.1164/rccm.201106-1094OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lindenauer PK, Stefan MS, Shieh MS, Pekow PS, Rothberg MB, Hill NS. Outcomes associated with invasive and noninvasive ventilation among patients hospitalized with exacerbations of chronic obstructive pulmonary disease. JAMA Intern Med. 2014;174(12):1982–1993. doi: 10.1001/jamainternmed.2014.5430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pasquale MK, Sun SX, Song F, Hartnett HJ, Stemkowski SA. Impact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly Medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757–764. doi: 10.2147/COPD.S36997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sklar MC, Beloncle F, Katsios CM, Brochard L, Friedrich JO. Extracorporeal carbon dioxide removal in patients with chronic obstructive pulmonary disease: a systematic review. Intensive Care Med. 2015;41(10):1752–1762. doi: 10.1007/s00134-015-3921-z. [DOI] [PubMed] [Google Scholar]
- 82.d’Andrea A, Banfi C, Bendjelid K, Giraud R. The use of extracorporeal carbon dioxide removal in acute chronic obstructive pulmonary disease exacerbation: a narrative review. Can J Anaesth. 2020;67(4):462–474. doi: 10.1007/s12630-019-01551-0. [DOI] [PubMed] [Google Scholar]
- 83.Hilty MP, Riva T, Cottini SR, Kleinert EM, Maggiorini A, Maggiorini M. Low flow veno-venous extracorporeal CO2 removal for acute hypercapnic respiratory failure. Minerva Anestesiol. 2017;83(8):812–823. doi: 10.23736/S0375-9393.17.11524-5. [DOI] [PubMed] [Google Scholar]
- 84.Bein T, Weber-Carstens S, Goldmann A, Müller T, Staudinger T, Brederlau J, et al. Lower tidal volume strategy (≈3 ml/kg) combined with extracorporeal CO2 removal versus ‘conventional’ protective ventilation (6 ml/kg) in severe ARDS: the prospective randomized Xtravent-study. Intensive Care Med. 2013;39(5):847–856. doi: 10.1007/s00134-012-2787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Combes A, Tonetti T, Fanelli V, Pham T, Pesenti A, Mancebo J, et al. Efficacy and safety of lower versus higher CO2 extraction devices to allow ultraprotective ventilation: secondary analysis of the SUPERNOVA study. Thorax. 2019;74(12):1179–1181. doi: 10.1136/thoraxjnl-2019-213591. [DOI] [PubMed] [Google Scholar]
- 86.McNamee JJ, Gillies MA, Barrett NA, Perkins GD, Tunnicliffe W, Young D, et al. Effect of lower tidal volume ventilation facilitated by extracorporeal carbon dioxide removal vs standard care ventilation on 90-day mortality in patients with acute hypoxemic respiratory failure: the REST randomized clinical trial. JAMA. 2021;326(11):1013–1023. doi: 10.1001/jama.2021.13374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Combes A, Auzinger G, Capellier G, Du Cheyron D, Clement I, Consales G, et al. ECCO2R therapy in the ICU: consensus of a European round table meeting. Crit Care. 2020;24(1):490. doi: 10.1186/s13054-020-03210-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dzierba AL, Abrams D, Brodie D. Medicating patients during extracorporeal membrane oxygenation: the evidence is building. Crit Care. 2017;21(1):66. doi: 10.1186/s13054-017-1644-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Shekar K, Fraser JF, Smith MT, Roberts JA. Pharmacokinetic changes in patients receiving extracorporeal membrane oxygenation. J Crit Care. 2012;27(6):741.e9–741.e18. doi: 10.1016/j.jcrc.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 90.Wildschut ED, Ahsman MJ, Allegaert K, Mathot RAA, Tibboel D. Determinants of drug absorption in different ECMO circuits. Intensive Care Med. 2010;36(12):2109–2116. doi: 10.1007/s00134-010-2041-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.di Nardo M, Wildschut ED. Drugs pharmacokinetics during veno-venous extracorporeal membrane oxygenation in pediatrics. J Thorac Dis. 2018;10(Suppl 5):S642–S652. doi: 10.21037/jtd.2017.11.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shekar K, Roberts JA, Mcdonald CI, Ghassabian S, Anstey C, Wallis SC, et al. Protein-bound drugs are prone to sequestration in the extracorporeal membrane oxygenation circuit: results from an ex vivo study. Crit Care. 2015;19(1):164. doi: 10.1186/s13054-015-0891-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gomez F, Veita J, Laudanski K. Antibiotics and ECMO in the adult population-persistent challenges and practical guides. Antibiot (Basel, Switzerland) 2022;11(3):338. doi: 10.3390/antibiotics11030338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shekar K, Fraser JF, Taccone SS, Welch S, Wallis SC, Mullany DV, et al. The combined effects of extracorporeal membrane oxygenation and renal replacement therapy on meropenem pharmacokinetics: a matched cohort study. Crit Care. 2014;18(6):565. doi: 10.1186/s13054-014-0565-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Blot SI, Pea F, Lipman J. The effect of pathophysiology on pharmacokinetics in the critically ill patient–concepts appraised by the example of antimicrobial agents. Adv Drug Deliv Rev. 2014;77:3–11. doi: 10.1016/j.addr.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 96.Gatti M, Cojutti PG, Bartoletti M, Tonetti T, Bianchini A, Ramirez S, et al. Expert clinical pharmacological advice may make an antimicrobial TDM program for emerging candidates more clinically useful in tailoring therapy of critically ill patients. Crit Care. 2022;26(1):178. doi: 10.1186/s13054-022-04050-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Abdul-Aziz MH, Alffenaar JWC, Bassetti M, Bracht H, Dimopoulos G, Marriott D, et al. Antimicrobial therapeutic drug monitoring in critically ill adult patients: a position paper. Intensive Care Med. 2020;46(6):1127–1153. doi: 10.1007/s00134-020-06050-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tonna JE, Abrams D, Brodie D, Greenwood JC, Rubio Mateo-Sidron JA, Usman A, et al. Management of adult patients supported with venovenous extracorporeal membrane oxygenation (VV ECMO): guideline from the extracorporeal life support organization (ELSO) ASAIO J. 2021;67(6):601–610. doi: 10.1097/MAT.0000000000001432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vasques F, Romitti F, Gattinoni L, Camporota L. How I wean patients from veno-venous extra-corporeal membrane oxygenation. Crit Care. 2019;23(1):316. doi: 10.1186/s13054-019-2592-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Akoumianaki E, Maggiore SM, Valenza F, Bellani G, Jubran A, Loring SH, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med. 2014;189(5):520–531. doi: 10.1164/rccm.201312-2193CI. [DOI] [PubMed] [Google Scholar]
- 101.Al-Fares AA, Ferguson ND, Ma J, Cypel M, Keshavjee S, Fan E, et al. Achieving safe liberation during weaning from VV-ECMO in patients with severe ARDS: the role of tidal volume and inspiratory effort. Chest. 2021;160(5):1704–1713. doi: 10.1016/j.chest.2021.05.068. [DOI] [PubMed] [Google Scholar]
- 102.Armutcu F. Organ crosstalk: the potent roles of inflammation and fibrotic changes in the course of organ interactions. Inflamm Res. 2019;68(10):825–839. doi: 10.1007/s00011-019-01271-7. [DOI] [PubMed] [Google Scholar]
- 103.Husain-Syed F, Slutsky AS, Ronco C. Lung-kidney cross-talk in the critically ill patient. Am J Respir Crit Care Med. 2016;194(4):402–414. doi: 10.1164/rccm.201602-0420CP. [DOI] [PubMed] [Google Scholar]
- 104.Ginès P, Solà E, Angeli P, Wong F, Nadim MK, Kamath P. Hepatorenal syndrome. Nat Rev Dis Prim. 2018;4(1):23. doi: 10.1038/s41572-018-0022-7. [DOI] [PubMed] [Google Scholar]
- 105.Husain-Syed F, Ricci Z, Brodie D, Vincent JL, Ranieri VM, Slutsky AS, et al. Extracorporeal organ support (ECOS) in critical illness and acute kidney injury: from native to artificial organ crosstalk. Intensive Care Med. 2018;44(9):1447–1459. doi: 10.1007/s00134-018-5329-z. [DOI] [PubMed] [Google Scholar]
- 106.Ronco C, Ricci Z, Husain-Syed F. From multiple organ support therapy to extracorporeal organ support in critically ill patients. Blood Purif. 2019;48(2):99–105. doi: 10.1159/000490694. [DOI] [PubMed] [Google Scholar]
- 107.Huber W, Ruiz de Garibay AP. Options in extracorporeal support of multiple organ failure. Med Klin Intensivmed Notfmed. 2020;115(Suppl 1):28–36. doi: 10.1007/s00063-020-00658-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article.