Abstract
Introduction
Prognostic nutritional index (PNI) is a novel inflammation marker that useful in predicting prognosis of certain conditions. We aimed to study PNI of the outpatient and inpatient subjects with established Covid-19 and also aimed to compare PNI of deceased and survived Covid-19 patients.
Methods
The patients with Covid-19 whom presented to outpatient or inpatient clinics of Abant Izzet Baysal University Hospital were enrolled to the study. PNI levels of the inpatients and outpatients, deceased and survived were compared. PNI values of deceased and survived in inpatients were also compared.
Results
Study population was consisted of 4419 subjects (2907 outpatients and 1512 inpatients). PNI of the inpatient (41.55 (36.42–47.1)) group was significantly lower than the PNI of the outpatient (51.95 (47.95–55.75)) subjects (p<0.001). The sensitivity and specificity of PNI (≤46.2 level) in determination of requirement inpatient treatment were 71.2% and 83.5%, respectively. PNI of the deceased patients (37(33.39–40.86)) was lower than the PNI of the survivors (50.45(45.6–54.65)), (p<0.001). The sensitivity and specificity of PNI at ≤44.55 level in determining mortality were 89.22% and 78.87%, respectively.
Conclusion
We suggest that PNI could serve as a reliable prognostic index in covid-19 patients. Reduced level of PNI should alert physicians since it is associated with need for hospitalization and mortality in this population.
Keywords: Covid-19, prognostic nutritional index, mortality, inflammation
Introduction
The new type of coronavirus-induced Covid-19 disease, named as SARS-CoV-2, which started from Wuhan city of China in December 2019 and spread all over the world in a short time, has become an important threat by causing severe respiratory tract infections with a mortal course1. The novel coronavirus disease led to the emergence of the first global pandemic of coronavirus origin2. The infection could begin with flu-like symptoms3. However, unlike patients with other common infectious diseases, patients with COVID-19 have a wide range of clinical manifestations, including complex and mixed lung conditions and multi-organ failure that can lead to death.
Recent evidence suggests that malnutrition is a critical prognostic factor in many diseases, including autoimmune conditions4, cardiovascular diseases5, lung diseases6, and malignancy7. A high degree of malnutrition is associated with high levels of inflammation8. Assessment of systemic immune nutritional status has been refined by adding the prognostic nutritional index (PNI) is a continuous variable based on serum albumin concentration and total lymphocyte count in peripheral blood9. PNI has been reported to be associated with poor survival and postoperative complications in patients with various conditions, but there are only limited reports regarding its role in Covid-19 course.
The aim of present study was to observe the association between PNI and length of hospital stay, necessity of intensive care unit admission, and mortality in patients with COVID-19.
Materials and Methods
Study Population
The patients with Covid-19 whom presented to outpatient or inpatient clinics of Abant Izzet Baysal University Hospital between March 2020 and October 2021 were enrolled to present cross sectional retrospective analysis after study protocol was approved by local ethics committee (date: 9th of November, 2021; decision no: 2021/266). All subjects have a positive RT- PCR throat swab result for covid-19. The patients with negative RT-PCR throat swab for Covid-19 were excluded from the study even if the clinical and radiological diagnosis of Covid-19 has been established. Indications for hospitalization of Covid-19 patients were as follows: dyspnea, reduced oxygen saturation (lower than 92%), pulmonary involvement in chest radiology and severe symptoms in elderly with accompanied chronic conditions (i.e. congestive heart failure, diabetes mellitus, hypertension or chronic obstructive pulmonary disease). Patients under 18 years of age were also excluded. Flow chart summarizes the inclusion and exclusion criteria.
Age, gender, hospitalization duration, prognosis (deceased or survived), necessity of intensive care, laboratory parameters (albumin, c reactive protein [CRP], lactate dehydrogenase [LDH], D-Dimer, Ferritin, white blood cell count [WBC], lymphocyte count [LYM]) were recorded after obtaining from institutional database and patients' files. PNI was calculated with the following formula: (10×serum albumin [g/dL])+(0.005×lymphocytes/µL). Patients whom were hospitalized were grouped as inpatients and patients treated by usual homecare were grouped as outpatients. Data of the inpatients and outpatients were compared. We also compared the data of the subjects who survived and deceased. Patients were followed up for up to 30 days for survival analysis, if they discharged from hospital before 30 day.
Statistical Analyses
IBM SPSS 16.0 software was used for statistical evaluation of the data. Compliance with the normal distribution was examined by the Kolmogorov-Smirnov test. Independent Sample t test for comparing two independent groups by comparing the arithmetic mean of the groups with normal distribution; One-Way ANOVA test for comparison of more than two independent groups; The Mann-Whitney U test was used to compare two independent groups by comparing the medians of the groups that did not show normal distribution, and the Kruskal-Wallis test was used to compare more than two independent groups. The relationship between categorical variables was compared with chi-square test. Survival results were obtained by Kaplan-Meier method, log-rank test was used in univariate analyzes and cox regression method was used in multivariate analyses. A p<0.05 was considered significant.
Results
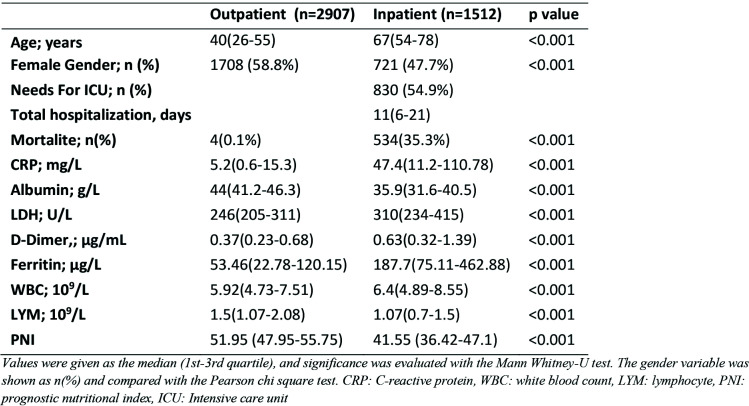
Study population was consisted of 4419 subjects; 2907 in outpatient group and 1512 patients in inpatient group. 2429 (55%) of the study population were female and 1990 (45%) were male. Mean age of the study population was 48.2±23 years. PNI of the inpatient (41.55 (36.42–47.1)) group was significantly lower than the PNI of the outpatient (51.95 (47.95–55.75)) subjects (p<0.001). Table 1 summarizes the characteristics of outpatients and inpatients. The sensitivity and specificity of PNI (≤46.2 level) in determination of requirement inpatient treatment were 71.2% and 83.5%, respectively (AUC: 0.837, p<0.001, 95% CI: 0.825–0.847). Table 2 shows the ROC analysis data of the study variables in determining requirement inpatient treatment. Serum albumin and PNI were best variables in determining inpatient treatment in Covid-19 subjects (figure 2).
Table 1.
Data of the inpatients and outpatients
Table 2.
Receiver operating characteristic (ROC) curve analysis to distinguish between hospitalized and non-hospitalized patients in COVID-19 patients by the markers studied
Figure 2.
shows the ROC curves of study variables in predicting mortality
The data and characteristics of the survived and deceased patients were also compared. Deceased (n=538) subjects were significantly older than survived (n=3881) subjects (75 (66–82) years versus 44 (29–61) years; p<0.001). PNI of the deceased patients (37(33.39–40.86)) was lower than the PNI of the survivors (50.45(45.6–54.65)). The difference was statistically significant (p<0.001). Table 3 summarizes the characteristics and laboratory data of the survived and deceased subjects. The sensitivity and specificity of PNI at ≤44.55 level in determining mortality were 89.22% and 78.87%, respectively (AUC: 0.902, p<0.001, 95%CI: 0.893- 0.910). Table 4 shows the ROC analysis data of the study variables in determining mortality. Figure 3 shows the ROC curves of study variables in predicting mortality. Univariate and multivariate analyses of the study variables in determining survival were summarized in table 5. Figure 4 shows Kaplan- Meier survival curves the study variables in determining overall survival in patients with Covid-19. Finally, inpatients sub-grouped into two according to mortality as deceased and survived. PNI of deceased and survived inpatients were 37(33.39–40.81) and 44.5(39.65–49.31), respectively (p<0.001). Table 6 shows data of the deceased and survived subgroups of inpatient subjects.
Table 3.
Comparison of study variables in deceased and survived patients
Table 4.
Receiver operating characteristic (ROC) curve analysis to distinguish between patients with and without mortality in all COVID-19 patients with the markers studied
Figure 3.
Kaplan-Meier survival curves the study variables in determining overall survival
Table 5.
Univariate and Multivariate Cox proportional hazard model for survival
Figure 4.
ROC curves study variables in predicting mortality in inpatients
Table 6.
Comparison of the data of deceased and survived inpatients
Of those inpatient subjects PNI (at ≤41.75 level) had 80.71% sensitivity and 64.83% specificity in predicting mortality (AUC: 0.779, p<0.001, 95%CI: 758 to 0.8). Table 7 shows ROC analysis data of the study variables in determining mortality in inpatients. Figure 5 shows the ROC curves study variables in predicting mortality in inpatients
Table 7.
Receiver operating characteristic (ROC) curve analysis to distinguish between patients with and without mortality in hospitalized COVID-19 patients with the markers studied
Discussion
The results of present study confirmed that PNI was a useful marker of inpatient treatment requirement and mortality in Covid-19 population. Moreover, PNI was also useful in predicting mortality in Covid-19 patients whom required treatment in hospital.
Calculation of PNI is dependent to two variables, serum albumin and blood lymphocyte count. Serum albumin is a negative acute phase marker meaning its serum level is reduced during inflammatory conditions10,11. On the other hand, reduced lymphocyte count has been found to be associated with poor prognosis in several conditions12–14. Thus, serum albumin and blood lymphocyte count together pose a better predictor of outcome in inflammatory conditions. Accordingly, we reported reduced PNI in subjects required treatment as inpatients compared to outpatients and in deceased patients compared to the survivors. These data suggest that PNI could be a reliable marker of prognosis in Covid-19.
The prognostic role of PNI has been well established in medical literature. Authors studied the role of PNI in patients received gastrointestinal surgery and reported that PNI was useful in estimation of the risk of surgery and in estimation of the subjects that require preoperative nutritional support15. Nozoe et al. investigated the efficacy of PNI in determination of the prognosis in subjects with colorectal carcinoma and claimed that preoperative PNI could be a reliable predictor of patient outcome in these subjects16. In addition, authors introduced PNI as a marker of poor overall survival in subjects with hepatocellular carcinoma17. These studies were followed by another study which reported PNI was a useful indicator of prognosis in breast cancer patients18. Subsequently, Okada et al.'s study showed that PNI was a useful predictor of postoperative complications and mortality in patients with non-small cell lung cancer19. PNI was also suggested as a novel prognostic index in subjects with malignant mesothelioma20. In a recent meta-analysis, PNI has been suggested as an effective indicator of outcome in patients with malignant conditions, especially gastrointestinal cancers21. Cancer is associated with continuous, low grade inflammatory burden as Covid-19 infection do. In accordance with the literature knowledge, in present study, we reported reduced PNI levels in inpatients compared to outpatients, in deceased compared to survived subjects and in deceased inpatients compared to survived inpatient subjects.
Not only malignant diseases but also other chronic conditions were associated with PNI. Authors suggested that PNI was a prognostic predictor in patients with cirrhosis22. Cheng et al. studied the association between PNI and survival in patients hospitalized for acute heart failure and found that PNI was an independent predictor of long term survival in this population23. Furthermore, PNI was associated with long-term cardiovascular outcomes in patients with stable coronary arterial disease24. Recently, authors studied PNI in subjects with aortic dissection and found that reduced PNI was associated with increased mortality25. Moreover, decreased levels of PNI has been found to be associated with development of contrast agent associated acute kidney injury in patients with acute myocardial infarction26. Cirrhosis, heart failure, aortic dissection and coronary artery disease are associated with some level of inflammation. Therefore, similar association between prognosis and PNI reported in present work is a result which consistent with literature data.
Retrospective design, which make impossible to control other variables, is a limitation of our study. Single center nature is another limitation of present work. However, this is the first study in literature that reported decreased PNI in deceased Covid-19 subjects compared to survived patients.
Conclusion
We suggest that PNI could serve as a reliable prognostic index in covid-19 patients. Reduced level of PNI should alert physicians since it is associated with need for hospitalization and mortality in this population.
Figure 1.
Serum albumin and PNI inpatient treatment in Covid-19 subjects
Acknowledgments
There are no acknowlegments for this article.
Declaration of funding
The authors have received no funding with respect to research, authorship, and/or publication of this article.
Declaration of financial/other relationships
The authors have no conflicts of interest.
Ethical Approval
This study was approved by ethics committee of Abant Izzet Baysal University (date: 9th of November, 2021; decision no: 2021/266).
Availability of data and materials
Data are available by corresponding author upon reasonable requests
References
- 1.Wei W, Wu X, Jin C, et al. Predictive Significance of the Prognostic Nutritional Index (PNI) in Patients with Severe COVID-19. J Immunol Res. 2021;2021:9917302. doi: 10.1155/2021/9917302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang L, Tian D, Liu W. [Strategies for vaccine development of COVID-19] Sheng Wu Gong Cheng Xue Bao. 2020;36(4):593–604. doi: 10.13345/j.cjb.200094. [DOI] [PubMed] [Google Scholar]
- 3.Aktas G. A comprehensive review on rational and effective treatment strategies against an invisible enemy; SARS Cov-2 infection. Exp Biomed Res. 2020;3(4):293–311. doi: 10.30714/j-ebr.2020463629. [DOI] [Google Scholar]
- 4.Dupont R, Longué M, Galinier A, et al. Impact of micronutrient deficiency & malnutrition in systemic sclerosis: Cohort study and literature review. Autoimmun Rev. 2018;17(11):1081–1089. doi: 10.1016/j.autrev.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Raposeiras Roubín S, Abu Assi E, Cespón Fernandez M, et al. Prevalence and Prognostic Significance of Malnutrition in Patients With Acute Coronary Syndrome. J Am Coll Cardiol. 2020;76(7):828–840. doi: 10.1016/j.jacc.2020.06.058. [DOI] [PubMed] [Google Scholar]
- 6.Lelijveld N, Kerac M, Seal A, et al. Long-term effects of severe acute malnutrition on lung function in Malawian children: a cohort study. Eur Respir J. 2017;49(4) doi: 10.1183/13993003.01301-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Capitanio U, Montorsi F. Does preoperative nutritional status affect survival in renal cell carcinoma? The debate continues. Eur Urol. 2011;59(6):929–930. doi: 10.1016/j.eururo.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Sueta D, Hokimoto S, Sakamoto K, et al. Validation of the high mortality rate of Malnutrition-Inflammation-Atherosclerosis syndrome: -Community-based observational study. Int J Cardiol. 2017;230:97–102. doi: 10.1016/j.ijcard.2016.12.072. [DOI] [PubMed] [Google Scholar]
- 9.Freeman AM, Morris PB, Barnard N, et al. Trending Cardiovascular Nutrition Controversies. J Am Coll Cardiol. 2017;69(9):1172–1187. doi: 10.1016/j.jacc.2016.10.086. [DOI] [PubMed] [Google Scholar]
- 10.Don BR, Kaysen G. Poor nutritional status and inflammation: serum albumin: relationship to inflammation and nutrition. Semin Dial. 2004;17(6):432–437. doi: 10.1111/j.0894-0959.2004.17603.x. [DOI] [PubMed] [Google Scholar]
- 11.Kaysen GA, Dubin JA, Müller HG, Rosales L, Levin NW, Mitch WE. Inflammation and reduced albumin synthesis associated with stable decline in serum albumin in hemodialysis patients. Kidney Int. 2004;65(4):1408–1415. doi: 10.1111/j.1523-1755.2004.00520.x. [DOI] [PubMed] [Google Scholar]
- 12.Feng F, Zheng G, Wang Q, et al. Low lymphocyte count and high monocyte count predicts poor prognosis of gastric cancer. BMC Gastroenterol. 2018;18(1):148. doi: 10.1186/s12876-018-0877-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu D, Wang Y, Zhao B, et al. Overall reduced lymphocyte especially T and B subsets closely related to the poor prognosis and the disease severity in severe patients with COVID-19 and diabetes mellitus. Diabetol Metab Syndr. 2021;13(1):5. doi: 10.1186/s13098-020-00622-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khalid A, Ali Jaffar M, Khan T, et al. Hematological and biochemical parameters as diagnostic and prognostic markers in SARS-COV-2 infected patients of Pakistan: a retrospective comparative analysis. Hematology. 2021;26(1):529–542. doi: 10.1080/16078454.2021.1950898. [DOI] [PubMed] [Google Scholar]
- 15.Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. 1980;139(1):160–167. doi: 10.1016/0002-9610(80)90246-9. [DOI] [PubMed] [Google Scholar]
- 16.Nozoe T, Kohno M, Iguchi T, et al. The prognostic nutritional index can be a prognostic indicator in colorectal carcinoma. Surg Today. 2012;42(6):532–535. doi: 10.1007/s00595-011-0061-0. [DOI] [PubMed] [Google Scholar]
- 17.Pinato DJ, North BV, Sharma R. A novel, externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the prognostic nutritional index (PNI) Br J Cancer. 2012;106(8):1439–1445. doi: 10.1038/bjc.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohri T, Mohri Y, Shigemori T, Takeuchi K, Itoh Y, Kato T. Impact of prognostic nutritional index on long-term outcomes in patients with breast cancer. World J Surg Oncol. 2016;14(1):170. doi: 10.1186/s12957-016-0920-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okada S, Shimada J, Kato D, Tsunezuka H, Teramukai S, Inoue M. Clinical Significance of Prognostic Nutritional Index After Surgical Treatment in Lung Cancer. Ann Thorac Surg. 2017;104(1):296–302. doi: 10.1016/j.athoracsur.2017.01.085. [DOI] [PubMed] [Google Scholar]
- 20.Yao ZH, Tian GY, Wan YY, et al. Prognostic nutritional index predicts outcomes of malignant pleural mesothelioma. J Cancer Res Clin Oncol. 2013;139(12):2117–2123. doi: 10.1007/s00432-013-1523-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun K, Chen S, Xu J, Li G, He Y. The prognostic significance of the prognostic nutritional index in cancer: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2014;140(9):1537–1549. doi: 10.1007/s00432-014-1714-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. 2005;21(2):113–117. doi: 10.1016/j.nut.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Cheng YL, Sung SH, Cheng HM, et al. Prognostic Nutritional Index and the Risk of Mortality in Patients With Acute Heart Failure. J Am Heart Assoc. 2017;6(6) doi: 10.1161/jaha.116.004876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wada H, Dohi T, Miyauchi K, et al. Relationship between the prognostic nutritional index and long-term clinical outcomes in patients with stable coronary artery disease. J Cardiol. 2018;72(2):155–161. doi: 10.1016/j.jjcc.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 25.Keskin HA, Kurtul A, Esenboğa K, Çiçek MC, Katırcıoğlu SF. Prognostic nutritional index predicts in-hospital mortality in patients with acute Stanford type A aortic dissection. Perfusion. 2021;36(7):710–716. doi: 10.1177/0267659120961937. [DOI] [PubMed] [Google Scholar]
- 26.Kurtul A, Gok M, Esenboga K. Prognostic Nutritional Index Predicts Contrast-Associated Acute Kidney Injury in Patients with ST-Segment Elevation Myocardial Infarction. Acta Cardiol Sin. 2021;37(5):496–503. doi: 10.6515/acs.202109_37(5).20210413a. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available by corresponding author upon reasonable requests