Abstract
Brown Tumour or Osteitis fibrous cystic or Von-Recklinghausen disease of bone is a non-malignant condition due to abnormal metabolism of bones in hyperparathyroidism. Although pathognomonic of hyperparathyroidism, brown tumours are rare and only case reports are found in literature. We report a case of brown tumour of mandible with recurrent episodes of bleeding. A 46 year old male patient presented in emergency with bleeding from ulceroproliferative mass from left floor of mouth. After control of bleeding, radiological, laboratory and histopathological investigations were done that led to the diagnosis of brown tumour of mandible in the presence of parathyroid adenoma of left lower parathyroid gland. Left upper and lower parthyroidectomy was done with segmental resection of mandible with mass and titanium plating. Brown tumour of facial bones is a rare entity. Very rarely it can reach enormous sizes to cause bleeding. Although parathyroidectomy and correction of parathormone levels cause regression of small tumours, large brown tumours with complications should be managed with surgical resection and reconstruction.
Keywords: Brown tumour, Mandible, Left, Segmental
Introduction
Hyperparathyroidism is a complex endocrine abnormality resulting from increased levels of parathormone. It can be primary, secondary and tertiary depending on the etiology [1]. Parathyroid adenomas are most common cause of primary hyperparathyroidism followed by 4 gland hyperplasia [2]. Brown tumours are non-malignant, non-neoplastic tumours formed due to increased bone metabolism in the presence of increased levels of parathormone. They are called brown tumours due to their gross appearance as a result of haemorrhage and hemosiderin deposition [3]. Brown tumours are in general rare entities and seen in chronic uncontrolled cases of hyperparathyroidism [4]. We present a rare case of a large brown tumour of mandible presenting as bleeding in emergency.
Case Report
A 46 year old male presented in emergency with bleeding from ulcero-proliferative mass of left floor of mouth along with swelling of left jaw. (Fig. 1) Patient had this mass since 5–6 months and there was no history of trauma. There was no history of any clinical symptoms or similar swellings elsewhere in the body. On examination there was an ulcer-proliferative mass of 5 × 4 cm in the left floor of mouth involving gingivobuccal sulcus and associated with left mandibular swelling. The mass pushed away the tongue to opposite side. (Fig. 2) There was active bleeding at presentation which was controlled by suturing and electrocautery. On CECT scan 56 × 36 × 62 mm lobulated, well defined, expansile, lytic and multi-septated mass was seen arising from left mandible with 48 × 25 mm intraoral component. (Fig. 3, 4) Also, 21 × 22 × 23 mm well defined septated altered signal intensity was noted in posterior region of left lobe of thyroid. (Fig. 5) Tc-99 m MIBI scan revealed intensely increased tracer localisation just adjacent to lower pole of left lobe of thyroid gland. These radiological investigations suggested parathyroid adenoma with brown tumour of mandible. Biopsy of mass consistent with brown tumour. Serum PTH levels were > 2500 pg/ml, serum calcium 13.2 mg/dl, serum phosphate 2.4 mg/dl, serum alkaline phosphatase 557 U/L, thyroid function test and renal function test were normal. All investigations confirmed the diagnosis of parathyroid adenoma with primary hyperparathyroidism with brown tumour of mandible. Since it was a large and ulcerated mass with bleeding, surgical excision was planned. 3D model was prepared for proper planning of surgery. (Fig. 6, 7) Patient was operated for left upper and lower parathyroidectomy with excision of mass and segmental mandibulectomy with titanium plating. (Fig. 8) Intra-operative serum PTH levels had decreased to less than 50% of preoperative values which suggested adequate parathyroidectomy. Histopathology confirmed the diagnosis of parathyroid adenoma of left lower parathyroid 3.5 × 2 × 1 cm and brown tumour of mandible 9 × 6.5 × 5 cm which is largest brown tumour of mandible in Asia. (Fig. 9) Post operative course of patient was uneventful and serum PTH declined further. Patient had an excellent cosmetic outcome. On follow up after 1 year Patient had no complaints and patients serum PTH levels were 25.3 pg/ml (normal).
Fig. 1.

Photograph of patient showing left jaw swelling
Fig. 2.

Intraoral photograph showing mass arising from floor of mouth with deviated tongue
Fig. 3.
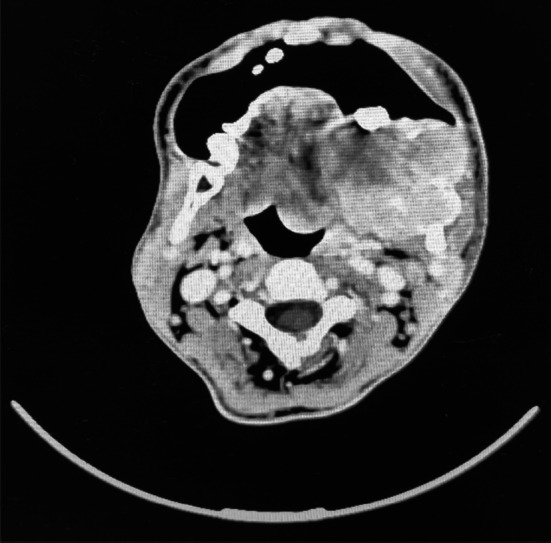
CECT image showing mass arising from left mandible
Fig. 4.
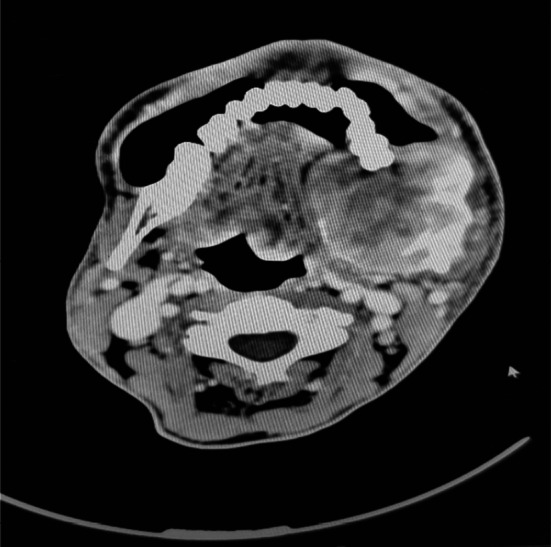
CECT showing 56 x 26 x 62 mm mass with intraoral component and tongue deviation
Fig. 5.
CECT showing left parathyroid adenoma
Fig. 6.

3D acrylic model of mandible - anterior view
Fig. 7.

3D acrylic model of mandible - superior view
Fig. 8.
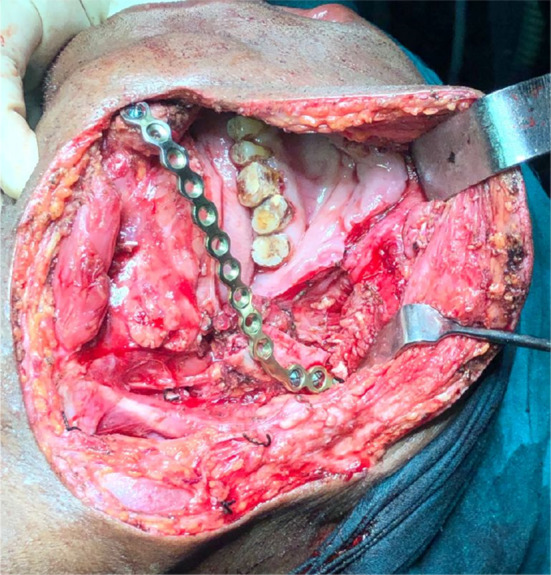
Intraoperative photograph showing defect post excision and titanium plate
Fig. 9.
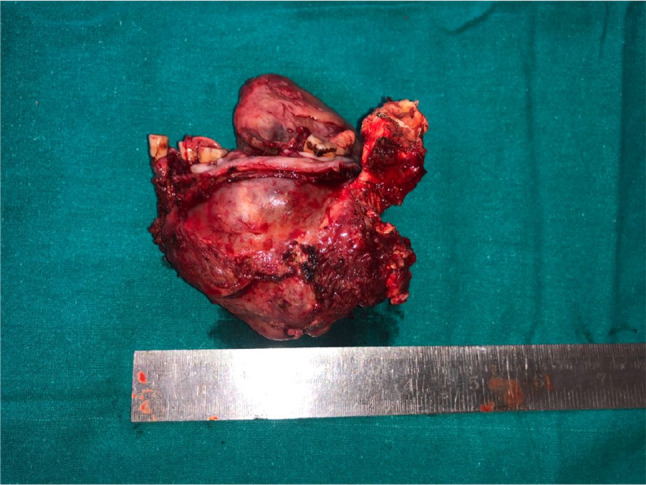
Photograph of pathological specimen
Discussion
Hyperparathyroidism can cause brown tumour affecting skeletal system throughout body [5]. Generally, these tumours are small in size and often multiple and asymptomatic and do not require treatment other than controlling hyperparathyroidism [6]. Interesting aspect of our case report is that our patient presented with bleeding from ulcerated brown tumour as initial presentation of primary hyperparathyroidism. Review of literature report cases causing facial disfigurement, speech difficulty, chewing difficulty, etc. but none reports bleeding as initial presentation [7]. It is advised that surgical resection of brown tumour is not required and it generally regress after adequate control of PTH levels post parathyroidectomy [8, 9]. According to review of literature conducted by Can O et al. in 2016, most of the cases of facial bone brown tumor were managed by adequate parathyroidectomy without surgical resection. But many of these failed to regress and recurred after follow up inspite of adequate serum PTH levels [10].
In our case since patient had episodes of bleeding and facial disfigurement, a decision of surgical excision of tumour with segmental mandibulectomy with titanium plate reconstruction was taken which gave patient excellent symptomatic relief and cosmetic outcome. After 1 year follow up patient had no complaints and patients serum PTH levels were normal.
Conclusion
With this case report we suggest that in patients with large browns tumour of facial bones having complications and facial disfigurement, surgical resection along with reconstruction should be considered in addition to adequate parathyroidectomy for speedy recovery and immediate symptomatic relief.
Abbreviations
- CECT
Contrast enhanced computed tomography
- Tc99-MIBI
Technetium 99 metoxyisobutyl isonitrile scan
- PTH
Parathormone
Funding
None.
Declarations
Conflict of interest
The authors declare no conflict of interests.
Ethical Approval
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shetty AD, Namitha J, James L. Brown tumor of mandible in association with primary hyperparathyroidism: a case report. J Int Oral Health. 2015;7(2):50–52. [PMC free article] [PubMed] [Google Scholar]
- 2.Xu B, Yu J, Lu Y, et al. Primary hyperparathyroidism presenting as a brown tumour in the mandible: a case report. BMC Endocr Discord. 2020;20:6. doi: 10.1186/s12902-019-0480-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Selvi F, Cakarer S, Tanakol R, Guler SD, Keskin C. Brown tumour of the maxilla and mandible: a rare complication of tertiary hyperparathyroidism. Dentomaxillofac Radiol. 2009;38(1):53–8. doi: 10.1259/dmfr/81694583. [DOI] [PubMed] [Google Scholar]
- 4.Agnihotri M, Kothari K, Naik L. Brown tumour of hyperparathyroidism. Diagn Cytopathol. 2017;45:43–44. doi: 10.1002/dc.23631. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg EH, Guralnic WC. Hyperparathyroidism. A review of 220 proved cases with special emphasis on findings in the jaws. Oral Surg. 1962;157(11):82–93. [Google Scholar]
- 6.Popovik-Monevska D, Bozovik-Dvojakovska S, Popovski V, Benedetti A, Grchev A, Koneski F. Brown tumour in the mandible and skull osteosclerosis associated with primary hyperparathyroidism—a case report. Open Access Maced J Med Sci. 2018;6(2):406–409. doi: 10.3889/oamjms.2018.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Can O, Boynuegri B, Gokce AM, et al. Brown tumours: A case report and review of the literature. Case Rep Nephrol Dial. 2016;6(1):46–52. doi: 10.1159/000444703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zwick OM, Vaqefi MR, Cockerham KP, McDermott MW. Brown tumour of secondary hyperthyroidism involving the superior orbit and frontal calvarium. Opthak Plant Reconstr Surg. 2006;22:304–306. doi: 10.1097/01.iop.0000225744.19613.3d. [DOI] [PubMed] [Google Scholar]
- 9.Kulak CA, Bandeira C, Voss D, Sobieszczyk SM, Silverberg SJ, Bandeira F, et al. Marked improvement in bone mass after parathyroidectomy in osteitis fibrous cystic. J Clin Endocrinol Metab. 1998;83(3):732–5. doi: 10.1210/jc.83.3.732. [DOI] [PubMed] [Google Scholar]
- 10.Leal CT, Lacativa PG, Gomes EM, et al. Surgical approach and clinical outcome of a deforming brown tumour at the maxilla in a patient with secondary hyperparathyroidism due to chronic renal failure. Are Bras Endocrinol Metabol. 2006;50:963–967. doi: 10.1590/S0004-27302006000500021. [DOI] [PubMed] [Google Scholar]



