Abstract
The aim of the study was to investigate the relations between anatomical structures that are susceptible to inadvertent injuries during the surgery using preoperative computed tomography (CT) scans. 153 CT scans were reviewed and the distance from the lamina papyracea (LP) to the midline and the distance of the anterior ethmoidal artery (AEA) to the skull base were measured bilaterally. Also, the depth of olfactory fossa was measured and categorized using the Keros classification. The measurements were analyzed to determine whether LP-to-midline distance was correlated with the distance between the AEA and the skull base and Keros classification. Additionally, correlation of Keros classification with the distance from the AEA to the skull base was investigated. In a total of 306 measurements, 26 (%8.49) were classified as Keros type I, 200 (65.35%) as Keros type II and 80 (25.14%) as Keros type III. Statistically, LP-to-midline distances on the right and left sides were significantly associated with the distance from the AEA to the skull base on the same side (R:p < 0.001, L:p = 0.01) and the Keros classification on the same side (R:p < 0.001, L:p = 0.004). Also, a significant association was found between the Keros classification and the distance from the AEA to the skull base (R:p < 0.001, L:p = 0.02). The locations of anatomical structures are defined in relation to each other during the development of maxillofacial bones. CT scans should be examined and anatomical structures and relations among them reviewed very carefully before ESS. Otherwise, some accidental injuries may arise during the surgery while trying to avoid complications.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12070-023-03931-x.
Keywords: Paranasal sinuses, Computerized tomography, Skull base, Keros classification, Anterior ethmoidal artery
Introduction
Endoscopic sinus surgery (ESS) is a surgical procedure used in many conditions such as inflammatory and neoplastic pathologies of the nasal cavity and paranasal sinuses [1]. Paranasal sinus computed tomography (CT) imaging is routinely obtained prior to ESS. In addition to examination of nasal pathology with CT, preoperative assessment of the anatomical structures and the relations between anatomical structures is essential.
Various minor and major complications may occur even in the case of extensive surgical experience of the operating surgeon. These complications include orbital hematoma, orbital subcutaneous emphysema, diplopia, blindness due to damage to lamina papyracea, hemorrhages related to anterior ethmoidal artery (AEA) injury, and cerebrospinal fluid leak and meningitis associated with trauma to the skull base [2, 3]. As well as experience and a good knowledge of anatomy, careful examination of CT sections preoperatively and also revisiting CT sections during the surgery, if necessary, has a key role in preventing complications.
There are studies in the literature that reported the relations between AEA and the ethmoid cavity [4, 5] and between AEA and the Keros classification [6]. In the present study, we explored whether the distance from the lamina papyracea to the midline was correlated with the distance from the AEA to the skull base and the Keros classification. Additionally, vertical and horizontal diameters of the ethmoid bulla air cells and the distance from the ethmoid bulla to the skull base were measured and its relations with anatomical structures was examined. Identification of the anatomical location of the lamina papyracea, the depth of the olfactory fossa and the position of the AEA within the nasal cavity is critical to avoid serious intraoperative complications.
The aim of the current study was to determine whether the distance from the lamina papyracea to the midline was correlated with the Keros classification and the distance from the AEA to the skull base and to highlight the importance of taking into account these relations when examining CT scans preoperatively.
Materials and methods
Patients from 18 to 65 years of age presenting to otorhinolaryngology clinic who underwent paranasal sinus CT imaging between February 2019 and February 2020 were included in the study. Computed tomography scans were retrospectively reviewed which were mostly obtained for a diagnosis of sinusitis, facial pain or before septoplasty/ septorhinoplasty surgery. Patients were excluded if they had altered skull base anatomy from prior surgical intervention, allergic fungal sinusitis, trauma, fibrous dysplasia, or other conditions causing distortion of sinunasal bony anatomy.
A total of 153 CT scans from 306 sides were included in the study and all measurements were performed by the same radiologist. All scans were acquired in 0.6 mm slice thickness (Rotation Time − 0.6 s, Pitch & Speed − 0.984:1–39.37 mm/rotation, 100 kV, 50 mA) using the 128-channel MDCT scanner (Revolution EVO CT, General Electric Healthcare, Milwaukee, Wisconsin, USA) in the bone window. All radiographic measurements were obtained using the institutional PACS system (SARUS workstation 3.2.2.1).
On CT, the distance from lamina papyracea to the midline bilaterally, the distance from the AEA to the skull base bilaterally, vertical and horizontal diameters of the ethmoid bulla bilaterally and the distance from the ethmoid bulla to the skull base and the depth of olfactory fossa bilaterally were measured and evaluated separately.
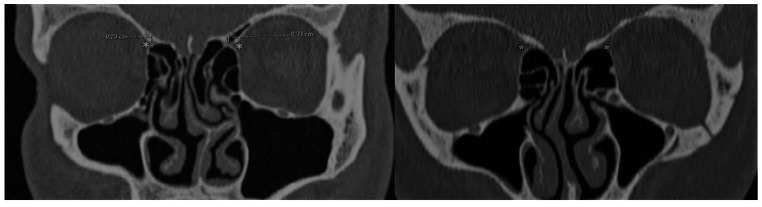
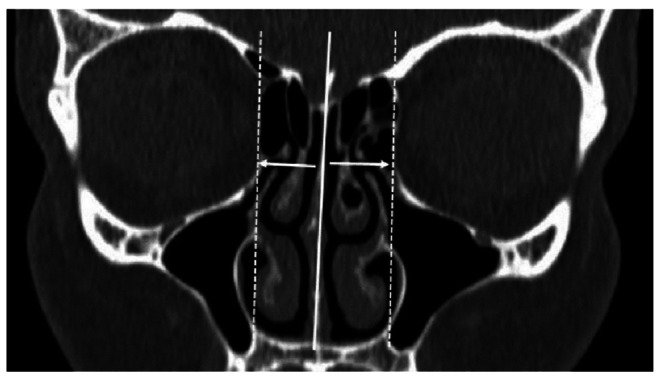
The distance from the lamina papyracea to the midline was defined as the distance from the most medial point of the lamina papyracea to the median line passing vertically through the crista galli (Fig. 1). When measuring the distance from the AEA to the skull base, it was considered 0 mm if the artery was adjacent to the skull base and the vertical distance of the artery from its medial point in the nasal cavity to the skull base was obtained if the artery ran separately from the skull base (Fig. 2). For ethmoid bulla measurements, both coronal and axial sections were examined to determine the vertical and horizontal diameters of the ethmoidal cell and measure the distance from the ethmoid bulla to the skull base in the coronal plane. The vertical distance between fovea ethmoidalis and cribriform plate along the lateral lamella was measured and categorized using the Keros classification as Keros type I: 1–3 mm, Keros type II: 3.1-7 mm, Keros type III: greater than 7 mm (Fig. 3). The study parameters were measured separately for right and left sides of the nasal cavity to investigate their correlations.
Fig. 1.
Coronal section of paranasal sinus computed tomography showing the measurement of the distance of the lamina papyracea to the midline on both sides
Fig. 2.
Coronal section of paranasal sinus computed tomography showing the measurement of the distance from the anterior ethmoidal artery to the skull base
* Anterior ethmoidal artery
Fig. 3.
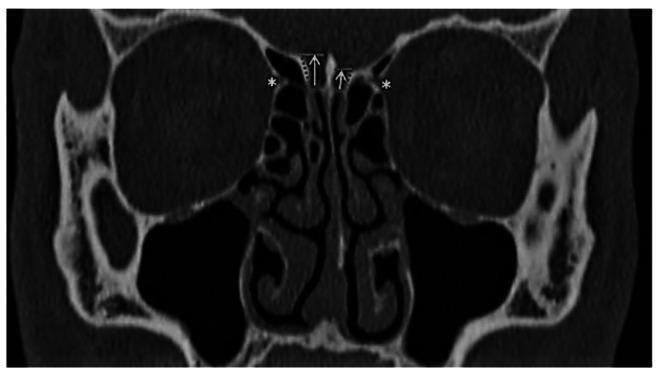
Coronal section of paranasal sinus computed tomography showing the measurement of the depth of the olfactory fossa
* Anterior ethmoidal artery
Ethics Approval
was obtained from the institutional review board prior to initiation of the study.
Statistical Analysis
Continuous, normally distributed data were expressed as mean ± SD, and non-normally distributed data as median with minimum-maximum range. Categorical data were presented as numbers and percentages. The Kolmogorov-Smirnov test was used to check whether the data was normally distributed or not. Spearman rank correlation coefficient was computed to assess correlations among paranasal measurement parameters. P values less than 0.05 were deemed statistically significant. The SPSS statistical software (SPSS for Windows, version 21.0; SPSS Inc., Chicago, IL, USA) was used for all statistical calculations.
Results
Of 153 CT scans meeting the study inclusion criteria, 78 (50.9%) belonged to male patients and 75 (49.1%) belonged to female patients. The mean age of the patients was 33.04 ± 12.30 years. The median distance from right LP to the midline was 12 mm (8–15) and the median distance from left LP to the midline was 12 mm (9–15). On the right side, the mean distance between the AEA and the skull base was 2.83 ± 1.94 mm. The artery ran parallel along the skull base in 24 (15.6%) scans. The longest distance from the AEA to the skull base was 11 mm. On the left side, the mean distance from the AEA to the skull base was 2.89 ± 1.90 mm and in 23 (15%) scans, the AEA ran along the skull base. The longest distance measured between the artery and the skull base was 9 mm.
The median vertical length of the ethmoid bulla was 13 mm on the right side (7–25) and 13.78 ± 3.92 mm on the left side. The median horizontal length of the ethmoid bulla was 8 mm (4–17) on the right side and 8 mm (4–14) on the left side. The average distance from the ethmoid bulla to the skull base was 9.28 ± 5.08 mm on the right side and 9.10 ± 4.39 mm on the left side. The shortest distance measured between the ethmoid bulla and the skull base was 1 mm bilaterally. LP-to-midline distance, the distance from the AEA to the skull base and the diameters of the ethmoidal bulla as measured by CT are shown in Table 1. Keros type I was identified in 26 (8.5%) scans, Keros type II in 200 (65.4%) scans and Keros type III in 80 (25.1%) scans (Table 2). Measurements of 50 (32.6%) patients showed asymmetry between the right and left sides based on Keros classification.
Table 1.
Paranasal computed tomography measurements
| LP-Midline (mm) | AEA-SB (mm) |
EB vertical diameter (mm) | EB horizontal diameter (mm) | EB-SB (mm) | |
|---|---|---|---|---|---|
| Right | 12 (8–15) | 2.83 ± 1.94 | 13 (7–25) | 8 (4–17) | 9.28 ± 5.08 |
| Left | 12 (9–15) | 2.89 ± 1.90 | 13.78 ± 3.92 | 8 (4–14) | 9.10 ± 4.39 |
All values are mean ± SD, median with minimum-maximum range
LP, Lamina papyracea; AEA, Anterior ethmoidal artery; SB, Skull base; EB, Ethmoidal bulla
Table 2.
Distribution of Keros classification
| Keros Type | Right | Left | Total | |||
|---|---|---|---|---|---|---|
| n | Percentage | n | Percentage | n | Percentage | |
| I | 17 | 11.1 | 9 | 5.9 | 26 | 8.5 |
| II | 98 | 64 | 102 | 66.7 | 200 | 65.4 |
| III | 38 | 24.9 | 42 | 27.4 | 80 | 26.1 |
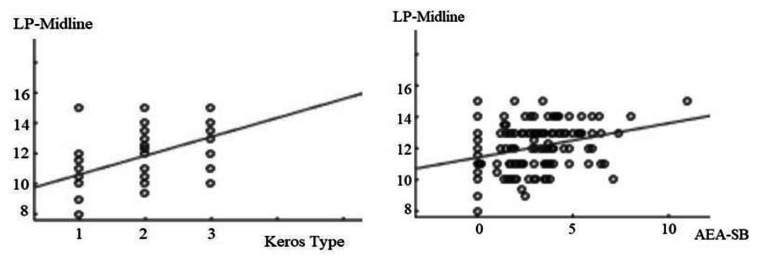
Statistically, right side LP-to-midline distance showed significant associations with right side Keros classification (p < 0.001) and right side AEA distance to the skull base (p < 0.001) (Fig. 4) and left side LP-to-midline distance was significantly associated with left side Keros classification (p = 0.004) and left side AEA distance to the skull base (p = 0.01) (Fig. 5) (Table 3).
Fig. 4.
Correlations of the distance from the lamina papyracea to the midline with the Keros classification and the distance between the anterior ethmoidal artery and the skull base on right side
LP, Lamina papyracea; AEA, Anterior ethmoidal artery; SB, Skull base
Fig. 5.
Correlations of the distance from the lamina papyracea to the midline with the Keros classification and the distance between the anterior ethmoidal artery and the skull base on left side
LP, Lamina papyracea; AEA, Anterior ethmoidal artery; SB, Skull base
Table 3.
Correlations of the distance from the lamina papyracea to the midline with the Keros classification and the distance between the anterior ethmoidal artery and the skull base on the same side
| p | r | ||
|---|---|---|---|
| Right LP-to-Midline | Right side Keros classification | < 0.001 | 0.51 |
| Right side AEA-SB | < 0.001 | 0.28 | |
| Left LP-to-Midline | Left side Keros classification | 0.004 | 0.23 |
| Left side AEA-SB | 0.01 | 0.29 | |
LP, Lamina papyracea; AEA, Anterior ethmoidal artery; SB, Skull base
In addition, LP-to-midline distances measured on the right and left sides were positively correlated with the transverse diameter of the ethmoid bulla on the corresponding side (R: p < 0.001, L: p = 0.002). Also, Keros classification for the right and left sides was positively correlated with the AEA distance to the skull base on the corresponding side (R: p < 0.001, L: p = 0.02) (Table 4). A positive correlation was found between the distance from the ethmoid bulla to the skull base and the distance of the AEA to the skull base in both sides (R: p < 0.001, L: p < 0.001).
Table 4.
Correlation of Keros classification and the distance from the anterior ethmoidal artery to the skull base on the same side
| p | r | ||
|---|---|---|---|
| Right side Keros classification | Right side AEA-SB | < 0.001 | 0.41 |
| Left side Keros classification | Left side AEA-SB | 0.02 | 0.29 |
AEA, Anterior ethmoidal artery; SB, Skull base
Discussion
Even with long-term experience of surgeons in performing ESS, complications may arise during or after the surgery. In a systematic review published in 2006, potentially most serious complications included cerebrospinal fluid leaks, bleeding requiring transfusion, periorbital/orbital fat exposure and orbital penetration [7]. A study that examined variations in LP position based on localization by middle meatal antrostomy aimed to improve awareness of LP variations among surgeons [8]. In a study by Özcan et al. reported that the lamina papyracea was located more medially in individuals with maxillary hypoplasia, leading to a higher risk of complications during the ESS [9]. Our study is the first to examine relations among LP position, the depth of olfactory fossa and location of anterior ethmoidal artery, all of which may be associated with the risk of accidental injuries.
Keros type II was most commonly observed in our study, in line with previous studies. While Keros type II was the most common and Keros type III was the least common in some studies [6, 10–12], others found most commonly Keros type II and Keros type I least commonly [13, 14]. Keros type II was also the most prevalent type and Keros type I was the least common type in our study. Since the depth of olfactory fossa is greatest in Keros type III, it is regarded as the most dangerous category. The depth of olfactory fossa must be evaluated by CT imaging before the surgery to avoid potential complications. Keeping in mind that the depth of fossa might be affected by the development and position of surrounding structures during the evolution of paranasal sinuses and maxillofacial bones, we examined the correlation of the distance between LP to the midline with the Keros classification. We found that the olfactory fossa was situated deeper as the distance of LP from the midline increased. This finding suggests that the risk of injury to the skull base may increase when there is a lower possibility of orbital penetration.
To our best knowledge, there is no published study which evaluated the relations of LP-to-midline distance with other parameters. Our study showed that as the distance of lamina papyracea increases from the midline, the olfactory fossa deepens and the anterior ethmoidal artery is located far from the skull base. The location of the anterior ethmoidal artery and even the Keros classification may not always be fully evaluated on preoperative CT scans due to extensive nasal pathology. In light of these data, one may have an idea on the depth of the olfactory fossa, Keros classification and the location of the anterior ethmoidal artery through an assessment of the distance of the lamina papyracea to the midline. Skorek et al. suggested a new definition of “dangerous ethmoid” based on the width of the olfactory fossa and its distance to the medial concha and to the medial wall of the orbit in addition to Keros classification [13].
In a study by Poteet et al., a positive correlation was found between the distance from the anterior ethmoidal artery to the skull base and Keros classification [6]. Consistently, we found increased distance between the anterior ethmoidal artery and the skull base as the depth of the olfactory fossa increased. Therefore, Keros classification may give an idea about the location of the anterior ethmoidal artery before the surgery. The distance from the anterior ethmoidal artery to the skull base is reduced when LP is located closer to the midline and the AEA may run adjacent to the skull base.
In a study investigating anatomical variations of the paranasal sinuses, large ethmoid bulla was detected at a rate of 10% within the ethmoidal variations grouped together [15]. Bortoli et al. examined the distance from the AEA to the ethmoidal bulla and found that this distance was shorter in individuals under 12 years of age than in individuals over 12 years of age [16]. The distance between the anatomical structures and their relations may change with age. In the current study, the vertical and horizontal diameters of the ethmoid bulla cell were measured to identify their correlations with other parameters. A positive correlation was found between the distance from lamina papyracea to the midline and the horizontal diameter of the ethmoid bulla. Since the horizontal diameter of the ethmoidal bulla becomes smaller with closer location of the lamina papyracea to the midline, care should be exercised to avoid orbital penetration when performing anterior ethmoidectomy. A positive correlation was also identified between the distance of ethmoid bulla to the skull base and the distance from the anterior ethmoidal artery to the skull base.
Conclusion
In conclusion, we found that the distance from the lamina papyracea to the midline was positively correlated with Keros classification and the distance from the anterior ethmoidal artery to the skull base. In addition, Keros classification correlated with the distance from the anterior ethmoidal artery to the skull base. CT scans should be examined and anatomical structures and relations among them reviewed very carefully before ESS. Otherwise, some accidental injuries may arise during the surgery while trying to avoid complications.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Funding
None.
Compliance with Ethical Standards
Ethical Rules
The study was conducted in accordance with the principles of the Helsinki Declaration and was approved with the 12/03/2020 dated and E1-20-386 numbered permission by the Ankara City Hospital Ethics Committee.
Informed Consent
None (Retrospective study).
Conflict of interest
The authors declare that there is no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Higgins TS, Lane AP. Chapter 12: surgery for sinunasal disease. Am J Rhinol Allergy. 2013;27(3):42–44. doi: 10.2500/ajra.2013.27.3897. [DOI] [PubMed] [Google Scholar]
- 2.Krings JG, Kallogjeri D, Wineland A, Nepple KG, Piccirillo JF, Getz AE. Complications of primary and revision functional endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2014;124(4):838–845. doi: 10.1002/lary.24401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stankiewicz JA, Lal D, Connor M, Welch K. Complications in endoscopic sinus surgery for chronic rhinosinusitis: a 25-year experience. Laryngoscope. 2011;121(12):2684–2701. doi: 10.1002/lary.21446. [DOI] [PubMed] [Google Scholar]
- 4.Pernas FG, Coughlin AM, Hughes SE, Riascos R, Maeso PA. A novel use of a landmark to avoid injury of the anterior ethmoidal artery during endoscopic sinus surgery. Am J Rhinol Allergy. 2011;25(1):54–57. doi: 10.2500/ajra.2011.25.3541. [DOI] [PubMed] [Google Scholar]
- 5.Han JK, Becker SS, Bomeli SR, Gross CW. Endoscopic localization of the anterior and posterior ethmoid arteries. Ann Otol Rhinol Laryngol. 2008;117(12):931–935. doi: 10.1177/000348940811701212. [DOI] [PubMed] [Google Scholar]
- 6.Poteet PS, Cox MD, Wang RA, Fitzgerald RT, Kanaan A. Analysis of the relationship between the location of the Anterior Ethmoid Artery and Keros classification. Otolaryngol Head Neck Surg. 2017;157(2):320–324. doi: 10.1177/0194599817696302. [DOI] [PubMed] [Google Scholar]
- 7.Dalziel K, Stein K, Round A, Garside R, Royle P. Endoscopic sinus surgery for the excision of nasal polyps: a systematic review of safety and effectiveness. Am J Rhinol. 2006;20(5):506–519. doi: 10.2500/ajr.2006.20.2923. [DOI] [PubMed] [Google Scholar]
- 8.Herzallah IR, Marglani OA, Shaikh AM. Variations of lamina papyracea position from the endoscopic view: a retrospective computed tomography analysis. Int Forum Allergy Rhinol. 2015;5(3):263–270. doi: 10.1002/alr.21450. [DOI] [PubMed] [Google Scholar]
- 9.Ozcan KM, Hizli O, Ulusoy H, Coskun ZU, Yildirim G. Localization of orbit in patients with maxillary sinus hypoplasia: a radiological study. Surg Radiol Anat. 2018;40(10):1099–1104. doi: 10.1007/s00276-018-2054-9. [DOI] [PubMed] [Google Scholar]
- 10.Babu AC, Nair M, Kuriakose AM. Olfactory fossa depth: CT analysis of 1200 patients. Indian J Radiol Imaging. 2018;28(4):395–400. doi: 10.4103/ijri.IJRI_119_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaplanoglu H, Kaplanoglu V, Dilli A, Toprak U, Hekimoglu B. An analysis of the anatomic variations of the paranasal sinuses and ethmoid roof using computed tomography. Eurasian J Med. 2013;45(2):115–125. doi: 10.5152/eajm.2013.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adeel M, Ikram M, Rajput MS, Arain A, Khattak YJ. Asymmetry of lateral lamella of the cribriform plate: a software-based analysis of coronal computed tomography and its clinical relevance in endoscopic sinus surgery. Surg Radiol Anat. 2013;35(9):843–847. doi: 10.1007/s00276-013-1106-4. [DOI] [PubMed] [Google Scholar]
- 13.Skorek A, Tretiakow D, Szmuda T, Przewozny T. Is the Keros classification alone enough to identify patients with the ‘dangerous ethmoid’? An anatomical study. Acta Otolaryngol. 2017;137(2):196–201. doi: 10.1080/00016489.2016.1225316. [DOI] [PubMed] [Google Scholar]
- 14.Mishra S, Chhetri ST, Pant AR, Shah SP, Manandhar S. Prevalence of dangerous ethmoid in a Tertiary Center in Eastern Nepal. JNMA J Nepal Med Assoc. 2019;57(219):311–314. doi: 10.31729/jnma.4637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alsowey AM, Abdulmonaem G, Elsammak A, Fouad Y. Diagnostic performance of Multidetector Computed Tomography (MDCT) in diagnosis of sinus variations. Pol J Radiol. 2017;82:713–725. doi: 10.12659/PJR.903684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bortoli VT, Martins RF, Negri KC. Study of anthropometric measurements of the Anterior Ethmoidal artery using three-dimensional scanning on 300 patients. Int Arch Otorhinolaryngol. 2017;21(2):115–121. doi: 10.1055/s-0037-1598598. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.