Abstract
Aims
In some cases, children with cleft palate undergo unnecessary tympanostomy along with palatoplasty because of inaccurate evaluations in determining the level of otitis media with effusion (OME). Recent studies have shown that wideband tympanometry (WBT) significantly contributes to the accurate evaluation of the middle ear status in children with cleft palate. Therefore, this study aimed to investigate WBT and auditory brainstem response (ABR) indices before and after cleft palate repair surgery.
Materials and Methods
The study involved 88 children with cleft palate, and ABR and WBT energy absorbance indices were measured in two phases. The first phase was conducted three months and three days prior to cleft palate repair surgery, and the second phase was carried out one, three, and six months after surgery.
Results
In the first phase, the energy absorbance index of low frequencies was below the normal range in all children, within the normal range at high frequencies in 78 children, and below the normal range in only 10 children three months before cleft palate surgery. In the second phase, the energy absorbance index and hearing thresholds at low frequencies after surgery showed a significant difference compared with the preoperative index (p = 0.001).
Conclusion
Monitoring WBT indices and hearing thresholds in children with cleft palate is effective in determining the appropriate surgery for children with otitis media with effusion (OME). Furthermore, the WBT plays a crucial role in accurately assessing middle ear function after cleft palate surgery.
Introduction
As a common congenital disorder, oral-facial clefts can occur in a syndromic or non-syndromic form [1]. Cleft palate is an example of a disorder that occurs when the palate fails to fuse during fetal growth [2]. Its prevalence has been reported to range from 0.18 to 0.77 per 1000 births in several studies [3–6]. Children with cleft palate are at a high risk for hearing loss [7], which can have a detrimental effect on their language, speech, and cognition development [8]. Therefore, it is crucial to monitor the hearing status of children with cleft palate. The eustachian tube is responsible for ventilating the middle ear by opening with the contraction of the tensor and levator veli palatini muscles [9]. This helps maintain air pressure balance in the middle ear. Improper air ventilation in the middle ear can result in negative pressure, leading to otitis [10]. In children with cleft palate, the eustachian tube is often severely blocked due to the inability of the tensor veli palatini muscle to open the tube during swallowing. This blockage is a significant contributing factor in the development of otitis media with effusion (OME) [11]. OME refers to the accumulation of fluid in the middle ear and has a high prevalence among children with cleft palate [12]. Kwan et al. reported an OME prevalence of up to 76.1%, with 16.9% of cases accompanied by at least moderate hearing loss [13].
Palatoplasty is the usual procedure performed to treat cleft palate and restore normal anatomy in children aged 6 to 12 months, leading to high satisfaction [14]. Studies have shown that palatoplasty has a positive impact on the opening of the eustachian tube during swallowing [15, 16]. For instance, Alper et al. reported that 39% and 62% of cases demonstrated eustachian tube opening before and after palatoplasty, respectively [16]. As a result, it is expected that middle ear ventilation will return to normal and OME will improve in some children after palatoplasty, eliminating the need for invasive procedures such as tympanostomy and the placement of ventilation tubes in the eardrum. The guidelines of the American Academy of Otolaryngology-Head and Neck Surgery Foundation (AAO-HNSF) recommend the use of tympanostomy tubes for children with cleft palate if they have type B tympanometry (using single-frequency tympanometry) and persistent OME for three months or longer [17]. Therefore, the use of tests that carefully monitor middle ear status and indicate improvement or lack thereof can help determine the necessity of invasive tympanostomy in children with cleft palate, potentially reducing the need for such interventions.
Tympanometry is a non-invasive test that examines sound wave transmission through the middle ear. The 226 Hz tympanometry is commonly used for clinical purposes [18]. Wideband tympanometry (WBT) is a new method for acoustic assessment of middle ear status over a wide frequency range [19]. It provides more comprehensive information about middle ear status compared to single-frequency tympanometry [20]. WBT can also assess broadband sound absorption indices at different frequencies and pressures [21].By conducting WBT before and after cleft palate repair surgery, it is possible to examine middle ear status and potentially avoid tympanostomy and ventilation tube placement if there is improvement in broadband tympanometric indices, confirmed by the outcome of brainstem auditory responses. Given the lack of studies on the improvement or non-improvement of wideband tympanometric indices before and after cleft palate surgery in children with OME, the present study aims to qualitatively examine WBT indices and the outcome of auditory brainstem responses before and after cleft palate repair surgery.
Methods
This clinical trail study was conducted at the Tohid audiology clinic and ISfahan cleft palate center. The study was approved by Shahid Beheshti university of medical sciences Ethics Commitee (approval Number IR.SBMU.RETECH.REC.1401.507), and it fulfilled the principles of the Declaration of Helsinki. Written informed consent were given by all the parents. all necessary considerations, including the consent of the participants and the confidentiality of their information, have been observed.
The study examined 88 children with cleft palate, consisting of 45 girls and 43 boys, with a mean age of 6.23 ± 0.17 months. The inclusion criteria were as follows: parental written consent, ages ranging from 6 to 9 months, presence of a sole cleft palate, bilateral otitis media with effusion and some degree of conductive hearing loss (CHL), and normal anatomy in the temporal bone area. Thus, out of the 1254 children with cleft lip and palate who visited the Tohid Hearing and Balance Center in Isfahan over a four-year period, 88 children with a mean age of 6.12 ± 0.11 months were included in the study. Prior to conducting audiological tests, the ear canal was examined, and if necessary, an otorhinolaryngologist specialist drained any mass present. The study consisted of two phases, with audiological evaluations including 226 Hz single-frequency tympanometry, wideband tympanometry, and auditory responses of the air and bone brainstem. The first phase took place three months and three days prior to cleft palate repair surgery. At the end of the first phase, children who exhibited any change or improvement in effusion level, no hearing loss, abnormal absorption (based on normal patterns in the device) below or above 1000 Hz, and moderate or higher conductive hearing loss underwent simultaneous cleft palate repair surgery and tympanostomy due to the possibility of total effusion, as indicated by previous studies [22, 23] and confirmed by an otorhinolaryngologist through microscopic observations. Consequently, 10 children (6 girls and 4 boys) were excluded from the study at the conclusion of this phase. The remaining 78 children proceeded to the second phase and underwent cleft palate repair surgery alone. Audiological evaluations were repeated one, three, and six months after the cleft palate repair surgery, and changes were analyzed. The audiological results of these 78 children were used for data analysis. The time intervals of one and six months after cleft palate surgery were chosen based on the methodology of a study conducted by Jain et al., while the interval of three months after cleft palate surgery was selected for accurate monitoring of changes in wideband tympanometry outcome and brainstem auditory responses [24].
Wideband and 226 Hz tympanometry evaluations were performed using the Titan intra-acoustic tympanometry device, manufactured in Denmark. The device was calibrated according to the IEC 60645-5/ANSI S3.39 standard before the test. Based on previous studies, the absorption index at 250 Hz was utilized to monitor the ideal positioning of the probe inside the ear canal. If the value exceeded 0.2, the test was repeated. Subsequently, absorption indices were obtained at low frequencies (1000 Hz and below) and high frequencies (above 1000 Hz). A comparison with the normal patterns in the device determined whether the absorption fell within the normal range for each age group.
The brainstem auditory response test was carried out using the Eclipse 25 device, manufactured by Interacoustic Company. The V wave threshold was determined through air conduction using the CE-chirp stimulus. Additionally, the brainstem auditory response was recorded via bone conduction using the CE-chirp stimulus to rule out sensorineural problems. The test was halted upon observation of the V wave at 20 dBnHL.
Statistical Analysis
Data analysis was performed using SPSS 21. Descriptive statistics were employed to calculate the mean, standard deviation, and percentages for the variables in all samples. Cochran’s Q test, with a significance level of 0.05, was used to compare the absorption index three days before and after cleft palate surgery. Significantly different results (p = 0.001) prompted the use of McNemar’s post hoc test with Bonferroni correction for pairwise comparisons between the absorption index three months prior to cleft palate surgery and each subsequent time interval. A significance level of 0.016 was applied.
The Friedman test, at a significance level of 0.05, was also employed to compare the air conduction thresholds three days before cleft palate surgery and at each subsequent time interval. Given a significant difference (p = 0.001), the Wilcoxon post hoc test with Bonferroni correction was used, at a significance level of 0.016, for paired comparisons between the air conduction thresholds three months before cleft palate surgery and each subsequent time interval.
Results
A total of 88 children underwent examination in the initial phase of the study. Three months prior to cleft palate surgery, all cases exhibited type B tympanometry at 226 Hz in both ears. Wideband tympanometry results indicated that the absorption of low frequencies in both ears of all children was below the normal range. Additionally, the absorption of high frequencies fell within the normal range in both ears of 39 children and below the normal range in 49 children. The mean ± standard deviations of air conduction thresholds for auditory brainstem responses were 48.06 ± 9.23 and 47.84 ± 9.70 dBnHL, respectively, in the right and left ears of the 88 children. In the group of 49 children with below-normal absorption at high frequencies, these values were 55.71 ± 3.81 and 55.91 ± 3.63 in the right and left ears, respectively. In the group of 39 children with normal absorption at high frequencies, the values were 38.46 ± 2.60 and 37.69 ± 3.01 in the right and left ears, respectively. Therefore, 49 children exhibited total effusion, while 39 children had partial effusion three months before cleft palate surgery. Furthermore, three days before the cleft palate surgery, all cases demonstrated type B tympanometry at 226 Hz in both ears. The wideband tympanometry results revealed that the absorption of low frequencies in both ears of all children remained below the normal range. However, 78 children exhibited normal absorption at high frequencies in both ears, while 10 children exhibited below-normal absorption. The mean ± standard deviations of air conduction thresholds for auditory brainstem responses were 42.44 ± 6.73 and 43.18 ± 7.03 in the right and left ears, respectively, for the 88 children. Among the 10 children with below-normal absorption at high frequencies, these values were 58.50 ± 3.37 and 60.50 ± 2.83, while for the 78 children with normal absorption at high frequencies, the values were 40.38 ± 3.49 and 40.96 ± 3.32 in the right and left ears, respectively. Consequently, 10 children underwent palatoplasty and simultaneous tympanostomy due to total effusion, and were thus excluded from the study. The results of the remaining 78 children are detailed below.
Figures 1 and 2 depict the results of 226 Hz and wideband tympanometry conducted on both ears of 78 children during the initial and subsequent phases of the research. Figure 3 shows The results of WBT tympanometry of a 12-month-old child before and after surgery. The data illustrates that, after surgery, there were 65, 37, and 7 children, respectively, who exhibited type B tympanometry and absorption levels below the normal range in their right ears at low frequencies one, three, and six months post-surgery. Similarly, in their left ears, 67, 40, and 7 children had type B tympanometry and absorption levels lower than the normal range during the same time intervals. The decrease in the number of children with abnormal absorption at low frequencies suggests an improvement in middle ear condition following cleft palate repair surgery within the mentioned time periods. Absorption remained normal and unchanged in all participants at high frequencies three days before the cleft palate surgery and during subsequent time intervals (with the exception of one individual six months after the surgery). Based on McNemar’s post hoc test with Bonferroni correction, a significant difference was observed in absorption measurements at low frequencies between both ears three days prior to cleft repair surgery and one month (p = 0.001), three months (p = 0.001), and six months (p = 0.001) after the surgery.
Fig. 1.
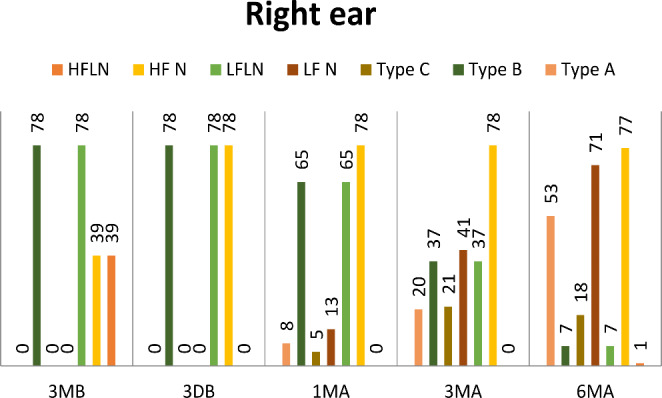
Results of single and wideband tympanometry in right ear. (LF N (low frequency in normal range), LF LN (low frequency lower than normal range), HF N (high frequency in normal rane), HF LN(high frequency lower than normal range))
Fig. 2.
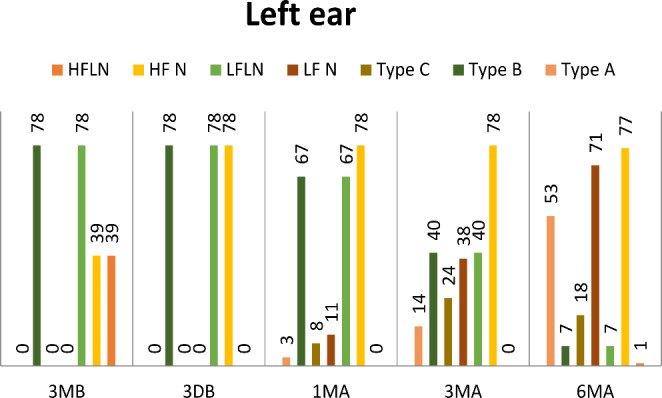
Results of single and wide band tympanometry in left ear. (LF N (low frequency in normal range), LF LN (low frequency lower than normal range), HF N (high frequency in normal range), HF LN(high frequency lower than normal range))
Fig. 3.
The results of wideband tympanometry of a 12-month-old child before and after cleft palate surgery. A: 3 months before cleft palate surgery, B: 3 days before cleft palate surgery, C: 3 month after cleft palate surgery, D: 6 month after cleft palate surgery
Since the absorption index at high frequencies remained consistent three days before cleft palate surgery and throughout the post-surgery intervals, it was not possible to draw a statistical comparison.
The air conduction thresholds were determined using click stimuli in accordance with brainstem auditory responses. Table 1 presents the mean threshold in dBnHL.
Table 1.
Mean ± standard deviation of auditory brainstem responses (dB nHL).
| Test time | Right ear | Left ear |
|---|---|---|
| 3 months before cleft palate surgery | 47.11 ± 9.31 | 46.73 ± 9.73 |
| 3 days before cleft palate surgery | 40.96 ± 3.32 | 4.38 ± 3.49 |
| 1 month after cleft palate surgery | 37.88 ± 7.28 | 37.56 ± 7.76 |
| 3 month after cleft palate surgery | 32.30 ± 9.42 | 30.51 ± 9.88 |
| 6 month after cleft palate surgery | 23.46 ± 7.31 | 23.20 ± 6.93 |
Top of Form
The Wilcoxon post hoc test with Bonferroni correction revealed significant differences in air conduction thresholds in the right ear three days prior to cleft palate repair surgery and one month (p = 0.009), three months (p = 0.001), and six months (p = 0.001) after the surgery. Similarly, there was a statistically significant difference in the air conduction thresholds of the left ear three days before the repair surgery and one month (p = 0.001), three months (p = 0.001), and six months (p = 0.001) after the surgery.
It should be noted that only one child exhibited absorption below the normal range at low and high frequencies six months after cleft palate surgery. Considering the potential presence of total effusion, as confirmed by the brainstem auditory responses, the child was promptly referred to an otorhinolaryngologist for medical treatment.
Discussion
The present study examined the effects of cleft palate repair surgery alone on the absorption index of the middle ear system in children with cleft palate and bilateral OME. This index was qualitatively investigated at low and high frequencies, along with the results of brainstem auditory responses before and after cleft palate repair surgery. The study indicated a significant difference in the absorption index at low frequencies three days before cleft palate repair surgery and at each time interval after the surgery. The reduced number of children with abnormal absorption at low frequencies in each time interval after cleft palate surgery demonstrated an improvement in the middle ear status using cleft palate repair surgery.
There are few studies on the effect of cleft palate repair surgery on middle ear status. Hoghoughi et al. examined 42 children with non-syndromic cleft palate using single-frequency tympanometric tests and brainstem auditory responses before and six months after cleft palate repair surgery. They reported that Intervelar veloplasty (IVVP) under magnification could improve middle ear effusion without the need to place a tympanostomy tube. This study indicated that 70% of children in the right ear and 66.6% of children in the left ear had tympanometry results change from Type B to Type A six months after cleft palate repair surgery [25]. In the present study, this percentage was 68% for both ears at the same time interval. Furthermore, 23% of individuals had Type C tympanometry; thus, the two studies showed great similarity.
In contrast to single-frequency tympanometry, wideband tympanometry data in these individuals indicated that 91% had normal results six months after surgery. Additionally, the number of individuals with normal results in wideband tympanometry at other time intervals (one and three months after surgery) was much higher than in single-frequency tympanometry (16.7% and 14.1% of the cases had normal wideband tympanometry results, and 10.3% and 3.9% had normal single-frequency tympanometry results in the right and left ears, respectively, one month after surgery. Furthermore, 52.6% and 48.7% of the cases had normal wideband tympanometry results, and 25.64% and 17.9% had normal single-frequency tympanometry results in the right and left ears, respectively, three months after surgery).
The absorption was within the normal range at all time intervals of the second phase at high frequencies, and only one case had abnormal absorption at both low and high frequencies. Therefore, this case was excluded from the study, possibly due to the possibility of total effusion according to the results of previous studies [22, 23].
Furthermore, wideband tympanometry can provide more information about the improvement of middle ear problems in comparison with single-frequency tympanometry. Hence, the middle ear status of these individuals can be monitored more accurately using wideband tympanometry. Several studies have indicated the importance of follow-up on the middle ear status in children with cleft palate [26–28]. Wang et al. examined 76 children with cleft palate and reported that the abnormalities in the middle ear system persisted for a long time in those with cleft palate, emphasizing the necessity of a long-term follow-up system [26]. Azman et al. studied 102 individuals aged 1–18 years with cleft palate and reported that long-term follow-up of their hearing status at specific time intervals allowed for conservative decision-making [27]. Since most studies utilized single-frequency tympanometry to monitor the middle ear status after cleft palate surgery, it was impossible to compare their results with the results of wideband tympanometry in the present study. Consistent with the results of the present study, Merchant et al. indicated that the effusion volume increased in the middle ear of children with OME as the absorption decreased at 1000 Hz and above [23].
There was a significant improvement in the hearing status of children in the study, as assessed by brainstem auditory responses after cleft palate surgery and over time (similar to the improvement of broadband absorption indices). The mean hearing threshold improved by almost 3 dBnHL one month after cleft palate surgery. Furthermore, the hearing improvement continued over time, and finally, the mean hearing threshold became normal six months after the surgery. The participants’ percentages demonstrate that 89.7% of children had normal air conduction thresholds in the right ear, and 88.5% had normal thresholds in the left ear six months after the surgery, indicating a full improvement in the hearing status for most participants. Jain et al. examined 75 children with cleft palate at 10 months and 5 years of age and reported that cleft palate repair surgery significantly improved their hearing thresholds six months after the surgery [24]. This result was consistent with the present study, but the improvement was insignificant one month after the surgery. Such a difference with the present study was likely due to their different inclusion criteria. Jain et al. investigated a wider age range compared to the present study. Furthermore, hearing measurements were also conducted three months before cleft palate surgery in the present study, and then children with abnormal absorption at high and low frequencies and moderate or higher hearing loss were excluded from the study. However, Jain et al. did not provide wideband absorption measurements for a more accurate examination of the middle ear status. Hoghoughi et al. also reported that the hearing threshold was normal in 79% of the cases in the right ear and 73.8% in the left ear six months after cleft palate surgery [25]. Their result was approximately consistent with the present study. Similar to the present study, Luo and Carroll indicated an improvement in hearing status over time after cleft palate surgery [29, 30].
Conclusion
Considering the aforementioned cases and the significant improvement in the absorption values and hearing status after cleft palate repair surgery, monitoring the broadband absorption indices and hearing thresholds seems very helpful in determining the type of surgery for children with OME. It thus prevents unnecessary tympanostomy and the placement of ventilation tubes.
Funding
No funding.
Declarations
Conflict of Interest
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Leslie EJ, Marazita ML (eds) (2013) Genetics of cleft lip and cleft palate. American Journal of Medical Genetics Part C: seminars in Medical Genetics. Wiley Online Library [DOI] [PMC free article] [PubMed]
- 2.Coleman J, Jr, Sykes J. The embryology, classification, epidemiology, and genetics of facial clefting. Facial Plast Surg Clin North Am. 2001;9(1):1–13. [PubMed] [Google Scholar]
- 3.Jamilian A, Nayeri F, Babayan A. Incidence of cleft lip and palate in Tehran. J Indian Soc Pedod Prev Dentistry. 2007;25(4):174. doi: 10.4103/0970-4388.37013. [DOI] [PubMed] [Google Scholar]
- 4.Kianifar H, Hasanzadeh N, Jahanbin A, Ezzati A, Kianifar H. Cleft lip and palate: a 30-year epidemiologic study in north-east of Iran. Iran J Otorhinolaryngol. 2015;27(78):35. [PMC free article] [PubMed] [Google Scholar]
- 5.Zandi M, Heidari A. An epidemiologic study of orofacial clefts in Hamedan city, Iran: a 15-year study. The Cleft palate-craniofacial journal. 2011;48(4):483–489. doi: 10.1597/09-035. [DOI] [PubMed] [Google Scholar]
- 6.Mirfazeli A, Kaviany N, Hosseinpour KR, Golalipour MJ. Incidence of cleft lip and palate in Gorgan-Northern Iran: an epidemiological study. Oman Med J. 2012;27(6):461. doi: 10.5001/omj.2012.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gould HJ. Hearing loss and cleft palate: the perspective of time. Cleft Palate Journal. 1990;27(1):36–39. doi: 10.1597/1545-1569_1990_027_0036_hlacpt_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 8.Delage H, Tuller L Language development and mild-to-moderate hearing loss: does language normalize with age? 2007 [DOI] [PubMed]
- 9.Kuehn DP, Moller KT. Speech and language issues in the cleft palate population: the state of the art. The Cleft palate-craniofacial journal. 2000;37(4):1–35. doi: 10.1597/1545-1569_2000_037_0348_saliit_2.3.co_2. [DOI] [Google Scholar]
- 10.Seibert JW, Danner CJ. Eustachian tube function and the middle ear. Otolaryngol Clin North Am. 2006;39(6):1221–1235. doi: 10.1016/j.otc.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 11.Doyle WJ, Cantekin EI, Bluestone CD. Eustachian tube function in cleft palate children. Annals of Otology Rhinology & Laryngology. 1980;89(3suppl):34–40. doi: 10.1177/00034894800890S311. [DOI] [PubMed] [Google Scholar]
- 12.Ponduri S, Bradley R, Ellis PE, Brookes ST, Sandy JR, Ness AR. The management of otitis media with early routine insertion of grommets in children with cleft palate—a systematic review. The Cleft Palate-Craniofacial Journal. 2009;46(1):30–38. doi: 10.1597/07-219.1. [DOI] [PubMed] [Google Scholar]
- 13.Kwan WM, Abdullah VJ, Liu K, Van Hasselt CA, Tong MC. Otitis media with effusion and hearing loss in chinese children with cleft lip and palate. The Cleft palate-craniofacial journal. 2011;48(6):684–689. doi: 10.1597/10-006. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal K. Cleft palate repair and variations. Indian J Plast Surg. 2009;42(S 01):S102–S9. doi: 10.4103/0970-0358.57197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doyle WJ, Reilly JS, Jardini L, Rovnak S. Effect of palatoplasty on the function of the eustachian tube in children with cleft palate. The Cleft Palate Journal. 1986;23(1):63–68. [PubMed] [Google Scholar]
- 16.Alper CM, Losee JE, Mandel EM, Seroky JT, Swarts JD, Doyle WJ. Pre-and post-palatoplasty eustachian tube function in infants with cleft palate. Int J Pediatr Otorhinolaryngol. 2012;76(3):388–391. doi: 10.1016/j.ijporl.2011.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenfeld RM, Schwartz SR, Pynnonen MA, Tunkel DE, Hussey HM, Fichera JS, et al. Clinical practice guideline: tympanostomy tubes in children. Otolaryngology—Head and Neck Surgery. 2013;149(1suppl):S1–S35. doi: 10.1177/0194599812468849. [DOI] [PubMed] [Google Scholar]
- 18.Rosowski JJ, Nakajima HH, Hamade MA, Mafoud L, Merchant GR, Halpin CF, et al. Ear-canal reflectance, umbo velocity and tympanometry in normal hearing adults. Ear Hear. 2012;33(1):19. doi: 10.1097/AUD.0b013e31822ccb76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Polat Z, Bas B, Hayir D, Bulut E, Atas A. Wideband tympanometry normative data for turkish young adult population. J Int Adv otology. 2015;11(2):157. doi: 10.5152/iao.2015.809. [DOI] [PubMed] [Google Scholar]
- 20.Demir E, Afacan NN, Celiker M, Celiker FB, İnecikli MF, Terzi S, et al. Can wideband tympanometry be used as a screening test for superior semicircular canal dehiscence? Clin Exp Otorhinolaryngol. 2019;12(3):249–254. doi: 10.21053/ceo.2018.01137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Margolis RH, Van Camp KJ, Wilson RH, Creten WL. Multifrequency tympanometry in normal ears. Audiology. 1985;24(1):44–53. doi: 10.3109/00206098509070096. [DOI] [PubMed] [Google Scholar]
- 22.Al-Salim S, Tempero RM, Johnson H, Merchant GR. Audiologic profiles of children with otitis media with effusion. Ear Hear. 2021;42(5):1195–1207. doi: 10.1097/AUD.0000000000001038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merchant GR, Al-Salim S, Tempero RM, Fitzpatrick D, Neely ST. Improving the differential diagnosis of otitis media with effusion using wideband acoustic immittance. Ear Hear. 2021;42(5):1183–1194. doi: 10.1097/AUD.0000000000001037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jain A, Yadav A, Bhola N, Nimonkar P, Borle R. Effect of palatoplasty on hearing ability of nonsyndromic cleft palate patients: a prospective clinical study. J Cleft Lip Palate Craniofac Anomalies. 2017;4(2):114. doi: 10.4103/jclpca.jclpca_24_17. [DOI] [Google Scholar]
- 25.Hoghoughi MA, Kazemi T, Khojasteh A, Habibagahi R, Kalkate Z, Zarei Z, et al. The effect of intervelar veloplasty under magnification (Sommerlad’s technique) without tympanostomy on middle ear effusion in cleft palate patients. BMC Pediatr. 2021;21(1):1–6. doi: 10.1186/s12887-021-02856-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang X, Feng S, Li F, Zhong Z, Chen Y, Peng Q, et al. Analysis of middle ear function of the patients with cleft palate after palatoplasty. Zhonghua er bi yan hou tou Jing wai ke za zhi = Chinese. J Otorhinolaryngol Head Neck Surg. 2021;56(6):586–589. doi: 10.3760/cma.j.cn115330-20200716-00595. [DOI] [PubMed] [Google Scholar]
- 27.Azman A, Manuel AM. Otological outcome in cleft lip and palate children with middle ear effusion. Int J Pediatr Otorhinolaryngol. 2020;138:110274. doi: 10.1016/j.ijporl.2020.110274. [DOI] [PubMed] [Google Scholar]
- 28.Mirashrafi F, Emami H, Bagheri Z, Rahavi-Ezabadi S (2022) Middle ear status in cleft lip and palate patients: a five-year Follow-Up. Iran J Otorhinolaryngol 34(5) [DOI] [PMC free article] [PubMed]
- 29.Lou Q, Zhu H, Luo Y, Zhou Z, Ma L, Ma X, et al. The effects of age at cleft palate repair on middle ear function and hearing level. The Cleft Palate-Craniofacial Journal. 2018;55(5):753–757. doi: 10.1177/1055665618754632. [DOI] [PubMed] [Google Scholar]
- 30.Carroll DJ, Padgitt NR, Liu M, Lander TA, Tibesar RJ, Sidman JD. The effect of cleft palate repair technique on hearing outcomes in children. Int J Pediatr Otorhinolaryngol. 2013;77(9):1518–1522. doi: 10.1016/j.ijporl.2013.06.021. [DOI] [PubMed] [Google Scholar]