Abstract
To compare the efficacy of conventional Macintosh laryngoscope with Airtraq videolaryngoscope for visualization of laryngeal structures to rule out recurrent laryngeal nerve injury at the end of thyroidectomy. This randomized double-blind control study was conducted following IEC-Human approval, prospective CTRI registration and written informed consent from participants. Patients of either sex, aged 18–65 years, ASA grade I/II, scheduled for thyroidectomy under GA were included. Group DL underwent direct laryngoscopy using Macintosh blade whereas group VL underwent laryngoscopy using Airtraq® videolaryngoscope. CL(Cormack-Lehane) grade of laryngeal view, time taken to achieve optimal view, haemodynamic parameters, Patient reactivity score(PRS) and complications were noted. Unpaired t-test, chi-square test were used. A total of 73 patients were included for study with 38 in group DL and 35 in group VL. The grade of laryngeal view was found to be significantly better with Airtraq® VL compared to Macintosh laryngoscope without the application of BURP (p < 0.05). In the DL group, 34.2% (n = 13) had a CL grade I, 36.8% (n = 14) had CL grade 2A, 13.2% had CL grade 2B (n = 5) and 15.8% (n = 6) had CL Grade 3 at the end of thyroidectomy. On the contrary, in the VL Group, 71.5% (n = 25) of the participants had a CL Grade I; whereas, 20% (n = 7) had a CL Grade 2A, 5.7% (n = 2) had CL grade 2B and 2.8% (n = 1) of participants had CL grade 3. The mean “time taken to achieve optimal view’ was comparable between the two groups (DL = 39.16 ± 105.53 s vs. VL = 38.89 ± 20.69 s) (p = 0.988).The haemodynamic parameters, Patient reactivity score and complications were comparable between the two groups. The performance of Airtraq® videolaryngoscope, a channelled VL is better than conventional Macintosh laryngoscope in terms of the optimal glottic view obtained to rule out recurrent laryngeal nerve palsy at the end of thyroidectomy.
Keywords: Videolaryngoscope; CL grade,Thyroidectomy; Macintosh laryngoscope
Introduction
Injury of Recurrent Laryngeal Nerve (RLN) is one of the severe complications of thyroid surgery [1, 2]. The incidence of this complication varies from 2 to 11% for temporary RLN injury and 0.6–1.6% for permanent RLN palsy [1, 3, 4]. The risk of RLN injury depends upon presence of malignancy, history of operation on the neck, surgeon experience, the side (left vs. right), grave’s disease, extent of surgery, presence of retrosternal goiter, toxic goiter and substernal goiter [1, 5].
In the routine clinical practice, to rule out RLN injury, vocal cord movement is assessed at the end of thyroidectomy before reversing the anaesthesia or awakening the patient. Therefore, a routine post-operative laryngoscopy is recommended at the end of thyroidectomy before reversal of anaesthesia; more so, in suspected cases [6]. Various techniques for this purpose are direct laryngoscopy following reversal of neuromuscular blockade, fibreoptic-assisted visualization of vocal cords via laryngeal mask airway(LMA) [7], LMA CTrach™ assisted visualization, [8] ultrasonography [9] and videolaryngoscopes (VL) [10–12].
Recently, various VLs [10–13] have been used to assess vocal cord mobility for this indication. Videolaryngoscope is an alternative to the conventional laryngoscope and has advantage of providing a better glottic view, lesser lifting force, stable haemodynamics and better patient comfort. In addition, its use does not mandate the alignment of three axes into one plane, and thus better visibility of the vocal cords when compared to the conventional laryngoscopy [14–16]. The latter feature is of specific advantage in this situation as the neck dressing post-thyroidectomy can limit the neck movement required for visualization of laryngeal structures.
The Airtraq® VL (Prodol Meditec S.A., Vizcaya, Spain), a channeled VL has all the aforementioned advantages over the conventional laryngoscope for this indication (Fig. 1). Recently, in two case reports, Aitraq® videolaryngoscope has been evaluated for assessing the vocal cord mobility following thyroidectomy and is found to be efficacious [10, 11]. However, in routine clinical practice, conventional laryngoscopy is mostly attempted to rule out RLN palsy at the end of thyroidectomy. On literature search, we could not retrieve any study comparing channelled VL like Airtraq® with the conventional macintosh laryngoscope for visualization of laryngeal structures to rule out RLN palsy at the end of thyroidectomy.
Fig. 1.

Airtraq® videolaryngoscope
Therefore, the present study was undertaken to compare the efficacy of Airtraq® VL with Macintosh laryngoscope in terms of the visualization of laryngeal structures, the time taken to obtain optimal view i.e. Cormack lehane (CL) grade 1 or 2, haemodynamic parameters, patient reactivity score(PRS) and complications, if any.
Methods
The present randomized double-blind controlled study was conducted following approval from institutional ethics committee- Human research (IEC-HR) [IEC-HR/2018/36/16R] and prospective registration at Clinical Trial Registry-India (http://ctri.nic.in) [CTRI/2018/12/022863] from November 2018 till April 2020. A written informed consent was taken from each participant.
Patients of either sex, aged 18 to 65 years of age, American society of anaesthesiologists (ASA) physical status I or II undergoing thyroidectomy under general anaesthesia (GA) were included. Patients were excluded if morbidly obese, in second or third trimester pregnancy, with limited mouth opening or pre-existing vocal cord dysfunction.
The randomization was done using a computer-generated random number table and the allocation concealment was done by using serially-numbered sealed opaque envelopes. Both the patient and the investigator who recorded the data were blinded to the group allocation. Patients were randomly allocated into one of the two groups. In Group DL—Patients underwent direct laryngoscopy using Macintosh blade to visualize laryngeal structures at the end of thyroidectomy; whereas, in group VL, patients underwent laryngoscopy using Airtraq® videolaryngoscope to visualize laryngeal structures at the end of thyroidectomy.
All patients received normal tidal volume pre-oxygenation with 100% oxygen for three minutes. All routine ASA recommended minimum-mandatory monitoring i.e. continuous ECG, heart rate (HR), pulse-oximetry, end tidal CO2, and intermittent NIBP were instituted. Baseline hemodynamic parameters were recorded. General anaesthesia was administered to all and the technique to secure airway was chosen depending upon the potential risk of difficult airway and the choice of anaesthesiologist. Dexamethasone 8 mg IV at the beginning of surgery and ondansetron 4 mg IV towards the end of surgery was administered for postoperative nausea and vomiting (PONV) prophylaxis to all the patients.
Following adequate reversal of neuromuscular blockade, endotracheal tube was removed and laryngoscopy using either Macintosh or videolaryngoscope was done to visualize the laryngeal structures to rule out RLN palsy. During this time, the depth of anaesthesia was maintained by using oxygen, nitrous oxide and sevoflurane. The CL grade (Table 1) was used to grade the laryngeal view obtained in both the groups [17]. The laryngeal view was considered optimal if it was either CL grade I or grade II; whereas, CL grade III and IV was considered as poor. The time taken to achieve optimal view of laryngeal structures with both the techniques was also recorded. It was measured from the time of ETT removal till the optimal laryngeal view i.e. grade I or II was obtained. In case of poor view, a repeat attempt of laryngoscopy with a different laryngoscopist or use of videolaryngoscope was considered. Backward upward rightward pressure (BURP) was applied to obtain the best possible laryngeal view if CL grade 1 was not obtained on first attempt. In addition, the depth of anaesthesia was checked and deepened, if needed. The number of attempts of laryngoscopy was also noted.
Table 1.
Cormack Lehane grading
| Grade 1 | Most of the cords visible |
|---|---|
| Grade 2A | Posterior cord visible |
| Grade 2B | Only arytenoids visible |
| Grade 3A | Epiglottis visible and liftable |
| Grade 3B | Epiglottis adherent to pharynx |
| Grade 4 | No laryngeal structures seen |
Patients’ comfort to laryngoscopy was assessed using patient reactivity score (PRS). It was rated on a 5-point PRS (1 = no grimace, 2 = grimacing facial expression, 3 = discomforting head movements, 4 = protective head and limb movements, 5 = coughing and gagging) [13, 18].
The baseline hemodynamic parameters i.e. HR, systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean blood pressure (MAP) were recorded immediately before the removal of ETT and then at the interval of two minutes till the optimal view was obtained in both the groups. In addition, any coughing, desaturation spells or any other airway complication were also noted.
The primary outcome was CL grade of laryngeal view and secondary outcomes were “time taken to achieve optimal view”, haemodynamic parameters i.e. HR, SBP, DBP, MAP during laryngoscopy, PRS and complications, if any.
Based on the previous study, the proportion of CL grade I and II with direct laryngoscopy when done for the assessment of laryngeal structure at the end of thyroidectomy has been reported to be 72% [19]. Considering a difference of 25% to be significant with the alpha error of 0.05 and 80% power of study, 32 patients are required in each group. Hence, a sample size of 64 patients was considered with 32 patients in each group.
Statistical analysis was performed using statistical package for the social sciences (SPSS) version 21.0. Continuous variables were expressed in means and standard deviation and categorical data was expressed in percentages. Statistical significance for continuous variables was assessed by unpaired t-test and for categorical variable, Chi-square test was used. A p-value less than 0.05 was considered statistically significant.
Results
Seventy seven patients were enrolled, out of which four were excluded. Amongst four, one patient had pre-existing unilateral vocal cord palsy, one was morbidly obese and two had limited mouth opening. Finally, a total of 73 patients were included with 38 in group DL and 35 in group VL (Fig. 2).
Fig. 2.
Consort flow diagram
Both the groups were comparable with respect to age, gender distribution, ASA physical status, and duration of surgery (Table 2). There was no significant difference in the baseline mallampati score (MP) score between the two groups. There was a higher proportion of individuals in Group DL that had an MPG score ≥ 2 (68.4%) compared to Group VL (48.6%); however, this difference was not significant (p = 0.226).
Table 2.
Patients’ characteristics
| Parameter | Group DL (n = 38) | Group VL (n = 35) | P-value | |
|---|---|---|---|---|
| Age of the patient (in years) Mean(± SD) | 36.13 (± 9.86) | 32.57 (± 10.82) | 0.146 | |
| Gender | Male | 5(13.1%) | 2 (5.7%) | 0.280 |
| Female | 33(86.9%) | 33(94.3%) | ||
| ASA Grade of the patient | ASA 1 | 34(89.5%) | 29(82.9%) | 0.411 |
| ASA 2 | 4(10.5%) | 6(17.1%) | ||
Group DL: Macintosh direct laryngoscope used to visualize glottic structures
Group VL: Airtraq videolaryngoscope used to visualize glottic structures
On baseline assessment at the time of endotracheal intubation, in the Group VL, 28 patients (80%) had CL grade of I, four patients had CL grade of 2A (11.5%),two had a baseline CL grade 2B (5.7%) and one patient had CL grade of 3(2.8%). Similarly, in Group DL, 23 patients (60.5%) had CL Grade I, eight patients (21.1%) had grade 2A and six patients (15.8%) had CL Grade 2B and one patient had CL grade 3(2.8%). The difference between the two groups based on their baseline CL grading at the time of intubation was comparable. (p = 0.290).
At the end of thyroidectomy, in the VL Group, majority i.e. 71.5% (n = 25) of the participants had a CL Grade I; whereas, 20% (n = 7) had a CL Grade 2A, 5.7% (n = 2) had CL grade 2B and 2.8% (n = 1) of participants had CL grade 3. In the DL group, 34.2% (n = 13) had a CL grade I and 36.8% (n = 14) had CL grade 2A and 13.2% had CL grade 2B (n = 5) and 15.8% (n = 6) had CL Grade 3.
Without the application of BURP, an optimal laryngeal view i.e. CL grade 1 or 2 was observed in 97.2% of patients in VL group as compared to 84.2% in DL group. On intergroup analysis, the difference was found to be statistically significant (p = 0.012) (Table 3).
Table 3.
Grade of Laryngeal view with BURP(in patients with CL grade ≥ 2 on first attempt) and without BURP
| Parameter | Group DL (n = 38) | Group VL (n = 35) | P-value | |
|---|---|---|---|---|
| CL Grade (without BURP) | 1 | 13(34.2%) | 25(71.5%) | 0.012* |
| 2A | 14(36.8%) | 7(20%) | ||
| 2B | 5(13.2%) | 2(5.7%) | ||
| 3 | 6(15.8%) | 1(2.8%) | ||
| 4 | 0 | 0 | ||
| CL Grade (with BURP) | 1 | 15(60%) | 7(70%) | 0.200 |
| 2A | 4(16%) | 3(30%) | ||
| 2B | 6(24%) | 0 | ||
| 3 | 0 | 0 | ||
| 4 | 0 | 0 | ||
| Total | 25 | 10 | ||
Group DL: Macintosh direct laryngoscope used to visualize glottic structures
Group VL: Airtraq videolaryngoscope used to visualize glottic structures
*The difference between group DL and group CL is statistically significant
However, on application of BURP, the CL grade was reassessed amongst the 25 patients in group DL in whom CL grade ≥ 2 on first attempt. It was observed that four patients (16%) had grade 2A and 6 patients had grade 2B (24%), respectively. In group DL, six patients in whom a CL grade of 3 was achieved on first attempt, the CL grade improved to 2B, while one patient in whom CL grade of 2B was achieved, the view improved to CL grade 1 on application of BURP. In group VL, two patients who had CL grade of 2B on first attempt, the view improved to 2A and six patients who had a CL grade of 2A, the view improved to CL grade I on application of BURP. On intergroup analysis, this difference between the two groups was not observed to be significant (p = 0.200) (Table 3).
The mean “time taken to achieve optimal view’ was comparable between the two groups i.e. (DL: 39.16 ± 15.53 s vs. VL: 38.89 ± 20.69 s) (p = 0.988).
Patients’ comfort to laryngoscopy was assessed using patient reactivity score (PRS) (1 = no grimace, 2 = grimacing facial expression, 3 = discomforting head movements, 4 = protective head and limb movements, 5 = coughing and gagging). Only one patient (2.6%) in group DL had PRS score of 5; whereas, rest all patients in both the groups had PRS score of 1. This difference was not statistically significant (p = 0.334).
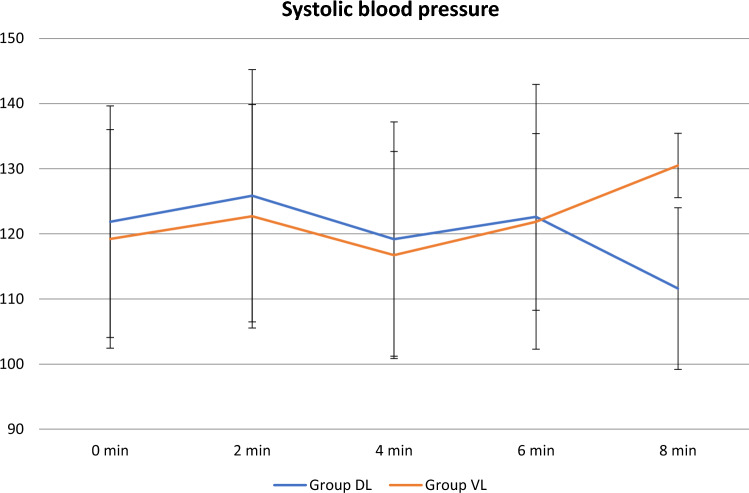
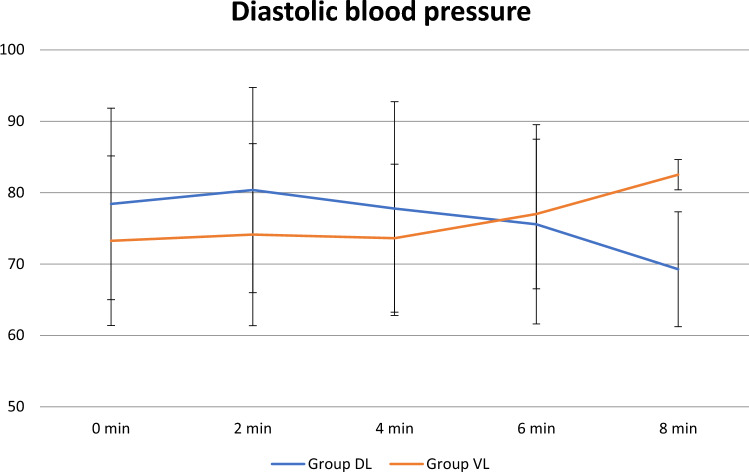
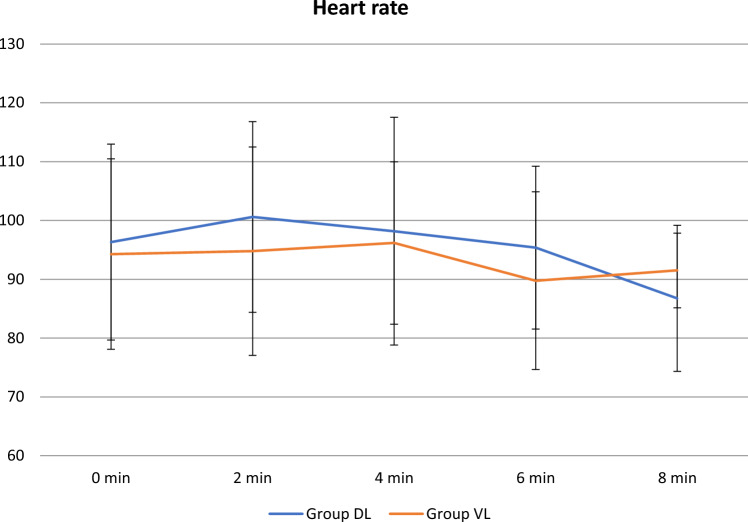
On intergroup analysis the mean SBP, DBP, MAP and HR at various time points was observed to be lesser in group VL than group DL except for the readings at the 8th minute. However, no statistically significant difference was observed at any time point (Figs. 3, 4 and 5).
Fig. 3.
Systolic blood pressure(SBP) at various time points in the two groups
Fig. 4.
Diastolic Blood pressure(DBP) at various time points in the two groups
Fig. 5.
Heart rate at various time points in the two groups
Among complications, only four patients (10.5%) had experienced desaturation in group DL compared to only two (5.7%) patients in Group VL. The oxygen saturation in all the four cases did not drop below 85%, which was managed with mask ventilation. Only one patient in group DL who had PRS of 5 had coughing and gagging. No other complications were observed in either group. Both the groups were comparable with respect to the adverse effects (p = 0.462).
Only two patients (5.3%) in Group DL had to undergo repeat attempts of laryngoscopy while one participant (2.9%) in Group VL underwent a repeat attempt by a different laryngoscopist. None of the patients in VL group needed conventional laryngoscopy. The difference was again not found to be significant (p = 0.605).
Discussion
In the present double-blinded randomized control study, the grade of laryngeal view was found to be significantly better (p < 0.05) with Airtraq® VL when compared to Macintosh laryngoscope. Other parameters like the “mean time taken to achieve optimal view”, haemodynamic parameters and patient reactivity score were comparable between the two groups.
Various techniques for visualization of laryngeal structures at the end of thyroidectomy are direct laryngoscopy following reversal of neuromuscular blockade, fibreoptic-assisted visualization of vocal cords via laryngeal mask airway (LMA) [7], LMA CTrach™ assisted visualization, [8] ultrasonography [9] and videolaryngoscopes [10–12]. The most commonly employed techniques are direct laryngoscopy and fibreoptic-assisted visualization via LMA [7]. The problems with direct laryngoscopy include obscured view, difficulty in laryngoscopy in difficult airway cases, precipitation of laryngospasm, considerable hemodynamic changes and patients’ discomfort, all often occurs due to the light plane of anaesthesia [7, 18]. Similarly, the problems with fibreoptic-assisted visualization via LMA include the availability of fiberoptic bronchoscope, expertise and brief cessation of oxygenation during the procedure [13, 20].
Various authors have reported the performance of different types of VLs for visualization of laryngeal structures at the end of thyroidectomy [10–13, 21]. The Airtraq® VL (Prodol Meditec S.A., Vizcaya, Spain) is a channeled VL which was developed in order to facilitate tracheal intubation in patients with normal or difficult airway and has recently been used in a few case reports to assess the vocal cord mobility following thyroidectomy [10, 11].
The channelled VLs have been observed to have superior laryngoscopic view when compared to the unchanneled VLs. Airtraq VL, a channeled VL has been evaluated only in a case report and a case series for this indication and has been found to have better laryngeal view [1, 10]. Other studies utilizing VLs for this indication have observed that channeled videolaryngoscopes like Airtraq® and Pentax AWS provide better Cormack-Lehane view, require lesser intubation time compared to unchanneled videolaryngoscopes, although the ease of blade insertion might be better in C-MAC compared to other channeled videolaryngoscopes [22, 23].
However, channeled and unchaneled VL has been compared by Priyanka et al. [13] They compared King vision, a channeled VL with Truview VL, an unchanneled VL for post thyroidectomy vocal cord visualization, and observed that both provided comparable laryngoscopic view with similar patient comfort; although, the time consumed for visualization of vocal cords was lesser with Truview. Except one [13], none of the aforementioned studies has documented the “time taken to achieve optimal view” post extubation.
However, the present is by far the first study validating the improved laryngeal view with the use of a channelled VL such as Airtraq® VL when compared to conventional laryngoscope at the end of thyroidectomy (p = 0.012). In the present study we have assessed “time taken to achieve optimal view” and observed it to be comparable with conventional laryngoscopy. On the contrary, a study by Maharaj et al. [24] has reported shorter “time taken to achieve optimal view” with Airtraq VL when compared to Macintosh laryngoscope and concluded Airtraq VL to have shorter learning curve.
In order to facilitate laryngoscopy to evaluate grade of view of laryngeal structures utilizing conventional laryngoscopes or VLs at the end of surgery, various aforementioned studies have used various drugs such as dexmedetomidine 1 μg/kg ten minutes prior to extubation, [13] propofol, [25] fentanyl [18] etc. However, in our study, the depth of anaesthesia during laryngoscopy was maintained by using oxygen, nitrous oxide and Sevoflurane ensuring the MAC between 0.8 and 1.
As far as the haemodynamics is concerned, no difference was observed between the two groups. This is in concordance to a study where no difference was observed in haemodynamics between the use of C-MAC VL, Truview Evo2 and videoendoscope when compared to Macintosh laryngoscope [26]. On the contrary, in another study, lesser haemodynamic response is observed with Glidescope VL when compared to Macintosh laryngoscope in controlled hypertensive patients [27].
We must consider that the channeled VLs such as Airtraq VL have the proven advantage for higher success rate of first attempt intubation which is advantageous for the present indication too as emergency reintubation may be warranted at the time of extubation as many of these patients undergoing thyroidectomy have difficult airway.
In the present study, the difference between the two groups based on PRS was not statistically significant (p = 0.334). The PRS have been used by previous two studies [13, 18]. Priyanka et al. [13] observed comparable scores with the use of channelled vs unchanelled VLs; however, Kundra et al. [18] had demonstrated a higher degree of discomfort during direct laryngoscopy compared to nasal fibreoptic endoscopy and tele-laryngoscopy for visualization of laryngeal structures following thyroidectomy.
Conclusion
We conclude that the performance of Airtraq® videolaryngoscope, a channeled VL is better than conventional Macintosh laryngoscope in terms of the optimal glottic view obtained to rule out recurrent laryngeal nerve palsy at the end of thyroidectomy. However, the “time taken to achieve optimal view”, haemodynamic parameters during the procedure, patient reactivity score and related complications have been found to be comparable between both the devices. We recommend further studies comparing a channeled VL like Airtraq® VL with other unchanneled VL aiming to visualize the laryngeal structures after extubation at the end of thyroidectomy.
Acknowledgements
All patients and doctors who were involved in the patient management
Author Contributions
GTC, PB: Conception and Drafting of manuscript. MM, AKS, RK: Drafting of manuscript.
Funding
The authors have not disclosed any funding.
Declarations
Conflict of interest
No competing interests to declare.
Ethics Approval
The study was conducted following approval from institutional ethics committee- Human research (IEC-HR) [IEC-HR/2018/36/16R] and prospective registration at Clinical Trial Registry-India (http://ctri.nic.in) [CTRI/2018/12/022863].
Informed Consent
The author certify that they have obtained appropriate written informed consent forms from all participants.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bai B, Chen W. Protective effects of intraoperative nerve monitoring (IONM) for recurrent laryngeal nerve injury in thyroidectomy: meta-analysis. Sci Rep. 2018;8(1):7761. doi: 10.1038/s41598-018-26219-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abadin SS, Kaplan EL, Angelos P. Malpractice litigation after thyroid surgery: the role of recurrent laryngeal nerve injuries, 1989–2009. Surgery. 2010;148(4):718–723. doi: 10.1016/j.surg.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 3.Thomusch O, Sekulla C, Walls G, Machens A, Dralle H. Intraoperative neuromonitoring of surgery for benign goiter. Am J Surg. 2002;183(6):673–678. doi: 10.1016/S0002-9610(02)00856-5. [DOI] [PubMed] [Google Scholar]
- 4.Yarbrough DE, Thompson GB, Kasperbauer JL, Harper CM, Grant CS. Intraoperative electromyographic monitoring of the recurrent laryngeal nerve in reoperative thyroid and parathyroid surgery. Surgery. 2004;136(6):1107–1115. doi: 10.1016/j.surg.2004.06.040. [DOI] [PubMed] [Google Scholar]
- 5.Dralle H, Sekulla C, Haerting J, Timmermann W, Neumann HJ, Kruse E, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004;136(6):1310–1322. doi: 10.1016/j.surg.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard Ba G, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol. 2014;81(Suppl 1):1–122. doi: 10.1111/cen.12515. [DOI] [PubMed] [Google Scholar]
- 7.Chilkoti GT, Agarwal M, Mohta M, Saxena AK, Sharma CS, Ahmed Z. A randomised preliminary study to compare the performance of fibreoptic bronchoscope and laryngeal mask airway CTrach (LMA CTrach) for visualisation of laryngeal structures at the end of thyroidectomy. Indian J Anaesth. 2020;64(8):704–709. doi: 10.4103/ija.IJA_138_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chilkoti G, Mohta M, Saxena AK. Preliminary experience with LMA CTrachTM for assessment of glottic structures during thyroidectomy. Anaesth Intensive Care. 2016;44(6):785–786. doi: 10.1177/0310057X1604400617. [DOI] [PubMed] [Google Scholar]
- 9.Anzer Shah M, George D (2020) An observational study to assess vocal cord mobility by laryngeal ultrasonography and direct laryngoscopy in total thyroidectomy patients. 7(5):5–8
- 10.Sastre JA, López T, Del Barrio ME. Airtraq® videolaryngoscope for assessing vocal cord mobility at the end of thyroidectomy. J Clin Anesth. 2017;1(38):3–4. doi: 10.1016/j.jclinane.2017.01.012. [DOI] [PubMed] [Google Scholar]
- 11.Bensghir M, Hemmaoui B, Houba A, Haimeur C, Kamili ND, Azendour H. Diagnosis of bilateral cord vocal paralysis by the Airtraq laryngoscope: A case report. Egypt J Anaesth. 2014;30(4):427–429. doi: 10.1016/j.egja.2014.05.002. [DOI] [Google Scholar]
- 12.Shamim F, Nafis M, Ikram M. Video laryngoscope aids in the assessment of vocal cord paralysis due to recurrent laryngeal nerve injury after thyroid surgery. J Anaesthesiol Clin Pharmacol. 2016;32(4):544–545. doi: 10.4103/0970-9185.173352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Priyanka A, Nag K, Hemanth Kumar V, Singh D, Kumar S, Sivashanmugam T. Comparison of king vision and truview laryngoscope for postextubation visualization of vocal cord mobility in patients undergoing thyroid and major neck surgeries: A randomized clinical trial. Anesth Essays Res. 2017;11(1):238. doi: 10.4103/0259-1162.200240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoshijima H, Maruyama K, Mihara T, Mieda T, Shiga T, Nagasaka H. Airtraq® reduces the hemodynamic response to tracheal intubation using single-lumen tubes in adults compared with the Macintosh laryngoscope: A systematic review and meta-analysis of randomized control trials. J Clin Anesth. 2018;47:86–94. doi: 10.1016/j.jclinane.2018.03.022. [DOI] [PubMed] [Google Scholar]
- 15.Hindman BJ, Santoni BG, Puttlitz CM, From RP, Todd MM. Intubation biomechanics: laryngoscope force and cervical spine motion during intubation with Macintosh and Airtraq laryngoscopes. Anesthesiology. 2014;121(2):260–271. doi: 10.1097/ALN.0000000000000263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dimitriou VK, Zogogiannis ID, Liotiri DG. Awake tracheal intubation using the Airtraq laryngoscope: a case series. Acta Anaesthesiol Scand. 2009;53(7):964–967. doi: 10.1111/j.1399-6576.2009.02012.x. [DOI] [PubMed] [Google Scholar]
- 17.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39(11):1105–1111. doi: 10.1111/j.1365-2044.1984.tb08932.x. [DOI] [PubMed] [Google Scholar]
- 18.Kundra P, Kumar V, Srinivasan K, Gopalakrishnan S, Krishnappa S. Laryngoscopic techniques to assess vocal cord mobility following thyroid surgery. ANZ J Surg. 2010;80(11):817–821. doi: 10.1111/j.1445-2197.2010.05441.x. [DOI] [PubMed] [Google Scholar]
- 19.Lacoste L, Karayan J, Lehuedé MS, Thomas D, Goudou-Sinha M, Ingrand P, et al. A comparison of direct, indirect, and fiberoptic laryngoscopy to evaluate vocal cord paralysis after thyroid surgery. Thyroid. 1996;6(1):17–21. doi: 10.1089/thy.1996.6.17. [DOI] [PubMed] [Google Scholar]
- 20.Ellard L, Brown DH, Wong DT. Extubation of a difficult airway after thyroidectomy: use of a flexible bronchoscope via the LMA-Classic™. Can J Anesth Can d’anesthésie. 2012;59(1):53–57. doi: 10.1007/s12630-011-9619-y. [DOI] [PubMed] [Google Scholar]
- 21.Tawfic QA, Bhakta P, Mishra P, Ahmed MA. Glidescope ® for assessment of recurrent laryngeal nerve integrity after thyroid surgery. Sultan Qaboos Univ Med J. 2011;11(4):527–528. [PMC free article] [PubMed] [Google Scholar]
- 22.Teoh WH, Saxena S, Shah MK, Sia AT. Comparison of three videolaryngoscopes: Pentax Airway Scope, C-MAC G vs the M laryngoscope for tracheal intubation. Anaesthesia. 2010;65(11):1126–32. doi: 10.1111/j.1365-2044.2010.06513.x. [DOI] [PubMed] [Google Scholar]
- 23.Jayaram K, Padhy S, Priyanka S. Comparison of channelled vs unchannelled video laryngoscope—A prospective randomised trial. Indian J Clin Anaesth. 2018;5(4):543–548. doi: 10.18231/2394-4994.2018.0103. [DOI] [Google Scholar]
- 24.Maharaj CH, Higgins BD, Harte BH, Laffey JG. Evaluation of intubation using the Airtraq or Macintosh laryngoscope by anaesthetists in easy and simulated difficult laryngoscopy—a manikin study. Anaesthesia. 2006;61(5):469–477. doi: 10.1111/j.1365-2044.2006.04547.x. [DOI] [PubMed] [Google Scholar]
- 25.Shin K, Lee GY, Baik HJ, Kim CH. Bilateral vocal cord palsy after thyroidectomy detected by McGrath videolaryngoscope. Korean J Endocr Surg. 2016;16(3):85. doi: 10.16956/kjes.2016.16.3.85. [DOI] [Google Scholar]
- 26.Pappu A, Sharma B, Jain R, Dua N, Sood J. A randomised comparative study of "videoendoscope" with the Truview EVO2, C-MAC D blade videolaryngoscope and the Macintosh laryngoscope. Indian J Anaesth. 2020;64(Suppl 3):S186–S192. doi: 10.4103/ija.IJA_313_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meshram TM, Ramachandran R, Trikha A, Rewari V. Haemodynamic responses following orotracheal intubation in patients with hypertension–-Macintosh direct laryngoscope versus Glidescope®videolaryngoscope. Indian J Anaesth. 2021;65(4):321–327. doi: 10.4103/ija.IJA_417_20. [DOI] [PMC free article] [PubMed] [Google Scholar]