Abstract
Oral and Oropharyngeal cancers are on rise year after year and Head and Neck Cancer rank sixth among all cancers worldwide. This study is an institutional based retrospective type of study conducted in a tertiary care hospital for a period of 6 months with an aim to identify the demographic profile of the patients and to correlate between the clinical and radiological findings of the disease using Cohen’s Kappa value. Both oral and oropharyngeal cancer was predominant in male population with commonest age being the 5th decade of life. Tongue was the most common site for oral cancer, on the other hand, base of tongue was commonest among oropharyngeal cancer. The disease extension was thoroughly examined clinically by palpation and 70 degree Hopkins Endoscope and also radiologically using appropriate imaging tools. The clinical and radiological T showed moderate degree of agreement for both oral and oropharyngeal cancers whereas clinical and radiological N showed a almost perfect degree of agreement.
Keywords: Tongue, Tonsil, Cancer, Lymph node, Restrospective
Introduction
Oral and Oropharyngeal cancer falls under the category of Head and Neck cancer. Head and Neck cancers usually begin in the cells lined by squamous epithetlium. Head and neck cancers ranks sixth among the most common cancer worldwide with approximately 630,000 new patients diagnosed annually resulting in more than 350,000 deaths every year [1]. In India, 20 per 100,000 population are affected by oral cancer which credits for about 30% of all types of cancer [2].The difference in incidence and pattern of the disease can be attributed to the ageing of the population, as well as regional differences in the prevalence of disease-specific risk factors [3]. Cancer of the oral cavity comprises those of lips, buccal mucosa, gums, retromolar trigone, hard palate, anterior 2/3rd of tongue, and floor of mouth. It is often diagnosed in late stages and the overall 5-year survival is below 50% but early diagnosis is associated with high survival rates [4]. Tobacco and alcohol are present in 90% of cases, having both a synergistic effect and thus becoming the most important risk factor of the disease [5]. Oropharyngeal carcinoma comprises carcinoma of tonsil, base of tongue, walls of the pharynx and the soft palate. These cancers are associated with human papillomavirus (HPV), especially HPV16. HPV infection, being the aetiology of oropharyngeal cancers was first shown by Gillison et al. [6].
Materials and Methods
Our study is an institutional based retrospective type of study. It was conducted in a tertiary care hospital with patients presenting in the Outpatient Department and Indoor ward of Otorhinolaryngology with ulceroproliferative lesion/mass in the oral cavity or oropharynx with histological proof of malignancy. The study was conducted for a period of 6 months. All patients included in the study were assessed clinically and radiology like CT scan or MRI (depending on the site of primary) were done to corroborate with the clinical finding. The clinical profile of each patient was studied in detail and relevant investigations were done in each of them. Indirect laryngoscopy and endoscopic examination using 70 degree Hopkins rigid endoscope was done when required to assess the extent of the tumour. Histopathalogical proof of malignancy was must before including them in our study. Correlation between clinical and radiological findings were assessed using Cohen’s Kappa value.
Results
Predominant age group in oral cancer was found to be 5th decade of life followed by 7th decade with mean age being 60.45.
Predominant age in oropharyngeal cancer was found to be 5th decade of life with mean age being 61.36.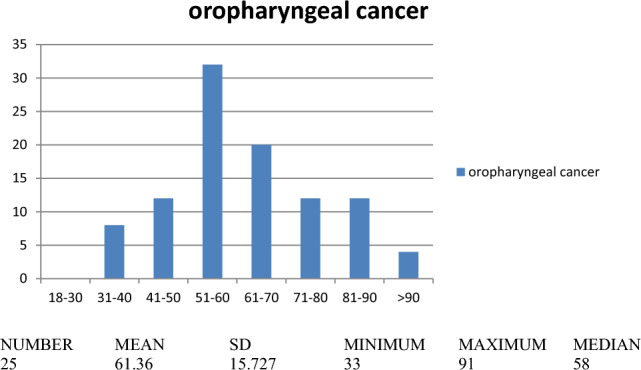
Male population were more affected then female population.
The most common site for oral malignancy was found to be lateral border of tongue accounting for 42.5% followed by floor of mouth and buccal mucosa accounting for 20% each.
The most common site for oropharyngeal malignancy was found to be base of tongue accounting for 48% followed by tonsil accounting for 36%.
Extension of the tumours were assessed radiologically and the subsites for the extension/invasion of disease were divided into involvementof skin, mandible, intrinsic/extrinsic muscles of tongue, medial pterygoid, floor of mouth, larynx, hypopharyx, nasopharynx, masticator space, parapharyngeal space, carotid artery encasement and lung metastatis. The disease extension is depicted diagrammatically below:
The lymph node status of the patient was assessed both clinically and radiologically. The result on the basis of radiology is summarized below:
| LN involvement | Oral cancer | Oropharyngeal cancer |
|---|---|---|
| I | 1 | 1 |
| I | 7 | 1 |
| II | 9 | 14 |
| III | 8 | 2 |
| IV | 0 | 0 |
| V | 0 | 0 |
| NIL | 25 | 11 |
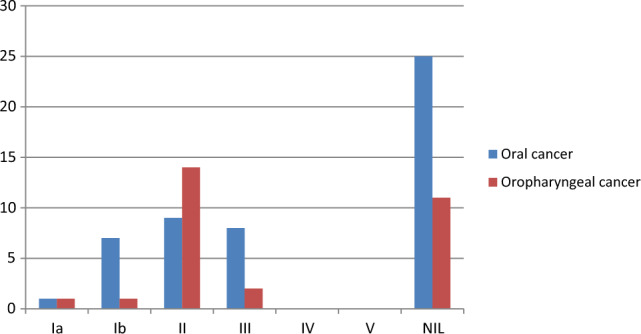
Hence, most of the oral cancers do not reveal any lymph node involvement.
Level II group of lymph nodes were involved majorly in oropharyngeal cancers.
In this study, we have correlated the clinical and radiological findings on the basis of:
Clinical ‘T’ and radiological ‘T’ staging.
Clinical ‘N’ and radiological ‘N’ staging.
Cohen kappa value for correlation between clinical and radiological T for oral cancer is 0.574 which means a moderate degree of agreement.
| Value | Asymp. Std. Error | Approx. T | Approx. Sig | ||
|---|---|---|---|---|---|
| Symmetric measures | |||||
| Measure of Agreement | Kappa | 0.574 | 0.098 | 6.468 | 0.000 |
| N of Valid Cases | 40 | ||||
Cohen kappa value for correlation between clinical and radiological T for oropharyngeal cancer is 0.465 which means a moderate degree of agreement.
| Value | Asymp. Std. Error | Approx. T | Approx. Sig | ||
|---|---|---|---|---|---|
| Symmetric measures | |||||
| Measure of agreement | Kappa | 0.465 | 0.118 | 4.599 | 0.000 |
| N of valid cases | 25 | ||||
Cohen kappa value for correlation between clinical and radiological N for oropharyngeal cancer is 0.868 which means a almost perfect degree of agreement.
| Value | Asymp. Std. Error | Approx. T | Approx. Sig | ||
|---|---|---|---|---|---|
| Symmetric measures | |||||
| Measure of Agreement | Kappa | 0.868 | 0.091 | 5.812 | 0.000 |
| N of Valid Cases | 25 | ||||
Cohen kappa value for correlation between clinical and radiological N for oral cancer is 0.861 which means a almost perfect degree of agreement.
| Value | Asymp. Std. Error | Approx. T | Approx. Sig | ||
|---|---|---|---|---|---|
| Symmetric Measures | |||||
| Measure of Agreement | Kappa | 0.861 | 0.075 | 8.745 | 0.000 |
| N of Valid Cases | 40 | ||||
Discussion
The age incidence of the patients resulted that the patients in their 5th and 7th decade of life have a higher chance of oral cancer with respective percentage being 22.5% and 17.5%. The age predominance among oropharyngeal cancer was found to be in 5th decade followed by 6th decade with respective frequency being 32% and 20%. The mean age for oral cancer and oropharyngeal cancer is 60.45 and 61.36 respectively. According to the study conducted by Nyi Nyi MP et.al, majority of patients (85.4%) were 50 years of age or older and the 60–69-year age group exhibited the highest frequency which is quite similar to this study [7]. The highest number of patients were in the age group 51–60 years in the study conducted by Singh A et.al, thus in accordance with this study [8].
The oral and oropharyngeal carcinoma both are more common among males as compared to females. Male: Female ratio for oral cancer was found to be 3:2. On the other hand, Male: Female ratio for oropharyngeal cancer was found to be 4:1. In our study, the total sample size being 65 including oral and oropharyngeal cancer, the combined percentage of male population is 67.7% and percentage of female population being 32.3% with ratio being 2.1:1. According to the study conducted by Agarwal et.al, among the combined population of oral and oropharyngeal cancers, 83% were male patients and 17% were female patients making male population being the dominant sex,which is similar to this study [8]. According to the study conducted by Rivera H et.al, among the combined population of oral and oropharyngeal cancers, 70% were male patients and 30% were female patients making male population being the dominant sex,thus in accordance with this study [9].
The most common site for oral cancer was found to be lateral border of tongue followed by floor of mouth and buccal mucosa with percentage being 42.5% for tongue and 20% each for floor of mouth and buccal mucosa. On the other hand,the most common site of oropharyngeal cancer was found to be base of tongue followed tonsil with percentage being 48% and 36% respectively. These results were in accordance with most of the previous records [8–10]. According to the study conducted by Nyi Nyi et.al, Tongue was the commonest oral cavity site, accounting for 50% of those cases, and the palatine tonsil comprised the majority of cases within the oropharynx, accounting for 82% of that group,thus, differing from our study where the base of tongue is the commonest anatomical site for oropharyngeal cancer [7]. However, the study conducted by Goel V et.al, buccal mucosa was the most frequently involved site accounting for 52.46% cases followed by tongue 31.15% and gingivobuccal sulcus in 16.39% cases [11].
Contrast Enhanced Computed Topography (CECT) or Magnectic Resonance Imaging (MRI) of oral cavity (with special reference to the involved site) and neck were performed to know the tumour size, exact extension of the tumour,depth of tumour invasion, lymph node status and subsequently assess the TNM and AJCC staging of the disease. In this study, mostly the oral cancers have invaded the muscles of tongue either intrinsic or extrinsic followed by invasion of the floor of mouth, whereas oropharyngeal cancers have more extension towards the larynx. 3 cases each were found to invade medial pterygoid muscle and hypopharynx. Only 1 case each were seen of mandibular periosteum invasion, carotid artery encasement, involvement of masticator space, paraparapharyngeal space, nasopharyx and metastasis to lung. None of the cases had involved the skin. Level II group of lymph nodes were found to be enlarged in majority of cases of both oral and oropharyngeal cancers.
In this study, correlation between clinical ‘T’ & ‘N’ and radiological ‘T’ &’N’ is assessed. In order to obtain the above correlation, Cohen’s Kappa value has been used. The degree of agreement between clinical and radiological ‘T’ of oropharyngeal cancer is k = 0.465 and that of oral cancer is k = 0.574 i.e. moderate agreement between the two in both the types of cancers. The degree of agreement between clinical and radiological ‘N’ of oral cancer is k = 0.861 and that of oropharyngeal cancer is k = 0.868 i.e. almost perfect agreement between the two in both the cancers. Both in oral and oropharyngeal cancers, 10 cases underwent upstaging of the disease radiologically as compared to clinically.
Conclusion
Oral and oropharyngeal cancers pose significant morbidity and mortality among patients, and there is an increasing trend of the disease year after year. Thus, the clinicians should pay great attention to oral mucosa since many non cancerous lesions may have high malignant potential. This study highlights the commonly affected anatomical locations and degree of invasiveness of the disease.With this study, we have tried to determine a correlation between the clinical and radiological findings of the disease.
Declarations
Conflict of interest
No conflict of interest present in the study.
Informed Consent
While undertaking the study, voluntary informed consent was taken from each patient in writing and full confidentiality of the patients has been retained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55(2):74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Sankaranarayanan R, Ramadas K, Thomas G. Effect of screening on oral cancer mortality in Kerala, India: a cluster-randomised controlled trial. Lancet. 2005;365(9475):1927–1933. doi: 10.1016/S0140-6736(05)66658-5. [DOI] [PubMed] [Google Scholar]
- 3.Manoharan N, Tyagi B, Raina V. Cancer incidences in rural Delhi—2004–05. Asian Pacific J Cancer Prev. 2010;11(1):73–78. [PubMed] [Google Scholar]
- 4.Greenlee RT, Hill-Harmon MB, Murray T, Thun M. Cancer statistics. Cancer J Clin. 2001;51(1):15–36. doi: 10.3322/canjclin.51.1.15. [DOI] [PubMed] [Google Scholar]
- 5.Blot WJ, McLaughlin JK, Winn DM. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48(11):3282–3287. [PubMed] [Google Scholar]
- 6.Gillison ML, Koch WM, Capone RB. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. Natl Cancer Inst. 2000;92:709–720. doi: 10.1093/jnci/92.9.709. [DOI] [PubMed] [Google Scholar]
- 7.Nyi Nyi MP, Gibson TN, Hanchard B, Waugh N, McNaughton D. Trends in incidence and age distribution of oral cavity and oropharyngeal squamous cell carcinomas, kingston and st andrew, Jamaica, 1978–2007. West Indian Med J. 2014;63(2):128–133. doi: 10.7727/wimj.2013.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh A, Thukral CL, Gupta K, Sood AS, Singla H, Singh K. Role of MRI in evaluation of malignant lesions of tongue and oral cavity. Pol J Radiol. 2017;82:92–99. doi: 10.12659/PJR.899352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rivera H, Nikitakis NG, Correnti M, Maissi S, Ponce JG. Oral and oropharyngeal cancer in a Venezuelan population. Acta Odontol Latinoam. 2008;21(2):175–180. [PubMed] [Google Scholar]
- 10.Bushra A, Khawer S, Waqar A, Altaf S. Biomedica 27, 2011/Bio-1.Doc P. 29 – 32
- 11.Goel V, Parihar PS, Parihar A, Goel AK, Waghwani K, Gupta R, Bhutekar U. Accuracy of MRI in prediction of tumour thickness and nodal stage in oral tongue and gingivobuccal cancer with clinical correlation and staging. J Clin Diagnostic Res JCDR. 2016;10(6):TC01–TC5. doi: 10.7860/JCDR/2016/17411.7905. [DOI] [PMC free article] [PubMed] [Google Scholar]


