Abstract
A foreign body is an object foreign to location where it found. Foreign body (FB) in ear, nose and aerodigestive tract are common problem seen in children and adults. This study aims to know foreign bodies in terms of type, age, site, gender distribution and method of removal. This prospective study was performed in tertiary care centre from 2020–2022. A total 185 patients with foreign bodies in ear, nose and aero digestive tract who were presented to casualty and OPD were included in study. Their demographic data, age of presentation, clinical presentation, foreign bodies types, site of lodgement and management were included in study. Out of 185 patients, 99 were male [53.51%], 86 were female [46.48%]. FB were found to be maximum in ear (44.32%) followed by nose (37.29%), aerodigestive tract (18.37%). The foreign bodies were removed with or without local anaesthesia in 155 patients and under general anaesthesia in only 30 patients. In some patient foreign bodies like coin, small ear ring was expelled out spontaneously. Left Ear FB (51.21%) was seen most commonly than right ear [45.12%] & both ears (3.67%). Right Side of nasal cavity was frequently involved (69.56%) than left nasal cavity [28.99%] & in both nasal cavities (1.45%). In aerodigestive tract, FB most commonly seen at cricopharynx level [38.23%]. The early childhood group had highest number of patients. Foreign bodies in ENT can be easy as well as difficult at times. Thorough and timely clinical and radiological examination helps in diagnosing and subsequent timely intervention.
Keywords: Foreign bodies, Ear, Nose, Aerodigestive tract, ENT
Introduction
Foreign body is any object in region it is not meant to be there. It can cause harm to body by its presence, so immediate medical attention is required [1]. Ear, nose and aerodigestive tract foreign bodies are common occurrences particularly among children although adult age group is also involved. The factors responsible for foreign bodies insertion into the ENT varies among children and adult. Foreign body in ear, nose and aerodigestive tract is diagnostic and therapeutic challenge to practicing otolaryngologist. Foreign body aspiration is more common in young children than adults since they explore the world with their hands and mouths and have incomplete dentition, limited oro-motor control and immature judgement for objects, so majority of these occur in children under age of 5 years [2]. Adults may aspirate when they are under influence of alcohol, sedatives or head trauma alter their judgement or mental status, with cervicofacial trauma or when neurogenic disease or physical conditions, such as dentures impair sensation [3]. The consequences are from mild disturbances up to life threatening complications so proper recognition and management of foreign bodies are required. So medical attention is important for foreign body removal [4, 5]. Foreign body can be introduced spontaneously or accidently in both adult and children. The symptoms caused by foreign bodies depend on the situation of the object, the nature of object and duration of lodgement. Symptoms in certain cases are absent and sometimes become so urgent that life depends directly on accurate diagnosis and speedy safe removal of the foreign body like in airway. Foreign bodies in ENT may present as mild to severe discomfort, pain, dysphagia, vomiting, choking, bleeding, discharge and impaired functioning of involved site. Respiratory symptoms after foreign body aspiration seen as cough, stridor, chest pain which arise within minute of foreign body entry into tracheobronchial tree causing significant morbidity and mortality so definitive treatment is needed. So, proper management for such cases is needed. The treatment of choice is endoscopic retrieval.
All the foreign bodies need to be removed as they cause acute and chronic complications such as laryngeal spasm, foreign body granuloma, mediastinitis, pericarditis, pneumothorax, pneumomediastinitis and vascular injury caused by perforating foreign bodies [6]. If foreign body is not removed then in ear, it causes oedema and trauma to external auditory canal and in nose it causes nasal infection and rhinolith formation. Aspiration of foreign body is preventable which can be very well avoided by imparting proper education to the parents and public about dangers and consequences about this. Foreign bodies may be classified as organic or inorganic, living or non-living, as per site of lodgement, type of foreign body. Here we will study foreign bodies in ear, nose and upper aerodigestive tract on the basis of history, examination and investigation, their incidence, type of foreign body, site of lodgement, common symptoms with which patient presented, age and gender distribution and their management.
Materials and Methods
Our objectives to conduct prospective study on foreign bodies in ear, nose and aerodigestive tract are-.
To study demographic data of patient presenting with foreign bodies in ear and upper aerodigestive tract.
To study type of foreign body and common site of foreign body lodgment.
To study various type of presentation due to foreign bodies impaction.
To study the management of foreign bodies and complications associated with it.
Inclusion Criteria
Patients presenting with history of ingestion or inhalation of foreign bodies with symptoms like dysphagia, drooling of saliva, stridor. Patients presenting with the history of inserting a foreign body in ear and nose with or without symptoms.
Exclusion Criteria
Foreign body in lower digestive tract, in terminal airway and patients not willing for any treatment or intervention.
A prospective study was performed in department of ENT in tertiary care hospital. A study includes patient with ear, nose and aerodigestive tract foreign bodies lodgement who presented in the ENT OPD and emergency room during the study period of 2 Years [from September 2020 to September 2022]. Patient was evaluated carefully with thorough history taking and complete ENT examinations. Anterior rhinoscopy was performed to diagnosis foreign body in nose. Rigid nasal endoscopic examination was performed in suspected cases of foreign body in nasal cavity that was not visualized with anterior rhinoscopy. Instrument such as jobson horn probe, Tilley’s forceps, crocodile forceps were used in foreign body removal from nose. Otoscopic examination was done for foreign bodies in ear and depending on nature, type, site of foreign body lodgement, they were removed by Wire Vectis, Jobson Horn probe, syringing and suctioning.
For patients with history of foreign body ingestion, imaging was done such as X-ray (antero-posterior & lateral view) including oral cavity, nasopharynx, larynx & esophagus, confirmation was done using computed tomography imaging. If a foreign body seen in oropharynx and hypopharynx then it was removed by laryngoscope or esophagoscope. If foreign body was seen in airway, then it was removed by rigid bronchoscope. Management of the patient depends on the type of foreign body, site of impaction and age of patient.
Observation and Results
During this study, 185 patients visited to hospital with foreign bodies in ear nose and aerodigestive tract.99 were male (53.51%) and 86 were female (46.48%). Of the 185 patients, 82(44.32%) had foreign body in ear, 69(37.29%) in nose and 34(18.37%) in aerodigestive tract. The most commonly involved age group was 0–10 years (74.59%).
The distribution of cases done in age group as 0–10 years ,11-20years,21–30 years,31–40 years,41–50 years,51–60 years and > 60 years.
Foreign Bodies in Ear
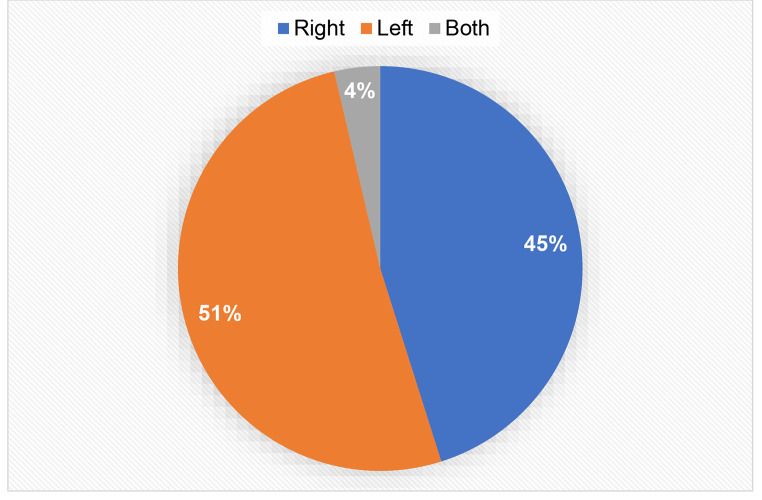
According to age wise, maximum cases seen within age group 0–10 years were 51 i.e. 62.19%. In the present study, male patient presented more commonly with foreign bodies in ear (57.31%) as compared to female (42.68%) (Table 1). Left Ear (51.21%) was seen most commonly involved.45.12% cases seen with foreign bodies in right ear (Fig. 1). In some patients, foreign body was seen in both ears (3.67%). Most commonly seen foreign bodies was pearl in 17 patients followed by matchstick in 10 patients. Most of foreign bodies were removed in OPD/casualty using jobson horn probe and syringing (96.35%). Only 3 cases (3.65%) required removal under GA as these patients were uncooperative/due to impaction of FB (Table 2). Tympanic membrane rupture was noted in two cases. Live insects were killed first by putting olive oil in ear before syringing. Most of foreign bodies were inserted by patient themselves (87.80%) in which most of seen in child and foreign body put by others were around (12.20%).
Table 1.
Distribution of ear, nose and aerodigestive tract foreign bodies by site, gender and age group
| Sex | Age(years) | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | female | 0–10 | 11–20 | 21–30 | 31–40 | 41–50 | 51–60 | > 60 | ||
| Ear | 47 (57.31%) | 35 (42.68%) | 51 | 7 | 9 | 5 | 7 | 0 | 3 | 82 |
| Nose | 34 (49.27%) | 35 (50.73%) | 66 | 1 | 1 | 1 | 0 | 0 | 0 | 69 |
| Aerodigestive tract | 18 (52.95%) | 16 (47.05%) | 20 | 2 | 2 | 1 | 7 | 0 | 2 | 34 |
| 185 | ||||||||||
Fig. 1.
Distribution of cases according to side of ear involved
Table 2.
Methods of removal of foreign bodies in ear, nose and aerodigestive tract
| Mode of management | No of cases | ||
|---|---|---|---|
| Ear | Nose | Aerodigestive tract | |
| Foreign bodies removed in OPD/Casualty/expelled spontaneously | 79 (96.35%) | 63 (91.31%) | 9 (26.47%) and 4 (11.76%) |
| Foreign bodies removed in OT | 3 (3.65%) | 6 (8.69%) | 21 (61.76%) |
| Total | 82 | 69 | 34 |
Foreign Bodies in Nose
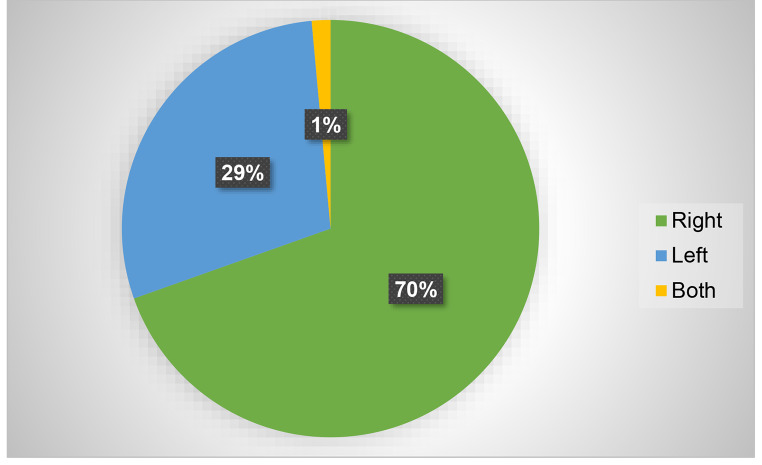
95.65% of cases presenting with foreign bodies in nose were commonly seen within 0–10 years of age. Some foreign bodies were also seen in adult age group. Most of the foreign bodies seen in female patient (50.73%) as compared to male (49.27%) {Table 1). Right Side of nasal cavity was frequently involved (69.56%) than left nasal cavity involvement (28.99%) (Fig. 2). One patient had foreign body in both nasal cavities (1.45%). Most of patients presented with complaining of nasal blockage followed by nasal bleed and foul-smelling discharge. Most of foreign bodies were removed in OPD/Casualty (91.31%). Rhinolith and impacted foreign bodies were removed in OT (8.69%) under general anaesthesia {Table 2). In 14 patients pearls were most common type of FB found in nose followed by button batteries in 8 patients. Most of foreign bodies were inserted by patient themselves (67%) specially in child and foreign body put by others were around 3%.
Fig. 2.
Distribution of cases according to side of nose involved
Foreign Bodies in Aerodigestive Tract
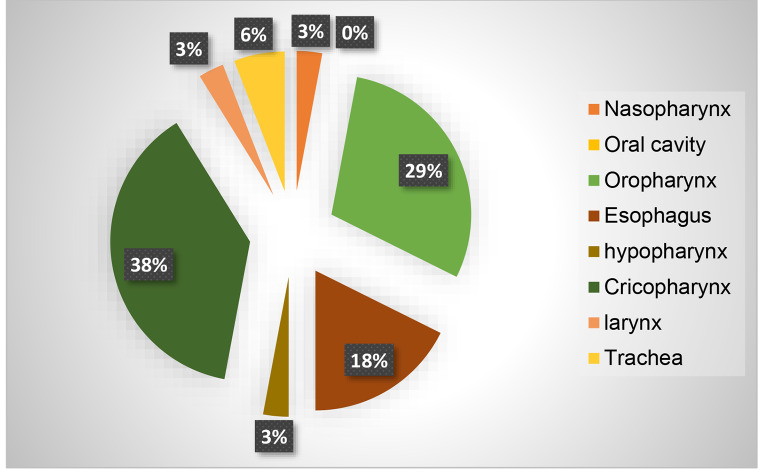
History of ingestion /aspiration of foreign bodies most commonly seen in children (58.83%) of age group 0–10 years. Most of foreign bodies seen in digestive tract (88.23%) and (11.76%) foreign bodies found in airway. Patient presenting with foreign bodies in the aerodigestive tract were male (52.95%) and females were (47.05%) (Table 1). So, it is more commonly seen in male patients. Cricopharynx (38.23%) was the most common site of foreign body impaction in patients presenting with foreign bodies in digestive tract (Fig. 3). Out of 34 patients, 21 patients foreign bodies were removed under general anaesthesia, remaining removed in OPD and Casualty, in some patient foreign bodies like small coin, small ear ring expelled out automatically (Table 2). The clinical features of these patients were mainly dysphagia, throat pain, foreign body sensation in throat and cough.in 3 patients bronchoscopy was done to remove foreign bodies from airway. In 17 patients direct laryngoscopy was done, in 6 patients esophagoscopy was done (Table 3).
Fig. 3.
site of foreign body in aerodigestive tract
Table 3.
Distribution of foreign bodies type
| Type | Number | Percentage |
|---|---|---|
| Inorganic | 139 | 75.13 |
| Organic | 46 | 24.47 |
| Total | 185 | 100 |
Discussion
The present study considered 185 patients examined for ENT foreign bodies in outpatient department and in emergency department of tertiary care centre for 2 years.
Age Incidence
Most of foreign bodies in ENT were most commonly seen in children of age group 0–10 years [58.83%]. The findings were similar in studies of Murty et al., Bruce et al., Stevens et al. & Shraga et al. wherein the age-group was similar [7–9, and 10].
Sex Incidence
Male patients were more common than female patients with ratio 1.15:1; Male preponderance was consistent in studies by Marshal et al., Yeh et al. and Pyman et al. [11, 12, and 13].
Inorganic objects like stone, dals, slate pencils, chalk piece, seeds, and coins were the most common foreign bodies. Inorganic foreign bodies were 75.13% and organic foreign bodies 24.47% (Table no 4).
Table 4.
Mode of Management
| Site of foreign body | Mode of management | No.of patients |
|---|---|---|
| Ear | Jonson horn probe and wire vectis |
7 7 |
| Posterior meatotomy | 1 | |
| syringing | 22 | |
| Microear forceps | 52 | |
| Digestive tract | ||
| Tonsil | Tilleys forceps | 7 |
| Vallecula | Direct laryngoscopy | 2 |
| Hypopharynx | Direct laryngoscopy | 1 |
| Cricopharynx | Direct laryngoscopy | 14 |
| Esophagus | esophagoscopy | 6 |
| Airway | ||
| Nose | Jonson horn, wire vectis, endoscopic retrieval |
63 6 |
| Nasopahrynx | Endoscopic removal | 1 |
| Larynx | Bronchoscopy | 1 |
| Trachea | bronchoscopy | 2 |
Site of Impaction
Most of the ear and nose foreign bodies were diagnosed and treated as OPD cases. Foreign bodies seen in ear was 44.32%, in nose 37.29% and in aerodigestive tract it was 18.37%, this study is similar to Endican S study [14]. Aerodigestive tract foreign bodies were more common in children, age group 0–10 years. In the digestive tract, cricopharynx was most common site and in airway, nose was most common site.
In the nose, pearl and button battery were most commonly seen. Nasal block and unilateral nasal discharge were the commonest complaints. In the nasal foreign bodies, right sided nasal foreign bodies seen more common than left side. Nasal block was most common symptom. Most of foreign bodies insertion was by patient themselves (97%) and more commonly by children. Direct removal of nasal foreign objects was done in 91.31%.
In the ear, pearl and matchstick were the most common foreign bodies found, which were almost like studies by Endican et al. & Akasakal et al. [15, 16]. In the ear foreign bodies, left side (51.21%) was more commonly involved than right side. Most of foreign bodies insertion was by patient themselves (87.80%) and more commonly by children. Direct removal of ear foreign objects was done in 96.35%. In ear, 96.35% of cases were managed in OPD and casualty. Only 3.65% needed general anesthesia.91.31% of nasal foreign body were removed in OPD and casualty, 8.69% cases needed general anaesthesia.
Difficulty in swallowing and throat pain were the most common symptoms in digestive tract foreign bodies. A history of an acute episode of coughing, stridor suggestive of foreign body in respiratory tract. Endoscopies should be carried out keeping the preparation for tracheostomy ready if need arises or if there is a danger of severely compromised airway preliminary tracheostomy may be done in the digestive tract, Fish bone was the most common foreign body in adults and Coins in children, similar to Adhikari et al. & Pokharel et al. [17, 18]. Scarf pin, wooden piece, pistachio shell were the foreign bodies seen in the airway. Majority of patients with foreign body, present within 1 day, but children with objects in the nose and bronchus have shown delayed presentation. Majority of foreign bodies in food passage were removed with esophagoscopy under general anaesthesia. In the removal of foreign bodies in the ear and nose, the complications were very few like tympanic membrane rupture and injury of nasal mucosa. No foreign body in the upper aerodigestive tract should be left alone with the hope that it will come out spontaneously. All the impacted foreign bodies should be removed via per oral endoscopy as soon as possible. Foreign body of the lower respiratory tract were associated with high incidence of mortality. Appropriate suction and haemostasis should be achieved prior to extubation. Unless severely impacted every attempt should be made to extract it one piece rather than fragment.
Conclusion
Foreign bodies in ear, nose and aerodigestive tract are very common complaint with which patients came to otolaryngologist. Most of the foreign bodies were seen in children. The site of impaction, size and shape of foreign body is important to plan further management protocol. Ear and nose foreign bodies were diagnosed and treated as OPD cases. Foreign body of the aerodigestive tract especially the one below the level of oropharynx was removed under general anaesthesia. Rapid or careless eating was the most common causative factor for foreign body in the digestive tract and carelessness on the part of caretaker was the cause in airway foreign bodies. Education of parents and public at large will go long way reducing these preventable in children. Early presentation, timely intervention and skilled removal by otorhinolaryngologist can prevent unnecessary complication and long-term sequelae in ear, nose and aerodigestive tract.
Funding
No funding sources.
Declarations
Compliance with ethical standards
Yes.
Conflict of Interest
None.
Ethical approval
This study was approved by institutional ethics committee.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sarkar S, Roychoudhury A, Roychaudhuri BK. Foreign bodies in ENT in a teaching hospital in Eastern India. Indian J Otolaryngol Head Neck Surg. 2010;62(2):118–120. doi: 10.1007/s12070-010-0040-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jackson C. In: Diseases of the air and food passages of foreign body origin. Jackson CL, editor. Philadelphia: WB Saunders; 1936. [Google Scholar]
- 3.Panieri E, Bass DH. The management of ingested foreign bodies in children - A review of 663 cases. European Journal of Emergency Medicine. 1995 June; 2(2):83–87. [DOI] [PubMed]
- 4.Passàli D., Lauriello M., Bellussi L., PassaliG. C., Passali F.M., Gregori D. Foreign body inhalation in children: An update. Acta Otorhinolaryngol. Ital. 2010; 30:27–32. [PMC free article] [PubMed]
- 5.Tan H.K., Brown K., McGill T., Kenna M.A., Lund D.P., Healy G.B. Airway foreign bodies (FB): A 10-year review. Int. J. Pediatr. Otorhinolaryngol. 2000; 56:91–99. 10.1016/S0165-5876(00)00391-8 [DOI] [PubMed]
- 6.Scher RL. Tegtmeyco CJ, Mclean WC. Vascular injury following foreign body perforation of the oesophagus – Review of the literature and report of a case. Ann Otol Rhinolaryngol. 1990 Sep; 99(9 pt 1):698–702. [DOI] [PubMed]
- 7.Murty PSN. Vijendra S Ingle, Ramakrishna S, Fahim A Shah, Varghese Philip. Foreign bodies in the upper aerodigestive tract. SQU Journal for Scientific Research. Medical Sciences. 2001; 3(2):117–120. [PMC free article] [PubMed]
- 8.Bruce F. Rothmann, Clifford R. Boeckman; foreign bodies in larynx and tracheobronchial tree in children. A review of 225 cases. Ann Otol-Rhinol. Laryngol, 1980, 80;434. [DOI] [PubMed]
- 9.Stevens C; Ardagh M, Abbott GD. Aerodigestive tract foreign bodies in children. One year’s experience at Christchurch Hospital Emergency Department. NZ Med J. 1996; 109(1024):232–3 [PubMed]
- 10.Shraga Blazer; foreign body in airway-review of 200 cases. A.J.D.C. vol 134, 1980; 68–71. [DOI] [PubMed]
- 11.Marshal Strome; Tracheobronchial foreign body an updated approach. Ann Otol.Rhinol. laryngol. 86, 1977;649. [DOI] [PubMed]
- 12.Yeh L.C. et al; foreign bodies in tracheobronchial tree in children -a review of cases over a twenty-year period.Chang Keng Hsueh, 21{1} 1998; 44–9. [PubMed]
- 13.Pyman C; Inhaled foreign bodies in childhood a review of 230 cases. Med J. of Australia, 1, 1975; 62–69. [PubMed]
- 14.Endican S, Garap JP, Dueby SP. Ear, nose and throat foreign bodies in Melanesian Children: An analysis of 1037 cases. In J Pediatr Otorhinolaryngol. 2006 May 15. [DOI] [PubMed]
- 15.Endican S, Garap, JP, Dubey SP. Ear, nose and throat foreign bodies in Melanesian children: an analysis of 1037 cases. Int J pediatr Otorhinolaryngol. 2006; 70(9);1539–45. [DOI] [PubMed]
- 16.Aksakal C. Management of foreign bodies in the ear, nose and throat in children: a review of 829 cases from Northern Anatolia. Otolaryngol Pol. 2020; 74(5):1–5. [DOI] [PubMed]
- 17.Adhikari P, Shrestha B L, Baskota D K, Sinha B K. Accidental foreign body ingestion: analysis of 163 cases. Int Arch Otorhinolaryngol. 2007; 11(3):267–270.
- 18.Pokharel R, Adhikari P, Bhusal C L, GuragainR P. Oesophageal foreign bodies in children. JNMA J Nepal Med Assoc. 2008; 47(172):186–188. [PubMed]