Abstract
The treatment of persistent tympanic membrane perforation is tympanoplasty. Presence of perforation in the anterior annulus of the patients undergoing tympanoplasty surgery is a commonly encountered problem in the postoperative period. In this study, we investigated the effects of supporting anterior tympanomeatal angle with a secondary layer of temporal muscle fascia graft in the patients undergoing type 1 tympanoplasty on postoperative hearing outcomes and early graft success. Twenty-seven patients from our clinic who underwent surgery due to chronic otitis media (COM) and whose anterior tympanomeatal angles were supported with temporal muscle fascia graft as a secondary layer were included in the study. Twelve of the patients were male and 15 of them were female. The mean age of the patients was 43,1 years. The data obtained with retrospective investigations of the patient files were statistically analyzed. Audiological results of 27 patients were obtained in the postoperative 3rd month and were compared with the preoperative results. Preoperative pure tone average of bone-conduction and air conduction were 14,68 ± 7,08 dB and 41,63 ± 9,83 dB, respectively. Postoperative pure tone averages of bone-conduction and air conduction were determined to be 15,02 ± 6,40 dB and 26,38 ± 12,79 dB, respectively. The grafts of all patients were intact at the postoperative 3rd month. We can describe the technique we used as modified sandwich tympanoplasty. In this study we found that in patients that undergoing type 1 tympanoplasty, supporting the anterior tympanomeatal angle with temporal muscle fascia graft as a secondary layer is successful in terms of hearing outcomes and graft success.
Keywords: Tympanoplasty, Temporal muscle fascia graft, Anterior angle, COM
Introduction
Chronic otitis media (COM) is a chronic inflammation of the middle ear and mastoid cavity associated with persistent tympanic membrane perforation and hearing loss. Surgical treatment of the disease is called tympanoplasty. Primary purpose of the tympanoplasty is eradication of the infection. Secondarily, it is aimed to reconstruct the hearing. Successful tympanoplasty depends on the totality and stability of tympanic membrane. The final position of the graft depends on the blood supply as well as the pressure changes between the middle and external ear.
Modern tympanoplasty was described for the first time by Zollner and Wullstein [1]. Various grafting materials like skin, temporalis fascia, fat tissue, perichondrium and cartilage are used to graft the perforation of the tympanic membrane. Success rate of surgery in tympanoplasty is decreased in total perforations and anterior perforations [2]. Various techniques such as underlay, overlay or under-over can be used to graft the perforation of the tympanic membrane. The underlay technique is quick and easy to perform, also ossicular chain can be observed and assessed. However, in anterior perforations, graft placement is difficult and there is a risk of medialization in this technique. The overlay technique allows good visualization of the anterior perforations and does not affect middle ear volume. However, there is a risk of developing keratin cysts within the tympanic membrane if there are remnants from the drum epithelium, and also a risk of blunting of the angle of anterior meatal recess and lateralization of the graft in this technique [3]. Over-underlay tympanoplasty is combination of the underlay and overlay techniques. It was developed to reduce the disadvantages of the underlay and overlay techniques. It can be performed in all types of perforations. In this technique, the exposure is very good, middle ear volume is not affected and it has a high success rate [4]. There are also other techniques called with the same terminology (sandwich tympanoplasty) by Farrior and Raghavan for the repair of tympanic membrane. While temporalis fascia is placed on the lateral and medial sides of the tympanic membrane at the technique described by Farrior in 1983 (fibrous layer is as the meat in the sandwich), pedunculated skin flap is used to cover the temporal muscle fascia graft at the technique described by Raghavan [5, 6].
In our study, tympanomeatal flap was returned to its place after temporal muscle fascia graft placed using under-over technique and a second temporal muscle fascia graft was placed at the anterior tympanomeatal angle. Success rates of graft and hearing results of the patients in the early postoperative period (postoperative 3rd month) were recorded. In our technique, the temporal fascia graft that we placed in the anterior angle region as the 2nd layer differs from the studies in the literature and, therefore we think that it will contribute to the literature.
Materials and Methods
Out of patients with chronic otitis media who applied to our clinic between March 2013 and June 2014, we included those with chronic persistent membrane perforation and hearing loss, who underwent type 1 tympanoplasty with the under-over technique and as a secondary layer temporal fascia placed in the anterior annular angle region. Before the start the study, power analysis was performed. G∗Power (v3.1.7) program was used and statistical analysis showed that there must be at least 20 patients in the study to get 80% power at the level of α = 0.05. The study protocol was approved by Local Ethical Committee and the study was performed in accordance with the Declaration of Helsinki guidelines. Written informed consent was obtained from all patients.
Patients who had central perforations, no ear discharge for at least 1 month, intact middle ear mucosa, no signs of clinical or radiological infection, no cholesteatoma, no ossicular chain pathology with intact and mobile ossicular chain and no previous ear surgery were included the study. Patients who had marginal or total perforations, underwent mastoidectomy, ossicular reconstruction, or cholesteatoma surgery were excluded from the study.
The status of graft and the results of audiological investigation of the patients were recorded at the 3rd month postoperative follow-up. The findings obtained were evaluated by using statistical analysis.
Surgical Technique
Tympanoplasty was performed via postauricular approach and temporalis muscle fascia was used as the graft for both main and second layer in all patients.
After passing through the skin and subcutaneous layers with postauricular incision, temporalis muscle fascia was exposed and temporalis fascia graft was harvested. Then a U-shaped incision was performed towards periosteum and periosteum was elevated. An incision was performed in the external ear canal at the level of Spine of Henle in the region between tympanosquamous and tympanomastoid sutures. Tympanic membrane perforation margins were freshened to de-epithelialize and encourage migration of the mucosal layer and epithelium. Canal incisions were made at 12 o’clock and 6 o’clock and associated with a round knife. A tympanomeatal flap was elevated to gain access to the tympanic cavity. Then the tympanic membrane remnants were elevated from the manubrium mallei and lateral process. The temporalis fascia graft is placed lateral to the long process of the malleus and medial to the tympanic membrane remnant and anterior annulus (Fig. 1) [4]. The middle ear was packed with dry absorbable gelatin sponge (Gelfoam, Pfizer Inc, New York, USA) (Fig. 2). After the graft was given its final position, the tympanomeatal flap was draped over the graft. After controlling whether the perforation margins were covered or not thoroughly by the graft, a second temporal muscle fascia graft was placed as an overlay over the tympanomeatal angle and to support the residual tympanic membrane from the anterior (Figs. 3 and 4). The external auditory canal was packed with Gelfoam, thus lateralization of the graft was prevented and the tympanomeatal flap was secured in its anatomic position (Fig. 4). Spongostan was placed in the external auditory canal; periosteum, subcutaneous layer and skin were sutured, and an extrafor tampon with antibiotic pomade was placed in the external auditory canal and mastoid bandage was applied.
Fig. 1.
Endoscopic view of the placement of main graft using the over-under technique during operation
Green arrow; indicates the main temporal muscle fascia graft
Fig. 2.
Endoscopic view of the placement of absorbable gelatin sponge in the middle ear during operation
Yellow arrow; indicates the absorbable gelatin sponge
Fig. 3.
Endoscopic view of the final position of the grafts during operation
Blue arrow; indicates final position of the main temporal muscle fascia graft, Green arrow; indicates final position of the second temporal muscle fascia graft
Fig. 4.
Endoscopic view of the final position of the tympanomeatal flap during operation
Green arrow; indicates final position of the the tympanomeatal flap, Blue arrow; indicates temporal muscle fascia graft, Red arrow; indicates absorbable gelatin sponge placed in the external ear canal
To summarize our technique; in addition to the main graft material we used in type 1 tympanoplasty operations with the over-under technique to close subtotal and central tympanic membrane perforations; we also supported the anterior annular region with an onlay 2nd layer of temporal muscle fascia graft. This prevented the opening of the graft in this region where graft opening/failure is most common (Fig. 5a and 5b).
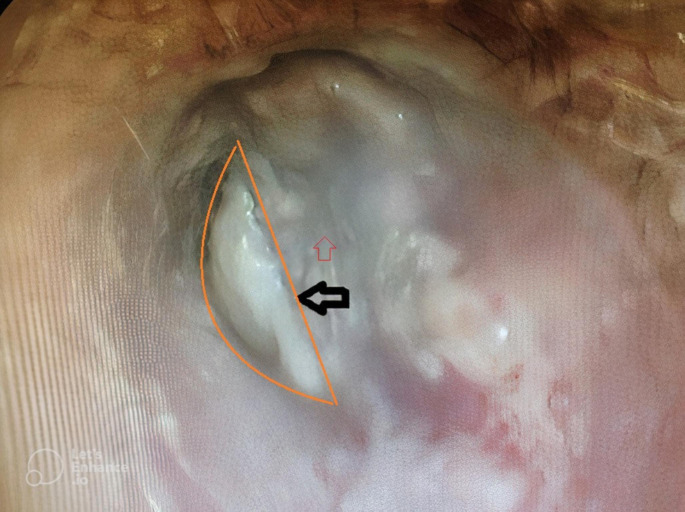
Fig. 5a.
Microscopic view of the tympanic membrane at the postoperative 12nd day
Black arrow and orange half circle; indicates the second temporal muscle fascia graft placed at anterior tympanomeatal angle, Blue arrow and half circle; indicates the main graft
Fig. 5b.
Endoscopic view of the tympanic membrane at the postoperative 12nd day
Black arrow and orange half circle; indicates the second temporal muscle fascia graft placed at anterior tympanomeatal angle, red arrow; indicates the main graft
Postoperative Follow up
Patients were given oral antibiotics (amoxicillin with clavulanic acid 1000 mg 2 × 1) for a week and analgesics (paracetamol 500 mg 2 × 1, as needed) in the postoperative period. During the first 3 days of the postoperative period, patients were followed daily with mastoid bandage. At the end of the first week of postoperative period, sutures were taken and ear canal pack was removed. Then under microscopic view, the external ear canal was aspirated and patients were started with ear drops with antibiotics (ciprofloxacin 2 × 1 drops, 10 days).
Follow-up was done on the first week, first month, third months, sixth months and first year postoperatively, and then yearly for five years. Audiological tests (pure tone audiometry, speech reception thereshold and speech discrimination tests) were performed during these routine control periods from the first month of control.
Statistical Evaluations
NCSS (Number Cruncher Statistical System) 2007&PASS (Power Analysis and Sample Size) 2008 Statistical Software (Utah, USA) program was used for the statistical analysis. During the evaluation of the study data, regarding the comparisons of descriptive statistical methods (Mean, Standard Deviation, Median, Minimum and Maximum) as well as preoperative and postoperative evaluation of quantitative data without normal distribution, Wilcoxon Signed Rank Test was used. Significance was evaluated at the levels of p < 0,01 and p < 0,05.
Results
Twelve of the patients were male and 15 were female. The mean age of the patients was 43,1 years. All patients had a subtotal and central perforation of the tympanic membrane. The graft was intact in all patients at the postoperative 3rd month follow-up.
While measurements of preoperative pure tone averages of air conduction were 41,63 ± 9,83 dB, postoperative pure tone averages of air conduction were 26,38 ± 12,79 dB. Average postoperative air-conduction improvement was 15,25 ± 9,81 dB (p = 0,001; p < 0,01). While measurements of preoperative pure tone averages of bone-conduction were 14,68 ± 7,08 dB, postoperative pure tone averages of bone-conduction were 15,02 ± 6,40 dB. Average postoperative bone-conduction improvement was 0,34 ± 5,72 dB (p = 0,662; p > 0,05) (Table 1; Fig. 6).
Table 1.
Preoperative-Postoperative Evaluations of Measurements Air-Conduction and Bone-Conduction
| Preop | Postop | Difference | p | ||
|---|---|---|---|---|---|
| Air- Conduction | Min-Max (Median) | 25–63 (44) | 8–60 (26) | 0,001** | |
| Mean ± SD | 41,63 ± 9,83 | 26,38 ± 12,79 | 15,25 ± 9,81 | ||
| Bone-Conduction | Min-Max (Median) | 5–32 (13) | 5–33 (14) | 0,662 | |
| Mean ± SD | 14,68 ± 7,08 | 15,02 ± 6,40 | 0,34 ± 5,72 |
Wilcoxon Signed Rank Test **p < 0,01
Fig. 6.

Changes in measurements of preoperative and postoperative air-conductions
Discussion
Tympanic membrane perforation is commonly seen in the otolaryngology clinic. Type 1 tympanoplasty is performed in order to close the perforation in the tympanic membrane, to eradicate infection and to reconstruct hearing. Although sound conduction outcomes are good in the tympanoplasty with single layer temporal fascia, medialization or lateralization of the graft may occur due to pressure changes. This situation negatively affects the overall success of tympanoplasty. Therefore, it is important that the graft does not move from its place and is stable.
The sandwich graft tympanoplasty is a double layer technique. It has been shown to be highly effective in restoring the integrity of the tympanic membrane [4]. We have modified this technique by using two temporalis fascia which is expected to provide a perfect balance between the stability and the acoustic sensitivity of the tympanic membrane. Temporalis fascia is under and overlaid. Thickness of graft is always the main concern for the audiological outcome of the surgery [6]. Since the layers we use are thin temporal fascia tissues, they affect the audiological results minimally.
Repair of the anterior perforation is more challenging than posterior perforation. Higher rates of graft medialization can be observed in anterior perforations due to lack of vision. Also, the re-openings in graft and higher graft failure rates are mostly seen in the anterior angle region due to the change in pressure and poor vascularization after the tympanoplasty operation. Therefore we hypothesis with our technique, this region is supported by the second layer which makes it more resistant to pressure changes, and accordingly, the success of the graft is higher. And we think this 2nd layer graft acts as insurance, thus; it increases the stability of the graft and prevents medialization or lateralization of graft. Moreover, in our technique double layer of graft with temporal fascia, thickness is optimum for acoustic sensitivity versus double layer graft with cartilage.
In the literature, studies that compare single layer and double layer; shows that the use of double layer graft (perichondrium + perichondrium/cartilage) increases the success of the graft compared to single layer (perichondrium or cartilage) [7]. In our study, the double-layered graft made with the modified sandwich technique has comparable stability to that of cartilage, and also significant improvement in hearing has been observed due to the fact that both layers are thin temporal fascia. Moreover; in the literature, there are studies reporting that the use of single-layered cartilage reduces the reperforation rate compared to single-layer fascia [8, 9], and our study shows that the rate of reperforation is reduced by the technique we used (although our technique does not use cartilage but only double-layer temporal muscle fascia), but there is no similar study in the literature.
In our cases, after placing temporalis fascia graft by using over under technique and repositioning tympanomeatal flap to its place, a second temporalis fascia graft was placed as an onlay over the anterior tympanomeatal angle as base, and including the anterior tympanomeatal angle. In the literature, it is reported that the blood supply of the anterior quadrant of tympanic membrane is weaker and therefore graft success is more difficult especially in this quadrant [10]. The aim of this technique is to increase the graft success in the perforations close to anterior tympanomeatal angle by preventing separation of the graft in this region and occurrence of gap in the anterior part with support of the anterior annulus. Also in central perforations, support of the graft by absorbable gelatin sponge from the medial, placing the second graft lateral to the main graft in the anterior tympanomeatal angle can increase the graft success by supporting this region that is at risk of surgical failure.
While preoperative pure tone averages of air conduction and bone-conduction were 41,63 ± 9,83 dB and 14,68 ± 7,08 dB, respectively, postoperative 3rd month pure tone averages of air conduction and bone-conduction were determined to be 26,38 ± 12,79 dB (p = 0,001; p < 0,01) and 15,02 ± 6,40 dB, respectively. Average air-conduction gain was determined to be 15,25 ± 9,81 dB. Van Baarle et al. [11] found the gain as 8.3 dB and Yılmaz et al. [12] found as 10 dB. The results of our study are similar with literature. We expect this gain obtained in the early postoperative period will increase further in the future follow-ups.
In our experience, our technique avoids medialization or lateralization of the graft, and also in our technique, even though a secondary layer graft is placed in the anterior annular angle area and this area is supported by this graft, this has no negative effect on hearing. And these are the advantages of our modified tympanoplasty technique. The success rate of tympanoplasty using temporalis fascia varies between 2% and 93.3% in the literature [12–14]. Although the graft success obtained in our study are early results, considering the results in the literature, our technique can be considered successful.
Conclusion
In tympanoplasty, problems such as fascia graft medialization, lateralization and reperforations are more common in single-layer graft techniques. A double layered graft technique such as our new technique, provides better results in postoperative graft success and hearing. When the early postoperative period results are evaluated; we think that in type 1 tympanoplasty with temporal muscle fascia graft by under-over technique, placement of onlay temporal facia graft as a second layer at anterior tympanomeatal angle, is successful in terms of graft success and hearing outcomes.
Authors’ contributions
Serhan Keskin: Study design, experimental applications, statistics, literature research, writing.
Arzu Tatlıpınar: Idea generation, study design, literature research, writing.
Vehip Beyazgün: Study design, idea generation, writing.
Tuğba Aslan Dündar: Experimental applications, statistics, writing.
Funding
There is no funding/ financial support.
Declarations
Ethics approval
The study protocol was approved by Local Ethical Committee before study.
Compliance with ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Conflict of Interest
None. This study was presented in 36. National Turkish Otolaryngology and Head Neck Surgery Meeting in Antalya, Turkey.
Informed Consent
Written informed consent was obtained from all patients.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rizer FM. Overlay versus underlay tympanoplasty. Part I: historical review of the literature. Laryngoscope. 1997;107:1–25. doi: 10.1097/00005537-199712001-00001. [DOI] [PubMed] [Google Scholar]
- 2.Adkins WY, White B. Type I tympanoplasty: influencing factors. Laryngoscope. 1984;94:916–918. doi: 10.1288/00005537-198407000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Sergi B, Galli J, De Corso E, Parilla C, Paludetti G. Overlay versus underlay myringoplasty: report of outcomes considering closure of perforation and hearing function. Acta Otorhinolaryngol Ital. 2011;31:366–371. [PMC free article] [PubMed] [Google Scholar]
- 4.Kartush JM, Michaelides EM, Becvarovski Z, LaRouere MJ. Over under tympanoplasty. Laryngoscope. 2002;112:802–807. doi: 10.1097/00005537-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Farrior JB. The anterior tympanomeatal angle in tympanoplasty: surgical techniques for the prevention of blunting. Laryngoscope. 1983;93:992–997. doi: 10.1288/00005537-198308000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Raghavan U, Malik DSI, Mahmoud NA. Myringoplasty: update on onlay pedicle skin flap and temporalis fascia sandwich graft. J Laryngol Otol. 2000;114:174–177. doi: 10.1258/0022215001905274. [DOI] [PubMed] [Google Scholar]
- 7.Bedri E, Korra B, Redleaf M, Worku A. Double-layer tympanic membrane graft in type I Tympanoplasty. Annals of Otology Rhinology & Laryngology Sep. 2019;128(9):795–801. doi: 10.1177/0003489419843551. [DOI] [PubMed] [Google Scholar]
- 8.Kolethekkat AA, Al Abri R, Al Zaabi K, et al. Cartilage rim augmented fascia tympanoplasty: a more effective composite graft model than temporalis fascia tympanoplasty. J Laryngol Otol. 2018;132:497–504. doi: 10.1017/S0022215118000762. [DOI] [PubMed] [Google Scholar]
- 9.Guler I, Baklaci D, Kuzucu I, Kum RO, Ozcan M. Comparison of temporalis fascia and tragal cartilage grafts in type 1 tympanoplasty in elderly patients. Auris Nasus Larynx Jun. 2019;46(3):319–323. doi: 10.1016/j.anl.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Hough JV. Revision tympanoplasty including anterior perforations and lateralization of grafts. Otolaryngol Clin North Am. 2006;39:661–675. doi: 10.1016/j.otc.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Van Baarle PW, Huygen PL, Brinkman WF. Findings in surgery for chronic otitis media. A retrospective data analysis of 2225 cases followed for 2 years. Clin Otolaryngol Allied Sci. 1983;8:151–158. doi: 10.1111/j.1365-2273.1983.tb01419.x. [DOI] [PubMed] [Google Scholar]
- 12.Yılmaz S, Karaman E, Güçlü E, Yaman H, Akkan N. Tip 1 Timpanoplasti Sonuçlarımız. Düzce Üniversitesi Tıp Fakültesi. Dergisi. 2009;11:33–36. [Google Scholar]
- 13.Mishiro Y, Sakagami M, Takahashi Y. Tympanoplasty with and without mastoidectomy for non-cholesteatomatous chronic otitis media. Eur Arch Otorhinolaryngol. 2001;258:13–15. doi: 10.1007/PL00007516. [DOI] [PubMed] [Google Scholar]
- 14.Tatlıpınar A, Gökçeer T, Tuncel A. Timpanoplastide temporal kas fasya greftinin başarısını etkileyen faktörler. KBB Forum. 2010;9(4):88–93. [Google Scholar]