Abstract
Several sports have published consensus statements on methods and reporting of epidemiological studies concerning injuries and illnesses with football (soccer) producing one of the first guidelines. This football-specific consensus statement was published in 2006 and required an update to align with scientific developments in the field. The International Olympic Committee (IOC) recently released a sports-generic consensus statement outlining methods for recording and reporting epidemiological data on injury and illness in sport and encouraged the development of sport-specific extensions.
The Fédération Internationale de Football Association Medical Scientific Advisory Board established a panel of 16 football medicine and/or science experts, two players and one coach. With a foundation in the IOC consensus statement, the panel performed literature reviews on each included subtopic and performed two rounds of voting prior to and during a 2-day consensus meeting. The panel agreed on 40 of 75 pre-meeting and 21 of 44 meeting voting statements, respectively. The methodology and definitions presented in this comprehensive football-specific extension should ensure more consistent study designs, data collection procedures and use of nomenclature in future epidemiological studies of football injuries and illnesses regardless of setting. It should facilitate comparisons across studies and pooling of data.
Keywords: Football, IOC, Consensus, Soccer, Epidemiology
Key points.
Standardised methods and reporting of studies on injuries and illnesses in sports are important to improve injury and illness management and prevention strategies.
The consensus statement for football published in 2006 covered only methodology in football injury epidemiological studies and required updating to align with scientific developments.
A diverse expert panel agreed on several recommendations in a football-specific extension of the International Olympic Committee (IOC) consensus statement on methods for recording and reporting epidemiological data on injury and illness in sport.
The main amendments from the IOC consensus statement were to use football-specific terminology, to define return to football after a health problem, to categorise the severity of a health problem in more detail, and to define match and perimatch exposures.
The proposed methodology and definitions presented in this comprehensive football-specific extension should ensure more consistent study designs, data collection procedures and use of nomenclature in future surveillance studies of football injuries and illnesses.
Methodological consistency should facilitate comparisons across studies and pooling of data.
Introduction
Continuous injury and illness surveillance is essential to assess and direct efforts to improve athlete health. Several consensus statements aimed at standardising methodology and reporting of epidemiological studies were published during the 2000s for both team and individual sports.1–12
The first consensus statement on injury definitions and data collection procedures in football was published in 2006,3 but requires an update to align with scientific developments on several aspects including onset, recurrent complaints and the inclusion of illness registration. The International Olympic Committee (IOC) recently released a sports-generic consensus statement on the methods for recording and reporting epidemiological data on injury and illness in sport.13 In that statement (hereafter referred to as the IOC consensus statement), there was a call for subsequent sport-specific extensions with more detailed recommendations relevant to a sport and/or setting. Sports-specific extensions have subsequently been published over the last 2 years for golf, tennis, cycling and Para sports.14–18 Sport-specific extensions should result in more consistent study designs, data collection procedures and nomenclature in future injury and illness surveillance studies in the sports targeted.
The objective of this comprehensive consensus statement is to provide a football-specific extension, with updated methodology and reporting of epidemiological studies in football.
Methods
The Fédération Internationale de Football Association (FIFA) Medical Subdivision and the associated Medical Scientific Advisory Board initiated this project.
Project planning and panel selection
A steering group (MW, TEA, MM, AMc and AMa) was established to plan the consensus procedure and the consensus meeting. A first online meeting was held on 8 March 2021 when potential participants based on scientific merits, different expertise fields, previous consensus experience, international confederation representation and equity were identified by the steering group. A second online meeting was held on 28 September 2021 at which AS joined the steering group, and the participant invitation list was finalised. AMa sent official invitation letters in October 2021, and all invitees except one accepted the invitation to participate and were available for the consensus meeting scheduled for 14–15 March 2022.
The consensus panel consisted of members of the FIFA Medical Subdivision and its Medical Scientific Advisory Board (including all steering group members) and representatives of the FIFA Medical Committee, the FIFA Medical Centres of Excellence and all six FIFA confederations worldwide. The panel members represented multiple stakeholder groups with relevant professions and expertise and reflected a broad range of clinical, scientific, sex and geographical representation (online supplemental table 1). The panel and author list consist of five women and eleven men, ages 28–77 years. Eleven panel members are physicians from different disciplines, three are sports scientists and two are sports physiotherapists. In order to include relevant stakeholder perspectives, we additionally invited two players and one coach from men’s and women’s professional football through personal connections. They participated online during parts of the consensus meeting and shared their personal perspectives and experiences with injuries and illnesses via a discussion with the panel members. They declined to participate in the voting procedures and in the writing of the manuscript.
bjsports-2022-106405supp001.pdf (242.4KB, pdf)
Meeting preparations and working groups
The steering group reviewed all existing consensus statements on injury and illness surveillance in sport and divided the panel members into working groups at the beginning of January 2022. The working groups were tasked to comprehensively review different subtopics in line with the subsections and main subheadings of the IOC consensus statement. Each working group consisted of 2–3 experts, led by a FIFA Medical Scientific Advisory Board member, and was given 4 weeks to draft an overview document of their topic. This overview document included the following points:
Descriptions/definitions from previous relevant consensus statements.
A brief summary of the IOC consensus statement recommendation(s).
Any potentially relevant adjustments from consensus extensions of other sports.
Non-systematic literature reviews of relevant topic-specific publications similar to the IOC consensus statement and other sport-specific extensions.
Initial preliminary recommendations for amendments and suggested voting statements for the consensus meeting.
Pre-meeting voting on the preliminary recommendations
The steering group reviewed the documents from all working groups in mid-February 2022, collated and aligned the voting statements related to each topic, and subsequently circulated for anonymous voting to all participants using a Microsoft Forms online questionnaire. Participants were given 1 week, including one reminder after 5 days, to complete the voting. Each statement was scored independently by all participants (100% response rate) using a 9-point Likert scale ranging from 1 (strongly disagree) to 9 (strongly agree), based on the Grading of Recommendations Assessment, Development and Evaluation scale.19 For each topic, there was also an optional free text box to allow participants to provide further comments on their scoring and to propose new or modified statements. A priori, we decided that agreement was reached if ≥70% of participants scored 7–9 and <15% of panel members scored 1–3, and disagreement if ≥70% scored 1–3 and <15% of panel members scored 7–9, respectively.20 Finally, the steering group reviewed the premeeting voting results, the optional free text comments, and any new or modified statements to develop the agenda and voting statements for the consensus meeting. The panel agreed on 40 of 75 pre-meeting voting statements (online supplemental table 2).
Consensus meeting
The consensus meeting took place in Zurich, Switzerland, 14–15 March 2022. Given the travel restrictions associated with the COVID-19 pandemic, one participant (MF) joined online, whereas the rest of the panel participants were present in-person. The steering group lead (MM) chaired the meeting. A working group representative presented their recommendations and discussion points along with the corresponding premeeting voting results and free-text comments. Statements reaching premeeting voting agreement were not discussed further unless there were related free text comments. All participants were provided the opportunity to present their views on statements not reaching premeeting agreement. Following each topic discussion, a subsequent round of anonymous voting, using the same scoring as for the premeeting voting, was carried out for all original statements that did not reach agreement initially as well as for all new and modified statements. The panel agreed on 21 of 44 meeting voting statements (online supplemental table 2).
Manuscript preparation
Following the consensus meeting, the steering group prepared a first draft of the manuscript and circulated it to the panel members for review. After that, based on feedback, a second draft was prepared and sent to all authors for final comments/approval. The manuscript was prepared while considering recent methodological recommendations,21 22 as well as the consensus-specific author guidelines.23 In particular, panel members were informed that they were able to present their potential dissent on statements that reached group agreement by writing a minority opinion in online supplemental table 2.
Consensus recommendations
The following sections provide an overview of recommended amendments to the IOC consensus statement with a summary in table 1.
Table 1.
Summary of the main additions and modifications to the IOC consensus statement13 relevant to football
| Topic | Amendments |
| Sport, athlete and competition | Football, player and match |
| Mechanism of injury | Football-specific player actions to be reported for sudden-onset injuries |
| Injury diagnosis | Hip and groin categorised separately (and not combined), and adding complete and partial tendon avulsions to the descriptive notes for tendon rupture |
| Table 6 | Adding percentage to the absolute number of injuries and to report the IQR for median time-loss days (not the CI) |
| Table 6 | Less focus on upper limb injuries and more focus on lower limb injuries |
| Injury severity categories | 0 days, 1–3 days, 4–7 days, 8–28 days, 29–90 days, 91–180 days and >180 days |
| Return to football | The date when the injured player returns to full unrestricted team training without modifications in duration and/or activities |
| Match exposure | Organised scheduled match play between opposing teams (not including internal training matches within the same team/club) |
| Prematch warm-up | Reported as a separate training category |
| Postmatch cool-down | Reported as other training |
| Rehabilitation sessions | Excluded from training exposure |
| Expressing risk | Reporting measures of occurrence |
| Players (according to age) | Adults or youths |
| Players (according to contract) | Amateurs or professionals |
| Players (non-organised) | Recreational players |
| Playing level | International league ranking (where accessible) and actual playing division (out of the total number of divisions in the league system) to be reported |
IOC, International Olympic Committee.
A full list of voting results, including any dissenting opinions or areas of disagreement, can be found in online supplemental table 2. A plain language summary is enclosed in online supplemental table 3. To adapt the general terminology to football, we agreed to replace athlete with player, sport(s) with football and competition with match throughout this consensus extension.
Defining and classifying health problems
Terminology
We support the IOC consensus statement definition of a health problem. For clarity, we integrated the health definition from the WHO and reformulated the wording to ‘any condition that reduces a player’s normal state of complete physical, mental and social well-being, irrespective of its consequences on the player’s football participation or performance or whether the player sought medical attention’. We agreed to adopt the recommended separation of health problems by their consequence of any complaint, medical attention and time loss.
Defining injury and illness
To harmonise with the separate categorisation of health problems according to the relationship to sports activity, we agreed to remove ‘participation in sports (football)’ in the definition of injury from the IOC consensus statement. Thus, the recommended definition of injury is: ‘tissue damage or other derangement of normal physical function, resulting from rapid or repetitive transfer of kinetic energy’. The definition of illness was modified by adding the word ‘health’ and replacing ‘related to’ with ‘considered as’. The recommended definition of illness is: ‘a health complaint or disorder experienced by a player not considered as an injury’. For example, a mental illness can be considered ‘related to’ a long-term injury but cannot be ‘considered as’ an injury.
Relationship to football activity
We recommend using the definition from the IOC consensus statement, dividing health problems as resulting directly from participation in football, indirectly from participation in football, or not at all related to participation in football.
Mode of onset
There was agreement to recommend using the definition of mode of onset from the IOC consensus statement, dividing health problems by presentation into sudden onset and gradual onset.
Mechanism of injury
The consensus of the panel was to recommend using the definition of mechanism of injury from the IOC consensus statement, dividing the sudden-onset injuries by mechanism into non-contact, indirect contact (person or object) and direct contact (person or object). For other football-specific contact categories, we added categories of person into opponent, team-mate, match official, pitch invader and other pitch-side staff, and objects into ball, goal post, pitch object, object from the crowd, and other (unspecified) object. Furthermore, we recommend expanding on the main injury-inciting circumstance by providing a general impression of the football-specific player actions that should be reported for all sudden-onset injuries (table 2). We recognise that there might be some overlap between actions (eg, if a player is running with the ball and simultaneously being tackled). In such cases, the player action considered most relevant for the injury should be selected. We acknowledge that this table requires additional validation and may likely be modified in the future as well as it only provides a general impression of injury mechanisms. A more detailed analysis of the injury inciting circumstances of specific injuries is recommended to better understand potential injury mechanisms. This can follow more comprehensive standardised reporting, such as recommended in the Football Injury Inciting Circumstances Classification System.24 Ideally, video reviews are recommended to be performed by both analysts and injured players, as this can potentially assist in determining a more accurate time of injury/symptom onset. For sudden-onset match injuries, details on any rule infringement (foul/no foul and any cards awarded by the referee to the players involved) should be reported.
Table 2.
Recommended reporting categories and definitions of player actions at the time of a sudden-onset injury
| Player action | Definition |
| Running | Running at any speed (acceleration/steady speed/deceleration), including linear, curved or other types of runs with or without the ball |
| Change of direction | A specific moment in a run with a sharp deviation (any angle) from the line of running with and without the ball |
| Kicking | Any type of kick, including shooting/passing/crossing/set pieces/penalty |
| Heading | Heading or attempting to head the ball (in a duel or alone) |
| Tackle | Injured player being tackled or is tackling an opponent with any body part |
| Landing | Landing on one or both feet after a jump |
| Falling | When a player is falling or diving—for example, loses balance/stability and ends up on the ground with any part of the body other than the feet |
| Controlling the ball | When a player attempts to control the ball—for example, while receiving the ball, reaching for the ball or sliding for the ball (not a sliding tackle) |
| Hit by ball | Any hit by the ball including a block, deflection or other accidental hits |
| Collision | Players unintentionally running/jumping into each other, the goal post or any other object on/around the pitch |
| Other player action | For example, a throw-in, setting off in a jump, or specific goalkeeper actions not included in the other categories |
| Unknown | The action of the player at the time of injury is unknown: either not witnessed by others, or the player is unable to recollect |
Multiple events and health problems
We agreed to recommend using the system from the IOC consensus statement on how to record multiple health problems during the study period (see figure 2 in that statement). The number of reported health problems and the number of players affected must be reported because these measures will unlikely be the same.
Subsequent, recurrent and/or exacerbation of health problems
We agreed to recommend using the categories from the IOC consensus statement where it should initially be determined whether a health problem following an index injury/illness is a subsequent injury/illness to the same location (body area/system) or a subsequent new injury/illness. As this is not clearly specified in the IOC consensus statement, we recommend that a subsequent health problem is called a recurrence if it is the same type/diagnosis; if not, it is called a subsequent local injury/illness. For recurrences, if the player’s health problem was fully healed/recovered and the player has returned to football, the subsequent health problem is called a reinjury/repeated illness; if not, it is called an exacerbation (table 3).
Table 3.
Examples of how to record subsequent injuries in football
| Index injury Diagnosis and injury date |
Subsequent injury Diagnosis and injury date |
Subsequent injury to the same location? | Same type/diagnosis as the index injury? | Was the index injury healed/fully recovered? | Classification |
| Biceps femoris muscle injury (right) 21 November 2022 |
Biceps femoris muscle injury (right) 18 December 2022 |
Yes | Yes | Yes | Recurrence: Re-injury |
| Biceps femoris muscle injury (right) 29 November 2022 |
Yes | Yes | No | Recurrence: Exacerbation | |
| Semimembranosus muscle injury (right) 18 December 2022 |
Yes | No | N/A | Subsequent local injury | |
| Biceps femoris muscle injury (left) 18 December 2022 |
No | N/A | N/A | Subsequent new injury |
N/A, not applicable.
A typical football-relevant example of an exacerbation is gradual-onset tendinopathies, where players can often play matches in parallel with modified football training and rehabilitation. Consequently, this injury is counted only once rather than recording several early reinjuries, which would distort the overall injury statistics; one further example of how to record subsequent injuries is seen in table 3. We recommend reporting details on injury recurrence in days rather than the categorisation of ‘early’ (within 2 months following return to football), ‘late’ (two to twelve months) and ‘delayed’ (more than twelve months) recurrences as was originally recommended in the 2006 football consensus statement.3
Football injury and illness diagnoses
We recommend classifying injuries according to body regions/areas, tissue types and pathology, and illnesses using organ systems/regions and aetiology, as categorised in tables 4–5 and 7–9 in the IOC consensus statement. Exceptions include dividing the body area ‘hip/groin’ to ‘hip’ and ‘groin’ and adding ‘complete and partial tendon avulsions’ to the notes for the pathology type tendon rupture.
The separation of the hip and groin areas will affect the grouping of diagnoses used in diagnostic coding systems and will need further standardisation to ensure reliable categorisation. For example, when using the Orchard Sport Injury & Illness Classification System (OSIICS),25 we recommend to group diagnostic codes related to:
Hip joint under ‘hip’ (codes beginning with GA, GC, GD, GE, GG, GL, GQ).
-
Muscles, tendons, bursae, abrasions etc (codes beginning with GB, GH, GI, GK, GM, GN, GO, GR, GT) may be grouped according to their position:
Anterior locations grouped under ‘groin’.
Lateral and posterior locations under ‘hip’.
Bone stress, fractures and non-specific diagnoses (codes beginning with GF, GG, GJ, GP, GS, GU, GZ) may be differentiated according to their proximity to either the pubic symphysis or the hip joint.
The IOC consensus statement recommends a structured, standardised overview table (see table 6 in that statement) to provide an overview of the most common injuries. We agreed to modify this table according to the most common injuries in football. We also recommend reporting the percentages of all injuries with the absolute numbers and the median with the IQR for time-loss days instead of a 95% CI. We recommend the revised overview table in the main manuscript be the minimum requirement for each future study (table 4). Importantly, studies should also specify data on training and match injuries in a separate table or an online supplemental file. We recommend that authors create at least one expanded table in a online supplemental file using the same structure and column headings but with a more extensive overview of diagnoses, ensuring player confidentiality for injuries with small numbers. Especially if the study objective is on specific injury types (eg, muscle injuries or fractures) and specific populations (eg, detailed apophysis injuries in youth players), it will also facilitate improved future pooling of data from studies.
Table 4.
Football-specific recommendations and additions to table 6 in the IOC consensus statement13
| Region | Injuries | Injury incidence | Median time-loss | Injury burden |
|
Body area
Tissue Type Diagnosis |
n (%) | Injuries/1000 hours (95% CI) | Days (IQR) | Days lost/1000 hours (95% CI) |
|
Head
Concussion |
||||
| Neck | ||||
| Shoulder | ||||
| Upper arm, elbow and forearm | ||||
| Wrist and hand | ||||
| Chest and thoracic spine | ||||
| Lumbosacral | ||||
| Non-specific low back pain | ||||
| Abdomen | ||||
|
Hip
Muscle/tendon Iliopsoas muscle injury Cartilage/synovium/bursa Femuroacetabular impingement syndrome |
||||
| Groin | ||||
| Muscle/tendon | ||||
| Adductor muscle injury | ||||
| Adductor-related groin pain | ||||
| Thigh | ||||
| Muscle/tendon | ||||
| Hamstring muscle injury | ||||
| Quadriceps muscle injury | ||||
| Muscle contusion | ||||
| Knee | ||||
| Muscle/tendon | ||||
| Patellar tendinopathy | ||||
| Cartilage/synovium/bursa | ||||
| Cartilage injury
Meniscal injury |
||||
| Ligament/joint capsule | ||||
| Anterior cruciate ligament injury | ||||
| Medial collateral ligament injury | ||||
| Lateral collateral ligament injury | ||||
| Posterior cruciate ligament injury | ||||
| Lower leg | ||||
| Muscle/tendon | ||||
| Calf muscle injury | ||||
| Achilles tendinopathy | ||||
| Muscle contusion | ||||
| Fracture (including stress fracture) | ||||
| Ankle | ||||
| Muscle/tendon | ||||
| Fracture (including stress fracture) | ||||
| Bone contusion | ||||
| Cartilage/synovium/bursa injury | ||||
| Ligament/joint capsule | ||||
| Lateral ligament injury | ||||
| Medial ligament injury | ||||
| Syndesmosis injury | ||||
| Foot | ||||
| Muscle/tendon | ||||
| Fracture (including stress fracture) | ||||
| Bone contusion |
IOC, International Olympic Committee.
There was an agreement to record and classify multiple injuries in the same event separately but only to count once for incidence calculations as per the IOC consensus statement. Injury severity should also be based on the principal (most severe) injury. For example, when a player sustains a wrist sprain and an anterior cruciate ligament (ACL) injury of the knee after a one-legged landing and fall following a heading duel, these injuries should be counted only once in the incidence statistics, and the severity determined according to the ACL injury.
Finally, we also encourage researchers to use recommended and updated sports-specific diagnostic coding systems, such as the Sport Medicine Diagnostic Coding System or the OSIICS, which has an accompanying Excel data file.26
Severity of health problems and return to football
Time-loss data distribution is likely to be right-skewed.13 Therefore, in line with the IOC consensus statement, aggregated data across players should report severity as the total number of days lost together with median days lost and quartiles. If large, normally distributed datasets report mean and SD, the median should also be reported to facilitate comparisons across studies. As recommended in the IOC consensus statement, describing severe health problems leading to retirement from football, permanent disability or death in days of time-loss is considered inappropriate. Also, there were no amendments regarding specific definitions of catastrophic injury or fatality.
Time loss from training and match play
We recommend using the concept of counting days from occurrence of a health problem to return to play from the IOC consensus statement. Specifically, we recommend that researchers record the number of days the player is unavailable for training or match play, that is, from the date of onset (day 0) to the date of return to football. We recommend using the following time bins when categorising injury severity: 0 days, 1–3 days, 4–7 days, 8–28 days, 29–90 days, 91–180 days and >180 days. The underlying rationale is that more detailed severity categories than designated in the IOC consensus statement can help to communicate the consequences of injuries, especially severe injuries, more precisely with other stakeholders such as the coaching staff, the club and national association management, media, etc. Table 5 presents examples of how to count time loss and categorise severity with elements combined from table 1 in the football consensus statement and table 10 in the IOC consensus statement.3 13 In the rare occurrences of injuries or illnesses leading to retirement from football, permanent disability or death should be excluded from the calculations of days lost and in the categorisation into severity categories.
Table 5.
Examples of how to record time-loss and calculate injury/illness severity in football
| Case | Medical attention/time-loss definition | Days lost | Severity category | Comment |
| A player interrupts a training session due to diarrhoea but resumes full training the following day | One time-loss illness | 0 | 0 days | Day 0 illness |
| A player injures the left hamstring muscle during a match and cannot continue to play. Images show a partial muscle rupture affecting the long head of the biceps femoris | One time-loss injury | 45 | 29–90 days | |
| A young player with Osgood-Schlatter disease reports knee pain at the start of a training camp and trains fully on Monday, Tuesday and Thursday but misses training sessions on Wednesday and Friday | One time-loss injury | 2 | 1–3 days | ‘Intermittent’ time-loss |
| A player sustains a thigh contusion on Sunday and can train on Monday and Tuesday, but is unable to train due to increased pain on Wednesday and returns to play next Monday | One time-loss injury with injury date ‘Sunday’, but with time-loss from Wednesday to Sunday | 5 | 4–7 days | ‘Delayed’ time-loss |
| A player suffers iliopsoas-related groin pain not resulting in any time-loss initially, followed by a 1 month pain-free period. The pain then relapses, requiring time loss from play for 3 weeks. Following another pain-free interval of 9 weeks, the player suffers hip joint-related pain indicative of femoral acetabular impingement syndrome requiring time loss from play for the remaining 6 weeks of the campaign | Record the first pain episode as a medical attention injury and both the second and third episodes as time-loss injuries | 0 21 42 |
0 days 8–28 days 29–90 days |
Index injury, recurrence (reinjury) and subsequent local injury with a medical attention injury definition No injury, index injury and subsequent local injury with a time-loss injury definition |
| A player steps on the forearm of a goalkeeper who suffers both a superficial laceration and contusion of the forearm with the development of an acute compartment syndrome requiring surgical intervention and 2 months off | The two injuries should be recorded separately but counted only once in the calculation of incidence with a time-loss definition | 0 61 |
0 days 29–90 days |
Multiple injuries with injury severity determined by the most severe injury |
| A senior footballer suffers a total Achilles tendon rupture when pushing off for a heading duel. It requires surgery, but the player suffers a deep wound infection with repeated surgeries needed. After 15 months, the player decides to retire from football | Retirement from football | N/A | N/A | Should be reported separately |
Return to football
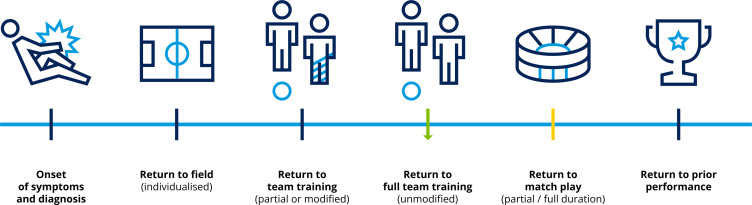
When reviewing the literature, we found three, somewhat differing models, interpreting and describing return to sport as a continuum.27–29 We believe it is important to understand that returning to football involves several stages, from injury to full team training, match play and preinjury performance.28
For injury and illness surveillance studies in football, however, there is a need for a fixed time point for return to football to standardise time-loss duration (figure 1). We, therefore, recommend defining this according to the date when the injured player returns to full unrestricted team training without modifications in duration and/or activities. Normally, return to training will precede return to match play. However, in cases where the player participates in partial or full match play prior to full team training, the date of this match should be recorded. In periods without training or matches (eg, during off-season periods), the date when the player is considered medically cleared and available for full team training should be used. Online supplemental table 4 shows the different stages of the return to football continuum illustrated for a player with ACL reconstruction.
Figure 1.
Overview of key time points in the return to football continuum modified from Ardern and Pruna.28 The green arrow highlights the recommended end time-point following a time-loss injury/illness in surveillance studies (first full team training). The yellow line highlights the date of the first match (partial or full duration), used if occurring prior to the first full team training.
Capturing and reporting player exposure
Training and match exposures
In agreement with the IOC consensus statement, we recommend recording exact exposure time for each player (player exposure) rather than estimating the number of training sessions and matches and their match duration during the study period (team exposure), also during multiday competitions. Similarly, we recommend defining training exposure as ‘physical activities performed by the player aimed at maintaining or improving their skills, physical condition and/or performance in football’. Ideally, at least in professional football, all training exposures should be monitored and assessed by objective measures such as wearable tracking and monitoring devices or motion-sensitive technology.
We modified the IOC consensus statement definition of match exposure: ‘organised scheduled match play between opposing teams (not including internal training matches)’. Namely, to include a friendly match between two different clubs but exclude a friendly match within the same team/club.
In line with the IOC consensus statement, however, we recommend tracking illness exposure based on the time players are under surveillance (eg, days or years) instead of using specific training and match exposures.
Training subcategories
Training exposure should be subcategorised into specific categories where possible. We recommend using the categories in the IOC consensus statement with minor modifications, with a prematch warm-up before kick-off reported as a separate training category and a postmatch cool-down as ‘other training’ to differentiate these activities from conventional football training sessions. The categories recommended are: (1) football-specific training, (2) prematch warm-up, (3) strength and conditioning and (4) other training. Importantly, rehabilitation and postrehabilitation transition sessions (included in ‘other training’ in the IOC consensus statement) should be excluded from training exposure because such sessions are part of the duration of the injury or illness.
Reporting measures of occurrence
To align with general epidemiological terminology, we recommend using the term ‘reporting measures of occurrence’ rather than ‘expressing risk’, as the measures in this section do not correspond to risk in probabilistic terms.30 With this general exception, we recommend following the descriptions of rates and proportions and expressing and communicating risk from the IOC consensus statement; for example, by presenting injury incidence as the number of injuries per 1000 hours.31
Burden of health problems
We recommend using the definition of injury burden in football as ‘the number of days lost per 1000 hours’ and illness burden as ‘the number of days lost per 365 player-days’ as in the IOC consensus statement. Both injury and illness burden can also be visualised using a risk matrix (see figure 5 in that statement).
Study population characteristics
As injuries and illnesses may differ between populations, we have added some recommended categories related to age and playing level for use in football epidemiological studies.
Age categorisation
We recommend classifying players as either adults or youths with a clear description of the age cut-off chosen to distinguish adult from youth players in each study. We also agreed that a minimum requirement should be reporting mean age, including both SD and range from the youngest to oldest player. In studies on mixed cohorts, such as female and male players, age data should be reported separately for each cohort, thus allowing the reader or researcher to extract data on, for example, female players only.
Playing level
FIFA defines players participating in organised football as either amateurs or professionals,32 and we agreed to harmonise with this categorisation. A professional is defined as a player who has a written contract with a club and is paid more for his/her footballing activity than the expenses he/she effectively incurs. Players not fulfilling these two criteria are amateurs. The term semi-professional, which represents an interface sometimes seen in the literature, is not clearly defined. Therefore, we do not recommend using this term, nor do we recommend using the term subelite for the same reason. The term elite is often used, especially in women’s football, even if they are amateurs,33 but it is rarely defined sufficiently. Unfortunately, league systems and the corresponding definitions of elite, vary from association to association (country to country) and from confederation to confederation.34 Official league rankings, such as the one from the Union des Associations Europénnes de Football,35 could help better classify the team or the cohort as being elite or not. We agreed that the sample needs to be specified for both international league ranking (where accessible) and the playing division (out of the total number of divisions in the league system). Moreover, we also recommend not using elite in studies on children’s football up to 12 years of age regardless of the setting, as this term has recently been questioned in this age group.34
At the highest club level, many players will have international duties during a study period. It is important to include these data with as many details as possible in order to document the overall load for players and ensure a full injury and illness overview.35 36 Finally, some players play football mainly for fun, fitness and social interaction rather than for competition.37 Although sometimes used interchangeably with amateur players in the literature, these players should be termed recreational players. This cohort includes non-organised football players outside the national league system, such as employee tournaments and ‘weekend warriors’.38
Data collection methods
We recommend following the considerations on data collection described in the IOC consensus statement, including encouraging researchers to use the extension of Strengthening the Reporting of Observational Studies in Epidemiology for Sport Injury and Illness Surveillance (STROBE-SIIS) and the accompanying STROBE-SIIS checklist.13
Validation and implementation
In addition to the IOC consensus statement, we also would like to stress the importance of using a surveillance system evaluated with methodological rigour, that is scientific soundness in terms of planning, data collection, analysis and reporting of results, and published in the scientific literature to reduce error and to improve the quality of health problem surveillance.39 We also recommend including relevant football stakeholders, such as players, coaches and governing bodies in the planning, implementation, evaluation and communication of findings.40 In addition, the identification of implementation principles and having a communication strategy for the preimplementation, implementation and postimplementation phases are recommended. Preimplementation encompasses the development and piloting of the surveillance system, implementation incorporates the definition of roles and responsibilities, and postimplementation refers to the football-specific interpretation and dissemination of outcomes.41 Finally, the provision of adequately skilled and experienced human resources as well as sufficient financial support is required to ensure the appropriate implementation of the programme.42 In line with this, medically trained personnel (rather than technical or coaching staff) should be recruited to record injury and illness data, as it has been shown that the quality of data and research outcomes are of a higher standard.39
Discussion
We provide an updated guideline on definitions, data collection procedures and reporting standards for studies on injuries and illnesses in football with the objective of improving injury and illness management and prevention strategies.
Research implications
This consensus extension should ensure more consistent study designs and the use of recommended nomenclature in future surveillance studies of football injuries and illnesses regardless of setting, thus facilitating comparisons across studies and pooling of data. Nonetheless, we think that a further update will likely be needed within the next decade from this publication because of an expected surge of new literature in the field and scientific developments. Until then, we encourage journal editors and peer reviewers to check that submitted manuscripts harmonise with the generic IOC consensus statement and the current football-specific consensus extension.
Limitations
There are some limitations to this football-specific consensus extension. First, we did not conduct a systematic literature search, including assessing evidence level, methodological quality and risk of bias among cited studies. Second, dissenting opinions have not been fully clarified or discussed within the main body of the manuscript. Importantly, despite the ensuing recommendations having met the predefined ‘threshold’ set for reaching agreement, there were nevertheless differing opinions within the panel (online supplemental table 2).21 Third, there was an under-representation of panel members from low-income countries, implying we may not have included specific context-related challenges. In general, the methodological recommendations can be carried out in low resource settings, as the injury and illness surveillance in its simplest form can be performed using paper and pen only. However, we acknowledge that there may be other practical challenges, which we have not covered in this process and these should be addressed in future updates. Fourth, we did not include a voting statement or a discussion around study preregistration. Study preregistration, not only for clinical trials but also for observational studies, allows editors, peer-reviewers and readers to transparently evaluate if the paper follows an a priori communicated protocol for the data collection procedure and planned analyses.43 We encourage researchers to preregister their injury and illness surveillance studies in the future. Fifth, in addition to adjustments specifically related to football, we also modified some of the general recommendations included in the IOC statement as our recommendation for future injury and illness surveillance studies in football. This includes dividing the body area ‘hip/groin’ to ‘hip’ and ‘groin’ and adding ‘complete and partial tendon avulsions’ to the notes for the pathology type tendon rupture. This means methodology across sports may vary slightly, but, for example, the ‘hip’ and ‘groin’ categories can easily be combined from table 4, if this is required to compare data with other sports. We therefore recommend that the IOC statement is revised at regular intervals, including considerations on fundamental changes proposed in all sport-specific extensions. Sixth, it was beyond the scope to also create guidelines for other variants of football such as futsal, beach soccer or Para football of which there are several categories. These variants and Para football can use some relevant parts of the current extension while their own consensus extensions are being created and published.
Conclusion
This comprehensive football-specific extension of the IOC consensus statement should ensure more consistent study designs, data collection procedures and use of nomenclature in future injury and illness surveillance studies in football, improving injury and illness management and prevention strategies. It should facilitate comparisons across studies and pooling of data.
Acknowledgments
We acknowledge the support of the FIFA Medical Subdivision, especially Mrs Mary Lawless, for administrative tasks. We are also grateful to Mr Steve McClaren, UK, for being the coach’s voice and to Ms Linda Sällström, Finland and Mr Alfred Finnbogason, Iceland, for being the players’ voices. We would also like to thank Dr John Orchard for his thoughts on the influence of the body area separation on the OSIICS.
Footnotes
Twitter: @MarkusWalden, @margo.mountjoy, @Alan_McCall_, @aserner, @andy_massey, @Jltol, @RoaldBahr, @1Michdhoo01, @bittencourt_nfn, @fdellavilla, @GregDupontSport, @drmarkfulcher, @ChristaJVR, @DonnaLu19, @DocThorAndersen
Correction notice: This article has been corrected since it published Online First. The supplementary file has been amended.
Contributors: MW and TEA: Conceptualisation, methodology, investigation, writing—original draft; MM: Conceptualisation, methodology, investigation, project administration, writing—review and editing; AMc and AMa: Conceptualisation, methodology, investigation, writing—review and editing; AS: Methodology, investigation, project administration, resources, data curation, writing - review and editing; JLT, RB, MD'H, NB, FDV, MD, GD, MF, DCJvR and DL: Investigation, writing—review and editing.
Funding: The consensus meeting in Zürich was sponsored by FIFA, including all costs for meeting facilities, travels and accommodations, but there were no daily allowances or other funding specifically for this consensus extension to panel members.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Orchard JW, Newman D, Stretch R, et al. Methods for injury surveillance in international cricket. Br J Sports Med 2005;39:e22. 10.1136/bjsm.2004.012732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Orchard JW, Ranson C, Olivier B, et al. International consensus statement on injury surveillance in cricket: a 2016 update. Br J Sports Med 2016;50:1245–51. 10.1136/bjsports-2016-096125 [DOI] [PubMed] [Google Scholar]
- 3. Fuller CW, Ekstrand J, Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Br J Sports Med 2006;40:193–201. 10.1136/bjsm.2005.025270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fuller CW, Molloy MG, Bagate C, et al. Consensus statement on injury definitions and data collection procedures for studies of injuries in rugby Union. Br J Sports Med 2007;41:328–31. 10.1136/bjsm.2006.033282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. King DA, Gabbett TJ, Gissane C, et al. Epidemiological studies of injuries in rugby league: suggestions for definitions, data collection and reporting methods. J Sci Med Sport 2009;12:12–19. 10.1016/j.jsams.2007.12.001 [DOI] [PubMed] [Google Scholar]
- 6. Pluim BM, Fuller CW, Batt ME, et al. Consensus statement on epidemiological studies of medical conditions in tennis, April 2009. Br J Sports Med 2009;43:893–7. 10.1136/bjsm.2009.064915 [DOI] [PubMed] [Google Scholar]
- 7. Turner M, Fuller CW, Egan D, et al. European consensus on epidemiological studies of injuries in the thoroughbred horse racing industry. Br J Sports Med 2012;46:704–8. 10.1136/bjsports-2011-090312 [DOI] [PubMed] [Google Scholar]
- 8. Timpka T, Alonso J-M, Jacobsson J, et al. Injury and illness definitions and data collection procedures for use in epidemiological studies in athletics (track and field): consensus statement. Br J Sports Med 2014;48:483–90. 10.1136/bjsports-2013-093241 [DOI] [PubMed] [Google Scholar]
- 9. Yamato TP, Saragiotto BT, Lopes AD. A consensus definition of running-related injury in recreational runners: a modified Delphi approach. J Orthop Sports Phys Ther 2015;45:375–80. 10.2519/jospt.2015.5741 [DOI] [PubMed] [Google Scholar]
- 10. Mountjoy M, Junge A, Alonso JM, et al. Consensus statement on the methodology of injury and illness surveillance in FINA (aquatic sports). Br J Sports Med 2016;50:590–6. 10.1136/bjsports-2015-095686 [DOI] [PubMed] [Google Scholar]
- 11. Gijon-Nogueron G, Ortega-Avila AB, Kaldau NC, et al. Data collection procedures and injury definitions in badminton: a consensus statement according to the Delphi approach. Clin J Sport Med 2022;32:e444–50. 10.1097/JSM.0000000000001048 [DOI] [PubMed] [Google Scholar]
- 12. Schwellnus M, Kipps C, Roberts WO, et al. Medical encounters (including injury and illness) at mass community-based endurance sports events: an international consensus statement on definitions and methods of data recording and reporting. Br J Sports Med 2019;53:1048–55. 10.1136/bjsports-2018-100092 [DOI] [PubMed] [Google Scholar]
- 13. Bahr R, Clarsen B, Derman W, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE extension for sport injury and illness surveillance (STROBE-SIIS)). Br J Sports Med 2020;54:372–89. 10.1136/bjsports-2019-101969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Murray A, Junge A, Robinson PG, et al. International consensus statement: methods for recording and reporting of epidemiological data on injuries and illnesses in golf. Br J Sports Med 2020;54:1136–41. 10.1136/bjsports-2020-102380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Verhagen E, Clarsen B, Capel-Davies J, et al. Tennis-specific extension of the International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020. Br J Sports Med 2021;55:9–13. 10.1136/bjsports-2020-102360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Clarsen B, Pluim BM, Moreno-Pérez V, et al. Methods for epidemiological studies in competitive cycling: an extension of the IOC consensus statement on methods for recording and reporting of epidemiological data on injury and illness in sport 2020. Br J Sports Med 2021;55:1262–9. 10.1136/bjsports-2020-103906 [DOI] [PubMed] [Google Scholar]
- 17. Heron N, Sarriegui I, Jones N, et al. International consensus statement on injury and illness reporting in professional road cycling. Phys Sportsmed 2021;49:130–6. 10.1080/00913847.2020.1830692 [DOI] [PubMed] [Google Scholar]
- 18. Derman W, Badenhorst M, Blauwet C, et al. Para sport translation of the IOC consensus on recording and reporting of data for injury and illness in sport. Br J Sports Med 2021;55:1068–76. 10.1136/bjsports-2020-103464 [DOI] [PubMed] [Google Scholar]
- 19. Guyatt GH, Oxman AD, Kunz R, et al. GRADE guidelines: 2. framing the question and deciding on important outcomes. J Clin Epidemiol 2011;64:395–400. 10.1016/j.jclinepi.2010.09.012 [DOI] [PubMed] [Google Scholar]
- 20. Williamson PR, Altman DG, Blazeby JM, et al. Developing core outcome sets for clinical trials: issues to consider. Trials 2012;13:132. 10.1186/1745-6215-13-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Shrier I. Consensus statements that fail to recognise dissent are flawed by design: a narrative review with 10 suggested improvements. Br J Sports Med 2021;55:545–9. 10.1136/bjsports-2020-102545 [DOI] [PubMed] [Google Scholar]
- 22. Blazey P, Crossley KM, Ardern CL, et al. It is time for consensus on ‘consensus statements’. Br J Sports Med 2022;56:306–7. 10.1136/bjsports-2021-104578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. British Medical Journal . BJSM author guidelines for consensus statements. accessed 26/09/2022: BJSM-Author-Guidelines-and-Considerations-for-Consensus-Statements-31-AUG-2021.pdf (bmj.com).
- 24. Aiello F, McCall A, Brown SJ. Development of a standardised system to classify injury inciting circumstances in football: the football injury Inciting circumstances classification system, in review 2022. [DOI] [PMC free article] [PubMed]
- 25. Orchard J, Genovesi F. Orchard Sports Injury and Illness Classification System (OSIICS) version 14 and Italian translation. Br J Sports Med 2022;56:1144–5. 10.1136/bjsports-2022-105828 [DOI] [PubMed] [Google Scholar]
- 26. Orchard JW, Meeuwisse W, Derman W, et al. Sport Medicine Diagnostic Coding System (SMDCS) and the Orchard Sports Injury and Illness Classification System (OSIICS): revised 2020 consensus versions. Br J Sports Med 2020;54:397–401. 10.1136/bjsports-2019-101921 [DOI] [PubMed] [Google Scholar]
- 27. Ardern C, Glasgow P, Schneiders A, et al. Consensus statement on return to sport from the first world Congress in sports physical therapy, Bern. Br J Sports Med 2016;2016:853–64. [DOI] [PubMed] [Google Scholar]
- 28. Ardern C, Pruna R. Return to play in football: a dynamic model. In Muscle Injury Guide: Prevention of and Return to Play from Muscle Injuries. In: Pruna R, Andersen TE, Clarsen B, et al., eds. Barca Innovation Hub, 2018: 80–1. [Google Scholar]
- 29. Buckthorpe M, Frizziero A, Roi GS. Update on functional recovery process for the injured athlete: return to sport continuum redefined. Br J Sports Med 2019;53:265–7. 10.1136/bjsports-2018-099341 [DOI] [PubMed] [Google Scholar]
- 30. Impellizzeri FM, McCall A, Meyer T, et al. Measures of (injury and illness) occurrence: a primer on epidemiological concepts and terminology for authors. Sci Med Football 2022;6:137–40. 10.1080/24733938.2022.2062897 [DOI] [PubMed] [Google Scholar]
- 31. van Mechelen W, Hlobil H, Kemper HCG. . Incidence, severity, aetiology and prevention of sports injuries. Sports Med 1992;14:82–99. 10.2165/00007256-199214020-00002 [DOI] [PubMed] [Google Scholar]
- 32. Fédération Internationale de Football Association . Regulations on the status and transfer of players. January 2021 edition. accessed 14/02/2022: g1ohngu7qdbxyo7kc38e-pdf.pdf (fifa.com).
- 33. Horan D, Blake C, Hägglund M, et al. Injuries in elite‐level women’s football—a two‐year prospective study in the Irish Women’s National League. Scand J Med Sci Sports 2022;32:177–90. 10.1111/sms.14062 [DOI] [PubMed] [Google Scholar]
- 34. McAuley ABT, Baker J, Kelly AL. Defining “elite” status in sport: from chaos to clarity. Ger J Exerc Sport Res 2022;52:193–7. 10.1007/s12662-021-00737-3 [DOI] [Google Scholar]
- 35. Union des Associations Europénnes de Football . Association Club coefficients. accessed 14/02/2022: country coefficients | UEFA coefficients | UEFA.com.
- 36. Waldén M, Hägglund M, Ekstrand J. UEFA Champions League study: a prospective study of injuries in professional football during the 2001-2002 season. Br J Sports Med 2005;39:542–6. 10.1136/bjsm.2004.014571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Krustrup P, Aagaard P, Nybo L, et al. Recreational football as a health promoting activity: a topical review. Scand J Med Sci Sports 2010;20:1–13. 10.1111/j.1600-0838.2010.01108.x [DOI] [PubMed] [Google Scholar]
- 38. Dönmez G, Korkusuz F, Özçakar L, et al. Injuries among recreational football players: results of a prospective cohort study. Clin J Sport Med 2018;28:249–54. 10.1097/JSM.0000000000000425 [DOI] [PubMed] [Google Scholar]
- 39. Ekegren CL, Gabbe BJ, Finch CF. Sports injury surveillance systems: a review of methods and data quality. Sports Med 2016;46:49–65. 10.1007/s40279-015-0410-z [DOI] [PubMed] [Google Scholar]
- 40. Harvey G, Kitson A. PARIHS revisited: from heuristic to integrated framework for the successful implementation of knowledge into practice. Implement Sci 2015;11:33. 10.1186/s13012-016-0398-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Moullin JC, Sabater-Hernández D, Fernandez-Llimos F, et al. A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. Health Res Policy Sys 2015;13:16. 10.1186/s12961-015-0005-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Finch CF, Staines C. Guidance for sports injury surveillance: the 20-year influence of the Australian sports injury data dictionary. Inj Prev 2018;24:372–80. 10.1136/injuryprev-2017-042580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Williams RJ, Tse T, Harlan WR, et al. Registration of observational studies: is it time? Can Med Assoc J 2010;182:43:1638–42. 10.1503/cmaj.092252 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjsports-2022-106405supp001.pdf (242.4KB, pdf)