Abstract
BACKGROUND
Observational studies investigating associations between cannabis use and blood pressure (BP)/hypertension are inconsistent.
METHODS
Cross-sectional data from the National Health and Nutrition Examination Survey (NHANES) were analyzed for five 2-year cycles between 2009 and 2018 representing 9,783 middle-aged adults (35–59 years). Hypertension was defined as systolic BP (SBP) ≥130, diastolic BP (DBP) ≥80, or a BP medication. Sample-weighted multivariable logistic regression models were used to assess associations between cannabis use and BP and hypertension.
RESULTS
One quarter of respondents (n = 2,228) reported a history of monthly cannabis use for more than 1 year, which was consistent over the study period (P for trend = 0.75). Approximately 48% (n = 4,831) met the definition of hypertension. While a significant positive trend was seen over time for mean SBP and DBP (P = <0.01 for both), no significant trend was seen in prevalent hypertension (P for trend = 0.23). In adjusted models, compared with never use, a history of monthly cannabis use for more than 1 year was not associated with increased BP (mean SBP: 124.5 mm Hg (95% confidence interval [CI], 122.4–126.6) vs. 122.6 (95% CI, 120.9–124.2); DBP: 74.7 mm Hg (95% CI, 73.1–76.2) vs. 74.1 (95% CI, 72.8–75.4)), or prevalent hypertension (odds ratio = 0.88 (95% CI, 0.62–1.24)). Results from analyses of duration of monthly use, and recency and frequency of recent use were similar.
CONCLUSIONS
A history of monthly cannabis use for more than 1 year was not independently associated with either increased BP or prevalent hypertension in a nationally representative sample of middle-aged US adults.
Keywords: blood pressure, cannabis, cardiovascular disease, hypertension, marijuana
Cardiovascular effects of Cannabis sativa L. (cannabis or marijuana) are mediated by cannabinoid receptors (i.e., CB1R and CB2R) in the central nervous and cardiovascular systems. Activation of CB1R has been linked to mechanisms of cardiometabolic disease, while activation of CB2R has shown anti-inflammatory and anti-oxidant effects in the cardiovascular system.1 Acute effects include dose-dependent increases in heart rate and cardiac contractility as well as centrally—and peripherally—mediated changes in vascular resistance and blood pressure (BP), including orthostatic hypotension.2 Notable interindividual variability is observed. Frequent use may lead to tolerance to these effects after a few weeks.3
Epidemiologic studies that explore the relationship between cannabis use and BP and/or hypertension have reported conflicting findings, depending on the study design, population, and measure of cannabis exposure. Most report a lack of association. However, some cross-sectional studies, including those using data from the National Health and Nutrition Examination Survey (NHANES), have reported significant positive associations between recent (past month) and frequent, recent cannabis use and systolic BP (SBP),4 as well as heavy use (>20 days in the past month) and elevated BP,5 but not diastolic BP (DBP) or prevalent hypertension.6 In contrast, a large (n = 91,161) cross-sectional study noted lower SBP, DBP, and pulse pressure among heavy lifetime cannabis users (more than 100 times in a lifetime).7 Longitudinal studies have found no association with changes in BP8 or incident hypertension.9
Prior studies have focused on recency (past month use) and frequency of recent use (days used in the past month), but not on the duration or timing of use beyond the past month. In the present analysis of NHANES data, we address this gap by assessing the relationship between both recent and regular cannabis use and BP and prevalent hypertension in a nationally representative sample of US middle-aged adults.
METHODS
Data sources and measurement
The NHANES is a series of nationally representative, cross-sectional examinations designed to monitor the health of the US population. Participants were selected from the noninstitutionalized, civilian population using a complex, stratified, multistage probability-cluster sampling design for in-home interviews and visits to a mobile examination center.10
Analytic sample
The analytic sample was limited to middle-aged adults (35–59 years) who participated in both the interview and mobile NHANES examinations during five 2-year cycles between 2009 and 2018. This included 9,783 (unweighted) [92,033,212 (weighted)] respondents who answered questions about their cannabis use using the Drug Use Questionnaire (DUQ) (administered to respondents up to 59 years of age), their use of antihypertensive medication using the Prescription Medications Questionnaire (PMQ) and had their BP measured by trained examiners at the mobile examination center. Respondents with relevant missing data from both the DUQ and the PMQ were excluded.
Independent variables
Cannabis use
Cannabis use was defined using questions from the DUQ11 and classified as “never use,” “no history of monthly use,” “history of monthly use” (i.e., a history of monthly use for more than 1 year), “recent use by those with a history of monthly use,” and “non-recent use by those with a history of monthly use” (Figure 1).
Figure 1.
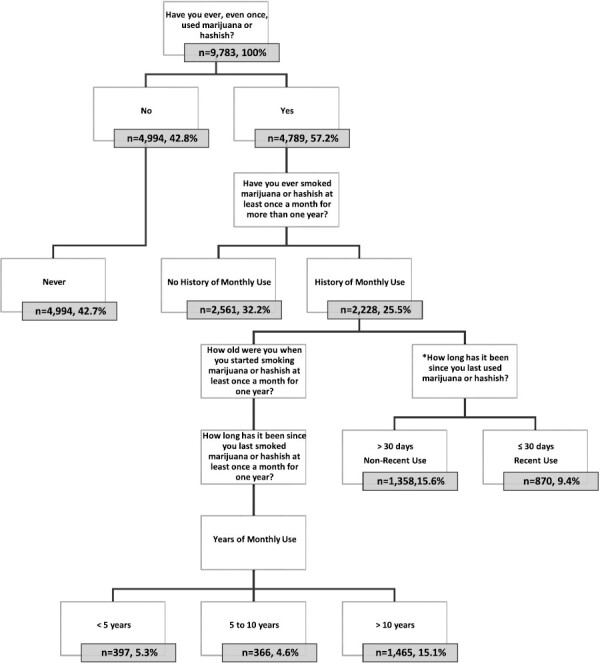
Flowchart of the analytic sample (unweighted). Notes: Years of monthly use was calculated by subtracting the number of years since using it monthly for a year from a respondent’s current age, and then subtracting the age at which they reported started using it monthly for a year. *This question was administered to all respondents reporting ever using marijuana or hashish. Only responses from those with a history of monthly use for more than a year were analyzed (except for the sensitivity analyses).
In sensitivity analyses, recent use was further categorized. Those reporting <10 days of use in the past month were categorized as “Light, recent” users, 10–20 days as “Moderate, recent” users, and >20 days as “Heavy, recent” users, as described elsewhere.12
Covariates
Covariates were obtained through self-report except for height and weight (used for body mass index [BMI]), which were measured by trained examiners. Covariates included sociodemographic factors such as age, sex, race/ethnicity, education, and household income. Age was self-reported in years. Sex was self-reported as male or female. Race/ethnicity was categorized as non-Hispanic White, non-Hispanic Black, Asian and other, or Hispanic (inclusive of Mexican American and Other Hispanic).
Health-related covariates included physical activity, BMI, cigarette smoking status, and alcohol use. Comprehensive information on covariates is available in Supplementary Methods and Results online.
Biomarkers (total cholesterol (mg/dl), HDL cholesterol (mg/dl), fasting blood glucose (mg/d), and HbA1c (%)) were objectively measured by American Society of Clinical Pathologists-certified medical technologists or medical laboratory technicians at the University of Minnesota, Minneapolis, MN. Dyslipidemia was defined as a total cholesterol to HDL ratio >5.0 or use of lipid-lowering medication. Prediabetes was defined as fasting blood glucose ≥100 or A1c ≥5.7%. Diabetes was defined as fasting blood glucose ≥126, or HbA1c >6.4% or use of antidiabetic medication.
Outcome
BP and hypertension
Resting BP was measured according to a standardized protocol in a clinical setting by examiners trained on American Heart Association guidelines for collecting BP.13 After a 5-minute resting period in a seated position, 3 consecutive BP readings were obtained. A fourth reading was obtained if one of the initial 3 measurements was interrupted or incomplete. Three complete SBP and DBP readings were averaged to an individual for mean SBP and mean DBP, respectively. Hypertension was defined as SBP ≥130 or diastolic ≥80 (per the 2017 ACC/AHA Guideline for High Blood Pressure in Adults)14 or use of antihypertensive medication. Complete BP data were available for 94% of respondents (n = 9,227).
Statistical methods
NHANES data are weighted using a complex process so that the survey population provides a representation of the population of the United States for each 2-year survey cycle. Per the guidelines provided on the NHANES website, weights were used for the smallest subsample used in this study.15 The analytic sample combines data from multiple survey cycles; the weights were adjusted per the instructions provided by NHANES.
Descriptive statistics were used to characterize the sample: weighted means and 95% confidence intervals (CIs) for continuous variables and weighted percentages and 95% CIs for nominal variables. Data management and statistical analyses were performed using SAS On-Demand for Academics (Copyright © 2014 SAS Institute, Cary, NC).
The primary analysis tested the association between a history of monthly cannabis use for more than 1 year and BP and prevalent hypertension. Secondary analyses included duration of monthly use (<5, 5–10, and >10 years) and recency of use (past month use) among those with a history of monthly use. Weighted multivariable logistic regression models were used to estimate adjusted mean differences and 95% CIs for BP, and adjusted odds ratios (ORs) and 95% CIs for hypertension, controlling for potential confounders.
Variables considered potential confounders in the multivariable analyses were sociodemographic variables such as age, gender, race/ethnicity, education level, and household income (model 1); behavioral risk factors such as cigarette, alcohol use, and physical activity (model 2); and BMI and Cardiovascular disease (CVD) risk factors, including total cholesterol to High-density lipoprotein (HDL) cholesterol ratio, HbA1c, antilipidemic and antidiabetic medications (model 3). Collinearity between independent variables was assessed in the final multivariate adjusted model by using Variance Inflation Factor and Tolerance. A P value of <0.05 was considered significant for all analyses.
Interaction
Multiplicative, first-order interactions were constructed in the multivariable adjusted regression models for variables designated a priori: age, sex, race/ethnicity, cigarette smoking status, and recency and frequency of cannabis use. Interaction terms were considered significant in the final multivariable adjusted model if P < 0.10.
Sensitivity analyses
Sensitivity analyses included the assessment of BP and prevalent hypertension across additional measures of cannabis use (recency and frequency).
RESULTS
The sample consisted of 9,783 respondents with 25% (n = 2,228) reporting a history of monthly cannabis use. Slightly less than half of all respondents (47.6%) met the definition of hypertension (Table 1). After adjusting for age and sex, hypertension prevalence was greater among male respondents of non-Hispanic Black, Asian and Other races, with less education, lower household income, more cigarette pack-years, and a higher BMI.
Table 1.
Age and sex adjusted characteristics of middle-aged adults by hypertension status, 2009–2018 (n = 9,783)
| Hypertension | No hypertension | |
|---|---|---|
| Unweighted frequency | n = 4,831 | n = 4,952 |
| Weighted percentage | 47.6% | 52.4% |
| Cannabis use, % (95% CI) | ||
| Never | 43.4 (41.0–45.7) | 42.3 (39.8–44.8) |
| No history of monthly use | 31.4 (29.2–33.6) | 33.0 (30.6–35.4) |
| History of monthly use | 25.2 (23.2–27.2) | 24.7 (22.7–26.8) |
| <5 y of monthly use | 5.3 (4.5–6.2) | 5.2 (4.2–6.2) |
| 5–10 y of monthly use | 4.5 (3.7–5.4) | 4.7 (3.8–5.6) |
| >10 y of monthly use | 15.4 (13.6–17.1) | 14.8 (13.0–16.7) |
| Sociodemographics, % (95% CI) | ||
| Sex | ||
| Male | 55.2 (53.1–57.3) | 44.1 (42.4–45.8) |
| Female | 44.8 (42.7–46.9) | 55.9 (54.2–57.6) |
| Age (YOA), mean (SE) | 48.9 (0.2) | 45.7 (0.2) |
| Race/ethnicity, % (95% CI) | ||
| Non-Hispanic White | 62.4 (58.5–66.3) | 67.8 (64.6–71.0) |
| Non-Hispanic Black, Asian and other | 21.9 (19.2–24.6) | 14.7 (13.0–16.4) |
| Hispanic (Inc. Mex. American) | 15.7 (13.3–18.1) | 17.5 (14.9–20.1) |
| Education % (95% CI) | ||
| High school or less | 38.4 (35.8–40.9) | 33.5 (30.4–36.5) |
| Some college | 33.8 (31.8–35.8) | 28.5 (26.6–30.4) |
| College graduate or above | 27.8 (25.2–30.5) | 38.0 (34.7–41.3) |
| Household income, annual $ % (95% CI) | ||
| $0–44,999 | 35.6 (33.0–38.2) | 28.9 (26.2–31.6) |
| $45,000–99,999 | 35.4 (32.9–37.9) | 33.6 (31.1–36.1) |
| ≥$100,000 | 29.0 (25.7–32.3) | 37.5 (34.1–41.0) |
| Lifestyle, behavioral, % (95% CI) | ||
| Alcohol use, % | ||
| No d/wk | 16.1 (14.6–17.6) | 14.7 (13.1–16.2) |
| ≤2 d/wk | 63.2 (61.0–65.4) | 65.2 (63.2–67.1) |
| >2 d/wk | 20.7 (18.4–22.9) | 20.2 (18.4–21.9) |
| Cigarette smoking pack-years, mean (SE) | 7.3 (0.3) | 6.3 (0.3) |
| Cigarette smoking status, % (95% CI) | ||
| Never | 22.1 (20.7–23.6) | 21.3 (19.4–23.1) |
| Past | 24.2 (22.1–26.4) | 21.8 (20.0–23.7) |
| Current | 53.6 (51.5–55.7) | 56.9 (54.6–59.2) |
| Physical activity (min/wk), mean (SE) | 336.9 (10.0) | 341.2 (9.1) |
| BMI, kg/m2, mean (SE) | 31.9 (0.2) | 28.0 (0.2) |
| Weight | ||
| Under/normal: BMI <25 | 16.6 (15.3–17.9) | 32.1 (30.1–34.2) |
| Overweight: BMI 25 to <30 | 29.5 (27.4–31.7) | 37.5 (35.5–39.4) |
| Obese: BMI ≥30 | 53.5 (51.3–55.7) | 29.9 (27.8–32.0) |
| Cardiometabolic medical history, % (95% CI) | ||
| Dyslipidemia | 39.4 (37.2–41.5) | 25.7 (24.0–27.3) |
| Antilipidemic medication | 19.6 (17.7–21.4) | 8.4 (7.2–9.7) |
| Diabetes or prediabetes | 52.8 (50.4–55.2) | 38.6 (36.4–40.9) |
| Antidiabetic medication | 12.3 (11.0–13.5) | 3.6 (2.9–4.2) |
Notes: Subgroups are represented by weighted percentages and 95% confidence intervals or weighted means with 95% confidence intervals. All comparisons are adjusted for age and sex, except for age, which is adjusted for sex, and sex, which is adjusted for age. Physical activity includes the following domains: Walk/bike for transportation, vigorous recreational, moderate recreational. Cannabis use variables are all standard NHANES variables, other than Years of Monthly Use, which is a calculation. Abbreviations: BMI, body mass index; CI, confidence interval; NHANES, National Health and Nutrition Examination Survey.
Slightly more than 40% of those with a history of monthly cannabis use reported current cigarette smoking. The percentage was higher (52.7%) among recent users with a history of monthly use. Overall, the prevalence of hypertension was only slightly higher among current cigarette smokers when compared with never cigarette smokers (48.3% vs. 45.3%).
Age-adjusted trends in cannabis use, BP, and hypertension
After adjusting for age and sex, the percentage of respondents reporting a history of monthly cannabis use fluctuated around 25% per 2-year cycle without a significant trend over time (P for trend = 0.75) (Table 2). A significant upward trend was seen in recent use, however, from 9.1% (95% CI, 7.1–11.1) in 2009–2010 to 13.9% (95% CI, 11.3–16.6) in 2017–2018 (P for trend <0.01), and in recent use by those with a history of monthly use, from 7.7% (95% CI, 5.8–9.6) in 2009–2010 to 11.7% (95% CI, 8.9–14.5) in 2017–2018 (P for trend = 0.02). A significant positive trend was also seen in mean SBP and DBP from 119.6 mm Hg (95% CI, 118.7–120.6) and 73.1 mm Hg (95% CI, 71.8–74.3), respectively, in 2009–2010 to 122.5 mm Hg (95% CI, 121.3–123.8) and 76.6 mm Hg (95% CI, 75.5–77.7) in 2017–2018 (P for trend = <0.01 for both). A nonsignificant upward trend was seen in hypertension prevalence (45.7% (95% CI, 41.1–50.3) in 2009–2010 to 48.9% (95% CI, 45.0–52.8) in 2017–2018; P for trend = 0.23).
Table 2.
Age and sex adjusted trends in characteristics of middle-aged adults, 2009–2018 (n = 9,783)
| 2009–2010 | 2011–2012 | 2013–2014 | 2015–2016 | 2017–2018 | P for trend | |
|---|---|---|---|---|---|---|
| Unweighted sample number | 2,141 | 1,795 | 2,057 | 1,947 | 1,843 | — |
| SBP, mean (SE) | 119.6 (118.7–120.6) | 120.8 (119.4–122.2) | 120.4 (119.3–121.5) | 122.6 (121.4–123.7) | 122.5 (121.3–123.8) | <0.0001 |
| DBP, mean (SE) | 73.1 (71.8–74.3) | 74.5 (73.8–75.2) | 73.2 (72.6–73.8) | 74.2 (73.1–75.2) | 76.6 (75.5–77.7) | 0.0004 |
| Hypertension, % (95% CI) | 45.7 (41.1–50.3) | 48.1 (45.7–50.5) | 43.6 (40.5–46.6) | 49.3 (46.4–52.2) | 48.9 (45.0–52.8) | 0.23 |
| Cannabis use, % (95% CI) | ||||||
| Never | 43.8 (38.4–49.2) | 41.1 (35.5–46.7) | 41.7 (38.1–45.4) | 44.3 (39.6–49.1) | 43.1 (39.6–46.5) | 0.80 |
| No history of monthly use | 31.9 (28.0–35.7) | 32.6 (27.5–37.6) | 33.8 (30.6–37.0) | 29.8 (26.7–32.9) | 33.2 (28.3–38.0) | 0.98 |
| History of monthly use | 24.4 (21.4–27.3) | 26.3 (22.4–30.3) | 24.5 (20.6–28.3) | 25.8 (22.2–29.5) | 23.8 (20.2–27.4) | 0.75 |
| <5 y of monthly use | 6.3 (5.1–7.5) | 5.3 (3.9–6.6) | 5.4 (3.8–7.0) | 4.8 (3.8–5.8) | 4.5 (2.6–6.4) | 0.10 |
| 5–10 y of monthly use | 4.8 (3.6–6.0) | 5.0 (3.4–6.6) | 3.8 (2.8–4.8) | 5.8 (3.9–7.7) | 3.8 (2.2–5.4) | 0.62 |
| >10 y of monthly use | 16.1 (13.3–18.9) | 15.3 (11.4–19.2) | 15.2 (12.1–18.3) | 15.5 (12.5–18.5) | 13.3 (10.8–15.7) | 0.42 |
| Sociodemographics, % (95% CI) | ||||||
| Sex—female | 49.4 (47.5–51.4) | 49.9 (45.6–54.3) | 51.3 (49.3–53.4) | 51.4 (49.2–53.6) | 51.2 (48.5–53.9) | 0.2410 |
| Age (YOA), mean (SE) | 46.9 (46.6–47.3) | 47.4 (46.8–48.0) | 47.1 (46.7–47.6) | 47.2 (46.7–47.8) | 47.6 (47.0–48.2) | 0.1698 |
| Race/ethnicity | ||||||
| Non-Hispanic White | 69.7 (62.6–76.7) | 67.6 (59.6–75.6) | 65.6 (58.9–72.4) | 64.2 (55.4–73.1) | 59.6 (53.7–65.6) | 0.0355 |
| Non-Hispanic Black, Asian and other | 10.7 (8.8–12.7) | 18.5 (12.5–24.5) | 18.7 (15.1–22.3) | 19.7 (13.9–25.5) | 22.4 (17.7–27.2) | 0.0004 |
| Hispanic (Inc. Mex. American) | 19.6 (13.0–26.3) | 13.9 (9.3–18.5) | 15.7 (10.4–20.9) | 16.1 (10.5–21.7) | 17.9 (13.7–22.2) | 0.9065 |
| Education | ||||||
| High school or less | 39.4 (36.1–42.6) | 36.4 (30.3–42.5) | 35.0 (29.0–41.0) | 33.4 (27.3–39.4) | 34.9 (30.3–39.5) | 0.1046 |
| Some college | 28.6 (26.6–30.5) | 30.1 (27.1–33.0) | 31.0 (28.1–33.9) | 32.9 (29.4–36.3) | 32.3 (29.0–35.5) | 0.0256 |
| College graduate or above | 31.9 (28.5–35.3) | 33.5 (27.7–39.3) | 34.0 (27.9–0.40.0) | 33.8 (26.5–41.0) | 32.8 (27.1–38.6) | 0.8098 |
| Household income, annual $ | ||||||
| $0–44,999 | 33.1 (29.3–36.8) | 36.3 (30.4–42.2) | 33.1 (25.9–40.2) | 27.8 (23.0–32.6) | 30.4 (27.0–33.8) | 0.0367 |
| $45,000–99,999 | 37.9 (33.4–42.4) | 33.7 (28.6–38.8) | 32.4 (29.5–35.4) | 35.9 (31.9–39.9) | 32.3 (27.8–36.8) | 0.2258 |
| ≥$100,000 | 29.1 (25.4–32.8) | 30.0 (22.1–38.0) | 34.5 (27.3–41.7) | 36.3 (28.8–43.9) | 37.3 (31.4–43.2) | 0.0129 |
| Lifestyle, behavioral, % (95% CI) | ||||||
| Alcohol use | ||||||
| No d/wk | 16.0 (13.7–18.3) | 15.8 (12.3–19.4) | 13.9 (11.1–16.6) | 15.1 (13.6–16.6) | 15.9 (13.2–18.6) | 0.8545 |
| ≤2 d/wk | 61.3 (57.7–64.9) | 59.8 (56.4–63.1) | 65.6 (61.9–69.2) | 64.3 (60.4–68.2) | 69.8 (66.8–72.8) | 0.0001 |
| >2 d/wk | 22.7 (20.1–25.4) | 24.4 (19.2–29.7) | 20.6 (17.2–24.0) | 20.6 (16.6–24.7) | 14.3 (12.0–16.6) | <0.0001 |
| Cigarette smoking status | ||||||
| Never | 21.4 (19.5–23.3) | 23.8 (20.3–27.2) | 21.8 (18.6–25.0) | 21.2 (18.1–24.4) | 20.3 (17.1–23.6) | 0.2817 |
| Past | 23.5 (19.9–27.0) | 22.9 (19.5–26.3) | 21.7 (19.0–24.4) | 24.1 (21.2–27.0) | 22.6 (19.5–25.7) | 0.9262 |
| Current | 55.1 (51.4–58.9) | 53.3 (50.1–56.5) | 56.5 (52.3–60.6) | 54.6 (51.1–58.2) | 57.1 (52.4–61.7) | 0.4173 |
| Cigarette smoking pack-years, mean (SE) | 7.2 (6.4–8.0) | 7.0 (6.1–7.9) | 6.7 (5.5–7.8) | 7. 5 (6.5–8.5) | 5.4 (4.0–6.8) | 0.0680 |
| Physical activity (min/wk), mean (SE) | 344.4 (308.7–380.2) | 365.1 (327.4–402.8) | 336.7 (308.3–365.1) | 333.2 (308.3–358.1) | 316.4 (283.7–349.1) | 0.1085 |
| BMI, kg/m2, mean (SE) | 29.2 (28.9–29.5) | 29.4 (28.9–30.0) | 29.8 (29.12–30.5) | 30.0 (29.3–30.8) | 30.5 (30.0–31.0) | 0.0001 |
| Weight | ||||||
| Under/normal: BMI <25 | 26.7 (23.5–29.9) | 25.5 (22.3–28.6) | 24.7 (22.3–27.1) | 24.6 (20.8–28.3) | 22.7 (19.8–25.7) | 0.0820 |
| Overweight: BMI 25 to <30 | 35.3 (32.3–38.4) | 35.7 (32.2–39.2) | 33.4 (30.2–36.6) | 32.2 (28.9–35.4) | 32.1 (28.9–35.3) | 0.0500 |
| Obese: BMI ≥30 | 37.6 (35.5–39.6) | 38.4 (35.2–41.6) | 41.2 (37.1–45.3) | 42.9 (37.5–48.2) | 44.7 (41.5–47.9) | 0.0003 |
| Cardiometabolic medical history, % (95% CI) | ||||||
| Dyslipidemia | 34.1 (32.6–35.7) | 33.7 (30.6–36.8) | 33.9 (31.1–36.7) | 31.9 (29.0–34.9) | 27.3 (24.7–29.8) | <0.0001 |
| Antilipidemic medication | 13.7 (12.0–15.4) | 14.2 (11.4–17.0) | 16.0 (13.1–19.0) | 12.5 (9.8–15.3) | 12.0 (9.4–14.5) | 0.1563 |
| Diabetes or prediabetes | 44.0 (41.6–46.3) | 43.8 (39.8–47.8) | 39.2 (35.3–43.1) | 47.8 (44.0–51.6) | 51.6 (47.6–55.5) | 0.0004 |
| Antidiabetic medication | 5.6 (4.2–7.0) | 7.0 (5.4–8.7) | 8.6 (6.7–10.4) | 7.8 (6.3–9.3) | 9.1 (6.9–11.4) | 0.0097 |
Notes: Subgroups by year are represented by weighted percentages and 95% confidence intervals or weighted means with 95% confidence intervals. All comparisons are adjusted for age and sex, except for age, which is adjusted for sex, and sex, which is adjusted for age. P values for tests of trends are derived from multiple linear regression models using dummy variables for each level of categorical variable. Physical activity includes the following domains: Walk/bike for transportation, vigorous recreational, moderate recreational. Cannabis use variables are all standard NHANES variables, other than Years of Monthly Use, which was calculated. Abbreviations: BMI, body mass index; CI, confidence interval; DBP, diastolic blood pressure; NHANES, National Health and Nutrition Examination Survey; SBP, systolic blood pressure.
*Designates P < 0.05.
No linear trends were seen in mean SBP and DBP (P for trend = 0.42 and 0.08, respectively) or hypertension prevalence (P for trend = 0.87) across cannabis use categories.
Cannabis use
Almost 44% of those who reported ever using cannabis also reported a history of monthly use. Of these, approximately 38% reported recent use. Recent use, overall, was reported by 11.1% of the total sample and 19.3% of those reporting ever using cannabis. Approximately 62% of monthly use occurred in the past, of which nearly 46% occurred more than 10 years ago (Table 3).
Table 3.
Cannabis use characteristics of respondents with a history of monthly use for more than 1 year, 2009–2018 (n = 2,228, 25.0%)
| Cannabis exposure | History of monthly use | ||
|---|---|---|---|
| All use | Recent use | Non-recent use | |
| (n = 2,228, 25.0%) | (n = 870, 37.7%) | (n = 1,358, 62.3%) | |
| Age started monthly use, mean (SE) | 18.8 (0.2) | 20.5 (0.4) | 17.7 (0.2) |
| Days of use, past month, mean (SE) | 15.3 (0.6) | 15.3 (0.6) | 0.0 (0.0) |
| Years of monthly use, mean (SE) | 16.5 (0.4) | 23.9 (0.6) | 12.0 (0.3) |
| Years of monthly use, n (%) | |||
| <5 y | 397 (21.0) | 58 (7.5) | 339 (29.2) |
| 5–10 y | 366 (18.5) | 47 (7.1) | 319 (25.4) |
| >10 y | 1,465 (60.5) | 765 (85.3) | 700 (45.5) |
| Years since monthly use, n (%) | |||
| <5 y | 1,034 (42.2) | 766 (85.5) | 268 (16.0) |
| 5–10 y | 253 (9.8) | 39 (4.7) | 214 (12.9) |
| >10 y | 941 (48.0) | 65 (9.8) | 876 (71.1) |
Notes: Subgroups are represented by unweighted frequencies and weighted percentages or weighted means/medians and standard errors. Cannabis use variables are all standard NHANES variables, other than years of monthly use, which is a calculation. Abbreviation: NHANES, National Health and Nutrition Examination Survey.
On average, those with a history of monthly use reported 16.5 years of monthly use. Recent users with a history of monthly use reported almost 24 years of monthly use and over 15 days of use in the past month. Approximately 85% of all recent users reported a history of monthly use. Those without a history of monthly use reported 3 days of use in the past month.
Cannabis use, BP, and hypertension
Adjusted mean BP and adjusted ORs for hypertension are reported in Table 4.
Table 4.
Adjusted mean blood pressure and adjusted odds ratios for hypertension by cannabis use status, 2009–2018
| Systolic BP (mm Hg) |
Diastolic BP (mm Hg) |
Hypertension 130/80 mm Hg |
|
|---|---|---|---|
| Mean (95% CI) | OR (95% CI) | ||
| Unadjusted | |||
| Never | 121.4 (120.6–122.2) | 74.5 (73.9–75.1) | 1.00 Reference |
| History of monthly use | |||
| No | 120.1 (119.2–120.9) | 73.9 (73.2–74.6) | 0.97 (0.84–1.11) |
| Yes | 123.0 (122.1–123.9)* | 74.6 (73.9–75.4) | 1.15 (1.01–1.31)* |
| Duration of monthly use | |||
| <5 y | 121.0 (119.3–122.7) | 74.7 (73.5–75.9) | 1.09 (0.84–1.40) |
| 5–10 y | 120.9 (119.2–122.5) | 73.0 (71.6–74.5) | 1.02 (0.79–1.33) |
| >10 y | 124.4 (123.2–125.6)* | 75.1 (74.2–76.0) | 1.22 (1.03–1.45)* |
| History of monthly use | |||
| Non-recent use | 122.9 (121.7–124.1) | 74.7 (73.8–75.6) | 1.09 (0.89–1.34) |
| Recent use | 123.2 (121.8–124.7) | 74.5 (73.4–75.7) | 1.19 (1.03–1.38)* |
| Model 1 (M1): Adjusted for sociodemographic variables | |||
| Never | 121.9 (121.2–122.7) | 74.7 (74.1–75.3) | 1.00 Reference |
| History of monthly use | 121.5 (120.7–122.3) | 74.3 (73.6–75.0) | 0.97 (0.84–1.10) |
| No | |||
| Yes | 122.4 (121.5–123.2) | 74.0 (73.2–74.8) | 0.92 (0.79–1.07) |
| Duration of monthly use | |||
| <5 y | 122.1 (120.4–123.9) | 74.7 (73.4–76.0) | 1.04 (0.79–1.39) |
| 5–10 y | 121.3 (119.6–123.0) | 72.8 (71.3–74.3) | 0.93 (0.70–1.23) |
| >10 y | 122.8 (121.6–123.9) | 74.1 (73.1–75.2) | 0.88 (0.73–1.06) |
| History of monthly use | |||
| Non-recent use | 122.1 (121.0–123.3) | 74.1 (73.2–75.0) | 0.91 (0.73–1.13) |
| Recent use | 122.7 (121.3–124.2) | 73.9 (72.5–75.2) | 0.93 (0.79–1.10) |
| Model 2 (M2): Adjusted for cigarette and alcohol use and physical activity | |||
| Never | 121.3 (120.4–122.2) | 74.1 (73.5–74.8) | 1.00 Reference |
| History of monthly use | |||
| No | 121.1 (120.0–122.3) | 74.4 (73.5–75.2) | 0.98 (0.82–1.17) |
| Yes | 123.2 (122.0–124.3)* | 74.9 (73.9–75.8) | 1.04 (0.85–1.27) |
| Duration of monthly use | |||
| <5 y | 122.9 (120.5–125.3) | 76.0 (74.5–77.4) | 1.14 (0.76–1.70) |
| 5–10 y | 122.7 (120.2–125.3) | 74.7 (72.5–76.8) | 1.18 (0.78–1.79) |
| >10 y | 123.4 (121.9–124.9) | 74.5 (73.1–75.9) | 0.96 (0.76–1.22) |
| History of monthly use | |||
| Non-recent use | 123.3 (121.7–124.9) | 75.0 (73.9–76.0) | 1.12 (0.83–1.51)) |
| Recent use | 123.0 (121.1–124.8) | 74.6 (72.7–76.6) | 1.00 (0.80–1.25) |
| Model 3 (M3): Adjusted for CVD risk factors | |||
| Never | 122.6 (120.9–124.2) | 74.1 (72.8–75.4) | 1.00 Reference |
| History of monthly use | |||
| No | 122.4 (120.7–124.0) | 74.2 (72.8–75.5) | 0.82 (0.62–1.08) |
| Yes | 124.5 (122.4–126.6) | 74.7 (73.1–76.2) | 0.91 (0.66–1.24) |
| Duration of monthly use | |||
| <5 y | 123.6 (120.3–127.0) | 75.9 (73.7–78.0) | 0.90 (0.54–1.49) |
| 5–10 y | 124.3 (121.1–127.4) | 74.4 (71.3–77.4) | 0.91 (0.49–1.70) |
| >10 y | 125.0 (122.3–127.7) | 74.2 (72.4–76.0) | 0.91 (0.62–1.33) |
| History of monthly use | |||
| Non-recent use | 124.3 (121.8–126.9) | 74.8 (73.1–76.5) | 1.03 (0.64–1.67) |
| Recent use | 124.9 (122.3–127.5) | 74.4 (72.2–76.7) | 0.85 (0.62–1.17) |
Notes: M1 adjusts for age, sex, race/ethnicity, education, and household income. M2: M1 + adjusts for cigarette and alcohol use and physical activity. M3 for BP: M2 + adjusts for BMI, total cholesterol to HDL cholesterol ratio, HbA1c, antihypertensive, antilipidemic, and antidiabetic medications. M3 for hypertension: M3 for BP minus antihypertensive medication. Abbreviations: BMI, body mass index; BP, blood pressure; CI, confidence interval; OR, odds ratio.
* P < 0.05 compared with never use.
Blood pressure
In unadjusted ANOVA models, a history of monthly use for more than 1 year was significantly associated with higher SBP when compared with never use (mean: 123.0 mm Hg (95% CI, 122.1–123.9) vs. 121.4 mm Hg (95% CI, 120.6–122.2)). This association was mainly due to a history of monthly use for more than 10 years (mean SBP: 124.4 mm Hg (95% CI, 123.2–125.6)). Recent and non-recent use by those with a history of monthly use were also associated with higher SBP (mean SBP: 123.2 (95% CI, 121.8–124.7) and 122.9 mm Hg (95% CI, 121.7–124.1), respectively).
After adjusting for sociodemographic variables, all significant associations between cannabis use and SBP were attenuated. After adjusting for cigarette and alcohol use and physical activity, a history of monthly use was again significantly associated with higher SBP (mean SBP: 123.2 mm Hg (95% CI, 122.0–124.3) compared with 121.3 mm Hg (95% CI, 120.4–122.2)). However, after adjusting for CVD risk factors, all significant associations between cannabis use and SBP were attenuated. No significant associations were found between any cannabis use category and DBP in any model (Figure 2a).
Figure 2.
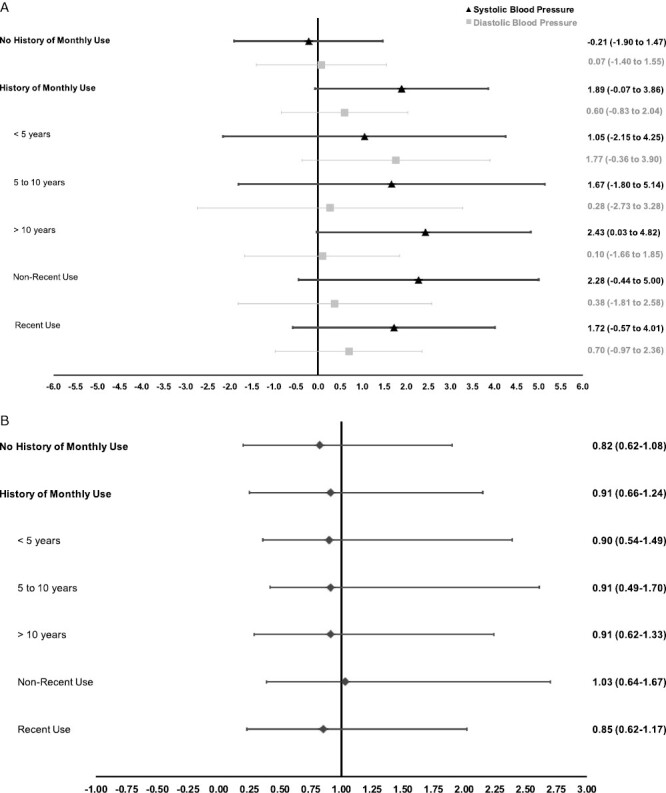
(a) Adjusted mean differences for blood pressure (mm Hg) by history of monthly use for more than 1 year, 2009–2018. (b) Adjusted odds ratios for hypertension by history of monthly use for more than 1 year, 2009–2018.
Hypertension
In unadjusted logistic regression models, as compared with never use, a history of monthly use was significantly associated with hypertension (OR: 1.15 (95% CI, 1.01–1.31)), mainly due to a history of monthly use for more than 10 years (OR: 1.22 (1.03–1.45)). Recent use among those with a history of monthly use was also significantly associated with hypertension. After adjusting for sociodemographic variables, cigarette and alcohol use, physical activity, and CVD risk factors, all associations were attenuated and null for every category of use (Figure 2b).
Interaction effects
Models exploring potential effect modification by age were significant for SBP for both history of monthly use and duration of monthly use (P for interaction 0.07 and 0.04, respectively) and for race/ethnicity for duration of monthly use only (P for interaction <0.01) (Supplementary Table S5 online). After accounting for multiple comparisons, only respondents between 45 and 59 years of age with a history of monthly use had significantly higher SBP than those in the 35 and 45 years of age group [i.e., 125.6 mm Hg (95% CI, 123.3–127.9) vs. 121.4 mm Hg (95% CI, 119.0–123.8), respectively].
After accounting for multiple comparisons, non-Hispanic Black, Asian and other respondents with a history of more than 10 years of monthly use had a significantly higher SBP than both Hispanic and non-Hispanic White respondents [i.e., 118.7 mm Hg (95% CI, 113.9–123.5) vs. 130.1 mm Hg (95% CI, 126.0–134.2) and 121.6 mm Hg (95% CI, 118.6–124.5)], respectively.
For hypertension, a significant interaction was only measured between no history of monthly use and race/ethnicity (P for interaction 0.08) (Supplementary Table S7 online).
Models exploring potential effect modification by frequency of monthly cannabis use (1–8, 9–24, or 25–30 times per month; and 1–2 or ≥3 joints or pipes per day) were nonsignificant for both BP and hypertension across 3 strata of duration of monthly use (<5, 5–10, or >10 years) (Supplementary Tables S6 and S8 online).
Sensitivity analyses
A sensitivity analysis was performed using additional measures of recency and frequency of recent cannabis use. In adjusted ANCOVA and logistic regression models, there were no associations between any category of recency or frequency of recent cannabis use and BP or hypertension (Supplementary Table S9 online).
DISCUSSION
In a nationally representative sample of middle-aged US adults, a history of monthly cannabis use for more than 1 year was not associated with increased BP or prevalent hypertension after adjusting for sociodemographic characteristics, lifestyle factors, BMI, and cardiovascular risk factors. Moreover, no associations were seen when cannabis use was stratified by duration of monthly use, recency of monthly use, or overall recency or frequency of recent use. Notably, these null findings were observed despite significant modest upward trends in recent cannabis use and recent use by those with a history of monthly use, as well as modest increases in mean SBP and DBP over the decade of observation.
A significant association between a history of monthly cannabis use and increased SBP was found after adjusting for cigarette and alcohol use and physical activity (i.e., Table 4, model 2). This association was likely due to negative confounding related to physical activity (i.e., respondents with a history of monthly use reported higher physical activity per week (406.0 min/wk vs. 358.6 for never users)). This finding is consistent with other studies showing that cannabis users tend to participate in more, not less, physical activity than nonusers.16
The results of our study are consistent with those reported by Shah et al., who observed no significant associations between recency and frequency of recent cannabis use, age of initiation, or sustained use, and hypertension. Their findings were based on analysis of a smaller sample (2017–2018 NHANES) but a wider age range (18 years and older). Importantly, while Shah et al. investigated “sustained use” (history of monthly use), to our knowledge, the present study is the first to evaluate the relationship between duration of monthly use, and recency of use among those with a history of monthly use, and BP and hypertension status using NHANES data.
With regard to recency and frequency of recent use only, our findings differ only slightly from a 2016 study utilizing 2005–2012 data from NHANES by Alshaarawy et al. in which recent use, but not frequency of recent use, was associated with modestly higher SBP (β = 1.4; 95% CI = 0.3, 2.3). No associations were found between cannabis use and prehypertension or hypertension. Similarly, a 2019 study by Vidot et al. using NHANES data (2005–2014) reported no associations for recent use, or frequency of recent use, and BP status or hypertension, except for higher odds of prehypertension (OR: 1.83, 95% CI, 1.24–2.70) and elevated BP (OR: 1.80, 95% CI, 1.13–2.88) in heavy, recent users (>20 days in the past 30 days). Neither of these previous studies controlled for physical activity nor other CVD risk factors, other than sex, age, and tobacco smoking, which may explain the differential results.
Strengths of the present study include the use of a nationally representative sample, a relatively large sample size, which was balanced across sociodemographic and other characteristics, and the use of a standardized objective outcome measure. The focus on history of monthly use, especially the duration of monthly use, is also a strength, given that the relationship of interest is based on a cumulative, recurrent exposure over time, not just recency or frequency of recent use.
Limitations include a cross-sectional design and the age limit of the NHANES Drug Use Questionnaire. Also, detailed measures of cannabis exposure were not available in the dataset, such as the actual amount of cannabis (grams of dried flower or extracted oil), and/or cannabinoids (milligrams of phytocannabinoids like Delta-9-tetrahydrocannabinol (THC), Cannabidiol (CBD), etc.), used and the method of use (e.g., inhalation, ingestion, etc.).
A history of monthly cannabis use for more than 1 year was not independently associated with either increased BP or prevalent hypertension in a study using a nationally representative sample of middle-aged US adults. Moreover, no significant associations were observed for duration of monthly use, recency, or frequency of recent use. The lack of association found in the present study contributes to the observational evidence suggesting frequent cannabis use over decades may not be associated with increased BP or hypertension in middle-aged US adults.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Erin Delker PhD for help with data analysis.
Contributor Information
Jamie Corroon, Department of Family Medicine, University of California San Diego, La Jolla, California, USA.
Igor Grant, Center for Medicinal Cannabis Research, Department of Psychiatry, University of California San Diego, La Jolla, California, USA.
Ryan Bradley, Herbert Wertheim School of Public Health and Human Longevity Science, University of California San Diego, La Jolla, California, USA.
Matthew A Allison, Department of Family Medicine, University of California San Diego, La Jolla, California, USA.
FUNDING
This study was funded by an National Institutes of Health, National Heart, Lung, and Blood Institute (NHLBI), T32 Grant (T32HL079891).
CONFLICT OF INTEREST
Dr Corroon is a member of the Board of Directors of CV Sciences, a manufacturer or hemp-derived CBD products.
REFERENCES
- 1. Pacher P, Steffens S, Haskó G, Schindler TH, Kunos G.. Cardiovascular effects of marijuana and synthetic cannabinoids: the good, the bad, and the ugly. Nat Rev Cardiol 2018; 15:151–166. [DOI] [PubMed] [Google Scholar]
- 2. Sidney S. Cardiovascular consequences of marijuana use. J Clin Pharmacol 2002; 42:64S–70S. [DOI] [PubMed] [Google Scholar]
- 3. Benowitz NL, Jones RT.. Cardiovascular and metabolic considerations in prolonged cannabinoid administration in man. J Clin Pharmacol 1981; 21:214S–223S. [DOI] [PubMed] [Google Scholar]
- 4. Alshaarawy O, Elbaz HA.. Cannabis use and blood pressure levels: United States National Health and Nutrition Examination Survey, 2005–2012. J Hypertens 2016; 34:1507–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vidot DC, Powers M, Gonzalez R, Jayaweera DT, Roy S, Dong C, Messiah SE.. Blood pressure and marijuana use: results from a decade of NHANES data. Am J Health Behav 2019; 43:887–897. [DOI] [PubMed] [Google Scholar]
- 6. Shah RM, Patel S, Shah S, Doshi S, Li A, Diamond JA.. Sustained cannabis use does not predispose clinical hypertension: findings from a national survey. J Clin Hypertens (Greenwich) 2023; 25:47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alexandre V. Association between cannabis use and blood pressure levels according to comorbidities and socioeconomic status. Sci Rep 2023; 13:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rodondi N, Pletcher MJ, Liu K, Hulley SB, Sidney S; Coronary Artery Risk Development in Young Adults (CARDIA) Study. Marijuana use, diet, body mass index, and cardiovascular risk factors (from the CARDIA study). Am J Cardiol 2006; 98:478–484. [DOI] [PubMed] [Google Scholar]
- 9. Haleem A, Hwang YJ, Elton-Marshall T, Rehm J, Imtiaz S.. The longitudinal relationship between cannabis use and hypertension. Drug Alcohol Rev 2021; 40:914–919. [DOI] [PubMed] [Google Scholar]
- 10. NHANES. About the National Health and Nutrition Examination Survey. Published 2020. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Updated 2020-01-08T07:25:03Z.
- 11. NHANES 2017–2018: Drug Use Data Documentation, Codebook, and Frequencies. Published 2022. https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/DUQ_J.htm#DUQ200
- 12. Vidot DC, Bispo JB, Hlaing WM, Prado G, Messiah SE.. Moderate and vigorous physical activity patterns among marijuana users: results from the 2007–2014 National Health and Nutrition Examination Surveys. Drug Alcohol Depend 2017; 178:43–48. [DOI] [PubMed] [Google Scholar]
- 13. Health Tech/Blood Pressure Procedures Manual. US Centers for Disease Control and Prevention, National Health and Nutrition Examination Survey, 2009. https://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/bp.pdf [Google Scholar]
- 14. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA, Williamson JD, Wright JT.. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension (Dallas, Tex: 1979) 2018; 71:1269–1324. [DOI] [PubMed] [Google Scholar]
- 15. Statistics National Center for Health. National Health and Nutrition Examination Survey, 2017–March 2020 Prepandemic File: Sample Design, Estimation, and Analytic Guidelines. 2022. https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/overviewbrief.aspx?Cycle=2017-2020 [PubMed] [Google Scholar]
- 16. Ong Lydia Q, John B, Citlali A, Paul C, Vincent B.. Cannabis use, sedentary behavior, and physical activity in a nationally representative sample of US adults. Harm Reduct J 2021; 18:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


