Abstract
Duchenne Muscular Dystrophy (DMD) is a neuromuscular disease that inevitably leads to total loss of autonomy. The new therapeutic strategies aim to both improve survival and optimise quality of life. Evaluating quality of life is nevertheless a major challenge. No DMD-specific quality of life scale to exists in French. We therefore produced a French translation of the English Duchenne Muscular Dystrophy module of the Pediatric Quality of Life Inventory (PedsQLTMDMD) following international recommendations. The study objective was to carry out a confirmatory validation of the French version of the PedsQLTMDMD for paediatric patients with DMD, using French multicentre descriptive cross-sectional data. The sample consisted of 107 patients. Internal consistency was acceptable for proxy-assessments, with Cronbach's alpha coefficients above 0.70, except for the Treatment dimension. For self-assessments, internal consistency was acceptable only for the Daily Activities dimension. Our results showed poor metric qualities for the French version of the PedsQLTMDMD based on a sample of about 100 children, but these results remained consistent with those of the original validation. This confirms the interest of its use in clinical practice.
Keywords: Neuromuscular disorder, Duchenne Muscular Dystrophy, Pediatric Quality of Life (PedsQL)
Background
Duchenne Muscular Dystrophy (DMD) is the most common progressive muscular dystrophy in children, with an incidence of 1/3,300 male births [1]. It is an inherited disease linked to the X chromosome resulting from pathogenic mutations in the DMD gene, which encodes a membrane cytoskeletal protein, dystrophin. DMD shows clinical motor, cardiac, respiratory and cognitive heterogeneity. The diagnosis is suggested by the following characteristic triad: progressive myopathic syndrome, Creatine Kinase increase, and pathological patterns of dystrophy. The development of the disease is progressive. Loss of walking ability inevitably occurs between the ages of 7 and 13 years, on average. Cognitive impairment is possible but varies between patients [2–4]. The course of DMD is marked by restrictive respiratory failure, cardiomyopathy, disorders of the static spine and nutritional difficulties [5, 6]. To date, there is no curative treatment, although coordinated multidisciplinary supportive care improves survival (adding about 15 to 20 years) [5–8]. The new therapeutic strategies, both current and future, aim to correct the primary genetic defect and thus limit the metabolic consequences and their functional impact. All these treatments aim to improve survival and optimise Quality of Life (QoL) [8].
QoL combines objective (socioeconomic), subjective (feelings of well-being), physical (chronic pathology) and cognitive factors. It is a measurable health indicator, which can be used as an outcome measurement in treatment trials or to assist decision-making in everyday medical practice. It is generally assessed using either generic scales or specific scales, through self- and/or proxy-assessments [9].
The evaluation of QoL in paediatrics requires the adaptation of factors such as age, possible activities, and family context. Those responsible for the child’s health (parents, caregivers, doctors) are directly involved in caregiving [9, 10].
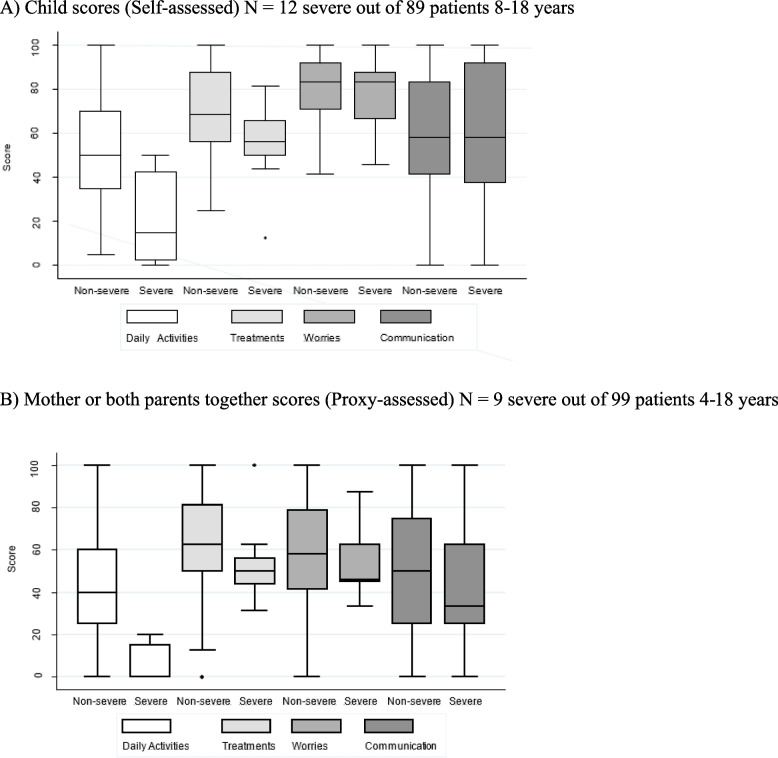
Given the specific features of DMD, it would be useful to have a specific scale in French. Currently, the Duchenne Muscular Dystrophy module of the Pediatric Quality of Life Inventory (PedsQLTMDMD) is one of the most widely used [11]. The scale was validated in English by Uzark et al. in 2012 (Fig. 1) [12] and in other languages, for example Chinese [13] and Thai [14]. The English version of PedsQLTMDMD was previously translated into French by our team in accordance with international recommendations and established guidelines.
Fig. 1.
English-language version of the PedsQLTMDMD
Forward translation (two independent bilingual, one French-mother-tongue and another English-mother-tongue, blinded translators) and back translation (one bilingual translator) were performed. Each step was reported in detail and submitted to the author of the original scale for agreement [15].
The objective of this study was to carry out a confirmatory validation of the French version (fv) of the DMD module of the PedsQL™ (PedsQLTMDMDfv) and document its metric properties in paediatric patients with DMD.
Materials and methods
PedsQLTMDMD’ scale
The PedsQLTMDMD targets three age groups: 5 to 7 years old, 8 to 12 years old, and 13 to 18 years old. It is available in two versions: proxy- and self-reports. The 18 items are divided into four dimensions: Daily Activities, Treatment, Worry, and Communication. Items are scored from 0 to 4 corresponding to ‘Never’, ‘Almost Never’, ‘Sometimes’, ‘Often’, and ‘Almost Always’. Dimension scores and a total score can be calculated and vary from 0 to 100. The closer the score is to 100, the better the QoL perceived by the child or caregiver. The recall period is one month.
The English version is used to assess QoL in clinical trials and daily clinical practice, given its robust internal consistency (close to 0.8) and adaptability to a wide range of ages.
Design and population
For this French multicentre descriptive cross-sectional study, children and their parents were included during a multidisciplinary consultation at their reference centre, between July 2018 and January 2019. Follow-up of the patients included in the study is being provided at the paediatric departments of the French Reference Centres for Neuromuscular Diseases in Toulouse, Bordeaux, Montpellier, Lyon, Reims, Strasbourg, Lille and Nantes.
The inclusion criteria were as follows: male children aged 5 to 18 years, carriers of genotyped DMD, registered in the BaMaRa database (national Rare Disease registry), and whose parents or guardians did not object to the child’s participation. The non-inclusion criteria were: inability to understand the questions, lack of parental authority, antidepressant or anti-psychotic treatment, non-French-speaking child and/or parents, and girl with DMD.
Data collection
At a biannual multidisciplinary consultation, the PedsQLTM3.0DMDfv was presented to the child and one or both parents by the child’s doctor or the psychologist of the department. Specifically, children over 8 years rated their own QoL and the parents of children of all ages also rated their child’s QoL. The questionnaires were completed separately in different rooms so that parents and children were not aware of each other’s responses. However, the child or the parent could consult the doctor/psychologist if they did not understand a question. The completion time was 15 to 20 min.
The score for each dimension of the DMD module was calculated as the average of the component items for the dimension. The response options were coded as follows: Never: 100 points, Almost Never: 75 points, Sometimes: 50 points, Often: 25 points, and Almost Always: 0 points, according to the authors’ instructions.
The following routine data were extracted directly from each patient’s medical records at the together with motor function (assessed by the Motor Function Measure/MFM [16], wheelchair use, and age at loss of walking ability); respiratory function (pulmonary function testing: forced vital capacity, respiratory support, type of respiratory support); cardiac function (left ventricular ejection fraction); nutritional status (weight, height, BMI, nutritional support by gastrostomy); school status (ordinary schooling, personal assistance, specialised schooling); and current drug treatment (corticosteroids, ACE inhibitors).
Statistical analysis
The response distributions of individual items, rates of floor and ceiling effects, are reported as frequencies and percentages, and subscale scores as mean ± standard deviation (SD), median and interquartile range, and minimum and maximum. The feasibility of the module was assessed using the percentage of missing data.
The internal consistency of each subscale was measured by Cronbach’s alpha coefficient in the whole sample and by age, with values above 0.70 considered as acceptable.
Construct validity was then examined. We investigated the structural validity of the module using a multi-trait scaling approach [17]. Polychoric correlations between individual items were estimated [18, 19]. Each item’s convergent validity was considered satisfactory if its correlation between with the other items within the same subscale and with its subscale score omitting that item (item-total correlation corrected for overlap) exceeded ≥ 0.40. Moreover, an item’s discriminant validity was judged sufficient if the item was more correlated with its own subscale than with the others.
Inter-subscale correlations were estimated. We used the Pearson correlation coefficient when the linearity of the association was demonstrated, or otherwise the Spearman rank correlation coefficient. We expected correlations between 0.30 and 0.70.
Construct validity was also assessed by the known-groups method. We anticipated lower patient and proxy PedsQLTM3.0DMD subscale scores with increasing DMD severity, defined as greater age, loss of walking ability, ventilation, Conversion Enzyme Inhibitor therapy, corticosteroid therapy. Severe DMD was also defined as non-outpatient and receiving ventilation.
Finally, agreement between the self‐assessed and proxy scores was measured by the intraclass correlation coefficient (ICC) estimated in a two-way mixed-effects model (absolute agreement) [20], and visually inspected using Bland and Altman plots. We used the same thresholds as Uzark et al. to interpret the ICC values, namely: ICC < 0.40 indicated poor-to-fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, good agreement; and 0.81–1.00, excellent agreement. Agreement between patients and their parents at the item level was evaluated through the proportion of observed agreement and the weighted kappa coefficient with quadratic weighting [21].
Analyses were performed with Stata14 and the R_v3.5.2Polycor package [22].
Ethics
The study was approved by the local Institutional Review Board (Southeast protection of individuals committee V) on 4 July 2018 (ID-RCB: 2018-A00895-50). An information note was given to the parents and an age-appropriate one to the child.
Results
Description of the sample, items and dimension scores
The analysis sample consisted of 107 patients: 16 in the 4–7 age group, 53 in the 8–11 age group, 38 in the 12–18 age group. The clinical characteristics according to age are set out in Table 1.
Table 1.
Patient characteristics by age group
| Age group | ||||
|---|---|---|---|---|
| 4–7 yrs | 8–11 yrs | 12–18 yrs | Total | |
| (N = 16) | (N = 53) | (N = 38) | (N = 107) | |
| Variable | n(%) | n(%) | n(%) | n(%) |
| Clinical diagnosis | ||||
| Deletion | 11 (84.6) | 31 (62.0) | 24 (64.9) | 66 (66.0) |
| Duplication | 1 (7.7) | 8 (16.0) | 3 (8.1) | 12 (12.0) |
| Point mutation | 1 (7.7) | 11 (22.0) | 10 (27.0) | 22 (22.0) |
| Walking ability acquired | ||||
| No | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Yes | 15 (100.0) | 53 (100.0) | 38 (100.0) | 106 (100.0) |
| N missing | 1 | 0 | 0 | |
| Loss of walking ability | ||||
| No | 15 (100.0) | 24 (46.2) | 0 (0.0) | 39 (37.1) |
| Yes | 0 (0.0) | 28 (53.8) | 38 (100.0) | 66 (62.9) |
| N missing | 1 | 1 | 0 | |
| Severity: not walking and ventilated | ||||
| No | 16 (100.0) | 50 (94.3) | 29 (76.3) | 95 (88.8) |
| Yes | 0 (0.0) | 3 (5.7) | 9 (23.7) | 12 (11.2) |
| N missing | 0 | 0 | 0 | |
| Medication treatment: corticosteroids | ||||
| No | 8 (57.1) | 10 (20.0) | 25 (65.8) | 43 (42.2) |
| Yes | 6 (42.9) | 40 (80.0) | 13 (34.2) | 59 (57.8) |
| N missing | 2 | 3 | 0 | |
The total MFM score ranged from 1 to 98.9% with a median of 57%. Among the 12 patients receiving non-invasive ventilation, ventilation was intermittent in 11 cases and continuous in one case. Nine of these patients were in the 12–18 age group. None were in the 5–7 age group.
For these 107 patients, we were able to use 89 self-reports (8–18 years) and 99 proxy-reports (5–18 years): 61 from the mother, and 38 from both parents together. The analysis of agreement between the responses to the self and proxy-assessments included 81 child-parent pairs: 49 pairs in the 8–11 age group and 32 pairs in the 12–18 age group.
Table 2 sets out the distribution of scores for the four dimensions: Daily activities, Treatment, Worry, and Communication. Parents’ scores ranged from 0 to 100 for all four dimensions. The self-report scores covered a narrower range, particularly for the Worry dimension (minimum score: 41.7 points). The variability of the scores (measured by standard deviation) appears to be lower for the self-report scores in general, especially for the Worry dimension.
Table 2.
Univariate description of the self- and proxy-assessment scores on the PedsQLTM3.0DMDfv
| Dimension | Self-assessment | Proxy-assessment | ||||||
|---|---|---|---|---|---|---|---|---|
| N | Min–Max | Med (IQR) | Mean (SD) | N | Min–Max | Med (IQR) | Mean (SD) | |
| Daily Activities | 89 | 0.0 – 100.0 | 45.0 (35.0 – 65.0) | 49.3 (26.3) | 99 | 0.0 – 100.0 | 40.0 (20.0 – 60.0) | 41.3 (25.2) |
| Treatment | 89 | 12.5 – 100.0 | 62.5 (56.3 – 81.3) | 67.3 (19.0) | 98 | 0.0 – 100.0 | 62.5 (43.8 – 81.3) | 62.0 (23.1) |
| Worry | 89 | 41.7 – 100.0 | 83.3 (70.8 – 91.7) | 80.9 (14.9) | 99 | 0.0 – 100.0 | 58.3 (41.7 – 79.2) | 58.0 (24.0) |
| Communication | 89 | 0.0 – 100.0 | 58.3 (41.7 – 83.3) | 58.2 (27.6) | 99 | 0.0 – 100.0 | 50.0 (25.0 – 75.0) | 48.0 (32.5) |
Non-responses to items were very rare. We observed no marked ceiling or floor effect.
Fidelity of the PedsQLTM3.0DMDfv
Internal consistency was acceptable for the proxy-assessments (Cronbach's alpha > 0.70) with the exeption of the Treatment dimension. For the self-assessments, internal consistency was acceptable only for the Daily Activities dimension. It was insufficient for the other dimensions (Table 3). Although the estimates among patients with severe disease were highly imprecise due to small numbers, the findings remained unchanged when stratified by disease severity (data not shown).
Table 3.
Internal consistency of the PedsQLTM3.0DMDfv Dimensions: Cronbach’s alpha
| Dimension | Child (self-assessments) | Proxy-assessments | |||||
|---|---|---|---|---|---|---|---|
| Total | Group 8–11 yrs | Group 12–18 yrs | Total | Group 4–7 yrs | Group 8–11 yrs | Group 12–18 yrs | |
| (n = 89) | (n = 51) | (n = 38) | (n = 99) | (n = 16) | (n = 51) | (n = 32) | |
| Daily Activities | |||||||
| Pearson | 0.74 | 0.72 | 0.70 | 0.81 | 0.86 | 0.75 | 0.66 |
| Polyc. + corr.cont | 0.78 | 0.73 | 0.69 | 0.82 | 0.68 | 0.69 | 0.74 |
| Treatment | |||||||
| Pearson | 0.43 | 0.41 | 0.51 | 0.68 | 0.79 | 0.53 | 0.76 |
| Polyc. + corr.cont | 0.50 | 0.51 | 0.44 | 0.70 | 0.69 | 0.52 | 0.70 |
| Worry | |||||||
| Pearson | 0.52 | 0.58 | 0.43 | 0.83 | 0.87 | 0.84 | 0.76 |
| Polyc. + corr.cont | 0.72 | 0.77 | 0.68 | 0.85 | † | 0.83 | 0.64 |
| Communication | |||||||
| Pearson | 0.66 | 0.60 | 0.68 | 0.87 | 0.85 | 0.85 | 0.90 |
| Polyc. + corr.cont | 0.69 | 0.56 | 0.66 | 0.89 | 0.75 | 0.84 | 0.81 |
Pearson: Cronbach alpha coefficient based on the Pearson correlation matrix
Polyc. + corr.cont: Cronbach alpha coefficient based on the polychoric correction matrix with correction for empty cells
† Not estimated, because one item had an empty category for the subgroup
Polychoric correlation coefficients showed a satisfactory convergent validity of each item for the self and proxy-assessments; the discriminant validity of each item was also satisfactory. Most of the correlations between the four dimensions of the self-assessments presented in Table 4 were moderate between 0.30 and 0.70. The correlations between the Daily Activities and Worry subscales were particularly weak. Notably, there was poor correlation between the Communication subscale and the other subscales. The correlations between scores for the parents on the four subscales were between 0.30 and 0.70, but weaker correlations were observed between the Communication subscale and the other subscales, especially for the evaluations concerning the 8- to 11-year-old patients (data not shown).
Table 4.
Inter-correlations between self-evaluation scores on the PedsQLTM3.0DMDfv, N = 89
| PedsQL™ Dimensions | ||||
|---|---|---|---|---|
| Daily Activities | Treatment | Worry | Communication | |
| Group 8–11 yrs | ||||
| Daily Activities | 1.000 | 0.566 | 0.156 † | 0.244 |
| Treatment | 0.566 | 1.000 | 0.531 † | 0.294 |
| Worry | 0.156 † | 0.531 † | 1.000 | 0.263 |
| Communication | 0.244 | 0.294 | 0.263 | 1.000 |
| Group 12–18 yrs | ||||
| Daily Activities | 1.000 | 0.535 | 0.214 † | 0.050 |
| Treatment | 0.535 | 1.000 | 0.297 † | 0.151 |
| Worry | 0.214 † | 0.297 † | 1.000 | 0.339 |
| Communication | 0.050 | 0.151 | 0.339 | 1.000 |
| All ages combined | ||||
| Daily Activities | 1.000 | 0.555 | 0.198 † | 0.054 |
| Treatment | 0.555 | 1.000 | 0.439 † | 0.189 |
| Worry | 0.198 † | 0.439 † | 1.000 | 0.258 |
| Communication | 0.054 | 0.189 | 0.258 | 1.000 |
Pearson’s correlation coefficient are presented
† Spearman’s correlation coefficient is presented due to a non linear monotone association between scores
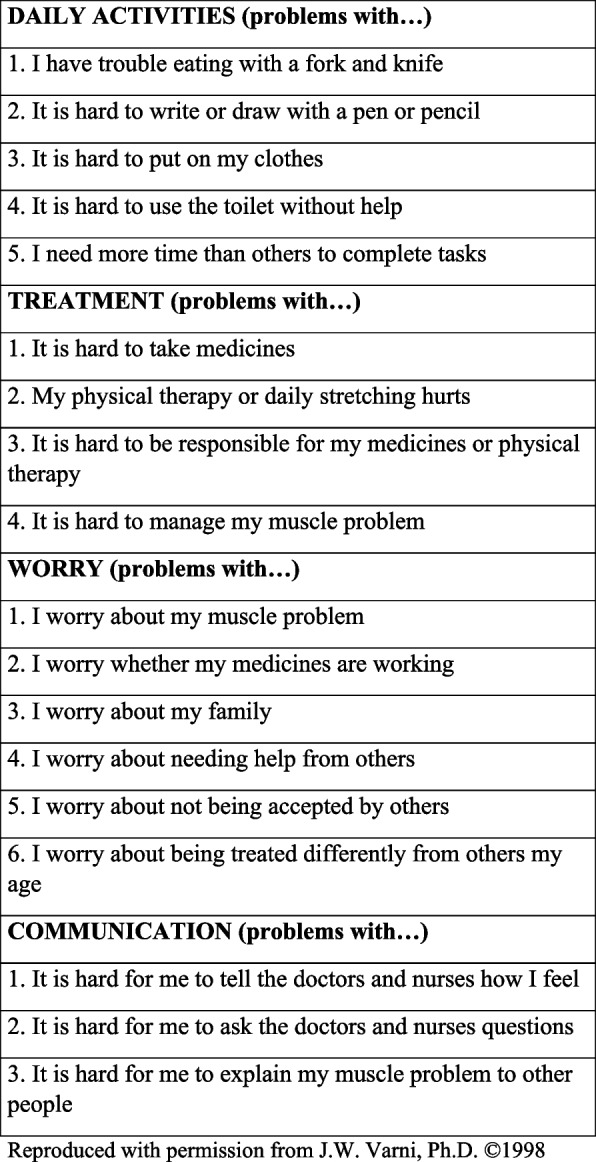
To analyse the discriminant validity of the PedsQLTM3.0DMDfv, we assessed whether disease severity was associated with the PedsQLTM3.0DMD scores. Figure 2 presents “Child” and “Mother” scores as a function of “Severity”. The QoL score was significantly lower in the Daily Activities dimension for both the self- and proxy-assessments.
Fig. 2.
Distribution of scores (“Child” and “Mother”) according to DMD severity. A Child scores (Self-assessed) N = 12 severe out of 89 patients 8–18 years. B Mother or both parents together scores (Proxy-assessed) N = 9 severe out of 99 patients 4–18 years
A total of 49 and 32 child-parent pairs were examined in the 8–11 and 12–18 age groups, respectively. Table 5 presents the difference (parent score-child score) between the children’s scores and those of their mothers or both parents together. The general trend indicated lower proxy scores than self-scores.
Table 5.
Description of the differences between the PedsQLTM3.0DMD self-assessed and proxy-assessed scores, and the reliability indices between the self- and proxy-assessments
| Domain | Self-assessment | Proxy-assessment | Mean difference | ICC 2-way mixed effects model | |||
|---|---|---|---|---|---|---|---|
| Dimension | N | Mean (SD) | N | Mean (SD) | N | Mean (SD) | [95% CI] |
| All ages combined | |||||||
| Daily Activities | 81 | 50.4 (26.0) | 81 | 38.1 (24.2) | 81 | -12.3 (14.1) | 0.75 [0.29–0.89] |
| Treatment | 81 | 66.8 (19.1) | 81 | 61.1 (23.2) | 81 | -5.7 (22.0) | 0.45 [0.26–0.61] |
| Worry | 81 | 81.2 (13.9) | 81 | 56.5 (23.0) | 81 | -24.7 (23.0) | 0.15 [-0.07–0.36] |
| Communication | 81 | 56.9 (27.3) | 81 | 46.5 (31.4) | 81 | -10.4 (36.3) | 0.23 [0.02–0.42] |
| Group: 8–11 yrs | |||||||
| Daily Activities | 49 | 59.5 (24.8) | 49 | 47.4 (24.1) | 49 | -12.0 (13.9) | 0.75 [0.28–0.90] |
| Treatment | 49 | 70.0 (18.8) | 49 | 65.5 (18.7) | 49 | -4.5 (18.3) | 0.51 [0.28–0.69] |
| Worry | 49 | 82.3 (15.0) | 49 | 57.2 (24.5) | 49 | -25.2 (23.3) | 0.19 [-0.08–0.45] |
| Communication | 49 | 52.4 (27.4) | 49 | 44.6 (30.8) | 49 | -7.8 (38.9) | 0.11 [-0.17–0.37] |
| Group: 12–18 yrs | |||||||
| Daily Activities | 32 | 36.6 (21.6) | 32 | 23.8 (16.3) | 32 | -12.8 (14.5) | 0.59 [0.08–0.82] |
| Treatment | 32 | 62.0 (18.9) | 32 | 54.5 (27.8) | 32 | -7.5 (27.0) | 0.34 [0.01–0.61] |
| Worry | 32 | 79.6 (12.0) | 32 | 55.4 (20.8) | 32 | -24.1 (22.7) | 0.05 [-0.11–0.27] |
| Communication | 32 | 63.8 (26.1) | 32 | 49.3 (32.6) | 32 | -14.5 (32.0) | 0.38 [0.06–0.63] |
The ICCs were low for the Worry and Communication subscales, indicating poor agreement in the parent–child dyads. They were low to moderate across age groups for the Treatment subscale, and fairly good for Daily Activities. This last result should be qualified, however, as the precision around the ICC estimate is specifically very low.
Discussion
Population
We obtained a representative sample in terms of diagnosis, with a predominance of deletions (66%), a 12% rate of duplications and a point mutation rate of 22% consistent with the literature [23]. The total MFM score varied from 1 to 98.90% (median of 57%) ranging from patients with less severe up to very severe motor impairment. Corticosteroids were administered to 57.8% of the population compared with 85% for the English-language validation, probably due to divergences between English and French language guidelines.
Fidelity of the PedsQLTM3.0DMDfv: internal consistency
Our results showed good internal consistency for the parents’ scores, except for the Treatment dimension. For the children, internal consistency was acceptable only in the Daily Activities dimension, which provides objective information on everyday living. In the validation study of the original English-language version, with 200 parents and 117 children (i) the internal consistency was better, with Cronbach's alpha close to 0.8 (ii) the difference between the children’s and parents’ data was less significant with parents’ data showing higher Cronbach's alphas, (iii) the lowest Cronbach's alpha for both datasets was in Treatment dimension [12].
In our French version, the lower internal consistency for both children and parents’ scores -compared to validation study of the original English-language version- could probably suggested a misunderstanding of the several items. For example, children found difficult to understand the concept of Treatment in our initial translation process. We therefore replaced it by Medicines and Physiotherapy. In clinical practice, this item could be even more specific with the names of the medications or the number of tablets taken per day, which would help the children to give a more precise answer. Another explanation could be that the heterogeneity of our sample, ranging from less severe up to severe impairments, could warrant this finding. We therefore conducted an assessment by severity, which allowed us to examine the scale’s internal consistency separately in several subgroups. It remained imprecise due to the low numbers, but conclusions did not change: the internal consistency was insufficient for the children’s questionnaires and satisfactory for the parents’ questionnaires, with a similar distribution of scores.
Analysis of internal consistency and its sensitivity revealed good internal consistency, especially for the responses from the parents’ group and the severe group of children. This analysis was not performed in the original validation.
In our study, the differences between the children’s and parents’ findings were greater than in the validation study of the original English version, with the parents’ data showing higher Cronbach's alphas. The lowest Cronbach's alpha for both datasets was for the Treatment dimension [12]. The difference can be explained by a change in the wording of items in our French translation. Indeed, although identical for all ages in the children’s or the parents’ questionnaires, the items were formulated differently for the children and their parents. This difference was marked for item 4: "I am having trouble living with my illness [children]" and "Difficulties in managing his/her muscle disorder [parents]". However, the back translation was correct. This item 4 seems to be related more to the Worry dimension than to the Treatment dimension. However, it is ranked in Treatment dimension (in the original version and consequently in our French translation) which can be a little confusing.
Internal consistency was lower for the Treatment dimension for the parents’ assessments and was better for the Daily Activities dimension (which provides objective and representative information on everyday living) for the children’s assessments. Our results were consistent with the original English version where the lowest Cronbach's alpha for both datasets was in the Treatment dimension [12].
Construct validity
First, the convergent validity was satisfactory for each item in the Daily Activities and Communication subscales, for both child and parent ratings. It was also good for the Treatment and Worry subscales, but only for the parents’ assessments. The correlation coefficients were higher in the Daily Activities dimension than in the other dimensions. These findings seem logical. The Daily Activities dimension reflects motor impairment and severity and is composed of objective items. The Worry and Communication dimensions are more subjective and are much more directly dependent on the child or the parents’ feelings, which makes probably them less reliable.
Second, several items from various dimensions were positively correlated with items of a different dimension. For example, item 3 of the Treatment dimension appeared to be more closely associated with the Daily Activities dimension sub-scores, which is consistent with the fact that the Daily Activities dimension is the more objective dimension and the one more closely linked to motor impairments.
The same pattern was found for item 4 of the Treatment dimension, which appeared to be associated with the Daily Activities, Treatment, and Worry dimensions. It is possible that this item could be too subjective in its interpretation. This analysis was not reported in the original validation article.
Third, most of the correlations between the questionnaire dimensions were moderate. The Communication dimension showed little correlation with the other dimensions. This raises the question of its relevance and therefore that of the notion of an overall QoL score. In the original validation, these correlations were not performed.
Finally, for the oldest children with severe DMD, the QoL reported by the children and their parents was significantly poorer for the Daily Activities dimension. For the other dimensions, the results were not significant. Our result was consistent with the original article where, for the Daily Activities dimension, QoL was significantly better for the 8–12-year-old children than for the 13–18-year-olds, both for children and parents. This previous result was reinforced by a significant difference -both for children and parents- between children needing mobility aids and those moving without assistance: QoL was deemed to be better for those who didn’t use mobility aids or could walk [12]. Similarly, Davis et al., in their 2010 study to validate the neuromuscular module for the DMD population, also found that children and parents reported a poorer QoL compared to a healthy population, most importantly in the physical dimension. QoL was significantly better in patients who did not use a wheelchair or very rarely compared to those who used one all the time [24]. Thus, as with previous studies, ours clearly demonstrated the progressive chronic condition component of DMD, leading to irreversibly reduced physical condition, mobility and autonomy, and consequently a gradual decline in QoL.
Agreement between self- and proxy-assessments
The overall trend was that proxy-assessments scores (parents) were lower than self-assessments (children): parents rated their child's QoL worse than their children thought. The difference was more marked for subjective items corresponding to feelings (Worry and Communication dimensions) compared to more objective items (Treatment and Daily Activities dimensions). For the Worry dimension, the correlation was better between proxy-assessment (parent) and self-assessment (child) scores when the child's QoL was good. Our findings showed the same trend as the original study: the ICC was between 0.61–0.80 for Daily Activities, which indicated good agreement, and moderate For Treatment and Worry (ICC = 0.41–0.60). The weakest ICC was for the Communication dimension [12]. This perception gap-both in original and in our translation- may be linked to the considerable difficulty parents had in understanding their position when replying to the questionnaire. Several parents thought that they had to assess their own QoL.
Our French version of the scale showed poor agreement between the parents and children, similar to the findings on the original English scale. The agreement was better for objective functions (activities of daily living) and lower for more subjective functions (Worry, emotions). Children appeared less worried than their parents in both versions. This result is consistent with literature on this subject and refers to the "disability paradox" or "well-being paradox" [25, 26], a process of adapting to changes in health and accommodation to illness. Children think they have a better QoL than their parents, because they have become accustomed to their diseases. This is the only life they know and they rate their QoL as relatively good, and perceive their well-being differently. Reference can also be made to the "coping strategy", an adaptation strategy that helps protect against the adverse effects of disease. Explaining the “disability paradox” to families might therefore give them a more positive view of their child's experience.
Another explanation to explain this difference is that parents have different perspectives on their child's illness, and they probably feel more anxious about the future. They adjust their perceptions based on their knowledge of the natural course of the disease and think negatively about the future [27]. Also, parents are often overwhelmed by the care and their negative perceptions can also be explained by the "burden” of being an informal caregiver [28]. DMD leads to intense and prolonged family involvement, leading to physical, psychological and financial consequences [29]. It will be probably necessary in the future to assess the parents’ QoL -or at least to collect data on their mental health or their own difficulties- in order to interpret the results more precisely.
Conclusion
Based on a representative sample (100 patients), we were able to demonsrate the useful metric qualities of the French version of the PedsQLTM3.0DMD. Our results, which are consistent with those of the original version, validate the relevance and use of the PedsQLTM3.0DMD and its use in clinical practice. We would therefore propose that the analysis of QoL in these patients be undertaken on a broader scale, or even systematically. We would also suggest that there is a need to take this factor into account in future therapeutic trials.
However, assessing the QoL of DMD' patients appears to be a complex task. PedsQLTM3.0DMD is a useful tool but several limitations have been reported. it seems useful to propose a more comprehensive tool that takes into account, for example, the affected muscles, the degree of severity, the level of pain and fatigue of the children, etc. Furthermore, the creation of a cognitive level-adjusted scale would appear to be suitable. In fact, we were unable to include all of our patients due to moderate to severe cognitive difficulties that prevented their understanding of the scale. If we could enlarge our population sample using a cognitive -level-adjusted scale, one example being the SOLE questionnaire [30], it would be useful to revise our data according to IQ level in the different subgroups to obtain more representative insights.
Acknowledgements
This work is dedicated to the children and their families who participated in the study. We would like to thank the author of the original scale for their support. The authors also thank Michèle Dufour, Raphaële Chasserieau, Christelle Peseux and Anne-Cécile Coville for their help.
Abbreviations
- DMD
Duchenne Muscular Dystrophy
- ICC
Intraclass Correlation Coefficient
- MFM
Motor Function Measure
- QoL
Quality of Life
- PedsQL
Pediatric Quality of Life
- SD
Standard Deviation
Authors’ contributions
EW and CC are principal investigator of the study, conceived the idea for the study, and was a major contributor in writing the protocol. EW, MB and CC analyzed and interpreted the data, conceived the first working plan based on results, and wrote the manuscript. VE and CA carried out the statistical analysis, wrote the statistical sections of the manuscript, and reviewed the final manuscript. UWL, YP, CV, SF, PS, CE, JMC, VL and EB was involved in study coordination, quality monitoring, patients inclusion. All the authors read and approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Funding
The project was completed without specific support.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the local Institutional Review Board (Southeast protection of individuals committee V) on 4 July 2018 (ID-RCB: 2018-A00895-50) and conducted in accordance with the Declaration of Helsinki. Written informed consent was provided by the participants and their legal guardian/next of kin.
Consent for publication
Not Applicable.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Elisabeth Wallach and Claude Cances these authors contributed equally to this work.
Contributor Information
Elisabeth Wallach, Email: wallach.a@chu-toulouse.fr.
Maelle Biotteau, Email: maelle.biotteau@inserm.fr.
References
- 1.Crisafulli S, Sultana J, Fontana A, Salvo F, Messina S, Trifirò G. Global epidemiology of Duchenne muscular dystrophy: an updated systematic review and meta-analysis. Orphanet J Rare Dis. 2020;15(1):141. doi: 10.1186/s13023-020-01430-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duan D, Goemans N, Takeda S, Mercuri E, Aartsma-Rus A. Duchenne muscular dystrophy. Nat Rev Dis Primers. 2021;7(1):13. doi: 10.1038/s41572-021-00248-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Falzarano MS, Scotton C, Passarelli C, Ferlini A. Duchenne muscular dystrophy: from diagnosis to therapy. Molecules (Basel, Switzerland) 2015;20(10):18168–18184. doi: 10.3390/molecules201018168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desguerre I, Christov C, Mayer M, Zeller R, Becane HM, Bastuji-Garin S, Leturcq F, Chiron C, Chelly J, Gherardi RK. Clinical heterogeneity of Duchenne muscular dystrophy (DMD): definition of sub-phenotypes and predictive criteria by long-term follow-up. PloS one. 2009;4(2):e4347. doi: 10.1371/journal.pone.0004347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birnkrant DJ, Bushby K, Bann CM, Apkon SD, Blackwell A, Brumbaugh D, Case LE, Clemens PR, Hadjiyannakis S, Pandya S, Street N, Tomezsko J, Wagner KR, Ward LM, Weber DR, DMD Care Considerations Working Group Diagnosis and management of Duchenne muscular dystrophy, part 1: diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. Lancet Neurol. 2018;17(3):251–267. doi: 10.1016/S1474-4422(18)30024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Birnkrant DJ, Bushby K, Bann CM, Alman BA, Apkon SD, Blackwell A, Case LE, Cripe L, Hadjiyannakis S, Olson AK, Sheehan DW, Bolen J, Weber DR, Ward LM, DMD Care Considerations Working Group Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol. 2018;17(4):347–361. doi: 10.1016/S1474-4422(18)30025-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nascimento Osorio A, Medina Cantillo J, Camacho Salas A, Madruga Garrido M, Vilchez Padilla JJ. Consensus on the diagnosis, treatment and follow-up of patients with Duchenne muscular dystrophy. Neurologia. 2019;34(7):469–481. doi: 10.1016/j.nrl.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Verhaart I, Aartsma-Rus A. Therapeutic developments for Duchenne muscular dystrophy. Nat Rev Neurol. 2019;15(7):373–386. doi: 10.1038/s41582-019-0203-3. [DOI] [PubMed] [Google Scholar]
- 9.Waters E, Davis E, Ronen GM, Rosenbaum P, Livingston M, Saigal S. Quality of life instruments for children and adolescents with neurodisabilities: how to choose the appropriate instrument. Dev Med Child Neurol. 2009;51(8):660–669. doi: 10.1111/j.1469-8749.2009.03324.x. [DOI] [PubMed] [Google Scholar]
- 10.Matza LS, Swensen AR, Flood EM, Secnik K, Leidy NK. Assessment of health-related quality of life in children: a review of conceptual, methodological, and regulatory issues. Value Health. 2004;7(1):79–92. doi: 10.1111/j.1524-4733.2004.71273.x. [DOI] [PubMed] [Google Scholar]
- 11.Powell PA, Carlton J, Woods HB, Mazzone P. Measuring quality of life in Duchenne muscular dystrophy: a systematic review of the content and structural validity of commonly used instruments. Health Qual Life Outcomes. 2020;18(1):263. doi: 10.1186/s12955-020-01511-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uzark K, King E, Cripe L, Spicer R, Sage J, Kinnett K, Wong B, Pratt J, Varni JW. Health-related quality of life in children and adolescents with Duchenne muscular dystrophy. Pediatrics. 2012;130(6):e1559–e1566. doi: 10.1542/peds.2012-0858. [DOI] [PubMed] [Google Scholar]
- 13.Hu J, Jiang L, Hong S, Cheng L, Kong M, Ye Y. Reliability and validity of the Chinese version of the Pediatric Quality Of Life InventoryTM (PedsQLTM) 3.0 neuromuscular module in children with Duchenne muscular dystrophy. Health Qual Life Outcomes. 2013;11:47. doi: 10.1186/1477-7525-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thongsing A, Likasitwattanakul S, Sanmaneechai O. Reliability and validity of the Thai version of the Pediatric quality of life inventory™ 3.0 Duchenne muscular dystrophy module in thai children with duchenne muscular dystrophy. Health Qual Life Outcomes. 2019;17(1):76. doi: 10.1186/s12955-019-1140-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wallach, E. & Cances, C. (2016). French version of Pediatric Quality Of Life InventoryTM (PedsQLTM) 3.0 neuromuscular module in children with Duchenne Muscular Dystrophy. https://eprovide.mapi-trust.org/instruments/pediatric-quality-of-life-inventory#need_this_questionnaire [DOI] [PMC free article] [PubMed]
- 16.Bérard C, Payan C, Hodgkinson I, Fermanian J, MFM Collaborative Study Group A motor function measure for neuromuscular diseases. Construction and validation study. Neuromuscular Disord. 2005;15(7):463–470. doi: 10.1016/j.nmd.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Fayers, P. M., & Machin, D. (2007). Quality of Life: The Assessment, Analysis and Interpretation of Patient-Reported Outcomes (2nd ed.). Chichester: John Wiley & Sons Ltd. http://dx.doi.org/10.1002/9780470024522
- 18.Brown MB, Benedetti JK. On the mean and variance of the tetrachoric correlation coefficient. Psychometrika. 1977;42:347–355. doi: 10.1007/BF02293655. [DOI] [Google Scholar]
- 19.Zumbo B, Gadermann A, Zeisser C. Ordinal versions of coefficients alpha and theta for likert rating scales. J Mod Appl Stat Methods. 2007;6:21–29. doi: 10.22237/jmasm/1177992180. [DOI] [Google Scholar]
- 20.Mcgraw K, Wong SP. Forming inferences about some intraclass correlation coefficients. Psychol Methods. 1996;1:30–46. doi: 10.1037/1082-989X.1.1.30. [DOI] [Google Scholar]
- 21.Fleiss J, Levin B, Paik M. In Statistical Methods for Rates and Proportions. Statistical Methods Rates Proportions. 2003;203:510–511. doi: 10.1002/0471445428. [DOI] [Google Scholar]
- 22.Fox, J. (2019). polycor: Polychoric and Polyserial Correlations..https://CRAN.R-project.org/package=polyco
- 23.Aartsma-Rus A, Ginjaar IB, Bushby K. The importance of genetic diagnosis for Duchenne muscular dystrophy. J Med Genet. 2016;53(3):145–151. doi: 10.1136/jmedgenet-2015-103387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davis SE, Hynan LS, Limbers CA, Andersen CM, Greene MC, Varni JW, Iannaccone ST. The PedsQL in pediatric patients with Duchenne muscular dystrophy: feasibility, reliability, and validity of the pediatric quality of life inventory neuromuscular module and generic core scales. J Clin Neuromuscul Dis. 2010;11(3):97–109. doi: 10.1097/CND.0b013e3181c5053b. [DOI] [PubMed] [Google Scholar]
- 25.Landfeldt E, Lindgren P, Bell CF, Guglieri M, Straub V, Lochmüller H, Bushby K. Health-related quality of life in patients with Duchenne muscular dystrophy: a multinational, cross-sectional study. Dev Med Child Neurol. 2016;58(5):508–515. doi: 10.1111/dmcn.12938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pangalila R. Quality of life in Duchenne muscular dystrophy: the disability paradox. Dev Med Child Neurol. 2016;58(5):435–436. doi: 10.1111/dmcn.12959. [DOI] [PubMed] [Google Scholar]
- 27.Pangalila RF, van den Bos GA, Bartels B, Bergen M, Stam HJ, Roebroeck ME. Prevalence of fatigue, pain, and affective disorders in adults with duchenne muscular dystrophy and their associations with quality of life. Arch Phys Med Rehabil. 2015;96(7):1242–1247. doi: 10.1016/j.apmr.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 28.Uttley L, Carlton J, Woods HB, Brazier J. A review of quality of life themes in Duchenne muscular dystrophy for patients and carers. Health Qual Life Outcomes. 2018;16(1):237. doi: 10.1186/s12955-018-1062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Landfeldt E, Lindgren P, Bell CF, Guglieri M, Straub V, Lochmüller H, Bushby K. Quantifying the burden of caregiving in Duchenne muscular dystrophy. J Neurol. 2016;263(5):906–915. doi: 10.1007/s00415-016-8080-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Orcesi S, Ariaudo G, Mercuri E, Beghi E, Rezzani C, Balottin U, SOLE NMDs Study Group A new self-report quality of life questionnaire for children with neuromuscular disorders: presentation of the instrument, rationale for its development, and some preliminary results. J Child Neurol. 2014;29(2):167–181. doi: 10.1177/0883073813511859. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.