Abstract
Seven years to the Global Taskforce on Cholera Control’s target of reducing cholera cases and deaths by 90% by 2030, Africa continues to experience a high incidence of the disease. In the last 20 years, more than 2.6 million cases and 60 000 deaths of the disease have been recorded, mostly in sub-Saharan Africa. Case Fatality Ratio remains consistently above the WHO-recommended 1% with a yearly average of 2.2%. Between 1 January 2022 and 16 July 2023, fourteen African countries reported 213 443 cases and 3951 deaths (CFR, 1.9%) of the disease. In this perspective article, based on available literature and the authors’ field experiences in Africa, we discuss the underlying reasons for the sustained transmission of the disease. We posit that in addition to the well-known risk factors for the disease, the chronic cholera situation in Africa is due to the poor socioeconomic development status, weak household and community resilience, low literacy levels, weak capacity of African countries to implement the 2005 International Health Regulation and the pervasively weak health system on the continent. Stemming this tide requires good leadership, partnership, political commitment, and equity in access to health services, water, and sanitation. Therefore, we recommend that African governments and stakeholders recognize and approach cholera prevention and control from the long-term development lens and leverage the current cholera emergency preparedness and response efforts on the continent to strengthen the affected countries’ health, water, and sanitation systems. We call on international organizations such as WHO and the Africa Centres for Diseases Control to support African governments in scaling up research and innovations aimed at better characterizing the epidemiology of cholera and developing evidence-based, context-specific, and innovative strategies for its prevention and control. These recommendations require long-term multisectoral and multidisciplinary approaches.
Keywords: Africa, Cholera epidemic, cholera prevention and control, community resilience, national action plan for health security, socioeconomic development
Background
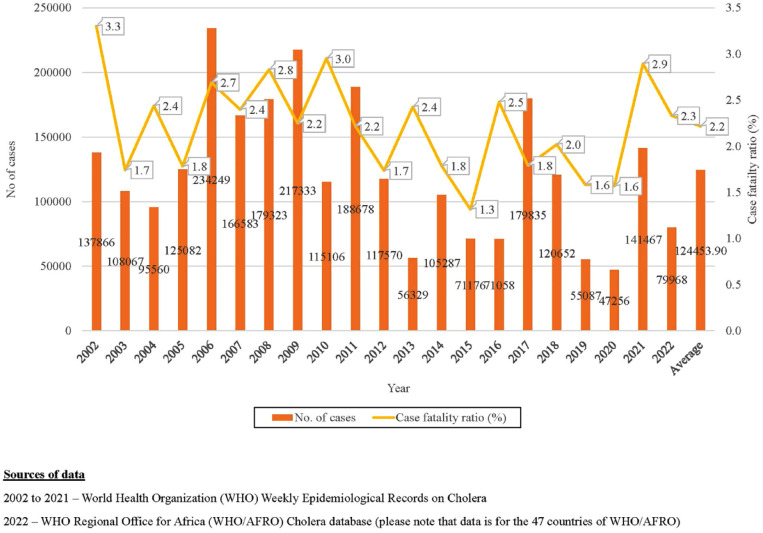
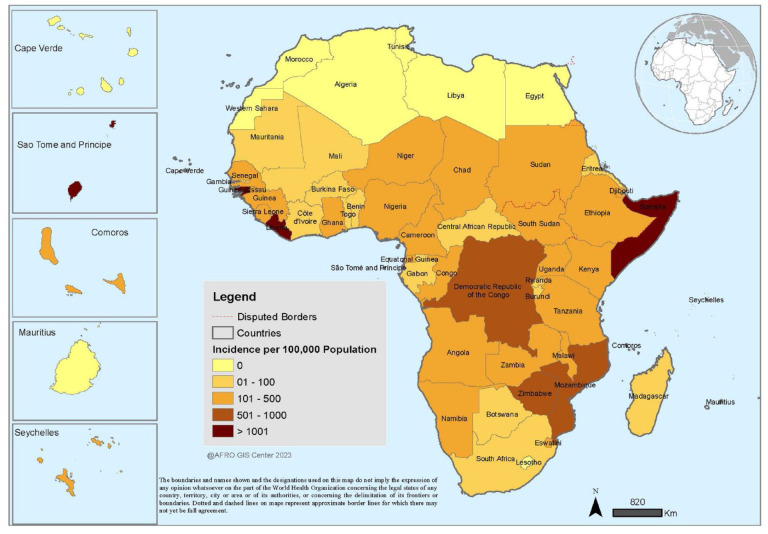
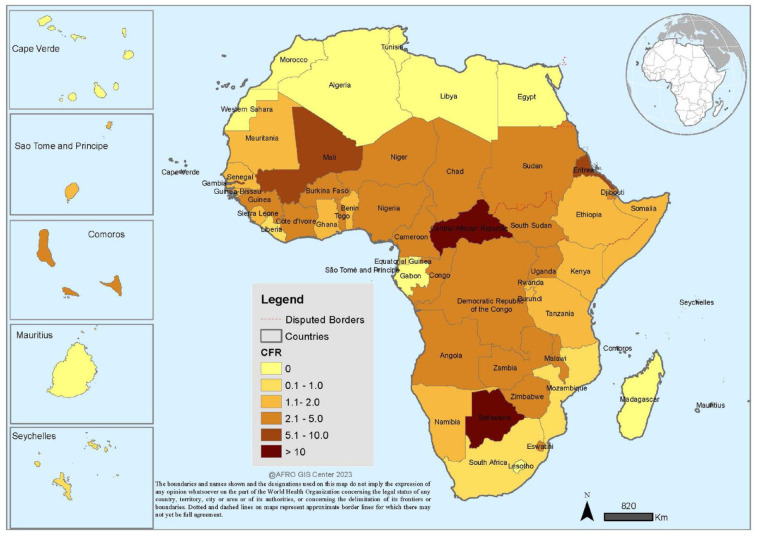
Cholera is not new to Africa. The seventh cholera pandemic reached the continent’s shores in 1971, and since then, the disease has spread rapidly and is now endemic in several countries. 1 According to the World Health Organization (WHO) data, more than 2.6 million cases and 60 000 deaths due to the disease have been recorded in the last 20 years (Figure 1), most of them in the sub-Saharan region of the continent (Figure 2).2,3 Case Fatality Ratio (CFR) remains consistently above the WHO-recommended 1% (yearly average of 2.2%), with an average of 23 countries affected yearly (Figures 1 and 3).3,4 Between 1 January 2022 to 16 July 2023, 14 African countries reported more than 213 443 cases and 3951 deaths (CFR, 1.9%) of the disease. 5 The African Regional Office of WHO (WHO/AFRO) issued an alert on the escalating situation on 9 February 2023. 6 Mintz and Guerrant have aptly described this burgeoning cholera situation in Africa as “a lion in our village” due to the unacceptable levels of morbidity and mortality associated with the disease. 7 Apart from the loss of lives, the disease causes massive economic losses, which further retard socioeconomic development in Africa. 8 Mogasale et al estimated an economic burden of US$130 million from cholera-related illness and its treatment in 44 African countries in 2015. 9 The repeated cholera outbreaks in several African countries point to the inability of the countries to eliminate endemic cholera while the persistently high CFR points to either inability to access good health care, poor health-seeking behaviors or poor management of cholera cases during outbreaks.
Figure 1.
Epidemiology of Cholera in Africa: 2002-2022.
Figure 2.
Cholera incidence per 100 000 population in Africa: 2002-2021.
Figure 3.
Cholera case fatality rate in Africa: 2002-2021.
Cholera is an acute diarrheal infection which is acquired through the ingestion of water or food that are contaminated by the cholera-toxin-producing strains of a bacteria known as Vibrio cholerae, namely serogroups 01 (divided into biotypes El Tor and Classical 01 both of which are divided into Ogawa and Inaba serotypes) and 0139. It has distinctive clinical presentations and can easily be diagnosed in the remotest of villages, even by a layperson. Although most patients are asymptomatic, 1 out of 10 present with vomiting, watery diarrhea, and dehydration, which could rapidly result in hypovolemic shock and death if not promptly treated. 10 Risk factors for transmission of the disease include, among others, consumption of contaminated water or food, lack of access to safe sanitation, inadequate handwashing, especially after using the toilet, increased rainfall, flooding, and lack of good drainage.11-16 Outbreak prevention and control are through the provision of adequate quantities of safe drinking water and improved sanitation to affected populations, enhancing personal hygiene and clinical management of cases. An oral cholera vaccine has been introduced and rolled out widely to prevent the spread of ongoing epidemics to unaffected areas and prevent epidemics in humanitarian settings.17-19 As a renewed effort to curb the scourge of the disease, the Global Taskforce on Cholera Control developed a global strategy for cholera control in 2017, with a 2030 target for a 90% reduction in cases and deaths, and elimination in 20 countries, and is currently supporting countries including those of Africa to implement the strategy. 20 Several African-led initiatives to scale up the prevention and control of the disease have been implemented with some success. For instance, in 2018, the 68th WHO regional committee for Africa adopted and is supporting all African Member States to scale up the global strategy implementation. 21 While in March 2023, a high-level ministerial conference resolved to scale up cholera preparedness and response on the continent. 22
Despite these ongoing initiatives and the ample understanding of the behavior of this well-known “lion,” why have African countries been unable to prevent it from killing its people? We agree with several researchers who have attributed the chronic cholera situation to, among other reasons, the increasing incidences of drought, flooding, conflicts, and population displacement on the continent.23-25 Nevertheless, we posit that other underlying issues continue to fuel the sustained incidence of cholera on the continent. In this perspective article, based on the evidence in the literature and our experiences in managing cholera epidemics in Africa at the strategic and operational level, we discuss the underlying socioeconomic and related reasons why there is a sustained incidence of the disease. We approached this from 2 perspectives: (1) Why is Africa unable to prevent cholera outbreaks from occurring? and (2) Why are African countries unable to control cholera outbreaks in a timely manner? We conclude by proposing practical recommendations for addressing this scourge.
Why is Africa Unable to Prevent Cholera Outbreaks From Occurring?
In our view, the deteriorating cholera situation is largely due to the pervasively poor socioeconomic development, which continues to fuel inequitable distribution and access to the social services that determine health outcomes such as water, sanitation, education, good housing, and healthcare on the continent.26-29 A good example is the 2008/2009 cholera outbreak in Zimbabwe, which occurred within the context of a socio-economic crisis in the country, resulting in the breakdown of the aging water and sanitation system of the country’s capital city of Harare. 30 This observation is corroborated by Talavera and Perez who demonstrated that cholera affects low-income countries more than countries with middle or high-income. 31 As a direct effect of poor socioeconomic development, the water and sanitation situation on the continent is dire. A 2020 estimate showed that only 27% of the population used safely managed sanitation, 39% used safely managed drinking water and 37% had access to basic hygiene. 32 Safe water supply and modern sewage disposal systems are either unavailable or derelict and unable to keep pace with population needs in many African countries. They are poorly maintained where they exist, resulting in disruptions contaminating drinking water sources, particularly in the aftermath of natural hazards. 33 Unfortunately, most African countries have largely approached these developmental challenges from an emergency lens within the context of cholera outbreak control. The emphasis has been on short-lived emergency-focused cholera prevention and control programs that do not address the underlying longer-term developmental problems associated with transmitting the disease. For instance, the funds used to implement short-term water and sanitation measures such as water trucking, procurement and distribution of water containers, and chlorine tablets over the years could have been better utilized to implement more effective long-term interventions aimed at providing safe water and sanitation facilities to communities in a sustainable manner. Another example is the risk factors for outbreaks, such as poor drainage systems, which often result in flooding during heavy rains but are hardly addressed by short-term cholera preparedness programs.
Another challenge for cholera prevention and control in Africa is rapid urbanization due to rural-to-urban drift and poor urban planning, which fuels the mushrooming of urban slums without a commensurate expansion in social services. Living conditions in these urban slums are usually extremely poor, with inequity in access to water and sanitation. Furthermore, poor housing and pervasive poverty, which are hallmarks of life in these unplanned urban settlements, create fertile grounds for disease outbreaks. Therefore, it is unsurprising that most cholera outbreaks on the continent often start in densely populated urban areas with gradual spread to the rural areas. This trend has been observed in Zambia, Nigeria, Zimbabwe, Tanzania, Kenya, and other countries.14,34-36 Finn and Cobbinah drew attention to the interface between informality in urban settlements and climate change and how these can potentiate each other. 37 This further increases the risk of cholera outbreaks in urban slums.
Patel et al identified the elements of a resilient community, including the availability of community resources, effective communication, local knowledge, training, and education. 38 Thus, household and community resilience are critical in preventing disease outbreaks, including cholera. Resilient households and communities would be able to resist, absorb and recover from the risks and effects of cholera outbreaks in a timely and efficient manner, thus preventing recurrent outbreaks. Unfortunately, this is not the case in most African communities. For instance, while a critical intervention for preventing cholera infection is handwashing with soap, many households in Africa lack access to drinking water, let alone water for handwashing. Where water is available, the households may be unable to afford soap. Lack of local knowledge and effective communication about cholera risks increases the risk of infection, undetected outbreaks, and lack of prevention at the household and community levels. While these challenges are not limited to cholera, they are critical in preventing other diseases such as COVID-19 and Ebola Virus Disease (EVD). Patel et al also rightly identified health (including the pre-existing status of health and access to healthcare services before, during and after emergency events) as one of the critical elements of a resilient community. 38 Health conditions such as HIV, tuberculosis, malnutrition etc., which are prevalent in sub-Saharan Africa, are fertile grounds for sustaining outbreaks such as cholera. The continent’s inadequate access to healthcare services further contributes to this challenge.
The relationship between low literacy, poverty (using household income as a measure), and inequality is undeniable, with low literacy almost always predicting lower income and exclusion, including from information about opportunities for betterment and resilience. 39 Literacy influences recognition of health risks, health-seeking behavior and the ability of an individual to make the right choices thus, literate individuals tend to enjoy better health and live longer. 40 Female literacy has been demonstrated to positively impact the health of the family and particularly the health of children 41 likewise, literacy is a major determinant of adult health. 42 Leckebusch and Abdussalam demonstrated the association between literacy and cholera infection. 43 They, like other researchers44-46 posit that adult literacy is inversely proportional to the number of cases and deaths of cholera. They further postulated that those with better literacy are more likely to make informed decisions to avoid contracting cholera and to seek healthcare when infected. Although Africa’s literacy levels have been on the increase in recent times, it is far behind those of other regions. 47 As of 2020, the average literacy level in sub-Saharan Africa was 67%, below the global average of 87% with cholera endemic countries such as South Sudan with as low as 35% literacy rate. The low literacy levels in Africa are thus another plausible reason cholera outbreaks continue to perpetuate in Africa. With such a low literacy level, recognizing and avoiding cholera risks, seeking appropriate and timely care, and comprehending cholera prevention messages becomes challenging.
Cholera has traditionally been viewed as a public health problem, which is a misnomer. It is, in fact, a multidimensional problem which requires multisectoral collaboration, coordination, and a multidisciplinary approach. While cholera outbreaks may be primarily a public health issue, the key factors such as lack of safe water and good sanitation leading to them are mostly under the purview of other sectors, as are the required financial resources that can be used to invest in these systems. 48 Unfortunately, such multisectoral coordination and collaboration are often fragmented in African settings due to a lack of strategic and empowered political leadership which could facilitate such collaborations. Bennett et al listed, among others, suboptimal high-level political commitment, varied understanding of the problem at hand across sectors and competition undermining collaboration as the challenges which hinder multisectoral collaborations. 49 Perhaps one of the greatest challenges in preventing cholera outbreaks in Africa is the lack of attention and funding for the disease compared to other equally important diseases of epidemic potential. For instance, a significant amount of resources are often committed to control outbreaks of diseases such as COVID-19 and EVD, yet cholera does not seem to receive the same attention although it’s magnitude and related economic burden far outweighs those of these other diseases. 49
Why Are African Countries Unable to Timely Contain Cholera Outbreaks When They Occur?
Arguably, one of the most plausible reasons for the inability of African countries to timely and effectively contain cholera outbreaks is the weak capacity to implement the International Health Regulations 2005 (IHR 2005). While good progress has been made in assessing the IHR (2005) core capacities and developing National Action Plans for Health Security (NAPHS), this has not translated into strengthening those capacities for more effective epidemic preparedness and response. As of April 2019, more than 80% of African countries had conducted joint external evaluations of their IHR core capacities and developed NAPHS in the sub-region. 50 However, the NAPHS, which is the main vehicle to address the gaps in the 19 technical core capacities of the IHR to prevent, detect and respond to outbreaks in an integrated manner, remains largely unimplemented due to a lack of funding and poor prioritization. Rather, emergency preparedness funds are largely channeled to fund vertical preparedness programs for diseases such as EVD, COVID-19, etc. For instance, between 2018 and 2019, the health partners in South Sudan spent over US$30 million to support an EVD disease preparedness program at the detriment of the country’s NAPHS, which was budgeted at an estimated US$69 million for 5 years. 51 This constituted a missed opportunity to strengthen national and sub-national health security.
Late detection and reporting of outbreaks are also critical challenges which have contributed to the high CFR of cholera in Africa in the last 20 years. 52 This is largely due to weak surveillance systems which fail to detect outbreaks on time. However, national authorities often delay declaring outbreaks due to social, political, and economic considerations. For instance, anecdotal evidence showed that the magnitude of the 2008/2009 cholera outbreak in Zimbabwe was largely due to the late detection and declaration of the outbreak. By the time the outbreak was officially declared, over 11 000 cases and almost 500 deaths had occurred. This delay also constrained the intensification of the response efforts, which did not commence until about 23 weeks after the first case was reported and by which time the peak of the outbreak had been surpassed. Similar experiences have been documented in South Sudan and elsewhere. 53 Many countries that eventually declare outbreaks refer to the disease as “Acute Watery Diarrhea” or “AWD” for economic and political reasons; this creates distortions in response efforts.
Africa’s weak health systems also constrain timely and effective containment of outbreaks. Shortage and high attrition of healthcare workers, inadequate knowledge of the existing staff on cholera management and shortage of the required essential medicines often result in poor outbreak management, ultimately resulting in high CFR. 54 Other health system challenges include sub-optimal infection prevention and control practices in the health facilities and communities, disruption of the supply chain for medical supplies, inadequate financing of cholera response efforts and poor oversight, governance and coordination capacity. For example, during the 2008/2009 cholera outbreak in Zimbabwe, the economic crisis at the time resulted in a breakdown of the country’s health systems with an acute shortage of staff and supplies. 55 Similar situations have also been observed in South Sudan, a country that has been in a chronic humanitarian crisis for a very long time. 56
Negative beliefs that prevent behavioral changes required for cholera prevention and control remain a critical problem in Africa. These practices are often driven by social, cultural, and religious factors. Outbreaks have been attributed to witchcraft, and other measures are preferred over public health measures in such situations. For instance, a study in Malawi showed that a section of the population believes that cholera is like a “wind” that would pass and thus does not need public health intervention. 57 Another study in the Democratic Republic of the Congo reported that witchcraft and breastfeeding were perceived as the causes of acute watery diarrhea. 58 Available evidence also points to the effect of social, cultural, and religious factors in the acceptance of cholera interventions. Msyamboza et al attributed the rejection of chlorinated water to its “bad taste.” 57 Studies have also linked the acceptance of oral cholera vaccines to social, cultural, and religious factors. 59 Distrust of national and local authorities due to ethnic, political, and religious reasons has also resulted in rejecting government-led cholera preventive activities and public health advice. This also fuels misinformation that propagates outbreaks.60,61
Cholera outbreak response strategies are largely reactive in Africa. Since the advent of the oral cholera vaccines, emphasis on preventing and controlling the disease has shifted from the traditional provision of water and sanitation approach to the vaccine, which is misleading. Furthermore, emergency preparedness and response are prioritized over longer-term cholera prevention and risk reduction interventions. Where they exist, preparedness efforts are often poorly planned and implemented, leaving countries unprepared for outbreaks. 17 Lastly, Africa’s porous borders with unregulated population movements between countries for commercial, cultural, and humanitarian reasons is also a major challenge in preventing and controlling cholera outbreaks on the continent.62,63 This is further compounded by poor cross-border coordination of prevention and control efforts.
Conclusion
Notwithstanding the well-understood epidemiology and risk factors for cholera, the disease has continued to cause high morbidity and mortality in the last 20 years. In addition to the well-known risk factors for the disease, we attribute the sustained transmission of the disease to the poor socioeconomic development status, weak household and community resilience, low literacy rates, weak capacity of countries to implement the IHR and the pervasively weak health system on the continent. Since the disease has become endemic in several African countries, taming the “lion” requires longer-term, holistic approaches to address the underlying developmental issues perpetuating it. This requires good leadership, partnership, and political commitment, underscored by the principles and targets of the Sustainable Development Goals of leaving no one behind and ensuring human rights and equity in access to health services, water, and sanitation.
Based on the foregoing, we propose a few recommendations. First, African governments and stakeholders should recognize and approach cholera prevention and control from the long-term development lens. In this regard, cholera prevention and control should be integrated into the national water, sanitation, and health sector strategic plans, with an appropriate whole-of-government approach and leadership to garner multisectoral commitment for control and elimination. Second, the ongoing cholera emergency preparedness and response efforts on the continent should be leveraged to strengthen affected countries’ health, water, and sanitation systems. Particularly, we advocate for funding and implementation of the NAPHS as a platform to strengthen regional and national health security and capacity for cholera outbreak detection and response across African countries using the One-Health approach. Third, a whole-of-society approach that prioritizes community participation using community resources and knowledge to strengthen community resilience, risk communication, education and engagement in cholera prevention and control is imperative. Fourth, international organizations such as WHO and the Africa Centres for Diseases Control should support African governments in scaling up research and innovations aimed at better characterizing the epidemiology of cholera and developing evidence-based, context-specific, and innovative strategies for its prevention and control. Furthermore, these organizations should support African governments to strengthen cross-border coordination and synchronization of cholera preparedness and response efforts. Importantly, we propose long-term multisectoral and multidisciplinary approaches to implement these recommendations.
Acknowledgments
The authors alone are responsible for the views expressed in this article, which do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: OOO is on the Editorial Board of the Health Services Insights Journal, while JNO is the Editor-in-Chief. They did not participate in any way in the handling of this manuscript.
Author Contributions: OOO conceived and wrote the article’s first draft. All authors read and provided significant inputs into all drafts of the article, agreed to be accountable for all aspects of the work and approved the final draft of the article for publication.
ORCID iD: Olushayo Oluseun Olu  https://orcid.org/0000-0001-6832-873X
https://orcid.org/0000-0001-6832-873X
References
- 1. Ali M, Nelson AR, Lopez AL, Sack DA. Updated global burden of cholera in endemic countries. PLoS Negl Trop Dis. 2015;9(6):1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Cholera, 2021. Wkly Epidemiol Rec. 2020;97:453-464. [Google Scholar]
- 3. Mengel MA, Delrieu I, Heyerdahl L, Gessner BD. Cholera outbreaks in Africa. In: Nair G, Takeda Y, eds. Cholera Outbreaks. Current Topics in Microbiology and Immunology. Vol. 379. Springer; 2014, pp. 117-144 [DOI] [PubMed] [Google Scholar]
- 4. Uwishema O, Okereke M, Onyeaka H, et al. Threats and outbreaks of cholera in Africa amidst COVID-19 pandemic: a double burden on Africa’s health systems. Trop Med Health. 2021;49:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. Cholera in the WHO African Region: Weekly Regional Cholera Bulletin – 17 July 2023. Accessed 1 August 2023. https://www.afro.who.int/publications/cholera-who-african-region-weekly-regional-cholera-bulletin-29-march-2023-cloned
- 6. World Health Organization. New cholera cases in Africa surging fast, reach a third of 2022 total in a month. 2022. Accessed April 25, 2023. https://www.afro.who.int/news/new-cholera-cases-africa-surging-fast-reach-third-2022-total-month
- 7. Mintz ED, Guerrant RL. A lion in our village — the unconscionable tragedy of cholera in Africa. N Engl J Med. 2009;360(11):1060-1063. https://www.nejm.org/doi/full/10.1056/NEJMp0810559 [DOI] [PubMed] [Google Scholar]
- 8. Kirigia JM, Sambo LG, Yokouide A, et al. Economic burden of cholera in the WHO African region. BMC Int Health Hum Rights. 2009;9:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mogasale V, Ngogoyo SM, Mogasale VV. Model-based estimation of the economic burden of cholera in Africa. BMJ Open. 2021;11(3):e044615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention. Cholera – Vibrio cholerae infection. CDC. Accessed April 11, 2023. https://www.cdc.gov/cholera/index.html [Google Scholar]
- 11. Qaserah AM, Al Amad MA, Al Serouri AA, Khader YS. Risk factors of cholera transmission in Al Hudaydah, Yemen: case-control study. JMIR Public Health Surveill. 2021;7(7):e27627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Challa JM, Getachew T, Debella A, et al. Inadequate hand washing, lack of clean drinking water and latrines as major determinants of cholera outbreak in Somali Region, Ethiopia in 2019. Front Public Health. 2022;10:845057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fagbamila IO, Abdulkarim MA, Aworh MK, et al. Cholera outbreak in some communities in North-East Nigeria, 2019: an unmatched case-control study. BMC Public Health. 2023;23(1):446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nanzaluka FH, Davis WW, Mutale L, et al. Risk factors for epidemic cholera in Lusaka, Zambia-2017. Am J Trop Med Hyg. 2020;103(2):646-651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sasaki S, Tambatamba B, Mulenga P, Suzuki H, Igarashi K. Spatial analysis of risk factor of cholera outbreak for 2003–2004 in a peri-urban area of Lusaka, Zambia. Am J Trop Med Hyg. 2008;79(3):414-421. [PubMed] [Google Scholar]
- 16. Sasaki S, Suzuki H, Fujino Y, Kimura Y, Cheelo M. Impact of drainage networks on cholera outbreaks in Lusaka, Zambia. Am J Public Health. 2009;99:1982-1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. World Health Organization. Cholera vaccines: WHO position paper – August 2017. Wkly Epidemiol Rec. 2017;92(34):477-498. [PubMed] [Google Scholar]
- 18. Sialubanje C, Kapina M, Chewe O, et al. Effectiveness of two doses of Euvichol-plus oral cholera vaccine in response to the 2017/2018 outbreak: a matched case–control study in Lusaka, Zambia. BMJ Open. 2022;12(11):e066945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Song KR, Lim JK, Park SE, et al. Oral cholera vaccine efficacy and effectiveness. Vaccines. 2021;9(12):1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Global Taskforce on Cholera Control. Ending cholera- A global roadmap to 2030. 2017. Accessed April 11, 2023. ending-cholera-a-global-roadmap-to-2030.pdf (gtfcc.org). https://www.gtfcc.org/about-cholera/roadmap-2030/
- 21. World Health Organization Regional Committee for Africa. Regional framework for the implementation of the global strategy for cholera prevention and control, 2018-2030. Accessed August 1, 2023. AFR-RC68-7CholeraControlStrategyFramework_PostRC68_0.pdf (who.int). [Google Scholar]
- 22. Africa Centres for Disease Control and Prevention. High-Level Emergency Ministerial Meeting on Cholera Epidemics and Climate-Related Public Health Emergencies. Africa CDC. Accessed August 1, 2023. [Google Scholar]
- 23. Mintz E. Taking aim at cholera. Lancet. 2018;391(10133):1868-1870. [DOI] [PubMed] [Google Scholar]
- 24. Burki T. Things have gone seriously wrong: global cholera surges. Lancet. 2023;401(10377):633-634. [DOI] [PubMed] [Google Scholar]
- 25. Musa SS, Ezie KN, Scott GY, et al. The challenges of addressing the cholera outbreak in Cameroon. Public Heal Pr. 2022;4:100295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Velimirovic B, Subramanian M, Sadek F. Socio-economic and environmental factors and human health example of cholera El Tor in Manila. Zentralbl Bakteriol Orig B. 1975;160(1):1-27. [PubMed] [Google Scholar]
- 27. Davies-Teye BBK, Vanotoo L, Yabani JB, Kwaakye-Maclean C. Socio-economic factors associated with cholera outbreak in southern Ghana, 2012: a case-control study. Int J Epidemiol. 2015;44(suppl_1):i188-i188. [Google Scholar]
- 28. Root ED, Rodd J, Yunus M, Emch M. The role of socioeconomic status in longitudinal trends of cholera in Matlab, Bangladesh, 1993-2007. PLoS Negl Trop Dis. 2013;7(1):e1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Collins AE, Lucas ME, Islam MS, Williams LE. Socio-economic and environmental origins of cholera epidemics in Mozambique: guidelines for tackling uncertainty in infectious disease prevention and control. Int J Environ Stud. 2006;63(5):537-549. [Google Scholar]
- 30. Chirisa I, Nyamadzawo L, Bandauko E, Mutsindikwa N. The 2008/2009 cholera outbreak in Harare, Zimbabwe: case of failure in urban environmental health and planning. Rev Environ Health. 2015;30(2):117-124. [DOI] [PubMed] [Google Scholar]
- 31. Talavera A, Perez EM. Is cholera disease associated with poverty? J Infect Dev Ctries. 2009;3(6):408-411. [DOI] [PubMed] [Google Scholar]
- 32. UNICEF/WHO Joint Monitoring Project. Progress on drinking water, sanitation and hygiene in Africa (2000-2020) - The JMP Snapshot Report, 5 years into the SDGs. Accessed May 22, 2023. JMP-Snapshot-Report-2022.pdf (unicef.org).
- 33. Chen WH, Azman AS. Mitigating Cholera in the aftermath of cyclone Idai. Am J Trop Med Hyg. 2019;101(5):960-962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lawoyin TO, Ogunbodede NA, Olumide EA, Onadeko MO. Outbreak of cholera in Ibadan, Nigeria. Eur J Epidemiol. 1999;15(4):367-370. [DOI] [PubMed] [Google Scholar]
- 35. Chambers K. Zimbabwe's battle against cholera. Lancet. 2009;373:993-994. [DOI] [PubMed] [Google Scholar]
- 36. Penrose K, de Castro MC, Werema J, Ryan ET. Informal urban settlements and cholera risk in dar es Salaam, Tanzania. PLoS Negl Trop Dis. 2010;4(3):e631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Finn BM, Cobbinah PB. African urbanisation at the confluence of informality and climate change. Urban Stud. 2023;60(3):405-424. [Google Scholar]
- 38. Patel SS, Rogers MB, Amlôt R, Rubin GJ. What do we mean by ‘community resilience’? A systematic literature review of how it is defined in the literature. PLoS Curr. 2017;9. doi: 10.1371/currents.dis.db775aff25efc5ac4f0660ad9c9f7db2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Movement for Canadian Literacy. Factsheet #9 – Literacy and poverty. Accessed May 22, 2023. Factsheet #9 - Literacy and Poverty (copian.ca).
- 40. Baker DP, Leon J, Smith Greenaway EG, Collins J, Movit M. The education effect on population health: a reassessment. Popul Dev Rev. 2011;37(2):307-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kickbusch IS. Health literacy: addressing the health and education divide. Health Promot Int. 2001;16(3):289-297. [DOI] [PubMed] [Google Scholar]
- 42. Smith-Greenaway E. Are literacy skills associated with young adults' health in Africa? Evidence from Malawi. Soc Sci Med. 2015;127:124-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Leckebusch GC, Abdussalam AF. Climate and socioeconomic influences on interannual variability of cholera in Nigeria. Health Place. 2015;34:107-117. [DOI] [PubMed] [Google Scholar]
- 44. Trærup SLM, Arigoni Ortiz R, Markandya A. The Health Impacts of Climate Change: A Study of Cholera in Tanzania. Basque Centre for Climate Change BC3. BC3 Working Paper Series 2010-01.
- 45. Ali M, Emch M, Donnay JP, Yunus M, Sack RB. The spatial epidemiology of cholera in an endemic area of Bangladesh. Soc Sci Med. 2002;55(6):1015-1024. [DOI] [PubMed] [Google Scholar]
- 46. Ackers ML, Quick RE, Drasbek CJ, Hutwagner L, Tauxe RV. Are there national risk factors for epidemic cholera? The correlation between socioeconomic and demographic indices and cholera incidence in Latin America. Int J Epidemiol. 1998;27(2):330-334. [DOI] [PubMed] [Google Scholar]
- 47. World Bank. Literacy rate, adult total (% of people aged 15 and above) – sub-Saharan Africa. Accessed May 12, 2023. worldbank.org [Google Scholar]
- 48. Usman A, Sarkinfada F, Mufunda J, et al. Recurrent cholera epidemics in Kano–northern Nigeria. Cent Afr J Med. 2005;51(3-4):34-38. [PubMed] [Google Scholar]
- 49. Bennett S, Glandon D, Rasanathan K. Governing multisectoral action for health in low-income and middle-income countries: unpacking the problem and rising to the challenge. BMJ Glob Health. 2018;3:e000880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Talisuna A, Yahaya AA, Rajatonirina SC, et al. Joint external evaluation of the International Health Regulation (2005) capacities: current status and lessons learnt in the WHO African region. BMJ Glob Health. 2019;4(6):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Olu OO, Lako R, Wamala JF, et al. What did we learn from preparing for cross-border transmission of Ebola virus disease into a complex humanitarian setting - the Republic of South Sudan? Infect Dis Poverty. 2020;9(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Omoleke SA, Ajibola O, Ajiboye JO, Raji RO. Quagmire of epidemic disease outbreaks reporting in Nigeria. BMJ Glob Health. 2018;3: e000659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Nsubuga F, Garang SC, Tut M, et al. Epidemiological description of a protracted cholera outbreak in Tonj East and Tonj North counties, former Warrap State, South Sudan, May-Oct 2017. BMC Infect Dis. 2019;19(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pietroni MAC. Case management of cholera. Vaccine. 2020;38:A105-A109. doi: 10.1016/j.vaccine.2019.09.098 [DOI] [PubMed] [Google Scholar]
- 55. Mason PR. Zimbabwe experiences the worst epidemic of cholera in Africa. J Infect Dev Ctries. 2009;3(2):148-151. [DOI] [PubMed] [Google Scholar]
- 56. Moszynski P. Cholera outbreak highlights poor health services in southern Sudan. BMJ Clin Res Ed. 2006;332(7541):570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Msyamboza KP, Kagoli M, M'bang'ombe M, Chipeta S, Masuku HD. Cholera outbreaks in Malawi in 1998-2012: social and cultural challenges in prevention and control. J Infect Dev Ctries. 2014;8(6):720-726. [DOI] [PubMed] [Google Scholar]
- 58. Merten S, Schaetti C, Manianga C, et al. Sociocultural determinants of anticipated vaccine acceptance for acute watery diarrhea in early childhood in Katanga Province, Democratic Republic of Congo. Am J Trop Med Hyg. 2013;89(3):419-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Schaetti C, Ali SM, Hutubessy R, et al. Social and cultural determinants of oral cholera vaccine uptake in Zanzibar. Hum Vaccin Immunother. 2012;8(9):1223-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Démolis R, Botão C, Heyerdahl LW, et al. A rapid qualitative assessment of oral cholera vaccine anticipated acceptability in a context of resistance towards cholera intervention in Nampula, Mozambique. Vaccine. 2018;36(44):6497-6505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Chigudu S. The politics of cholera, crisis and citizenship in urban Zimbabwe: ‘People were dying like flies. Afr Aff. 2019;118(472):413-434. [Google Scholar]
- 62. Bwire G, Mwesawina M, Baluku Y, Kanyanda SS, Orach CG. Cross-border cholera outbreaks in sub-Saharan Africa, the mystery behind the silent illness: what needs to be done? PLoS One. 2016;11(6):e0156674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Buliva E, Elnossery S, Okwarah P, et al. Cholera prevention, control strategies, challenges and World Health Organization initiatives in the Eastern Mediterranean Region: a narrative review. Heliyon. 2023;9(5):e15598. [DOI] [PMC free article] [PubMed] [Google Scholar]