Abstract
Objective:
To evaluate whether neurobehavioral symptoms differ between groups of Veterans with mild traumatic brain injury (mTBI) classified by health characteristics.
Participants:
71,934 post-9/11 Veterans with mTBI from the Chronic Effects of Neurotrauma Consortium Epidemiology Warfighter cohort.
Design:
Cross-sectional analysis of retrospective cohort.
Main Measures:
Health phenotypes identified using latent class analysis of health and function over 5 years. Symptom severity measured using Neurobehavioral Symptom Inventory; domains included vestibular, somatic, cognitive, and affective.
Results:
Veterans classified as Moderately Healthy had the lowest symptom burden while the Polytrauma Phenotype group had the highest. After accounting for sociodemographic and injury characteristics, Polytrauma Phenotype Veterans had about three times the odds of reporting severe symptoms in each domain compared to Moderately Healthy Veterans. Those Veterans who were initially Moderately Healthy but whose health declined over time had about twice the odds of severe symptoms as consistently healthier Veterans. The strongest associations were in the affective domain. Compared to the Moderately Healthy group, Veterans in other phenotypes were more likely to report symptoms substantially interfered with their daily lives (OR range: 1.3–2.8).
Conclusion:
Symptom severity and interference varied by phenotype, including between Veterans with stable and declining health. Ameliorating severe symptoms, particularly in the affective domain, could improve health trajectories following mTBI.
Keywords: traumatic brain injury, neurobehavioral manifestations, health trajectory, Veteran, health status, affective, phenotype
An estimated 17% of Veterans of post-9/11 conflicts have experienced traumatic brain injuries during military service.1 The majority of these injuries are classified as mild traumatic brain injury (mTBI),1,2 defined as an impact to the head that is accompanied by one or more of the following symptoms despite normal day-of-injury neuroimaging: a loss of consciousness for up to 30 minutes, changes in thinking or mental state, and/or post-traumatic amnesia.3,4 Typically, symptoms associated with mTBI subside in the first three months post-injury,5,6 however, there are possible long-term consequences including persistent headache, changes in vision and hearing, and chronic neck pain.4 Recent evidence suggests that the long-term outcomes of mTBI among service members are substantial. In a study of Veterans with combat blast-related mTBI, most experienced declines in function and quality of life between years one and five post-injury and fared worse than combat-deployed peers without mTBI.7 Furthermore, when mTBI co-occurs with post-traumatic stress disorder (PTSD) and/or depression, disability and negative employment outcomes are common.8
Our understanding of the long-term consequences of combat-related mTBI remains incomplete. One gap in knowledge relates to the factors associated with health trajectories among Veterans with mTBI. In a recent study, Pugh and colleagues identified five patient phenotypes among a large cohort of post-9/11 Veterans with mTBI: Moderately Healthy, Moderately Healthy+Decline, Mental Health, Polytrauma+Improvement, and Polytrauma.9 These subgroups were identified based on latent models using clinical and self-reported data from the Department of Veterans Affairs (VA) and Department of Defense (DoD). Veterans in the MoH group had relatively low probabilities of pain and of mental health and sensory conditions. Likewise, those in the MoH+Decline group had low probabilities of pain and other conditions initially but these probabilities increased the five years of follow-up. The Polytrauma group was characterized by higher probabilities of mental health conditions, pain, and other post-concussion symptoms throughout the five year period. Similar patterns were evident in the Polytrauma+Improvement group in year one, with a significant reduction noted in the probabilities of diagnoses over the five years of follow-up. The Mental Health group was defined by increasing probabilities of having mental health conditions diagnosed over the five year period.9 The health status and characteristics of these groups differed substantially from one another and, like another study by MacDonald and colleagues,7 suggest long-term and ongoing health burden associated with mTBI.
The current study sought to extend these findings by examining the relationship between neurobehavioral symptoms and multimorbidity among Veterans with combat-related mTBI. We were interested in determining whether neurobehavioral symptom experience – both the presence of and disruption from these symptoms – differed between latent groups of post-9/11 deployed Veterans with mTBI. We were particularly interested in whether we could distinguish between Veterans whose health tended to improve or decline in the years following their initial TBI screening through the VA since any differences identified might be useful targets for intervention to improve long-term health trajectories among these Veterans. We hypothesized that symptom burden would be lowest in the Moderately Healthy group given that they generally had the lowest probability of health conditions. We expected the Polytrauma+Improvement group to have a somewhat similar symptom burden compared to the Moderately Healthy group since we hypothesized this lower symptom burden may have partially explained their improved trajectory over time. We also hypothesized that symptoms would be significantly higher in (1) the Moderately Healthy+Decline group compared to the Moderately Healthy group and (2) the Polytrauma Phenotype compared to the Polytrauma+Improvement group. In other words, we expected that a higher symptom burden would be associated with poorer health trajectories over time. Finally, we hypothesized that the association between phenotype group and neurobehavioral symptoms would differ by sex given the differences reported in both symptom experience and health outcomes among male and female Veterans.10,11
Methods
Cohort
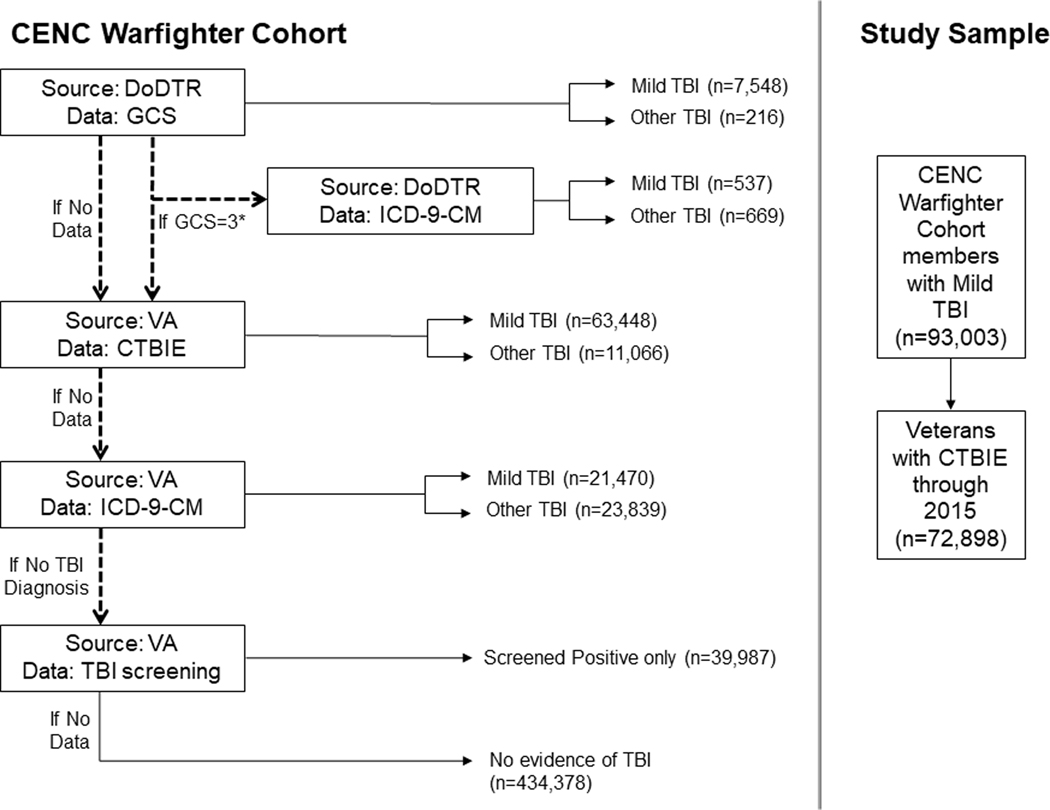
We used data from the Chronic Effects of Neurotrauma Consortium (CENC)9 Epidemiology study Warfighter Cohort, which comprises Veterans who were deployed in support of post-9/11 conflicts based on the Operations Enduring and Iraqi Freedom and Operation New Dawn (OEF/OIF/OND) roster file from the Department of Defense’s Defense Manpower Data Center. For those included in the OEF/OIF/OND roster file, we compiled and merged inpatient and outpatient healthcare data and pharmacy records from the United States Veterans Health Administration (VHA) between October 1, 2001-September 30, 2014, combined with data from the Department of Defense Trauma Registry (DoDTR) for those who were treated for trauma during deployment. The CENC Warfighter Cohort includes Veterans who first received VHA care between October 1, 2001 and September 30, 2011 and who received care at least once a year for at least three years during the study period. We further restricted the cohort to those who received care at least once after the VHA initiated the mandatory TBI screening program for post-9/11 Veterans program in 2007. Briefly, mTBI was classified using the hierarchical algorithm based on the most clinically relevant data available shown in Figure 1.
Figure 1.
Flow diagram for Chronic Effects of Neurotrauma (CENC) Warfighter cohort and this study.
For this analysis, we included Veterans who were classified as having mTBI based on the algorithm developed for the CENC Warfighter Cohort and completed the Comprehensive TBI Evaluation (CTBIE) through 2015.9 CTBIE data are limited to post-9/11 Veterans who screen positive for a possible TBI12 and who complete the CTBIE.13 A positive TBI screen is defined as a Veteran identifying at least one experience or symptom in each of the following four areas: (1) experiencing a blast, explosion, vehicular crash, fragment or bullet wound above the shoulders, or fall during deployment; (2) after the event, losing consciousness, being dazed or confused, not remembering the event, or having a concussion or head injury; (3) after the event having at least one of the following problems start or get worse: memory problems, balance problems or dizziness, light sensitivity, irritability, sleep problems, or headache; and (4) in the past week, experiencing any of the symptoms listed in item 3.13 If the Veteran screened positively for TBI they were referred on for the CTBIE which includes a physical examination, medical and psychiatric history, combat experience including etiology for potential concussive events and duration of loss/alteration of consciousness and posttraumatic amnesia, demographics, and the Neurobehavioral Symptom Inventory-22 (NSI).13 The date of mTBI is not included in the administrative data and therefore was not used in this study. This study received institutional review board approval from the University of Texas Health Science Center at San Antonio, the University of Utah, the Bedford VHA Hospital, and the Department of Defense (DoD) Human Research Protection Office with a waiver of informed consent.
Self-Reported Symptom Experience: Neurobehavioral Symptom Inventory-22
The NSI is a self-reported measure that uses a 5-point Likert scale to assess how much the respondent was disturbed by a list of 22 symptoms over the past 30 days.14–16 Response options range from 0, representing that a symptom is rarely or never present and that it is not a problem at all, to 4, indicating a very severe problem that is almost always present, has interfered with the respondent’s performance at work, school, or home, and that they feel they could not function without help.14
Based on work by Meterko et al.,17 we used the four-dimension subscales of the NSI identified by this group: vestibular, somatosensory, cognitive, and affective. The table in Supplemental Digital Content 1 lists which items are included in each subscale. In addition to the four domains, we also included a self-report measure of the overall impact of NSI symptoms on the Veteran’s life. Specifically, Veterans reported how much the various symptoms evaluated by the NSI interfered with their life in the past 30 days. This item was rated on the same 0–4 scale ranging from not at all to extremely.
We calculated the total NSI and subscale scores. We also were interested in classifying respondents into two groups based on experiencing relatively low and relatively high symptom burden. Consistent with work by Iverson and colleagues,10 we chose to dichotomize scores at 3 so that scores of 0–2.9 (no problem to moderate problem) indicate less symptom severity while scores of 3.0–4 (severe or very severe impacts) indicate more severe symptoms. Since the number of items in each subscale varies, we calculated the mean score accounting for the number of items so that all means remain on a 0–4 scale. We required that Veterans answer all items in a subscale in order to be included.
Based on concerns about over-reporting, researchers have developed the Validity-10 subset of the NSI, which includes symptoms not commonly reported among people with TBI and may therefore represent inaccurate reports.18 The Validity-10 is calculated by adding scores from the items that relate to the following symptoms: feeling dizzy, loss of balance, poor coordination, nausea, vision problems, hearing difficulty, noise sensitivity, change in taste/smell, difficulty making decisions, and slowed thinking. A score greater than of 22 or higher on these symptoms has been proposed to represent over-reporting. We calculated the Validity-10 score for all Veterans and excluded those with a score greater than 22.18
As noted above, the NSI is part of the CTBIE. It is routinely collected only at the time of the CTBIE exam; therefore, that we used only the NSI measured at the time of CTBIE in this study. On average, the CTBIE exam, including the NSI, was completed 25.8 months (SD=29.6) after the Veteran initiated VA care in the study sample. The median time to completion was 14 months.
Comorbidity Phenotype
A previous study using the CENC Warfighter Cohort used latent class analysis to identify five comorbidity phenotypes among Veterans with mTBI: Moderately Healthy (MoH), MoH+Decline, Polytrauma+Improvement, Polytrauma, and Mental Health.9 These latent groups were identified using indicators of the presence of various mental health conditions (i.e., depression, substance use disorder), post-concussive symptoms (i.e. anxiety, tinnitus, hearing loss, vestibular dysfunction, blurred vision), pain concerns, sleep problems, and obesity based on International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) diagnosis codes from inpatient and outpatient data in each year over a 5-year period beginning with the date of entry into VA care.9 The latent class model was developed using only one 5-year period for each Veteran, and each Veteran was assigned to the one phenotype group for which they had the highest probability of membership based on that 5-year period of data following their entry into VA care. The NSI was not used to develop the latent class model or to assign Veterans phenotype groups.
Covariates
We collected personal and military history information from VHA datasets. We included age at the time of CTBIE (19–29, 30–39, 40–49, 50–59, 60–69), sex (male, female), educational attainment (less than high school, high school or equivalent, some college, college graduate or graduate degree), marital status (married or not married), race and ethnicity (white, non-Hispanic; black, non-Hispanic; Asian, non-Hispanic; Native American or Pacific Islander, non-Hispanic; Hispanic; unknown). We also classified Veterans according to their service branch (Air Force, Army, Coast Guard, Navy, or Marines), component (active duty, National Guard or Reserve), rank (enlisted, warrant or officer), injury mechanism (blast only, non-blast only, blast and non-blast, no blast and no non-blast), and other TBI experience (TBI preceding and/or following deployment).
Statistical Analyses
We calculated and reported mean overall and scaled mean domain scores along with the percent of respondents whose average score was 3.0 or higher. We used logistic regression to estimate the odds of having severe or very severe symptoms associated with phenotype group membership, accounting for a variety of sociodemographic and injury characteristics: age group, race/ethnicity, sex, educational attainment, marital status, service branch, component, rank, injury mechanism, and other TBI history. We used the MoH phenotype as our reference group and therefore the odds ratios compare the odds of having severe/very severe symptoms in a given phenotype to the odds of having severe/very severe symptoms in the MoH group. Because we compared various symptom domains in separate models, we used a Bonferroni-corrected p-value to account for multiple comparisons. Since there were 5 different analyses (4 domains and interference) we used 0.05/5=0.01 as our alpha value. We tested each model for effect modification by sex, and considered a p-value of 0.05 to indicate significant differences between male and female Veterans. We conducted one sensitivity analysis in which we excluded respondents who had Validity-10 scores greater than 22. All analyses were conducted using SAS ® Version 9.2 (SAS Institute, Cary, NC).
Although the phenotype groups were created using longitudinal data, this study utilizes a cross-sectional design. Because we did not have the injury date and because the CTBIE exam was not necessarily completed at the beginning of the follow-up period used to assign Veterans to a phenotype group, we cannot be sure that the symptom measure preceded the Veteran’s trajectory. The timing of the NSI varied in relation to the five years of data collection for the latent class analysis and therefore we cannot disentangle whether the symptoms impacted the trajectories or the changing trajectories drove the symptoms. However, in most cases the CTBIE occurred within the first 2 years of follow-up given that most post-9/11 Veterans seen during the study period would have received TBI screening shortly after initiating VA care. Veterans in the Polytrauma and Polytrauma+Improve phenotypes tended to have the CTBIE earlier in their follow-up (i.e., 12 months, on average) than the MoH and MoH+Decline groups (mean 48 and 27 months, respectively), suggesting that people with more health concerns were evaluated more quickly.
Results
Of the 93,003 Veterans in the CENC Warfighter cohort with mTBI, 72,898 had data in the CTBIE. We required these Veterans not be missing age, sex, or phenotype group and therefore our final study sample was 71,934 (Figure 1). The majority of Veterans in the sample were men, younger than 40 years old, white, non-Hispanic who had served on active duty in the Army (Table 1). The demographic characteristics of Veterans across groups generally were similar, although the Polytrauma+Improvement and Mental Health phenotypes tended to be somewhat younger, were less likely to be married, had less educational attainment, and were more commonly in the Marines than those in the other comorbidity phenotypes.
Table 1.
Demographic and injury characteristics of post-9/11 Veterans with mTBI by comorbidity phenotype.
| Variable | Category | Moderately Healthy (MoH)(n=20,837) | Moderately Healthy + Decline (n=14,267) | Polytrauma Phenotype (n=9,288) | Polytrauma + Improvement (n=13,751) | Mental Health (n=14,753) |
|---|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | % (n) | ||
| Age at CTBIE | 19–29 | 45.4 (9455) | 47.9 (6830) | 49.4 (4591) | 60.8 (8360) | 65.6 (9674) |
| 30–39 | 30.9 (6436) | 30.5 (4350) | 30.3 (2810) | 23.7 (3258) | 24.6 (3630) | |
| 40–49 | 17.8 (3701) | 17.6 (2514) | 17.0 (1579) | 12.8 (1766) | 8.1 (1199) | |
| 50–59 | 5.4 (1120) | 3.6 (511) | 3.2 (297) | 2.4 (323) | 1.6 (236) | |
| 60–69 | 0.6 (125) | 0.5 (64) | 0.1 (11) | 0.3 (44) | 0.1 (14) | |
| Sex | Male | 93.9 (19573) | 93.7 (13365) | 93.0 (8640) | 95.7 (13154) | 95.8 (14135) |
| Female | 6.1 (1,264) | 6.3 (902) | 7.0 (648) | 4.3 (597) | 4.2 (618) | |
| Educational attainment | Less than high school | 1.4 (297) | 1.4 (201) | 1.5 (137) | 1.5 (202) | 1.7 (243) |
| High school or equivalent | 55.3 (11519) | 57.67 (8217) | 57.5 (5348) | 60.2 (8273) | 63.6 (9380) | |
| Some college | 34.4 (7174) | 34.0 (4857) | 34.5 (3205) | 32.2 (4434) | 30.5 (4495) | |
| College graduate or higher | 7.9 (1646) | 5.9 (837) | 5.4 (502) | 5.3 (725) | 3.5 (514) | |
| Unknown | 1.0 (201) | 1.1 (157) | 1.0 (96) | 0.9 (117) | 0.8 (121) | |
| Marital status | Married | 50.6 (10541) | 55.0 (7845) | 53.9 (5008) | 50.8 (6983) | 39.0 (5747) |
| Not married | 49.4 (10296) | 45.0 (6422) | 46.1 (4280) | 49.2 (6768) | 61.0 (9006) | |
| Unknown | 0.6 (134) | 0.8 (118) | 0.6 (59) | 0.5 (69) | 0.5 (80) | |
| Race/ ethnicity | White | 67.3 (14017) | 67.8 (9573) | 68.8 (6392) | 71.1 (9770) | 71.5 (10542) |
| Black | 14.3 (2979) | 14.1 (2013) | 13.3 (1231) | 11.7 (1613) | 12.9 (1897) | |
| Asian | 2.3 (480) | 2.1 (306) | 2.0 (188) | 2.5 (343) | 1.7 (246) | |
| Native American/ Pacific Islander | 1.6 (336) | 1.8 (261) | 2.0 (183) | 1.7 (239) | 1.9 (280) | |
| Hispanic | 13.6 (2823) | 13.4 (1917) | 13.5 (1257) | 12.2 (1679) | 11.6 (1709) | |
| Unknown | 1.0 (202) | 0.7 (99) | 0.4 (36) | 0.8 (107) | 0.5 (79) | |
| Service branch | Air Force | 3.7 (775) | 3.3 (472) | 3.8 (348) | 3.3 (456) | 2.2 (330) |
| Army | 72.9 (15184) | 75.1 (10712) | 75.5 (7015) | 69.2 (9515) | 72.2 (10652) | |
| Coast Guard or Navy | 6.1 (1270) | 5.6 (799) | 5.4 (504) | 5.3 (724) | 4.5 (661) | |
| Marine Corps | 17.3 (3608) | 16.0 (2286) | 15.3 (1421) | 22.2 (3056) | 21.1 (3110) | |
| Component | Active duty | 56.1 (11694) | 67.1 (9572) | 69.9 (6489) | 71.2 (9787) | 73.6 (10854) |
| National Guard or Reserve | 43.9 (9143) | 32.9 (4695) | 30.1 (2799) | 28.8 (3964) | 26.4 (3899) | |
| Rank | Enlisted | 95.3 (19860) | 96.5 (13774) | 97.4 (9046) | 97.0 (13343) | 98.4 (14515) |
| Warrant or officer | 4.7 () | 3.5 (493) | 2.6 (242) | 3.0 (408) | 1.6 (238) | |
| Injury mechanism | Blast only | 38.8 (8076) | 38.7 (5521) | 36.9 (3427) | 39.5 (5434) | 42.5 (6270) |
| Non-blast only | 24.9 (5188) | 20.4 (2916) | 18.2 (1686) | 18.2 (2503) | 16.6 (2444) | |
| Both blast and non-blast | 33.9 (7054) | 38.6 (5513) | 43.2 (4012) | 40.9 (5618) | 39.2 (5777) | |
| Neither | 1.2 (256) | 1.0 (146) | 1.2 (112) | 1.0 (137) | 1.0 (144) | |
| Missing | 1.3 (263) | 1.2 (173) | 0.6 (51) | 0.4 (59) | 0.8 (118) | |
| Other TBI experiences | TBI before deployment only | 18.7 (3904) | 15.7 (2233) | 15.7 (1456) | 18.1 (2484) | 16.5 (2431) |
| TBI after deployment only | 4.2 (873) | 5.2 (741) | 5.6 (519) | 4.0 (556) | 5.5 (815) | |
| TBI both before and after deployment | 2.6 (540) | 3.2 (462) | 3.5 (322) | 2.6 (359) | 3.5 (513) | |
| No TBI history | 67.8 (14130) | 69.0 (9842) | 68.1 (6322) | 69.1 (9504) | 67.8 (10007) | |
| Missing | 6.7 (1390) | 6.9 (989) | 7.2 (669) | 6.2 (848) | 6.7 (987) |
Post-9/11 Veterans include those who served in Operation Iraqi Freedom, Operation Enduring Freedom, and Operation New Dawn; the conflicts that occurred in Iraq and Afghanistan beginning in 2001.
mTBI: Mild traumatic brain injury
CTBIE: Comprehensive Traumatic Brain Injury Evaluation; the examination conducted by the VA that includes the Neurobehavioral Symptom Inventory
Symptom Severity and Interference by Phenotype
Veterans in the Polytrauma phenotype had the highest mean NSI overall (total) scores followed sequentially by Veterans in the MoH+Decline, Mental Health, Polytrauma+Improvement, and MoH groups (Table 2). This pattern generally held within each of the domains, although the MoH+Decline and Mental Health phenotypes occasionally alternated order in terms of severity. Within each phenotype, average symptom severity was highest within the affective domain followed by the cognitive domain, then somatosensory, and finally the vestibular domain. This trend was similar whether comparing mean scores or the percent of Veterans reporting severe or very severe symptom burden. The frequency of Veterans reporting severe or very severe symptoms (mean ≥3) varied considerably by domain. Fewer than one in ten experienced severe vestibular or somatosensory symptoms, between one in six and one in three experienced severe cognitive symptoms, and between one in five and one in two reported severe affective symptoms.
Table 2.
Average NSI overall and scaled domain and interference scores and the percent of Veterans in each group whose average scaled score was greater than or equal to 3, indicating severe or very severe symptoms on average, by phenotype group.
| NSI Domain | Comorbidity Phenotype | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Moderately Healthy | Moderately Healthy + Decline | Polytrauma Phenotype | Polytrauma + Improvement | Mental Health | ||||||
| Mean (SD) | % Mean ≥32 | Mean (SD) | % Mean ≥32 | Mean (SD) | % Mean ≥32 | Mean (SD) | % Mean ≥32 | Mean (SD) | % Mean ≥32 | |
| NSI Overall | 33.2 (16.8) | NA | 42.1 (16.3) | NA | 47.1 (15.6) |
NA | 36.9 (15.7) | NA | 40.9 (15.8) |
NA |
| Domain and Interference Scores | ||||||||||
| Vestibular subscale | 1.0 (0.8) | 2.6% | 1.3 (0.9) | 5.2% | 1.5 (0.9) | 7.1% | 1.1 (0.8) | 2.7% | 1.2 (0.8) | 3.3% |
| Somatosensory subscale | 1.2 (0.8) | 2.6% | 1.6 (0.8) | 4.9% | 1.7 (0.8) | 7.2% | 1.4 (0.7) | 2.7% | 1.4 (0.8) | 3.4% |
| Cognitive subscale | 1.7 (1.1) | 16.5% | 2.2 (1.0) | 28.6% | 2.5 (1.0) | 37.9% | 1.9 (1.0) | 19.3% | 2.2 (1.0) | 29.0% |
| Affective subscale | 2.0 (1.0) | 20.5% | 2.5 (0.9) | 35.9% | 2.8 (0.8) | 48.6% | 2.2 (0.9) | 24.6% | 2.6 (0.9) | 39.6% |
| Neurobehavioral symptom interference | 2.0 (0.9) | 28.4% | 2.4 (0.9) | 45.1% | 2.7 (0.8) | 56.3% | 2.2 (0.9) | 34.5% | 2.5 (0.9) | 46.2% |
NSI: Neurobehavioral Symptom Inventory-22
Notes: Mean subscale scores are transformed to account for the number of items in the subscale; therefore, the range is 0–4, as on individual items. Pain is included in the somatosensory subscale and also reported separately.
Average scores relating to how much the neurobehavioral symptoms evaluated in the NSI interfered with the Veteran’s daily life followed the same pattern as the NSI scores themselves. MoH Veterans had the lowest scores and Polytrauma Veterans reported the greatest impact of neurobehavioral symptoms on daily life. Across phenotype groups, a substantial proportion of Veterans reported severe interference resulting from symptoms, ranging from 28% of the MoH group to 56% of the Polytrauma phenotype.
Differences between Phenotype Pairs of Interest
We found no evidence of effect modification by sex (p>0.05 for all interactions between sex and phenotype). Our first hypothesis was that the MoH and Polytrauma+Improvement groups would have similar symptom burden, which we found to be true: compared to Veterans in the MoH phenotype, those in the Polytrauma+Improvement phenotype generally had similar odds of severe symptoms after accounting for a variety of sociodemographic and injury characteristics (Table 3). Our other hypotheses compared two pairs of phenotypes: MoH vs. MoH+Decline and Polytrauma vs. Polytrauma+Improvement. Relative to the MoH phenotype, Veterans in the MoH+Decline phenotype had about twice the odds of experiencing severe/very severe symptom burdens across all domains (OR range: 2.0–2.2) as well as of the overall symptom interference (OR=1.8). We calculated estimates comparing the two Polytrauma groups directly and found the Polytrauma phenotype group was much more likely to report severe affective (OR=2.8, 95%CI: 2.6–3.0), vestibular (OR=2.6, 95%CI: 2.4–2.9), somatosensory (OR=2.5, 95CI: 2.2–2.8), and cognitive (OR=2.4, 95%CI: 2.3–2.6) symptoms and symptom interference (OR=1.7, 95%CI: 1.6–1.8) compared to the Polytrauma+Improvement phenotype.
Table 3.
Logistic regression results estimating the association between Neurobehavioral Symptom Inventory (NSI) subscale scores and group membership.
| Comorbidity Phenotype | Severe or Very Severe Symptoms (Average Scaled NSI Score ≥3.0) | ||||
|---|---|---|---|---|---|
| Vestibular | Somato-sensory | Cognitive | Affective | Interference | |
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Moderately Healthy | 1.0 (Ref) |
1.0 (Ref) |
1.0 (Ref) |
1.0 (Ref) |
1.0 (Ref) |
| Moderately Healthy + Decline | 2.1* (1.8–2.4) |
2.0* (1.8–2.3) |
2.0* (1.9–2.1) |
2.2* (2.0–2.3) |
1.9* (1.8–2.0) |
| Polytrauma + Improvement | 1.2 (1.0–1.4) |
1.2 (1.1–1.4) |
1.2* (1.2–1.3) |
1.3* (1.2–1.4) |
1.3* (1.3–1.4) |
| Polytrauma Phenotype | 2.9* (2.6–3.3) |
2.9* (2.6–3.3) |
3.0* (2.9–3.2) |
3.6* (3.4–3.8) |
2.8* (2.7–3.0) |
| Mental Health | 1.5* (1.3–1.7) |
1.5* (1.4–1.8) |
2.1* (2.0–2.3) |
2.6* (2.5–2.8) |
2.1* (2.0–2.2) |
p<0.0001
OR: odds ratio
CI: confidence interval
Ref: Reference group
All models are adjusted for: age group at the time of NSI (30–39, 40–49, 50–59, 60–69 years), race/ethnicity (white, non-Hispanic; black, non-Hispanic; Asian, non-Hispanic; Native American or Pacific Islander, non-Hispanic; Hispanic; unknown), sex (men, women), educational attainment (less than high school, high school or equivalent, some college, college graduate or graduate degree), marital status (married or not), service branch (Air Force, Army, Coast Guard or Navy, Marines), component (active duty, National Guard or Reserve), rank (enlisted, warrant or officer),injury mechanism (blast only, non-blast only, blast and non-blast), and other TBI history (no other TBI, other TBI pre-deployment, other TBI post-deployment, other TBI both pre- and post-deployment).
Colors indicate magnitude of difference between Moderately Healthy Veterans and comparison group. Green represents similar (OR: 0.7–1.4), yellow indicates small differences (OR: 1.5–1.9), light red indicates moderate differences (OR: 2.0–2.4), and dark red indicates large differences (OR: 2.5 or higher).
Other Associations between Phenotype and Symptom Severity
Compared to Veterans in the MoH phenotype, the Mental Health phenotype had modestly increased odds of severe symptoms in the vestibular and somatic domains (OR=1.5) and more substantial increases in the odds of severe cognitive and affective symptoms (OR=2.2 and 2.6, respectively). Veterans in the Polytrauma phenotype were substantially more likely than MoH phenotype Veterans to have severe symptoms across all domains (OR range: 2.9–3.6) and also more likely to report severe interference from these symptoms (OR=2.2). All differences reported were statistically significant (p<0.0001).
Covariate Associations
Several of the covariates included in the models were statistically significantly associated with experiencing severe or very severe symptom burden. Across domains, older Veterans, women, Veterans who identified as Black or Hispanic, Veterans who had experienced blast and/or non-blast injuries, and Veterans who had other TBIs following deployment were generally more likely to report greater symptom burdens. The full model results including these covariates is available in Supplemental Table 2.
Sensitivity Analysis
Overall, 9,332 Veterans or 12.8% of the sample had Validity-10 scores greater than 22, suggesting possible symptom over-reporting. There was variability in the proportion of respondents with high Validity-10 scores across phenotypes: 8.3% of MoH, 9.6% of Polytrauma+Improvement, 13.0% of Mental Health, 16.1% of MoH+Decline, and 22.3% of Polytrauma phenotypes. After excluding these Veterans from the analysis, the odds ratios for severe or very severe symptoms were generally attenuated but the patterns were similar to those observed in the full sample (Supplemental Table 3). Specifically, the point estimates were smaller in the vestibular and somatosensory domains, which are the domains where most of the Validity-10 items come from. Point estimates were similar to those in the main analysis in the cognitive domain, and virtually unchanged in the affective domain across all phenotypes.
Discussion
We found substantial variation in the severity of symptoms among post-9/11 Veterans with mTBI based on the comorbidity phenotype to which they belonged. While it was not surprising that Veterans with better health trajectories (i.e., MoH and Polytrauma+Improvement) reported fewer symptoms related to mTBI, the association between symptom experience and health trajectory was quite strong. We found that Veterans in the MoH+Decline and Polytrauma phenotypes were more affected by neurobehavioral symptoms across all domains – vestibular, somatosensory, cognitive, and affective – compared to MoH and Polytrauma+Improve phenotypes, respectively. In both cases, the largest point estimate was for symptoms in the affective domain. This is consistent with previous work that co-occurring mental health conditions like PTSD account for much of the symptom burden reported by Veterans with mTBI,15 and suggests that clinical management approaches focusing on these affective symptoms could reduce symptom severity. Contrary to our expectation, the relationship between phenotype and symptom disruption was consistent across male and female Veterans.
This study extends previous work to identify potential links between severe symptom burden and health trajectories. Our finding that substantial symptom burden exists among Veterans with mTBI, even those whose injury was not recent, is consistent with several recent studies showing long-term impacts of mTBI among Veterans.7,19–21 It may be possible to improve health trajectories by clinically addressing and tracking severe symptoms captured by the NSI and focusing on treating affective symptoms like fatigue, sleep problems, anxiety, depressed mood, and irritability. While these affective symptoms could result from other diagnoses like depression and post-traumatic stress disorder,22 both of which are common in post-9/11 Veterans with mTBI,8,23 targeting the symptoms could nonetheless impact a Veteran’s health trajectory, regardless of co-occurring diagnoses. There is limited evidence, however, to guide clinicians on the best interventions or treatment approaches for complex conditions that co-occur with mTBI.24,25 While promising interventions for co-occuring mTBI and conditions like PTSD and sleep disorders have recently been described or proposed26,27, these data suggest that additional research into evidence-based approaches for these Veterans is needed. It is possible that other, more urgent health needs are being addressed among Veterans and their affective symptoms are not being addressed as early in the treatment process. It was not possible to describe the details of care in this study, but it would be helpful to do so in the future to form evidence-based practice recommendations for improving trajectories among Veterans with mTBI.
When we evaluated scores across phenotype groups using the Validity-10 measure, we found a lower percentage of Veterans with potential over-reporting in the relatively healthy groups (MoH and Polytrauma+Improvement) than in the other phenotypes. Particularly striking was the observation that more than one in five Veterans Polytrauma phenotype were excluded from the analysis because of high Validity-10 scores. Their high symptom burden is not surprising given the broad array of symptoms associated with polytrauma. However, this result suggests that high Validity-10 scores occur more commonly among Veterans with more substantial comorbidity. We encourage researchers to consider that using the Validity-10 cut point of 22 with the NSI may inadvertently bias samples by eliminating Veterans with the most complex injury histories and health care needs.
This study has several limitations. The first is its cross-sectional nature. Specifically, the latent groups were constructed using multiple years of data that could have included the time of the CTBIE and therefore the NSI measure. Another limitation is that we used depression and PTSD diagnoses in constructing the latent classes and therefore did not test for effect modification by these conditions or separately adjust for them.8,22,23 Finally, these data represent only Veterans who used the VA system for health care and therefore may not represent the entire population of post-9/11 veterans who experienced mTBI. The strengths of this study include the large sample size that is generally representative of deployed troops,8,28 the combination of self-reported and clinical measures, and the use of a common and validated measure of symptom burden.
Conclusion
The variation in symptom severity and the interference of these symptoms based on Veterans’ health trajectory suggests a relationship between mTBI-related symptoms and health status and outcomes. Longitudinal research is needed to determine whether the symptom domain or severity can reliably indicate Veterans’ future health trajectories and also to more fully assess how changes in neurobehavioral symptoms impact changes in these trajectories. Timely clinical symptom management may be one approach to influencing health trajectories to prevent declines in well-being among Veterans with mTBI, regardless of whether they are otherwise relatively healthy or have substantial comorbidity.
Supplementary Material
Funding source:
This work was supported by the Chronic Effects of Neurotrauma Consortium (CENC) by joint U.S. Department of Defense W81XWH-13-2-0095-04 (Yaffe) and the U.S. Department of Veterans Affairs funds, I01CX001246 (Pugh)
Footnotes
Conflicts of interest: None declared
References
- 1.Lindquist LK, Love HC, Elbogen EB. Traumatic Brain Injury in Iraq and Afghanistan Veterans: New Results from a National Random Sample Study. J Neuropsychiatry Clin Neurosci. 2017;29(3):254–259. doi: 10.1176/appi.neuropsych.16050100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DoD Worldwide Numbers for TBI. DVBIC. https://dvbic.dcoe.mil/dod-worldwide-numbers-tbi. Published June 9, 2016. Accessed June 26, 2019. [Google Scholar]
- 3.The Management of Concussion-mild Traumatic Brain Injury, Working Group. VA/DoD Clinical Practice Guideline for the Management of Concussion-Mild Traumatic Brain Injury. Department of Veterans Affairs and Department of Defense; 2016:133. https://www.healthquality.va.gov/guidelines/Rehab/mtbi/mTBICPGFullCPG50821816.pdf. Accessed June 26, 2019. [Google Scholar]
- 4.US Department of Health & Human Services; Centers for Disease Control (CDC); National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem: (371602004–001). 2003. doi: 10.1037/e371602004-001 [DOI] [Google Scholar]
- 5.Carroll LJ, Cassidy JD, Peloso PM, et al. Prognosis for mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med. 2004;(43 Suppl):84–105. [DOI] [PubMed] [Google Scholar]
- 6.Iverson GL. Outcome from mild traumatic brain injury. Curr Opin Psychiatry. 2005;18(3):301–317. doi: 10.1097/01.yco.0000165601.29047.ae [DOI] [PubMed] [Google Scholar]
- 7.Mac Donald CL, Barber J, Jordan M, et al. Early Clinical Predictors of 5-Year Outcome After Concussive Blast Traumatic Brain Injury. JAMA Neurol. 2017;74(7):821–829. doi: 10.1001/jamaneurol.2017.0143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972 [DOI] [PubMed] [Google Scholar]
- 9.Pugh MJ, Swan AA, Amuan ME, et al. Deployment, suicide, and overdose among comorbidity phenotypes following mild traumatic brain injury: A retrospective cohort study from the Chronic Effects of Neurotrauma Consortium. PloS One. 2019;14(9):e0222674. doi: 10.1371/journal.pone.0222674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iverson KM, Hendricks AM, Kimerling R, et al. Psychiatric diagnoses and neurobehavioral symptom severity among OEF/OIF VA patients with deployment-related traumatic brain injury: a gender compa... - PubMed - NCBI. Women’s Health Issues. 2011;21:S210–S217. doi:doi: 10.1016/j.whi.2011.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cogan AM, McCaughey VK, Scholten J. Gender Differences in Outcomes after Traumatic Brain Injury among Service Members and Veterans. PM R. August 2019. doi: 10.1002/pmrj.12237 [DOI] [PubMed] [Google Scholar]
- 12.Donnelly KT, Donnelly JP, Dunnam M, et al. Reliability, Sensitivity, and Specificity of the VA Traumatic Brain Injury Screening Tool. The Journal of Head Trauma Rehabilitation. 2011;26(6):439. doi: 10.1097/HTR.0b013e3182005de3 [DOI] [PubMed] [Google Scholar]
- 13.Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1184 - Screening and evaluation of traumatic brain injury (TBI) in Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans. April 2017. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=5376. Accessed March 24, 2019.
- 14.Cicerone KD, Kalmar K. Does premorbid depression influence post-concussive symptoms and neuropsychological functioning? Brain Inj. 1997;11(9):643–648. [DOI] [PubMed] [Google Scholar]
- 15.Belanger HG, Kretzmer T, Vanderploeg RD, French LM. Symptom complaints following combat-related traumatic brain injury: relationship to traumatic brain injury severity and posttraumatic stress disorder. J Int Neuropsychol Soc. 2010;16(1):194–199. doi: 10.1017/S1355617709990841 [DOI] [PubMed] [Google Scholar]
- 16.Soble JR, Silva MA, Vanderploeg RD, et al. Normative Data for the Neurobehavioral Symptom Inventory (NSI) and post-concussion symptom profiles among TBI, PTSD, and nonclinical samples. Clin Neuropsychol 2014;28(4):614–632. doi: 10.1080/13854046.2014.894576 [DOI] [PubMed] [Google Scholar]
- 17.Meterko M, Baker E, Stolzmann KL, Hendricks AM, Cicerone KD, Lew HL. Psychometric assessment of the Neurobehavioral Symptom Inventory-22: the structure of persistent postconcussive symptoms following deployment-related mild traumatic brain injury among veterans. J Head Trauma Rehabil. 2012;27(1):55–62. doi: 10.1097/HTR.0b013e318230fb17 [DOI] [PubMed] [Google Scholar]
- 18.Vanderploeg RD, Cooper DB, Belanger HG, et al. Screening for postdeployment conditions: development and cross-validation of an embedded validity scale in the neurobehavioral symptom inventory. J Head Trauma Rehabil. 2014;29(1):1–10. doi: 10.1097/HTR.0b013e318281966e [DOI] [PubMed] [Google Scholar]
- 19.Mortera MH, Kinirons SA, Simantov J, Klingbeil H. Long-Term Neurobehavioral Symptoms and Return to Productivity in Operation Enduring Freedom/Operation Iraqi Freedom Veterans With and Without Traumatic Brain Injury. Arch Phys Med Rehabil. 2018;99(2S):S50–S57. doi: 10.1016/j.apmr.2016.11.026 [DOI] [PubMed] [Google Scholar]
- 20.Pugh MJ, Swan AA, Carlson KF, et al. Traumatic Brain Injury Severity, Comorbidity, Social Support, Family Functioning, and Community Reintegration Among Veterans of the Afghanistan and Iraq Wars. Arch Phys Med Rehabil. 2018;99(2S):S40–S49. doi: 10.1016/j.apmr.2017.05.021 [DOI] [PubMed] [Google Scholar]
- 21.Swan AA, Amuan ME, Morissette SB, et al. Long-term physical and mental health outcomes associated with traumatic brain injury severity in post-9/11 veterans: A retrospective cohort study. Brain Inj. 2018;32(13–14):1637–1650. doi: 10.1080/02699052.2018.1518539 [DOI] [PubMed] [Google Scholar]
- 22.Andrews RJ, Fonda JR, Levin LK, McGlinchey RE, Milberg WP. Comprehensive analysis of the predictors of neurobehavioral symptom reporting in veterans. Neurology. 2018;91(8):e732–e745. doi: 10.1212/WNL.0000000000006034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DePalma RG. Combat TBI: History, Epidemiology, and Injury Modes. In: Kobeissy FH, ed. Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects. Frontiers in Neuroengineering. Boca Raton (FL): CRC Press/Taylor & Francis; 2015. http://www.ncbi.nlm.nih.gov/books/NBK299230/. Accessed March 24, 2019. [Google Scholar]
- 24.Defense and Veterans Brain Injury Center. Research Review on Mild Traumatic Brain Injury and Posttraumatic Stress Disorder; 2018:19. https://dvbic.dcoe.mil/sites/default//files/dvbic_research_research-review_mildtbi-ptsd_v2.0_2018-06-08_508.pdf. Accessed January 1, 2020.
- 25.Otis J, McGlinchey RE, Vasterling, Jennifer J, Kerns R. Complicating Factors Associated with Mild Traumatic Brain Injury: Impact on Pain and Posttraumatic Stress Disorder Treatment. J Clin Psychol Med Settings. 2011;18(2):145–154. doi: 10.1007/s10880-011-9239-2 [DOI] [PubMed] [Google Scholar]
- 26.Wolf G, Mauntel G, Kretzmer T, et al. Comorbid Posttraumatic Stress Disorder and Traumatic Brain Injury: Generalization of Prolonged-Exposure PTSD Treatment Outcomes to Postconcussive Syptoms, Cognition, and Self-Efficacy in Veterans and Active Duty Service Members. J Head Trauma Rehabil. 2018;33(2):E53–E63. doi: 10.1097/HTR.0000000000000344 [DOI] [PubMed] [Google Scholar]
- 27.Wickwire E, Schnyer D, Germain A, et al. Sleep, Sleep Disorders, and Circadian Health following Mild Traumatic Brain Injury in Adults: Review and Research Agenda. J Neurotrauma. 2018;35(22):2615–2631. doi: 10.1089/neu.2017.5243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Institute of Medicine (US) Committee on the Initial Assessment of Readjustment Needs of Military Personnel V. OPERATION ENDURING FREEDOM AND OPERATION IRAQI FREEDOM: DEMOGRAPHICS AND IMPACT. National Academies Press (US); 2010. https://www.ncbi.nlm.nih.gov/books/NBK220068/. Accessed June 28, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.