Abstract
Background
Two surgical techniques were compared : Standard BIO-RSA, performed with a glenoid eccentric reaming along with a cylindric bone graft augmentation vs. the Angled BIO-RSA, performed with a glenoid concentric reaming and a defect correction with an angled bone graft.
Methods
Patients undergoing RSA from January 2016 to April 2019, with one of the two techniques being performed, were retrospectively reviewed. Glenoids were classified according to Favard. Clinical (Constant-Murley, VAS and ROM) and radiographic (superior tilt correction) data were collected pre-operatively and at 12 months post-operatively.
Results
141 shoulders were included. Angled BIO-RSA group showed statistically significant better outcomes in terms of forward flexion (149.9° Vs 139.3°) and abduction (136.4° Vs 126.7°). The use of an Angled BIO-RSA showed a statistically significant better superior tilt correction (1.252° Vs 4.09°). Angled BIO-RSA, leads to a better inclination correction and a mean postoperative tilt value inferior to 5° in E1 and E3 differently from standard BIO-RSA.
Discussion
Both techniques were able to correct glenoid superior inclination with excellent postoperative short-term results. However, angled BIO-RSA technique appears to be more effective in ensuring a correct inclination of the prosthetic glenoid component with better clinical outcomes.
Keywords: RSA angle, reverse shoulder arthroplasty, tilt, glenoid inclination, BIORSA, angled BIO-RSA
Introduction
Appropriate positioning of glenoid baseplate in terms of inclination and version is one of the most relevant factors to succeed in Reverse Total Shoulder Arthroplasty (RSA) surgery. 1
Improper management of the glenoid bone defect might lead to a wrong positioning of the baseplate.
This would increase the risk of implant failure, instability and scapular notching resulting in kinematics alterations and reduced clinical outcomes.2–6
Favard classified the four most common patterns of coronal glenoid erosion: absent (E0), central concentric (E1), eccentric superior (E2 and E3), and inferior (E4) erosion. 7 Boileau et al. 8 showed that Favard's E1 and E3 subtypes 9 are both the most common and difficult glenoid morphotypes to manage due to a greater risk of underestimating the correction. Several RSA baseplates, due to their length and shape, have to be placed in the lower part of the glenoid surface to improve deltoid tensioning and reduce the risk of scapular notching. 10 It has been shown that the glenosphere baseplate should be placed perpendicular to both the supraspinatus fossa and the Friedman line.2,11–13 Moreover, literature reports how the Reverse Shoulder Arthroplasty angle (RSA angle) appears to be the best parameter to assess the lower glenoid surface inclination preoperatively resulting much more accurate than Total shoulder Arthroplasty - TSA (or β) angle to provide a measure of the superior glenoid inclination, especially for E1 and E3 glenoids. 2
Several procedures have been described to manage glenoid bone defect and implant the baseplate with the correct inclination, nevertheless, the optimal method to be used in RSA surgery is still controversial.1,14–19
Recent studies report how glenoid lateralization (both bony or metallic), increasing the remaining rotator cuff and deltoid tension, maximizes impingement free arc Range of Motion (ROM) and might lead to better clinical outcomes and smaller risk of instability.20–24
There were two purposes of the present study. The first one was to evaluate the differences between the preoperative TSA and RSA angle in measuring the glenoid inclination in shoulders classified according to Favard.
The second purpose was to evaluate and compare two different techniques of managing glenoid inclination: Eccentric reaming/Standard BIO-RSA (Bony Increased Off-set) vs Angled BIO-RSA in terms of postoperative inclination correction and clinical outcomes.
Our hypothesis was that RSA angle show a significantly greater value than TSA angle in E1 and E3 glenoids and angled BIO-RSA leads to both better inclination correction and postoperative clinical outcomes.
Methods
This retrospective comparative cohort study has been performed at the Policlinico Universitario Campus Bio-Medico analysing the hospital database to quantify the outcomes of rTSA carried out with the addition of Standard or Angled BIO-RSA between January 2016 and April 2019. The Aequalis Ascend Flex Reversed Shoulder system prosthesis with a 145° onlay short curved stem (Wright Medical Group – Memphis,TN) was used for each patient.
Inclusion criteria were the following: age range from 45 to 85 yrs, patients undergoing first rTSA implantation, diagnosis of cuff tear arthropathy (CTA), preoperative CT available, glenoid retroversion < 10°, use of BIO-RSA, absence of neoplastic diseases or active infection at the treated site and no history of proximal humeral fracture.
The exclusion criteria were the following: cervical radiculitis (cervical spine MRI was performed in case of a related neck disease suspected), previous shoulder surgery, psychiatric or systemic inflammatory disease, post-traumatic avascular necrosis, diagnosis of proximal humerus fracture, BMI > 35, axillary nerve injury and a deltoid muscle, evaluated clinically, not functioning properly.
Based on the technique used for glenoid correction, patients have been divided into two groups: Standard BIO-RSA group and Angled BIO-RSA group.
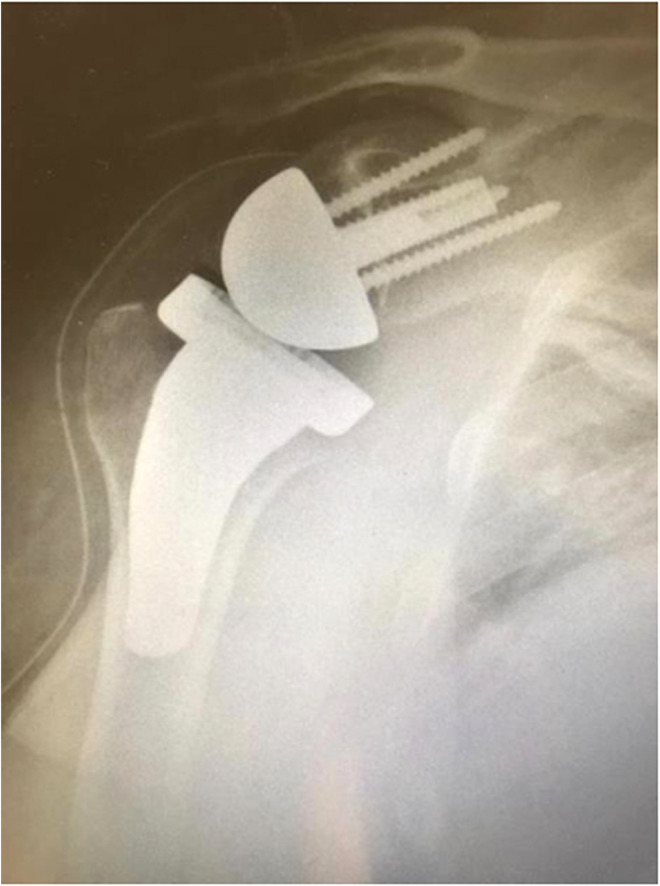
The first group was treated with a Standard BIO-RSA (cylindric glenoid bone graft) along with an eccentric reaming. The second group treatment included a concentric reaming and the correction of the inclination with an angled bone graft (Angled BIO-RSA). (Figure 1)
Figure 1.
A postoperative angled BIO-RSA radiograph.
From 2016 to the beginning of 2018 all the RSA included in this study were carried out with eccentric reaming and Standard BIO-RSA. After that, the senior author decided to shift and start using the Angled BIO-RSA procedure. Patients were informed about the surgical technique performed. The following description of the surgical techniques were standardized for both groups of patients. The patient was placed in a beach-chair position. The deltopectoral approach was preferred. Both the coracoacromial ligament and the subscapularis tendon were incised.
A 2.5 cm diameter autologous bone graft was harvested from the humeral head using two different cut guides depending on the technique used. Standard BIO-RSA grafts had a cylindrical shape and a thickness of 1 cm; whereas angled BIO-RSA grafts had an asymmetric thickness with a 12° angle (12.5 mm thick) and were carried out using an oblique cutting guide.
Our aim was to place the baseplate perpendicular to the line of the supraspinatus floor.2,8 In both groups a 10 ° inferior tilted hole guide was used to place the pin in the glenoid.
In Standard BIO-RSA group, eccentric reaming of the glenoid bone surface was performed in order to correct abnormal inclination.
Conversely, in Angled BIO-RSA group the reamer was used to abrade the glenoid until the subchondral plate was reached usually at a depth of approximately 2 to 4 mm.
The glenoid graft-baseplate was placed and fixed as low as possible to reduce the risk of notching.
A trial glenosphere is introduced. After the reduction, the stability was tested. The arm was placed in various degrees of rotation, flexion and abduction. When stability was satisfactory, the definite glenosphere was placed on the metaglene and the chosen humeral component was placed in the humerus.
When possible, without needing an excessive lateral traction, the subscapularis tendon was repaired.
The deltopectoral interval was sutured over a closed suction drainage system. The subcutaneous tissue and skin were closed routinely. All surgical procedures were performed by the senior author.
A power analysis was performed considering a 5.7point difference (MCID) in the Constant-Murley score (CS) between the groups. 25
Preoperative radiological evaluation was performed with both radiographs (AP projection) and CT scan.
TSA angle, glenoid retroversion and posterior humeral subluxation have been analysed using the BluePrint software (Imascap - Plouzané, France), whereas the Reverse Shoulder Arthroplasty (RSA) angle was calculated on 2D CT scans.
Therefore, preoperative MRI scans were examined for all patients, in order to confirm the diagnosis of Rotator Cuff Arthropathy (RCA). Shoulders were classified according to Favard 7 in four patterns of glenoid erosion.
TSA and RSA angle correction was evaluated post-operatively with a true antero-posterior shoulder projection (Grashey View) radiograph at 12 months. Patients have been assessed using the CS, the Visual Analogue Scale (VAS) and ROM in terms of abduction, forward flexion, internal and external rotation (at 0 ° and 90 ° of abduction) pre and post-operatively at 12 months of follow-up. All those values were compared between the groups in terms of statistical significance and MCID.
Descriptive statistics, including means and standard deviations, were reported for outcome variables. After assessment of the distribution with the Kolmogorov-Smirnov test, unpaired t tests and MannWhitney U tests were respectively used to compare parametric and nonparametric variables. Mean and standard deviation (SD) were calculated. A p value of.05 was referred to as statistically significant. SPSS version 17.0 (SPSS, Chicago, Illinois) was used to analyse data.
The graphical representations were performed using the GraphPad Prism version 8.0.2 software.
Results
A total of 141 shoulders belonging to 135 patients, 97 women and 38 men, were included (6 patients were operated bilaterally). The mean age and BMI of the included patients was respectively 69.1 ± 9.4 yrs and 26.9 ± 4.5 yrs. The mean follow-up was 24.5 + /- 11.5 months with a minimum follow-up of 12 months. Eighty-two (58,2%) and fifty-nine (41,8%) shoulders were treated using respectively a Standard and an Angled BIO-RSA. No significant differences in terms of age, gender and BMI were found comparing the demographic data of the two groups (Table 1).
Table 1.
Demographics and perioperative data of the two groups of patients.; BMI: body mass index; M/F: male/female; R/L: right/left; SD: standard deviation.
| Standard BIO-RSA | Angled BIO-RSA | p value | |
|---|---|---|---|
| Shoulders | 82 | 59 | |
| Age (mean ± SD) | 69.87 ± 7.69 | 68.15 ± 6.46 | .166 |
| Gender (M/F) | 21/57 | 17/40 | .751 |
| BMI (mean ± SD) | 26.40 ± 4.51 | 27.70 ± 1.57 | .372 |
| Side (R/L) | 56/26 | 38/21 | .629 |
Therefore, E1 (50.4%) and E3 (29.8%) were the most common glenoid subtypes diagnosed among the shoulders treated (80.2%). Those two glenoid subtypes have shown the greatest preoperative difference between RSA and TSA angle as shown in Table 2.
Table 2.
Difference between RSA and TSA angle in each type of glenoid classified according to favard.
| TSA Angle (°) | RSA Angle (°) | RSA - TSA (°) | |
|---|---|---|---|
| E0 (n = 19) | 5.67 ± 2.85 | 12.20 ± 3.10 | 6.53 ± 1.20 |
| E1 (n = 71) | 8.05 ± 3.20 | 20.41 ± 4.02 | 12.36 ± 3.42 |
| E2 (n = 9) | 15.64 ± 4.68 | 17.82 ± 4.40 | 2.18 ± 4.40 |
| E3 (n = 42) | 16.25 ± 3.63 | 24.93 ± 5.74 | 8.68 ± 4.75 |
No statistically significant difference was found comparing the two groups preoperative RSA values (20.01 ± 6.14° versus 22.14 ± 6.65°; p:.053). Therefore, the values of preoperative glenoid version and posterior humeral subluxation did not show significant differences between the two groups.
Postoperative RSA angle showed a significant smaller value in Angled BIO-RSA group (1.252 ± 6.14° Vs. 4.09 ± 8.85°; p:.036) as shown in Figure 2.
Figure 2.
Comparison of post-operative tilt between angled Bio-RSA and Reaming + Standard Bio-RSA.
A postoperative RSA value higher than 0° has been considered as uncorrected, whereas a postoperative RSA between −10° and 0° has been considered as corrected. Comparing the two groups in terms of the ratio corrected /uncorrected (C/U) postoperative glenoid inclination, the Standard BIO-RSA group showed a smaller significant value (p:.028) as shown in Figure 3.
Figure 3.
Two groups comparison in terms of corrected over uncorrected (C/U) postoperative glenoid inclination.
The Postoperative TILT values classified in terms of glenoid inclination subtypes are shown in Figure 4.
Figure 4.
Comparison of postoperative TILT between the two techniques, in terms of favard glenoid classification.
The Standard BIO-RSA group leaded to a smaller (closer to 0°) postoperative RSA angle in E0 (p:.543) and E2 (p:.640), whereas the Angled BIO-RSA leaded to a smaller postoperative RSA angle in E1 (p:.089) and E3 (p:.307). However, both those results were non statistically significant.
In relation to the surgical procedure performed, no significant differences were recorded comparing the two groups in terms of liner thickness, humeral stem, baseplate and glenosphere size.
Preoperative clinical outcomes comparison did not show any significant difference between the two groups. Both Angled and Standard BIO-RSA groups showed a significant improvement after surgery in terms of Constant score, VAS and ROM (p < .001).
The comparison of clinical outcomes at latest follow-up are shown in Table 3.
Table 3.
Post operative comparison of the two techniques of correcting glenoid inclination in terms of ROM (range of motion), VAS (visual analogue scale) and CS (constant–murley) score. Extrarotation 0° : Extrarotation at 0 ° of Abduction; Extrarotation 90°: Extrarotation at 90° of Abduction; SD: Standard Deviation.
| Standard BIO-RSA | Angled BIO-RSA | p value | |
|---|---|---|---|
| VAS (mean ± SD) | 2.17 ± 2.47 | 1.69 ± 1.95 | .572 |
| Constant Score (mean ± SD) | 64.40 ± 13.78 | 67.78 ± 9.88 | .110 |
| Flexion (mean ± SD) | 139.3° ± 26.79° | 149.9° ± 25.25° | .019 * |
| Abduction (mean ± SD) | 126.7° ± 29.27° | 136.4° ± 24.21° | .040 * |
| Extrarotation 0° (mean ± SD) | 37.20° ± 17.61° | 32.88° ± 14.83° | .128 |
| Extrarotation 90° (mean ± SD) | 52.74° ± 26.02° | 45.85° ± 24.79° | .116 |
| Intrarotation | 3.87 ± 2.3 | 4.03 ± 1.8 | .07 |
Despite CS, VAS and part of ROM (Extrarotation at 0°/90° and Intrarotation) showed similar values, forward flexion and abduction were significant higher in Angled BIO-RSA group (149.9 ± 25.3° Vs. 139.3 ± 26.8°, p:.019; 136.4 ± 24.2° Vs. 126.7 ± 29.3°, p:.040).
Actually, among those two features, only active abduction reached a Minimal Clinically Important Difference (MCID). 25
Three cases of infection and two fractures (acromion and scapular spine) were recorded in Standard BIO-RSA group. Two cases of infection and one acromial fracture were recorded in Angled BIO-RSA group. No cases of post-operative instability or aseptic loosening have been recorded.
The overall scapular notching rate, considering all subtypes, did not show statistically significant differences between the groups (13 and 9 respectively in Standard and Angled BIO-RSA group).
Discussion
The most important finding of this study is that the use of an Angled BIO-RSA leads to better post-operative inclination and clinical outcomes than Standard BIO-RSA added to eccentric glenoid reaming (1.25 Vs. 4.1 - p:.036). Glenoids classified as E1 and E3 have been shown to be both the most frequent (E1 + E3 = 80.2%) and with the greatest RSA-TSA differences.
As the baseplate is placed in the lower half of the glenoid surface, E1 and E3 subtypes are at greater risk of post-operative superior inclination (Figure 5).
Figure 5.
Preoperative RSA based on glenoid surface inclination classification.
Glenoid inclination, as described by Hughes et al. 26 and Maurer et al., 27 is commonly considered to be the angle (the β angle) between the floor of the supraspinatus fossa and the line of the glenoid fossa.
Although the β angle is appropriate for measuring glenoid component inclination in TSA, it is not proper in RSA.
Boileau et al., 2 described and validated a new useful method, while performing RSA, to measure the lower half glenoid inclination, using both radiography and/or computed tomography (CT scan) in order to avoid a superior postoperative component tilt: the RSA Angle.
As shown by Boileau et al., 8 E1 (central concentric glenoid erosion) and E3 (superior glenoid erosion) glenoid morphologies are the most common subtypes in CTA. Particular attention should be paid to those two subtypes, due to the increased risk of implanting the baseplate with a superior inclination. 9
Although controversy exists over which one is the best method to correct glenoid inclination in RSA, it seems essential to place the glenosphere baseplate perpendicular to the floor of the supraspinatus fossa. This is performed correcting the preoperative RSA angle in order to avoid a postoperative superior tilt.28–30
Glenosphere baseplate superior inclination increases the implant-bone interface stress, leading to impingement between the polyethylene humeral insert and the scapular abutment. 11 It might cause medial polyethylene wear, scapular notching, and aseptic loosening of the glenoid implant.4–6,16,31
Frequently an excessive amount of glenoid vault bone should be removed from the lower part of the glenoid (eccentric reaming technique) in order to correct the preoperative RSA angle. This has driven the physicians to search for other surgical solutions to preserve the bone stock.
Angled BIO-RSA is a relative recent technique, with results poorly described in the literature. This technique seems to be useful in case of Walch B2 / C or Favard E1 / E3 glenoids in order to preserve through a more conservative reaming the greatest amount of glenoid vault bone. Excessive eccentric reaming could lead to place the baseplate within poor quality bone.2,32
The Angled graft has probably a smaller lateralizing effect than the standard graft, whereas its main role is to restore and correct the glenoid morphology. 32
This study showed that Angled BIO-RSA allows better management of glenoid erosion in RCA, leading to a better glenoid component inclination closer to 0°.
Significant better postoperative clinical outcomes were outlined in Angled BIO-RSA group compared to standard BIO-RSA/eccentric reaming technique group, in terms of abduction and forward flexion. However, it must be emphasized that only active abduction reached a MCID. No other statistically significant differences were found in terms of Constant Score, VAS, internal and external rotation. Both techniques improved significantly the clinical outcomes compared to preoperative values.
Angled BIO-RSA has shown to lead to an overall better postoperative inclination, as the majority of shoulders were classified as E1 and E3. Whereas in E0 and E2, which are the less common subtypes, eccentric reaming and standard BIO-RSA has shown to better manage, with a mean postoperative RSA value closer to 0°, the glenoid erosions. In those two subtypes the RSA-TSA difference has been shown to be little.
Although angled BIO-RSA showed better inclination correction in E1 and E3 than standard BIO-RSA, the difference was not statistically significant. However angled graft leaded to postoperative mean tilt values in both subtypes inferior to 5° (E1:1.05° and E3: 1.71°).
Eccentric reaming/Standard BIO-RSA leaded to a mean postoperative inclination value ≥ 5° in both E1 and E3. (E1:5.61° and E3: 5.00°).
Boileau et al. 20 stated that until 5°, a RSA angle has to be considered neutral. Therefore, our results showed that in E1 and E3 only Angled BIO-RSA enabled the mean postoperative inclination to be within this range.
A more precise and closer to 0° inclination of the glenoid component (increasing the impingement-free arc ROM) might be the reason for the better clinical outcomes.33,34
Preoperative radiographic and CT evaluation are essential to avoid baseplate malpositioning and poor RSA angle correction. The use of a software for preoperative planning enables the physician to choose
the appropriate angulation, size and shape of the bone graft in order to correct properly the glenoid inclination. 27
To our knowledge, this is the first study comparing clinical and radiographic outcomes of angled BIO-RSA and eccentric reaming plus standard BIO-RSA.
This study has some limitations: it retrospectively reports clinical and radiographic outcomes of RSA with a mean follow-up of two years; patients are not randomized to the two techniques; and each group of patients received surgery in a different period. Furthermore, the shift from one technique to the other, which was decided by the senior author, might pose a bias.
Future prospective randomized clinical studies with longer follow-ups, greater number of patients, and multiple scores used are needed to confirm our results.
Potential future studies should compare Angled BIO-RSA with Angled MIO-RSA in correcting glenoid erosions.
Therefore, the use of angled BIO-RSA seems to be more effective than eccentric reaming/standard BIO-RSA, to correct glenoid inclination leading to better clinical outcomes in patients with RCA.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iDs: Edoardo Giovannetti de Sanctis https://orcid.org/0000-0002-6012-1651
Pietro Gregori https://orcid.org/0000-0002-0727-2231
Supplemental material: Supplemental material for this article is available online.
References
- 1.Seidl AJ, Williams GR, Boileau P. Challenges in reverse shoulder arthroplasty: addressing glenoid bone loss. Orthopedics 2016; 39: 14–23. [DOI] [PubMed] [Google Scholar]
- 2.Boileau P, Morin-Salvo N, Gauci MO, et al. Angled BIO-RSA (bony-increased offset-reverse shoulder arthroplasty): a solution for the management of glenoid bone loss and erosion. J Shoulder Elbow Surg 2017; 26: 2133–2142. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P. Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res 2016; 102(1 Suppl): S33–S43. [DOI] [PubMed] [Google Scholar]
- 4.Frankle MA, Teramoto A, Luo ZPet al. et al. Glenoid morphology in reverse shoulder arthroplasty: classification and surgical implications. J Shoulder Elbow Surg 2009; 18: 874–885. [DOI] [PubMed] [Google Scholar]
- 5.Sirveaux F, Favard L, Oudet Det al. et al. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 2004; 86: 388–395. [DOI] [PubMed] [Google Scholar]
- 6.Gutierrez S, Greiwe RM, Frankle MA, et al. 3rd. Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg 2007; 16(3 Suppl): S9–S12. [DOI] [PubMed] [Google Scholar]
- 7.Levigne C, Boileau P, Favard L, et al. Scapular notching in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2008; 17: 925–935. [DOI] [PubMed] [Google Scholar]
- 8.Boileau P, Gauci MO, Wagner ER, et al. The reverse shoulder arthroplasty angle: a new measurement of glenoid inclination for reverse shoulder arthroplasty. J Shoulder Elbow Surg 2019; 28: 1281–1290. [DOI] [PubMed] [Google Scholar]
- 9.Favard L, Berhouet J, Walch Get al. et al. Superior glenoid inclination and glenoid bone loss : definition, assessment, biomechanical consequences, and surgical options. Orthopade 2017; 46: 1015–1021. [DOI] [PubMed] [Google Scholar]
- 10.Nyffeler RW, Werner CM, Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg 2005; 14: 524–528. [DOI] [PubMed] [Google Scholar]
- 11.Falaise V, Levigne C, Favard L, et al. Scapular notching in reverse shoulder arthroplasties: the influence of glenometaphyseal angle. Orthop Traumatol Surg Res 2011; 97(6 Suppl): S131–S137. [DOI] [PubMed] [Google Scholar]
- 12.Boileau P, Moineau G, Roussanne Yet al. et al. Bony increased-offset reversed shoulder arthroplasty: minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res 2011; 469: 2558–2567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Simovitch RW, Zumstein MA, Lohri Eet al. et al. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am 2007; 89: 588–600. [DOI] [PubMed] [Google Scholar]
- 14.Dilisio MF, Warner JJ, Walch G. Accuracy of the subchondral smile and surface referencing techniques in reverse shoulder arthroplasty. Orthopedics 2016; 39: e615–e620. [DOI] [PubMed] [Google Scholar]
- 15.Edwards TB, Trappey GJ, Riley Cet al. et al. Inferior tilt of the glenoid component does not decrease scapular notching in reverse shoulder arthroplasty: results of a prospective randomized study. J Shoulder Elbow Surg 2012; 21: 641–646. [DOI] [PubMed] [Google Scholar]
- 16.Laver L, Garrigues GE. Avoiding superior tilt in reverse shoulder arthroplasty: a review of the literature and technical recommendations. J Shoulder Elbow Surg 2014; 23: 1582–1590. [DOI] [PubMed] [Google Scholar]
- 17.Boileau P, Moineau G, Roussanne Yet al. et al. Bony increased offset-reversed shoulder arthroplasty (BIO-RSA). JBJS Essent Surg Tech 2017; 7: e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu JE, Ricchetti ET, Huffman GRet al. et al. Addressing glenoid bone deficiency and asymmetric posterior erosion in shoulder arthroplasty. J Shoulder Elbow Surg 2013; 22: 1298–1308. [DOI] [PubMed] [Google Scholar]
- 19.Williams GR, Jr., Iannotti JP. Options for glenoid bone loss: composites of prosthetics and biologics. J Shoulder Elbow Surg 2007; 16(5 Suppl): S267–S272. [DOI] [PubMed] [Google Scholar]
- 20.Boileau P, Morin-Salvo N, Bessiere Cet al. et al. Bony increased-offset-reverse shoulder arthroplasty: 5 to 10 years’ follow-up. J Shoulder Elbow Surg 2020; 29: 2111–2122. [DOI] [PubMed] [Google Scholar]
- 21.Nunes B, Linhares D, Costa F, et al. Lateralized versus nonlateralized glenospheres in reverse shoulder arthroplasty: a systematic review with meta-analysis. J Shoulder Elbow Surg 2021; 30: 1700–1713. [DOI] [PubMed] [Google Scholar]
- 22.Werner BS, Chaoui J, Walch G. The influence of humeral neck shaft angle and glenoid lateralization on range of motion in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2017; 26: 1726–1731. [DOI] [PubMed] [Google Scholar]
- 23.Ladermann A, Denard PJ, Collin P, et al. Effect of humeral stem and glenosphere designs on range of motion and muscle length in reverse shoulder arthroplasty. Int Orthop 2020; 44: 519–530. [DOI] [PubMed] [Google Scholar]
- 24.Greiner S, Schmidt C, Herrmann Set al. et al. Clinical performance of lateralized versus non-lateralized reverse shoulder arthroplasty: a prospective randomized study. J Shoulder Elbow Surg 2015; 24: 1397–1404. [DOI] [PubMed] [Google Scholar]
- 25.Simovitch R, Flurin PH, Wright Tet al. et al. Quantifying success after total shoulder arthroplasty: the minimal clinically important difference. J Shoulder Elbow Surg 2018; 27: 298–305. [DOI] [PubMed] [Google Scholar]
- 26.Hughes RE, Bryant CR, Hall JM, et al. Glenoid inclination is associated with full-thickness rotator cuff tears. Clin Orthop Relat Res 2003; 407: 86–91. [DOI] [PubMed] [Google Scholar]
- 27.Maurer A, Fucentese SF, Pfirrmann CW, et al. Assessment of glenoid inclination on routine clinical radiographs and computed tomography examinations of the shoulder. J Shoulder Elbow Surg 2012; 21: 1096–1103. [DOI] [PubMed] [Google Scholar]
- 28.Churchill RS, Brems JJ, Kotschi H. Glenoid size, inclination, and version: an anatomic study. J Shoulder Elbow Surg 2001; 10: 327–332. [DOI] [PubMed] [Google Scholar]
- 29.Roche C, Flurin PH, Wright Tet al. et al. An evaluation of the relationships between reverse shoulder design parameters and range of motion, impingement, and stability. J Shoulder Elbow Surg 2009; 18: 734–741. [DOI] [PubMed] [Google Scholar]
- 30.Boileau P, Watkinson D, Hatzidakis AMet al. et al. Neer award 2005: the grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 2006; 15: 527–540. [DOI] [PubMed] [Google Scholar]
- 31.Gutierrez S, Walker M, Willis Met al. et al. Effects of tilt and glenosphere eccentricity on baseplate/bone interface forces in a computational model, validated by a mechanical model, of reverse shoulder arthroplasty. J Shoulder Elbow Surg 2011; 20: 732–739. [DOI] [PubMed] [Google Scholar]
- 32.Chen X, Reddy AS, Kontaxis A, et al. Version correction via eccentric reaming compromises remaining bone quality in B2 glenoids: a computational study. Clin Orthop Relat Res 2017; 475: 3090–3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wall B, Nove-Josserand L, O’Connor DPet al. et al. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am 2007; 89: 1476–1485. [DOI] [PubMed] [Google Scholar]
- 34.Greiner S, Schmidt C, Konig Cet al. et al. Lateralized reverse shoulder arthroplasty maintains rotational function of the remaining rotator cuff. Clin Orthop Relat Res 2013; 471: 940–946. [DOI] [PMC free article] [PubMed] [Google Scholar]