Abstract
Simple Summary
It is now thought that bacteria in the gut and tumour of patients with pancreatic cancer play an important role in the growth of the cancer and its sensitivity to chemotherapy. It has been shown that pancreatic exocrine insufficiency (PEI), common in pancreatic cancer patients, is linked to poorer outcomes. Conversely, it has also been demonstrated that treatment with pancreatic enzyme replacement therapy (PERT) can improve survival in pancreatic cancer patients. The reasons for this are not fully understood, but it is possible that PEI alters the gut and tumour microbiome of pancreatic cancer patients towards a less favourable composition, whereas PERT can reverse these changes and make the gut and tumour microbiome more favourable. If true, this could represent an opportunity for the development of new diagnostic tests and therapies for pancreatic cancer, which remains one of the deadliest cancers.
Abstract
Pancreatic exocrine insufficiency (PEI) is common amongst pancreatic cancer patients and is associated with poorer treatment outcomes. Pancreatic enzyme replacement therapy (PERT) is known to improve outcomes in pancreatic cancer, but the mechanisms are not fully understood. The aim of this narrative literature review is to summarise the current evidence linking PEI with microbiome dysbiosis, assess how microbiome composition may be impacted by PERT treatment, and look towards possible future diagnostic and therapeutic targets in this area. Early evidence in the literature reveals that there are complex mechanisms by which pancreatic secretions modulate the gut microbiome, so when these are disturbed, as in PEI, gut microbiome dysbiosis occurs. PERT has been shown to return the gut microbiome towards normal, so called rebiosis, in animal studies. Gut microbiome dysbiosis has multiple downstream effects in pancreatic cancer such as modulation of the immune response and the response to chemotherapeutic agents. It therefore represents a possible future target for future therapies. In conclusion, it is likely that the gut microbiome of pancreatic cancer patients with PEI exhibits dysbiosis and that this may potentially be reversible with PERT. However, further human studies are required to determine if this is indeed the case.
Keywords: pancreatic cancer, microbiome, pancreatic exocrine insufficiency, pancreatic enzyme replacement therapy
1. Introduction
1.1. The Human Microbiota
The human microbiota is a term used to describe the approximately 100 trillion microorganisms present in each individual [1,2,3]. With the emergence of more sophisticated bacterial genome sequencing [4,5,6,7], there is increasing interest in the interactions between the human microbiota and the human host. Such sequencing techniques include organism-level profiling with 16s rRNA gene sequencing or the more sophisticated gene-level profiling possible with metagenomic and metatranscriptomic sequencing [4,5,6,7]. These sequencing techniques have allowed a greater understanding not only of the composition of these microbial communities, but also an insight into their function [4,5,6,7], and the role they may play in the wider metabolic and immune function of the host [8].
1.2. The Gut Microbiome
A microbiome is defined as a population of microorganisms in conjunction with their genes in a specific body system; as such the microbial community in the bowel is referred to as the gut microbiome [1,2,3]. It has been demonstrated that the gut microbiome plays a key role in modulating host metabolic and immune function [9]. Within the gut, it has been demonstrated that the gut microbiome plays an important role in the development and progression of inflammatory bowel disease [10,11,12] and colorectal cancer [13,14]. Recent evidence highlights a functional role of the gut microbiome not only in cancer development and progression but also in defining the efficacy and toxicity of chemotherapeutic agents [15]. Beyond the gut however, it is thought that the gut microbiome is also linked to the progression of certain conditions such as chronic liver disease [16,17] and pancreatic ductal adenocarcinoma (PDAC) [18,19]. In terms of mechanisms, it is thought that bacteria and their metabolites exert their effects through translocation via the portal circulation, mesenteric lymph nodes or directly through the biliary and pancreatic duct systems [20,21,22]. All this combined means that the gut microbiome is increasingly viewed as a potential route for future diagnostic tests and a therapeutic target for many different conditions, including PDAC.
1.3. Pancreatic Ductal Adenocarcinoma
Whilst progress has been made in the treatment of other major malignancy types, PDAC remains one of the leading causes of cancer death worldwide, with 5-year survival rates persistently below 10% [23,24,25]. One reason for this poor survival is the tendency for PDAC to present late, meaning that many patients already have involvement of nearby major vascular structures which can preclude curative resection [26]. Similarly, many PDAC patients have distant metastatic disease at presentation, with the majority being hepatic due to the portal drainage of the pancreas [27,28,29], and current international practice guidelines advise against resection of PDAC in the setting of liver metastases [30,31,32,33,34]. Should the tumour be resectable and the patient receive systemic therapy, 5-year survival can reach up to 30% [35].
Even when surgical resection is achieved, there is a high likelihood that the patient will experience disease recurrence [36]; 75% of patients who undergo surgical resection and adjuvant therapy for primary PDAC will experience recurrence within 2 years [23,37,38]. As a result, there is an urgent need for new diagnostic and therapeutic targets in this challenging disease. The gut microbiome may represent one of the more promising prospects for future therapies.
1.4. Changes in the Gut Microbiome in PDAC Patients
It is increasingly appreciated that the gut microbiome is linked to the evolution of PDAC, with a recent study identifying changes in the gut microbiome that are present early in the disease process [19]. Further evidence that the gut microbiome may play an active role in the progression of PDAC comes from differences reported in the composition of the gut microbiome between short-term survival (STS) and long-term survival (LTS) PDAC patients, with greater diversity being associated with a more favourable prognosis [39].
1.5. Pancreatic Exocrine Insufficiency in Pancreatic Cancer
Pancreatic exocrine insufficiency (PEI) is defined as insufficient secretion of pancreatic enzymes and bicarbonate to maintain a normal digestion [40]. PEI has been shown to be both prevalent and progressive amongst patients with pancreatic cancer. A recent prospective cohort study used the 13C mixed triglyceride breath test to investigate the prevalence of PEI amongst 254 patients awaiting pancreatoduodenectomy for an oncologic indication [41]. This study reported an incidence of 32.8% in those awaiting resection [41]. In addition, a systematic review in 2016 identified four studies evaluating PEI preoperatively, all using faecal elastase (FE-1), and found a median prevalence of 44% (range 42–47%) [42]. This results from lower enzyme secretion due to tumour burden as well as reduced enzyme delivery and activation as a consequence of pancreatic duct obstruction, which prevents the passage of enzymes and their accompanying bicarbonate-rich fluid into the duodenum [43]. Following pancreatoduodenectomy, there is also significant disruption to the physiological mechanisms by which pancreatic secretion is controlled, with some data indicating that the method of reconstruction may influence the degree of postoperative endocrine and exocrine pancreatic function [44,45].
Untreated PEI has a significant impact on quality of life and leads to a range of mentally and physically distressing symptoms including frequency, urgency, bloating, diarrhoea, fatty stool flatulence, loss of appetite and vomiting [46,47]. A major consequence is maldigestion resulting in malabsorption, malnutrition, and the ensuing nutritional deficiencies (including albumin, pre-albumin, transferrin, lipoproteins, fat soluble vitamins, calcium, magnesium, zinc, thiamine, and folic acid [48,49]). Clinically, PEI is associated with an increased risk of osteoporosis, sarcopenia, and cardiovascular events [50,51,52]. In pancreatic cancer, sarcopenia has been associated with increased perioperative mortality and reduced overall survival. There are multiple neural and hormonal factors that influence sarcopenia in PC and many of these also have interactions with the gut microbiome [53,54]. PEI has also been shown to increase length of stay, post-operative complications and costs following pancreatic resection [55,56]. It is also likely that PEI associated with PDAC leads to important changes in the gut microbiome which, if more clearly understood, could lead to the identification of new diagnostic and therapeutic targets.
1.6. Pancreatic Enzyme Replacement Therapy
Pancreatic enzyme replacement therapy (PERT) refers to the oral administration of capsules containing commercially produced digestive enzymes, namely lipase, protease and lipase. Treatment of PEI with PERT has been shown to improve quality of life [57,58] and also significantly increases survival in resectable and unresectable pancreatic cancer patients [59,60]. This has led the United Kingdom’s National Institute of Health and Care Excellence (NICE) to recommend PERT for pancreatic cancer patients [61,62] without the need for a positive diagnostic test. This was supported by UK specialty consensus guidelines release in 2021 [62]. The underlying basis for the beneficial effects of PERT are not fully understood, but contributing factors appear to be related to the ability to alleviate malabsorption [63,64], which allows patients to tolerate physiologically demanding treatments such as major pancreatic resection and/or chemotherapy. On a micronutrient level, the absorption of fat-soluble vitamins appears crucial. For example, Vitamin D modulates the function of stromal cells (e.g., fibroblasts) in patients with PDAC [65] and deficiency is associated with poorer survival in advanced pancreatic cancer [66]. Recently, interest has been increasing in the intestinal microbiome as a modulator of many diseases (e.g., inflammatory bowel disease) although how PEI may affect this is still being understood.
1.7. Pancreatic Exocrine Insufficiency and the Intestinal Microbiome
PEI is thought to lead to changes in the composition of the gut microbiome, leading to a state of dysbiosis characterised by an imbalance in microbiome diversity [67,68,69,70]. Understanding how the microbiome and PEI are interconnected could aid the search for novel diagnostic and therapeutic targets and help improve outcomes in PDAC. Indeed, recent evidence indicates a role for the gut microbiome in the aetiology and progression of PDAC [19] and has also linked changes in the gut microbiome to outcome and treatment response [20,39,71,72,73]. The aim of this review is to summarise the current evidence linking PEI with microbiome dysbiosis, assess how microbiome composition may be influenced by PERT treatment, and look towards possible future diagnostic and therapeutic targets in this area.
2. The Interaction between Pancreatic Exocrine Function and Gut Microbiome
2.1. Effects of Pancreatic Exocrine Insufficiency on the Gut Microbiome
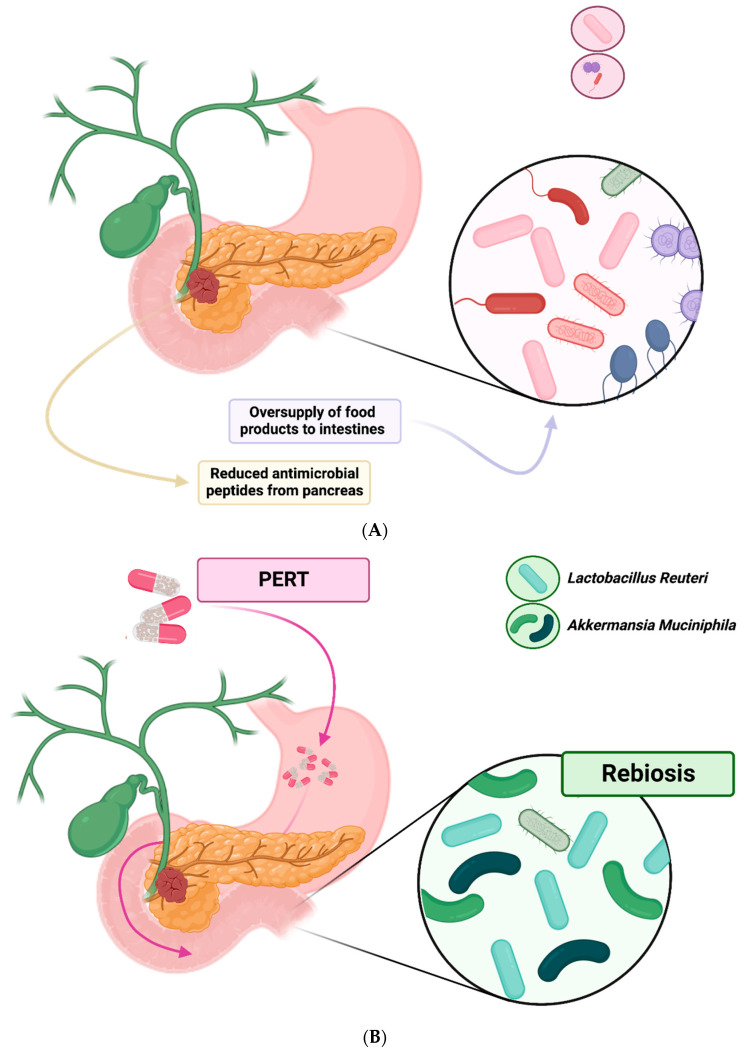
PEI is prevalent in patients with PC and there is emerging evidence that pancreatic exocrine function is closely linked to the composition of the gut microbiome [67,68,69]. Differences in the gut microbiome have been reported in patients with PEI, the main changes observed being a reduction in alpha-diversity, small intestine bacterial overgrowth and loss of ‘beneficial’ bacteria [67,68,69]. A large population-based study by Frost et al. gives significant insight into the importance of pancreatic exocrine function in regulating the gut microbiome [67]. This study compared the composition of the gut microbiome, via 16S rRNA gene sequencing of stool samples, to pancreatic function, using pancreatic elastase levels in over 1700 patients [67]. Their results showed that changes in the gut microbiome composition were much more closely linked to pancreatic exocrine function, rather than other commonly measured host factors such as age, dietary factors, diabetes or smoking [67]. This led the authors to conclude that pancreatic exocrine function appeared to be the most important host factor involved in shaping the human intestinal microbiome [67]. It is therefore likely that patients with pancreatic cancer, many of whom have PEI [42], will also have a deranged gut microbiome (Figure 1A) [19].
Figure 1.
(A) mechanisms of dysbiosis in PEI; (B) mechanisms of rebiosis in PEI.
2.2. Pancreatic Regulation of Gut Microbiome
With increasing interest in the role that pancreatic exocrine function plays in the regulation of the gut microbiome, attention has turned towards the exact mechanisms by which pancreatic exocrine products influence gut bacteria. There are three main cell types in the adult pancreas: acinar cells that produce digestive enzymes; duct epithelial cells that produce a bicarbonate rich fluid which functions to carry digestive enzymes into the digestive tract and also to establish an optimal pH for enzyme function, and the cells of the Islets of Langerhans, which have an endocrine function, producing hormones such as glucagon and insulin [74,75]. In one large study, the role of the two main exocrine cell types (acinar and ductal) were investigated separately [67]. Acinar cell function was quantified with an immunochemical faecal elastase assay [76,77], and ductal cell function was assessed using secretin-stimulated magnetic resonance cholangiopancreatography (sMRCP) [67,78]. The results from this study demonstrated that acinar cell function was more closely related to gut microbiome composition than ductal cell function [67].
Acinar cells produce many different products, so determining which of these play a role in the composition of the gut microbiome has also been investigated. It has been shown that pancreatic secretions possess both bacteriostatic activity against common bacterial pathogens and fungistatic activity against Candida albicans [79]. However, this function of canine pancreatic secretions persisted when digestive enzymes were inhibited, which likely indicates that digestive enzymes are not the main factors that regulate the intestinal flora [67,79]. Apart from digestive enzymes, it has been shown that the pancreas produces antimicrobial peptides [67,80,81,82]. One such example of important antimicrobial peptides produced by the pancreas are cathelicidins, these are small proteolytically activated peptides shown to be active against bacteria, fungi and some viruses [83]. Murine studies have indicated that cathelicidin-related antimicrobial peptide (CRAMP) plays an important role in the regulation of the intestinal microbiome; when genetic modifications were made to reduce levels of CRAMP production in the murine pancreas, fatal bacterial overgrowth in the intestine occurred [81]. In human studies however, cathelicidin antimicrobial peptide (CAMP) levels in faeces have not been shown to be different in patients with PEI compared to healthy controls [67], this does not necessarily mean that this peptide is unimportant and may be due to sampling difficulties [67]. These products and their roles are summarised in Table 1.
Table 1.
Summary of exocrine pancreatic products and their effect on the gut microbiome.
| Exocrine Pancreatic Product |
Example | Source Pancreatic Cell Type | Function | Effect on Gut Microbiome |
|---|---|---|---|---|
| Bicarbonate rich fluid | - | Duct epithelial cell | Carry pancreatic enzymes into small intestine. Optimise pH for enzyme action. |
sMRCP indicates negligible role |
| Digestive enzymes | Lipase, protease, amylase | Acinar cell | Digest food products |
Oversupply of food products leads to significant changes especially complex carbohydrates. Inhibition in canine models did not affect composition of microbiome. |
| Antimicrobial peptides | CAMP and CRAMP | Acinar cell | Bacteriostatic properties | Murine studies indicate a regulatory role for the gut microbiome. Human studies remain inconclusive due to sampling issues |
sMRCP = secretin-stimulated magnetic resonance cholangiopancreatography CAMP = cathelicidin antimicrobial peptide; CRAMP = cathelicidin-related antimicrobial peptide.
Another mechanism by which it is thought PEI may lead to significant changes in the gut microbiome is by the oversupply of food products to the intestine, leading to the overgrowth of dominant bacteria [70]. In particular, it has been suggested that the increased availability of complex carbohydrates, seen in patients with PEI due to reduced digestive activity, may act as a substrate for certain communities within the gut microbiome [67]. Given that acinar cell activity has been closely linked to gut microbiome composition in humans [67], and the main function of these cells is to produce digestive enzymes, this seems like another plausible mechanism by which PEI may influence gut microbiome composition.
2.3. Gut Microbiome Changes from Pancreatic Exocrine Insufficiency in Different Disease States
Whilst there is credible evidence from both animal and human studies to suggest that PEI leads to significant changes in the gut microbiome, it is important to understand the impact that different disease processes leading to PEI in humans may have on the gut microbiome, such as chronic pancreatitis (CP) and pancreatic cancer (PC). For example, chronic pancreatitis (CP) is one of the main causes of PEI in humans and is known to be linked to changes in the gut microbiome [68,69,70,84], but it is often caused by excessive smoking or alcohol consumption, which in themselves may lead to changes in the gut microbiome. Indeed, a recent study in which the gut microbiome of chronic pancreatitis patients was investigated with 16S rRNA gene sequencing and compared to a matched population of healthy controls described some important findings [68]. The study by Frost et al. reported that not only did CP lead to significant changes in the gut microbiome, namely reduced microbial diversity and increased abundance of pathogenic bacteria, but more importantly these changes were independent of exocrine function (measured with stool elastase) [68]. This suggests that gut microbiome changes in pancreatic disease are not solely related to reduced pancreatic exocrine function.
At present, there is limited data on the changes in the gut microbiome related to PEI in PC patients. It is plausible that, as observed in CP patients [68], there are multiple factors influencing the gut microbiome composition in PC patients, beyond just PEI. For example, many PC patients experience cancer cachexia, characterised by systemic inflammation and nutritional depletion [53]. Links between the state of cancer cachexia and the gut microbiome have been drawn [85,86] and this means that changes in the gut microbiome in PC patients are likely to differ to those in CP patients, even though both experience PEI. As such, further study is required to understand the changes in the gut microbiome changes in different pancreatic disease processes such as CP and PC. Improved understanding of the changes to the gut microbiome in both CP and PC patients will inform future studies investigating therapeutics that aim to return the gut microbiome towards a healthier phenotype in these patients.
2.4. Effects of Pancreatic Enzyme Replacement on the Gut Microbiome
From the evidence outlined above, it appears that PEI is associated with gut microbiome dysbiosis, which in turn is thought to be associated with multiple adverse downstream effects. Therefore, it is desirable to identify strategies by which harmful effects of PEI on the gut microbiome may be mitigated and the microbiome returned towards a healthier state. One logical method in PC patients would be through pancreatic enzyme replacement therapy (PERT), which is frequently under prescribed, despite being recommended for all with pancreatic cancer by national practice guidelines [61,62]. In animal models, PERT has been shown to reverse changes to the microbiome caused by PEI [87,88]. Specifically, an increase in beneficial bacterial species, such as Akkermansia muciniphila and Lactobacillus reuteri [87,88], and a reduction in species associated with dysbiosis such as Prevotella and those of the phylum Proteobacteria [87]. This reestablishment of a healthy complex microbiome after dysbiosis has occurred (sometimes referred to as ‘rebiosis’ [69]) (Figure 1B), reduces intestinal inflammation, improves PEI-associated symptoms and mediates nutritional decline [69,88]. Therefore, it may be a further mechanism by which PERT acts to improve quality of life [57,58] and survival amongst pancreatic cancer patients [59,60] (Figure 2). That said, some animal evidence has suggested that the gut microbiome of animals treated with PERT still exhibits important differences to healthy controls [89]. As a result, further study is required to evaluate to what degree PERT can return the gut microbiome of PC patients with PEI towards a healthier composition and whether this translates into improved outcomes.
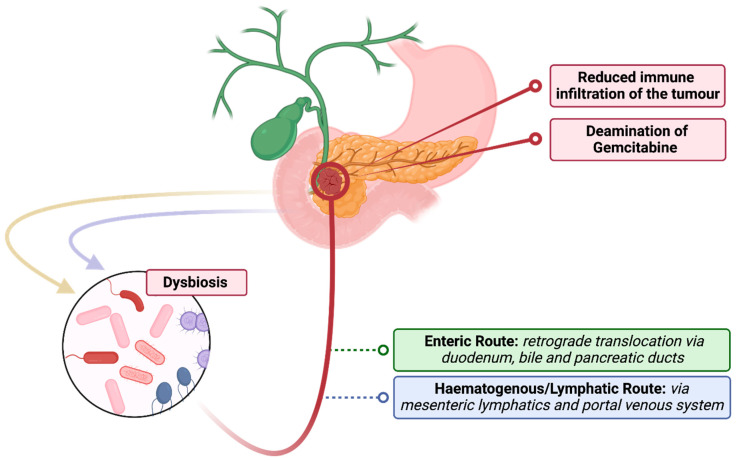
Figure 2.
Links between gut microbiome and pancreatic tumour microbiome.
3. Effects of the Intestinal Microbiome in Pancreatic Cancer Patients
3.1. Intestinal Microbiome and Clinical Outcomes in Pancreatic Cancer
Associations between microbiome composition and clinical outcome for patients with PDAC are now being observed. Differences in intestinal microbiome composition between patients with short-term survival (STS) and long-term survival (LTS) have been demonstrated with 16S rRNA gene sequencing [21,39]. An increasing abundance of Acinetobacter was identified in the highly aggressive ‘basal-like’ subtype of pancreatic ductal adenocarcinoma (PDAC) using metagenomic sequencing of resected tumours [90]. However, in the absence of mechanistic insights, these findings remain associative rather than causative.
3.2. Extraintestinal Effects of the Gut Microbiome in Pancreatic Disease
The effects of intestinal microbiome dysbiosis have been shown to extend beyond the intestinal tract in patients with pancreatic disease. In acute and chronic pancreatitis, a frequent clinical issue is the colonisation of pancreatic necrosis and fluid collections with pathogenic bacteria. Evidence suggests that numbers of beneficial bacterial species such as Faecalibacterium [91,92] and Fusicatenibacter [93] are reduced in patients with CP [68]. These bacterial species are thought to play an anti-inflammatory role in the colon and preserve the intestinal barrier through the production of short-chain fatty acids and lactate [91,92], reducing the chance of extraintestinal translocation of pathogenic bacteria [93,94]. As a result, gut microbiome changes can be directly related to the severity of the disease [68,95].
Importantly, for pancreatic cancer patients, it is now appreciated that pancreatic tumours themselves harbour a population of bacteria, referred to as the tumour microbiome [21,73,96,97], which has been shown to influence the prognosis of PDAC [21,39,98]. Relevant to this article, it has been shown that the gut microbiome influences the composition of this tumour microbiome in pancreatic cancer [39]. The exact mechanism for this remains debated, but possible routes include retrograde translocation from the gut, via the duodenum and bile/pancreatic ducts, spread from the portal circulation or mesenteric lymph nodes (Figure 2) [20,21,22]. The importance of the tumour microbiome is attracting increasing interest [96,99] and has been shown to differentiate between different phenotypes of pancreatic cancer, as well as influencing clinical outcome [39,90]. For example, some human pancreatic tumours are colonised by Gammaproteobacteria, a subset of which possess an isoform of cytidine deaminase, which is capable of metabolising gemcitabine into an inactive form [21] and, in so doing, increases the tumour’s chemoresistance and therefore reduces treatment efficacy [100,101]. Evidence of clinical benefit in modulating the tumour microbiome has also been demonstrated in a recent large cohort study which showed that peri-chemotherapy antibiotics in metastatic PDAC patients improved cancer-specific survival [102]. Interestingly, a survival benefit was seen only in patients receiving gemcitabine, not fluorouracil, adding to the growing body of evidence that bacteria-mediated gemcitabine resistance is prevalent in PDAC patients [20] and could represent a target for future therapies.
3.3. Tumour Microbiome and Immune Infiltration
A further route by which it is thought that the tumour microbiome influences the prognosis of PDAC includes local immunosuppression and subsequent accelerated oncogenesis [103,104,105,106]. A relationship between the tumour microbiome and tumour immune infiltration has been demonstrated [103] with an increase in infiltration of CD8+ T cells reported following ablation of the tumour microbiome with antibiotics [103]. Furthermore, transfer of selected bacteria from PDAC tissue accelerated tumorigenesis [103]. This highlights a possible mechanism by which a more favourable gut microbiome, which is observed through appropriate treatment of PEI with PERT, may influence cancer-related outcomes in PDAC patients. Future studies should therefore seek to compare the gut and tumour microbiome composition to immune infiltration of tumours, for example via immunohistochemistry, to further investigate this relationship.
4. Diagnostic and Therapeutic Applications for Greater Understanding of the Gut Microbiome in Pancreatic Cancer Patients
4.1. Use of Intestinal Microbiome Testing for Diagnosis of Pancreatic Exocrine Insufficiency
If changes in the microbiome are observed in PEI, then it may also be possible to diagnose this using intestinal microbiome sequencing from stool samples. The incidence of PEI pre-operatively is challenging to assess, and no ideal diagnostic test currently exists. The secretin test and coefficient of fat absorption (CFA) are accurate but expensive and unpleasant, whilst faecal elastase (FE-1), although suitable for routine use, has poor sensitivity in mild PEI [107]. Traditionally, a combination of patient reported symptoms, such as steatorrhoea, and faecal elastase (FE-1) have been used to diagnose PEI. However, the diagnostic accuracy of FE-1 has been questioned, especially amongst those who have undergone surgical resection where the increased ratio of faecal fat to FE-1 reduces the sensitivity of the test [107,108]. The 13C mixed triglyceride breath test is emerging as a promising diagnostic tool [109], but expense and time limit its use to specialist or research centres only [109,110]. Therefore, if changes in the microbiome in patients with PEI are further understood, these could be measured and quantified to be used as a new diagnostic test.
4.2. Titration of Pancreatic Enzyme Replacement Therapy
Given the difficulties in diagnosing PEI in routine clinical practice, monitoring the response to PERT is arguably even more challenging. Whilst UK NICE recommend consideration of PERT treatment for all patients following pancreatic resection [61,62] without the need for a positive diagnostic test, it can be challenging to ensure that each patient is taking the correct dose. If changes in the intestinal microbiome with PERT treatment in PEI patients are quantifiable, then it may be possible to monitor long-term trends with PERT treatment and make dose changes accordingly using stool sample sequencing.
4.3. Positive Effects of Pancreatic Enzyme Replacement Therapies on the Intestinal Microbiome
As described above, early evidence suggests that by modulating the gut microbiome it may be possible to alter the composition of the tumour microbiome. This has been demonstrated in animal studies using faecal microbiota transplantation (FMT) [39,73]. Using the knowledge that differences in intestinal microbiome composition between short-term survival (STS) and long-term survival (LTS) patients have been demonstrated with 16S rRNA gene sequencing [21,39]; researchers sought to modulate the intestinal microbiome with FMT. Interestingly, it has been shown that via FMT from STS and LTS patients into mice, it is possible to modulate the tumour microbiome and thus affect tumour growth [39]. This could also link to some possible benefits of PERT as, if treatment is able to return the intestinal microbiome of pancreatic cancer patients towards a healthy composition, this may positively influence the tumour microbiome. Given that Acinetobacter abundance has been associated with aggressive ‘basal-like’ tumours [90], it is noteworthy that this can be reduced in the gut microbiome of a porcine PEI model reduced after administration of PERT [87]. The potential ability of PERT to modulate the intestinal microbiome, and consequently the tumour microbiome, may be an important determinant of clinical outcome and is worthy of more thorough investigation.
5. Conclusions and Future Directions
It is likely that the gut microbiome of pancreatic cancer patients with PEI exhibits profound dysbiosis and that this may potentially be reversible with PERT. However, further research is needed to conclude if this is indeed the case. Future research should seek to elucidate the specific changes that occur in PC patients with PEI as these are likely to be different to gut microbiome changes in patients with other, benign causes of PEI such as cystic fibrosis or CP. It would also be important to investigate whether the gut microbiome of PC patients who have PEI treated with PERT experience a return of gut microbiome towards that of healthy controls. It is also important to acknowledge that supplements, such as probiotics as well as faecal microbiota transplantation, can influence the composition of the gut microbiome and therefore may also be beneficial in PC [111].
In addition, the downstream effects of gut microbiome dysbiosis in PC patients with PEI need to be further explored and understood. For example, future studies should seek to compare the gut microbiome with the tumour microbiome in PC patients with and without PEI. Similarly, the interaction between the gut microbiome and the immune system in this cohort should be further investigated. This could be achieved by measuring the peripheral immune state in PC patients with and without PEI, or before and after PERT treatment. Equally, the immune infiltration of resected tumours could be compared to the gut microbiome of PC patients and their degree of exocrine function and/or PERT treatment.
It is also important to investigate the extent to which the gut microbiome influences chemosensitivity in PC patients, and whether this is influenced by the degree of PEI or PERT. This may be achieved by monitoring treatment response to neoadjuvant chemotherapy via Ca19-9 levels, radiological response or tumour regression grading of resected specimens, and correlating this to exocrine function and PERT treatment.
In summary, it has been recognised that untreated PEI is harmful in PC patients and that PERT treatment leads to improved outcomes. It has been proposed that this is likely due to improved nutritional status, thus allowing more patients to undergo physiologically demanding treatments, but it is possible that treatment of PEI with PERT in PC patients leads to a more favourable gut microbiome. This in turn may modulate the tumour microbiome, thereby directly influencing tumour growth and the quality of the tumour-specific immune response. The effect of PEI and PERT on the gut microbiome of pancreatic cancer patients is a vital area for future study and may open the door to much needed new diagnostic and therapeutic options for this challenging condition.
Author Contributions
Conceptualization, J.M.H.-S., L.A.H., S.F.P.-B. and K.J.R.; methodology, J.M.H.-S., L.A.H., S.F.P.-B. and K.J.R.; writing—original draft preparation, J.M.H.-S., L.A.H., S.F.P.-B. and K.J.R.; writing—review and editing, N.M., A.E.F., A.D.B., P.M. and K.J.R.; supervision, A.E.F., A.D.B., P.M. and K.J.R. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
A.D.B. is funded by an MRC Senior Clinical Fellowship (ref MR/X006433/1).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Lederberg J., Mccray A.T. COMMENTARY ‘Ome Sweet’ Omics-A Genealogical Treasury of Words. Science. 2001;15:8. [Google Scholar]
- 2.Marchesi J.R., Ravel J. The vocabulary of microbiome research: A proposal. Microbiome. 2015;3:31. doi: 10.1186/s40168-015-0094-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mullish B.H., Quraishi M.N., Segal J.P., Ianiro G., Iqbal T.H. The gut microbiome: What every gastroenterologist needs to know. Frontline Gastroenterol. 2021;12:118–127. doi: 10.1136/flgastro-2019-101376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song S., Jarvie T., Hattori M. Our second genome-human metagenome: How next-generation sequencer changes our life through microbiology. Adv. Microb. Physiol. 2013;62:119–144. doi: 10.1016/B978-0-12-410515-7.00003-2. [DOI] [PubMed] [Google Scholar]
- 5.Zhang W., Li F., Nie L. Integrating multiple “omics” analysis for microbial biology: Application and methodologies. Microbiology. 2010;156:287–301. doi: 10.1099/mic.0.034793-0. [DOI] [PubMed] [Google Scholar]
- 6.Medini D., Serruto D., Parkhill J., Relman D.A., Donati C., Moxon R., Falkow S., Rappuoli R. Microbiology in the post-genomic era. Nat. Rev. Microbiol. 2008;6:419–430. doi: 10.1038/nrmicro1901. [DOI] [PubMed] [Google Scholar]
- 7.Kyrpides N.C. Fifteen years of microbial genomics: Meeting the challenges and fulfilling the dream. Nat. Biotechnol. 2009;27:627–632. doi: 10.1038/nbt.1552. [DOI] [PubMed] [Google Scholar]
- 8.Fan Y., Pedersen O. Gut microbiota in human metabolic health and disease. Nat. Rev. Microbiol. 2020;19:55–71. doi: 10.1038/s41579-020-0433-9. [DOI] [PubMed] [Google Scholar]
- 9.Durack J., Lynch S.V. The gut microbiome: Relationships with disease and opportunities for therapy. J. Exp. Med. 2019;216:20. doi: 10.1084/jem.20180448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lepage P., Hösler R., Spehlmann M.E., Rehman A., Zvirbliene A., Begun A., Ott S., Kupcinskas L., Doré J., Raedler A., et al. Twin study indicates loss of interaction between microbiota and mucosa of patients with ulcerative colitis. Gastroenterology. 2011;141:227–236. doi: 10.1053/j.gastro.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 11.Dicksved J., Halfvarson J., Rosenquist M., Järnerot G., Tysk C., Apajalahti J., Engstrand L., Jansson J.K. Molecular analysis of the gut microbiota of identical twins with Crohn’s disease. ISME J. 2008;2:716–727. doi: 10.1038/ismej.2008.37. [DOI] [PubMed] [Google Scholar]
- 12.Segal J.P., Mullish B.H., Quraishi M.N., Acharjee A., Williams H.R.T., Iqbal T., Hart A.L., Marchesi J.R. The application of omics techniques to understand the role of the gut microbiota in inflammatory bowel disease. Ther. Adv. Gastroenterol. 2019;12:1756284818822250. doi: 10.1177/1756284818822250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mullish B.H., Osborne L.S., Marchesi J.R., Mcdonald J.A. The implementation of omics technologies in cancer microbiome research. Ecancermedicalscience. 2018;12:864. doi: 10.3332/ecancer.2018.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi F., Liu G., Lin Y., Guo C.L., Han J., Chu E.S.H., Shi C., Li Y., Zhang H., Hu C., et al. Altered gut microbiome composition by appendectomy contributes to colorectal cancer. Oncogene. 2022;42:530–540. doi: 10.1038/s41388-022-02569-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chrysostomou D., Roberts L.A., Marchesi J.R., Kinross J.M. Gut Microbiota Modulation of Efficacy and Toxicity of Cancer Chemotherapy and Immunotherapy. Gastroenterology. 2022;164:198–213. doi: 10.1053/j.gastro.2022.10.018. [DOI] [PubMed] [Google Scholar]
- 16.Schwenger K.J., Clermont-Dejean N., Allard J.P. The role of the gut microbiome in chronic liver disease: The clinical evidence revised. JHEP Rep. 2019;1:214. doi: 10.1016/j.jhepr.2019.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tilg H., Cani P.D., Mayer E.A. Gut microbiome and liver diseases. Gut. 2016;65:2035–2044. doi: 10.1136/gutjnl-2016-312729. [DOI] [PubMed] [Google Scholar]
- 18.Nagata N., Nishijima S., Kojima Y., Hisada Y., Imbe K., Miyoshi-Akiyama T., Suda W., Kimura M., Aoki R., Sekine K., et al. Metagenomic Identification of Microbial Signatures Predicting Pancreatic Cancer from a Multinational Study. Gastroenterology. 2022;163:222–238. doi: 10.1053/j.gastro.2022.03.054. [DOI] [PubMed] [Google Scholar]
- 19.Kartal E., Schmidt T.S.B., Molina-Montes E., Rodríguez-Perales S., Wirbel J., Maistrenko O.M., Akanni W.A., Alashkar Alhamwe B., Alves R.J., Carrato A., et al. A faecal microbiota signature with high specificity for pancreatic cancer. Gut. 2022;71:1359–1372. doi: 10.1136/gutjnl-2021-324755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas R.M., Jobin C. Microbiota in pancreatic health and disease: The next frontier in microbiome research. Nat. Rev. Gastroenterol. Hepatol. 2019;17:53–64. doi: 10.1038/s41575-019-0242-7. [DOI] [PubMed] [Google Scholar]
- 21.Geller L.T., Barzily-Rokni M., Danino T., Jonas O.H., Shental N., Nejman D., Gavert N., Zwang Y., Cooper Z.A., Shee K., et al. Potential role of intratumor bacteria in mediating tumor resistance to the chemotherapeutic drug gemcitabine. Science. 2017;357:1156–1160. doi: 10.1126/science.aah5043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Langheinrich M., Wirtz S., Kneis B., Gittler M.M., Tyc O., Schierwagen R., Brunner M., Krautz C., Weber G.F., Pilarsky C., et al. Microbiome Patterns in Matched Bile, Duodenal, Pancreatic Tumor Tissue, Drainage, and Stool Samples: Association with Preoperative Stenting and Postoperative Pancreatic Fistula Development. J. Clin. Med. 2020;9:2785. doi: 10.3390/jcm9092785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oettle H., Neuhaus P., Hochhaus A., Hartmann J.T., Gellert K., Ridwelski K., Niedergethmann M., Zülke C., Fahlke J., Arning M.B., et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: The CONKO-001 randomized trial. JAMA. 2013;310:1473–1481. doi: 10.1001/jama.2013.279201. [DOI] [PubMed] [Google Scholar]
- 24.Neoptolemos J.P., Palmer D.H., Ghaneh P., Psarelli E.E., Valle J.W., Halloran C.M., Faluyi O., O’Reilly D.A., Cunningham D., Wadsley J., et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): A multicentre, open-label, randomised, phase 3 trial. Lancet. 2017;389:1011–1024. doi: 10.1016/S0140-6736(16)32409-6. [DOI] [PubMed] [Google Scholar]
- 25.Kleeff J., Korc M., Apte M., La Vecchia C., Johnson C.D., Biankin A.V., Neale R.E., Tempero M., Tuveson D.A., Hruban R.H., et al. Pancreatic cancer. Nat. Rev. Dis. Prim. 2016;2:16022. doi: 10.1038/nrdp.2016.22. [DOI] [PubMed] [Google Scholar]
- 26.Isaji S., Mizuno S., Windsor J.A., Bassi C., Fernández-del Castillo C., Hackert T., Hayasaki A., Katz M.H.G., Kim S.W., Kishiwada M., et al. International consensus on definition and criteria of borderline resectable pancreatic ductal adenocarcinoma 2017. Pancreatology. 2018;18:2–11. doi: 10.1016/j.pan.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 27.Matsuda Y., Hagio M., Naito Z., Ishiwata T. Clinicopathological features of 30 autopsy cases of pancreatic carcinoma. J. Nippon Med. Sch. 2012;79:459–467. doi: 10.1272/jnms.79.459. [DOI] [PubMed] [Google Scholar]
- 28.Mierke F., Hempel S., Distler M., Aust D.E., Saeger H.D., Weitz J., Welsch T. Impact of Portal Vein Involvement from Pancreatic Cancer on Metastatic Pattern After Surgical Resection. Ann. Surg. Oncol. 2016;23:730–736. doi: 10.1245/s10434-016-5515-6. [DOI] [PubMed] [Google Scholar]
- 29.Bissolati M., Sandri M.T., Burtulo G., Zorzino L., Balzano G., Braga M. Portal vein-circulating tumor cells predict liver metastases in patients with resectable pancreatic cancer. Tumour Biol. 2015;36:991–996. doi: 10.1007/s13277-014-2716-0. [DOI] [PubMed] [Google Scholar]
- 30.Conroy T., Galais M.-P., Raoul J.-L., Bouché O., Gourgou-Bourgade S., Douillard J.-Y., Etienne P.-L., Boige V., Martel-Lafay I., Michel P., et al. Definitive chemoradiotherapy with FOLFOX versus fluorouracil and cisplatin in patients with oesophageal cancer (PRODIGE5/ACCORD17): Final results of a randomised, phase 2/3 trial. Lancet Oncol. 2014;15:305–314. doi: 10.1016/S1470-2045(14)70028-2. [DOI] [PubMed] [Google Scholar]
- 31.Von Hoff D.D., Ervin T., Arena F.P., Chiorean E.G., Infante J., Moore M., Seay T., Tjulandin S.A., Ma W.W., Saleh M.N., et al. Increased Survival in Pancreatic Cancer with nab-Paclitaxel plus Gemcitabine. N. Engl. J. Med. 2013;369:1691–1703. doi: 10.1056/NEJMoa1304369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tempero M.A., Malafa M.P., Behrman S.W., Benson A.B., Casper E.S., Chiorean E.G., Chung V., Cohen S.J., Czito B., Engebretson A., et al. Pancreatic adenocarcinoma, version 2.2014: Featured updates to the NCCN guidelines. J. Natl. Compr. Cancer Netw. 2014;12:1083–1093. doi: 10.6004/jnccn.2014.0106. [DOI] [PubMed] [Google Scholar]
- 33.Bellon E., Gebauer F., Tachezy M., Izbicki J.R., Bockhorn M. Pancreatic cancer and liver metastases: State of the art. Updates Surg. 2016;68:247–251. doi: 10.1007/s13304-016-0407-7. [DOI] [PubMed] [Google Scholar]
- 34.Seufferlein T., Bachet J.B., Van cutsem E., Rougier P. Pancreatic adenocarcinoma: ESMO-ESDO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2012;23((Suppl. 7)):vii33–vii40. doi: 10.1093/annonc/mds224. [DOI] [PubMed] [Google Scholar]
- 35.Merz V., Mangiameli D., Zecchetto C., Quinzii A., Pietrobono S., Messina C., Casalino S., Gaule M., Pesoni C., Vitale P., et al. Predictive Biomarkers for a Personalized Approach in Resectable Pancreatic Cancer. Front. Surg. 2022;9:866173. doi: 10.3389/fsurg.2022.866173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Daamen L.A., Groot V.P., Besselink M.G., Bosscha K., Busch O.R., Cirkel G.A., van Dam R.M., Festen S., Groot Koerkamp B., Haj Mohammad N., et al. Detection, Treatment, and Survival of Pancreatic Cancer Recurrence in the Netherlands. Ann. Surg. 2020;275:769–775. doi: 10.1097/SLA.0000000000004093. [DOI] [PubMed] [Google Scholar]
- 37.Sinn M., Bahra M., Liersch T., Gellert K., Messmann H., Bechstein W., Waldschmidt D., Jacobasch L., Wilhelm M., Rau B.M., et al. CONKO-005: Adjuvant Chemotherapy with Gemcitabine Plus Erlotinib Versus Gemcitabine Alone in Patients After R0 Resection of Pancreatic Cancer: A Multicenter Randomized Phase III Trial. J. Clin. Oncol. 2017;35:3330–3337. doi: 10.1200/JCO.2017.72.6463. [DOI] [PubMed] [Google Scholar]
- 38.Neoptolemos J.P., Stocken D.D., Bassi C., Ghaneh P., Cunningham D., Goldstein D., Padbury R., Moore M.J., Gallinger S., Mariette C., et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: A randomized controlled trial. JAMA. 2010;304:1073–1081. doi: 10.1001/jama.2010.1275. [DOI] [PubMed] [Google Scholar]
- 39.Riquelme E., Zhang Y., Zhang L., Montiel M., Zoltan M., Dong W., Quesada P., Sahin I., Chandra V., San Lucas A., et al. Tumor Microbiome Diversity and Composition Influence Pancreatic Cancer Outcomes. Cell. 2019;178:795–806.e12. doi: 10.1016/j.cell.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dominguez-Muñoz J.E. Diagnosis and treatment of pancreatic exocrine insufficiency. Curr. Opin. Gastroenterol. 2018;34:349–354. doi: 10.1097/MOG.0000000000000459. [DOI] [PubMed] [Google Scholar]
- 41.Hartman V., Roeyen E., Bracke B., Huysentruyt F., De Gendt S., Chapelle T., Ysebaert D., Hendrikx B., Roeyen G. Prevalence of pancreatic exocrine insufficiency after pancreatic surgery measured by 13C mixed triglyceride breath test: A prospective cohort study. Pancreatology. 2023;23:563–568. doi: 10.1016/j.pan.2023.05.012. [DOI] [PubMed] [Google Scholar]
- 42.Tseng D.S.J., Molenaar I.Q., Besselink M.G., Van Eijck C.H., Rinkes I.H.B., Van Santvoort H.C. Pancreatic exocrine insufficiency in patients with pancreatic or periampullary cancer a systematic review. Pancreas. 2016;45:325–330. doi: 10.1097/MPA.0000000000000473. [DOI] [PubMed] [Google Scholar]
- 43.Powell-Brett S., de Liguori Carino N., Roberts K. Understanding pancreatic exocrine insufficiency and replacement therapy in pancreatic cancer. Eur. J. Surg. Oncol. 2021;47:539–544. doi: 10.1016/j.ejso.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 44.Chirletti Professor P., Peparini N., Caronna R., Papini F., Vietri Professor F., Gualdi G. Monitoring Fibrosis of the Pancreatic Remnant after a Pancreaticoduodenectomy with Dynamic MRI: Are the Results Independent of the Adopted Reconstructive Technique? J. Surg. Res. 2010;164:e49–e52. doi: 10.1016/j.jss.2010.05.065. [DOI] [PubMed] [Google Scholar]
- 45.Zaccari P., Ribichini E., Stigliano S., Serrao G., Scalese G., Caronna R., Chirletti P., Severi C. Occurrence of Pathological Abdominal Fat Distribution After Pancreaticoduodenectomy at Long-term Follow-up: A Single-Center Experience. Pancreas. 2021;50:E15–E16. doi: 10.1097/MPA.0000000000001725. [DOI] [PubMed] [Google Scholar]
- 46.Johnson C.D., Arbuckle R., Bonner N., Connett G., Dominguez-Munoz E., Levy P., Staab D., Williamson N., Lerch M.M. Qualitative Assessment of the Symptoms and Impact of Pancreatic Exocrine Insufficiency (PEI) to Inform the Development of a Patient-Reported Outcome (PRO) Instrument. Patient. 2017;10:615–628. doi: 10.1007/s40271-017-0233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Johnson C.D., Williamson N., Janssen-van Solingen G., Arbuckle R., Johnson C., Simpson S., Staab D., Dominguez-Munoz E., Levy P., Connett G., et al. Psychometric evaluation of a patient-reported outcome measure in pancreatic exocrine insufficiency (PEI) Pancreatology. 2019;19:182–190. doi: 10.1016/j.pan.2018.11.013. [DOI] [PubMed] [Google Scholar]
- 48.Gilliland T.M., Villafane-Ferriol N., Shah K.P., Shah R.M., Tran Cao H.S., Massarweh N.N., Silberfein E.J., Choi E.A., Hsu C., McElhany A.L., et al. Nutritional and Metabolic Derangements in Pancreatic Cancer and Pancreatic Resection. Nutrients. 2017;9:243. doi: 10.3390/nu9030243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lindkvist B., Phillips M.E., Domínguez-Muñoz J.E. Clinical, anthropometric and laboratory nutritional markers of pancreatic exocrine insufficiency: Prevalence and diagnostic use. Pancreatology. 2015;15:589–597. doi: 10.1016/j.pan.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 50.Shintakuya R., Uemura K., Murakami Y., Kondo N., Nakagawa N., Urabe K., Okano K., Awai K., Higaki T., Sueda T. Sarcopenia is closely associated with pancreatic exocrine insufficiency in patients with pancreatic disease. Pancreatology. 2017;17:70–75. doi: 10.1016/j.pan.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 51.de la Iglesia D., Vallejo-Senra N., López-López A., Iglesias-Garcia J., Lariño-Noia J., Nieto-García L., Domínguez-Muñoz J.E. Pancreatic exocrine insufficiency and cardiovascular risk in patients with chronic pancreatitis: A prospective, longitudinal cohort study. J. Gastroenterol. Hepatol. 2019;34:277–283. doi: 10.1111/jgh.14460. [DOI] [PubMed] [Google Scholar]
- 52.Sikkens E.C.M., Cahen D.L., Koch A.D., Braat H., Poley J.W., Kuipers E.J., Bruno M.J. The prevalence of fat-soluble vitamin deficiencies and a decreased bone mass in patients with chronic pancreatitis. Pancreatology. 2013;13:238–242. doi: 10.1016/j.pan.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 53.Skipworth R.J.E., Stewart G.D., Dejong C.H.C., Preston T., Fearon K.C.H. Pathophysiology of cancer cachexia: Much more than host-tumour interaction? Clin. Nutr. 2007;26:667–676. doi: 10.1016/j.clnu.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 54.Fearon K.C.H., Baracos V.E. Cachexia in pancreatic cancer: New treatment options and measures of success. HPB. 2010;12:323. doi: 10.1111/j.1477-2574.2010.00178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Partelli S., Frulloni L., Minniti C., Bassi C., Barugola G., D’Onofrio M., Crippa S., Falconi M. Faecal elastase-1 is an independent predictor of survival in advanced pancreatic cancer. Dig. Liver Dis. 2012;44:945–951. doi: 10.1016/j.dld.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 56.Heerkens H.D., van Berkel L., Tseng D.S.J., Monninkhof E.M., van Santvoort H.C., Hagendoorn J., Borel Rinkes I.H.M., Lips I.M., Intven M., Molenaar I.Q. Long-term health-related quality of life after pancreatic resection for malignancy in patients with and without severe postoperative complications. HPB. 2018;20:188–195. doi: 10.1016/j.hpb.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 57.Landers A., Brown H., Strother M. The effectiveness of pancreatic enzyme replacement therapy for malabsorption in advanced pancreatic cancer, a pilot study. Palliat. Care Res. Treat. 2019;12:1178224218825270. doi: 10.1177/1178224218825270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seiler C.M., Izbicki J., Varga-Szabõ L., Czakõ L., Fiõk J., Sperti C., Lerch M.M., Pezzilli R., Vasileva G., Pap Á., et al. Randomised clinical trial: A 1-week, double-blind, placebo-controlled study of pancreatin 25 000 Ph. Eur. minimicrospheres (Creon 25000 MMS) for pancreatic exocrine insufficiency after pancreatic surgery, with a 1-year open-label extension. Aliment. Pharmacol. Ther. 2013;37:691–702. doi: 10.1111/apt.12236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Roberts K.J., Bannister C.A., Schrem H. Enzyme replacement improves survival among patients with pancreatic cancer: Results of a population based study. Pancreatology. 2019;19:114–121. doi: 10.1016/j.pan.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 60.Roberts K.J., Schrem H., Hodson J., Angelico R., Dasari B.V.M., Coldham C.A., Marudanayagam R., Sutcliffe R.P., Muiesan P., Isaac J., et al. Pancreas exocrine replacement therapy is associated with increased survival following pancreatoduodenectomy for periampullary malignancy. HPB. 2017;19:859–867. doi: 10.1016/j.hpb.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 61.Pancreatic Cancer in Adults: Diagnosis and Management NICE Guideline. 2018. [(accessed on 3 January 2023)]. Available online: www.nice.org.uk/guidance/ng85.
- 62.Phillips M.E., Hopper A.D., Leeds J.S., Roberts K.J., McGeeney L., Duggan S.N., Kumar R. Consensus for the management of pancreatic exocrine insufficiency: UK practical guidelines. BMJ Open Gastroenterol. 2021;8:e000643. doi: 10.1136/bmjgast-2021-000643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim H., Yoon Y.S., Han Y., Kwon W., Kim S.W., Han H.S., Yoon D.S., Park J.S., Park S.J., Han S.S., et al. Effects of pancreatic enzyme replacement therapy on body weight and nutritional assessments after pancreatoduodenectomy in a randomized trial. Clin. Gastroenterol. Hepatol. 2020;18:926–934. doi: 10.1016/j.cgh.2019.08.061. [DOI] [PubMed] [Google Scholar]
- 64.Bruno M.J., Haverkort E.B., Tijssen G.P., Tytgat G.N.J., Van Leeuwen D.J. Placebo controlled trial of enteric coated pancreatin microsphere treatment in patients with unresectable cancer of the pancreatic head region. Gut. 1998;42:92–96. doi: 10.1136/gut.42.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sherman M.H., Yu R.T., Engle D.D., Ding N., Atkins A.R., Tiriac H., Collisson E.A., Connor F., Van Dyke T., Kozlov S., et al. Vitamin D Receptor-Mediated Stromal Reprogramming Suppresses Pancreatitis and Enhances Pancreatic Cancer Therapy. Cell. 2014;159:80. doi: 10.1016/j.cell.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cho M., Peddi P.F., Ding K., Chen L., Thomas D., Wang J., Lockhart A.C., Tan B., Wang-Gillam A. Vitamin D deficiency and prognostics among patients with pancreatic adenocarcinoma. J. Transl. Med. 2013;11:1–6. doi: 10.1186/1479-5876-11-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Frost F., Kacprowski T., Rühlemann M., Bülow R., Kühn J.P., Franke A., Heinsen F.A., Pietzner M., Nauck M., Völker U., et al. Impaired Exocrine Pancreatic Function Associates With Changes in Intestinal Microbiota Composition and Diversity. Gastroenterology. 2019;156:1010–1015. doi: 10.1053/j.gastro.2018.10.047. [DOI] [PubMed] [Google Scholar]
- 68.Frost F., Weiss F.U., Sendler M., Kacprowski T., Rühlemann M., Bang C., Franke A., Völker U., Völzke H., Lamprecht G., et al. The Gut Microbiome in Patients With Chronic Pancreatitis Is Characterized by Significant Dysbiosis and Overgrowth by Opportunistic Pathogens. Clin. Transl. Gastroenterol. 2020;11:e00232. doi: 10.14309/ctg.0000000000000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Petersen C., Round J.L. Defining dysbiosis and its influence on host immunity and disease. Cell. Microbiol. 2014;16:1024–1033. doi: 10.1111/cmi.12308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Trespi E., Ferrieri A. Intestinal bacterial overgrowth during chronic pancreatitis. Curr. Med. Res. Opin. 1999;15:47–52. doi: 10.1185/03007999909115173. [DOI] [PubMed] [Google Scholar]
- 71.Li J.J., Zhu M., Kashyap P.C., Chia N., Tran N.H., McWilliams R.R., Bekaii-Saab T.S., Ma W.W. The role of microbiome in pancreatic cancer. Cancer Metastasis Rev. 2021;40:777. doi: 10.1007/s10555-021-09982-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sammallahti H., Kokkola A., Rezasoltani S., Ghanbari R., Aghdaei H.A., Knuutila S., Puolakkainen P., Sarhadi V.K. Microbiota Alterations and Their Association with Oncogenomic Changes in Pancreatic Cancer Patients. Int. J. Mol. Sci. 2021;22:12978. doi: 10.3390/ijms222312978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Merali N., Chouari T., Kayani K., Rayner C.J., Jiménez J.I., Krell J., Giovannetti E., Bagwan I., Relph K., Rockall T.A., et al. A Comprehensive Review of the Current and Future Role of the Microbiome in Pancreatic Ductal Adenocarcinoma. Cancers. 2022;14:1020. doi: 10.3390/cancers14041020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pandol S. The Exocrine Pancreas. Morgan & Claypool Life Sciences; San Rafael, CA, USA: 2010. [PubMed] [Google Scholar]
- 75.Nicetto D., McCarthy R.L., Zaret K.S. Epigenetic Mechanisms in Liver and Pancreas Generation and Regeneration. Epigenetics Regen. 2019;11:231–257. doi: 10.1016/B978-0-12-814879-2.00010-8. [DOI] [Google Scholar]
- 76.Struyvenberg M.R., Martin C.R., Freedman S.D. Practical guide to exocrine pancreatic insufficiency—Breaking the myths. BMC Med. 2017;15:29. doi: 10.1186/s12916-017-0783-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dominici R., Franzini C. Fecal elastase-1 as a test for pancreatic function: A review. Clin. Chem. Lab. Med. 2002;40:325–332. doi: 10.1515/CCLM.2002.051. [DOI] [PubMed] [Google Scholar]
- 78.Anaizi A., Hart P.A., Conwell D.L. Diagnosing Chronic Pancreatitis. Dig. Dis. Sci. 2017;62:1713. doi: 10.1007/s10620-017-4493-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rubinstein E., Mark Z., Haspel J., Ben-Ari G., Dreznik Z., Mirelman D., Tadmor A. Antibacterial Activity of the Pancreatic Fluid. Gastroenterology. 1985;88:927–932. doi: 10.1016/S0016-5085(85)80009-3. [DOI] [PubMed] [Google Scholar]
- 80.Pierzynowski S.G., Sharma P., Sobczyk J., Garwacki S., Barej W., Westrom B. Comparative study of antibacterial activity of pancreatic juice in six mammalian species. Pancreas. 1993;8:546–550. doi: 10.1097/00006676-199309000-00003. [DOI] [PubMed] [Google Scholar]
- 81.Ahuja M., Schwartz D.M., Tandon M., Son A., Zeng M., Swaim W., Eckhaus M., Hoffman V., Cui Y., Xiao B., et al. Orai1-Mediated Antimicrobial Secretion from Pancreatic Acini Shapes the Gut Microbiome and Regulates Gut Innate Immunity. Cell Metab. 2017;25:635–646. doi: 10.1016/j.cmet.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bassi C., Fontana R., Vesentini S., Cavallini G., Marchiori L., Falconi M., Corra S., Pederzoli P. Antibacterial and mezlocillin-enhancing activity of pure human pancreatic fluid. Int. J. Pancreatol. 1991;10:293–297. doi: 10.1007/BF02924168. [DOI] [PubMed] [Google Scholar]
- 83.Kościuczuk E.M., Lisowski P., Jarczak J., Strzałkowska N., Jóźwik A., Horbańczuk J., Krzyżewski J., Zwierzchowski L., Bagnicka E. Cathelicidins: Family of antimicrobial peptides. A review. Mol. Biol. Rep. 2012;39:10957–10970. doi: 10.1007/s11033-012-1997-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhou C.H., Meng Y.T., Xu J.J., Fang X., Zhao J.L., Zhou W., Zhao J., Han J.C., Zhang L., Wang K.X., et al. Altered diversity and composition of gut microbiota in Chinese patients with chronic pancreatitis. Pancreatology. 2020;20:16–24. doi: 10.1016/j.pan.2019.11.013. [DOI] [PubMed] [Google Scholar]
- 85.Herremans K.M., Riner A.N., Cameron M.E., Trevino J.G. The Microbiota and Cancer Cachexia. Int. J. Mol. Sci. 2019;20:6267. doi: 10.3390/ijms20246267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Panebianco C., Villani A., Potenza A., Favaro E., Finocchiaro C., Perri F., Pazienza V. Targeting Gut Microbiota in Cancer Cachexia: Towards New Treatment Options. Int. J. Mol. Sci. 2023;24:1849. doi: 10.3390/ijms24031849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ritz S., Hahn D., Wami H.T., Tegelkamp K., Dobrindt U., Schnekenburger J. Gut microbiome as a response marker for pancreatic enzyme replacement therapy in a porcine model of exocrine pancreas insufficiency. Microb. Cell Fact. 2020;19:221. doi: 10.1186/s12934-020-01482-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Nishiyama H., Nagai T., Kudo M., Okazaki Y., Azuma Y., Watanabe T., Goto S., Ogata H., Sakurai T. Supplementation of pancreatic digestive enzymes alters the composition of intestinal microbiota in mice. Biochem. Biophys. Res. Commun. 2017;495:273–279. doi: 10.1016/j.bbrc.2017.10.130. [DOI] [PubMed] [Google Scholar]
- 89.Isaiah A., Parambeth J.C., Steiner J.M., Lidbury J.A., Suchodolski J.S. The fecal microbiome of dogs with exocrine pancreatic insufficiency. Anaerobe. 2017;45:50–58. doi: 10.1016/j.anaerobe.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 90.Guo W., Zhang Y., Guo S., Mei Z., Liao H., Dong H., Wu K., Ye H., Zhang Y., Zhu Y., et al. Tumor microbiome contributes to an aggressive phenotype in the basal-like subtype of pancreatic cancer. Commun. Biol. 2021;4:1019. doi: 10.1038/s42003-021-02557-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Polansky O., Sekelova Z., Faldynova M., Sebkova A., Sisak F., Rychlik I. Important Metabolic Pathways and Biological Processes Expressed by Chicken Cecal Microbiota. Appl. Environ. Microbiol. 2015;82:1569–1576. doi: 10.1128/AEM.03473-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Topping D.L., Clifton P.M. Short-chain fatty acids and human colonic function: Roles of resistant starch and nonstarch polysaccharides. Physiol. Rev. 2001;81:1031–1064. doi: 10.1152/physrev.2001.81.3.1031. [DOI] [PubMed] [Google Scholar]
- 93.Takada T., Kurakawa T., Tsuji H., Nomoto K. Fusicatenibacter saccharivorans gen. nov., sp. nov., isolated from human faeces. Int. J. Syst. Evol. Microbiol. 2013;63:3691–3696. doi: 10.1099/ijs.0.045823-0. [DOI] [PubMed] [Google Scholar]
- 94.Ménard S., Candalh C., Bambou J.C., Terpend K., Cerf-Bensussan N., Heyman M. Lactic acid bacteria secrete metabolites retaining anti-inflammatory properties after intestinal transport. Gut. 2004;53:821–828. doi: 10.1136/gut.2003.026252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hoque R., Farooq A., Ghani A., Gorelick F., Mehal W.Z. Lactate reduces liver and pancreatic injury in Toll-like receptor- and inflammasome-mediated inflammation via GPR81-mediated suppression of innate immunity. Gastroenterology. 2014;146:1763–1774. doi: 10.1053/j.gastro.2014.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Johnston C.D., Bullman S. The tumour-associated microbiome. Nat. Rev. Gastroenterol. Hepatol. 2022;19:347–348. doi: 10.1038/s41575-022-00609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liu J., Zhang Y. Intratumor microbiome in cancer progression: Current developments, challenges and future trends. Biomark. Res. 2022;10:1–18. doi: 10.1186/s40364-022-00381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Balachandran V.P., Łuksza M., Zhao J.N., Makarov V., Moral J.A., Remark R., Herbst B., Askan G., Bhanot U., Senbabaoglu Y., et al. Identification of unique neoantigen qualities in long-term survivors of pancreatic cancer. Nature. 2017;551:S12–S16. doi: 10.1038/nature24462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nejman D., Livyatan I., Fuks G., Gavert N., Zwang Y., Geller L.T., Rotter-Maskowitz A., Weiser R., Mallel G., Gigi E., et al. The human tumor microbiome is composed of tumor type-specific intracellular bacteria. Science. 2020;368:973–980. doi: 10.1126/science.aay9189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sayin S., Rosener B., Li C.G., Ho B., Ponomarova O., Ward D.V., Walhout A.J.M., Mitchell A. Evolved bacterial resistance to the chemotherapy gemcitabine modulates its efficacy in co-cultured cancer cells. Elife. 2023;12:1–23. doi: 10.7554/eLife.83140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tintelnot J., Xu Y., Lesker T.R., Schönlein M., Konczalla L., Giannou A.D., Pelczar P., Kylies D., Puelles V.G., Bielecka A.A., et al. Microbiota-derived 3-IAA influences chemotherapy efficacy in pancreatic cancer. Nature. 2023;615:168–174. doi: 10.1038/s41586-023-05728-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fulop D.J., Zylberberg H.M., Wu Y.L., Aronson A., Labiner A.J., Wisnivesky J., Cohen D.J., Sigel K.M., Lucas A.L. Association of Antibiotic Receipt with Survival Among Patients with Metastatic Pancreatic Ductal Adenocarcinoma Receiving Chemotherapy. JAMA Netw. Open. 2023;6:e234254. doi: 10.1001/jamanetworkopen.2023.4254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pushalkar S., Hundeyin M., Daley D., Zambirinis C.P., Kurz E., Mishra A., Mohan N., Aykut B., Usyk M., Torres L.E., et al. The Pancreatic Cancer Microbiome Promotes Oncogenesis by Induction of Innate and Adaptive Immune Suppression. Cancer Discov. 2018;8:403–416. doi: 10.1158/2159-8290.CD-17-1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Thomas R.M., Gharaibeh R.Z., Gauthier J., Beveridge M., Pope J.L., Guijarro M.V., Yu Q., He Z., Ohland C., Newsome R., et al. Intestinal microbiota enhances pancreatic carcinogenesis in preclinical models. Carcinogenesis. 2018;39:1068–1078. doi: 10.1093/carcin/bgy073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sethi V., Kurtom S., Tarique M., Lavania S., Malchiodi Z., Hellmund L., Zhang L., Sharma U., Giri B., Garg B., et al. Gut Microbiota Promotes Tumor Growth in Mice by Modulating Immune Response. Gastroenterology. 2018;155:33–37.e6. doi: 10.1053/j.gastro.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Daley D. The role of the microbiome in pancreatic oncogenesis. Int. Immunol. 2022;34:447–454. doi: 10.1093/intimm/dxac036. [DOI] [PubMed] [Google Scholar]
- 107.Benini L., Amodio A., Campagnola P., Agugiaro F., Cristofori C., Micciolo R., Magro A., Gabbrielli A., Cabrini G., Moser L., et al. Fecal elastase-1 is useful in the detection of steatorrhea in patients with pancreatic diseases but not after pancreatic resection. Pancreatology. 2013;13:38–42. doi: 10.1016/j.pan.2012.11.307. [DOI] [PubMed] [Google Scholar]
- 108.Halloran C.M., Cox T.F., Chauhan S., Raraty M.G.T., Sutton R., Neoptolemos J.P., Ghaneh P. Partial Pancreatic Resection for Pancreatic Malignancy Is Associated with Sustained Pancreatic Exocrine Failure and Reduced Quality of Life: A Prospective Study. Pancreatology. 2011;11:535–545. doi: 10.1159/000333308. [DOI] [PubMed] [Google Scholar]
- 109.Domínguez-Muñoz J., Nieto L., Pancreas M.V. Development and diagnostic accuracy of a breath test for pancreatic exocrine insufficiency in chronic pancreatitis. Pancreas. 2016;45:241–247. doi: 10.1097/MPA.0000000000000434. [DOI] [PubMed] [Google Scholar]
- 110.Powell-Brett S., Hall L., Edwards M., Roberts K. A systematic review and meta-analysis of the accuracy and methodology of the 13C mixed triglyceride breath test for the evaluation of pancreatic function. Pancreatology. 2023;23:283–293. doi: 10.1016/j.pan.2023.02.004. [DOI] [PubMed] [Google Scholar]
- 111.Halle-Smith J.M., Hall L.A., Powell-Brett S.F., Merali N., Frampton A., Roberts K.J. Realising the therapeutic potential of the human microbiota in metastatic pancreatic ductal adenocarcinoma. Clin. Surg. Oncol. 2023;2:100020. doi: 10.1016/j.cson.2023.100020. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.