Abstract
The issue of tight glucose control with intensive insulin therapy in critically ill patients remains controversial. Although compelling evidence supports this strategy in postoperative patients who have undergone cardiac surgery, the use of tight glucose control has been challenged in other situations, including in medical critically ill patients and in those who have undergone non-cardiac surgery. Similarly, the mechanisms that underlie the effects of high-dose insulin are not fully elucidated. These arguments emphasize the need to study the effects of tight glucose control in a large heterogeneous cohort of intensive care unit patients.
Keywords: cardiac surgery, critically ill, hyperglycemia, insulin, metabolism
Until the end of the past millenium, relatively little attention was given to control of blood sugar levels. In critically ill patients, hyperglycaemia was considered to be physiological because it results from the metabolic and hormonal changes that accompany the stress response to injury. In most intensive care units (ICUs), blood sugar was checked every 4–6 hours and hyperglycaemia (defined as blood sugar levels >10–12 mmol/l [180–216 mg/dl]) was corrected by subcutaneous or intravenous insulin. The presence of pre-existing diabetes mellitus or post-neurosurgical status often prompted more intense control of hyperglycaemia. Furthermore, the issue of glucose control was discussed in few sessions or satellite symposia during intensive care meetings.
The deleterious effects of hyperglycaemia during critical illness have been characterized over the past few years, and include an increased susceptibility to infections and thromboses, macrovascular and microvascular changes, and delayed wound healing, among other effects (for review [1]). Renewed interest in control of hyperglycaemia in critically ill patients (Fig. 1) followed the publication of a study conducted by Van den Berghe and coworkers in 2001 [2]. Those investigators reported a 43% decrease in relative intensive care mortality as well as consistent decreases in several surrogate markers of disease severity in patients randomly assigned to tight glucose control by intensive intravenous insulin therapy. A post hoc multivariate logistic regression analysis of these data suggested that control of hyperglycaemia played a more important role than did the amount of insulin administered [3]. Interestingly enough, at least two recent retrospective, large-scale studies [4,5] confirmed that outcome was improved in patients whose average blood glucose was maintained below 8 mmol/l (144 mg/dl; Table 1).
Figure 1.
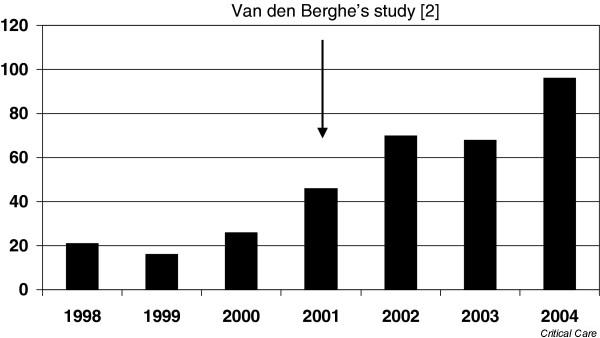
Number of publications retrieved from the Medline (Pubmed®) database using the keywords 'insulin therapy' or 'hyperglycemia' plus 'critically ill' from 1998 to September 2004.
Table 1.
Features of recent studies of glucose control in intensive care units
| Reference | ||||
| [2] | [4] | [5] | [7] | |
| Design | Prospective, interventional | Retrospective, observational | Retrospective, observational | Retrospective, observational |
| Target glucose levels (mmol/l) | ||||
| Intervention | 4.4–6.1 | <8.0 | 4.4–7.8 | |
| Control | 10.0–11.1 | Not available | 10.0–11.1 | >12.0 |
| Types of admission (n) | ||||
| Surgical | 1548 | 462 | 573 | 160 |
| Medical | 0 | 61 | 1027 | 0 |
| Cardiac surgery (% of total) | 63 | 85 | 0 | 0 |
| Median APACHE II score | 9 | 16 | 16 | Not available |
| ICU mortality (%) | ||||
| Intervention | 4.6 | Not available | 14.8 | 3.3 |
| Control | 8.0 | 20.9 | ||
| Primary end-points | ICU mortality | ICU mortality | ICU mortality | Infection rate, length of hospital stay |
| Secondary end-points | In-hospital mortality, organ dysfunction, tranfusion rate, critical illness polyneuropathy, infection rate | Organ dysfunction, transfusion rate, length of ICU stay, infection rate | ||
APACHE, Acute Physiology and Chronic Health Evaluation; ICU, intensive care unit.
Although the findings reported by Van den Berghe and coworkers are impressive, some concern arose regarding the applicability of these results to other types of patients. Of the patients studied, 63% were admitted for follow up after cardiac surgery; this high proportion was felt to be consistent with a particular benefit from tight glucose control with intensive insulin in these patients, but there is uncertainty regarding whether tight glucose control is beneficial in patients who have not undergone cardiac surgery. Fear of life-threatening hypoglycaemia and increased workload and costs probably underlie the reluctance of many intensivists to launch systematic protocols of tight glucose control. Indeed, many intensivists still use a high glucose threshold (10 mmol/l [180 mg/dl]) [6]. In a European survey (unpublished data) we found considerable variation in the glycaemic thresholds employed in ICUs, which ranged from 6 to 11.1 mmol/l (108–200 mg/dl).
Some arguments against generalized use of tight glucose control are reported in the present issue of Critical Care by Vriesendorp and coworkers [7]. In a retrospective study performed at one centre in Amsterdam, those authors found that, after oesophageal surgery in patients without significant cardiovascular compromise (ASA class I–II), postoperative hyperglycaemia was not a risk factor for infectious complications. Only by univariate analysis were they able to find an improvement in patients with blood glucose levels below 9.3 mmol/l (167 mg/dl) in terms of length of ICU stay. These findings differ strikingly from those of other studies [2,4,5]. Although the report by Vriesendorp and coworkers challenges the concept of tight glucose control, it can hardly be considered a major piece of evidence against it. Indeed, blood glucose concentrations were presented as means of values recorded only over 48 hours, whereas the ICU stay extended up to 71 days, with a median of 3 days. Insulin was administered to only 9% of the patients during the 48-hour period of observation. In addition, patients received a mean of only 22.5 g glucose/day, and were fed early after surgery with an enteral solution of 'immunonutrients' – a potential confounding factor with respect to infectious morbidity. However, despite these limitations, as well as others that are acknowledged by the authors, the findings of the study support the hypothesis that tight glucose control could be of greater benefit to patients with cardiovascular disease than to those without.
In conclusion, as recently suggested by Van den Berghe [8], further studies are needed to confirm the benefits of tight blood glucose control with intensive insulin therapy in a heterogeneous population of ICU patients. Hence, a large randomized prospective multicentre trial is warranted. Such study will also help in determining the physiological importance of the effects of insulin and, more importantly, will provide intensive care workers with key information for guiding the management of blood glucose in critically ill patients.
Abbreviation
ICU = intensive care unit.
Competing interests
The author(s) declare that they have no competing interests.
See related research article http://ccforum.com/content/8/6/R437
References
- Preiser JC, Devos P, Van den Berghe G. Tight control of glycaemia in critically ill patients. Curr Opin Clin Nutr Metab Care. 2002;5:533–537. doi: 10.1097/00075197-200209000-00012. [DOI] [PubMed] [Google Scholar]
- Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P, Bouillon R. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359–1367. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- Van den Berghe G, Wouters PJ, Bouillon R, Weekers F, Verwaest C, Schetz M, Vlasselaers D, Ferdinande P, Lauwers P. Outcome benefit of intensive insulin therapy in the critically ill: Insulin dose versus glycemic control. Crit Care Med. 2003;31:359–366. doi: 10.1097/01.CCM.0000045568.12881.10. [DOI] [PubMed] [Google Scholar]
- Finney SJ, Zekveld C, Elia A, Evans TW. Glucose control and mortality in critically ill patients. JAMA. 2003;290:2041–2047. doi: 10.1001/jama.290.15.2041. [DOI] [PubMed] [Google Scholar]
- Krinsley JS. Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc . 2004;79:992–1000. doi: 10.4065/79.8.992. [DOI] [PubMed] [Google Scholar]
- McMullin J, Brozek J, Jaeschke R, Hamielec C, Dhingra V, Rocker G, Freitag A, Gibson J, Cook D. Glycemic control in the ICU: a multicenter survey. Intensive Care Med. 2004;30:798–803. doi: 10.1007/s00134-004-2242-4. [DOI] [PubMed] [Google Scholar]
- Vriesendorp TM, DeVries JH, Hulscher JBF, Holleman F, van Lanschot JJB, Hoekstra JBL. Early postoperative hyperglycaemia is not a risk factor for infectious complications and prolonged in-hospital stay in patients undergoing oesophagectomy: a retrospective analysis of a prospective trial. Crit Care. 2004;8:R437–R442. doi: 10.1186/cc2970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Berghe G. Tight blood glucose control with insulin in 'real-life' intensive care. Mayo Clin Proc. 2004;79:977–978. doi: 10.4065/79.8.977. [DOI] [PubMed] [Google Scholar]


