Abstract
Background
Homebirth preference is the intention/plan to give birth outside health facilities with the help of unskilled birth attendants. The preference to give birth at home without a skilled birth attendant leads to care-seeking delays, intrapartum mortality, multiple stillbirths, and postpartum morbidities and mortality. Therefore, this study aimed to estimate the pooled prevalence of homebirth preference and associated factors among pregnant women in Ethiopia.
Methods
Search of Google Scholar, Medline, PubMed, Cochrane Library and Web of Science were done for this study from 20th August 2022 to 6th November 2022. For data extraction and analysis, the standardized data extraction checklist and Stata version 14 were used respectively. Sentence as “Cochrane Q test statistics and I2 statistics were used to check heterogeneity of the studies. The pooled prevalence of homebirth preference was estimated using a random-effects model. The association between homebirth preference and independent variables was determined using an odd ratio with a 95% confidence interval. A funnel plot and Egger’s test were used to assess publication bias.
Results
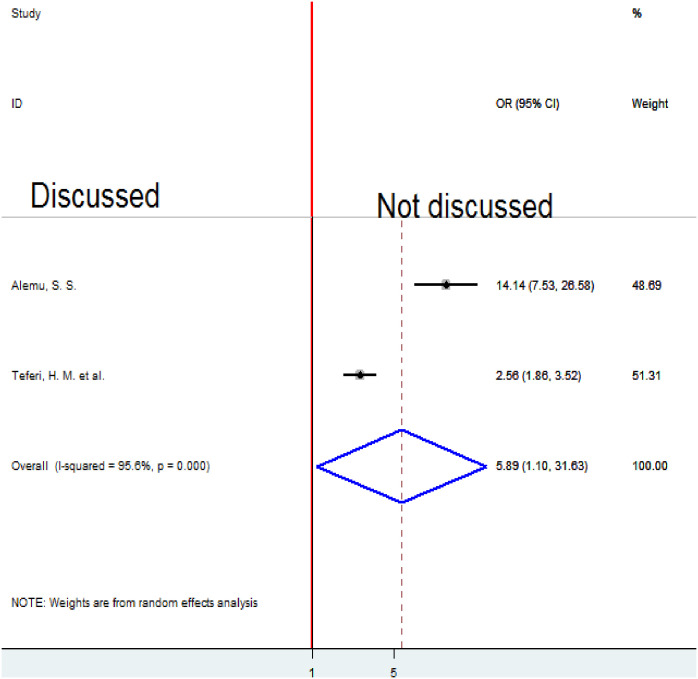
A total of 976 research articles were identified. Seven studies that fulfilled eligibility criteria were included in this systematic review and meta-analysis. The pooled prevalence of homebirth preference in Ethiopia was 39.62% (95% CI 27.98, 51.26). The current meta-analysis revealed that average monthly income <1800 ETB (OR = 2.66, 95% CI 1.44, 4.90) lack of ANC follow-up (OR = 2.57, 95%CI 1.32, 5.01), being multipara (OR = 1.77, 95%CI 1.39, 2.25), poor knowledge about obstetric danger sign (OR = 5.75, 95%CI 1.o2, 32.42), and not discussing the place of delivery with a partner (OR = 5.89 (95%CI 1.1, 31.63) were significantly associated with homebirth preference.
Conclusion
This systematic review and meta-analysis examined the substantial prevalence of homebirth preference in Ethiopia which may contribute maternal and child health crisis. The homebirth preference was associated with low average monthly income (<1800 ETB), lack of ANC follow-up, multipara, poor knowledge about obstetric danger signs, and not discussing with their partner the place of delivery. Improving knowledge of pregnant women about the benefit of health facility delivery and obstetric danger signs is necessary to decrease the prevalence of homebirth preference; for these can reduce negative outcomes occurred during delivery.
Background
Homebirth preference is the intention/plan to give birth outside health facilities with the help of unskilled birth attendants [1]. The preference to give birth at home without a skilled birth attendant leads to care-seeking delays, intrapartum mortality, multiple stillbirths, and postpartum morbidities and mortality [2]. Once a mother plans to give birth at home, the probability of giving birth in healthcare facilities is reduced which increases the risk of maternal fatality rate, but in Sub-Saharan Africa, many women still prefer to give birth at home without a skilled birth attendant [3]. Even though Ethiopia has devised critical strategies, including promoting institutional delivery services for lowering maternal morbidity and mortality, a significant number of women gave birth in their homes in the country [4].
In Ethiopia, a substantial percentage of pregnant mothers prefer to give birth at home [5]. According to the 2019 Mini Ethiopian Demographic and Health Survey report, of all live births in the five years before the survey, only 50% were delivered by a skilled provider [6]. In some parts of Ethiopia regions, more than three-fourths of mothers gave birth at home [4].
Although most maternal health care is free in Ethiopia, home birth rates are reported to be high [7]. Giving birth at home results in premature birth, umbilical cord infection, being accidentally knocked on the head during delivery, breach presentation, and severe maternal anemia which are the main causes of infant mortality [8]. Patients with postpartum hemorrhage who gave birth outside of a hospital had a higher risk of receiving blood transfusion [9].
In Ethiopia, different studies were conducted to determine the homebirth preference and associated factors among pregnant women, which show a great variation across different geographical areas and periods due to different factors such as lack of transportation, low awareness of the advantages of skilled attendance at delivery, little role in making decisions and economic constraints and not discussing the place of delivery with a partner [1, 4, 5, 10].
To guarantee the prevention, detection, and management of problems, all women should have access to skilled care during pregnancy and childbirth. Despite Ethiopia having created several measures for promoting institutional delivery services, home deliveries are still high in different areas [1, 5].
Even though studies have reported on homebirth preference and associated factors among pregnant women in Ethiopia, there is no nationally representative pooled data on homebirth preference and associated factors among pregnant women in Ethiopia. Furthermore, previous studies report varying between regions within the country. Therefore, this systematic review and meta-analysis aimed to provide pooled representative national data on homebirth preference and associated factors in Ethiopia.
Methods
Search strategy
Initially, the PROSPERO database and database of abstracts of reviews of effects (DARE) (http://www.library.UCSF.edu) were searched to check whether published and/or ongoing projects exist related to the topic. The research articles’ search strategy, selection of studies, data extraction, and result reporting were done following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11, 12]. A PICO principle was adapted for searching terms. The research articles used for this systematic review and meta-analysis were identified through Google Scholar, Medline/Pub Med, Cochrane Library, the Web of Science, Hinari, Science Direct, ProQuest, African Journals Online, and online university repositories (University of Gondar, Addis Ababa, Jimma, and Haramaya University) search engines by developing search strategies. Boolean operators such as OR, AND, and NOT were used with search terms such as “Preference”, “Desire”, “need”, “intention”,”choice”, “homebirth”, “home delivery”, “Place of delivery”, “place of Birth”, “unskilled birth attendant”, “associated factors” “determinants”, “risk factors”, “predictors”) “reproductive age women”, “pregnant women/mother” and “Ethiopia”. Identified research articles were screened to make sure that all relevant literature was included. Literature was downloaded to Endnote (version X7.8) to maintain and manage citations and facilitate the review process [13].
Eligibility criteria
In this systematic review and meta-analysis, we included:-
All studies that were conducted on homebirth preference and/or associated factors among pregnant women in Ethiopia.
All types of articles that were published in the form of journal articles
Master’s theses and dissertations in the English language.
Outcome measurement
There were two main outcomes. The first outcome of interest was the prevalence, the pooled prevalence of pregnant women preferring homebirth. From primary studies, homebirth preference was operationalized as the choice or desire, or intention of women to give birth at their own homes. The second outcome was the factors associated with homebirth preference, which was determined using the odds ratio (OR) and calculated based on binary outcomes from the included primary studies. The variables included in the review were education, average monthly income, transport access, ANC follow-up (Yes versus No), parity (primipara versus multipara), previous place of delivery (home/health institution), discussion on a place of delivery with a partner (discussed/not discussed) and knowledge (poor/ knowledgeable). Women were asked about the history of ANC follow-up for the current pregnancy. The variable was measured by the binary variable "Yes" for those women who used to visit one and above ANC visits and "No" for women who did not visit ANC during the current pregnancy.
Data extraction and quality assessment
The Joanna Briggs Institute (JBI) quality appraisal checklist for cross-sectional studies quality assessment instrument was used to rate the included study’s level of quality [14]. On Microsoft Excel, three data extractors (JW, EM, and ML) extracted data using a standard data extraction checklist. In the beginning, duplicate articles were removed and search results from databases were combined using reference management software (Endnote version X7.8). Following that, research articles were evaluated and disqualified based on their titles and abstracts. The remaining research articles were evaluated based on full-text publications. The eligibility of the primary studies was assessed following the established inclusion and exclusion criteria. The data extraction checklist for the first outcome (prevalence of homebirth choice) contained the authors’ names, year of publication, location (an area where studies were conducted), study design, sample size, response rate, and the number of participants with the homebirth preference. Data were retrieved in two by two table formats for the second outcome (factors associated with homebirth preference), and the log OR was computed based on the results of the source articles. After discussion for potential consensus, discrepancies between the three independent reviewers were resolved by adding more reviewers (MD, AT, WB, and KM). When the included primary articles lacked sufficient information, the corresponding authors of the research articles were contacted via email.
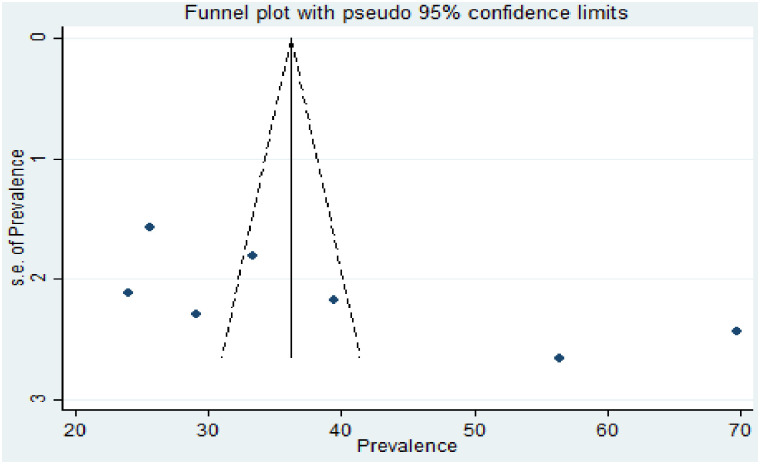
Data analysis and synthesis
The data were exported to STATA version 14.0 and used to calculate the pooled effect size with 95% CI. To check heterogeneity among the included studies, the Cochran Q test (Chi-squared statistic) and I2 statistic on forest plots were computed. Cochran’s Q statistical heterogeneity test is declared statistically significant at p ≤ 0.05. I2 statistics range from 0 to 100% and I2 statistic values of 0, 25, 50, and 75% were considered as no, low, moderate, and high degrees of heterogeneity, respectively [15]. A random-effects model was used to determine the pooled prevalence of homebirth preference and the pooled effect size of associated factors when a high degree of heterogeneity was observed for the first and second outcomes. To identify the source of potential random variation, subgroup analysis was conducted based on the region where the studies were conducted and based on the timing of the study. Meta-regression was computed to see the presence of statistically significant heterogeneity. Publication bias was assessed by using a funnel plot. The symmetry of the funnel plot is an indicator of the absence of publication bias (Fig 5). In addition, Egger’s (p-value = 0.079 weighted regression and Begg’s tests (p-value = 0.051) were used to check the absence of publication bias. Statistical nonsignificance of publication bias was declared at a p-value of greater than 0.05 [16].
Result
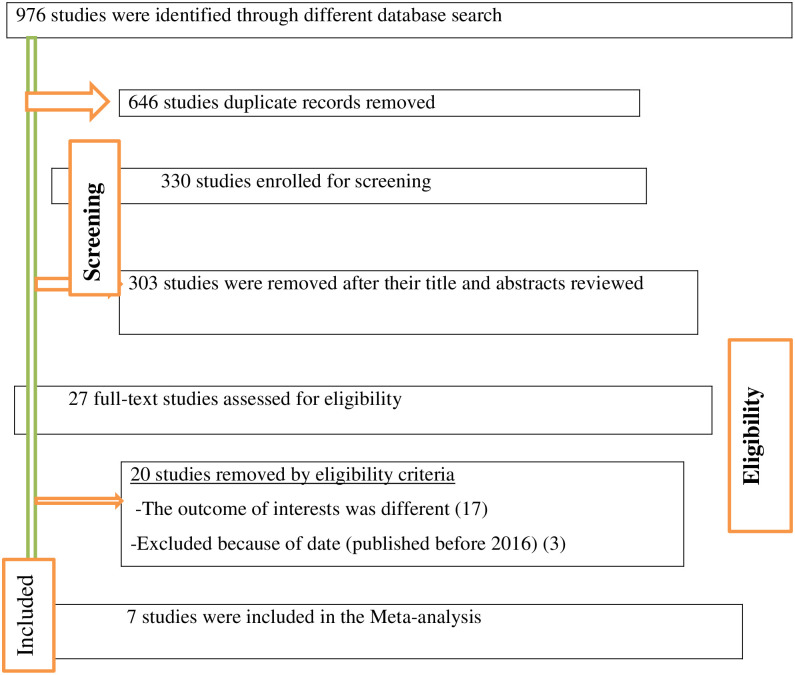
976 studies were found via the data bases, then 646 articles recorded from these studies were found to be duplicates and were eliminated while 303 irrelevant research publications were excluded from our analysis after being reviewed for titles and abstracts. Twenty studies were eliminated after reviewing the whole texts of the remaining publications because they did not adhere to the predetermined eligibility requirements. The final systematic review and meta-analysis included the remaining seven (7) research articles (Fig 1).
Fig 1. PRISMA flow diagram of included studies in the systematic review and meta-analysis of the prevalence of homebirth preference and associated factors among pregnant women in Ethiopia, 2022.
Characteristics of included studies
All of the seven studies included in this study were published between 2019 to 2022 in peer review journals [5, 10, 17–21]. A total of 3458 study participants were included in the current systematic review and meta-analysis. The smallest sample size was 346 from a study conducted in the Amhara region, Simada district [18], and the largest sample size was 769 from a study conducted in SNNPR [10]. All included research articles were cross-sectional studies with 4 prospective cross-sectional study designs nature [5, 17, 19, 21] and 3 retrospective cross-sectional study designs [10, 18, 20]. Regarding study setting, two studies were conducted in the Amhara region [18, 19], two studies in the SNNPR [10, 21], one study was from the Afar region [17], one study was conducted in the Oromia region [20] and one study conducted from PMA survey data [5] (Table 1).
Table 1. Summary of included studies on the prevalence of homebirth preference in Ethiopia, 2022.
| SN | Author | Publication year | Region | Study area | Study design | Sample size | Quality score | Prevalence(95%CI) |
|---|---|---|---|---|---|---|---|---|
| 1 | Alemu et al. [10] | 2019 | SNNR | Wonago | Cross-sectional | 769 | 7 | 25.62(22.53,28.70) |
| 2 | Kahsay et al. [17] | 2019 | Afar | Zone 3 | Cross-sectional | 357 | 7 | 69.75(64.98,74.51) |
| 3 | Mekie and Taklual [18] | 2019 | Amhara | Simada | Cross-sectional | 346 | 8 | 56.36(51.13,61.58) |
| 4 | Tsegaye et al. [19] | 2019 | Amhara | Debretabor | Cross-sectional | 394 | 7 | 29.19(24.70,33.68) |
| 5 | Bekuma et al. [20] | 2020 | Oromia | Jimma Arjo | Cross-sectional | 506 | 8 | 39.53(35.27,43.79) |
| 6 | Alemu et al. [21] | 2022 | SNNPR | Arba Minch S.S | Cross-sectional | 408 | 9 | 24.02(19.87,28.17) |
| 7 | Teferi et al. [5] | 2022 | PMA | PMA survey | Cross-sectional | 678 | 9 | 33.33(29.78,36.88) |
Note: CI; confidence interval, SNNPR; Southern Nation Nationalities, and people region
Prevalence of homebirth preference
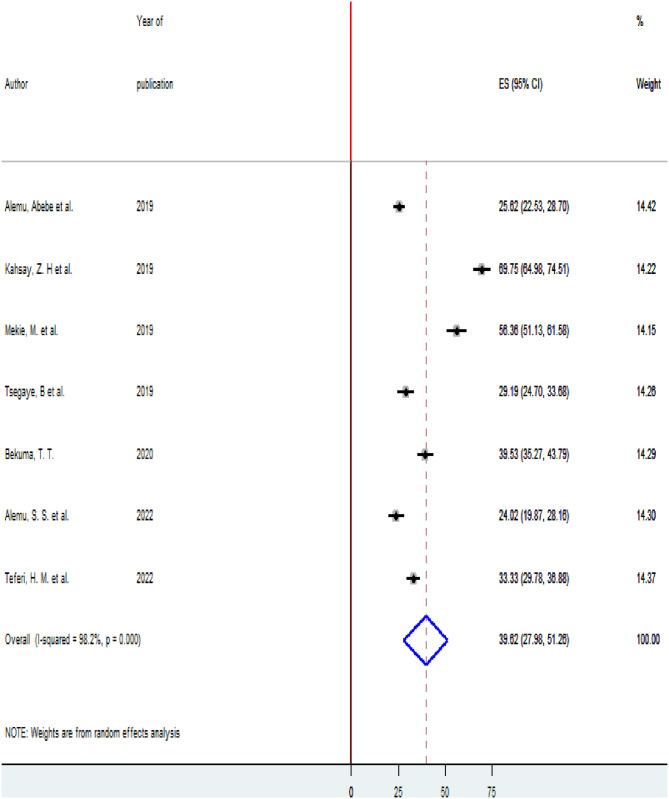
High heterogeneity was observed across the included studies (I2 = 98.2, p < 0.001) thus, a random-effects model was used to estimate the pooled prevalence of homebirth Preference. The prevalence of homebirth Preference was 39.62% (95% CI 27.98, 51.26). The highest 69.75(95% CI 64.98,74.51) prevalence of homebirth Preference was observed in Zone 3, Afar region [17] and the lowest 24.02(19.87,28.17) prevalence of homebirth Preference was reported in Arba Minch zuria surveillance site, SNNPR [21] (Fig 2).
Fig 2. Forest plot of the pooled estimate of the prevalence of homebirth preference in Ethiopia, 2022.
To check for underlying heterogeneity, meta-regression models were done by using sample size and year of publication, but there was statistically insignificant underlying heterogeneity (p = 0.309) and (p = 0.421), respectively (Table 2).
Table 2. Meta-regression analysis based on sample size and year of publication.
| Variables | Coefficients | p-value |
|---|---|---|
| Year of publication | -4.295715 | 0.421 |
| Sample size | -.0471067 | 0.309 |
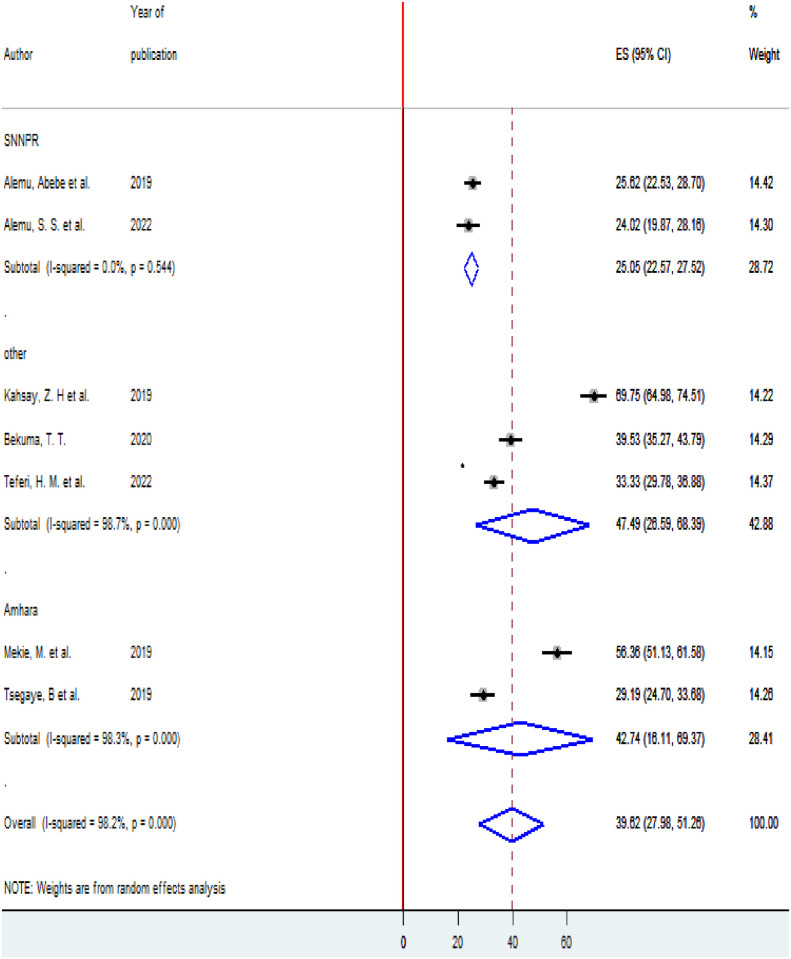
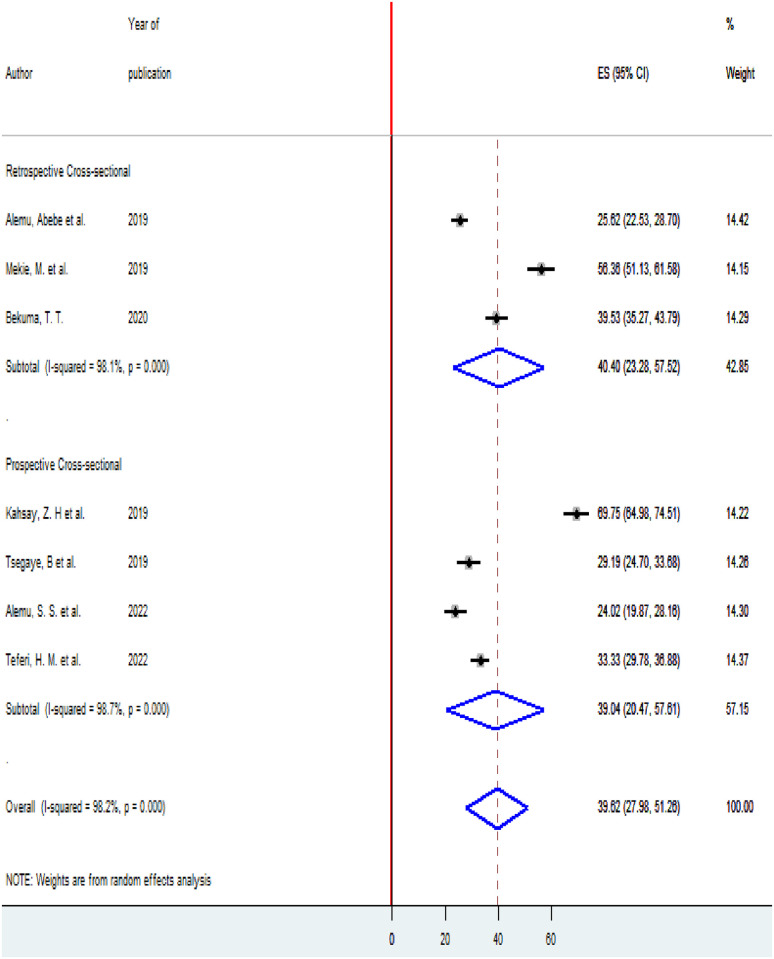
Subgroup analysis
To see heterogeneity among the included studies, subgroup analysis was executed based on the area where the studies were conducted and the timing of studies (prospective and retrospective cross-sectional studies). According to where the studies conducted, the highest prevalence of homebirth Preference 47.49(95% CI 26.59,68.39) was observed in other (Oromia, Afar, and PMA survey data regions) [5, 17, 20] and the lowest prevalence of homebirth Preference 25.05(22.57,27.52) was reported in SNNPR (Fig 3). According to the timing of the study, nearly the prevalence of homebirth Preference was equal among retrospective studies 40.4% (95% CI 23.28, 57.52) and prospective studies 39.04 (95% CI 20.47, 57.81) (Fig 4).
Fig 3. Subgroup analysis of the prevalence of homebirth preference among pregnant women in Ethiopia based on the region, 2022.
Fig 4. Subgroup analysis of the prevalence of homebirth preference among pregnant women in Ethiopia based on the timing of the study, 2022.
Publication bias
To see the presence of publication bias, the graphical funnel plot and Egger’s test at a 5% significance level were executed. The visual examination of the funnel plot presented symmetrically which is an indicator for the absence of publication bias (Fig 5). Egger’s test also showed the absence of publication bias at a 5% significance level (p = 0.079).
Fig 5. Funnel plot with 95% confidence limit of the prevalence of homebirth preference in Ethiopia, 2022.
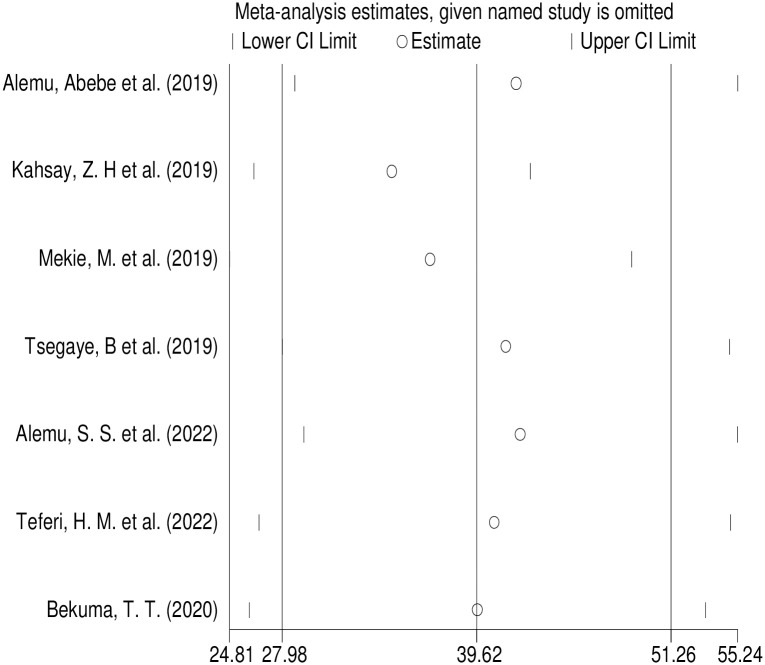
Sensitivity analysis
Outliers were detected by Sensitivity analysis showing that there was no single study that influence the overall included studies (Fig 6).
Fig 6. Result of sensitivity analysis of homebirth preference in Ethiopia, 2022.
Factors associated with homebirth preference
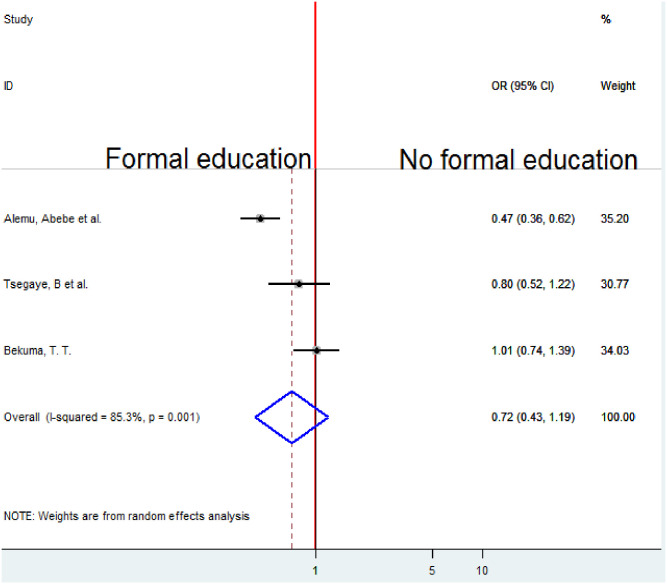
Association between education and homebirth preference
To examine the association between maternal Education and homebirth preference, three studies were included in the analysis [10, 19, 20]. The pooled association between maternal education and homebirth preference was estimated by a random-effects model (I2 = 85.3%, P-value = 0.001). The pooled result of the analysis indicates that the association between maternal education and homebirth preference was not statistically significant (OR = 0.72, CI 0.43, 1.19) (Fig 7).
Fig 7. Forest plot of the pooled estimate of the association between education and homebirth preference in Ethiopia, 2022.
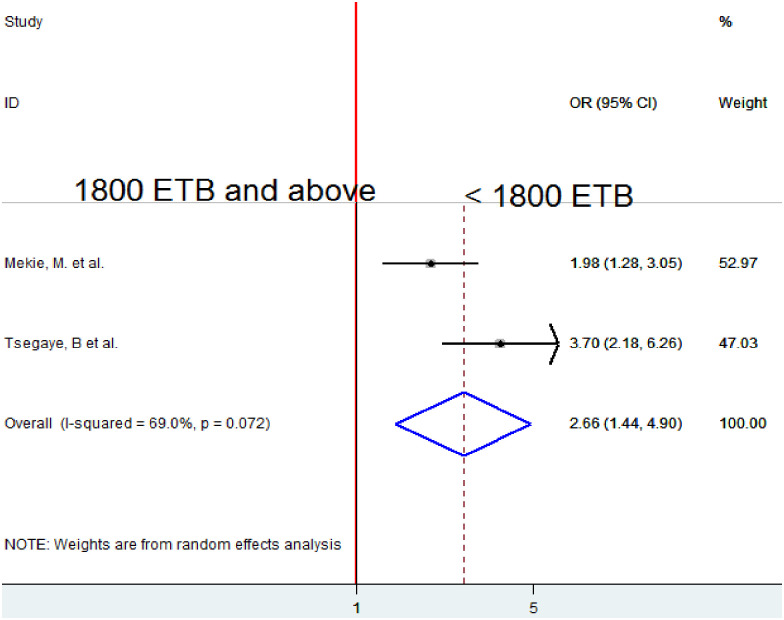
Association between monthly income and homebirth preference
To examine the association between average monthly income and homebirth preference, two studies were included in the analysis [18, 19]. The pooled association between average monthly income and homebirth preference was estimated by using A random-effects model due to moderate heterogeneity (I2 = 69.0%). The pooled result of the analysis indicated that average monthly income < 1800 ETB was significantly associated with homebirth preference. Mothers who got <1800 ETB prefer homebirth 2.66 times more likely as compared to those who get 1800 ETB and above (OR = 2.66, 95% CI 1.44, 4.90) (Fig 8).
Fig 8. Forest plot of the pooled estimate of the association between monthly income and homebirth preference in Ethiopia, 2022.
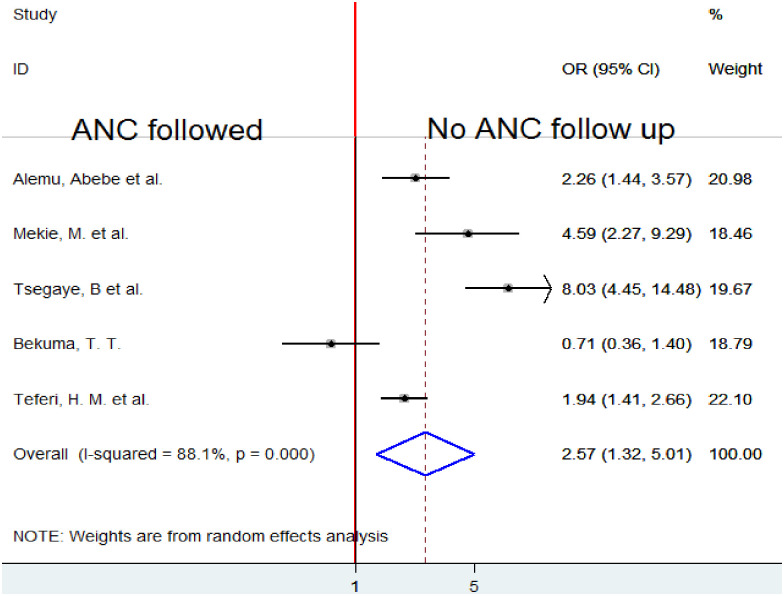
Association between ANC follow up and homebirth preference
Five studies [5, 10, 18–20] were analyzed to look at the association between ANC follow-up and desire for homebirth. Due to substantial heterogeneity (I2 = 88.1%, p-value 0.001), a random-effects model was employed to quantify the pooled association between ANC follow-up and preference for home birth. The analysis’s combined findings show that choosing to give delivery at home was associated with not receiving ANC follow-up. Women who did not have ANC follow-up during pregnancy were 2.57 times more likely to desire homebirth than those who did (OR = 2.57, 95%CI 1.32, 5.01) (Fig 9).
Fig 9. Forest plot of the pooled estimate of the association between ANC follow-up and homebirth preference in Ethiopia, 2022.
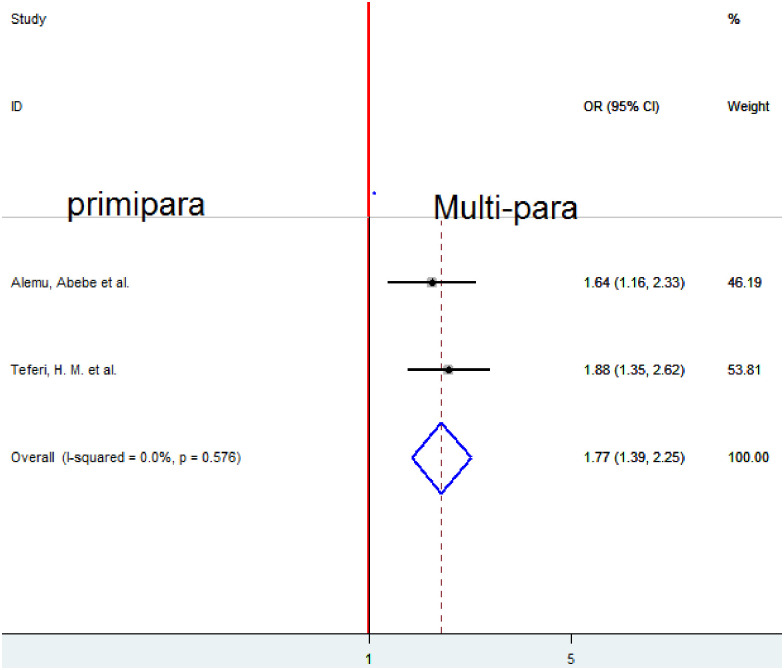
Association between parity and homebirth preference
To examine the association between parity and homebirth preference, two studies were included in the analysis [5, 10]. A fixed-effect model was employed to estimate the pooled association between parity and homebirth preference because of no heterogeneity (I2 = 0%, p-value < 0.576). The pooled result of the analysis indicates that parity was significantly associated with homebirth preference. Women of multipara prefer homebirth 1.77 times more likely as compared to those primiparas (OR = 1.77, 95%CI 1.39, 2.25) (Fig 10).
Fig 10. Forest plot of the pooled estimate of the association between parity and homebirth preference in Ethiopia, 2022.
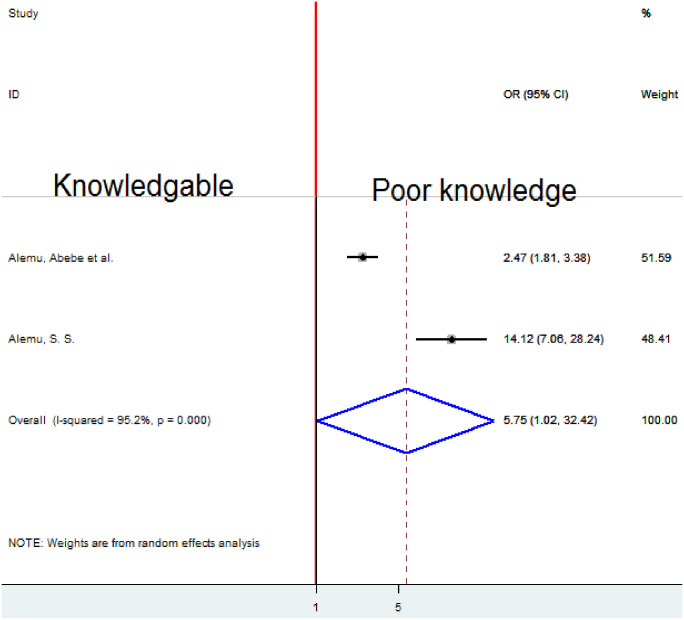
Association between knowledge of obstetric danger signs and homebirth preference
Two studies [10, 21] were analyzed to determine whether knowledge of obstetric danger signs and choice of homebirth were related. Due to substantial heterogeneity (I2 = 95.2%, p-value 0.001), to quantify the pooled association between knowledge of obstetric danger signs and preference for homebirth a random-effects model was employed. Poor knowledge was significantly associated with a desire for home birth, according to the analysis’s pooled result. When compared to women who were aware of obstetric hazard indications, those with poor knowledge were 5.75 times more likely to prefer homebirth (OR = 5.75, 95%CI 1.o2, 32.42) (Fig 11).
Fig 11. Forest plot of the pooled estimate of association knowledge about danger signs and homebirth preference in Ethiopia, 2022.
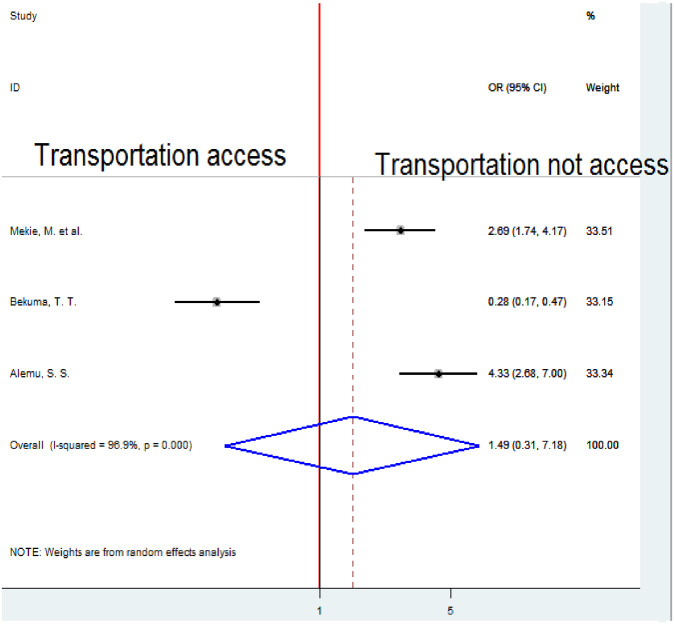
Association between transportation service accessibility and homebirth preference
To examine the association between transportation service access and homebirth preference, three studies were included in the analysis [18, 20, 21]. To estimate the pooled association between transportation service access and homebirth preference A random-effects model was employed because of significant heterogeneity (I2 = 96.9%, p-value < 0.001). The pooled result of the analysis indicated an insignificant association between transportation service access and homebirth preference (Fig 12).
Fig 12. Forest plot of the pooled estimate of the association between transportation access and homebirth preference in Ethiopia, 2022.
Association between delivery place discussion and homebirth preference
To examine the association between delivery place discussion and homebirth preference, two studies were included in the analysis [5, 21]. The pooled association between delivery place discussion and homebirth preference was examined by random-effects model, for high heterogeneity (I2 = 95.6%, p-value < 0.001). The pooled result of the analysis indicates that not having a delivery place discussion with a partner was significantly associated with homebirth preference. Women who did not discuss with their partners a place of delivery prefer homebirth 5.89 times more likely as compared to those who discussed with their partners (OR = 5.89 (95%CI 1.1, 31.63) (Fig 13).
Fig 13. Forest plot of the pooled estimate of the association between delivery place discussion and homebirth preference in Ethiopia, 2022.
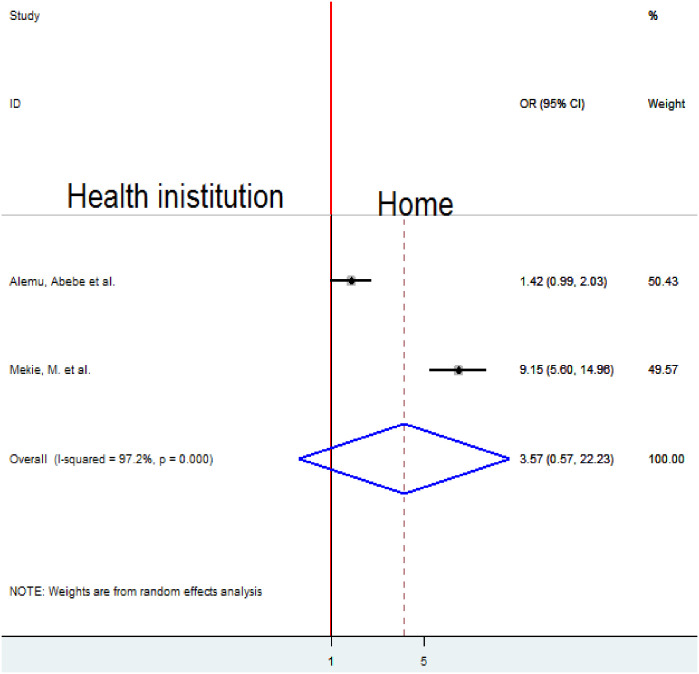
Association between the place of last delivery and homebirth preference
To examine the association between the place of last delivery and homebirth preference, two studies were included in the analysis [10, 18]. The pooled result of the association between the place of last delivery and homebirth preference was assessed by a random-effects model for the reason of high heterogeneity (I2 = 97.2%, p-value < 0.001). The pooled result of the analysis indicated an insignificant association between the place of last delivery and homebirth preference (Fig 14).
Fig 14. Forest plot of the pooled estimate of the association between place of last delivery and homebirth preference in Ethiopia, 2022.
Discussion
This systematic review and meta-analysis assessed homebirth preference and associated factors in Ethiopia, 2022. The prevalence of homebirth preference among pregnant women in Ethiopia was 39.62% (95% CI 27.98, 51.26). Even though WHO and EFMOH inspire every woman to give birth at a health institution, this systematic review and meta-analysis revealed that the prevalence of homebirth preference is high. This result is in line with a study done in Nigeria 39.3% [22]. But the finding of this systematic review and meta-analysis is higher than the finding of the study conducted in Tanzania (25.5%) [23]. A possible explanation for this inconsistent finding might be due to the local versus national study populations involved in these studies. The discrepancy could be due to the difference in the study subjects. The previous study was undertaken among all reproductive women whereas most of the participants of this systematic review and meta-analysis were pregnant mothers. Pregnant women’s favorite for homebirth declines as gestational age upturns because most pregnant women start ANC follow-up after the second trimester. Therefore, they get counseling about the advantages of institutional delivery.
This systematic review and meta-analysis revealed that low average monthly income (< 1800 ETB) was significantly associated with homebirth preference. Women with low average monthly income were about 3 fold times more likely to prefer homebirth than their counterparts. This finding is consistent with the study done in Tanzania [24]. Health care in Ethiopia for pregnant women is free. The reason might be healthcare facilities seldom run out of stock, demanding pregnant mothers charge some expenses for supplies or services. Besides, women from a distance pay a transportation fee to go to a health facility for maternity care. Therefore, pregnant women with better incomes are better to pay for transport and other health care payments.
Poor knowledge about obstetrical danger signs was significantly associated with home birth preference. Homebirth preference among women who had poor knowledge about danger signs was about 6 fold times higher compared to knowledgeable women. This is supported by the findings of studies undertaken in Ghana [25]. The possible explanation might be that maternal education and counseling which are given during ANC follow-up can change and boost the knowledge of pregnant mothers. As a result, this systematic review and meta-analysis indicated failure to attend ANC was significantly associated with homebirth preference. This result reveals that someone who has ANC follow-up can have advice and counseling regarding obstetric danger signs. This can enhance women’s intention to give birth at the health institution. As the knowledge of women about obstetric danger signs is boosted, understanding the benefits of health institution delivery becomes more efficient than homebirth.
In this systematic review and meta-analysis, multipara mothers were about 2 fold times more likely to prefer homebirth compared to nulliparous women in Ethiopia. This finding is in line with a study conducted in Ghana [26]. This might be due to their previous childbirth understanding.
Mothers not attended ANC visits in the current pregnancy were about 3 fold times more likely to prefer home delivery than those who attended ANC in Ethiopia. This finding is consistent with studies conducted in Nigeria [22]. It might be women who had ANC visits by health professionals had better opportunities to be counseled regarding birth preparedness, complication readiness, and place of delivery which may enhance delivery at a health institution than preferring to give birth at their own home.
This systematic review and meta-analysis found that women who did not discuss the place of their delivery with their partners were about six times more likely to desire a homebirth than those who did. Studies conducted in Tanzania and Mozambique in the past have produced consistent results [27]. If a woman who is pregnant is financially reliant on her spouse and the partner is unaware of the benefits of institutional birth, he may be able to choose the location of the delivery on his own because he is the source of the money. When couples debate where to give birth, there is a chance that the advantages and disadvantages of homebirth will come up. Partners disclose that the burden might come to them due to homebirth. They may decide to give birth at a health institution. Thus, why, not discussing with a partner may result in home birth.
Strength and limitation
This systematic review and meta-analysis has strengths; various databases were used to search for literature, both published and unpublished studies were searched and relevant studies were included after intensive quality assessment. Because less than 10 studies were included in the final analysis, it is difficult to get the exact estimation of publication bias from the funnel plot.
Conclusion
This systematic review and meta-analysis examined the substantial prevalence of homebirth preference in Ethiopia which may contribute maternal and child health crisis. The homebirth preference was associated with a low average monthly income (<1800 ETB), lack of ANC follow-up, multipara, poor knowledge about obstetric danger signs, and not discussing with their partner a place of delivery. Furthermore, a discrepancy was also found in different regions of the country. So, community-based awareness creation is mandatory to improve ANC follow-up and enhance knowledge about obstetric danger signs. The health policy of the country should include a mechanism that encourages couples to discuss together the exact choice of the right place of delivery to minimize perinatal and postpartum complications. Community health workers in the country should routinely deliver the basic knowledge of obstetric danger signs to pregnant mothers at a community level.
Supporting information
(DOCX)
(ZIP)
Acknowledgments
We would like to thank all authors of the studies included in this systematic review and meta-analysis.
Abbreviations
- ANC
Antenatal care
- CI
Confidence interval
- EFMOH
Ethiopian Federal Ministry of Health
- OR
Odd ratio
- SNNPR
Southern Nation nationality and people region
- WHO
World Health Organization
Data Availability
All relevant data are within the paper and its Supporting information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Shiferaw S., et al., Why do women prefer home births in Ethiopia? BMC Pregnancy and Childbirth, 2013. 13(1): p. 5. doi: 10.1186/1471-2393-13-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cofie L.E., et al., Birth location preferences of mothers and fathers in rural Ghana: Implications for pregnancy, labor, and birth outcomes. BMC Pregnancy and Childbirth, 2015. 15(1): p. 165. doi: 10.1186/s12884-015-0604-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fantaye A.W., Gunawardena N., and Yaya S., Preferences for formal and traditional sources of childbirth and postnatal care among women in rural Africa: a systematic review. PloS One, 2019. 14(9): p. e0222110. doi: 10.1371/journal.pone.0222110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aychiluhm S.B., et al., Geographical clustering and geographically weighted regression analysis of home delivery and its determinants in developing regions of Ethiopia: a spatial analysis. Emerging Themes in Epidemiology, 2022. 19(1): p. 8. doi: 10.1186/s12982-022-00117-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teferi H.M., San Sebastian M., and Baroudi M., Factors associated with home delivery preference among pregnant women in Ethiopia: a cross-sectional study. Glob Health Action, 2022. 15(1): p. 2080934. doi: 10.1080/16549716.2022.2080934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ethiopian Public Health Institute—EPHI, Federal Ministry of Health—FMoH, and ICF, Ethiopia Mini Demographic and Health Survey 2019. 2021, EPHI/FMoH/ICF: Addis Ababa, Ethiopia.
- 7.Nigusie A., et al., Community perception of barriers and facilitators to institutional delivery care-seeking behavior in Northwest Ethiopia: a qualitative study. Reproductive Health, 2022. 19(1): p. 193. doi: 10.1186/s12978-022-01497-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mutharayappa K. and Prabhuswamy P., Factors and Consequences of Home Deliveries: A Study in Rural Karnataka. Journal of Health Management, 2003. 5(1): p. 17–35. [Google Scholar]
- 9.Kolin D.A., et al., Risk factors for blood transfusion in traumatic and postpartum hemorrhage patients: Analysis of the CRASH-2 and WOMAN trials. PLOS ONE, 2020. 15(6): p. e0233274. doi: 10.1371/journal.pone.0233274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alemu A., Amenu G., and Feyiso M., Women’s preference of home delivery in Wonago District, Gedeo Zone, Southern Ethiopia 2018. J Gynecol Obstet, 2019. 7(3): p. 85. [Google Scholar]
- 11.Moher D., et al., Guidelines and Guidance-Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine, 2009. 6(7): p. 698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D., et al., Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Medicine, 2009. 6(7): p. e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Institute J.B., Meta-analysis of statistics: Assessment and review instrument (JBI MASTARI). Adelaide: Joanna Briggs Institute, 2006. 20032007. [Google Scholar]
- 14.Luchini C., et al., Assessing the quality of studies in meta-analyses: Advantages and limitations of the Newcastle Ottawa Scale. World J Meta-Anal, 2017. 5(4): p. 80–84. [Google Scholar]
- 15.Higgins J.P., and Thompson S.G., Quantifying heterogeneity in a meta-analysis. Stat Med, 2002. 21(11): p. 1539–58. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 16.Begg C.B. and Mazumdar M., Operating characteristics of a rank correlation test for publication bias. Biometrics, 1994. 50(4): p. 1088–101. [PubMed] [Google Scholar]
- 17.Kahsay Z.H., et al., Pregnant Women’s Intentions to Deliver at a Health Facility in the Pastoralist Communities of Afar, Ethiopia: An Application of the Health Belief Model. Int J Environ Res Public Health, 2019. 16(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mekie M. and Taklual W., Delivery place preference and its associated factors among women who deliver in the last 12 months in Simada district of Amhara Region, Northwest Ethiopia: a community-based cross-sectional study. BMC Res Notes, 2019. 12(1): p. 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsegaye B., et al., Level and factors associated with a preference of institutional delivery among pregnant woman in Debre-tabor town, North West Ethiopia, 2017: a community-based cross-sectional study. BMC Res Notes, 2019. 12(1): p. 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bekuma T.T., et al., Factors Affecting Choice of Childbirth Place among Childbearing Age Women in Western Ethiopia: A Community-Based Cross-Sectional Study. Int J Reprod Med, 2020. 2020: p. 4371513. doi: 10.1155/2020/4371513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alemu S.S., et al., Preference of homebirth and associated factors among pregnant women in Arba Minch health and demographic surveillance site, Southern Ethiopia. PLoS One, 2022. 17(10): p. e0276682. doi: 10.1371/journal.pone.0276682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Envuladu E., et al., Factors determining the choice of a place of delivery among pregnant women in Russia village of Jos North, Nigeria: achieving the MDGs 4 and 5. International Journal of Medicine and Biomedical Research, 2013. 2(1): p. 23–27. [Google Scholar]
- 23.Exavery A, K., Njozi M, Tani K, Doctor HV, Hingora A, Phillips Access to institutional delivery care and reasons for home delivery in three districts of Tanzania. International journal for equity in health, 2014. 13(1): p. 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ngowi A.F., et al., Women’s determinant factors for a preferred place of delivery in Dodoma region Tanzania: a cross-sectional study. Reproductive Health, 2017. 14(1): p. 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nakua E.K., et al., Home birth without skilled attendants despite millennium villages project intervention in Ghana: insight from a survey of women’s perceptions of skilled obstetric care. BMC Pregnancy and Childbirth 2015. 15: p. 243. doi: 10.1186/s12884-015-0674-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boah M., et al., “I couldn’t buy the items so I didn’t go to deliver at the health facility” Home delivery among rural women in northern Ghana: A mixed-method analysis. PLOS ONE, 2020. 15(3): p. e0230341. doi: 10.1371/journal.pone.0230341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mpembeni RNM, K. J., Leshabari MT, et al., Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth, 2007. 7(1–7). [DOI] [PMC free article] [PubMed] [Google Scholar]