Abstract
Background:
HIV self-testing (HIVST) can increase the reach of HIV testing. PrEP clients may be ideal distributors of HIVST kits and PrEP information within their social networks. This study uses the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework to evaluate the distribution of HIVST bundled with PrEP information (“Test-to-PrEP” kits) among egocentric friendship networks of PrEP users.
Methods:
The study was conducted in Miami from November 2021 to March 2022. Enrolled PrEP clients (egos; n=100) were offered Test-to-PrEP kits for distribution. Egos and Test-to-PrEP kit users completed brief online surveys. Descriptive statistics are reported for participants, their reported network members, and users of the Test-to-PrEP kits. Logistic and Poisson regression assessed the relationship between characteristics of egos, alters, and the distribution of Test-to-PrEP kits.
Results:
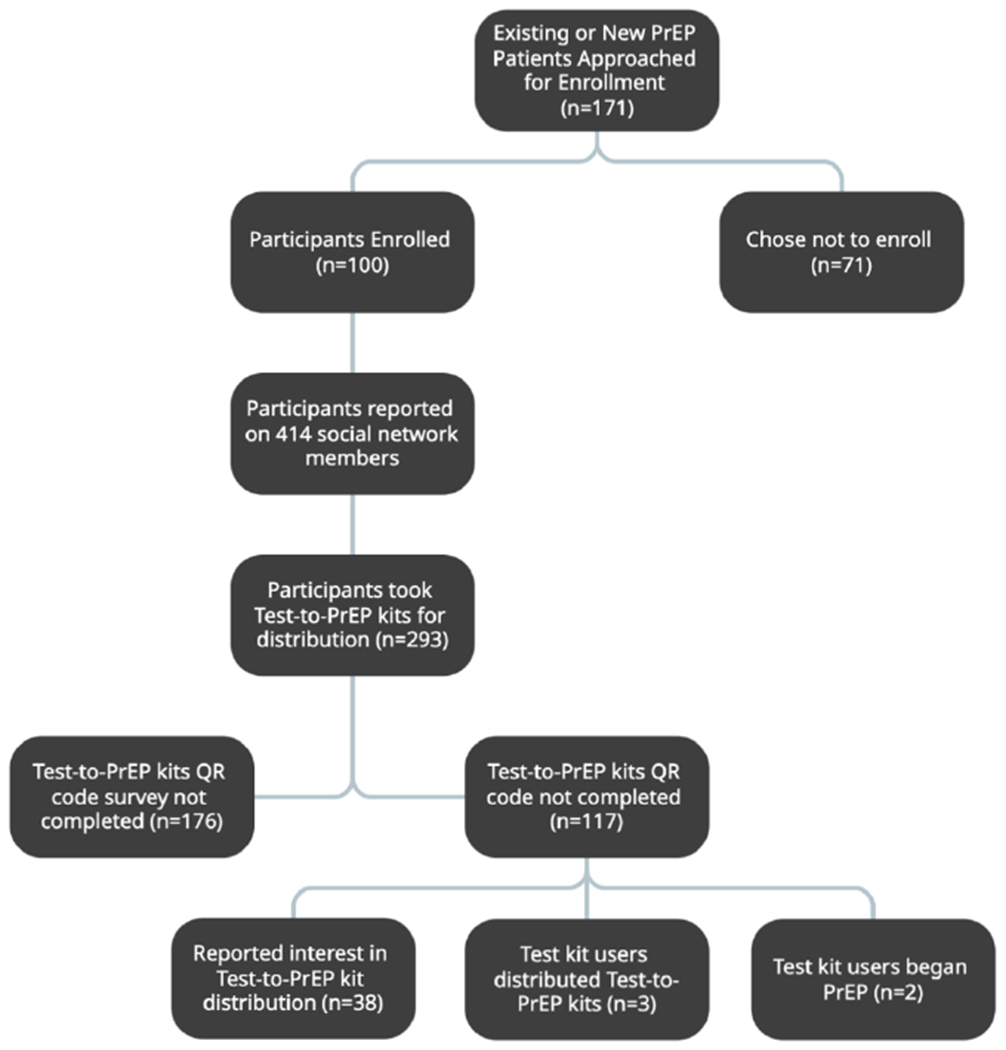
The 100 enrolled egos reported a total of 414 alters. Participants received 293 Test-to-PrEP kits for distribution with 47 of the 100 participants distributing at least one kit. Of those who scanned the QR code and responded to the survey, 16.2% reported no previous HIV test and 38.5% reported no prior knowledge of PrEP; 32.5% reported interest in distributing Test-to-PrEP kits, three successfully distributed kits, and two initiated PrEP.
Conclusions:
An approach using PrEP clients’ social networks can disseminate HIVST bundled with PrEP information to critical populations including individuals lacking knowledge of PrEP or who have never been tested for HIV. Future studies will assess whether this use of network effects can increase reach and efficiency of HIV testing and PrEP information distribution.
Keywords: HIV testing, HIV self-test kit, implementation science, social network, PrEP, men who have sex with men, HIV prevention
Introduction
The United States (US) Department of Health and Human Services’ Ending the HIV Epidemic (EHE) Initiative aims to reduce new HIV infections in the US by 90% by 2030[1]. To achieve this, innovations in and the scaling up of targeted HIV testing and prevention strategies are critical[2]. This work is particularly urgent for sexual, racial, and ethnic minority communities disproportionately impacted by HIV[3]. The Miami metropolitan area, a majority-minority community with about 70% of the population identifying as Hispanic/Latino, has among the highest rates of new HIV diagnoses in the US[4, 5]. Strategies to improve the reach of available interventions to priority populations are needed; using social networks of current pre-exposure prophylaxis (PrEP) clients to disseminate HIV self-test kits (HIVST) and PrEP information is one such approach.
HIV self-testing has been shown to address multiple barriers to testing including access, stigma and privacy concerns related to testing sites [6]. Research focused on internet-based self-test distribution demonstrated the ability of HIVST to reach populations who never tested for HIV or are testing below the CDC recommended frequency[6, 7]. Studies have leveraged social networks to encourage participants to refer their sexual partners and friends for HIV testing in clinical and community-based organization settings, demonstrating the feasibility of working with people living with HIV or prioritized for HIV prevention to recruit social, sexual, and drug-use network members for HIV counseling, testing, and referral[8, 9]. The Social Networks Demonstration Project worked with nine community-based organizations in seven different US cities to use “a social network strategy to access and provide HIV testing to a population of persons with a high prevalence of undiagnosed HIV infection” [8]. This peer-driven approach was shown to be highly effective and points to the power of social-networks for increasing HIV testing.
In 2012, the Food and Drug Administration (FDA) approved PrEP for prevention of HIV acquisition[10]. Despite the more widespread availability of this important option for highly effective prevention, the U.S Centers for Disease Control and Prevention (CDC) estimated that in 2019 only 18% of people at risk for HIV were prescribed PrEP[11]. Interventions to increase knowledge of and access to PrEP for all regardless of sexual and gender identity are needed[12–14]. Utilizing the social networks of current PrEP clients for distribution of PrEP information has the potential to expand to reach to new PrEP candidates. Our previous pilot work distributed 148 OraQuick HIVST kits to social network members through 50 PrEP clients, establishing the feasibility of this approach[15]. Feedback from clients participating in this pilot study indicated that 74% found the kits to be “very easy to use”, with 87.5% being “completely comfortable offering the HIVST kits” to their social network members[15]. These tailored approaches are rooted in the Social Contagion Theory, which postulates that ideas, beliefs, and behaviors will spread through network connections[16]. Guided by Social Contagion Theory we capitalize on the social network intervention theory of induction, leveraging existing ties or relationships in a social network to spread information and behaviors[17]. We now expand upon this preliminary work to evaluate the distribution of HIVST bundled with PrEP information (“Test-to-PrEP” kits) among social networks of current PrEP users using the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework.
Developed by Glasgow et al., (1999), the RE-AIM framework was first conceived to evaluate and improve the external validity and sustainability of public health interventions[18]. To evaluate the feasibility and acceptance of Test-to-PrEP kits, we utilized the RE-AIM framework that works to describe the reach, effectiveness, adaptation, implementation, and maintenance of the intervention. In this study, we focus on two dimensions: reach and adoption. We examine the characteristics of those individuals who distributed Test-to-PrEP kits as well as those who received and scanned the HIVST.
Methods
Setting
The PrEP program at the University of Miami operates brick-and-mortar and mobile clinics that provide PrEP, non-occupational post-exposure prophylaxis (nPEP), and sexually transmitted infection (STI) testing and treatment as well as HIV rapid entry into care, at no cost, in six high priority areas throughout Miami-Dade County. Services are offered daily at the brick-and-mortar clinic, and weekly at each site on a rotating basis through the mobile clinic. This study recruited and enrolled new and existing PrEP program clients seen at these clinics from November 2021 to March 2022.
Human Subjects Research Review
Prior to onset of study activities, approval was obtained from the University of Miami Institutional Review Board. Written or electronic consent in English or Spanish was provided and obtained from all participants.
The Test-to-PrEP Kit Intervention
The Test-to-PrEP kit intervention aimed to increase access to HIV testing and awareness of HIV and PrEP. Kit development was informed by a community advisory board and previous research[15]. Test-to-PrEP kits included an Ora-Quick In-Home (OraSure Technologies, Inc, Bethlehem, PA) oral fluid HIV self-test packaged with manufacturer-issued usage instructions, and locally designed and created educational materials related to PrEP and HIV testing. This bilingual (English/Spanish) resource outlined steps to take if an HIV self-test result was positive, PrEP and PEP information, and locally tailored information regarding how to access these services. Additionally, a unique quick-response (QR) code was created for and affixed to the front of each HIV self-test. These codes, and the self-test user surveys that opened when the QR was scanned, were electronically paired to the study identification (ID) number of the PrEP client participant that accepted the Test-to-PrEP kit.
Overview of Assessments
This study included current PrEP clients (egos), members of their social networks who egos believed were appropriate users of the kit (alters), and those who received the Test-to-PrEP kits and completed the associated survey (kit users). At the end of initial or quarterly PrEP follow-up visits, clients (n=171) were approached and assessed for study eligibility and interest. Demographic characteristics such as gender, age, race, country of birth, and ethnicity were captured for all individuals approached. Eligible clients were 18 years or older and had received a PrEP prescription from the program. Participants (n=100) completed informed consent procedures, were briefed on study goals, and offered up to four Test-to-PrEP kits to distribute among their social networks. Participants were counseled by trained study staff on use of the HIVST and other included materials using a templated discussion instrument. Participants (egos) were asked to create a distribution plan for the kits. Study staff instructed participants to ask kit users to scan the QR code and complete the survey once they had performed the HIVST. Egos received a $30 gift card after completing each survey for their time and participation. Those who received an HIVST kit from a participant and completed the survey received a $15 electronic gift card for their time and participation. Participants (egos) then received an additional $10 for every completed kit user survey that was associated with their study ID number. A flowchart describing the study steps can be seen in figure 1. Following orientation to the Test-to-PrEP kit, participants completed a short two-part (approximately 15 minutes each) survey to capture information about themselves (egos) and their alters. This survey was developed and administered through Network Canvas, a free, open source, set of tools specifically designed to collect social network data[19]. Kit users were asked to complete a brief (approximately 10 minute) survey. The kit user survey (accessed via QR code) was administered through Qualtrics web-based survey software [Qualtrics, Provo, UT]. For those approached to participate but declined, de-identified demographic information was collected including race, ethnicity, country of birth, gender, and age[20]. All assessments were provided in English and Spanish.
Figure 1.
RE-AIM Framework:
The RE-AIM framework was used to evaluate the Reach and Adoption of Test-to-PrEP kit distribution at the individual level through egocentric social networks. Reach was assessed at the Test-to-PrEP kit user level as the number of kits with successfully scanned codes and the characteristics of those individuals who scanned the QR code and completed the linked survey. Adoption was assessed as the number of individuals who participated in the study relative to those who were approached, and at the ego level as the number of Test-to-PrEP kits taken by the current PrEP clients (egos). Additionally, we recorded the reported perception of their network members (alters) likelihood to talk about Test-to-PrEP kits, likelihood to encourage use of HIV self-test, and likelihood to distribute Test-to-PrEP kits.
Participant/Ego-level Characteristics:
In part one of the baseline survey, participants (egos) provided their age, race, ethnicity, gender, sex assigned at birth, country of birth, the perceived gender of their sex partner(s), whether they were a new or existing PrEP user at the time of enrollment, and the number of Test-to-PrEP kits they accepted. A 3-month follow-up survey was also conducted with participants by telephone to assess their experience with Test-to-PrEP kit distribution.
Dyadic-level Characteristics (Ego-Alter):
In part two of the baseline survey, participants (egos) reported demographic information for up to 12 alters including their perceived age, gender, race, and ethnicity. Additionally, participants (egos) were asked to describe their relationship with the identified alter. Characteristics of ego-alter communications and interactions, perceived barriers, and facilitators to Test-to-PrEP kit distribution, and the strength of the connection between the ego and alter (e.g., trust, frequency of interaction) were also captured.
Kit User Characteristics:
The Test-to-PrEP kit user survey included demographic questions to capture the user’s age, race, gender, and ethnicity. This survey included questions about number of sex partners kit users had in the past year and the type of relationship they shared with the Test-to-PrEP kit distributor (friend, family member, sexual partner, or other). Additionally, kit users were asked to rate the following single items on a scale from 0-100: PrEP knowledge prior to and following receipt of the Test-to-PrEP kit, ease of use of HIVST, comfort with HIVST format, quality of HIVST information, quality of information about HIV, quality of information about PrEP, and likelihood of PrEP use prior to and after receipt of the Test-to-PrEP kit. Kit users were asked to indicate any interest in becoming a distributor of Test-to-PrEP kits themselves. Those with interest in distributing kits could provide their contact information for study staff to reach out. The result of the HIVST and date of last HIV test (prior to performing the self-test) were also requested.
Data Analysis
Statistical Analysis was performed using R (R Core Team, 2022)[21]. Demographic and other characteristics were summarized using frequencies and proportions for categorical variables and means and ranges for continuous variables. Descriptive statistics of egos’ characteristics, alters’ characteristics (as reported by egos), and the characteristics of Test-to-PrEP kit users who scanned the QR code and completed the linked survey are displayed in Tables 1, 2, and 3, respectively. While we asked egos to report on alters to whom they planned on distributing Test-to-PrEP kits, we did not have confirmation that the alters (described in Table 2) were identical to those who received the Test-to-PrEP kits (described in Table 3). For the following analysis, we assume the alters described by the egos serve as proxies for all Test-to-PrEP kit users, as Test-to-PrEP kit users’ demographics closely mirrored those of the alters.
Table 1:
Ego Level Demographic Characteristics
| Demographic Characteristics | Overall (N = 100) |
|---|---|
| Age | |
| Mean (SD) | 37.4 (9.86) |
| Median [Min, Max] | 36.0 [19.0, 62.0] |
| Ethnicity | |
| Non-Hispanic | 19 (18.6%) |
| Hispanic/Latino | 83 (81.4%) |
| Race | |
| White | 62 (60.8%) |
| Black or African American | 10 (9.8%) |
| Asian | 1 (1.0%) |
| Multi-Racial | 6 (5.9%) |
| Other | 23 (22.5%) |
| Gender Identity | |
| Female | 6 (5.9%) |
| Male | 96 (94.1%) |
| Sex assigned at birth | |
| Female | 6 (5.9%) |
| Male | 96 (94.1%) |
| Born in the United States | |
| No | 82 (80.4%) |
| Yes | 20 (19.6%) |
| Partner Gender Identity | |
| Cisgender Male | 90 (88.2%) |
| Cisgender Female | 10 (9.8%) |
| Trans Woman | 1 (1.0%) |
| Trans Man | 1 (1.0%) |
| Recruitment Type: | |
| PrEP Initial | 26 (25.5%) |
| PrEP Follow-Up | 74 (72.5%) |
| Number of kits accepted (total = 293) | |
| Mean (SD) | 2.96 (1.15) |
| Median [Min, Max] | 3.00 [1.00, 4.00] |
Table 2:
Alter Level Demographic Characteristics
| Demographic Characteristics | Overall (N=414) |
|---|---|
| Perceived Ethnicity | |
| Hispanic/Latino | 313 (75.6%) |
| Non-Hispanic | 97 (23.4%) |
| Missing | 4 (1.0%) |
| Perceived Gender Identity | |
| Cisgender Male | 268 (64.7%) |
| Cisgender Female | 143 (34.5%) |
| Trans Woman | 1 (0.2%) |
| Tran Man | 2 (0.5%) |
| Perceived Age Range | |
| 18 - 29 | 119 (28.7%) |
| 30 - 39 | 197 (47.6%) |
| 40 - 49 | 66 (15.9%) |
| 50 + | 28 (6.8%) |
| Missing | 4 (1.0%) |
| Alter Relationship Type | |
| Friend | 260 (62.8%) |
| Sexual Partner | 65 (15.7%) |
| Co-worker | 33 (7.9%) |
| Neighbor | 15 (3.6%) |
| Family Member | 31 (7.6%) |
| Other | 10 (2.4%) |
Table 3:
Test Kit Recipient Demographics
| Demographic Characteristics | Overall (N=117) |
|---|---|
| Number of Sex Partners in the Past Year | |
| Mean (SD) | 5.85 (11.4) |
| Median [Min, Max] | 3.00 [0, 100] |
| Missing | 18 (15.4%) |
| Who gave you the HIV self-test kit? | |
| Friend | 84 (71.8%) |
| Sexual Partner | 3 (2.6%) |
| Family Member | 16 (13.7%) |
| Casual Acquaintance | 0 (0%) |
| I don’t know | 0 (0%) |
| Directly from the clinic | 6 (5.1%) |
| Missing | 8 (6.8%) |
| Did you use the HIV self-test? | |
| Yes, Used it myself | 95 (81.2%) |
| Yes, Helped someone else use the test kit | 6 (5.1%) |
| No, I plan to use it some other time | 8 (6.8%) |
| No, and I do not plan to use it | 0 (0%) |
| Missing | 8 (6.8%) |
| What was the result of the HIV self-test that you did? | |
| Reactive/ Positive | 2 (1.7%) |
| Non-reactive/ Negative | 96 (82.1%) |
| Indeterminate | 1 (0.9%) |
| Prefer not to say | 2 (1.7%) |
| Missing | 16 (13.7%) |
| Do you have a plan in place for a confirmatory test? | |
| Yes, contacted and have an appointment | 2 (1.7%) |
| Yes, I have a plan but no appointment | 3 (2.6%) |
| No, Please help me arrange a test | 0 (0%) |
| Missing | 112 (95.7%) |
| When was the last time that you had an HIV test (not counting this self-test kit)? | |
| Last 6 months | 51 (43.6%) |
| 6 -12 months ago | 21 (17.9%) |
| More than a year ago | 18 (15.4%) |
| Never | 19 (16.2%) |
| Prefer not to say | 0 (0%) |
| Missing | 8 (6.8%) |
| Before today, had you ever heard about Pre-Exposure Prophylaxis (PrEP) for HIV prevention? | |
| Yes | 60 (51.3%) |
| No | 45 (38.5%) |
| Prefer not to answer | 2 (1.7%) |
| Missing | 10 (8.5%) |
| Choose one or more races that you consider yourself to be | |
| White | 73 (62.4%) |
| Black or African American | 13 (11.1%) |
| American Indian or Alaskan Native | 0 (0%) |
| Asian | 3 (2.6%) |
| Native Hawaiian or Pacific Islander | 0 (0%) |
| Other | 15 (12.8%) |
| Missing | 13 (11.1%) |
| Sex Assigned at Birth | |
| Male | 68 (58.1%) |
| Female | 39 (33.3%) |
| Intersex | 0 (0%) |
| Prefer not to say | 0 (0%) |
| Missing | 10 (8.5%) |
| Gender | |
| Male | 66 (56.4%) |
| Female | 39 (33.3%) |
| Non-binary/third gender/ two spirit/ gender fluid | 0 (0%) |
| Prefer not to say | 2 (1.7%) |
| Missing | 10 (8.5%) |
| Identifies as Hispanic or Latino | |
| Non-Hispanic or Latino | 31 (26.5%) |
| Hispanic/Latino | 86 (73.5%) |
| Ease of Use of the self-test kit (scale 0-100) | |
| Mean (SD) | 96.7 (10.0) |
| Median [Min, Max] | 100 [50.0, 100] |
| Missing | 16 (13.7%) |
| Comfort with the self-test kit (scale 0-100) | |
| Mean (SD) | 96.5 (10.6) |
| Median [Min, Max] | 100 [45.0, 100] |
| Missing | 16 (13.7%) |
| Quality of information about how the self-test kit works (scale 0-100) | |
| Mean (SD) | 95.4 (15.9) |
| Median [Min, Max] | 100 [0, 100] |
| Missing | 16 (13.7%) |
| Quality of information about HIV (scale 0-100) | |
| Mean (SD) | 98.9 (4.71) |
| Median [Min, Max] | 100 [65.0, 100] |
| Missing | 17 (14.5%) |
| Quality of information about PrEP (scale 0-100) | |
| Mean (SD) | 96.2 (12.8) |
| Median [Min, Max] | 100 [0, 100] |
| Missing | 17 (14.5%) |
| Identities of Sexual Partners | |
| Male | 70 (59.8%) |
| Female | 22 (18.8%) |
| Non-binary/third gender/ two spirit/ gender fluid | 1 (0.9%) |
| Transgender male | 0 (0%) |
| Transgender female | 0 (0%) |
| Prefer not to say | 2 (1.7%) |
| Have not had sex in the past 12 months | 5 (4.3%) |
| Missing | 17 (14.5%) |
| History of PrEP | |
| No, Never taken PrEP | 80 (68.4%) |
| Yes, Took PrEP but stopped | 8 (6.8%) |
| Yes, Currently on PrEP | 20 (17.1%) |
| Missing | 9 (7.7%) |
| How likely are you to take PrEP for HIV prevention - before receiving the kit | |
| Mean (SD) | 58.8 (38.7) |
| Median [Min, Max] | 57.0 [0, 100] |
| Missing | 40 (34.2%) |
| How likely are you to take PrEP for HIV prevention - after receiving the kit | |
| Mean (SD) | 77.9 (28.4) |
| Median [Min, Max] | 96.0 [0, 100] |
| Missing | 39 (33.3%) |
Results from the logistic regression can be found in Supplemental Digital Content 2, which is the results of ego-level logistic regression. The outcome of interest in the logistic regression was success in Test-to-PrEP kit distribution. This was measured by asking each ego whether they had successfully distributed any of their Test-to-PrEP kits (binary; yes/no). The outcome of interest in the Poisson regression was the number of Test-to-PrEP kits distributed. This was measured by asking each ego how many of the Test-to-PrEP kits they were able to successfully distribute (count; 0-4). Poisson regression was chosen as opposed to negative binomial regression based on the models standardized residuals predominantly falling between −2 and 2. Given the exploratory nature of the regression analysis we will view a p-value of below 0.1 as trending towards significance with a value of 0.05 or below suggesting statistical significance.
Results
Reach
Test-to-PrEP Kit User Characteristics:
Of the 293 Test-to-PrEP kits accepted by egos 117 were successfully used by the recipient and the QR code-linked survey completed (kit users; 39.9%). Of the 117 kit users, 73.5% were Hispanic/Latino, 62.4% were White, 58.1% identified as male, and 59.5% identified their partners as male. Kit users described themselves as predominantly friends with egos (71.8%), reported a mean of 5.85 sexual partners in the last year, and 43.6% reported their last HIV test to have occurred within 6 months. Knowledge of PrEP prior to receipt of the kit was reported by 51.3% of kit users. Test-to-PrEP kit users reported a nearly 20-point increase in PrEP knowledge after receiving the Test-to-PrEP kit (before score: 58.8, after score: 77.9). The mean response scores for likelihood to take PrEP prior to receipt of the kit and after receipt of the kit were 58.8 and 77.9 (on scale of 0-100), respectively. Kit users also reported on the ease of use of the HIV self-test kit, their comfort with the HIV self-test, the quality of information about HIV, and the quality of information about PrEP. Each question had a scale of 0 – 100 and the responses were 96.7, 96.5, 95.4, and 98.9, respectively. Table 3 contains the complete characteristics of the HIV self-test users.
Adoption
Ego characteristics:
Of the 100 egos who participated in the egocentric network survey, 81.4% were Hispanic/Latino, 60.8% were White, 94.1% identified as male, and 80.4% were born outside of the United States. The mean age of egos was 37.4 years, and the majority reported the gender of their sexual partners to be cisgender male (88.2%). Egos were primarily follow-up PrEP clients (72.5%) and the mean number of kits accepted was approximately 3. Forty-seven egos successfully distributed the Test-to-PrEP kits. Table 1 shows the complete demographic information for the ego level.
Non–participant Characteristics:
Of the 171 individuals approached to participate in the distribution of HIVST kits, 71 individuals chose not to participate. The non-participants did not differ significantly from participants on age, race, gender, ethnicity, or country of birth. Non-participants were predominantly Hispanic/Latino (71.9%), White (83%), reported their gender as male (94.3%), were born outside of the United States (74.6%) and had a mean age of 38.4 years.
Alter Characteristics:
The egos reported a total of 414 friendship group members (alters) who they believed would be an appropriate Test-to-PrEP kit recipient. The alter characteristics represent the ego’s perception of their friendship network members (alters). Alters were described as predominantly Hispanic/Latino (75.6%), cisgender male (64.7%), between 30 and 39 years old (47.6%) and were identified as friends (62.8%). Table 2 describes alters’ reported characteristics.
Regression Model
Logistic Regression Model:
The log odds of successful distribution of Test-to-PrEP kits were −2.56 times as likely for those egos who were existing PrEP clients compared to those who were new to PrEP clients (Log Odds: −2.08; p-value = 0.09), similarly suggesting that those egos who were new to PrEP were better distributors of Test-to-PrEP kits. The log odds of successful distribution of Test-to-PrEP kits were 1.89 times greater for those egos who reported they were likely to encourage PrEP use to their alters (Log Odds: 1.89; p-value = 0.10), indicating that those who were likely to encourage PrEP use were more likely to successfully distribute Test-to-PrEP kits.
Poisson Regression Model:
The difference in the logs of expected counts is 0.301 units lower for those already on PrEP compared to those who were initiating PrEP use (Estimate: −0.31; p-value = <0.01). The number of Test-to- PrEP kits distributed was 0.03 units lower for each additional year spent in the United States (Estimate: - 0.03; p-value = <0.01). If a participant were to increase their number of social network members by one, the difference in the logs of expected Test-to- PrEP kits distributed would be expected to increase by 0.06 (Estimate: 0.06; p-value = <0.01).
Discussion
There is urgent need for the implementation of interventions that allow for the scale-up of HIV testing and PrEP engagement, particularly among populations underrepresented in testing and PrEP care. This study used the RE-AIM framework to evaluate the Reach and Adoption of Test-to-PrEP kits through egocentric social networks. While the acceptability and feasibility of HIV self-testing is widely documented[6, 22–24], our results demonstrate the opportunity to provide HIV testing and PrEP information to persons who might be hesitant or unable to seek clinic- or community-based testing. The program reached critical populations for HIV testing and PrEP information dissemination; 16.2% reported no previous HIV test, and 38.5% reported never having heard about PrEP for HIV prevention prior to receiving the Test-to-PrEP kit. This work expands upon past studies that found social networks to be successful modes for information distribution [25–27], by demonstrating that social networks facilitate Test-To-PrEP kit distribution and successfully reach and educate individuals who previously lacked PrEP knowledge. To our knowledge, ours is the first study to use a social network-based strategy for distribution of HIVST kits by current PrEP users. Prior work utilizing social network-based strategies to encourage testing and care linkage has been similarly successful in increasing testing among people of color with increased risk for HIV [28–31].
Like previous findings our results suggest a notable increase in PrEP knowledge after receiving the kit[32, 33]. Test-to-PrEP kit users also reported that the HIVST was easy to use, individuals were comfortable using the Test-to-PrEP kits, and the Test-to-PrEP kits contained high quality information about both HIV and PrEP. While our original metric of measurement for reach was the number of Test-to-PrEP kits used, an additional strength was the ability to assess and track reach beyond the test kit recipient. Of the 117 successfully distributed kits, 38 of the Test-to-PrEP kit users reported potential interest in distributing Test-to-PrEP kits themselves, three of those 38 were successfully recruited as distributors, and two of the kit users began using PrEP themselves. These findings suggest the reach of the project was greater than initially anticipated, that the distribution of Test-to-PrEP kits can reach beyond a single social network to expand HIV testing and PrEP knowledge. Additionally, an unanticipated but very positive outcome was a small but direct impact of Test-to-PrEP kits on PrEP uptake.
High adoption of the Test-to-PrEP kit strategy by PrEP clients approached in the clinic reinforces the utility and feasibility of leveraging social networks to increase access to HIV testing and enhance PrEP knowledge in populations experiencing heightened risk for HIV. These findings are consistent with prior work that found the use of social network-based testing to be an effective mode for promoting HIVST and peer-to-peer distribution[34–36].
After employing logistic regression and Poisson regression of egocentric sexual networks to further identify correlates of successful Test-to-PrEP kit distribution, we found that the number of friends reported in the friendship network, whether the ego was a new PrEP user, and the time spent in the United States were associated with successful Test-to-PrEP kit distribution. Our findings suggest that those who are themselves new to PrEP are better kit distributors. Prior work has largely focused on identifying peer leaders and the importance of peer influence on PrEP information dissemination [25, 37, 38]. Our findings indicate the importance of peer groups with whom individuals can share and engage in conversations on sensitive topics such as PrEP use and HIV testing. Our work suggests that clients recently initiated in PrEP care may be a powerful source of PrEP information and intervention proliferation. While further exploration is needed, one hypothesis is that individuals newly initiating PrEP and moving from the “preparation” to “action” stages of change may have peak information and motivation regarding PrEP and therefore be particularly effective agents of social network activation on this topic [39, 40].
The findings of this study are subject to limitations. Compared to traditional HIV testing programs, self-testing comes with challenges to understanding and documenting who used the test and, challenges related to the documentation of the test results and linkage to HIV care or services. However, the bundling of the PrEP information and HIVST kit offers multiple resources to help participants interpret the results and access care services. The customized QR codes allowed us to determine which egos successfully distributed the kits by collecting information from kit recipients who completed the survey linked to each ego. As sexual behavior information collected included only sexual partner identity and number of sexual partners, our ability to calculate PrEP eligibility was limited. Thus, while we noted significant Test-to-PrEP kit distribution to women, a group not frequently engaged in PrEP services, it is not known whether these women would be appropriate candidates for PrEP.
The impact, reach, and lessons learned from this project demonstrate the strengths of using social network approaches to disseminate an integrated PrEP information and HIVST kit, and the potential of employing PrEP users, particularly new PrEP users, as knowledgeable activators of their networks. The framework developed through this project can be leveraged in other EHE priority areas. Future work is needed to further explore our findings and to refine approaches for deploying Test-to-PrEP kits optimally to reach priority populations for HIV testing and PrEP engagement.
Conclusion:
This project demonstrated several important facets of the Test-to-PrEP kit including its reach, adoption, ease of use, and feasibility of distribution through social networks. Our findings suggest PrEP clients’ social networks can be leveraged to expand HIV testing and PrEP information to populations often understudied including individuals of a variety of genders and sexual identities who were lacking prior knowledge of PrEP. An unanticipated but very positive outcome was the direct impact of Test-to-PrEP kits on recipients’ PrEP uptake and the ability to reach populations who are often under-engaged (e.g., women). These promising Test-to-PrEP results require further evaluation to determine scalability, implementation, maintenance, and effectiveness in different settings.
Supplementary Material
Conflicts of Interest and Source of Funding:
The authors declare there are no potential conflicts of interest. This work was supported by Miami Center for AIDS Research Ending the HIV Epidemic administrative supplement (NIH/NIAIDS P30AI169643) awarded to M.K. and S.D.L.
References:
- 1.Prevention, C.f.D.C.a., Ending the HIV Epidemic in the U.S. (EHE). [Google Scholar]
- 2.HIV.gov. What Is Ending the HIV Epidemic: A Plan for America? 2020. [Google Scholar]
- 3.HIV Surveillance Report, 2019. 2021: Centers for Disease Control and Prevention. [Google Scholar]
- 4.HIV diagnoses- flhealthcharts.gov. Florida Department of Health. [Google Scholar]
- 5.Bureau, U.S.C., Population Estimates, July 1, 2022 (V2022) — Miami-Dade County, Florida. 2022. [Google Scholar]
- 6.Hecht J, et al. , Increasing Access to HIV Testing Through Direct-to-Consumer HIV Self-Test Distribution - United States, March 31, 2020-March 30, 2021. MMWR Morb Mortal Wkly Rep, 2021. 70(38): p. 1322–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menza TW, et al. , Rapid Uptake of Home-Based HIV Self-testing During Social Distancing for SARS-CoV2 Infection in Oregon. AIDS Behav, 2021. 25(1): p. 167–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kimbrough LW, et al. , Accessing Social Networks With High Rates of Undiagnosed HIV Infection: The Social Networks Demonstration Project. American journal of public health (1971), 2009. 99(6): p. 1093–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGoy SL, et al. , Use of Social Network Strategy Among Young Black Men Who Have Sex With Men for HIV Testing, Linkage to Care, and Reengagement in Care, Tennessee, 2013-2016. Public Health Rep, 2018. 133(2_suppl): p. 43s–51s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tanner M, et al. , Preexposure Prophylaxis for Prevention of HIV Acquisition Among Adolescents: Clinical Considerations. Morbidity and Mortality Weekly Report,, 2020(RR-3): p. 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garrison LE and Haberer JE, Pre-exposure Prophylaxis Uptake, Adherence, and Persistence: A Narrative Review of Interventions in the U.S. Am J Prev Med, 2021. 61(5 Suppl 1): p. S73–S86. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention, PrEP for HIV Prevention in the U.S., V.H. National Center for HIV, STD, and TB Prevention, Editor. 2021. [Google Scholar]
- 13.Sherman SG, et al. , PrEP awareness, eligibility, and interest among people who inject drugs in Baltimore, Maryland. Drug and alcohol dependence, 2019. 195: p. 148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute of Drug Abuse, Awareness and Use of Pre-Exposure Prophylaxis for HIV Rise in At-Risk Groups, But Not Enough., in https://nida.nih.gov/news-events/nida-notes/2021/03/awareness-use-pre-exposure-prophylaxis-for-hiv-rise-in-at-risk-groups-but-not-enough. 2021.
- 15.King K, et al. , Feasibility and Acceptability of HIV Self-Test Kit Distribution Through PrEP Clients’ Social and Sexual Networks to Increase HIV Testing and PrEP Information. J Acquir Immune Defic Syndr, 2022. 90(S1): p. S105–S113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Christakis NA and Fowler JH, Social contagion theory: examining dynamic social networks and human behavior. Stat Med, 2013. 32(4): p. 556–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hunter RF, et al. , Social network interventions for health behaviours and outcomes: A systematic review and meta-analysis. PLoS Med, 2019. 16(9): p. e1002890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glasgow RE, Vogt TM, and Boles SM, Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health, 1999. 89(9): p. 1322–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birkett M, et al. , Network Canvas: Key decisions in the design of an interviewer assisted network data collection software suite. Soc Networks, 2021. 66: p. 114–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qualtrics. 2005. [Google Scholar]
- 21.R: A language and environment for statistical computing, in R Core Team. 2014: R Foundation for Statistical Computing. [Google Scholar]
- 22.MacGowan RJ, et al. , Effect of Internet-Distributed HIV Self-tests on HIV Diagnosis and Behavioral Outcomes in Men Who Have Sex With Men: A Randomized Clinical Trial. JAMA Intern Med, 2020. 180(1): p. 117–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shava E, et al. , Feasibility of oral HIV self-testing in female sex workers in Gaborone, Botswana. PLoS One, 2021. 16(11): p. e0259508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mukora-Mutseyekwa F, et al. , Implementation of a campus-based and peer-delivered HIV self-testing intervention to improve the uptake of HIV testing services among university students in Zimbabwe: the SAYS initiative. BMC Health Serv Res, 2022. 22(1): p. 222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shrader CH, et al. , The Association Between Social and Spatial Closeness With PrEP Conversations Among Latino Men Who Have Sex With Men. J Acquir Immune Defic Syndr, 2021. 88(4): p. 366–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kanamori M, et al. , The association between egocentric sexual networks and sexual meeting venues with PrEP conversation and encouragement for use among Latinx men who have sex with men. AIDS Care, 2022: p. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shrader CH, et al. , PrEP Use and PrEP Use Disclosure are Associated with Condom Use During Sex: A Multilevel Analysis of Latino MSM Egocentric Sexual Networks. AIDS Behav, 2021. 25(5): p. 1636–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fuqua V, et al. , Using social networks to reach Black MSM for HIV testing and linkage to care. AIDS Behav, 2012. 16(2): p. 256–65. [DOI] [PubMed] [Google Scholar]
- 29.Kimbrough LW, et al. , Accessing social networks with high rates of undiagnosed HIV infection: The social networks demonstration project. Am J Public Health, 2009. 99(6): p. 1093–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Adebajo S, et al. , Evaluating the effect of HIV prevention strategies on uptake of HIV counselling and testing among male most-at-risk-populations in Nigeria; a cross-sectional analysis. Sex Transm Infect, 2015. 91(8): p. 555–60. [DOI] [PubMed] [Google Scholar]
- 31.Lightfoot MA, et al. , Using a Social Network Strategy to Distribute HIV Self-Test Kits to African American and Latino MSM. J Acquir Immune Defic Syndr, 2018. 79(1): p. 38–45. [DOI] [PubMed] [Google Scholar]
- 32.Okoboi S, et al. , Peer distribution of HIV self-test kits to men who have sex with men to identify undiagnosed HIV infection in Uganda: A pilot study. PLoS One, 2020. 15(1): p. e0227741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xiao W, et al. , Sexual network distribution of HIV self-testing kits: Findings from the process evaluation of an intervention for men who have sex with men in China. PLoS One, 2020. 15(4): p. e0232094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pettifor A, et al. , HIV self-testing among young women in rural South Africa: A randomized controlled trial comparing clinic-based HIV testing to the choice of either clinic testing or HIV self-testing with secondary distribution to peers and partners. EClinicalMedicine, 2020. 21: p. 100327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Iwelunmor J, et al. , The 4 youth by youth HIV self-testing crowdsourcing contest: A qualitative evaluation. PLoS One, 2020. 15(5): p. e0233698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matovu JKB, et al. , Formative research to inform the development of a peer-led HIV self-testing intervention to improve HIV testing uptake and linkage to HIV care among adolescents, young people and adult men in Kasensero fishing community, Rakai, Uganda: a qualitative study. BMC Public Health, 2020. 20(1): p. 1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quinn KG, et al. , The Influence of Peers on PrEP Perceptions and Use Among Young Black Gay, Bisexual, and Other Men Who Have Sex with Men: A Qualitative Examination. Arch Sex Behav, 2020. 49(6): p. 2129–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Young LE, et al. , PrEP Chicago: A randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clin Trials, 2018. 15(1): p. 44–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prochaska JO and Velicer WF, The transtheoretical model of health behavior change. Am J Health Promot, 1997. 12(1): p. 38–48. [DOI] [PubMed] [Google Scholar]
- 40.Parsons JT, et al. , Uptake of HIV Pre-Exposure Prophylaxis (PrEP) in a National Cohort of Gay and Bisexual Men in the United States. J Acquir Immune Defic Syndr, 2017. 74(3): p. 285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


