Abstract
Type I interferon receptor knockout (IFNAR−/−) mice are not able to generate a complete innate immune response; therefore, these mice are often considered to assess the pathogenicity of emerging viruses. We infected IFNAR−/− mice with a low or high dose of Lloviu virus (LLOV) or Bombali virus (BOMV) by the intranasal (IN) or intraperitoneal (IP) route and compared virus loads at early and late time points after infection. No signs of disease and no viral RNA were detected after IN infection regardless of LLOV dose. In contrast, IP infections resulted in increased viral loads in the high-dose LLOV and BOMV groups at the early time point. The low-dose LLOV and BOMV groups achieved higher viral loads at the late time point. However, there was 100% survival in all groups and no signs of disease. In conclusion, our results indicate a limited value of the IFNAR−/− mouse model for investigation of the pathogenicity of LLOV and BOMV.
Keywords: Cuevavirus, Ebolavirus, emerging filovirus, intranasal infection, intraperitoneal infection
The Filoviridae family consists of negative-sense, single-stranded, nonsegmented RNA viruses that can cause hemorrhagic diseases in humans and nonhuman primates (NHPs). The family encompasses 6 genera, Cuevavirus, Dianlovirus, Ebolavirus, Marburgvirus, Striavirus, and Thamnovirus, which contain at least 1 viral species each [1]. The most prominent members of the family are Ebola virus (EBOV) and Marburg virus (MARV), which have caused numerous outbreaks throughout Central and West Africa [2]. Yet, not all filoviruses can cause disease in humans and are considered apathogenic, such as Reston virus (RESTV) [2]. Two emerging filoviruses, Lloviu virus (LLOV) and Bombali virus (BOMV), have been identified within the past few decades. However, their pathogenic potential in humans is currently unknown [3, 4].
LLOV, a member of the Cuevavirus genus, was first identified in Schreiber's bats in the Cueva del Lloviu in Spain [5]. In 2016, it was found within the same bat species in Hungary and infectious virus was isolated from bat samples in 2022 [6]. BOMV, a member of the Ebolavirus genus, was first identified in free-tailed bats in the Bombali district of Sierra Leone in 2016 [7]. To date, infectious BOMV has yet to be isolated; however, recombinant virus was successfully generated applying reverse genetics techniques in cell culture and used here to assess its pathogenic potential [4].
Immunocompetent mouse models generally require a rodent-adapted filovirus to adequately evaluate disease and pathogenicity. Immunodeficient mice, especially type I interferon receptor knockout (IFNAR−/−) mice, have been shown to be susceptible to wild-type (wt) filovirus infection [8]. Previous work reported that IFNAR−/− mice succumbed to infection of Sudan virus (SUDV), EBOV, or MARV. However, neither Bundibugyo virus (BDBV), Taï Forest virus (TAFV), or RESTV infection results in signs of disease in IFNAR−/− mice [9, 10]. Because the IFNAR−/− mice are susceptible to some wt filovirus infections, they were the logical first choice to assess the pathogenic potential of LLOV and BOMV.
METHODS
Ethics Statement
All infectious work with filoviruses was performed following standard operating procedures approved by the Rocky Mountain Laboratories (RML) Institutional Biosafety Committee in the maximum containment laboratory at RML, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health. Animal work was performed in accordance with the recommendations described in the Guide for the Care and Use of Laboratory Animals of the National Institute of Health, the Office of Animal Welfare and the United States Department of Agriculture and was approved by the RML Animal Care and Use Committee (ACUC). Procedures were conducted in animals anesthetized by trained personnel under the supervision of veterinary staff. Food and water were available ad libitum. End point criteria as specified by RML ACUC-approved clinical score parameters were used to determine when animals were humanely euthanized.
Cell Lines and Viruses
Vero, Vero 76, and Huh7 cells were grown at 37°C and 5% CO2 in Dulbecco's modified Eagle's medium (DMEM; Sigma-Aldrich) containing 4.5 g/L D-glucose supplemented with 10% fetal bovine serum (FBS; Wisent, Inc), 2 mM L-glutamine, 50 U/mL penicillin, and 50 μg/mL streptomycin (all Thermo Fisher Scientific). SubK12-08 cells [11] were grown in RPMI-1640 media supplemented with 10% FBS, 2% MEM amino acid solution (50 ×), 110 mg/L sodium pyruvate, and 100 ug/mL Primocin (all Thermo Fisher Scientific). All cell lines were grown at 37°C in 5% CO2. RESTV [12], EBOV-Mayinga [13], recombinant LLOV (reverse genetics; rgLLOV) [14], wtLLOV [6], and recombinant BOMV [4] were grown on Vero E6 cells and deep-sequenced prior to study start. The wtLLOV from Hungary [6] was contaminated with mycoplasma and underwent cleanup using Mycoplasma-EX Kit (PromoKine) according to manufacturer's specifications. Propagation of wtLLOV in Vero E6 cells resulted in the highest viral RNA levels (Supplementary Figure 1) sufficient for genome sequencing and demonstrated with the least number of genome mutations after sequencing, therefore the wtLLOV stock was grown on Vero E6 cells. During cleanup and propagation, the mycoplasma-free wtLLOV stock (GenBank OQ630505) acquired 2 mutations (1 silent in VP35; 1 coding in glycoprotein [GP]) when compared to the sequence of the parental Hungarian strain (GenBank MZ541881; Supplementary Table 1).
LLOV Growth Kinetics
Vero E6, Vero, Vero 76, Huh7, or SubK12-08 cells were infected with 1:500 (5 mL/flask) of purified wtLLOV in plain DMEM media in a T150 cell culture flask and incubated 1 hour at 37°C. After 1 hour, media (2% FBS DMEM) was added (20 mL/flask) and incubated at 37°C and monitored for cytopathic effect, which was minimal in all tested cell lines. A sample was taken from each flask/day for viral RNA isolation to determine cell line and day for viral stock harvest. Purified wtLLOV titer was determined by immunofluorescence assay as previously described [15] using Lloviu virus VP35 antibody (Cell Signaling Technology) and secondary antibody Alexa Fluor 488 goat anti-rabbit IgG (Thermo Fisher Scientific).
IFNAR−/− Mouse Studies
Groups of adult C57BL/6 IFNAR−/− mice (male and female; n = 10/group) were infected intranasally (IN) with 50 µL/mouse containing 100 (low dose) 50% tissue culture infectious dose (TCID50) of wtLLOV or EBOV or 100 000 (high dose) TCID50 of RESTV or wtLLOV. At 7 days postinfection (dpi), 4 mice in each group were euthanized for sample collection. Groups of adult C57BL/6 IFNAR−/− mice (male and female; n = 14/group) were infected intraperitoneally (IP) with 0.2 mL/mouse containing 100 (low dose) TCID50 of wtLLOV, rgLLOV, BOMV, or EBOV or 100 000 (high dose) TCID50 of RESTV, wtLLOV, rgLLOV, or BOMV. At 3 (wtLLOV, BOMV) or 6 dpi (wtLLOV, rgLLOV, BOMV, RESTV, EBOV) 4 mice in each group were euthanized for sample collection. The mice were observed at least once daily for clinical signs of disease and humanely euthanized when they reached end point criteria.
RNA Extraction and RT-qPCR
RNA from growth kinetics, whole blood (EDTA) and tissue samples was extracted and 1-step real-time quantitative polymerase chain reaction (RT-qPCR) was performed as previously described [16]. The following primer/probe set based on the L polymerase was used for LLOV (Integrated DNA Technologies): forward primer 5′-AGAAAGAAACTCTCCTTCATCAGG-3′, reverse primer 5′-ACTCAATGAATGGTCGAGTGAA-3′, and probe 56-FAM/ACCATGTAC/ZEN/AAGTTCGTGGAGCGA/3IABkFQ/. Specific primer-probe sets for BOMV [4], RESTV [17], and EBOV [18] were described previously. RNA from viral stocks was used alongside samples as standards with known concentrations.
Enzyme-Linked Immunosorbent Assay
Serum was inactivated by gamma-irradiation (4 MRad) and removed from the maximum containment laboratory according to standard operating procedures approved by the RML Institutional Biosafety Committee. Enzyme-linked immunosorbent assay (ELISA) was performed as previously described [19]. LLOV GP, EBOV GP, and RESTV GP antigens were previously described [20]. BOMV GP was generated following the protocol described by Nakayama et al [19].
Histopathology and Immunohistochemistry
Tissue samples were fixed for 7 days in 10% neutral buffered formalin and processed as previously described [21]. An anti-LLOV VP35 antibody (catalog No. 72219; Cell Signaling) was used for immunohistochemistry.
Statistical Analysis
Two-way ANOVA with Tukey multiple comparisons was performed between groups for the RT-qPCR assays using Prism (version 9.3.1; GraphPad Software).
RESULTS
Intranasal Inoculation of LLOV in IFNAR−/− Mice Does not Lead to a Productive Infection
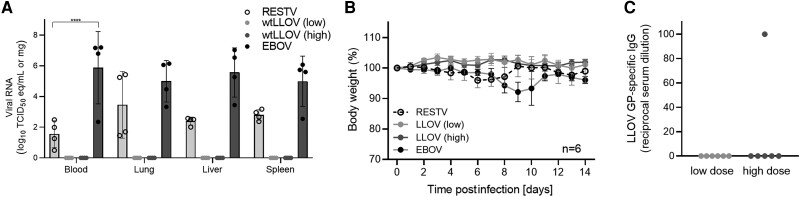
As the infectious wtLLOV was isolated from lung samples of infected Schreiber's bats [6], we first IN infected IFNAR−/− mice with wtLLOV at either 100 (low-dose) or 100 000 (high-dose) TCID50. Infection with high-dose RESTV or low-dose EBOV served as control. At 7 dpi, 4 mice in each group were euthanized for viral load analysis. We were unable to detect any LLOV RNA in collected samples regardless of infection dose (Figure 1A). There was no disease in any LLOV-infected mice as demonstrated by minimal body weight changes and the survival of all mice (Figure 1B and Supplementary Table 2). However, RESTV and EBOV RNA was detected in the collected samples confirming that filovirus infection of IFNAR−/− mice via the IN route is possible. While RESTV-infected mice all survived without signs of disease, the EBOV-infected mice developed prolonged disease with limited weight loss and 33% of the infected mice survived (Figure 1B and Supplementary Table 2). At study end, our LLOV GP-specific ELISA demonstrated no seroconversion for the LLOV low-dose group and only 1 mouse in the high-dose group had LLOV GP-specific IgG (Figure 1C). It appears that infection by the IN route fails to establish a productive LLOV infection in IFNAR−/− mice.
Figure 1.
Intranasal LLOV infection. IFNAR−/− mice (n = 10) were infected intranasally with either 100 (low-dose) or 100 000 (high-dose) TCID50 of LLOV, RESTV, or EBOV. At 7 days postinfection, 4 mice in each group were euthanized for sample analysis. A, Viral RNA in blood, lung, liver, and spleen. Geometric mean and standard deviation are depicted. B, Body weight changes over time. C, LLOV GP-specific IgG in serum at study end (day 28). B, C Mean and standard error of the mean are depicted. Statistical significance is indicated as ****P < .0001. Abbreviations: EBOV, Ebola virus; GP, glycoprotein; IFNAR−/−, type I interferon receptor knockout; IgG, immunoglobulin G; LLOV, Lloviu virus; RESTV, Reston virus; TCID50, 50% tissue culture infectious dose; wt, wild type.
Intraperitoneal Infections of Emerging Filoviruses in IFNAR−/− Mice
Infection by the IP route is the standard used in filovirus rodent models and was pursued next with wtLLOV, rgLLOV [14], and BOMV [4]. Again, EBOV and RESTV infections served as controls. Groups of 14 mice were infected on day 0, and 4 mice in each group were euthanized at 3 or 6 dpi for viral load determination. RESTV infection resulted in limited body weight changes and 100% survival, whereas EBOV infection caused uniform lethality in the IFNAR−/− mice (Supplementary Table 2) with viral RNA levels in the range as previously described (Figure 2A and 2D) [9, 10]. All high-dose LLOV- and BOMV-infected mice had detectable levels of viral RNA at 3 dpi regardless of sample type or viral stock, which declined by 6 dpi. At 6 dpi the viral RNA levels had increased within the low-dose groups compared to the 3 dpi time point (Figure 2A and 2D). Interestingly, wtLLOV-infected mice had higher viral RNA levels compared to rgLLOV mice within the blood, but minimal differences within the liver and spleen (Figure 2A). Histopathology samples were only collected for wtLLOV infection. No significant histopathology findings were observed in the spleen or liver of the low-dose wtLLOV group. However, in the high-dose wtLLOV group, 3 of 4 mice at 3 dpi displayed rare sporadic single-cell LLOV VP35 immunoreactivity of mononuclear cells in the splenic red pulp and circulating hepatic mononuclear cells presumed to reflect macrophages and circulating monocytes, respectively (Supplementary Figure 2). No immunoreactivity was observed in samples collected at 6 dpi (Supplementary Figure 2). All LLOV- and BOMV-infected mice survived with no signs of disease as evidenced by minimal body weight changes regardless of virus or dose (Figure 2B and 2E, and Supplementary Table 2). At study end, seroconversion and, therefore, confirmation of viral infection was investigated using LLOV or BOMV GP-specific IgG ELISAs. We found that all rgLLOV-infected mice seroconverted except for 1 mouse in the high-dose group. Similarly, only 1 mouse in the low-dose wtLLOV group did not seroconvert (Figure 2C). In contrast, 2 mice in each dose group of the BOMV-infected mice did not develop BOMV GP-specific antibodies implying that IP inoculation might not have led to a productive infection with BOMV (Figure 2F).
Figure 2.
Intraperitoneal infections of emerging filoviruses. IFNAR−/− mice were infected intraperitoneally with either 100 (low-dose) TCID50 EBOV, rgLLOV, wtLLOV, or BOMV, or 100 000 (high-dose) TCID50 of rgLLOV, wtLLOV, BOMV, or RESTV. At 3 or 6 days postinfection, 4 mice in each group were euthanized for sample analysis. A and D, Viral RNA in blood, liver, and spleen. B and E, Body weight changes over time. C, LLOV GP-specific or (F) BOMV GP-specific IgG in serum at study end (day 28). A, C, D, F Geometric mean and geometric standard deviation are depicted. B, E Mean and standard error of the mean are depicted. Statistical significance indicated as ****P < .0001. Abbreviations: BOMV, Bombali virus; EBOV, Ebola virus; FFU, focus-forming unit; GP, glycoprotein; IFNAR−/−,type I interferon receptor knockout; IgG, immunoglobulin G; RESTV, Reston virus; rgLLOV, reverse genetics Lloviu virus; TCID50, 50% tissue culture infectious dose; wtLLOV, wild-type Lloviu virus.
DISCUSSION
Our studies demonstrate that IN inoculation of LLOV IFNAR−/− mice does not result in infection; however, IN infection with EBOV leads to partial lethality. Smither et al reported similar results for EBOV after aerosol infection where 2 of 5 IFNAR−/− mice succumbed to disease while 3 of 5 showed no clinical signs of disease [22]. However, Lever et al demonstrated 100% mortality after aerosol EBOV and MARV infection in IFNAR−/− mice, but 100% survival after aerosol SUDV infection [23]. In contrast to IP infection, IN and aerosol infection can result in variability of the infectious dose taken up by each mouse which may account for the differences observed in survival between groups. In addition, the viral isolate and its number of cell culture passages, which could cause mutations, may contribute to the differences in outcome. The current study describes the emergence of a single mutation during propagation within the LLOV GP coding region resulting in an amino acid substitution. This single mutation could potentially impact LLOV pathogenicity because GP is the determinant of viral tropism and mediator of host cell entry [24]. However, as this amino acid substitution is located in the very N-terminal region of GP1, just outside the mapped receptor-binding domain [25], its impact may be limited but should be investigated in future studies. Finally, we can only speculate that filoviruses may be less likely to replicate efficiently within the upper respiratory tract of mice. This may be different in other animal species, as ferrets can be productively infected by the IN route with several filoviruses and develop lethal disease [26].
Previous data demonstrated that IP infection of certain isolates of SUDV and EBOV can cause lethal disease in IFNAR−/− mice while all mice survived after IP infection with BDBV, TAFV, or RESTV [9, 10]. Interestingly, these results do not entirely reflect disease development and lethality in humans or NHPs [27–29]. Our findings add to the expanding body of evidence that the type I interferon response may play different roles in filovirus pathogenicity depending on the filovirus species represented and sometimes even on the virus isolate used [9, 10, 30].
This is also the first report of LLOV and BOMV infection of IFNAR−/− mice. While we can productively infect these mice with BOMV and LLOV by the IP route, all mice survived the infection with minimal signs of disease. Interestingly, the recombinant LLOV clone was not as pathogenic as wtLLOV in IFNAR−/− mice. The first published wtLLOV sequence lacks important sequence information, including the intergenic region between the VP24 and L genes and the 5′ trailer region. To complement the missing sequences, rgLLOV was equipped with an artificial VP24-L intergenic region and the MARV trailer region [14]. These sequence differences between rgLLOV and wtLLOV might account for the observed differences in pathogenicity, highlighting the value of wt filovirus isolates and the necessity of complete viral sequence information for pathogenicity assessments. However, one could also consider creating a rodent-adapted rgLLOV by introducing mutations in VP24, which in previous studies have been shown to play a role in EBOV adaptation and virulence in rodent models [31, 32]. Such studies would expand our knowledge about the impact of these mutations on filovirus IFN antagonism and immune evasion. As the IFNAR−/− mouse model has limited predictive value for the human pathogenic potential of filoviruses [9, 10, 30], we cannot exclude that both viruses may be able to infect NHPs and humans, and may even cause disease in those species as demonstrated for RESTV in macaques [12]. However, previous data for BOMV in humanized mice suggest that the virus may possess an even lower potential to cause human disease compared to RESTV [33].
The results herein demonstrate that the IFNAR−/− mouse model has limited value for the assessment of the pathogenicity of these emerging filoviruses. While this model has been used for the evaluation of countermeasure efficacy for other emerging viruses like Zika virus [34] and Crimean Congo hemorrhagic fever virus [35], the lack of disease and only relatively low levels of viral replication hamper its use as a model for countermeasure evaluation against multiple wt filoviruses including LLOV and BOMV. Further studies in other immunocompetent filovirus animal models susceptible to wt virus infection, such as the Collaborative Cross mice, ferrets, and NHPs with LLOV and BOMV, are needed to investigate their pathogenic potential and establish an animal disease model.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Supplementary Material
Contributor Information
Paige Fletcher, Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA.
Friederike Feldmann, Rocky Mountain Veterinary Branch, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA.
Ayato Takada, Division of Global Epidemiology, International Institute for Zoonosis Control, Hokkaido University, Sapporo, Japan.
Nicholas A Crossland, National Emerging Infectious Diseases Laboratories, Boston University School of Medicine, Boston, Massachusetts, USA; Department of Pathology and Laboratory Medicine, Boston University School of Medicine, Boston, Massachusetts, USA.
Adam J Hume, National Emerging Infectious Diseases Laboratories, Boston University School of Medicine, Boston, Massachusetts, USA; Department of Microbiology, Boston University School of Medicine, Boston, Massachusetts, USA.
César Albariño, Viral Special Pathogens Branch, Centers for Disease Control and Prevention, Atlanta, Georgia, USA.
Gábor Kemenesi, National Laboratory of Virology, Szentágothai Research Center, University of Pécs, Pécs, Hungary; Institute of Biology, Faculty of Sciences, University of Pécs, Pécs, Hungary.
Heinz Feldmann, Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA.
Elke Mühlberger, National Emerging Infectious Diseases Laboratories, Boston University School of Medicine, Boston, Massachusetts, USA; Department of Microbiology, Boston University School of Medicine, Boston, Massachusetts, USA.
Andrea Marzi, Laboratory of Virology, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA.
Notes
Acknowledgments. We thank members of the Rocky Mountain Veterinary Branch for supporting the mouse studies and members of the Research Technology Branch for sequencing the filovirus stocks. We are grateful to Dr Antony W. Wood at Cell Signaling Technology for providing the LLOV anti-VP35 antibody.
Disclaimer . The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institutes of Health.
Financial support . This work was supported by the Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH). A. T. received support from the Science and Technology Research Partnership for Sustainable Development (grant number JP22jm0110019); from the Japan Agency for Medical Research and Development. This work used NIH S10 Shared Instrumentation Grants (grant numbers S10-OD026983 and SS10-OD030269).
Supplement sponsorship . This article appears as part of the supplement “10th International Symposium on Filoviruses.”
References
- 1. Kuhn JH, Amarasinghe GK, Basler CF, et al. ICTV virus taxonomy profile: filoviridae. J Gen Virol 2019; 100:911–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Marzi A, Banadyga L. Ebola virus (filoviridae). In: Bamford DH, Zuckerman M, eds. Encyclopedia of virology. 4th ed. Vol. 2. 2021:232–44. [Google Scholar]
- 3. Burk R, Bollinger L, Johnson JC, et al. Neglected filoviruses. FEMS Microbiol Rev 2016; 40:494–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McMullan LK, Flint M, Jenks MH, et al. Characterization of Bombali virus, a new bat filovirus. SSRN, doi: 10.2139/ssrn.4035855, 15February2022, preprint: not peer reviewed. [DOI] [Google Scholar]
- 5. Negredo A, Palacios G, Vazquez-Moron S, et al. Discovery of an ebolavirus-like filovirus in Europe. PLoS Pathog 2011; 7:e1002304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kemenesi G, Toth GE, Mayora-Neto M, et al. Isolation of infectious Lloviu virus from Schreiber's Bats in Hungary. Nat Commun 2022; 13:1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goldstein T, Anthony SJ, Gbakima A, et al. The discovery of Bombali virus adds further support for bats as hosts of ebolaviruses. Nat Microbiol 2018; 3:1084–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wong G, Qiu XG. Type I interferon receptor knockout mice as models for infection of highly pathogenic viruses with outbreak potential. Zool Res 2018; 39:3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bray M. The role of type I interferon response in the resistance of mice to filovirus infection. J Gen Virol 2001; 82:1365–73. [DOI] [PubMed] [Google Scholar]
- 10. Brannan JM, Froude JW, Prugar LI, et al. Interferon alpha/beta receptor-deficient mice as a model for Ebola virus disease. J Infect Dis 2015; 212(Suppl 2):S282–94. [DOI] [PubMed] [Google Scholar]
- 11. Takadate Y, Manzoor R, Saito T, et al. Receptor-mediated host cell preference of a bat-derived filovirus, Lloviu virus. Microorganisms 2020; 8:1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jahrling PB, Geisbert TW, Jaax NK, Hanes MA, Ksiazek TG, Peters CJ. Experimental infection of cynomolgus macaques with Ebola-Reston filoviruses from the 1989–1990 U.S. epizootic. Arch Virol Suppl 1996; 11:115–34. [DOI] [PubMed] [Google Scholar]
- 13. Marzi A, Feldmann F, Hanley PW, Scott DP, Gunther S, Feldmann H. Delayed disease progression in cynomolgus macaques infected with Ebola virus Makona strain. Emerg Infect Dis 2015; 21:1777–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hume AJ, Heiden B, Olejnik J, et al. Recombinant Lloviu virus as a tool to study viral replication and host responses. PLoS Pathog 2022; 18:e1010268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bhatia B, Meade-White K, Haddock E, Feldmann F, Marzi A, Feldmann H. A live-attenuated viral vector vaccine protects mice against lethal challenge with Kyasanur Forest disease virus. NPJ Vaccines 2021; 6:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. O'Donnell KL, Feldmann F, Kaza B, et al. Rapid protection of nonhuman primates against Marburg virus disease using a single low-dose VSV-based vaccine. EBioMedicine 2023; 89:104463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Haddock E, Saturday G, Feldmann F, et al. Reston virus causes severe respiratory disease in young domestic pigs. Proc Natl Acad Sci U S A 2021; 118:e2015657118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. de Wit E, Rosenke K, Fischer RJ, et al. Ebola laboratory response at the Eternal Love Winning Africa campus, Monrovia, Liberia, 2014–2015. J Infect Dis 2016; 214:S169–S76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nakayama E, Yokoyama A, Miyamoto H, et al. Enzyme-linked immunosorbent assay for detection of filovirus species-specific antibodies. Clin Vaccine Immunol 2010; 17:1723–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Changula K, Kajihara M, Mori-Kajihara A, et al. Seroprevalence of filovirus infection of rousettus aegyptiacus bats in Zambia. J Infect Dis 2018; 218:S312–S7. [DOI] [PubMed] [Google Scholar]
- 21. Rosenbloom R, Gavrish I, Tseng AE, et al. Progression and dissemination of pulmonary Mycobacterium avium infection in a susceptible immunocompetent mouse model. Int J Mol Sci 2022; 23:5999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smither SJ, Eastaugh L, Ngugi S, et al. Ebola virus Makona shows reduced lethality in an immune-deficient mouse model. J Infect Dis 2016; 214:S268–S74. [DOI] [PubMed] [Google Scholar]
- 23. Lever MS, Piercy TJ, Steward JA, et al. Lethality and pathogenesis of airborne infection with filoviruses in A129 alpha/beta −/− interferon receptor-deficient mice. J Med Microbiol 2012; 61:8–15. [DOI] [PubMed] [Google Scholar]
- 24. Takada A. Filovirus tropism: cellular molecules for viral entry. Front Microbiol 2012; 3:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kuhn JH, Radoshitzky SR, Guth AC, et al. Conserved receptor-binding domains of lake Victoria marburgvirus and Zaire ebolavirus bind a common receptor. J Biol Chem 2006; 281:15951–8. [DOI] [PubMed] [Google Scholar]
- 26. Schiffman Z, Liu G, Cao W, et al. The ferret as a model for filovirus pathogenesis and countermeasure evaluation. ILAR J 2022; 61:62–71. [DOI] [PubMed] [Google Scholar]
- 27. Nakayama E, Saijo M. Animal models for Ebola and Marburg virus infections. Front Microbiol 2013; 4:267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. St Claire MC, Ragland DR, Bollinger L, Jahrling PB. Animal models of ebolavirus infection. Comp Med 2017; 67:253–62. [PMC free article] [PubMed] [Google Scholar]
- 29. Languon S, Quaye O. Filovirus disease outbreaks: a chronological overview. Virology (Auckl) 2019; 10:1178122X19849927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Marzi A, Chadinah S, Haddock E, et al. Recently identified mutations in the Ebola virus–Makona genome do not alter pathogenicity in animal models. Cell Rep 2018; 23:1806–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Banadyga L, Dolan MA, Ebihara H. Rodent-adapted filoviruses and the molecular basis of pathogenesis. J Mol Biol 2016; 428:3449–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pappalardo M, Reddin IG, Cantoni D, Rossman JS, Michaelis M, Wass MN. Changes associated with Ebola virus adaptation to novel species. Bioinformatics 2017; 33:1911–5. [DOI] [PubMed] [Google Scholar]
- 33. Bodmer BS, Breithaupt A, Heung M, et al. In vivo characterization of the novel ebolavirus Bombali virus suggests a low pathogenic potential for humans. Emerg Microbes Infect 2023; 12:2164216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Marzi A, Emanuel J, Callison J, et al. Lethal Zika virus disease models in young and older interferon α/β receptor knock out mice. Front Cell Infect Microbiol 2018; 8:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hawman DW, Meade-White K, Haddock E, et al. Crimean-Congo hemorrhagic fever mouse model recapitulating human convalescence. J Virol 2019; 93:e00554-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.