Abstract
Ocular complications of Ebola virus disease are well-documented and long-term sequelae in survivors are common and lead to considerable morbidity. However, little is currently known regarding EBOV's tropism and replication kinetics within the eye. To date, limited studies have utilized in vitro infections of ocular cell lines and analyses of archived pathology samples to investigate these issues. Here, we employed ex vivo cultures of cynomolgus macaque eyes to determine the tropism of EBOV in 7 different ocular tissues: cornea, anterior sclera with bulbar conjunctiva, ciliary body, iris, lens, neural retina, and retina pigment epithelium. We report that, except for neural retina, all tissues supported EBOV replication. Retina pigment epithelium produced the fastest growth and highest viral RNA loads, although the differences were not statistically significant. Immunohistochemical staining confirmed and further characterized infection. This study demonstrates that EBOV has a broad tropism within the eye.
Keywords: Ebola, EBOV, EVD, Ebola virus, Ebola virus disease, eye, ocular, tropism
Ebola virus disease (EVD) in humans results from infection with the zoonotic filovirus Ebola virus (EBOV), species Zaire ebolavirus [1]. While ocular complications of EVD in humans were known prior to the 2013–2016 EVD epidemic in West Africa [2, 3], the largest and longest EVD epidemic on record [4], this event revealed a much fuller extent to which EVD can affect the eye. These effects include both short-term complications of active infection, such as conjunctivitis, subconjunctival hemorrhages, and vision loss of unclear etiology [5, 6], and long-term sequelae in convalescent survivors, such as uveitis, retinal lesions, and cataract [7–10]. In 1 case, persistence of infectious virus was documented in aqueous humor months after convalescence [11]. It has also been suggested that the eye may serve as a route of transmission [12], and studies have demonstrated that macaques can be infected with EBOV via the conjunctiva [13, 14]. Nevertheless, relatively little is known regarding the specifics of EBOV infection within the eye. In this study, our goal was to determine the ocular tropism of EBOV in a model organism known to closely reflect human pathogenesis of EVD—the cynomolgus macaque (Macaca fascicularis)—using ex vivo cultures of 7 different ocular tissues.
METHODS
Tissue Harvest
Two cynomolgus macaques (Macaca fascicularis) that were not part of any study protocol required euthanasia for noninfectious wellness concerns. Eyes were harvested from the animals and dissected immediately following euthanasia. Seven tissues were isolated from each eye under sterile conditions with a dissecting microscope: cornea, anterior sclera with bulbar conjunctiva, ciliary body, iris, lens, neural retina, and retina pigment epithelium. These tissues from each of the 4 eyes were then divided equally into 2 specimens, creating 8 total replicates of each tissue, and allowed to equilibrate (37°C, 5% CO2) in appropriate media for 24 hours prior to inoculation with virus.
Culture Media
Five types of culture media were prepared for use with the different tissues as follows: (1) M199 with Earle's salts and 0.1% bovine serum albumin (for lens) [15]; (2) Dulbecco’s Modified Eagle’s Medium (DMEM) with 20% fetal bovine serum (FBS) (for retina pigment epithelium and iris) [16]; (3) DMEM/F-12 with 20% FBS (for cornea and sclera with bulbar conjunctiva) [17]; (4) neurobasal-A supplemented with 10% FBS, 2% B-27, and 1% N-2 (for neural retina) [18]; and (5) DMEM with 10% FBS (for ciliary body) [19]. All media were supplemented with 50 μg/mL L-glutamine, 50 μg/mL streptomycin, 50 IU/mL penicillin, and 2.5 μg/mL amphotericin B.
Ebola Virus Infection of Tissue
Six-well plates were prepared containing 1 tissue sample per well. Each tissue sample was inoculated for 1 hour with 100 TCID50 (50% tissue culture infectious dose) EBOV Makona C07 diluted in appropriate media. The tissue samples were washed twice following inoculation prior to the addition of 7 mL of fresh appropriate media. All tissue samples were incubated at 37°C with 5% CO2. Supernatant was sampled at 0, 24, 48, 72, 96, and 120 hours postinoculation for quantification of viral RNA and tissue samples were collected at the end of the experiment for pathology. All infectious work took place within biosafety level 4 (BSL-4) containment, and all samples were removed from BSL-4 using approved virus inactivation protocols.
Ebola Virus Droplet Digital PCR
Viral RNA was extracted from the supernatant with a QIAGEN QIAamp Viral RNA Mini Kit per the manufacturer's instructions and was then quantified with a Bio-Rad QX200 droplet digital polymerase chain reaction (ddPCR) system with automated droplet generation by a Bio-Rad AutoDG instrument. The 1-step assay utilized targeted a portion of the EBOV polymerase (L) gene as previously described [20], with primer and probe (2 probes were used) sequences as follows: 5′-CAGCCAGCAATTTCTTCCAT-3′, 5′-TTTCGGTTGCTGTTTCTGTG-3′, 56-FAM/ATCATTGGC/ZEN/RTACTGGAGGAGCAG/3IABkFQ, and 56-FAM/TCATTGGCG/ZEN/TACTGGAGGAGCAGG/3IABkFQ.5. The results from the ddPCR quantification are reported as log10 EBOV RNA copies/mL and were confirmed with a quantitative reverse transcription PCR (qRT-PCR) assay using a standard curve.
Histology
Tissues were fixed in 10% neutral buffered formalin with 2 fixative changes for a minimum of 7 days. Tissues were placed in cassettes and processed with a Sakura VIP-6 Tissue Tek using a graded series of ethanol, xylene, and PureAffin. Embedded tissues were sectioned at 5 µm and dried overnight at 42°C prior to staining. Specific anti-EBOV immunoreactivity was detected using a rabbit polyclonal anti-EBOV VP40 antibody (kindly provided by Dr Yoshihiro Kawaoka, University of Wisconsin-Madison) at a 1:2000 dilution using the Discovery ULTRA automated staining platform with a Discovery purple kit.
Data Analysis
All data were prepared and statistical analysis was performed with GraphPad Prism 9.5.1. The exact nature of the tests used are described where appropriate. Significance was assessed at P ≤ .05.
RESULTS
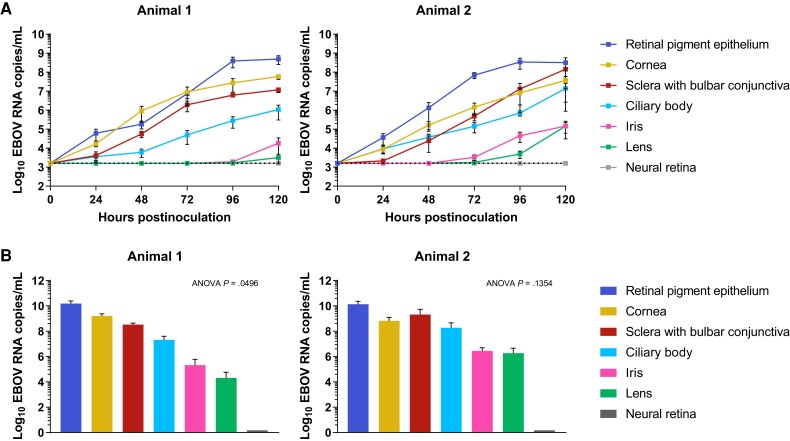
Six of the 7 cultured tissues (cornea, anterior sclera with bulbar conjunctiva, ciliary body, iris, lens, and retina pigment epithelium) supported EBOV replication, with only neural retina failing to produce any detectable growth (Figure 1). Retina pigment epithelium consistently demonstrated the most rapid growth kinetics and produced the highest end viral RNA load. Iris and lens both demonstrated delayed growth kinetics and produced the lowest end viral titers. Only retina pigment epithelium appeared to reach peak viral RNA load over the 5 days of sampling; growth curves from the other tissues appeared to still be in a logarithmic growth phase at the final time point. Cornea and sclera with bulbar conjunctiva produced similar viral growth in all 8 replicates; retina pigment epithelium failed to produce growth in 1 replicate; ciliary body produced growth in 6 of 8 replicates; iris and lens produced growth in half (n = 4) of the replicates. None of the neural retina replicates produced any detectable growth.
Figure 1.
Ebola virus (EBOV) growth in 7 ex vivo cynomolgus macaque ocular tissues. A, Growth curves for each tissue per animal. Individual points represent means and error bars represent standard error. The dotted line represents the limit of detection for the assay (3.2 log10 EBOV RNA copies/mL). Each tissue has 4 replicates per animal at every time point except for neural retina, which has only 2 replicates for animal 1 (2 were lost during the initial inoculation and washing procedure). No growth was detected in any of the neural retina replicates (gray line). B, Area under the curve for the growth curves by animal. Means are shown and error bars represent standard error. The P values for 1-way ANOVA are shown. Post hoc analysis of the 1-way ANOVA results with Tukey's multiple comparison test demonstrated no significant (P ≤ .05) differences between pairs of means.
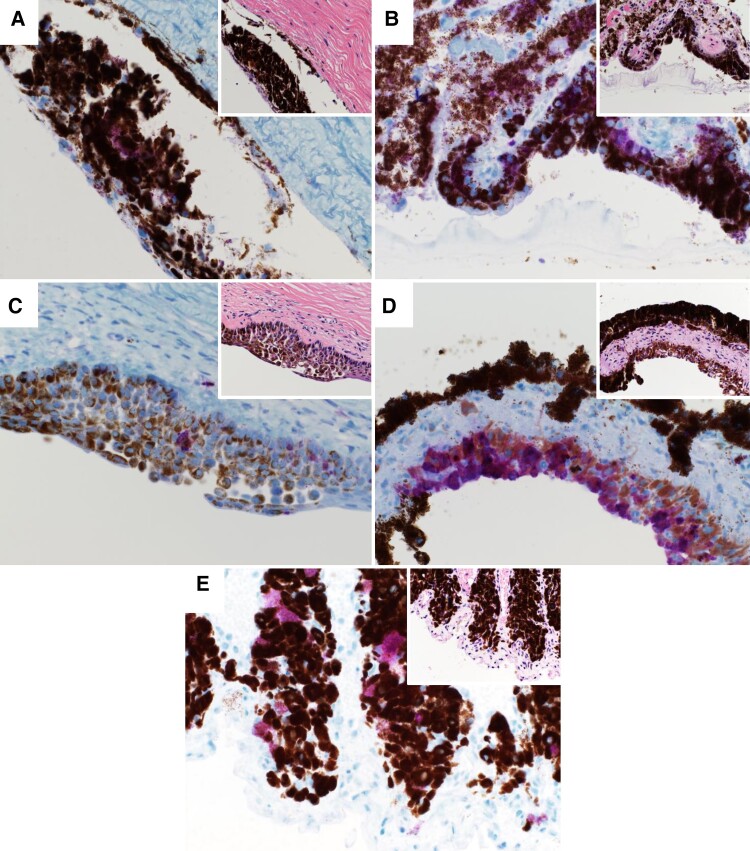
On histopathological examination, abundant pigment within the sclera, ciliary body, iris, and a focal area within the cornea obscured cellular detail; however, no inflammatory cell infiltrate was noted (Figure 2). A focal area of the corneal epithelium was thickened and disrupted with few individual necrotic epithelial cells. EBOV immunohistochemical staining revealed scattered EBOV immunoreactivity in the scleral epithelium, moderate immunoreactivity in epithelial cells of the ciliary body and cornea, and abundant stromal cells and melanocytes within the iris.
Figure 2.
Histopathology of cynomolgus macaque ocular tissues following ex vivo infection with Ebola virus. Large images show immunohistochemical staining for Ebola virus, 40 × magnification; insets show hematoxylin and eosin staining, 40 × magnification: (A) sclera with bulbar conjunctiva; (B) ciliary body; (C) cornea; (D) iris; and (E) retina pigment epithelium.
The 7 tissue types appeared to be viable upon gross microscopic examination at the end of the experiment, and 5 of the 7 tissues (cornea, anterior sclera with bulbar conjunctiva, ciliary body, iris, and retina pigment epithelium) also had viability confirmed by histopathological examination (Figure 2). However, amongst the individual replicates of tissues, 2 of the ciliary body samples and 1 of the retina pigment epithelium samples were contaminated at the end of the experiment. These 3 replicates also failed to produce any viral growth (as noted above). Lens and neural retina tissues were unable to be adequately prepared for histopathological examination due to the extremely delicate nature of these tissues, particularly after they were subdivided for the experiments conducted here.
DISCUSSION
Here we have shown that EBOV has a broad tropism within the eye. Macaques are the gold-standard model for EVD and this experiment utilized freshly harvested and dissected ex vivo ocular tissues from 2 animals. Previous EBOV challenge studies in macaques have noted the development of ocular sequelae in survivors and/or molecular evidence of persistent EBOV infection in various ocular tissues [21–23]—findings consistent with human EVD. One previous in vitro study utilizing immortalized human retina pigment epithelium cells found EBOV replication was supported to high titers and speculated that retina pigment epithelium may serve as a potential ocular reservoir for EBOV, particularly given the unique immunological profile consisting of an upregulated type I interferon (IFN) response in these tissues (EBOV has been observed to suppress type I IFN responses in most other tissues) [24]. Our findings reported here suggest that, while retina pigment epithelium does indeed apparently support EBOV growth to high titers, the overall dynamics of EBOV replication and persistence in the eye may be dependent upon multiple tissue types, given the broad tropism we observed.
Comparisons between the growth kinetics of EBOV in these tissues should be approached cautiously, as each tissue sample likely varied significantly in terms of overall cellular content (eg, the lens is comprised predominantly of crystallin protein and the only cellular component is a thin anterior epithelium) and therefore a standardized inoculum multiplicity of infection could not be used between tissue types.
Given the prevalence of ocular sequelae in EVD survivors and the possibility of ocular transmission of EBOV, further investigation is needed. A multifaceted approach using clinical data, animal studies, in vitro culture—and, as we have done here, ex vivo experiments with fresh ocular tissues—can best further our understanding of EBOV in the eye.
Contributor Information
M Jeremiah Matson, Laboratory of Virology, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA; Department of Internal Medicine, University of Utah Health, Salt Lake City, Utah, USA.
Trent Bushmaker, Laboratory of Virology, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA.
Dana P Scott, Rocky Mountain Veterinary Branch, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA.
Rebecca Rosenke, Rocky Mountain Veterinary Branch, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA.
Greg Saturday, Rocky Mountain Veterinary Branch, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA.
Daniel S Chertow, Laboratory of Virology, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA; Critical Care Medicine Department, Clinical Center, National Institutes of Health, Bethesda, Maryland, USA.
Vincent J Munster, Laboratory of Virology, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, Montana, USA.
Notes
Author contributions. M. J. M. conceived the study, performed experiments, analyzed data, and wrote the manuscript. T. B. performed experiments and approved the manuscript. D. P. S., R. R., and G. S. prepared and analyzed pathology specimens and approved the manuscript. D. S. C. analyzed data, and edited and approved the manuscript. V. J. M. performed experiments, analyzed data, and edited and approved the manuscript.
Acknowledgments. We are very grateful for the training and guidance on ocular dissection and ex vivo ocular tissue culture techniques provided by Professor Frank Lovicu, PhD, University of Sydney Faculty of Medicine and Health, Sydney, Australia. We also thank Jamie Lovaglio, DVM and Friederike Feldmann, MS, both at NIH/NIAID Rocky Mountain Laboratories, for their assistance in harvesting the eyes used for this study and with conducting the infection experiments in BSL-4 containment, respectively.
Financial support. This work was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Supplement sponsorship . This article appears as part of the supplement “10th International Symposium on Filoviruses.”
References
- 1. Feldmann H, Sprecher A, Geisbert TW. Ebola. N Engl J Med 2020; 382:1832–42. [DOI] [PubMed] [Google Scholar]
- 2. Bwaka MA, Bonnet MJ, Calain P, et al. Ebola hemorrhagic fever in Kikwit, Democratic Republic of the Congo: clinical observations in 103 patients. J Infect Dis 1999; 179(Suppl 1):S1–7. [DOI] [PubMed] [Google Scholar]
- 3. Kibadi K, Mupapa K, Kuvula K, et al. Late ophthalmologic manifestations in survivors of the 1995 Ebola virus epidemic in Kikwit, Democratic Republic of the Congo. J Infect Dis 1999; 179(Suppl 1):S13–4. [DOI] [PubMed] [Google Scholar]
- 4. Matson MJ, Chertow DS, Munster VJ. Delayed recognition of Ebola virus disease is associated with longer and larger outbreaks. Emerg Microbes Infect 2020; 9:291–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fitzpatrick G, Vogt F, Moi Gbabai OB, et al. The contribution of Ebola viral load at admission and other patient characteristics to mortality in a Medecins Sans Frontieres Ebola Case Management Centre, Kailahun, Sierra Leone, June-October 2014. J Infect Dis 2015; 212:1752–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Oza S, Sesay AA, Russell NJ, et al. Symptom- and laboratory-based Ebola risk scores to differentiate likely Ebola infections. Emerg Infect Dis 2017; 23:1792–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mattia JG, Vandy MJ, Chang JC, et al. Early clinical sequelae of Ebola virus disease in Sierra Leone: a cross-sectional study. Lancet Infect Dis 2016; 16:331–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jagadesh S, Sevalie S, Fatoma R, et al. Disability among Ebola survivors and their close contacts in Sierra Leone: a retrospective case-controlled cohort study. Clin Infect Dis 2018; 66:131–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Group PIS, Sneller MC, Reilly C, et al. A longitudinal study of Ebola sequelae in Liberia. N Engl J Med 2019; 380:924–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Steptoe PJ, Momorie F, Fornah AD, et al. Multimodal imaging and spatial analysis of Ebola retinal lesions in 14 survivors of Ebola virus disease. JAMA Ophthalmol 2018; 136:689–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Varkey JB, Shantha JG, Crozier I, et al. Persistence of Ebola virus in ocular fluid during convalescence. N Engl J Med 2015; 372:2423–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Judson S, Prescott J, Munster V. Understanding Ebola virus transmission. Viruses 2015; 7:511–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mire CE, Geisbert JB, Agans KN, Deer DJ, Fenton KA, Geisbert TW. Oral and conjunctival exposure of nonhuman primates to low doses of Ebola Makona virus. J Infect Dis 2016; 214(Suppl 3):S263–S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cross RW, Prasad AN, Woolsey CB, et al. Natural history of nonhuman primates after conjunctival exposure to Ebola virus. Sci Rep 2023; 13:4175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wojciechowski MC, Mahmutovic L, Shu DY, Lovicu FJ. ERK1/2 signaling is required for the initiation but not progression of TGFβ-induced lens epithelial to mesenchymal transition (EMT). Exp Eye Res 2017; 159:98–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sugita S, Streilein JW. Iris pigment epithelium expressing CD86 (B7-2) directly suppresses T cell activation in vitro via binding to cytotoxic T lymphocyte-associated antigen 4. J Exp Med 2003; 198:161–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Smeringaiova I, Utheim TP, Jirsova K. Ex vivo expansion and characterization of human corneal endothelium for transplantation: a review. Stem Cell Res Ther 2021; 12:554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schaeffer J, Delpech C, Albert F, Belin S, Nawabi H. Adult mouse retina explants: from ex vivo to in vivo model of central nervous system injuries. Front Mol Neurosci 2020; 13:599948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tamimi Y, Skarie JM, Footz T, Berry FB, Link BA, Walter MA. FGF19 is a target for FOXC1 regulation in ciliary body-derived cells. Hum Mol Genet 2006; 15:3229–40. [DOI] [PubMed] [Google Scholar]
- 20. de Wit E, Rosenke K, Fischer RJ, et al. Ebola laboratory response at the Eternal Love Winning Africa campus, Monrovia, Liberia, 2014–2015. J Infect Dis 2016; 214(Suppl 3):S169–S76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Alves DA, Honko AN, Kortepeter MG, et al. Necrotizing scleritis, conjunctivitis, and other pathologic findings in the left eye and brain of an Ebola virus–infected rhesus macaque (Macaca mulatta) with apparent recovery and a delayed time of death. J Infect Dis 2016; 213:57–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zeng X, Blancett CD, Koistinen KA, et al. Identification and pathological characterization of persistent asymptomatic Ebola virus infection in rhesus monkeys. Nat Microbiol 2017; 2:17113. [DOI] [PubMed] [Google Scholar]
- 23. Worwa G, Cooper TK, Yeh S, et al. Persistent intraocular Ebola virus RNA is associated with severe uveitis in a convalescent rhesus monkey. Commun Biol 2022; 5:1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Smith JR, Todd S, Ashander LM, et al. Retinal pigment epithelial cells are a potential reservoir for Ebola virus in the human eye. Transl Vis Sci Technol 2017; 6:12. [DOI] [PMC free article] [PubMed] [Google Scholar]