Abstract
Background:
There is a debate over the use of aspirin after total knee arthroplasty (TKA) for venous thromboembolism (VTE) prophylaxis. To evaluate the clinical effectiveness and safety of aspirin after TKA, the authors performed a meta-analysis of randomized controlled trials that compared aspirin with low-molecular-weight heparin (LMWH).
Methods:
PubMed, Cochrane Library, Embase, and Web of Science were last searched on 31 January 2023 for studies comparing the effect of VTE prophylaxis between aspirin and LMWH. The results of eligible studies were analyzed in terms of VTE, deep venous thrombosis, pulmonary embolism, and bleeding complications rates.
Results:
Six randomized controlled trials including 6772 patients met the inclusion criteria. LMWH showed a statistically significant reduction in the overall VTE rate (RR 1.46, 95% CI: 1.16–1.84). No significant differences in deep venous thrombosis, pulmonary embolism, and bleeding complications rates were found between aspirin and LMWH.
Conclusion:
Compared with LMWH, aspirin presents a higher risk of VTE after TKA. In terms of safety, aspirin and LMWH show comparable outcomes. The results do not support the role of aspirin role as an anticoagulant for preventing VTE after TKA.
Keywords: aspirin, low-molecular-weight heparin (LMWH), total knee arthroplasty (TKA), venous thromboembolism prophylaxis
Introduction
Highlights
Aspirin has a higher risk of venous thromboembolism (VTE) compared to low-molecular-weight heparin as a prophylactic medication for VTE after knee joint arthroplasty.
Aspirin and low-molecular-weight heparin have similar outcomes in terms of bleeding complications.
Aspirin is not recommended as a VTE prophylactic medication for patients after knee joint arthroplasty.
Low-molecular-weight heparin (LMWH) is a classic strategy for thromboprophylaxis following joint replacement surgery, but it is inconvenient and adds complexity to the cost of post-total knee arthroplasty (TKA) care1,2. According to reports, a 30-day supply of rivaroxaban costs ~$379–$450, while LMWH is estimated to range from $450 to $8903. In contrast, aspirin costs around $2 per month and does not require monitoring3. Simplified and affordable alternative therapies are desired, such as using aspirin alone as a prophylaxis for venous thromboembolism (VTE) after TKA, which was recommended by the National Institute for Health and Care Excellence (NICE) in 20184. Many countries have started using aspirin as a thromboprophylaxis strategy after joint replacement surgery3,5–9. There are no updated guidelines advising against the use of aspirin for TKA prevention.
The research on aspirin for thromboprophylaxis in TKA remains an important topic. A recent meta-analysis found that there was no statistically significant difference in the clinical efficacy and safety of aspirin compared to other anticoagulants used for VTE prophylaxis after THR and TKA10. A large randomized controlled trial (RCT) investigated the effectiveness of using aspirin as a thromboprophylaxis strategy following knee or hip replacement, and the results showed that aspirin had a higher risk of VTE compared to LMWH11. Some recently published RCTs on the use of aspirin for thromboprophylaxis after TKA are available, but they have not been incorporated into guidelines11–13.
Our study included three updated researches11–13, including a large RCT (n=9711), which will contribute to the updating of guidelines and guide clinical practice. We hypothesize that aspirin may be less effective than LMWH in preventing thrombosis after TKA, but it may carry a lower risk of bleeding. To assess the clinical effectiveness and safety of aspirin after TKA, we conducted a meta-analysis of RCTs that compared aspirin with LMWH.
Methods
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and has been reported in line with the AMSTAR (Assessing the methodological quality of systematic reviews) Guidelines14,15. The study protocol was registered on PROSPERO.
Search strategy and selection criteria
Comprehensive literature search for studies comparing aspirin with LMWH after TKA was conducted (last search on 31 January 2023) in the electronic databases PubMed, Cochrane Library, Embase, and Web of Science. After removing duplicate articles, four reviewers independently screened the titles and abstracts to identify eligible RCTs.
Furthermore, the same four reviewers independently reviewed the full texts of the articles identified above. The inclusion criteria were: TKA, aspirin versus LMWH for prophylactic anticoagulation, and availability of VTE [including deep venous thrombosis (DVT) and/or pulmonary embolism (PE)] rate or complication rate. Studies of revised TKA and non-RCTs were excluded. Disagreements on the eligibility of full-text articles, if any, were resolved by discussion with a senior author.
Data extraction
The same four reviewers independently extracted the desired data from the included studies using a standardized form, including: first author, year of publication, country, number of included patients, patient characteristics, the incidence of VTE, DVT, PE, wound, and bleeding complications. For the missing data, we contacted the authors to acquire the original data as far as possible, and if failed, the values would be derived from figures using Plot Digitizer. Disagreements, if any, were resolved by discussion.
Quality assessment
The same four reviewers independently assessed the included studies for the risk of bias using the Cochrane Collaboration’s risk of Bias Tool. This tool consists of seven domains of bias (random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias), and each domain was rated as of a low, unclear, or high risk of bias. Discrepancies, if any, were resolved by discussion.
Primary and secondary outcomes
The primary outcome of the study is the total incidence of VTE, with the endpoint of VTE being either DVT or PE. DVT is defined as thrombosis in the deep veins of the lower limbs detected through doppler ultrasound, CT, or venography. PE, on the other hand, refers to pulmonary artery embolism identified through CT or venography. The secondary outcome of the study is bleeding complications, which can be classified as major or minor bleeding. Major bleeding includes a decrease in hemoglobin of greater than or equal to 2 g/dl, transfusion of greater than or equal to 2 units of packed red blood cells, symptomatic bleeding in a critical area, or fatal bleeding. Meanwhile, minor bleeding refers to bleeding that does not meet the criteria for major bleeding or clinically relevant nonmajor bleeding (which requires or prolongs hospitalization or results in laboratory testing, imaging, compression, a procedure, an interruption of the study medication, or a change in concomitant therapies).
Statistical analysis
The outcomes of this study were VTE, DVT, PE, and bleeding complications rates, which were extracted in the form of dichotomous variable as an absolute number and percentage. Considering the potential heterogeneity arising from the timing, frequency, and dosage of medication administration, we used the DerSimonian–Laird random-effects model for analysis, and the results were presented as a risk ratio with a 95% CI. A subgroup analysis based on different VTE endpoints and bleeding sites was conducted. All analyses were performed using R Version 4.3.1.
Results
Literature search
Figure 1 shows the flow chart of literature search and study selection. After screening the titles and abstracts, 510 studies were excluded. Then, 11 studies were reviewed by full-text and 5 studies were removed based on the inclusion criteria. Eventually, six RCTs11–13,16–18 with a total of 6772 patients were included for final analyses.
Figure 1.
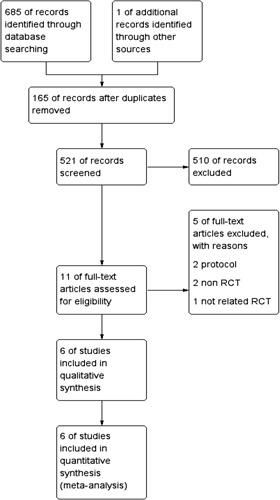
Flowchart of literature retrieval.
Baseline study characteristics
Table 1 shows the baseline characteristics of the included RCTs. The dosage of aspirin for prophylactic anticoagulation was 100 mg in five studies11–13,16,18 and 325 mg in one study17. Besides drug prevention, three studies11,17,18 also adopted mechanical VTE prophylaxis in both the aspirin group and LMWH group, and one study16 adopted mechanical prophylaxis only in the aspirin group. Four studies11–13,16 followed up with the patients for 90 days, one study18 followed up for 4 weeks, and one study17 followed up for 6 weeks.
Table 1.
Study characteristic.
| Patient number | Mean (SD or range) age, years | Sex (female/male) | Dosage and duration | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Country | Aspirin | LMWH | Aspirin | LMWH | Aspirin | LMWH | Aspirin | LMWH | Use of mechanical VTE prophylaxis | Routine DVT screening or symptomatic DVT | DVT diagnostic methods | Follow-up duration | Outcome of VTE risk of aspirin, RR (95% CI) |
| Fuente 13 | Mexico | 188 | 214 | 70.33 | 71.31 | 0.85 | 1.04 | 100 mg/d, for 30 days | Enoxaparin 40–60 mg, for 30 days | NA | NA | Venous ultrasonography | 90 days | 0.59 [0.10–3.47] |
| Gelfer 16 | Israel | 28 | 20 | 68 (10.4) | 67 (8.7) | 1.61 | 1.90 | 100 mg/d, duration NS | Enoxaparin 40 mg/d, duration NS | Pneumatic compression system in aspirin group only | Routine screening (5 8 days after surgery) plus any symptomatic VTE during follow-up | Venogram for screening plus venous ultrasonography for symptomatic events | 90 days | 0.71 [0.20–2.52] |
| Sidhu 11 | Australia | 3348 | 2357 | 67.0 (61.0–74.0) | 68.0 (61.0–74.0) | 1.30 | 1.33 | 100 mg/d, for 14 days | Enoxaparin 40 mg/d, for 14 days | Compression stockings in both group | Symptomatic | Venous ultrasonography | 90 days | 1.65 [1.23–221] |
| Westrich 17 | USA | 136 | 139 | 69.0 (12.1) | 68.9 (9.6) | 1.57 | 2.02 | 325 mg/d, for 28 days | Enoxaparin 40 mg/d, for 28 days | Calf compression device in both groups | Routine screening (3–5 days after surgery) plus any symptomatic VTE during follow-up | Venous ultrasonography | 6 weeks | 1.32 [0.76–2.29] |
| Zhou 12 | China | 60 | 60 | 66.4 (7.6) | 64.1 (6.7) | 1.31 | 1.07 | 100 mg/d, for 30 days | Dalteparin sodium 2500 IU/d, for 30 days | NA | Routine screening (3,7,30,60, and 90 days after surgery) | Venous ultrasonography | 90 days | 1.40 [0.47–4.17] |
| Zou 18 | China | 110 | 112 | 62.7 (47–79) | 65.7 (54–80) | 2.93 | 4.6 | 100 mg/d, for 14 days | Enoxaparin 4000 U/d, for 14 days | Elastic bandages and ankle pump in both groups | Routing screening (2 and 4 weeks after surgery) | Venous ultrasonography | 4 weeks | 1.31 [0.69–2.50] |
DVT, deep vein thrombosis; LMWH, low-molecular-weight heparin; NA, not addressed; RR, risk ratio; VTE, venous thromboembolism.
Quality assessment
All studies11–13,16–18 were rated as of a high risk in blinding of participants and personnel because the aspirin was orally taken while LMWH was injected. However, this should not cause the bias in analysis in view of that the outcomes were objectively assessed and the blinding of outcome assessment was well implemented. Bias in baseline characteristics was detected in one study16 in which more patients in the LMWH group suffered from ischemic heart disease and diabetes and the pneumatic compression system was used only in the aspirin group. Figure 2 shows the distribution of bias.
Figure 2.
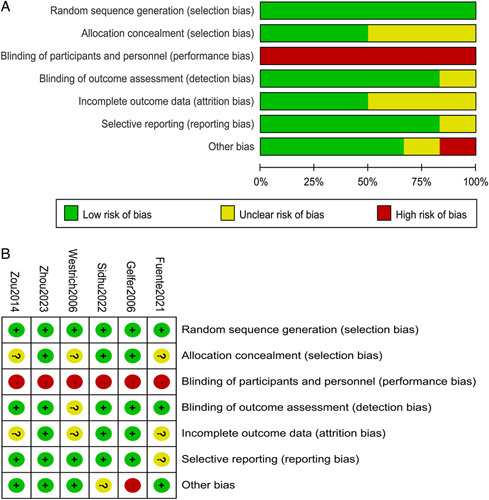
Graph of the risk of bias for the included randomized controlled trials (A); Summary of the risk of bias for the included randomized controlled trials (B).
VTE and bleeding complication
In the included studies comparing aspirin with LMWH, the overall pooled effect showed that aspirin was associated with a statistically significant higher risk in the overall VTE rate (RR 1.46; 95% CI: 1.16–1.84) (Fig. 3).
Figure 3.
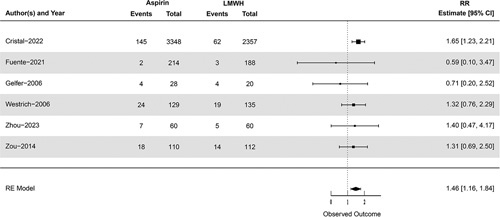
The pooled effect of venous thromboembolism rate.
Four studies reported the bleeding complications rate, and the pooled effect showed that there was no statistically significant difference between the two groups (RR 0.90; 95% CI: 0.71–1.14) (Fig. 4A).
Figure 4.
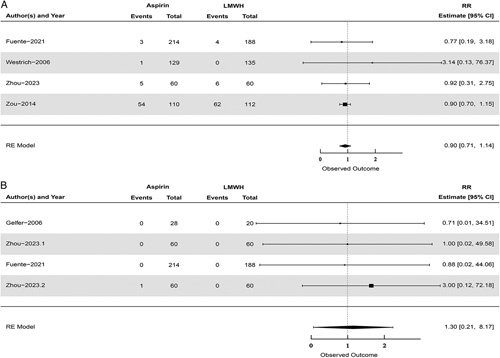
The pooled effect of bleeding complication rate (A). The pooled effect of gastrointestinal bleeding (B).
Subgroup analysis
Subgroup analysis was performed according to the different endpoint of VTE. It showed that there was no statistically significance on DVT (RR 1.22; 95% CI: 0.84–1.75) (Fig. 5A) or PE (RR 0.99; 95% CI: 0.25–3.98) (Fig. 5B).
Figure 5.
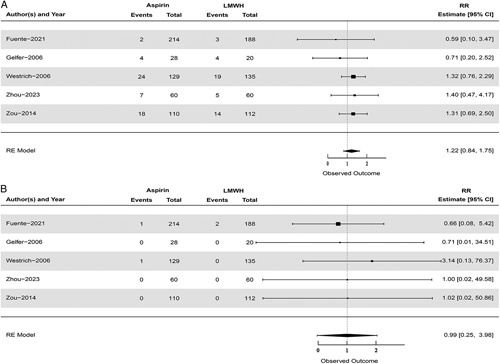
The pooled effect of DVT (A); The pooled effect of PE (B).
As a nonselective cyclooxygenase inhibitor, gastrointestinal bleeding was a hot topic for aspirin. Subgroup analysis was also performed for gastrointestinal bleeding on bleeding complication. The pooled result showed that there was no statistically significance on gastrointestinal bleeding between aspirin and LMWH (RR 1.30; 95% CI: 0.21–8.17) (Fig. 4B).
Discussion
This meta-analysis demonstrated that aspirin could not significantly reduce the risk of VTE through VTE prophylaxis in patients undergoing TKA in comparison with LMWH. There were no differences in the risk of bleeding complications, but cautions must be taken when interpreting the results of bleeding complications. Although there was variation in the duration of medication use among the included studies, the duration of aspirin and LMWH use remained consistent within each study. Furthermore, except for the study conducted by Westrich et al.17, which utilized a relatively higher dosage of aspirin, the other studies employed doses commonly used in clinical practice. Additionally, in the study by Gelfer et al.16, mechanical thromboprophylaxis was only implemented in the aspirin group and not in the LMWH group. In summary, these biases may have favored supporting the use of aspirin, but ultimately, aspirin still showed a statistically significant higher risk of VTE. Therefore, we do not recommend the use of aspirin for VTE prevention following TKA.
A recent meta-analysis10 comparing the clinical effectiveness and safety between aspirin and other anticoagulants indicated that aspirin was not statistically significantly different from other anticoagulants in terms of VTE prophylaxis after total knee and hip arthroplasty. The study combined all other anticoagulants as one comparator versus aspirin, but there was a possibility that some anticoagulants were superior to while others were inferior to aspirin, resulting in an undifferentiated synthesis outcome. The risk of VTE after TKA is deemed 2–5 times higher than that after THA, so combining TKA and THA may exaggerate the actual efficacy of aspirin in TKA. In our meta-analysis, we only compared the clinical outcome between aspirin and LMWH for VTE prophylaxis after TKA. The results showed that aspirin had comparable bleeding complication rates with LMWH but a higher risk of VTE. Therefore, we consider that the current evidence does not support the continued use of aspirin for VTE prophylactic anticoagulation after TKA.
Aspirin, also known as acetylsalicylic acid, inhibits the activity of platelets, which are blood cells that play a crucial role in forming blood clots19. By reducing platelet activity, aspirin helps to prevent the formation of blood clots in the surgical area. Platelets start forming a hemostatic clot within seconds to minutes after joint replacement surgery to stop bleeding and prevent excessive blood loss19,20. The platelets first form a temporary plug, followed by a more stable fibrin clot19,20. The time taken for complete clot formation varies based on factors such as the extent of surgery and individual patient characteristics19–22. Aspirin (75, 100, or 150 mg/d) for 14 days was recommended for TKA, beginning within 24 h postoperatively4,11.
Enoxaparin and Dalteparin are commonly used LMWHs. LMWH, on the other hand, works by inhibiting the activity of several blood clotting factors23. By doing so, it helps to prevent the formation of blood clots in the deep veins of the leg. LMWH also has anti-inflammatory properties that may further reduce the risk of blood clots24. The timing for starting an application to effectively reduce the risk of bleeding depends on the specific application and the patient’s individual circumstances21,22. The exact timing and duration of the application will depend on various factors, including the type of surgery, the patient’s medical history and risk factors for bleeding, and any medications that the patient is taking25. LMWH (40 mg/d) beginning within 24 h postoperatively for 14 days were recommended for TKA11,26. More studies are needed to explore the concrete VTE prophylactic strategy about drug administration time, dose, and duration.
Based on data collected from the English National Health Service, it has been found that LMWH is a more cost-effective option than the new oral anticoagulants for elective total knee replacement27,28. As a matter of fact, LMWH is only ranked second to aspirin in this regard27,28. However, it is worth noting that the results are subject to a high degree of uncertainty28. Aside from the clinical efficacy and cost-effectiveness of chemoprophylaxis regimen, adherence also counts in VTE prophylaxis. As an oral medicine, aspirin can be easily taken for outpatients. In comparison, the administration of LMWH requires daily injections by either the patients themselves or health care professionals, which restricts its use to some degree. An RCT comparing the postdischarge adherence with VTE prophylaxis after orthopedic trauma between aspirin and LMWH showed that the two were comparable in terms of adherence but patients in the LMWH group were more likely to feel hassled of their regimens29. For the analysis of factors which might contribute to the adherence, it was found that younger patients, male patients or patients without insurance were associated with a lower rate of adherence29. It is worth noting that there are some exceptions in the clinical use of LMWH. LMWH cannot be used in patients with renal insufficiency but is recommended for pregnant patients for the prevention and treatment of VTE30. Regarding the timing of anticoagulant administration after TKA, it is important to balance the risk of bleeding with the risk of clotting and more studies are needed to explore the concrete VTE prophylactic strategy about drug administration time, dose, and duration.
There are several limitations in our study. Firstly, not all the incidence rates of DVT, PE, and bleeding complications were available in the included studies, which may have reduced the reliability of the pooled outcomes in subgroup analysis. In the subgroup analysis of different endpoints of VTE, the influential study by Sidhu et al.11 was not included. In the subgroup analysis of gastrointestinal bleeding, three out of four included studies did not report any cases of gastrointestinal bleeding, resulting in only one study being analyzed and an extremely wide credible interval. Secondly, there is heterogeneity in our research. Heterogeneity may arise from variations in aspirin dosage and duration, the utilization of mechanical VTE prophylaxis, and the duration of follow-up in the included studies. Thirdly, the studies included in our analysis did not implement participant blinding, which may introduce a certain unpredictable direction of bias to the results. Lastly, the number of included studies was small, so more high-quality studies are needed to further confirm the efficacy and safety of VTE prophylactic anticoagulation. Considering that most of the included studies were not blinded and the presence of heterogeneity among the studies, we classify the recommendation against using aspirin for VTE prevention following TKA as level Ⅱ evidence. In the future, more research is needed to explore the optimal dosage and duration of prophylactic anticoagulation and evaluate the effectiveness and value of different medications based on this foundation.
Conclusion
In terms of the clinical effectiveness of VTE prophylactic anticoagulation after TKA, aspirin presents an obviously higher risk of VTE in comparison with LMWH. Aspirin and LMWH show comparable outcomes in bleeding complications rates. However, more high-quality studies are needed to further confirm the role of aspirin in prophylactic anticoagulation.
Ethical approval and consent to participate
As the literature included in the meta-analysis got ethics approval, no additional ethics approval was required.
Sources of funding
None.
Author contribution
J.H.M., W.J.L., and S.G.G.: proposed the design, searched the literature, collected, analyzed and interpret the data, and wrote the report; W.J.L., Y.F.X., H.T.: searched the literature, and collected, analyzed and interpreted the data; Y.M.W.: searched the literature, designed the figures and tables, and wrote the report.
Conflicts of interest disclosure
The authors declare that they have no financial conflict of interest with regard to the content of this report.
Research registration unique identifying number (UIN)
Name of the registry: PROSPERO (International prospective register of systematic reviews).
Unique Identifying number or registration ID: CRD42022372717.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=372717
Guarantor
Shuguang Gao.
Data availability statement
All the data is available in the article.
Footnotes
J.M. and W.L. have contributed equally to this work and share first authorship.
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article
Published online 11 August 2023
Contributor Information
Jiahao Meng, Email: 1773834816@qq.com.
Weijie Liu, Email: 1374750551@qq.com.
Yifan Xiao, Email: 568807916@qq.com.
Hang Tang, Email: 1412972206@qq.com.
Yumei Wu, Email: 2648565027@qq.com.
Shuguang Gao, Email: gaoshuguang0341@qq.com.
References
- 1.Marcucci M, Etxeandia-Ikobaltzeta I, Yang S, et al. Benefits and harms of direct oral anticoagulation and low molecular weight heparin for thromboprophylaxis in patients undergoing non-cardiac surgery: systematic review and network meta-analysis of randomised trials. BMJ 2022;376:e066785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewis S, Glen J, Dawoud D, et al. Venous thromboembolism prophylaxis strategies for people undergoing elective total knee replacement: a systematic review and network meta-analysis. Lancet Haematol 2019;6:e530–e539. [DOI] [PubMed] [Google Scholar]
- 3.Hood BR, Cowen ME, Zheng HT, et al. Association of aspirin with prevention of venous thromboembolism in patients after total knee arthroplasty compared with other anticoagulants: a noninferiority analysis. JAMA Surg 2019;154:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence. Venous Thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism: National Guidelines Centre. 2018. Accessed 23 July 2022. https://www.nice.org.uk/guidance/ng89/evidence [PubMed] [Google Scholar]
- 5.Faour M, Piuzzi NS, Brigati DP, et al. Low-dose aspirin is safe and effective for venous thromboembolism prophylaxis following total knee arthroplasty. J Arthroplasty 2018;33(7s):S131–s135. [DOI] [PubMed] [Google Scholar]
- 6.Matzko C, Berliner ZP, Husk G, et al. Equivalent VTE rates after total joint arthroplasty using thromboprophylaxis with aspirin versus potent anticoagulants: retrospective analysis of 4562 cases across a diverse healthcare system. Arthroplasty (London, England) 2021;3:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McHale S, Williams M, O’Mahony C, et al. Should we use dabigatran or aspirin thromboprophylaxis in total hip and knee arthroplasty? A natural experiment. J Orthop 2019;16:563–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Najafi F, Kendal JK, Peterson NV, et al. Low-dose aspirin for venous thromboembolism prophylaxis is associated with lower rates of periprosthetic joint infection after total joint arthroplasty. J Arthroplasty 2022;37:2444–2448.e2441. [DOI] [PubMed] [Google Scholar]
- 9.Tang A, Sicat CS, Singh V, et al. Aspirin use for venous thromboembolism prevention is safe and effective in overweight and obese patients undergoing revision total hip and knee arthroplasty. J Arthroplasty 2021;36(7s):S337–s344. [DOI] [PubMed] [Google Scholar]
- 10.Matharu GS, Kunutsor SK, Judge A, et al. Clinical effectiveness and safety of aspirin for venous thromboembolism prophylaxis after total hip and knee replacement: a systematic review and meta-analysis of randomized clinical trials. JAMA Int Med 2020;180:376–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sidhu VS, Kelly TL, Pratt N, et al. Effect of aspirin vs enoxaparin on symptomatic venous thromboembolism in patients undergoing hip or knee arthroplasty: the CRISTAL randomized trial. JAMA 2022;328:719–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou LB, Wang CC, Zhang LT, et al. Effectiveness of different antithrombotic agents in combination with tranexamic acid for venous thromboembolism prophylaxis and blood management after total knee replacement: a prospective randomized study. BMC Musculoskelet Disord 2023;24:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cortes-De la Fuente AA, Villalobos-Campuzano C, Bucio-Paticio B, et al. Comparative study between enoxaparin and salicylic acetyl acid in antithrombotic prophylaxis for patients undergoing total knee arthroplasty. Acta Ortop Mex 2021;35:163–168. [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gelfer Y, Tavor H, Oron A, et al. Deep vein thrombosis prevention in joint arthroplasties: continuous enhanced circulation therapy vs low molecular weight heparin. J Arthroplasty 2006;21:206–214. [DOI] [PubMed] [Google Scholar]
- 17.Westrich GH, Bottner F, Windsor RE, et al. VenaFlow plus Lovenox vs VenaFlow plus aspirin for thromboembolic disease prophylaxis in total knee arthroplasty. J Arthroplasty 2006;21(6 Suppl 2):139–143. [DOI] [PubMed] [Google Scholar]
- 18.Zou Y, Tian S, Wang Y, et al. Administering aspirin, rivaroxaban and low-molecular-weight heparin to prevent deep venous thrombosis after total knee arthroplasty. Blood Coagul Fibrinolysis 2014;25:660–664. [DOI] [PubMed] [Google Scholar]
- 19.Undas A, Brummel-Ziedins K, Mann KG. Why does aspirin decrease the risk of venous thromboembolism? On old and novel antithrombotic effects of acetyl salicylic acid. J Thromb Haemost 2014;12:1776–1787. [DOI] [PubMed] [Google Scholar]
- 20.Chang JC. Pathogenesis of two faces of DVT: new identity of venous thromboembolism as combined micro-macrothrombosis via unifying mechanism based on “Two-Path Unifying Theory” of hemostasis and “Two-Activation Theory of the Endothelium”. Life (Basel, Switzerland) 2022;12:220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Damnjanović Z, Jovanović M, Stojanović M. Correlation between the climatic factors and the pathogenesis of deep vein thrombosis. Hippokratia 2013;17:203–206. [PMC free article] [PubMed] [Google Scholar]
- 22.Lichota A, Szewczyk EM, Gwozdzinski K. Factors affecting the formation and treatment of thrombosis by natural and synthetic compounds. Int J Mol Sci 2020;21:7975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gray E, Mulloy B, Barrowcliffe TW. Heparin and low-molecular-weight heparin. Thromb Haemost 2008;99:807–818. [DOI] [PubMed] [Google Scholar]
- 24.Vitiello A, Ferrara F. Low molecular weight heparin, anti-inflammatory/immunoregulatory and antiviral effects, a short update. Cardiovasc Drugs Ther 2023;37:277–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Srinivasan D, Watzak B. Anticoagulant use in real time. J Pharm Pract 2013;26:270–279. [DOI] [PubMed] [Google Scholar]
- 26.Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141(2 Suppl):e278S–e325S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kapoor A, Chuang W, Radhakrishnan N, et al. Cost effectiveness of venous thromboembolism pharmacological prophylaxis in total hip and knee replacement: a systematic review. Pharmacoeconomics 2010;28:521–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dawoud DM, Wonderling D, Glen J, et al. Cost-utility analysis of venous thromboembolism prophylaxis strategies for people undergoing elective total hip and total knee replacement surgeries in the english national health service. Front Pharmacol 2018;9:1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haac BE, Van Besien R, O’Hara NN, et al. Post-discharge adherence with venous thromboembolism prophylaxis after orthopedic trauma: results from a randomized controlled trial of aspirin versus low molecular weight heparin. J Trauma Acute Care Surg 2018;84:564–574. [DOI] [PubMed] [Google Scholar]
- 30.Bates SM, Greer IA, Middeldorp S, et al. VTE, thrombophilia, antithrombotic therapy, and pregnancy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141(2 Suppl):e691S–e736S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data is available in the article.


