Abstract
We describe a medial approach to the coronoid where the flexor-pronator mass is released from its humeral origin by creating a proximally based tendinous flap. This technique facilitates access to the coronoid, preservation of the medial collateral ligament origin, and repair of the flexor-pronator mass. This approach has utility for all coronoid fracture variations but especially the O’Driscoll anteromedial subtype 3, which includes fractures of the sublime tubercle, the anteromedial facet, and the coronoid tip.
Key Words: coronoid fracture, elbow dislocation, medial approach elbow, posteromedial rotatory instability
A greater understanding of coronoid fractures and the recognition of the role of the sublime tubercle has improved the treatment of these injuries and the prevention of their sequelae.1,2
In the management of coronoid fractures, the surgical approach should provide ample exposure, allowing access to the coronoid tip, the anteromedial facet, and the sublime tubercle. Access to these fragments is a critical component of achieving elbow stability with anatomic reduction and internal fixation. Difficulties exposing the coronoid include obstruction by the overlying flexor-pronator mass (FPM), the need to preserve the origin of the medial collateral ligament (MCL), and protection of the ulnar nerve.
We describe a medial approach to the coronoid where the FPM is step-cut and reflected from its humeral origin. This facilitates access to the coronoid, preservation of the MCL origin, and the subsequent repair of the FPM. Commonly used medial approaches to the elbow do not describe a complete release of the FPM from its humeral origin. These approaches include the Hotchkiss “over the top”,3 the Taylor-Sham,4,5 the flexor carpi ulnaris (FCU) split,5–8 the extended medial,6,7 and the Smith9 (Table 1). Our approach releases the FPM off the medial epicondyle leaving the ulnar head of the FCU intact. This provides wide exposure to the coronoid for the management of fracture.
TABLE 1.
Summarization of Described Medial Approaches to the Elbow
| References | Approach | Interval | Management of the FCU | Management of the epicondylar origin of the FPM |
|---|---|---|---|---|
| Hotchkiss and Kasparyan3 | “over the top” | FPM & FCU | Intact | Partial release of FPM, retracted anteriorly |
| Taylor et al4, Bates et al5 | Taylor-Sham | Ulna and ulnar head of FCU | Ulnar head is elevated | Preserved |
| Jost et al6, Ring8 | FCU split | Humeral and ulnar heads of FCU | Split | Preserved |
| Jost et al6 | Extended medial | FCU & PL (superficial) and FCU & FDS (deep) | Lifted and retracted posteriorly | Lifted off the capsule |
| Smith et al9 | Smith | FCU & PL (superficial) and FCU & FDS (deep) | Preserved | Partial release of FPM, retracted posteriorly |
| Current work | Wide coronoid | Humeral and ulnar heads of FCU | Split | Elevated |
FCU indicates flexor carpi ulnaris; FDS, flexor digitorum superficialis; FPM, flexor-pronator mass; PL, palmaris longus.
ANATOMY
The coronoid process is a critical multi-planar stabilizer of the elbow. Structurally, the coronoid is a buttress, preventing posterior and medial dislocation of the ulna, and it contributes to valgus stability by being the insertion site of the anterior part of the medial collateral ligament.10 The coronoid functions as the primary restraint to valgus stress and posteromedial instability. The morphology of the coronoid renders it vulnerable to injury as a substantial proportion is offset medially in relation to the long axis of the ulna.11 The sublime tubercle of the coronoid is the insertion for the anterior and transverse bundles of the MCL. Valgus stability is provided by the combined effect of the MCL and the flexor musculature.
SURGICAL TECHNIQUE
A 10-to-12-centimeter (cm) incision is made starting 4 cm proximal to the medial condyle and coursing distally over the FCU and ulnar nerve (Fig. 1A). Full-thickness skin flaps are raised, taking care to preserve the branches of the medial antebrachial cutaneous nerve, which courses across the surgical field.
FIGURE 1.
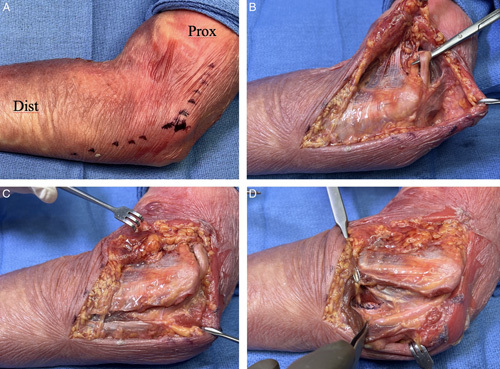
A 10 to 12 cm incision is made that begins 4 cm proximal (P) to the medial condyle (A). The ulnar nerve is identified proximal to the medial condyle (B). The Ligament of Osborne is released, and the humeral and ulnar heads of the flexor capri ulnaris are separated (C). The ulnar nerve is mobilized posteriorly, and the floor of the sheath, which overlies the sublime tubercle is incised. The ulna is exposed, taking care to maintain the insertion of the medial collateral ligament on the sublime tubercle (D).
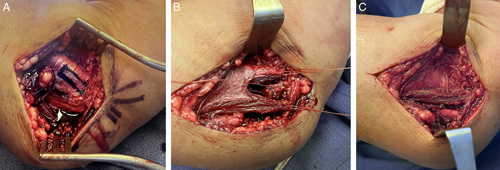
The ulnar nerve is identified and released through the length of the incision (Fig. 1B). Osbourne’s fascia is released, and the 2 heads of the FCU are separated to expose the ulnar nerve (Fig. 1C). In our experience, an incision ~6 cm distal from the medial condyle provides ample access to coronoid fractures and their common variants. In cases with fracture extension distally, surgeon discretion will determine if further distal extension of the approach is warranted. Articular ulnar nerve branches to the elbow may be divided, and attempts are made to preserve proximal motor branches, particularly those to the ulnar head of the FCU. The nerve can be left in situ or moved anteriorly according to need. The ulnar nerve is mobilized from its sheath and the floor of the sheath is longitudinally incised (Fig. 1D). Subperiosteal dissection on the ulna begins distal to the fracture line. The surgeon identifies the MCL insertion onto the sublime tubercle. Often, the entirety of the ligament insertion is contained in the fractured fragment. The fractured fragment is mobilized taking care to maintain its continuity with the ligament insertion. The MCL insertion on the fractured sublime tubercle is traced proximally to its origin at the axilla of the medial condyle. It is imperative that this structure be preserved to prevent subsequent instability. The plane between the MCL and the FPM is developed to separate these structures and ensure the continuity of the MCL. The FPM is released from the medial epicondyle by creating a proximally based tendinous flap (Fig. 2A). This allows reflection of the FPM anteriorly and distally to provide access to fractures of the anteromedial rim and tip of the coronoid (Fig. 2B and C). This release is similar to the technique performed for submuscular ulnar nerve transposition. Direct visualization of the joint surface is achieved by releasing the capsule and opening the medial joint space by applying valgus stress. Here the surgeon can confirm the delineation between the remaining FPM and the MCL insertion onto the sublime tubercle (Fig. 3). Now the fractured fragments can be provisionally pinned, then internal fixation applied (Fig. 4A and B). The FPM is repaired to the tendinous flap on the medial condyle using #2 braided suture or surgeon preference. The first stitch is placed centrally to restore anatomic alignment and length (Fig. 4C), and interrupted figure-of-8 sutures are used to complete the repair (Fig. 4D). Postoperatively, the wrist is splinted in neutral. The initiation of elbow motion is dependent on case variables including patient tolerance. The goal is to begin active/active-assisted elbow motion at ~1 week postoperatively. External loading begins at ~6 weeks.
FIGURE 2.

The flexor-pronator mass is released from the medial condyle by creating a proximally based tendinous flap (A) and elevated to expose the anteromedial facet and tip of the coronoid (B and C).
FIGURE 3.
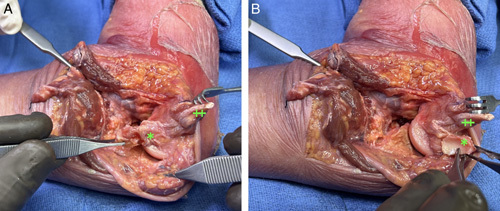
The sublime tubercle fragment (*) is mobilized in continuity with the insertion of the anterior band of the medial collateral ligament (A), which is separated from the flexor-pronator mass (‡) (B).
FIGURE 4.
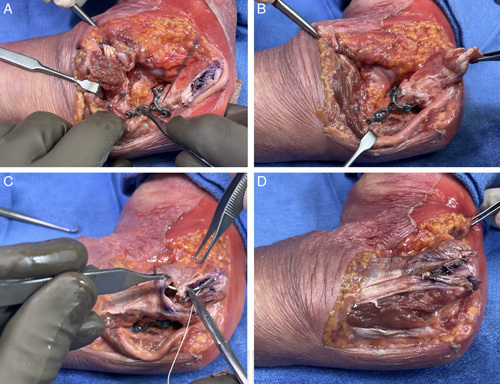
The fractured fragment is provisionally pinned (A), then a medial coronoid plate and screws are applied for fixation (B). The flexor-pronator mass is repaired to the tendinous flap on the medial condyle (C), and the deep muscular layer is closed to protect the ulnar nerve (D).
Our approach provides exposure from the sublime tubercle to the greater sigmoid notch, which facilitates fracture reduction and fixation. Furthermore, the release and reflection of the FPM prevent this structure from interfering with anatomic reduction and internal fixation.
EXPECTED OUTCOMES
When surgically repairing a coronoid fracture, the surgeon will have to determine the best approach. Contributory factors include fracture pattern and the morphology of the coronoid, which can complicate visualization. This technique allows the surgeon to simultaneously access the anterior lip of the coronoid as well as the sublime tubercle in cases where both may require fixation.
Complications
As with most medial elbow approaches, sensory neuroma of the medial antebrachial cutaneous nerve can become problematic, and the pain they cause can impede progress in occupational therapy. These branches should be preserved when possible, and if injured, they should be transected far from the site of wound scar formation. Similarly, the ulnar nerve must be carefully managed to prevent iatrogenic injury. The decision to leave it transposed anteriorly or to replace it in its bed is dependent on the presence of prominent fixation hardware and/or nerve instability. Inadvertent release or transection of the MCL is a risk in all medial approaches to the coronoid, and maintaining anatomical orientation is important to mitigate the risk of this error.
After coronoid fixation, valgus force must be avoided to protect the ligament or avulsion of the anteromedial facet, and varus force must be avoided to prevent displacement of coronoid fragments. Early rehabilitation should avoid shoulder abduction to prevent internal rotation torque on the elbow, and no significant weight should be borne until fracture healing.
Though of theoretical concern, subsequent disruption of the FPM repair has never been an issue in our hands. The side-to-side repair is very stout with consistent healing. It is certainly reasonable to eliminate the tongue-cut and then elevate the entire FPM from the humerus. The repair would utilize suture anchor(s) or transosseous tunnels. However, it is our opinion that the tendinous flap repair may be a more robust construct due to the available surface area of the tendon for reapproximation. Further, this option may be more time efficient. The variables involved in this decision include the preference for a tendon-to-tendon or tendon-to-bone repair and the requisite techniques for each option.
DISCUSSION
There are numerous medial approaches to the elbow, each with described benefits and applications. In general, these approaches do not afford simultaneous wide exposure of the anterior and medial coronoid. The Hotchkiss ‘over the top’ approach excises the medial intermuscular septum and releases the brachialis off the anterior distal humerus.3 The FPM is split in line with its fibers between the FCU and pronator teres, leaving ~1.5 cm of the FCU on the medial epicondyle. The FCU is not released from the medial epicondyle. The Taylor-Sham approach and its variations describe the posterior-to-anterior elevation of the FPM, including the ulnar head of the FCU.4,5 The ulnar nerve is transposed anteriorly. The FCU split approach utilizes the floor of the cubital tunnel and the interval between the 2 heads of the FCU.6,8 The anterior portion of the FCU and FPM are elevated off the medial epicondyle and retracted anteriorly. The FCU is not fully elevated from the medial epicondyle. The extended medial approach uses the raphe between the FCU and palmaris longus superficially, and in the deep layer, the interval between the FCU and FDS.6 As described by Jost et al, the FPM is lifted off the capsule.6 Similar to the extended medial approach, the Smith approach uses the interval between the FCU and palmaris longus superficially, and in the deep layer, the interval between the FCU and FDS.9 The tissue is split to the MCL, working proximally toward the medial epicondyle. There is no release from the medial epicondyle of the humerus. The distal extent of the incision is described as 1 cm distal to the insertion of the ulnar collateral ligament.
Case 1
A 60-year-old male was in a motor vehicle accident, sustaining an elbow fracture and dislocation. The patient was transported to the hospital, where the elbow was reduced and splinted in the emergency room. Investigation revealed a fracture of the anteromedial facet of the coronoid (Fig. 5A and B). A medial coronoid plate and screws were applied for the fixation of the fracture (Fig. 5C and D) using a medial approach with tendinous flap release of the flexor-pronator mass from the medial condyle (Fig. 6).
FIGURE 5.
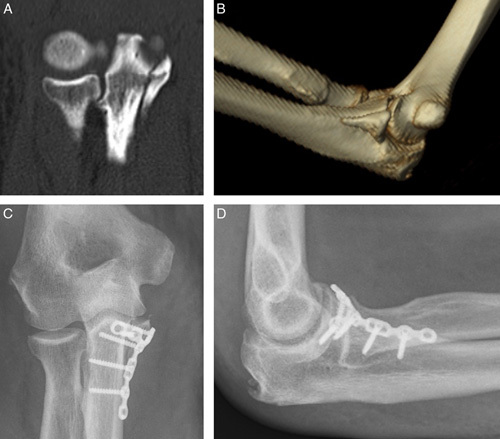
Computed tomography (A) and 3-dimensional reconstruction (B) demonstrating an anteromedial facet fracture of the coronoid. A medial approach to the coronoid was used for internal fixation with a medial coronoid plate (C and D).
FIGURE 6.
The medial approach utilizes a proximally based tendinous flap to release the flexor-pronator mass from the medial condyle (A and B). Following fracture fixation, the flexor-pronator mass is repaired to the tendinous flap (C).
Case 2
A 71-year-old female suffered a ground-level fall and presented with a complex elbow dislocation and medial facet coronoid fracture (Fig. 7A and B). The patient was reduced and splinted, and radiographic investigation demonstrated articular joint fragments of the anteromedial facet of the coronoid. The elbow reduction was nonconcentric with a large medial facet coronoid fracture fragment. A combined lateral and medial approach were utilized to address the joint instability and coronoid fracture. A temporary internal joint stabilizer was placed laterally to maintain concentric elbow reduction and allow early postoperative rehabilitation. A medial coronoid plate and screws were used for internal fixation of the fracture (Fig. 7C and D). At 2 years postoperatively, the patient demonstrated satisfactory recovery with motion comparable to the contralateral arm and no identifiable deficits during activities of daily living.
FIGURE 7.
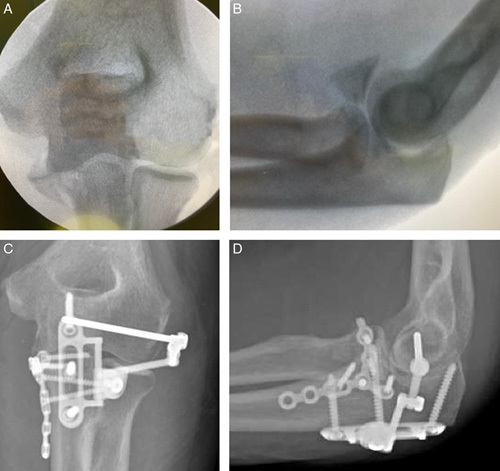
Fluoroscopy demonstrating an unstable elbow with anteromedial facet fracture of the coronoid (A and B). Treatment consisted of an internal joint stabilizer implanted through a lateral approach and fracture fixation with a medial coronoid plate, implanted through a medial approach (C and D).
CONCLUSION
Wide access to the coronoid is limited in the existing medial approaches. Our described approach provides ample exposure across the coronoid from the sublime tubercle to the tip. This approach has utility for all coronoid fracture variations but especially the O’Driscoll anteromedial subtype 3, which includes fractures of the sublime tubercle, the anteromedial facet, and the coronoid tip.
Footnotes
Conflicts of Interest and Source of Funding: J.L.O. discloses patents 8506606 and 8608741 issued to Skeletal Dynamics. Irrevocable trusts of which J.L.O. and his family members are the beneficiaries and own stock in Skeletal Dynamics, and Skeletal Dynamics reimburses expenses when J.L.O. speaks or presents on the company’s behalf. F.R., R.R.L.G., N.A.H., and D.M.M. disclose a relationship with Skeletal Dynamics that includes consulting and speaker’s bureau. D.M.M. discloses a relationship with Axogen that includes the speaker’s bureau. For the remaining author none were declared.
Contributor Information
Jorge L. Orbay, Email: jlorbay@gmail.com.
John J. Heifner, Email: johnjheifner@gmail.com.
Robert R.L. Gray, Email: rgreezy@gmail.com.
Francisco Rubio, Email: frubiomd@gmail.com.
Nathan A. Hoekzema, Email: hoekzema.nathan@gmail.com.
Deana M. Mercer, Email: deanamercermd@gmail.com.
REFERENCES
- 1.O’Driscoll SW. Classification and evaluation of recurrent instability of the elbow. Clin Orthop Relat Res. 2000;370:34–43. [DOI] [PubMed] [Google Scholar]
- 2.O’Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–134. [PubMed] [Google Scholar]
- 3.Hotchkiss RN, Kasparyan NG. The medial “over the top” approach to the elbow. Tech Orthop. 2000;15:105–112. [Google Scholar]
- 4.Taylor TK, Scham SM. A posteromedial approach to the proximal end of the ulna for the internal fixation of olecranon fractures. J Trauma. 1969;9:594–602. [DOI] [PubMed] [Google Scholar]
- 5.Bates T, Lynch TB, Achay J, et al. Medial elbow exposure: Modified Taylor-Scham Versus Flexor Carpi Ulnaris-Split. J Orthop Trauma. 2023;37:e63–e67. [DOI] [PubMed] [Google Scholar]
- 6.Jost B, Benninger E, Erhardt JB, et al. The extended medial elbow approach-a cadaveric study. J Shoulder Elbow Surg. 2015;24:1074–1080. [DOI] [PubMed] [Google Scholar]
- 7.Huang AL, Hackl M, Chan AHW, et al. Medial elbow exposure: an anatomic comparison of 5 approaches. J Shoulder Elbow Surg. 2021;30:512–519. [DOI] [PubMed] [Google Scholar]
- 8.Ring D. Fractures of the coronoid process of the ulna. J Hand Surg Am. 2006;31:1679–1689. [DOI] [PubMed] [Google Scholar]
- 9.Smith GR, Altchek DW, Pagnani MJ, et al. A muscle-splitting approach to the ulnar collateral ligament of the elbow. Neuroanatomy and operative technique. Am J Sports Med. 1996;24:575–580. [DOI] [PubMed] [Google Scholar]
- 10.Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84:547–551. [DOI] [PubMed] [Google Scholar]
- 11.Doornberg JN, de Jong IM, Lindenhovius AL, et al. The anteromedial facet of the coronoid process of the ulna. J Shoulder Elbow Surg. 2007;16:667–670. [DOI] [PubMed] [Google Scholar]


